14efe272c327009919d96e0646514cb2.ppt
- Количество слайдов: 57
 The Implementation of a Gated Stereotactic Technique for Radiation Treatment of the Liver Alison Giddings RTT, MSc Clinical Educator Radiation Therapy Vancouver Centre BCCA May 28 – 30, 2015, Montréal, Québec
The Implementation of a Gated Stereotactic Technique for Radiation Treatment of the Liver Alison Giddings RTT, MSc Clinical Educator Radiation Therapy Vancouver Centre BCCA May 28 – 30, 2015, Montréal, Québec
 Disclosure Statement: No Conflict of Interest I do not have an affiliation, financial or otherwise, with a pharmaceutical company, medical device or communications organization. I have no conflicts of interest to disclose ( i. e. no industry funding received or other commercial relationships). I have no financial relationship or advisory role with pharmaceutical or device-making companies, or CME provider. I will be discussing the results of ____ (“off-label” use), which is currently classified by Health Canada as investigational for the intended use. I will not discuss or describe in my presentation at the meeting the investigational or unlabeled ("off-label") use of a medical device, product, or pharmaceutical that is classified by Health Canada as investigational for the intended use. May 28 – 30, 2015, Montréal, Québec
Disclosure Statement: No Conflict of Interest I do not have an affiliation, financial or otherwise, with a pharmaceutical company, medical device or communications organization. I have no conflicts of interest to disclose ( i. e. no industry funding received or other commercial relationships). I have no financial relationship or advisory role with pharmaceutical or device-making companies, or CME provider. I will be discussing the results of ____ (“off-label” use), which is currently classified by Health Canada as investigational for the intended use. I will not discuss or describe in my presentation at the meeting the investigational or unlabeled ("off-label") use of a medical device, product, or pharmaceutical that is classified by Health Canada as investigational for the intended use. May 28 – 30, 2015, Montréal, Québec
 Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
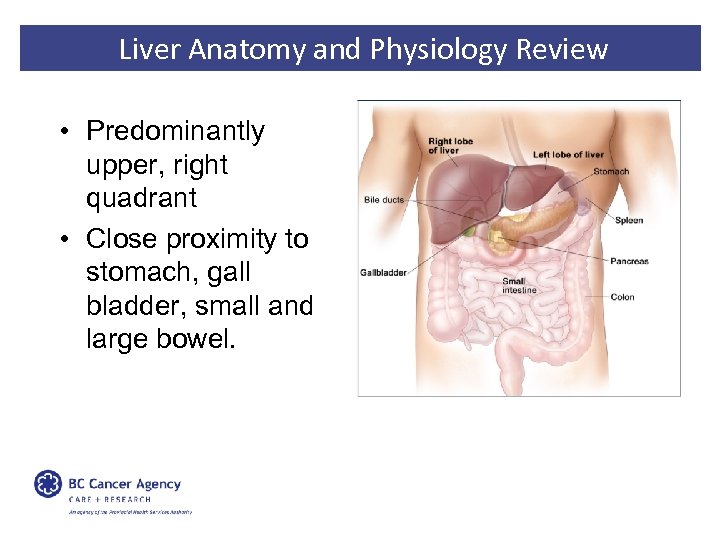 Liver Anatomy and Physiology Review • Predominantly upper, right quadrant • Close proximity to stomach, gall bladder, small and large bowel.
Liver Anatomy and Physiology Review • Predominantly upper, right quadrant • Close proximity to stomach, gall bladder, small and large bowel.
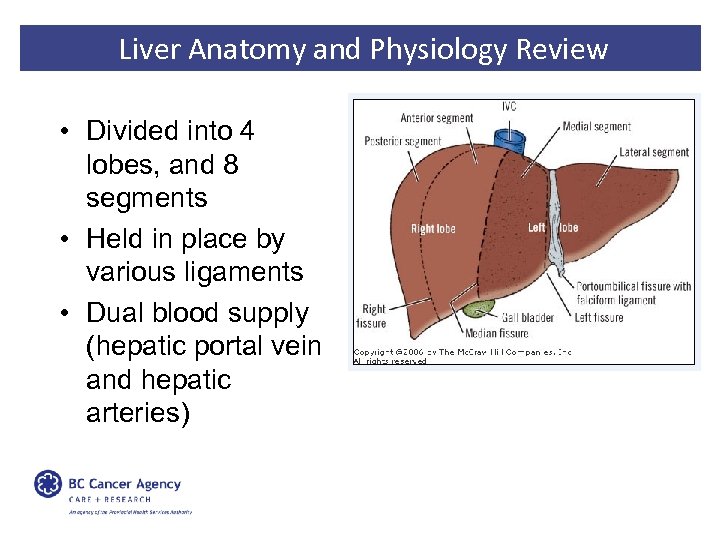 Liver Anatomy and Physiology Review • Divided into 4 lobes, and 8 segments • Held in place by various ligaments • Dual blood supply (hepatic portal vein and hepatic arteries)
Liver Anatomy and Physiology Review • Divided into 4 lobes, and 8 segments • Held in place by various ligaments • Dual blood supply (hepatic portal vein and hepatic arteries)
 Liver Anatomy and Physiology Review • Production – of bile and blood plasma components • Metabolism – of carbohydrates, lipids and proteins • Detoxification – removes toxins from blood • Storage – of vitamins, minerals and nutrients • Immune system – sinusoids lined with Kupffer cells (macrophages)
Liver Anatomy and Physiology Review • Production – of bile and blood plasma components • Metabolism – of carbohydrates, lipids and proteins • Detoxification – removes toxins from blood • Storage – of vitamins, minerals and nutrients • Immune system – sinusoids lined with Kupffer cells (macrophages)
 Primary Liver Cancer • Primary liver cancer is the 6 th most common cancer worldwide • The 2 nd largest contributor to cancer deaths • HCC (hepatocellular carcinoma) is most common type (80%) • Highest rates in Asia and Africa • 5 year survival rate of 14%
Primary Liver Cancer • Primary liver cancer is the 6 th most common cancer worldwide • The 2 nd largest contributor to cancer deaths • HCC (hepatocellular carcinoma) is most common type (80%) • Highest rates in Asia and Africa • 5 year survival rate of 14%
 Hepatocellular Carcinoma Well defined risk factors • Cirrohsis of the liver – Strongest predisposing factor – 80% of HCC pt’s have cirrohsis • Cirrohsis caused by: – Hepatitis B and C virus – Excess alcohol consumption – Nonalcoholic fatty liver disease
Hepatocellular Carcinoma Well defined risk factors • Cirrohsis of the liver – Strongest predisposing factor – 80% of HCC pt’s have cirrohsis • Cirrohsis caused by: – Hepatitis B and C virus – Excess alcohol consumption – Nonalcoholic fatty liver disease
 Hepatocellular Carcinoma Prevention? ? • Vegetable consumption • Coffee and tea consumption • Fish and white meat consumption All associated with significant decreased risk
Hepatocellular Carcinoma Prevention? ? • Vegetable consumption • Coffee and tea consumption • Fish and white meat consumption All associated with significant decreased risk
 Liver Metastases from a variety of cancers • • Colorectal Lung Breast Bladder Esophagus Head and Neck Pancreas Mets from Colorectal ca most significant when considering stereotactic treatment
Liver Metastases from a variety of cancers • • Colorectal Lung Breast Bladder Esophagus Head and Neck Pancreas Mets from Colorectal ca most significant when considering stereotactic treatment
 Colorectal Metastases • The liver is often the first site of mets for colorectal ca – Due to location and venous blood flow to portal vein • Frequently oligometastases – 40% of colorectal patients with mets, have mets confined to the liver
Colorectal Metastases • The liver is often the first site of mets for colorectal ca – Due to location and venous blood flow to portal vein • Frequently oligometastases – 40% of colorectal patients with mets, have mets confined to the liver
 HCC - Management “Gold Standard” – Resection or liver transplantation – Resection if: • • • Normal hepatic function No portal hypertension Sufficient liver remnant Solitary tumour No vascular invasion Plus the “usual suspects” = 70 -80% of patients are not surgical candidates
HCC - Management “Gold Standard” – Resection or liver transplantation – Resection if: • • • Normal hepatic function No portal hypertension Sufficient liver remnant Solitary tumour No vascular invasion Plus the “usual suspects” = 70 -80% of patients are not surgical candidates
 HCC - Management Alternatives to surgery • Embolization – Transarterial chemoembolization (TACE) – Radioembolization • Thermal ablation – Radiofrequency ablation – Cryoablation • Chemical ablation – Percutaneous ethanol injection
HCC - Management Alternatives to surgery • Embolization – Transarterial chemoembolization (TACE) – Radioembolization • Thermal ablation – Radiofrequency ablation – Cryoablation • Chemical ablation – Percutaneous ethanol injection
 HCC - Management And more recently… • Stereotactic radiation therapy! Traditionally, XRT used rarely for short term palliation Advances in immobilization, tumour delineation and target localization Re-examining it’s use
HCC - Management And more recently… • Stereotactic radiation therapy! Traditionally, XRT used rarely for short term palliation Advances in immobilization, tumour delineation and target localization Re-examining it’s use
 Radiation Tx to the Liver What’s the rub? Toxicity Organ motion
Radiation Tx to the Liver What’s the rub? Toxicity Organ motion
 Toxicity • Radiation–induced liver disease (RILD) – Veno-occlusive disease – Ascites, increased weight and girth, hepatomegaly, increased liver enzymes – 4 -8 weeks following radiation • Limited by doses under: – 30 Gy (whole liver) – 35 Gy (two-thirds of liver) – 50 Gy (one-third of liver) • Based on 2 Gy fractions
Toxicity • Radiation–induced liver disease (RILD) – Veno-occlusive disease – Ascites, increased weight and girth, hepatomegaly, increased liver enzymes – 4 -8 weeks following radiation • Limited by doses under: – 30 Gy (whole liver) – 35 Gy (two-thirds of liver) – 50 Gy (one-third of liver) • Based on 2 Gy fractions
 Toxicity • Must also consider adjacent organs – – Stomach Bowel Biliary system Vasculature Obstruction, fistula, ulceration
Toxicity • Must also consider adjacent organs – – Stomach Bowel Biliary system Vasculature Obstruction, fistula, ulceration
 Organ Motion • Liver adjacent to diaphragm • Potentially several cm’s of movement with respiration • Requires large internal target volume (ITV) to treat throughout breathing cycle
Organ Motion • Liver adjacent to diaphragm • Potentially several cm’s of movement with respiration • Requires large internal target volume (ITV) to treat throughout breathing cycle
 Radiation Tx to the Liver What’s the rub? Toxicity Precision → “Stereotactic” Organ motion Accuracy → Gating
Radiation Tx to the Liver What’s the rub? Toxicity Precision → “Stereotactic” Organ motion Accuracy → Gating
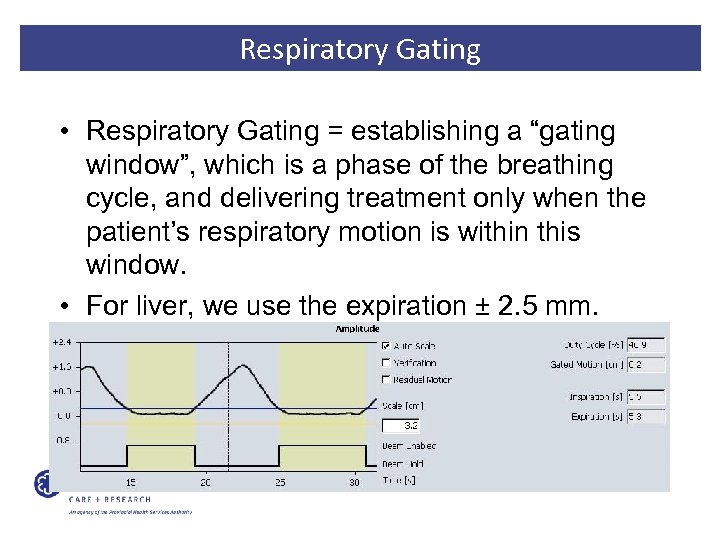 Respiratory Gating • Respiratory Gating = establishing a “gating window”, which is a phase of the breathing cycle, and delivering treatment only when the patient’s respiratory motion is within this window. • For liver, we use the expiration ± 2. 5 mm.
Respiratory Gating • Respiratory Gating = establishing a “gating window”, which is a phase of the breathing cycle, and delivering treatment only when the patient’s respiratory motion is within this window. • For liver, we use the expiration ± 2. 5 mm.
 Stereotactic Radiation Treatment to Liver Various published trials: – 2 year local control 40 -100% – Toxicity ≥Grade 3 for up to 40% (in a few studies) – Various forms of motion management used…or not Bottom line: Can be effective…but be careful!
Stereotactic Radiation Treatment to Liver Various published trials: – 2 year local control 40 -100% – Toxicity ≥Grade 3 for up to 40% (in a few studies) – Various forms of motion management used…or not Bottom line: Can be effective…but be careful!
 Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
 Vancouver
Vancouver
 Vancouver
Vancouver
 BCCA Vancouver Centre
BCCA Vancouver Centre
 Patient Eligibility • HCC or Colorectal mets – Not suitable for surgery – Not suitable for embolization (TACE) or ablation (RFA) • Or incomplete response to these This is also part of the “why”….
Patient Eligibility • HCC or Colorectal mets – Not suitable for surgery – Not suitable for embolization (TACE) or ablation (RFA) • Or incomplete response to these This is also part of the “why”….
 Patient Eligibility • Gold seed fiducial placement – – 3 – 5 fiducials Percutaneously or using endoscopy Healthy tissue within 1 cm of tumour Or within tumour if simultaneous with biopsy • May use existing surgical clips or stents • Need at least 3 for our matching software
Patient Eligibility • Gold seed fiducial placement – – 3 – 5 fiducials Percutaneously or using endoscopy Healthy tissue within 1 cm of tumour Or within tumour if simultaneous with biopsy • May use existing surgical clips or stents • Need at least 3 for our matching software
 Patient Eligibility Mould room
Patient Eligibility Mould room
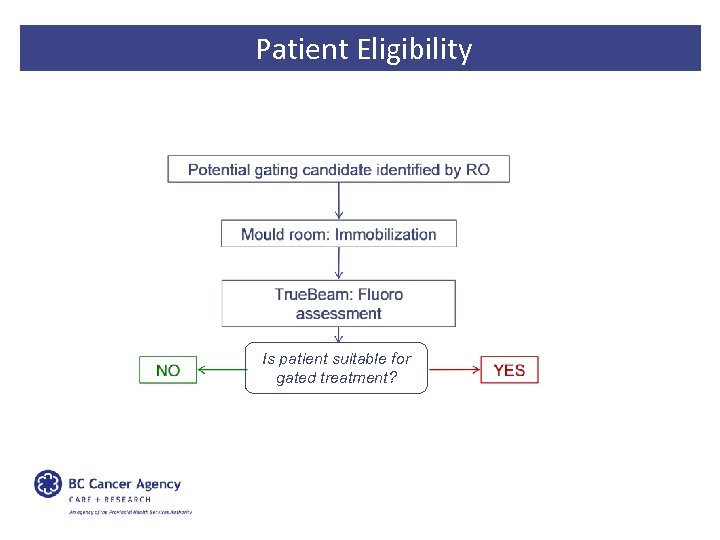 Patient Eligibility Is patient suitable for gated treatment?
Patient Eligibility Is patient suitable for gated treatment?

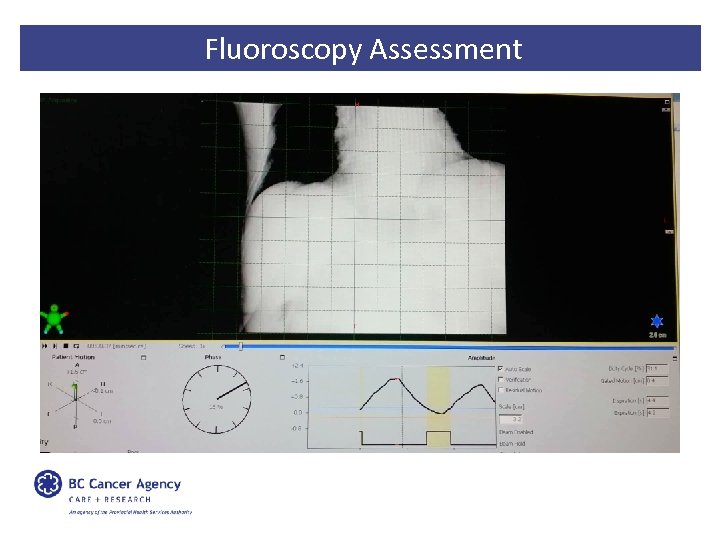 Fluoroscopy Assessment
Fluoroscopy Assessment
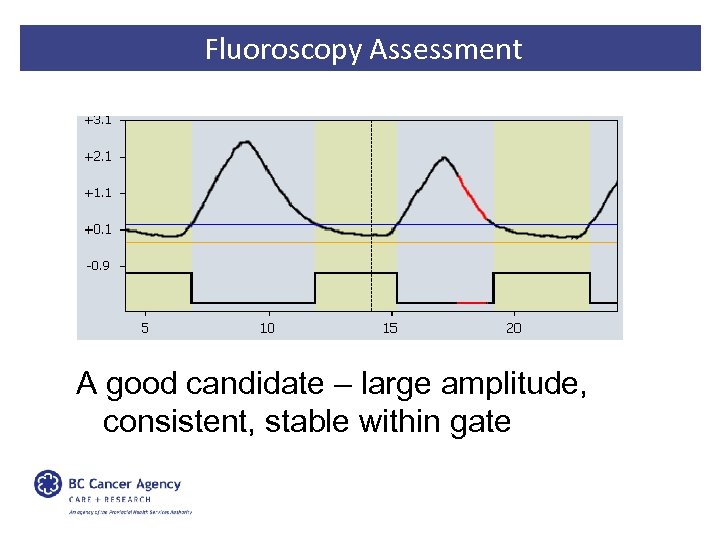
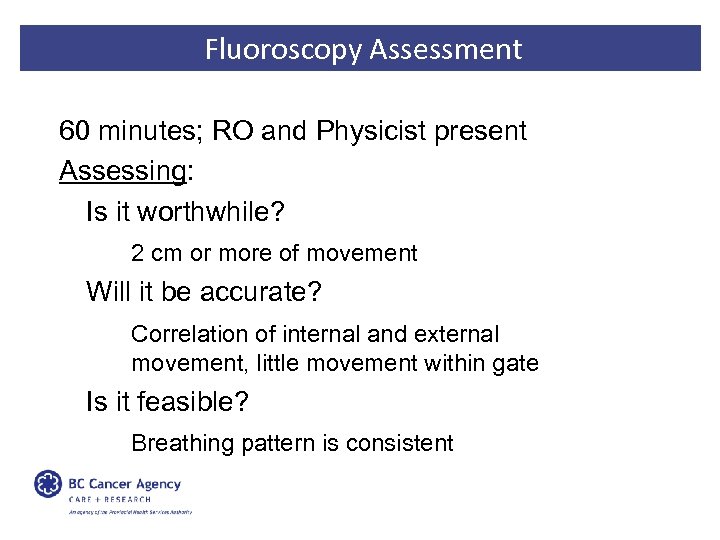 Fluoroscopy Assessment 60 minutes; RO and Physicist present Assessing: Is it worthwhile? 2 cm or more of movement Will it be accurate? Correlation of internal and external movement, little movement within gate Is it feasible? Breathing pattern is consistent
Fluoroscopy Assessment 60 minutes; RO and Physicist present Assessing: Is it worthwhile? 2 cm or more of movement Will it be accurate? Correlation of internal and external movement, little movement within gate Is it feasible? Breathing pattern is consistent
 Fluoroscopy Assessment A good candidate – large amplitude, consistent, stable within gate
Fluoroscopy Assessment A good candidate – large amplitude, consistent, stable within gate
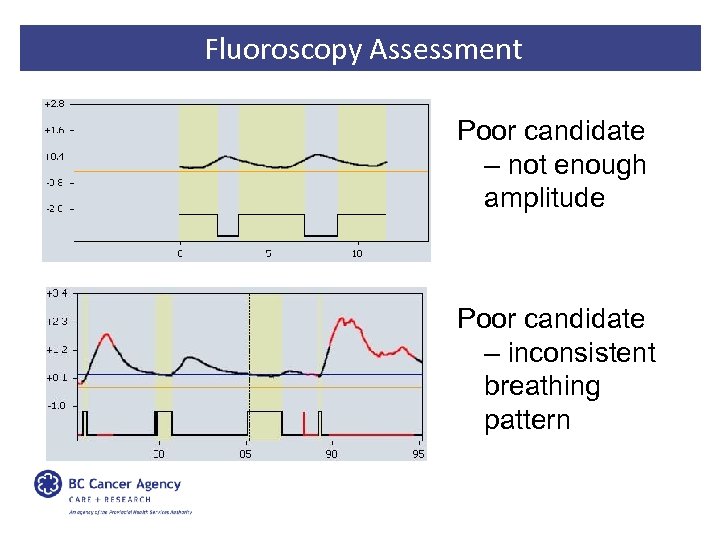 Fluoroscopy Assessment Poor candidate – not enough amplitude Poor candidate – inconsistent breathing pattern
Fluoroscopy Assessment Poor candidate – not enough amplitude Poor candidate – inconsistent breathing pattern
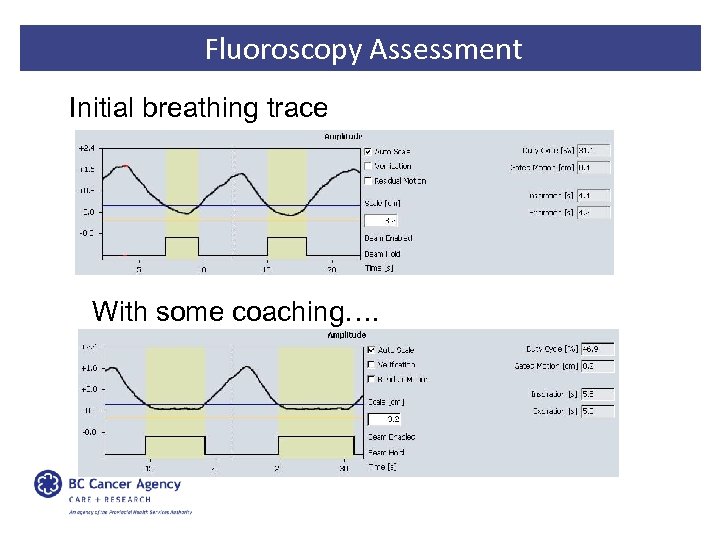 Fluoroscopy Assessment Initial breathing trace With some coaching….
Fluoroscopy Assessment Initial breathing trace With some coaching….
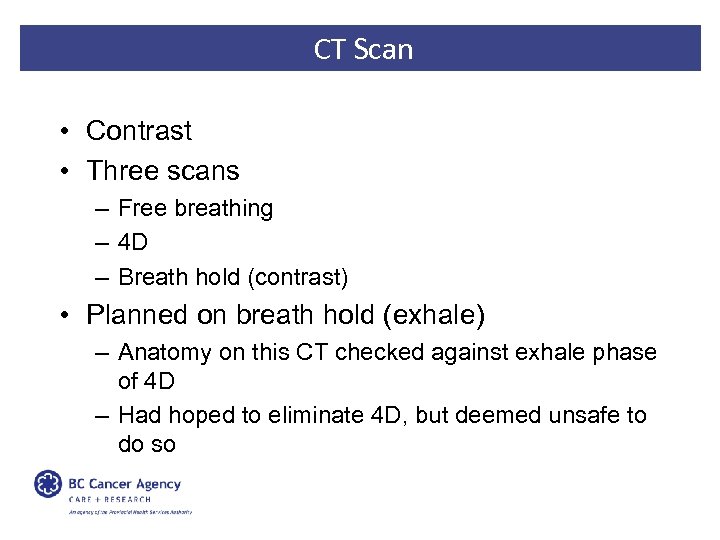 CT Scan • Contrast • Three scans – Free breathing – 4 D – Breath hold (contrast) • Planned on breath hold (exhale) – Anatomy on this CT checked against exhale phase of 4 D – Had hoped to eliminate 4 D, but deemed unsafe to do so
CT Scan • Contrast • Three scans – Free breathing – 4 D – Breath hold (contrast) • Planned on breath hold (exhale) – Anatomy on this CT checked against exhale phase of 4 D – Had hoped to eliminate 4 D, but deemed unsafe to do so
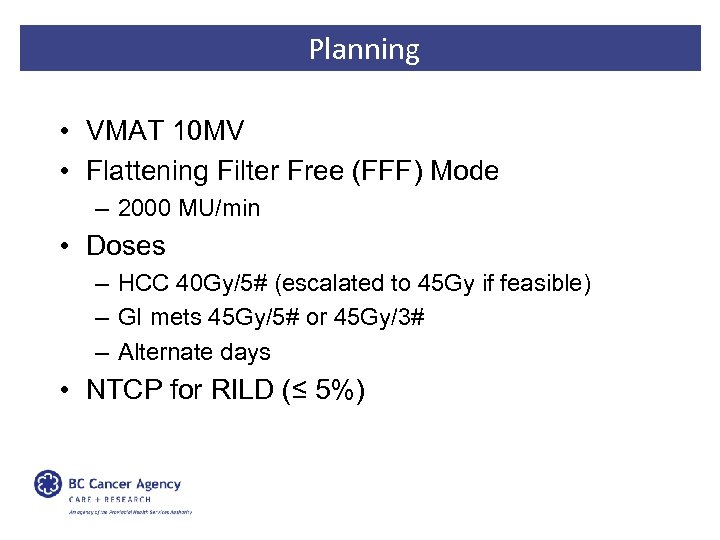 Planning • VMAT 10 MV • Flattening Filter Free (FFF) Mode – 2000 MU/min • Doses – HCC 40 Gy/5# (escalated to 45 Gy if feasible) – GI mets 45 Gy/5# or 45 Gy/3# – Alternate days • NTCP for RILD (≤ 5%)
Planning • VMAT 10 MV • Flattening Filter Free (FFF) Mode – 2000 MU/min • Doses – HCC 40 Gy/5# (escalated to 45 Gy if feasible) – GI mets 45 Gy/5# or 45 Gy/3# – Alternate days • NTCP for RILD (≤ 5%)
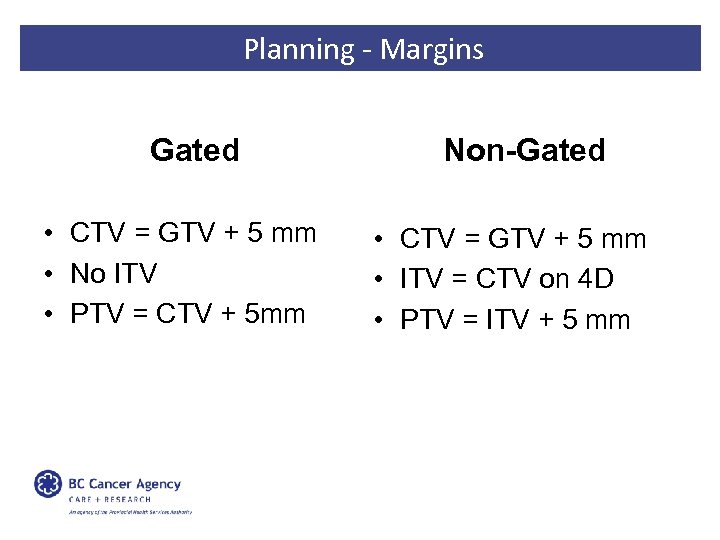 Planning - Margins Gated • CTV = GTV + 5 mm • No ITV • PTV = CTV + 5 mm Non-Gated • CTV = GTV + 5 mm • ITV = CTV on 4 D • PTV = ITV + 5 mm
Planning - Margins Gated • CTV = GTV + 5 mm • No ITV • PTV = CTV + 5 mm Non-Gated • CTV = GTV + 5 mm • ITV = CTV on 4 D • PTV = ITV + 5 mm
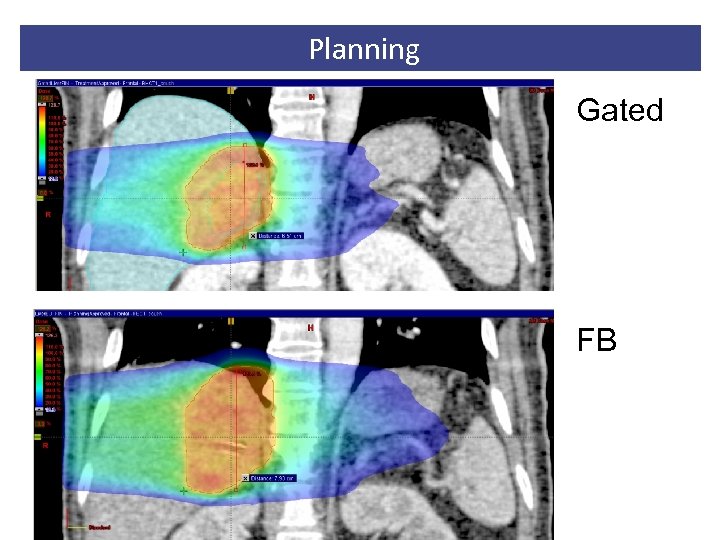 Planning Gated FB
Planning Gated FB
 Treatment
Treatment
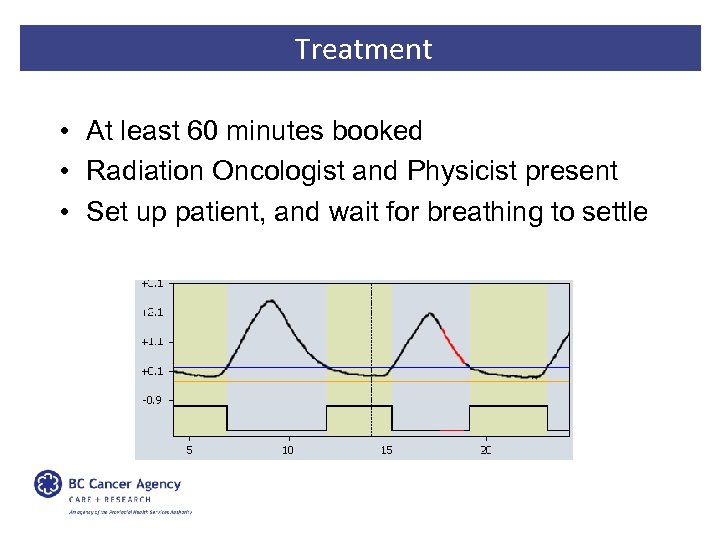 Treatment • At least 60 minutes booked • Radiation Oncologist and Physicist present • Set up patient, and wait for breathing to settle
Treatment • At least 60 minutes booked • Radiation Oncologist and Physicist present • Set up patient, and wait for breathing to settle
 Treatment Orthogonal k. V’s ↓ Anatomy match ↓ Marker match ↓ Move to match ↓ Fluoro confirmation ↓ Treat
Treatment Orthogonal k. V’s ↓ Anatomy match ↓ Marker match ↓ Move to match ↓ Fluoro confirmation ↓ Treat
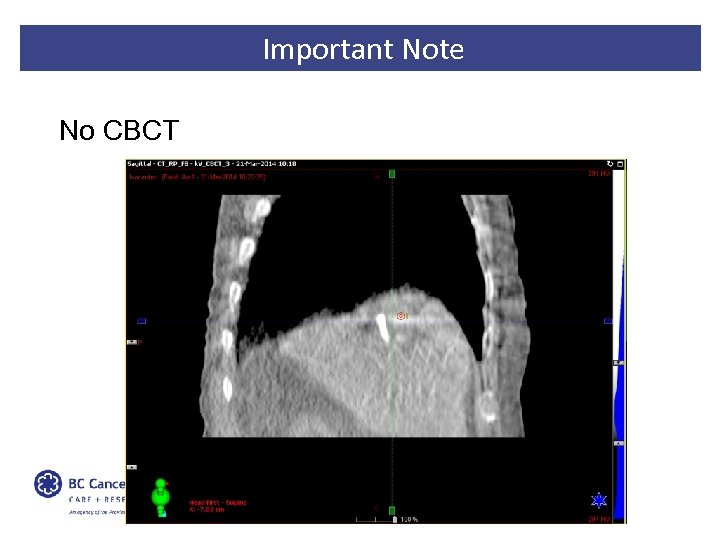 Important Note No CBCT
Important Note No CBCT
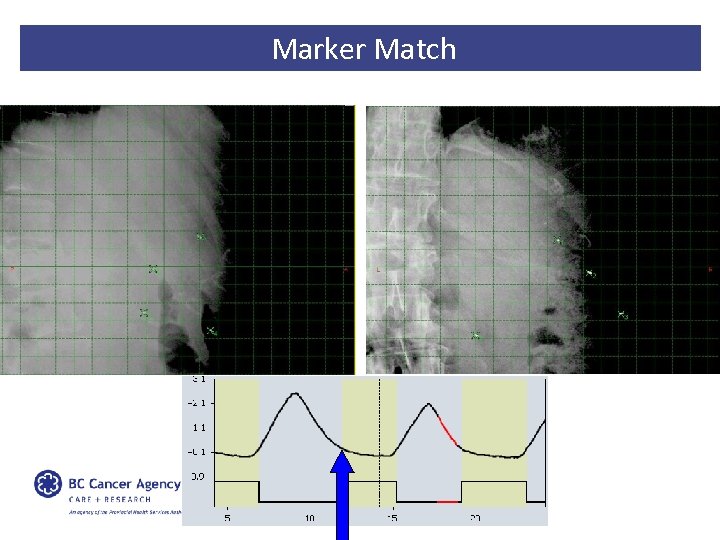 Marker Match
Marker Match
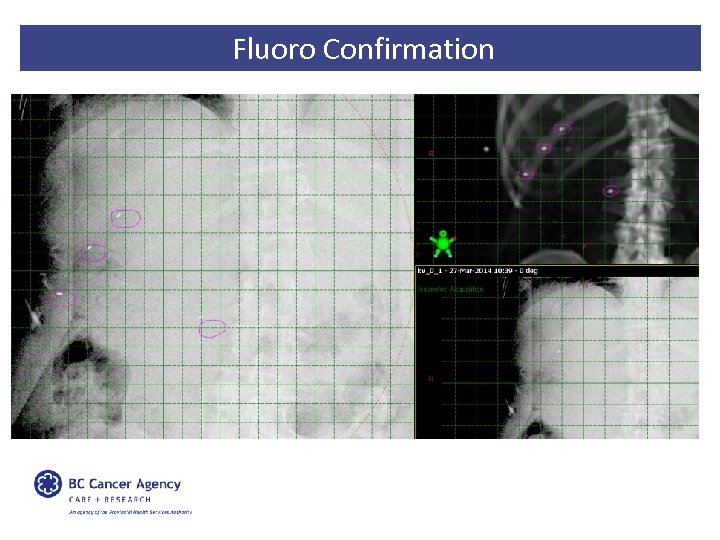 Fluoro Confirmation
Fluoro Confirmation
 Treatment
Treatment
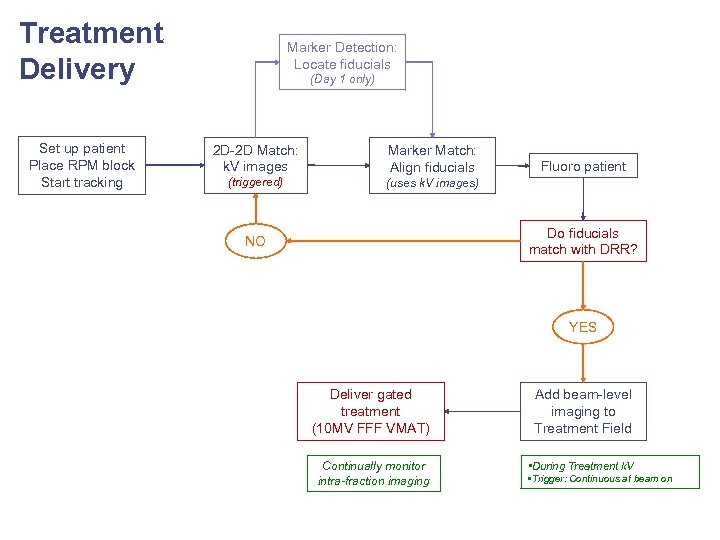 Treatment Delivery Set up patient Place RPM block Start tracking Marker Detection: Locate fiducials (Day 1 only) 2 D-2 D Match: k. V images Marker Match: Align fiducials (triggered) (uses k. V images) Fluoro patient Do fiducials match with DRR? NO YES Deliver gated treatment (10 MV FFF VMAT) Add beam-level imaging to Treatment Field Continually monitor intra-fraction imaging • During Treatment k. V • Trigger: Continuous at beam on
Treatment Delivery Set up patient Place RPM block Start tracking Marker Detection: Locate fiducials (Day 1 only) 2 D-2 D Match: k. V images Marker Match: Align fiducials (triggered) (uses k. V images) Fluoro patient Do fiducials match with DRR? NO YES Deliver gated treatment (10 MV FFF VMAT) Add beam-level imaging to Treatment Field Continually monitor intra-fraction imaging • During Treatment k. V • Trigger: Continuous at beam on
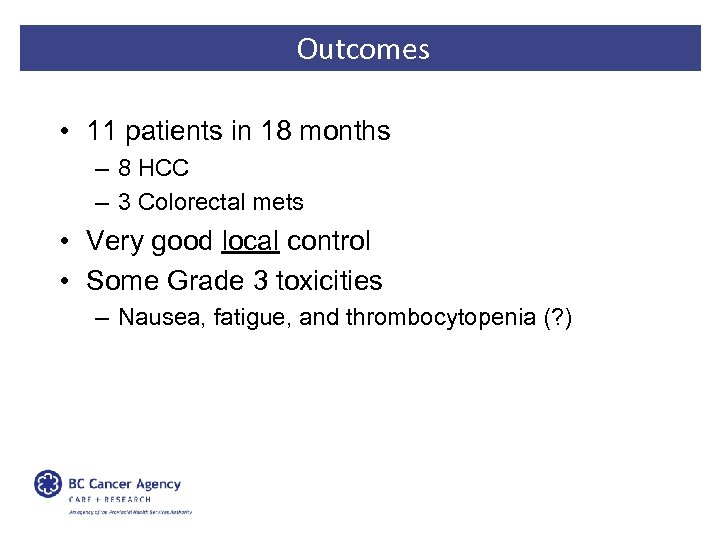 Outcomes • 11 patients in 18 months – 8 HCC – 3 Colorectal mets • Very good local control • Some Grade 3 toxicities – Nausea, fatigue, and thrombocytopenia (? )
Outcomes • 11 patients in 18 months – 8 HCC – 3 Colorectal mets • Very good local control • Some Grade 3 toxicities – Nausea, fatigue, and thrombocytopenia (? )
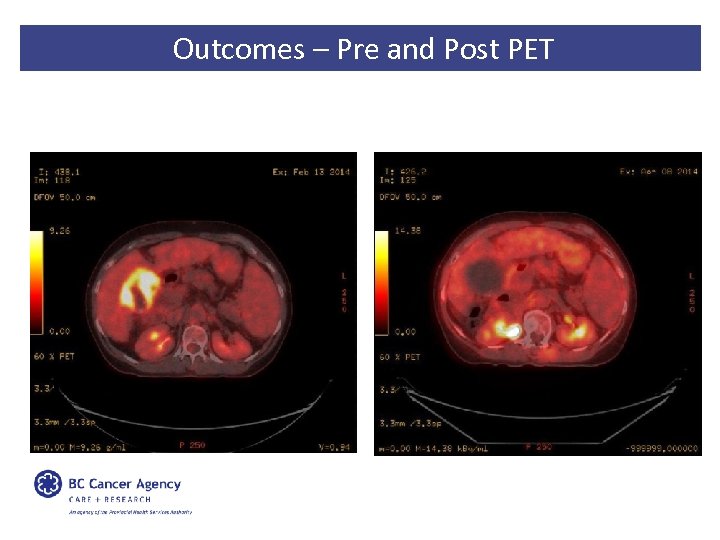 Outcomes – Pre and Post PET
Outcomes – Pre and Post PET
 Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
Outline • Context – – Anatomy and Physiology Tumours of the liver Management of liver tumours Challenges of RT to liver • Vancouver Centre’s Liver Gating technique • Implementation Considerations
 Implementation Considerations • Training – Time booked on unit – Detailed procedure – Timing of training • Education – Invest in more general education Ø Create buy-in, engage staff
Implementation Considerations • Training – Time booked on unit – Detailed procedure – Timing of training • Education – Invest in more general education Ø Create buy-in, engage staff
 Implementation Considerations • Fluoroscopy – Assessment – Different mindset for RT’s • Breath coaching – Too little vs too much – Various tools available • Patient suitability
Implementation Considerations • Fluoroscopy – Assessment – Different mindset for RT’s • Breath coaching – Too little vs too much – Various tools available • Patient suitability
 Implementation Considerations Resource Use Patient Outcomes Innovation Equality
Implementation Considerations Resource Use Patient Outcomes Innovation Equality
 Implementation Considerations Frequency Expertise
Implementation Considerations Frequency Expertise
 Implementation Considerations • Communication is key! • Great opportunity for interdisciplinary collaboration
Implementation Considerations • Communication is key! • Great opportunity for interdisciplinary collaboration
 Acknowledgements • Thank you very much to those that helped: – – – Richard Lee Ph. D FCCPM Moira Pearson MSc, MCCPM Cathy Crumley ACT, CMD Dr. Roy Ma Jenny Soo ACT, MEd • Thank you to the CAMRT for inviting me!
Acknowledgements • Thank you very much to those that helped: – – – Richard Lee Ph. D FCCPM Moira Pearson MSc, MCCPM Cathy Crumley ACT, CMD Dr. Roy Ma Jenny Soo ACT, MEd • Thank you to the CAMRT for inviting me!
 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Dawood O, Mahadevan A, Goodman K. Stereotactic body radiation therapy for liver metastases. European Journal of Cancer. 2009; 45: 2947 -2959. Tinkle CL, Haas-Kogan D. Hepatocellular carcinoma: natural history, current management and emerging tools. Biologics: Targets and Therapy; 2012; 6: 207 -219. Yang Y, et al. Increased intake of vegetables, but not fruit, reduces risk for hepatocellular carcinoma: a meta-analysis. Gastoenterology. 2014; 147(5): 1031 -42. Bravi F, et al. Coffee reduces risk for hepatocellular carcinoma: an updated meta-analysis. Clin Gastroenterol Hepatol. 2013; 11(11): 1413 -1421. Luo J, et al. Systematic review with meta-analysis: meat consumption and the risk of hepatocellular carcinoma. Aliment Pharmacol Ther. 2014; 39(9): 913 -22. Kennedy A. Radioembolization of hepatic tumors. J Gastrointest Oncol. 2014; 5(3): 178 -189. Mc. Glynn KA, et al. Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 2015; 19: 223 -238. Habib A, et al. Locoregional therapy of hepatocellular carcinoma. Clin Liv Dis. 2015; 19: 401 -420. Simpson HN and Mc. Guire BM. Screening and detection of hepatocellular carcinoma. Clin Liver Dis. 2015; 19: 295 -307. Addissie BD and Roberts LR. Classification and staging of hepatocellular carcinoma: and aid to clinical decisionmaking. Clin Liver Dis. 2015; 19: 277 -294. Martin A, Gaya A. Stereotactic body radiotherapy: a review. Clinical Oncology. 2010; 22: 157 -172. Fong Y, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 cases. Ann Surg. 1999; 230: 309 -321. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003; 362: 1907 -17. Yamashita H, et al. Survival outcomes after stereotactic body radiotherapy for 79 Japanese patients with hepatocellular carcinoma. Journal of Radiation Research. 2015; 56(3): 561 -567. Kalogeridi A, et al. Role of radiotherapy in the management of hepatocellular carcinoma: a systematic review. World J Hepatol. 2015; 7(1): 101 -112.
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Dawood O, Mahadevan A, Goodman K. Stereotactic body radiation therapy for liver metastases. European Journal of Cancer. 2009; 45: 2947 -2959. Tinkle CL, Haas-Kogan D. Hepatocellular carcinoma: natural history, current management and emerging tools. Biologics: Targets and Therapy; 2012; 6: 207 -219. Yang Y, et al. Increased intake of vegetables, but not fruit, reduces risk for hepatocellular carcinoma: a meta-analysis. Gastoenterology. 2014; 147(5): 1031 -42. Bravi F, et al. Coffee reduces risk for hepatocellular carcinoma: an updated meta-analysis. Clin Gastroenterol Hepatol. 2013; 11(11): 1413 -1421. Luo J, et al. Systematic review with meta-analysis: meat consumption and the risk of hepatocellular carcinoma. Aliment Pharmacol Ther. 2014; 39(9): 913 -22. Kennedy A. Radioembolization of hepatic tumors. J Gastrointest Oncol. 2014; 5(3): 178 -189. Mc. Glynn KA, et al. Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis. 2015; 19: 223 -238. Habib A, et al. Locoregional therapy of hepatocellular carcinoma. Clin Liv Dis. 2015; 19: 401 -420. Simpson HN and Mc. Guire BM. Screening and detection of hepatocellular carcinoma. Clin Liver Dis. 2015; 19: 295 -307. Addissie BD and Roberts LR. Classification and staging of hepatocellular carcinoma: and aid to clinical decisionmaking. Clin Liver Dis. 2015; 19: 277 -294. Martin A, Gaya A. Stereotactic body radiotherapy: a review. Clinical Oncology. 2010; 22: 157 -172. Fong Y, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 cases. Ann Surg. 1999; 230: 309 -321. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003; 362: 1907 -17. Yamashita H, et al. Survival outcomes after stereotactic body radiotherapy for 79 Japanese patients with hepatocellular carcinoma. Journal of Radiation Research. 2015; 56(3): 561 -567. Kalogeridi A, et al. Role of radiotherapy in the management of hepatocellular carcinoma: a systematic review. World J Hepatol. 2015; 7(1): 101 -112.


