724a2973c7a446f6fed0cae5d30c1f9c.ppt
- Количество слайдов: 66
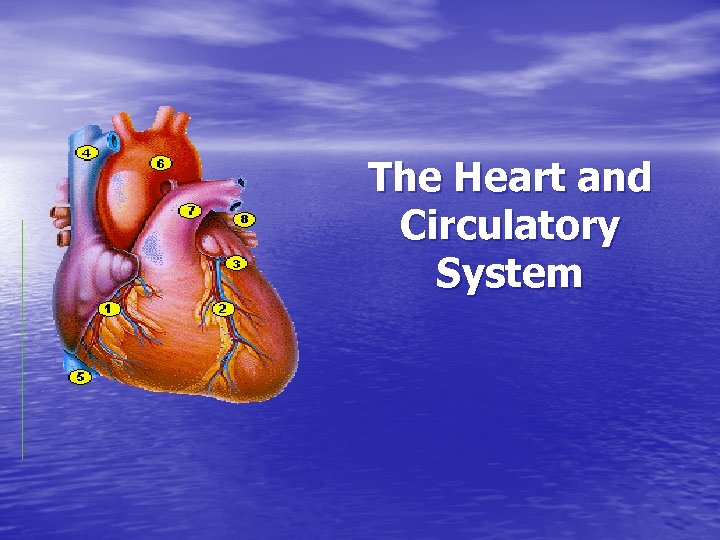 The Heart and Circulatory System
The Heart and Circulatory System
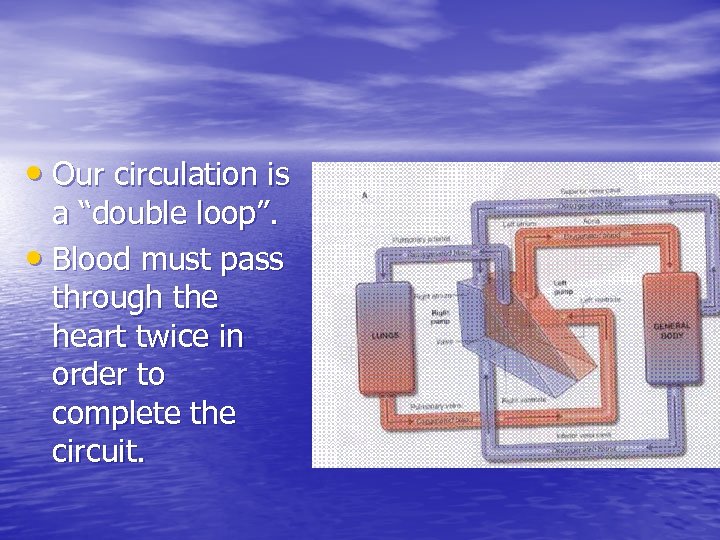 • Our circulation is a “double loop”. • Blood must pass through the heart twice in order to complete the circuit.
• Our circulation is a “double loop”. • Blood must pass through the heart twice in order to complete the circuit.
 THE HEART • The APEX of the heart is where the APICAL • • HEARTBEAT can be heart. It is in the 5 th intercostal space, about 4” (10 cm) to the left, midclavicular. The superior left corner is deep to costal cartilage #2, 1” to the left of midsternum. The inferior right corner is 1” to the right of midsternal, deep to costal cartilage #6.
THE HEART • The APEX of the heart is where the APICAL • • HEARTBEAT can be heart. It is in the 5 th intercostal space, about 4” (10 cm) to the left, midclavicular. The superior left corner is deep to costal cartilage #2, 1” to the left of midsternum. The inferior right corner is 1” to the right of midsternal, deep to costal cartilage #6.
 • The final placement of the heart would 1. 2. 3. require an axis placed: Tilted to the left Tilted anteriorly Rotated so the anterior side is to the left.
• The final placement of the heart would 1. 2. 3. require an axis placed: Tilted to the left Tilted anteriorly Rotated so the anterior side is to the left.
 Heart Chambers • Anatomically, the heart has 4 chambers. • Functionally, the heart has 2 chambers or pump circuits.
Heart Chambers • Anatomically, the heart has 4 chambers. • Functionally, the heart has 2 chambers or pump circuits.
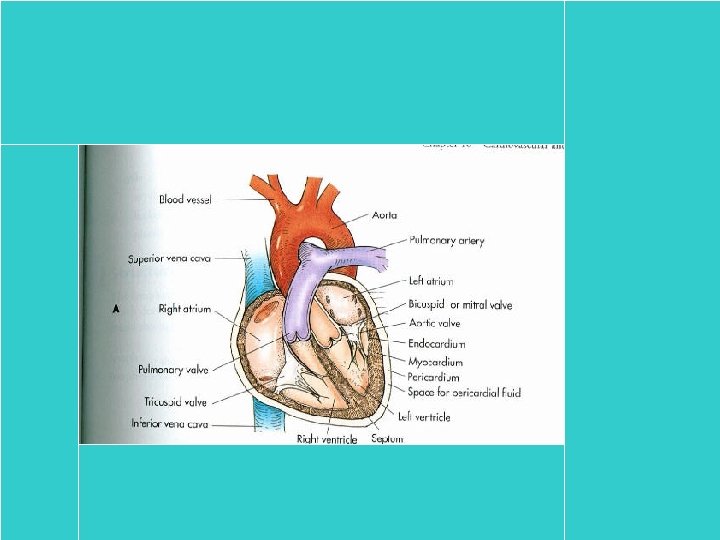
 • The top chambers are ATRIA (singular- atrium). • The bottom chambers are VENTRICLES. • The walls of the atrium are much thinner compared with the ventricles.
• The top chambers are ATRIA (singular- atrium). • The bottom chambers are VENTRICLES. • The walls of the atrium are much thinner compared with the ventricles.
 • Topograhically, there is a small flap of tissue called the AURICLE. • Connected to the chambers are large vessels: vena cavae, pulmonary arteries or trunk, pulmonary veins, and the aorta.
• Topograhically, there is a small flap of tissue called the AURICLE. • Connected to the chambers are large vessels: vena cavae, pulmonary arteries or trunk, pulmonary veins, and the aorta.
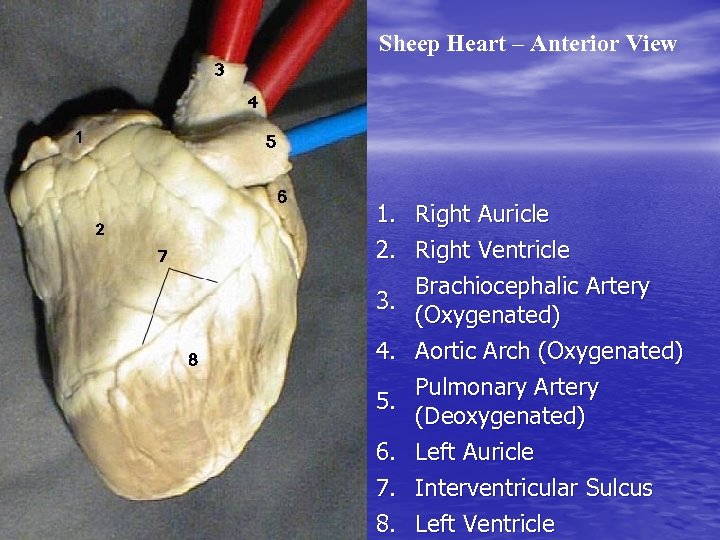 Sheep Heart – Anterior View 1. Right Auricle 2. Right Ventricle Brachiocephalic Artery 3. (Oxygenated) 4. Aortic Arch (Oxygenated) Pulmonary Artery 5. (Deoxygenated) 6. Left Auricle 7. Interventricular Sulcus 8. Left Ventricle
Sheep Heart – Anterior View 1. Right Auricle 2. Right Ventricle Brachiocephalic Artery 3. (Oxygenated) 4. Aortic Arch (Oxygenated) Pulmonary Artery 5. (Deoxygenated) 6. Left Auricle 7. Interventricular Sulcus 8. Left Ventricle
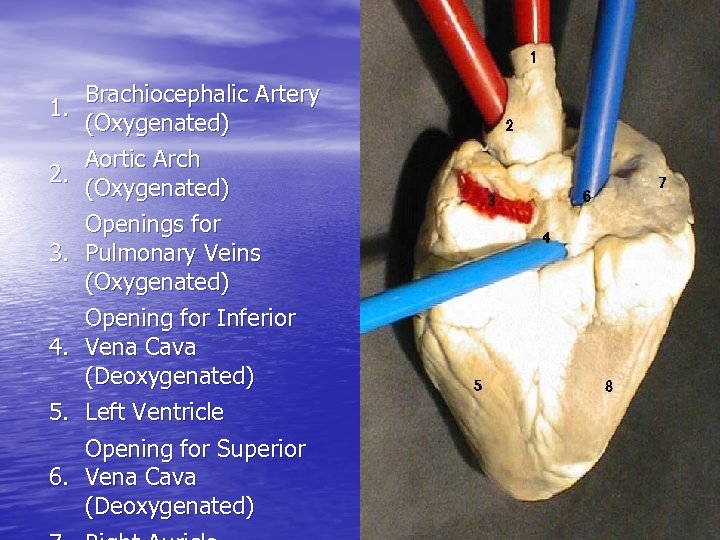 1. 2. 3. 4. 5. Brachiocephalic Artery (Oxygenated) Aortic Arch (Oxygenated) Openings for Pulmonary Veins (Oxygenated) Opening for Inferior Vena Cava (Deoxygenated) Left Ventricle Opening for Superior 6. Vena Cava (Deoxygenated)
1. 2. 3. 4. 5. Brachiocephalic Artery (Oxygenated) Aortic Arch (Oxygenated) Openings for Pulmonary Veins (Oxygenated) Opening for Inferior Vena Cava (Deoxygenated) Left Ventricle Opening for Superior 6. Vena Cava (Deoxygenated)
 • If we look at the heart from the anterior side, we the right side of the heart. • Blood returns to the heart (right atrium) via the SUPERIOR and INFERIOR VENA CAVAE and CORONARY SINUS.
• If we look at the heart from the anterior side, we the right side of the heart. • Blood returns to the heart (right atrium) via the SUPERIOR and INFERIOR VENA CAVAE and CORONARY SINUS.
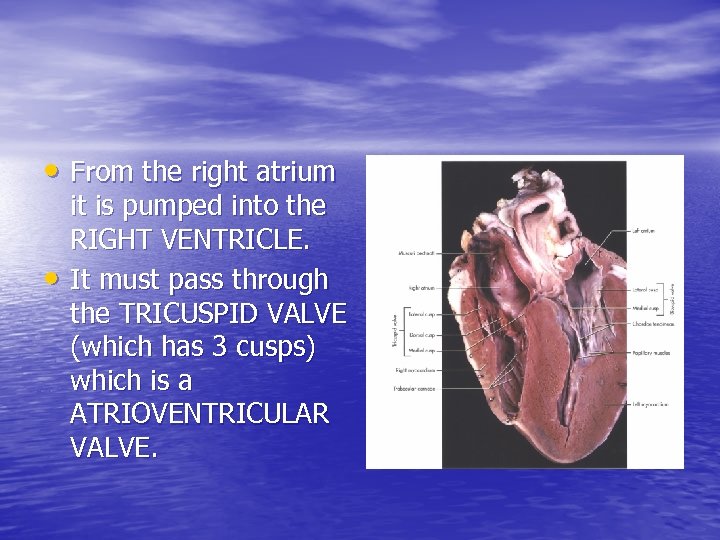 • From the right atrium • it is pumped into the RIGHT VENTRICLE. It must pass through the TRICUSPID VALVE (which has 3 cusps) which is a ATRIOVENTRICULAR VALVE.
• From the right atrium • it is pumped into the RIGHT VENTRICLE. It must pass through the TRICUSPID VALVE (which has 3 cusps) which is a ATRIOVENTRICULAR VALVE.
 • From the right ventricle, the blood then passes through the PULMONARY SEMILUNAR VALVE and into the PULMONARY TRUNK. • The pulmonary trunk carries blood to the lungs for re-oxygenation in the alveoli.
• From the right ventricle, the blood then passes through the PULMONARY SEMILUNAR VALVE and into the PULMONARY TRUNK. • The pulmonary trunk carries blood to the lungs for re-oxygenation in the alveoli.
 • All the valves are made of connective tissue and function to prevent backflow of blood. • Problems with the valves cause a disorder called PROLAPSE or MURMUR.
• All the valves are made of connective tissue and function to prevent backflow of blood. • Problems with the valves cause a disorder called PROLAPSE or MURMUR.
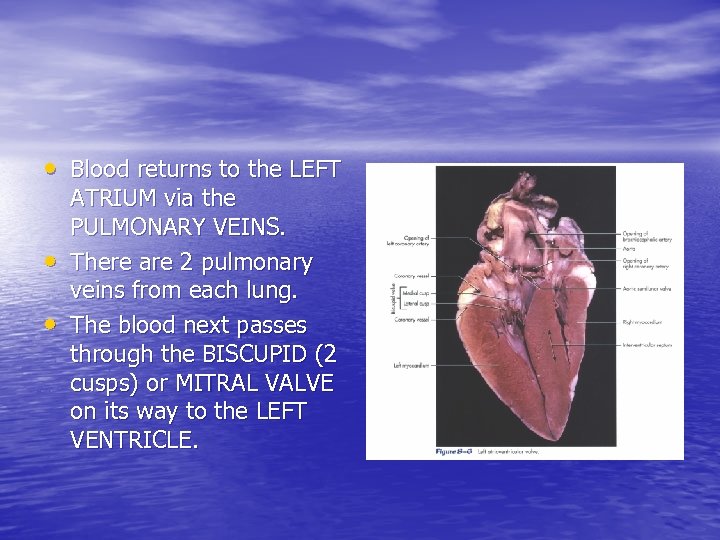 • Blood returns to the LEFT • • ATRIUM via the PULMONARY VEINS. There are 2 pulmonary veins from each lung. The blood next passes through the BISCUPID (2 cusps) or MITRAL VALVE on its way to the LEFT VENTRICLE.
• Blood returns to the LEFT • • ATRIUM via the PULMONARY VEINS. There are 2 pulmonary veins from each lung. The blood next passes through the BISCUPID (2 cusps) or MITRAL VALVE on its way to the LEFT VENTRICLE.
 • From the left ventricle, blood passes through the AORTIC SEMILUNAR VALVE into the AORTA. • To remember that the TRICUSPID VALVE comes before the BICUSPID VALVE, remember the saying: “Try before you buy”
• From the left ventricle, blood passes through the AORTIC SEMILUNAR VALVE into the AORTA. • To remember that the TRICUSPID VALVE comes before the BICUSPID VALVE, remember the saying: “Try before you buy”
 VALVES • The valves open passively during ventricular relaxation. • They close passively during ventricular contraction. • The CHORDAE TENDINEAE connect the edge of the AV valve to the PAPILLARY MUSCLE.
VALVES • The valves open passively during ventricular relaxation. • They close passively during ventricular contraction. • The CHORDAE TENDINEAE connect the edge of the AV valve to the PAPILLARY MUSCLE.
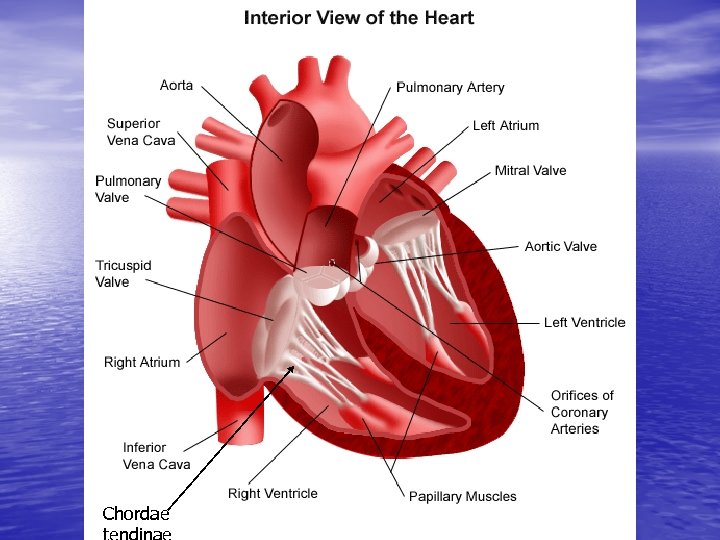 Chordae
Chordae
 • These muscles prevent the valves from being forced closed in reverse. • The chords contract when the papillary muscles pull on them. • The papillary muscles DO NOT cause the valves to open or close.
• These muscles prevent the valves from being forced closed in reverse. • The chords contract when the papillary muscles pull on them. • The papillary muscles DO NOT cause the valves to open or close.
 • The SEMILUNAR VALVES are found between the ventricles and the large arteries leaving the ventricles. • They are TRICUSPID in structure. Heart sounds are caused by the closing of these valves.
• The SEMILUNAR VALVES are found between the ventricles and the large arteries leaving the ventricles. • They are TRICUSPID in structure. Heart sounds are caused by the closing of these valves.
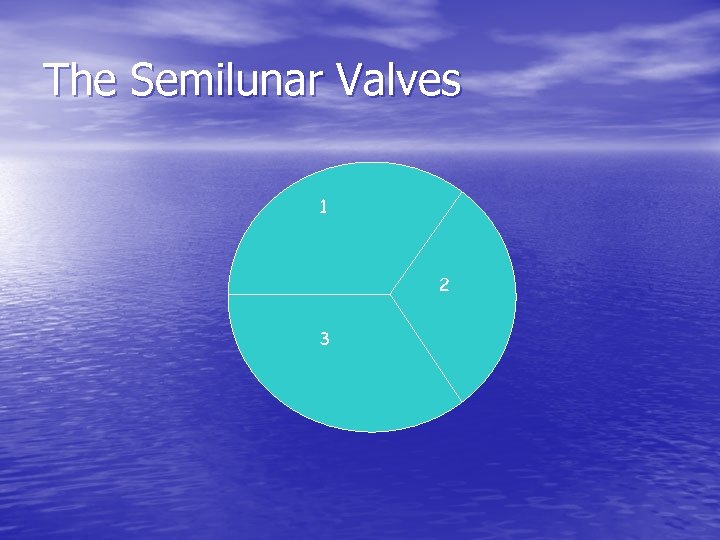 The Semilunar Valves 1 2 3
The Semilunar Valves 1 2 3
 • SUMMARY: 4 chambers 4 valves 4 vessels ARTERIES=carry blood AWAY from the heart. VEINS = carry blood TOWARD the heart.
• SUMMARY: 4 chambers 4 valves 4 vessels ARTERIES=carry blood AWAY from the heart. VEINS = carry blood TOWARD the heart.
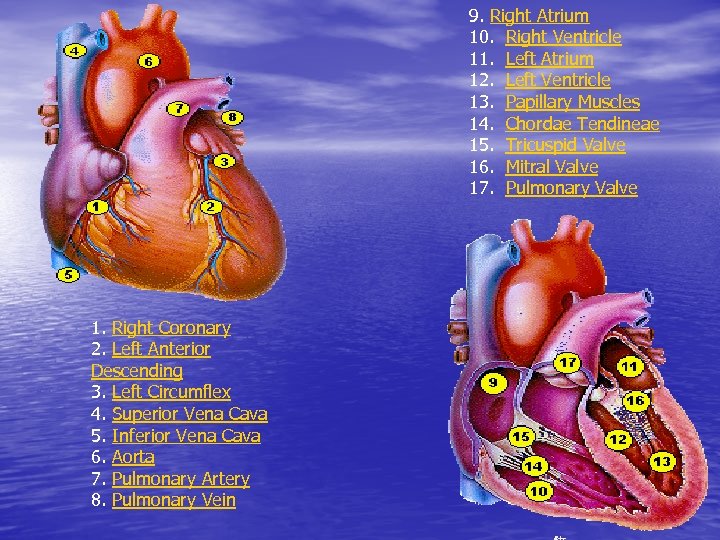 9. Right Atrium 10. Right Ventricle 11. Left Atrium 12. Left Ventricle 13. Papillary Muscles 14. Chordae Tendineae 15. Tricuspid Valve 16. Mitral Valve 17. Pulmonary Valve 1. Right Coronary 2. Left Anterior Descending 3. Left Circumflex 4. Superior Vena Cava 5. Inferior Vena Cava 6. Aorta 7. Pulmonary Artery 8. Pulmonary Vein
9. Right Atrium 10. Right Ventricle 11. Left Atrium 12. Left Ventricle 13. Papillary Muscles 14. Chordae Tendineae 15. Tricuspid Valve 16. Mitral Valve 17. Pulmonary Valve 1. Right Coronary 2. Left Anterior Descending 3. Left Circumflex 4. Superior Vena Cava 5. Inferior Vena Cava 6. Aorta 7. Pulmonary Artery 8. Pulmonary Vein
 CIRCULATION • The importance of circulation is the movement of • • materials into and out of the cells. Cells require O 2 and need to get rid of CO 2. This is accomplished by two processes: BULK FLOW and DIFFUSION.
CIRCULATION • The importance of circulation is the movement of • • materials into and out of the cells. Cells require O 2 and need to get rid of CO 2. This is accomplished by two processes: BULK FLOW and DIFFUSION.
 Bulk Flow • Bulk flow is the movement of blood over significant distances in a short period of time. Accomplished by pressure gradients. • Blood moves from areas of high pressure to areas of low pressure.
Bulk Flow • Bulk flow is the movement of blood over significant distances in a short period of time. Accomplished by pressure gradients. • Blood moves from areas of high pressure to areas of low pressure.
 • We establish pressure gradients by using: 1. 2. 3. 4. heart gravity skeletal muscle smooth muscle
• We establish pressure gradients by using: 1. 2. 3. 4. heart gravity skeletal muscle smooth muscle
 Diffusion • Diffusion is the random movement of molecules with net movement from areas of high concentration to areas of low concentration. • It is only effective over short distances. • It only happens in capillaries.
Diffusion • Diffusion is the random movement of molecules with net movement from areas of high concentration to areas of low concentration. • It is only effective over short distances. • It only happens in capillaries.
 • This can happen because capillaries are blood vessels that are only one cell thick. • Capillaries are the FUNCTIONAL UNIT of circulation with the cells.
• This can happen because capillaries are blood vessels that are only one cell thick. • Capillaries are the FUNCTIONAL UNIT of circulation with the cells.
 • The circulatory system is a CLOSED SYSTEM with three main components: 1. heart (bulk flow) 2. vessels (direct flow) 3. blood (used for transport)
• The circulatory system is a CLOSED SYSTEM with three main components: 1. heart (bulk flow) 2. vessels (direct flow) 3. blood (used for transport)
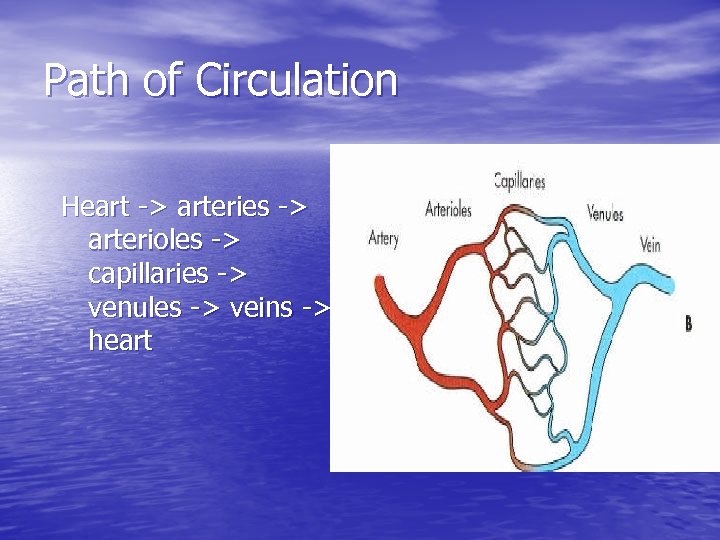 Path of Circulation Heart -> arteries -> arterioles -> capillaries -> venules -> veins -> heart
Path of Circulation Heart -> arteries -> arterioles -> capillaries -> venules -> veins -> heart
 • Arterioles are small arteries and have a lumen diameter of about 0. 5 mm. Their anatomy is the same as arteries.
• Arterioles are small arteries and have a lumen diameter of about 0. 5 mm. Their anatomy is the same as arteries.
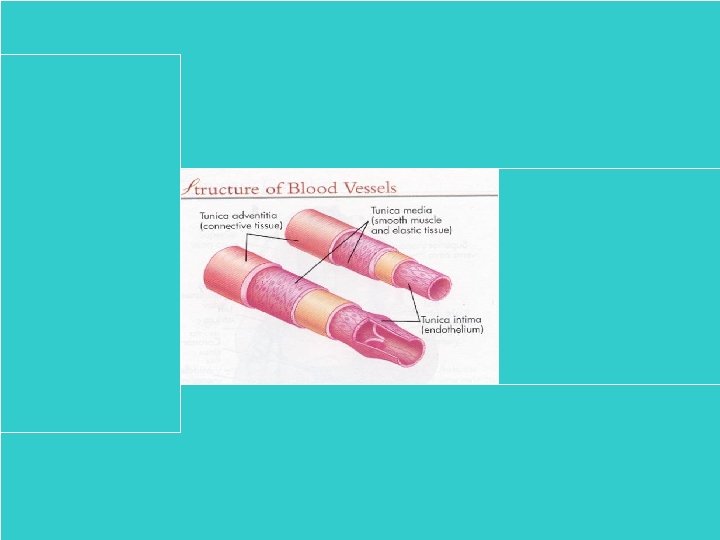
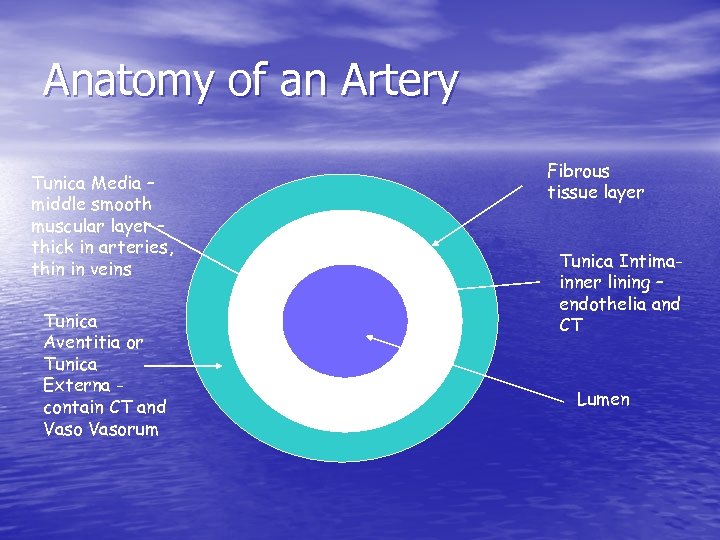 Anatomy of an Artery Tunica Media – middle smooth muscular layer – thick in arteries, thin in veins Tunica Aventitia or Tunica Externa contain CT and Vasorum Fibrous tissue layer Tunica Intimainner lining – endothelia and CT Lumen
Anatomy of an Artery Tunica Media – middle smooth muscular layer – thick in arteries, thin in veins Tunica Aventitia or Tunica Externa contain CT and Vasorum Fibrous tissue layer Tunica Intimainner lining – endothelia and CT Lumen
 • Recall that the arteries have a muscular pump to • • help blood get to the needed body parts. Veins do not have this pump. Skeletal muscle contractions help move the blood upward toward the heart. Also, veins have VALVES which prevent backflow of blood (gravity)
• Recall that the arteries have a muscular pump to • • help blood get to the needed body parts. Veins do not have this pump. Skeletal muscle contractions help move the blood upward toward the heart. Also, veins have VALVES which prevent backflow of blood (gravity)
 • When blood cannot travel back toward the heart, it can accumulate in the veins. This causes a dilation of the vein, or VARICOSE VEINS.
• When blood cannot travel back toward the heart, it can accumulate in the veins. This causes a dilation of the vein, or VARICOSE VEINS.
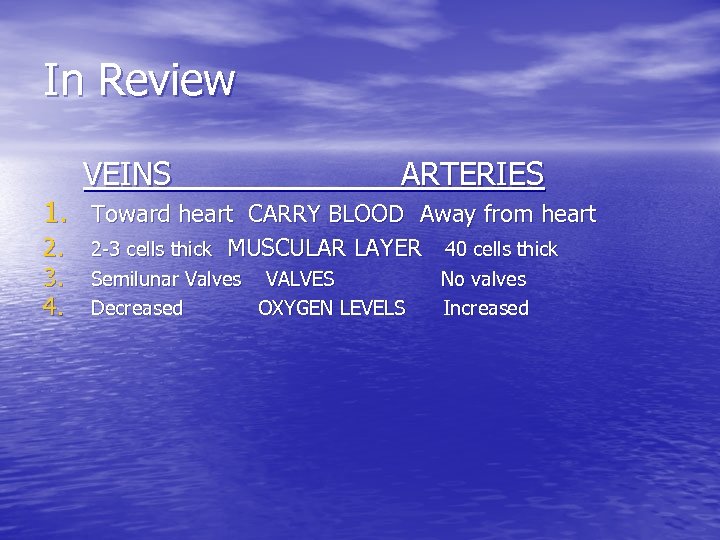 In Review VEINS ARTERIES 1. Toward heart CARRY BLOOD Away from heart 2. 3. 4. 2 -3 cells thick MUSCULAR LAYER 40 cells thick Semilunar Valves VALVES No valves Decreased OXYGEN LEVELS Increased
In Review VEINS ARTERIES 1. Toward heart CARRY BLOOD Away from heart 2. 3. 4. 2 -3 cells thick MUSCULAR LAYER 40 cells thick Semilunar Valves VALVES No valves Decreased OXYGEN LEVELS Increased
 Categories of Circulation 1. Pulmonary Circulation- • Blood from right ventricle goes through the pulmonary trunk to lungs and back to left atrium. There is much lower hydrostatic pressure than in the systemic circulation.
Categories of Circulation 1. Pulmonary Circulation- • Blood from right ventricle goes through the pulmonary trunk to lungs and back to left atrium. There is much lower hydrostatic pressure than in the systemic circulation.
 • 2. Systemic Circulation The second major circulatory loop. Blood leaves the left ventricle and is pumped throughout the body. It ends up in the right atrium. This loop includes blood supply to the GI tract to help with nutrient absroption.
• 2. Systemic Circulation The second major circulatory loop. Blood leaves the left ventricle and is pumped throughout the body. It ends up in the right atrium. This loop includes blood supply to the GI tract to help with nutrient absroption.
 Collateral Circulation • Allows blood to flow around a blockage. • Arterioles meet head on in an ANASTOMOSIS. • Anastomoses serve as a natural bypass.
Collateral Circulation • Allows blood to flow around a blockage. • Arterioles meet head on in an ANASTOMOSIS. • Anastomoses serve as a natural bypass.
 Portal Circulation • Veins from pancreas, spleen, small intestine, and stomach empty into the portal vein in the liver. • After excess glucose is removed and detoxification occurs, blood enters the hepatic portal vein to be returned to the vena cava and the general circulation.
Portal Circulation • Veins from pancreas, spleen, small intestine, and stomach empty into the portal vein in the liver. • After excess glucose is removed and detoxification occurs, blood enters the hepatic portal vein to be returned to the vena cava and the general circulation.
 Fetal Circulation - needed because the fetal lung is not functional. Fetal oxygen source is the PLACENTA. - blood from mother and fetus do not mix, but rather is in 2 adjacent capillary beds. - permeable materials can pass through the adjacent capillary beds causing the fetus to be exposed to whatever is in the mother’s bloodstream.
Fetal Circulation - needed because the fetal lung is not functional. Fetal oxygen source is the PLACENTA. - blood from mother and fetus do not mix, but rather is in 2 adjacent capillary beds. - permeable materials can pass through the adjacent capillary beds causing the fetus to be exposed to whatever is in the mother’s bloodstream.
 Blood flows from the placenta to the fetus via on UMBILICAL VEIN. - The UV has the most oxygen rich blood for the fetus. - This vein branches with one part going to the FETAL LIVER and the other going to the INFERIOR VENA CAVAE (DUCTUS VENOSIS). - Blood then enters the right atrium. Blood so far is MIXED (both oxygenated and deoxygenated).
Blood flows from the placenta to the fetus via on UMBILICAL VEIN. - The UV has the most oxygen rich blood for the fetus. - This vein branches with one part going to the FETAL LIVER and the other going to the INFERIOR VENA CAVAE (DUCTUS VENOSIS). - Blood then enters the right atrium. Blood so far is MIXED (both oxygenated and deoxygenated).
 • This blood is then combined with deoxygenated blood from the coronary sinus and superior vena cavae. • There is a hole (foramen) between the atria. This is called the FORAMEN OVALE. • There is also a linkage between the pulmonary artery and the aorta. This is called the DUCTUS ARTERIOSUS.
• This blood is then combined with deoxygenated blood from the coronary sinus and superior vena cavae. • There is a hole (foramen) between the atria. This is called the FORAMEN OVALE. • There is also a linkage between the pulmonary artery and the aorta. This is called the DUCTUS ARTERIOSUS.
 • The UMBILICAL ARTERIES branch from the INTERNAL ILIAC ARTERIES found in the pelvis. The ILA’s are branches of the COMMON ILIAC ARTERIES which are the terminal branches of the aorta.
• The UMBILICAL ARTERIES branch from the INTERNAL ILIAC ARTERIES found in the pelvis. The ILA’s are branches of the COMMON ILIAC ARTERIES which are the terminal branches of the aorta.
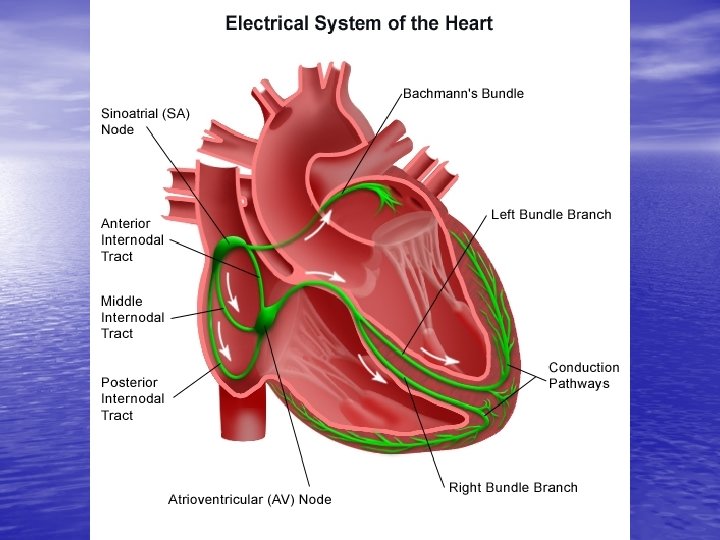
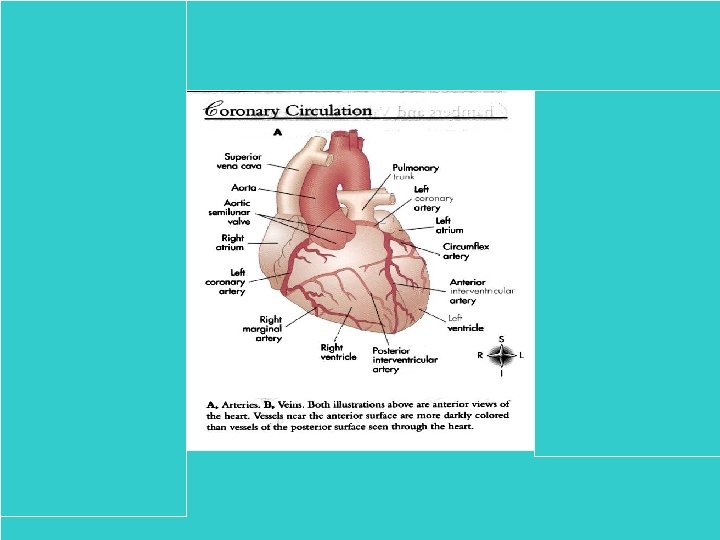
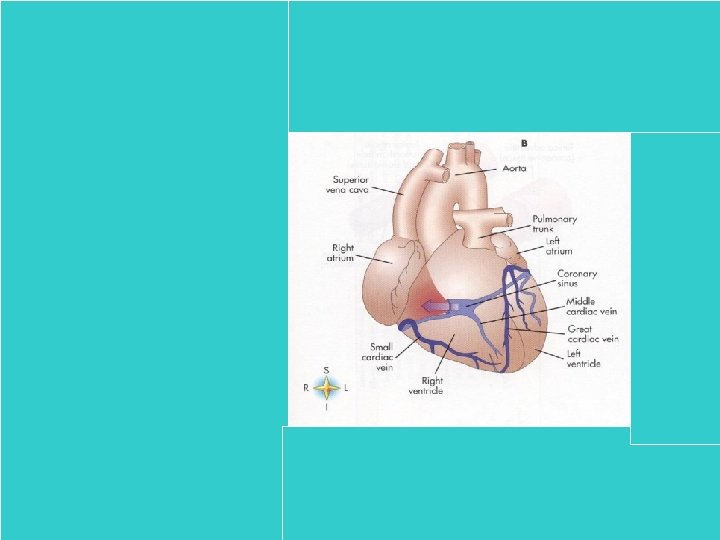
 Coronary Circulation - heart has a separate circulation. - these coronary vessels are the ones treated in “bypass” surgery. - CORONARY SULCUS or ATRIOVENTRICULAR GROOVE - INTERVENTRICULAR SULCUS. - The coronary arteries and veins are located within these grooves.
Coronary Circulation - heart has a separate circulation. - these coronary vessels are the ones treated in “bypass” surgery. - CORONARY SULCUS or ATRIOVENTRICULAR GROOVE - INTERVENTRICULAR SULCUS. - The coronary arteries and veins are located within these grooves.
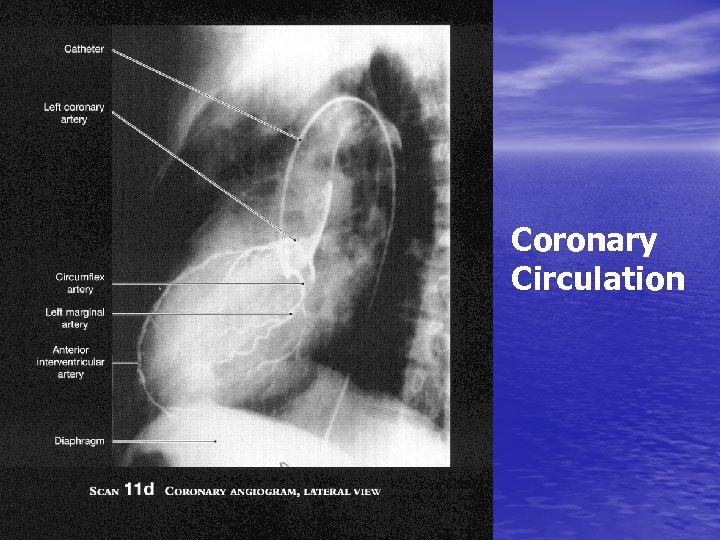 Coronary Circulation
Coronary Circulation
 • Each blood cell must pass through the heart twice in order to complete a full circulatory circuit.
• Each blood cell must pass through the heart twice in order to complete a full circulatory circuit.
 Lymphatics (in general) • The lymphatic system is a system that collects and • • • recycles fluids that have leaked from the circulation. It is also involved in fighting infections. It is made of a series of LYMPH VESSELS and tiny beanshaped NODES. Lymph tissue is located in various parts of the body including; thymus, tonsils, spleen, and bone marrow. The lymph tissue is eventually drained into the vena cava to go into the right atrium.
Lymphatics (in general) • The lymphatic system is a system that collects and • • • recycles fluids that have leaked from the circulation. It is also involved in fighting infections. It is made of a series of LYMPH VESSELS and tiny beanshaped NODES. Lymph tissue is located in various parts of the body including; thymus, tonsils, spleen, and bone marrow. The lymph tissue is eventually drained into the vena cava to go into the right atrium.
 What is carried in the blood? • Respiratory gasses (oxygen and CO 2) • Nutrients • Hormones • Defense cells/Immune cells • Repair cells It also regulates body temperature by carrying warmth from the center of the body to the periphery.
What is carried in the blood? • Respiratory gasses (oxygen and CO 2) • Nutrients • Hormones • Defense cells/Immune cells • Repair cells It also regulates body temperature by carrying warmth from the center of the body to the periphery.
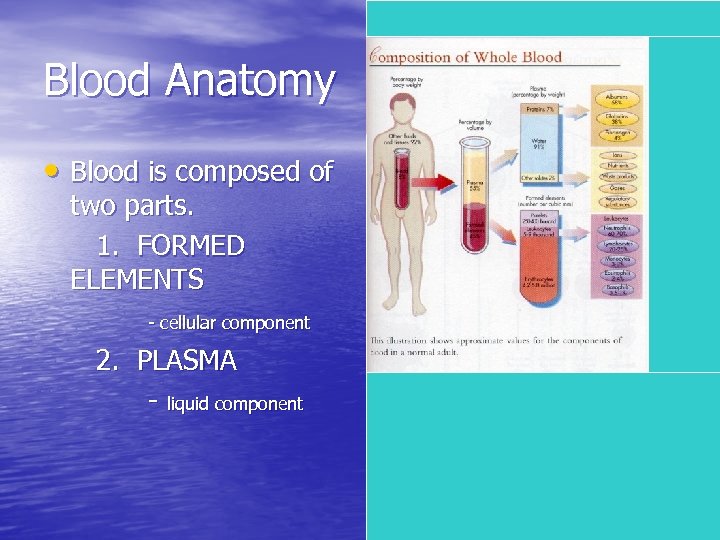 Blood Anatomy • Blood is composed of two parts. 1. FORMED ELEMENTS - cellular component 2. PLASMA - liquid component
Blood Anatomy • Blood is composed of two parts. 1. FORMED ELEMENTS - cellular component 2. PLASMA - liquid component
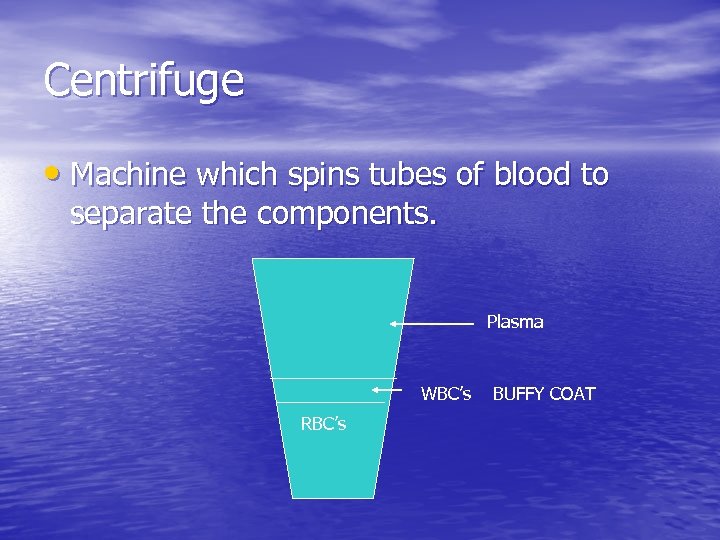 Centrifuge • Machine which spins tubes of blood to separate the components. Plasma WBC’s RBC’s BUFFY COAT
Centrifuge • Machine which spins tubes of blood to separate the components. Plasma WBC’s RBC’s BUFFY COAT
 Plasma • A straw-colored, sticky fluid. • Contains over 100 different kinds of molecules. • Contains three proteins: a. Albumin – important in keeping osmotic pressure constant. Also important in wound healing. b. Globulins – important for antibody production and transport of other molecules. c. Fibrinogen – important for blood clotting
Plasma • A straw-colored, sticky fluid. • Contains over 100 different kinds of molecules. • Contains three proteins: a. Albumin – important in keeping osmotic pressure constant. Also important in wound healing. b. Globulins – important for antibody production and transport of other molecules. c. Fibrinogen – important for blood clotting
 Formed Elements • These are the “blood cells” 1. Erythrocytes a. RBC’s b. Carry oxygen c. No nuclei or organelles d. % of blood volume that contain erythrocytes is known as the HEMATOCRIT.
Formed Elements • These are the “blood cells” 1. Erythrocytes a. RBC’s b. Carry oxygen c. No nuclei or organelles d. % of blood volume that contain erythrocytes is known as the HEMATOCRIT.
 e. cytoplasm is filled with HEMOGLOBIN. f. Hemoglobin is the oxygen carrying protein. g. Pick up oxygen in the lung capillaries and release carbon dioxide. h. Spherical shaped i. When the shaped changes, individual cells have difficulty entering and traveling through the capillary lumen. j. Efficient oxygen transporters as they do not use any of the oxygen they transport. This is because they do not have organelles (mitochondria). The erythrocytes must get their energy through anaerobic means.
e. cytoplasm is filled with HEMOGLOBIN. f. Hemoglobin is the oxygen carrying protein. g. Pick up oxygen in the lung capillaries and release carbon dioxide. h. Spherical shaped i. When the shaped changes, individual cells have difficulty entering and traveling through the capillary lumen. j. Efficient oxygen transporters as they do not use any of the oxygen they transport. This is because they do not have organelles (mitochondria). The erythrocytes must get their energy through anaerobic means.
 k. Live for 120 days. Therefore, it is easy to use them for clinical testing. For example, glucose binds to the RBC. The more glucose that is bound to the RBC, the higher the patients average blood sugar levels. Hb. A 1 C is a measurement of how much sugar is bound to the RBC. If this test is performed every 120 days, physicians can determine the range of blood sugar control.
k. Live for 120 days. Therefore, it is easy to use them for clinical testing. For example, glucose binds to the RBC. The more glucose that is bound to the RBC, the higher the patients average blood sugar levels. Hb. A 1 C is a measurement of how much sugar is bound to the RBC. If this test is performed every 120 days, physicians can determine the range of blood sugar control.
 LEUKOCYTES • • • White Blood Cells (WBC) Crucial to the bodies defense against disease. Have all the organelles and nuclei of a true cell. Leukocytes perform their function outside the circulatory system. They function in the connective tissue (where infections usually occur). When a leukocyte senses an infection, it moves out of the circulation by squeezing out between the endothelial cells which line the blood vessels. This is known as DIAPEDESIS. Once outside the circulation, the WBC’s use amoeboid motion to find the offending organism.
LEUKOCYTES • • • White Blood Cells (WBC) Crucial to the bodies defense against disease. Have all the organelles and nuclei of a true cell. Leukocytes perform their function outside the circulatory system. They function in the connective tissue (where infections usually occur). When a leukocyte senses an infection, it moves out of the circulation by squeezing out between the endothelial cells which line the blood vessels. This is known as DIAPEDESIS. Once outside the circulation, the WBC’s use amoeboid motion to find the offending organism.
 5 Types of Leukocytes Granulocytes 1. Neutrophils – most abundant - lobuated nuclei - “Polymorphonuclear Leukocytes” (PMN’s) - “Polys” or “Segs” - phagocytize and destroy bacteria.
5 Types of Leukocytes Granulocytes 1. Neutrophils – most abundant - lobuated nuclei - “Polymorphonuclear Leukocytes” (PMN’s) - “Polys” or “Segs” - phagocytize and destroy bacteria.
 2. Eosinophils - rarely found - nuclei with only 2 lobes - stain red with acidic dye “Eosin” - fight parasites and parasitic diseases
2. Eosinophils - rarely found - nuclei with only 2 lobes - stain red with acidic dye “Eosin” - fight parasites and parasitic diseases
 3. Basophils - rarest of all WBC’s - nuclei stain dark with basic stain - secrete histamine to mediate allergic reactions.
3. Basophils - rarest of all WBC’s - nuclei stain dark with basic stain - secrete histamine to mediate allergic reactions.
 • Agranulocytes 1. Lymphocytes - most important cell in the immune system - function in the connective tissue, not the bloodstream - important for fighting infection - substances that cause a reaction from a lymphocyte is called an ANTIGEN. - 2 types of lymphocytes: T-cells (kill organisms directly) B-cells (become mast cells
• Agranulocytes 1. Lymphocytes - most important cell in the immune system - function in the connective tissue, not the bloodstream - important for fighting infection - substances that cause a reaction from a lymphocyte is called an ANTIGEN. - 2 types of lymphocytes: T-cells (kill organisms directly) B-cells (become mast cells
 2. Monocytes - become macrophages which ingest a wide variety of foreign debris
2. Monocytes - become macrophages which ingest a wide variety of foreign debris
 CLINICAL CORELLATION A complete blood count (CBC) - Quantifies the various cell types found in - the blood. A DIFFERENTIAL identifies the percentage of each type of leukocyte.
CLINICAL CORELLATION A complete blood count (CBC) - Quantifies the various cell types found in - the blood. A DIFFERENTIAL identifies the percentage of each type of leukocyte.
 Platelets • Known as THROMBOCYTES • Function to plug small tears in the walls of the • • • blood vessels to limit bleeding. Adhere to exposed collagen at the edges of a tear. Release THROMBOPLASTIN, a molecule that initates clotting. Platelets adhere only to damaged blood vessels. When a clot develops or persists in an intact blood vessel, a THROMBUS results.
Platelets • Known as THROMBOCYTES • Function to plug small tears in the walls of the • • • blood vessels to limit bleeding. Adhere to exposed collagen at the edges of a tear. Release THROMBOPLASTIN, a molecule that initates clotting. Platelets adhere only to damaged blood vessels. When a clot develops or persists in an intact blood vessel, a THROMBUS results.


