430151292d48805d1d1aa1541e7ac841.ppt
- Количество слайдов: 142
THE FOURTH UNIVERSITY OF STELLENBOSCH GYNAECOLOGICAL SURGERY SYMPOSIUM (2008) Endometrial Ablation – Indications, Techniques and Outcomes Alan Alperstein Gynaecologist Kingsbury House Claremont Cape Town alan@kingsburyhouse. co. za
Disclosures § Private practice § Part time Consultant @ GSH – Ho. F § (Reproductive Medicine) § SAMS – Council § SASOG - Council § ISGE – ex Board Member for Africa § Beneficiary: Novo § Lilly § Wyeth § Gynecare § Boston Scientific § Tyco/Covidien § Honoraria and travel
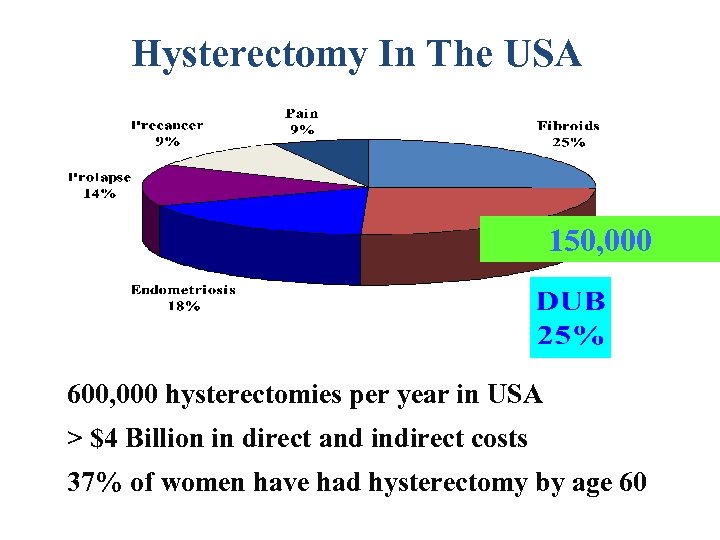
Hysterectomy In The USA 150, 000 600, 000 hysterectomies per year in USA > $4 Billion in direct and indirect costs 37% of women have had hysterectomy by age 60
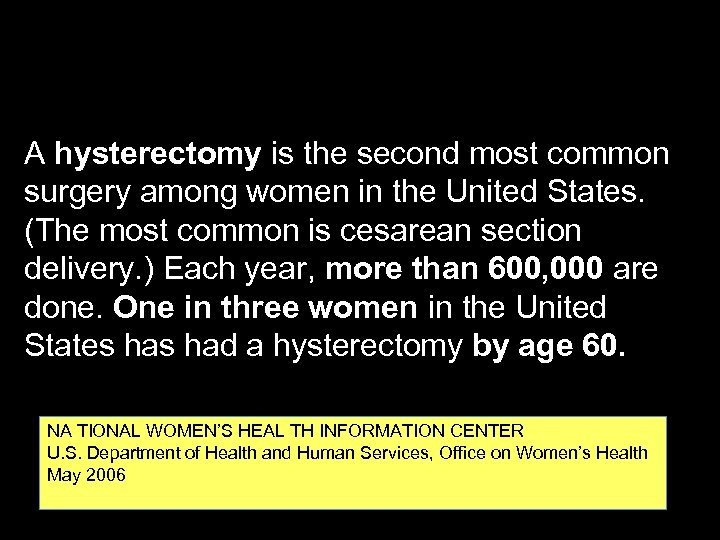
A hysterectomy is the second most common surgery among women in the United States. (The most common is cesarean section delivery. ) Each year, more than 600, 000 are done. One in three women in the United States had a hysterectomy by age 60. NA TIONAL WOMEN’S HEAL TH INFORMATION CENTER U. S. Department of Health and Human Services, Office on Women’s Health May 2006
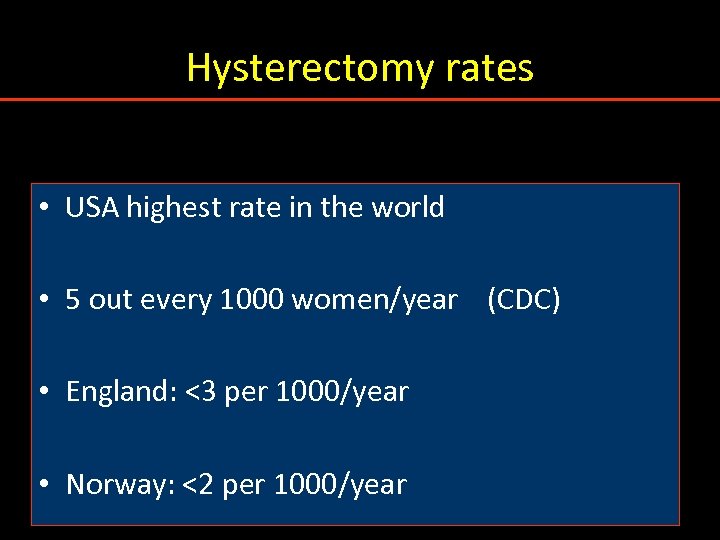
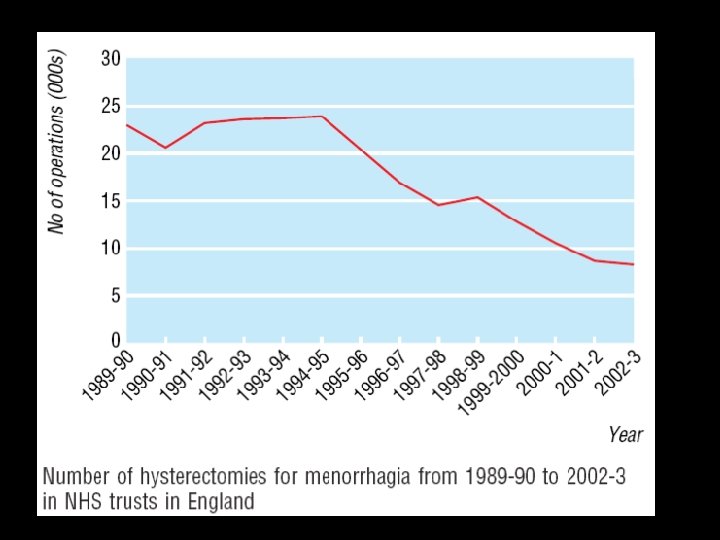
Hysterectomy rates • USA highest rate in the world • 5 out every 1000 women/year (CDC) • England: <3 per 1000/year • Norway: <2 per 1000/year
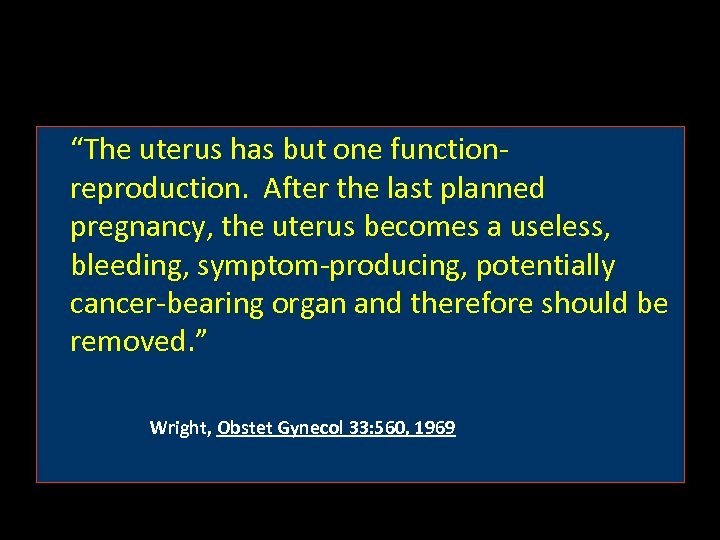
“The uterus has but one functionreproduction. After the last planned pregnancy, the uterus becomes a useless, bleeding, symptom-producing, potentially cancer-bearing organ and therefore should be removed. ” Wright, Obstet Gynecol 33: 560, 1969
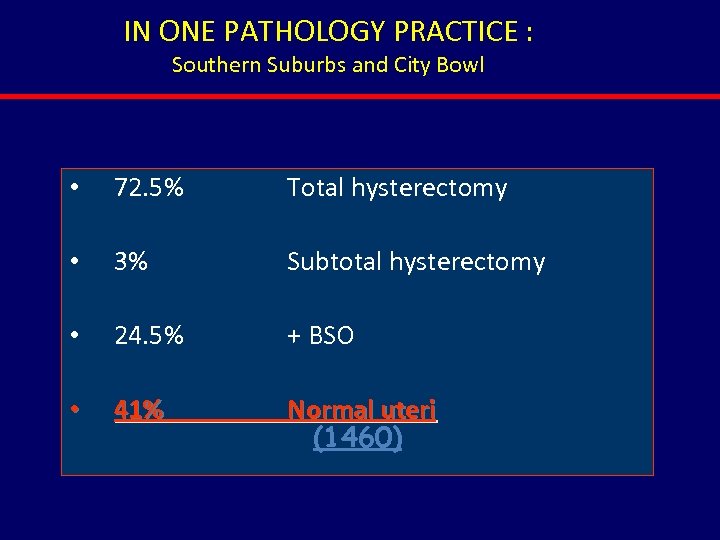
IN ONE PATHOLOGY PRACTICE : Southern Suburbs and City Bowl • 72. 5% Total hysterectomy • 3% Subtotal hysterectomy • 24. 5% + BSO • 41% Normal uteri (1460)
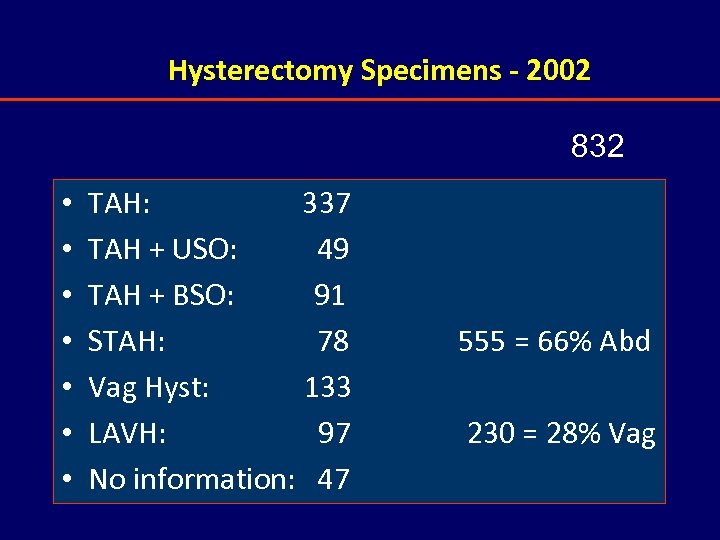
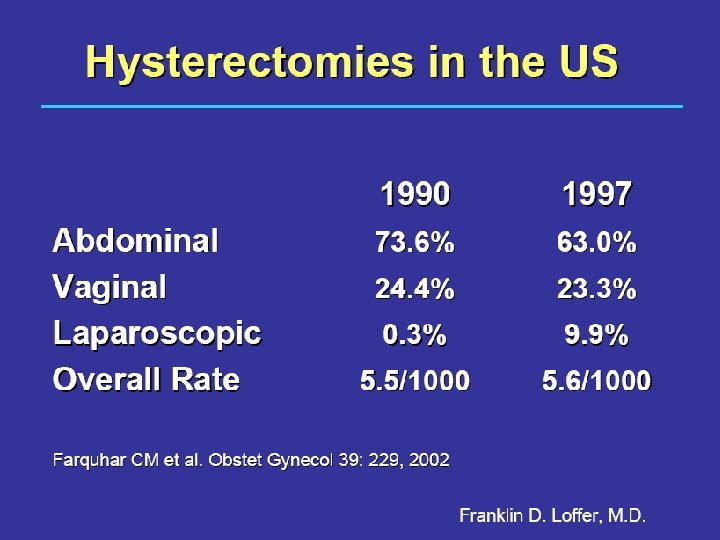
Hysterectomy Specimens - 2002 832 • • TAH: 337 TAH + USO: 49 TAH + BSO: 91 STAH: 78 Vag Hyst: 133 LAVH: 97 No information: 47 555 = 66% Abd 230 = 28% Vag
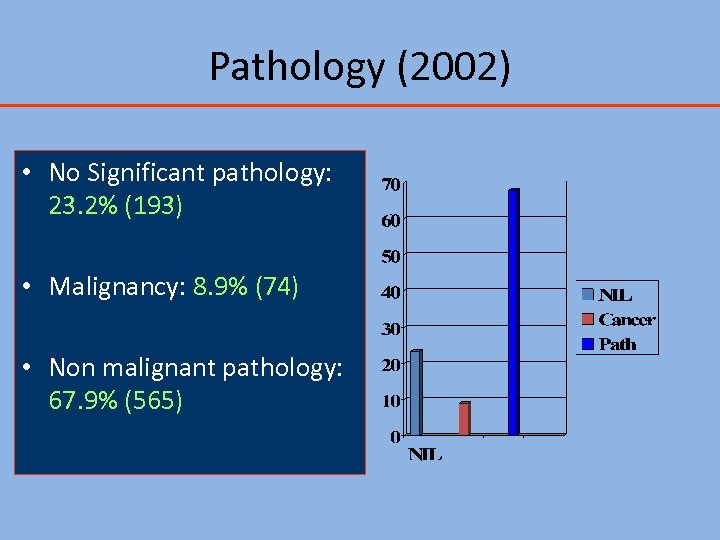
Pathology (2002) • No Significant pathology: 23. 2% (193) • Malignancy: 8. 9% (74) • Non malignant pathology: 67. 9% (565)
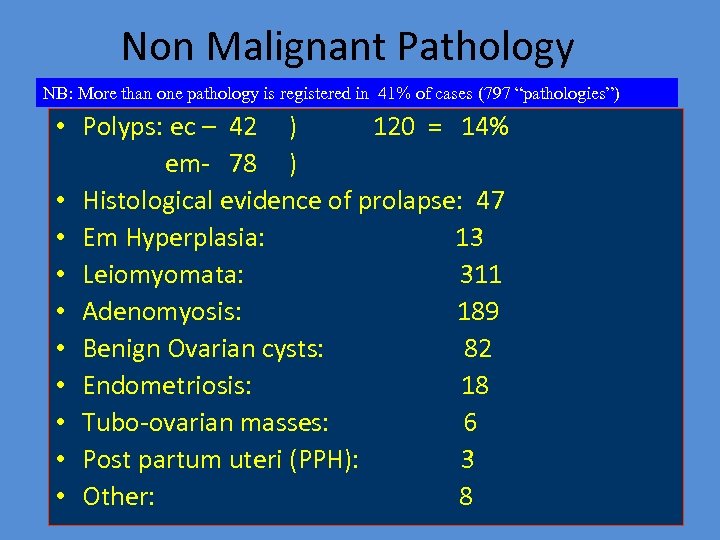
Non Malignant Pathology NB: More than one pathology is registered in 41% of cases (797 “pathologies”) • Polyps: ec – 42 ) 120 = 14% em- 78 ) • Histological evidence of prolapse: 47 • Em Hyperplasia: 13 • Leiomyomata: 311 • Adenomyosis: 189 • Benign Ovarian cysts: 82 • Endometriosis: 18 • Tubo-ovarian masses: 6 • Post partum uteri (PPH): 3 • Other: 8


Alternatives to Hysterectomy Are there any…………. ?
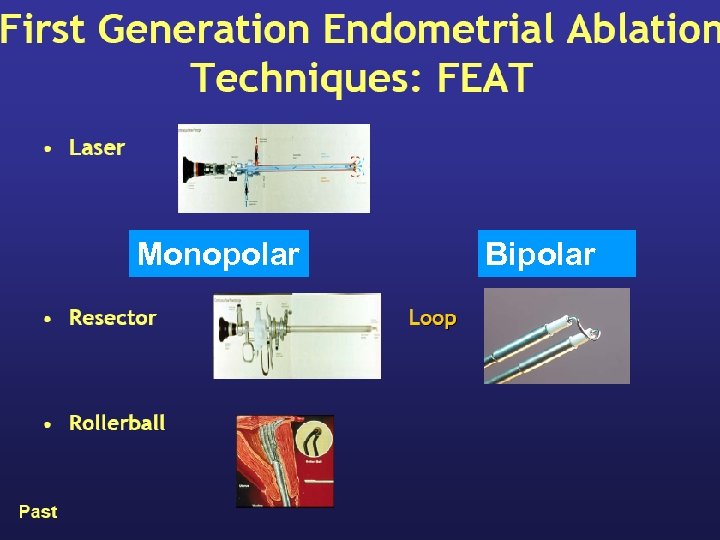
Monopolar Bipolar
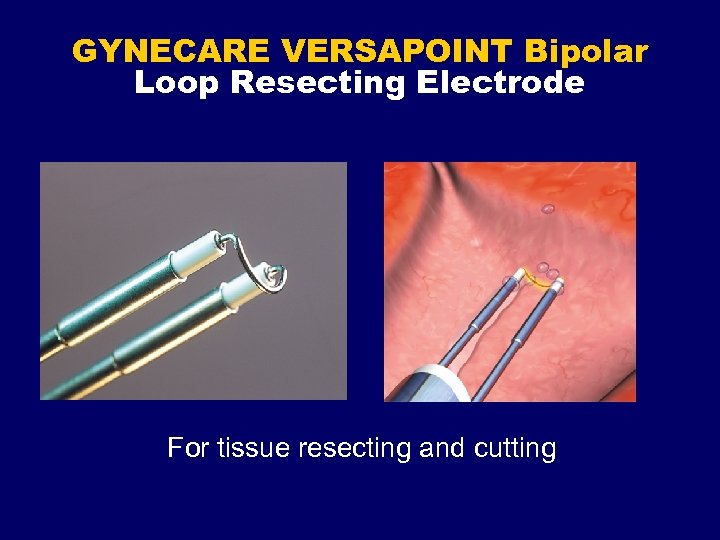
GYNECARE VERSAPOINT Bipolar Loop Resecting Electrode For tissue resecting and cutting
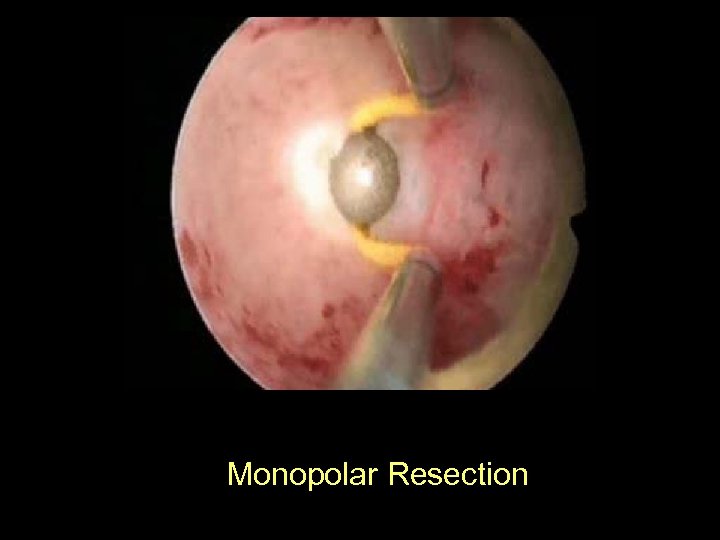
Monopolar Resection
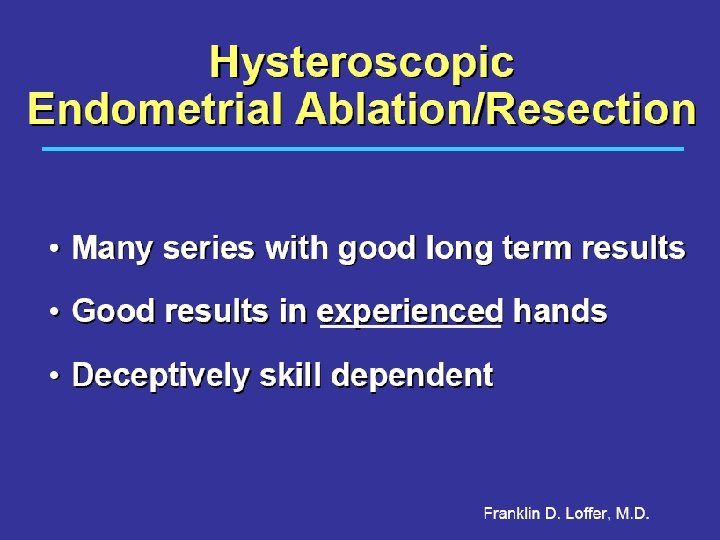
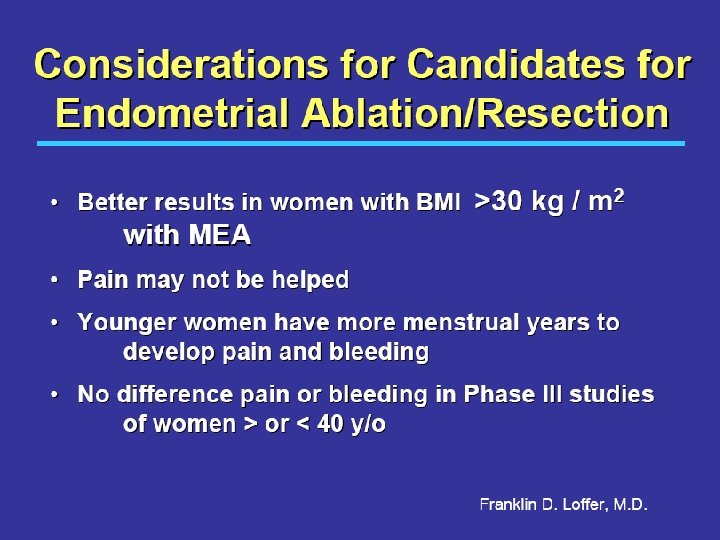
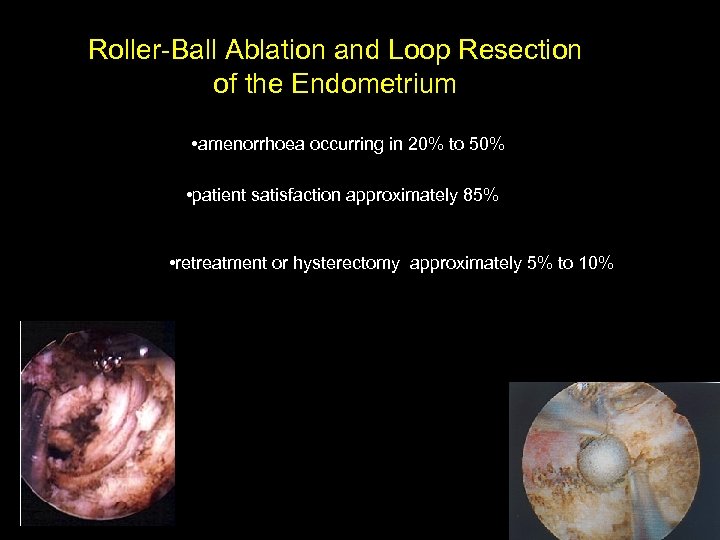
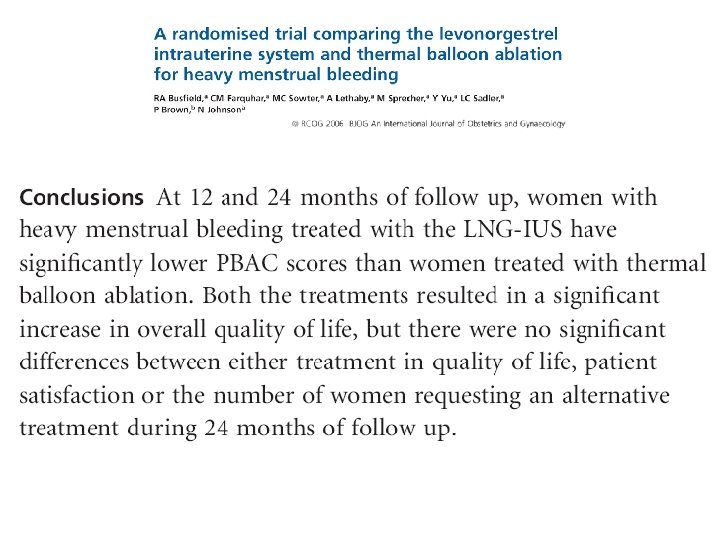
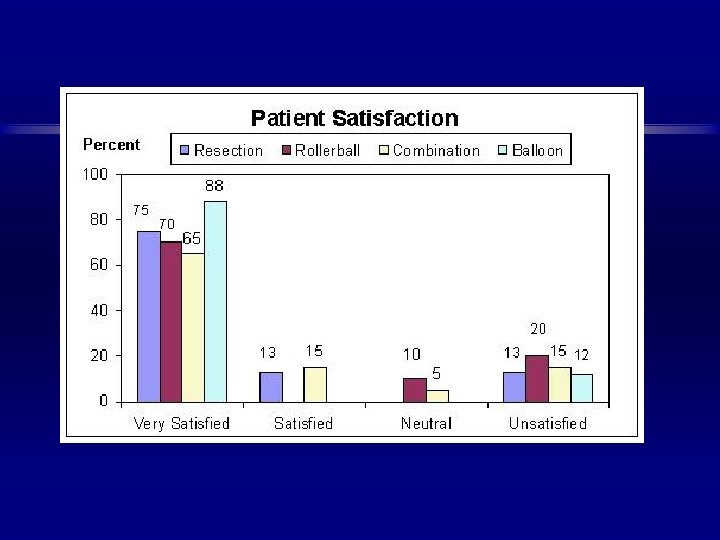
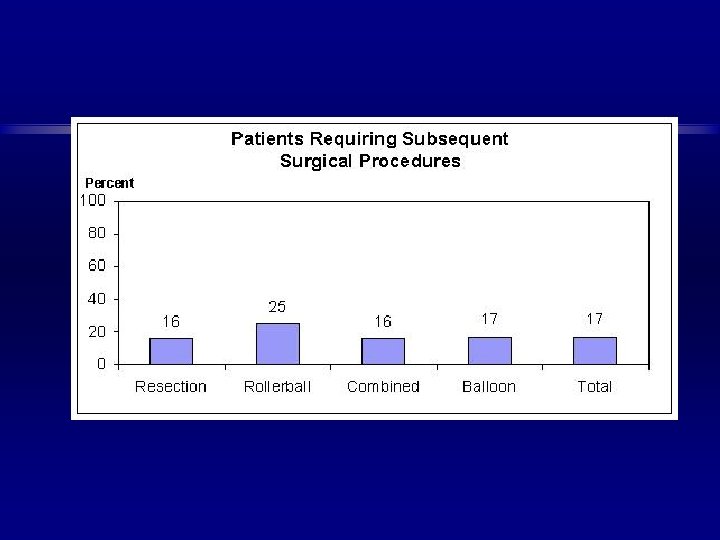
Roller-Ball Ablation and Loop Resection of the Endometrium • amenorrhoea occurring in 20% to 50% • patient satisfaction approximately 85% • retreatment or hysterectomy approximately 5% to 10%
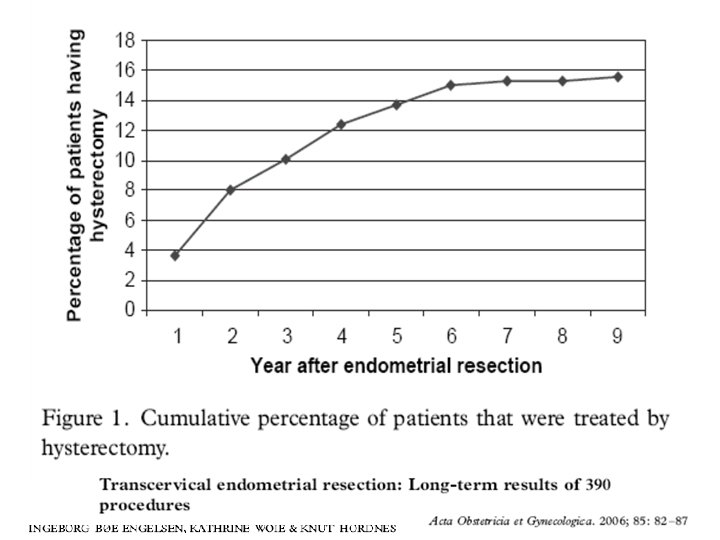
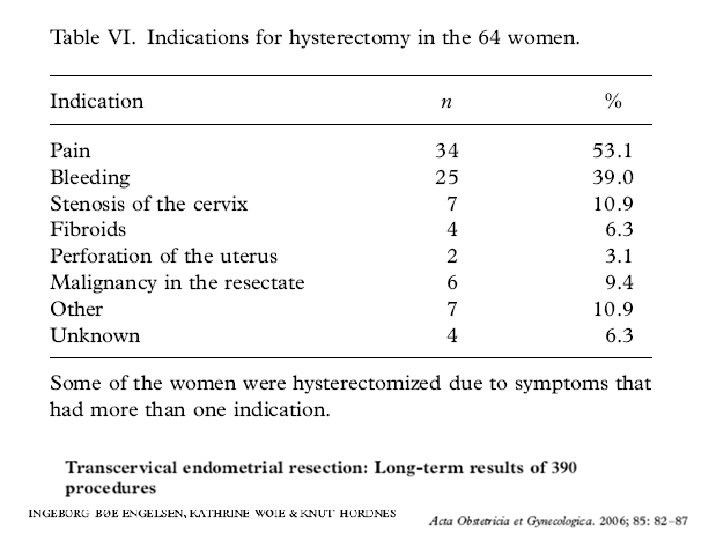
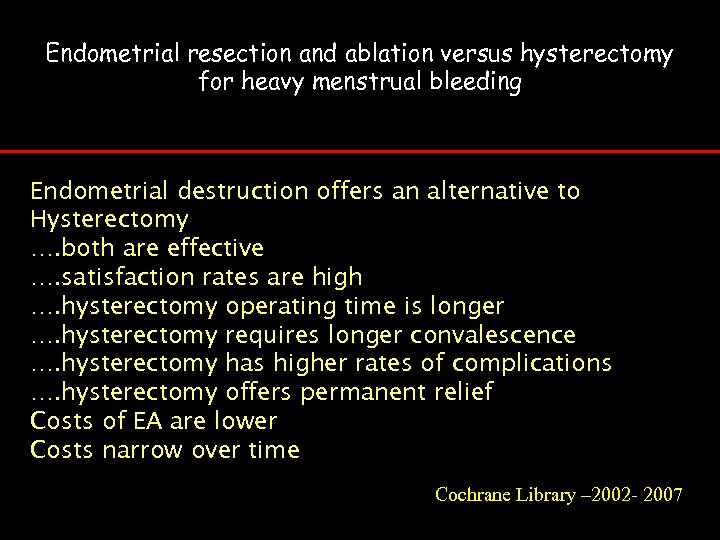
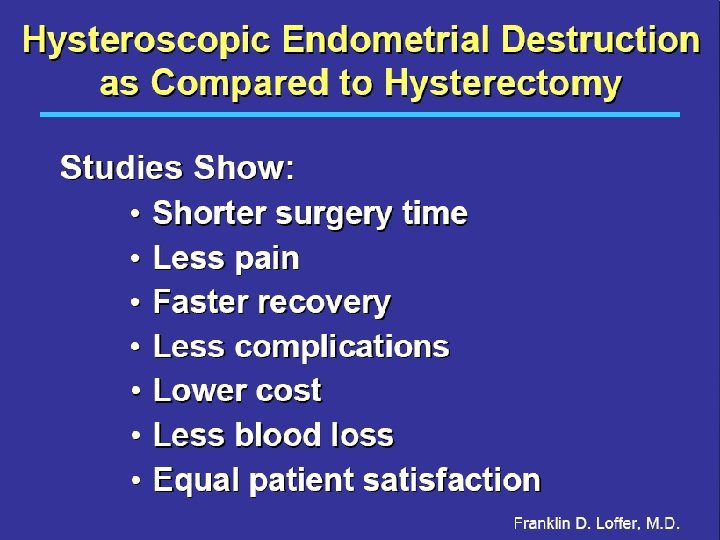
Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding Endometrial destruction offers an alternative to Hysterectomy …. both are effective …. satisfaction rates are high …. hysterectomy operating time is longer …. hysterectomy requires longer convalescence …. hysterectomy has higher rates of complications …. hysterectomy offers permanent relief Costs of EA are lower Costs narrow over time Cochrane Library – 2002 - 2007
Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding A Lethaby Cochrane Rev Abstract. 2006; © 2006 The Cochrane Collaboration Posted 10/01/2006 Authors' conclusions Endometrial destruction offers an alternative to hysterectomy as a surgical treatment for heavy menstrual bleeding. Both procedures are effective and satisfaction rates are high. Although hysterectomy is associated with a longer operating time, a longer recovery period and higher rates of post – operative complications, it offers permanent relief from heavy menstrual bleeding. The cost of endometrial destruction is significantly lower than hysterectomy but since re – treatment is often necessary the cost difference narrows over time.
Conclusions: • Alternatives to hysterectomy exist • Commonly-held “indications” for hysterectomy are often more subjective than substantiated by science • Physician bias or inexperience with new surgical techniques may explain why hysterectomy is recommended more often than conservative measures
July 2000
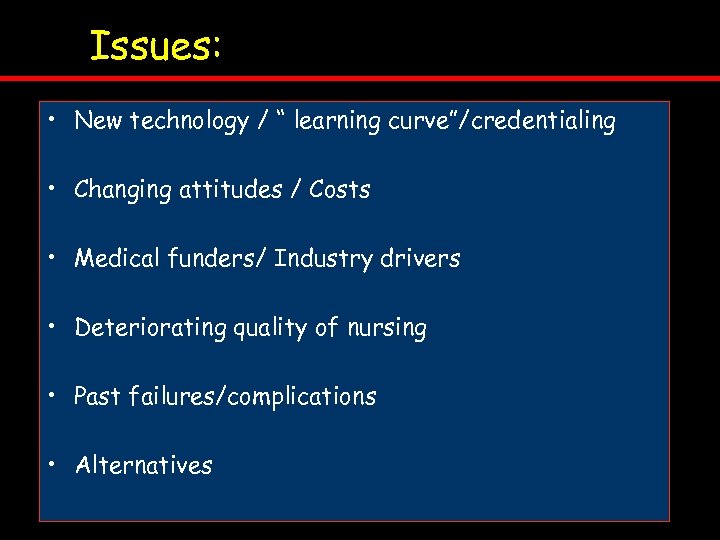
Issues: • New technology / “ learning curve”/credentialing • Changing attitudes / Costs • Medical funders/ Industry drivers • Deteriorating quality of nursing • Past failures/complications • Alternatives
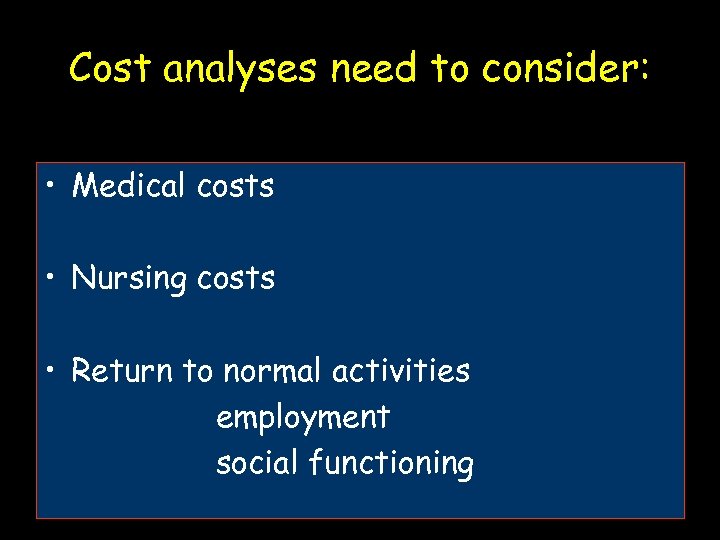
Cost analyses need to consider: • Medical costs • Nursing costs • Return to normal activities employment social functioning
Global Endometrial Ablation
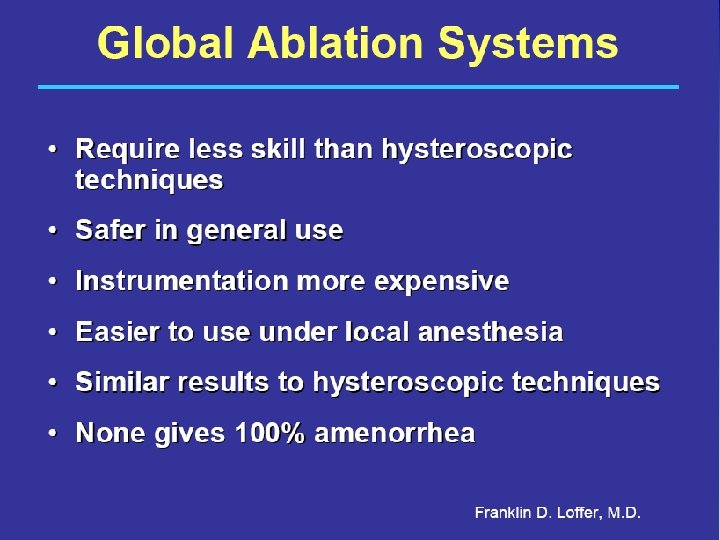


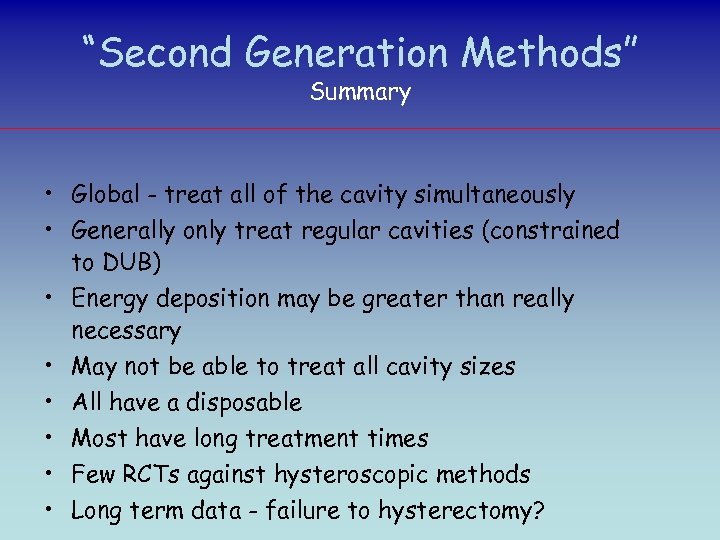
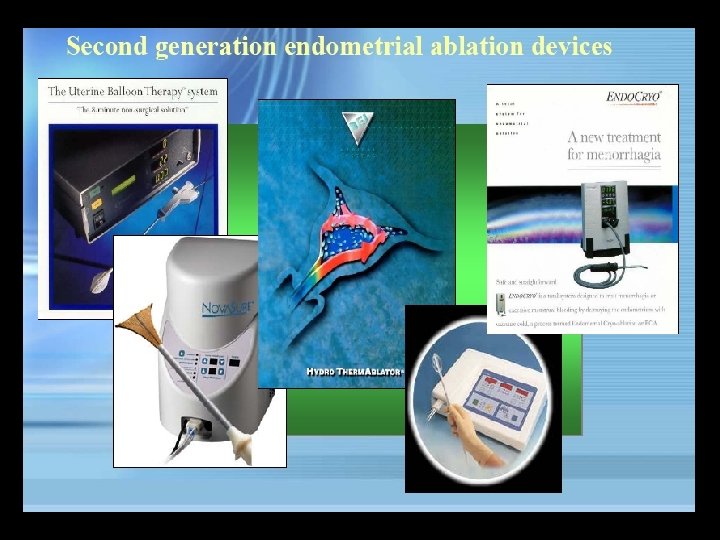
“Second Generation Methods” Summary • Global - treat all of the cavity simultaneously • Generally only treat regular cavities (constrained to DUB) • Energy deposition may be greater than really necessary • May not be able to treat all cavity sizes • All have a disposable • Most have long treatment times • Few RCTs against hysteroscopic methods • Long term data - failure to hysterectomy?
Criteria to treat: Women must have: üfamily complete üfailed medical therapy 1. Endometriosis/adenomyosis excluded on history and clinical examination
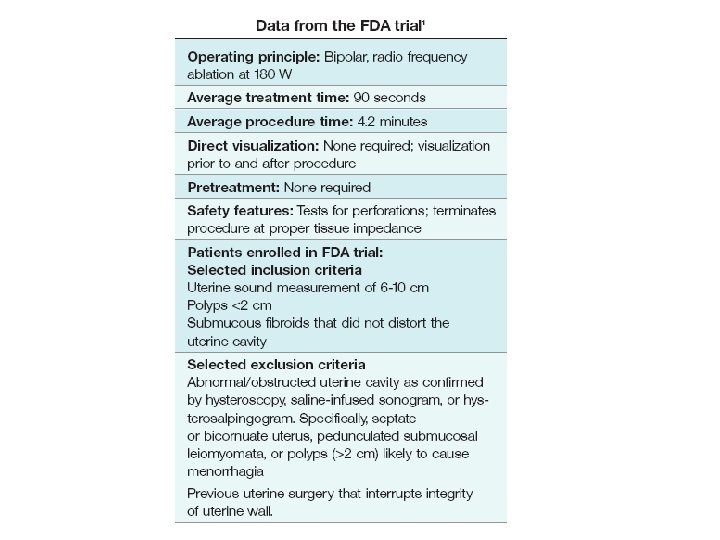
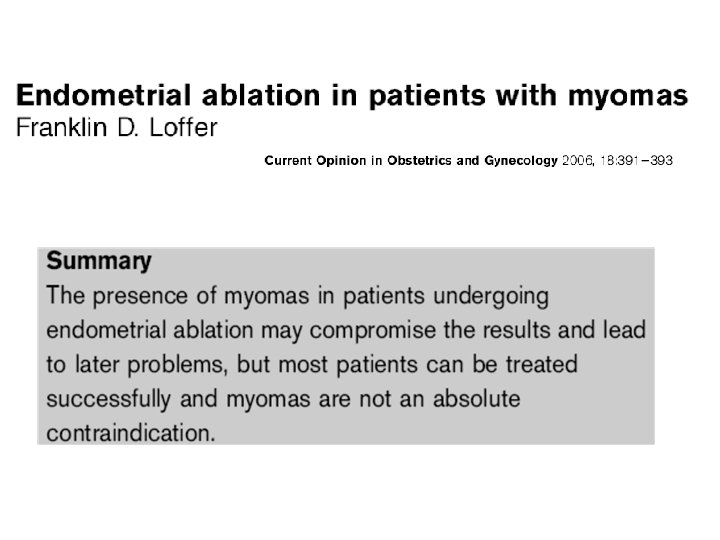
2. The uterus must be carefully assessed preoperatively by ultrasound or Saline infusion sonography scan or hysteroscopy to exclude uterine fibroids, polyps, or other pathology distorting the uterine cavity. 3. The total uterine length must not exceed 10 cm on ultrasound scan, or 9 cm on uterine sounding
4. Endometrium must have normal histology on a biopsy specimen. 5. The pap smear must be negative
. . 6. It is good clinical practice that all surgeons intending to perform endometrial destruction be familiar with the techniques to be employed, and have received adequate training in their use.








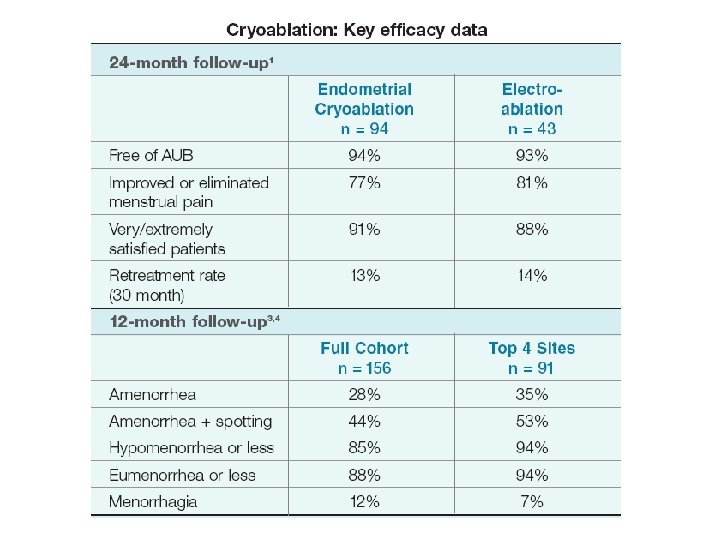
Her Option – cryo ablation

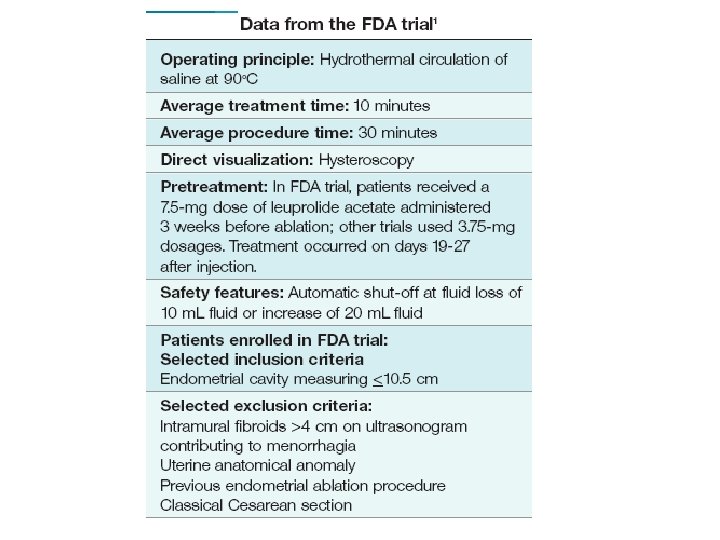
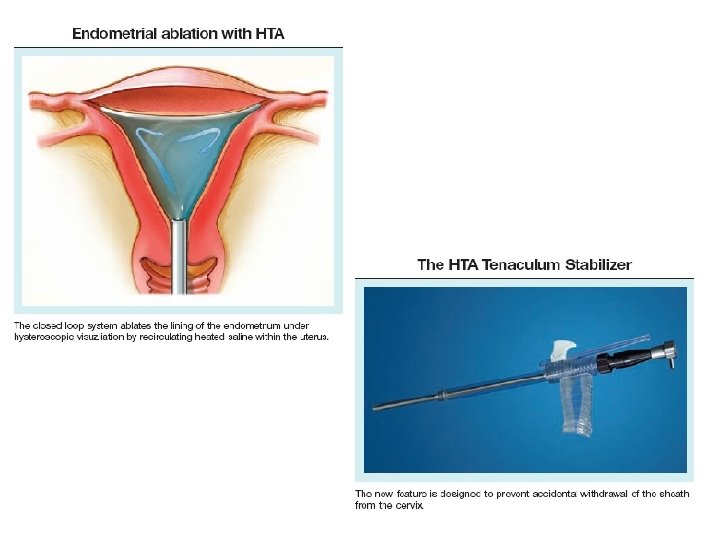
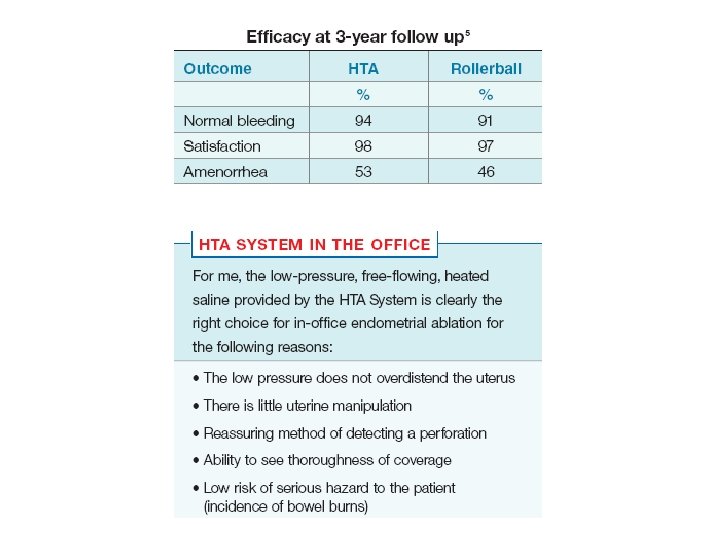
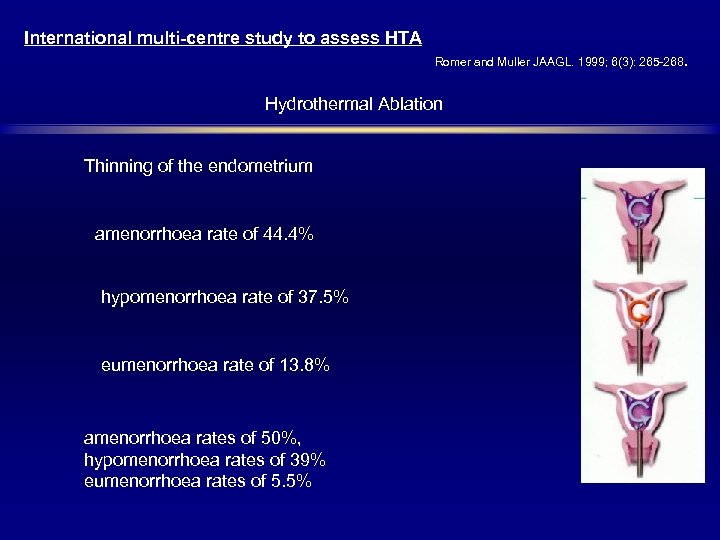
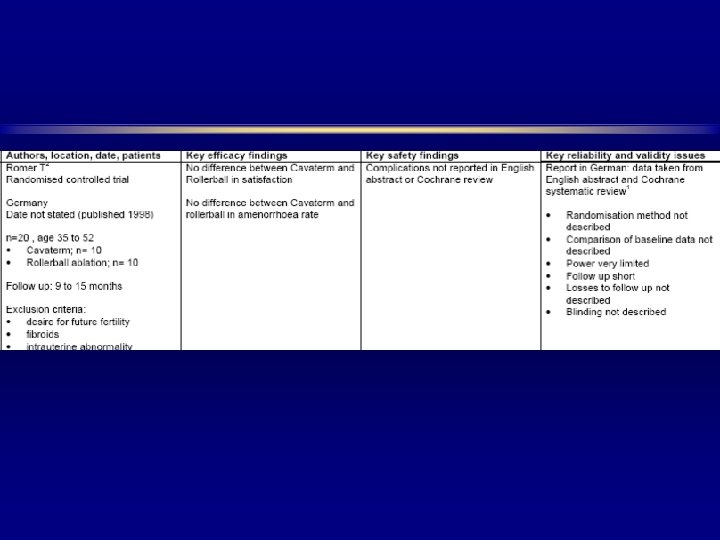
International multi-centre study to assess HTA Romer and Muller JAAGL. 1999; 6(3): 265 -268. Hydrothermal Ablation Thinning of the endometrium amenorrhoea rate of 44. 4% hypomenorrhoea rate of 37. 5% eumenorrhoea rate of 13. 8% amenorrhoea rates of 50%, hypomenorrhoea rates of 39% eumenorrhoea rates of 5. 5%

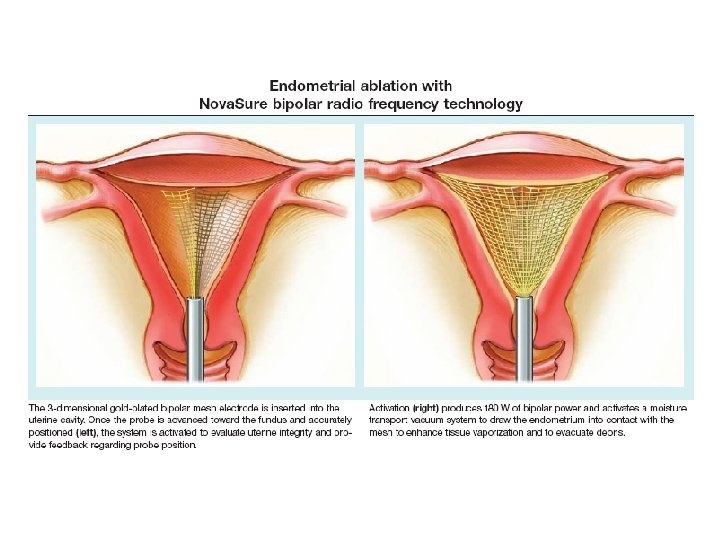
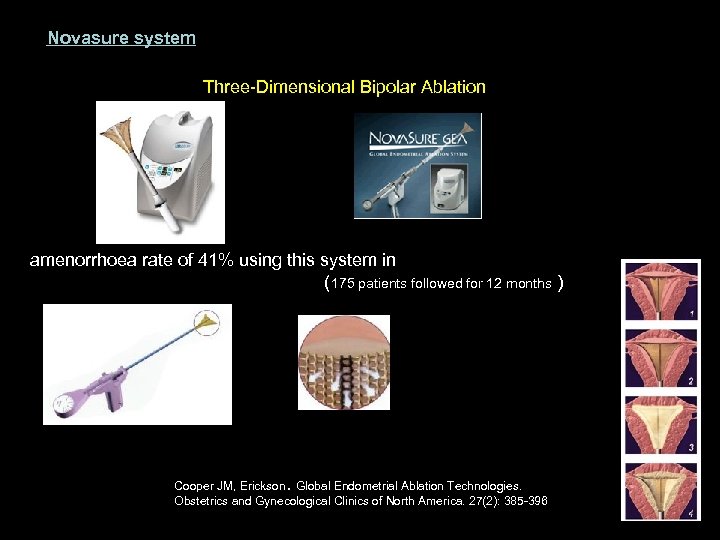
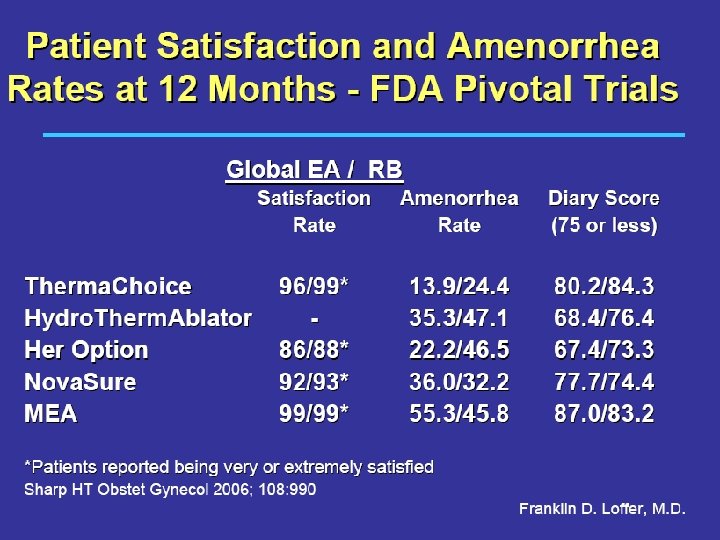
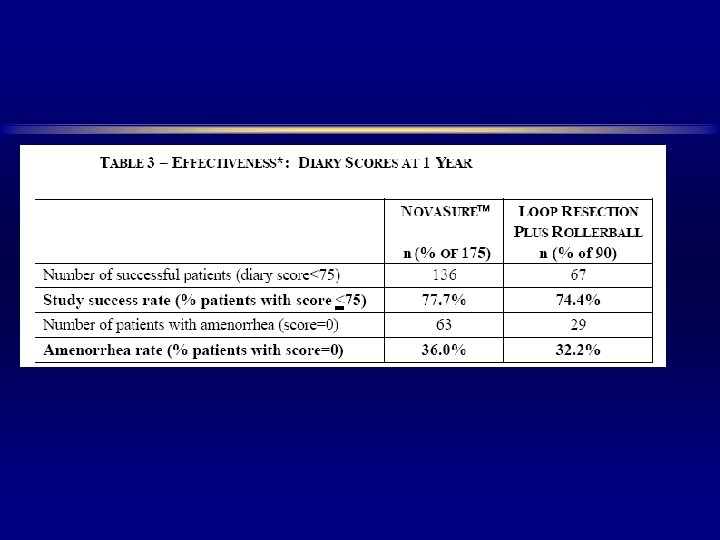
Novasure system Three-Dimensional Bipolar Ablation amenorrhoea rate of 41% using this system in ( 175 patients followed for 12 months ) Cooper JM, Erickson. Global Endometrial Ablation Technologies. Obstetrics and Gynecological Clinics of North America. 27(2): 385 -396


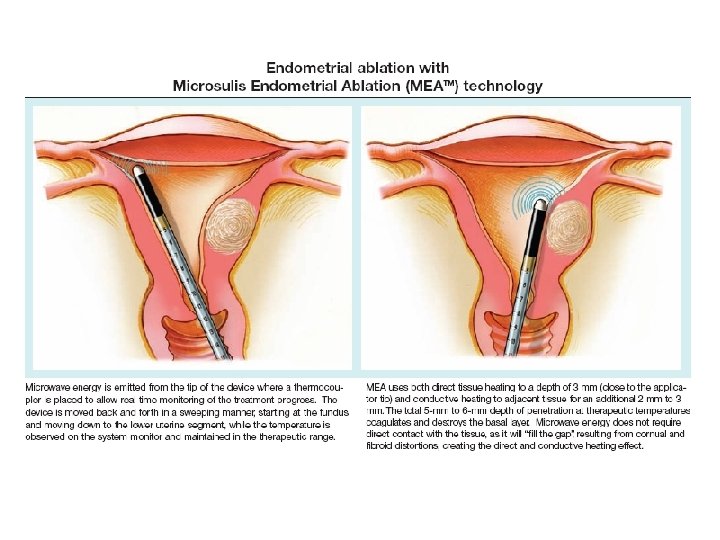
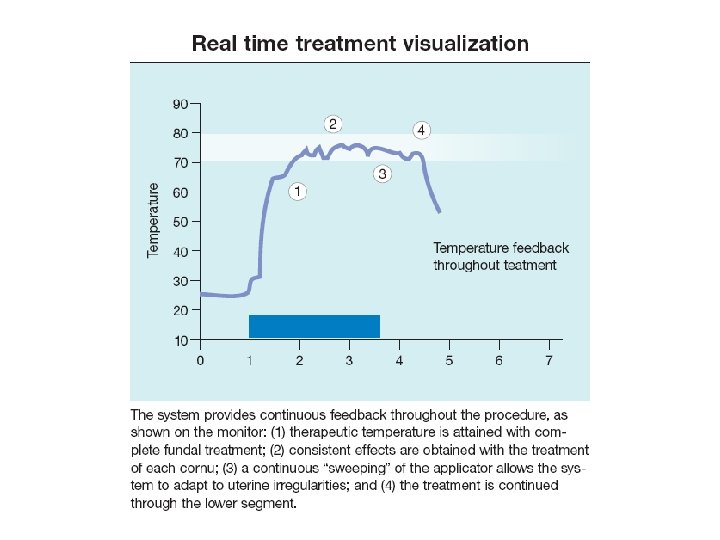
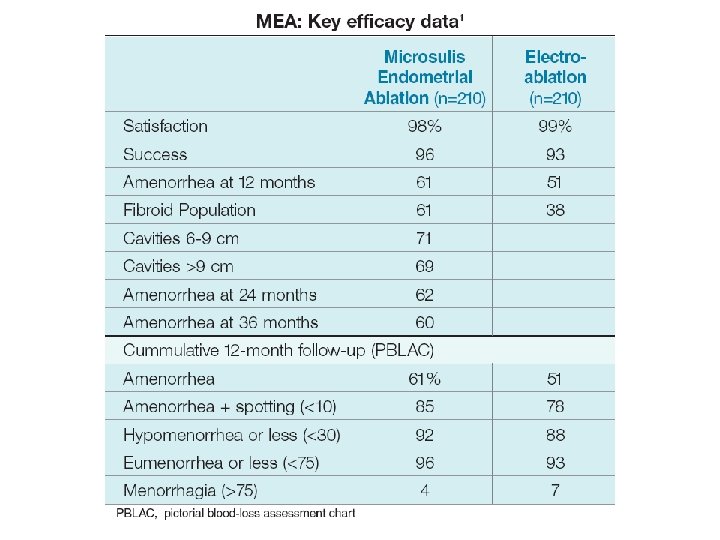
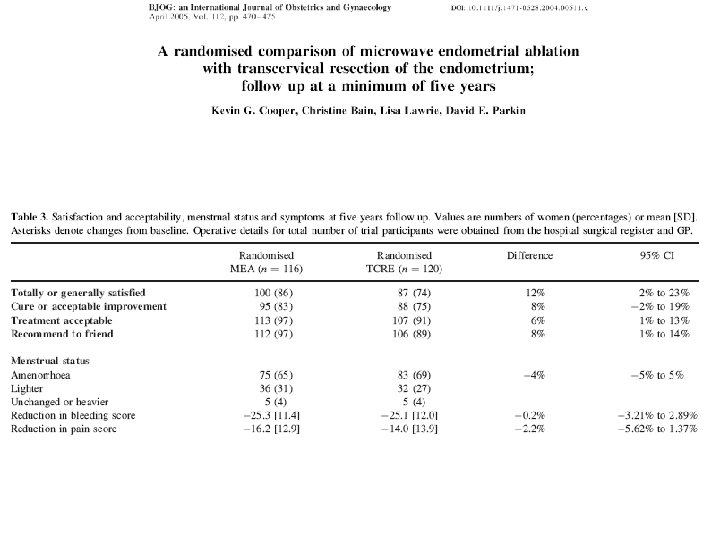
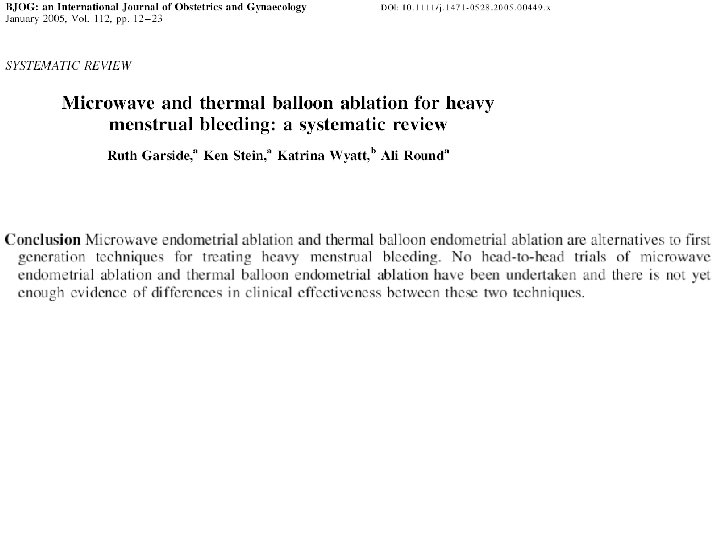
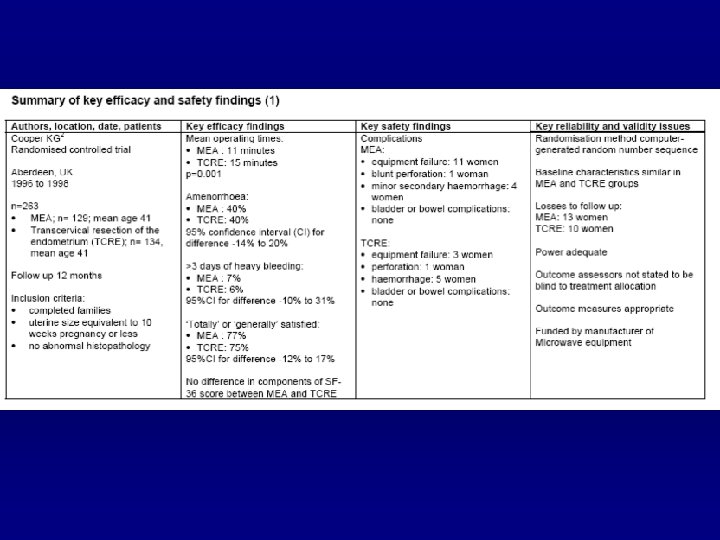
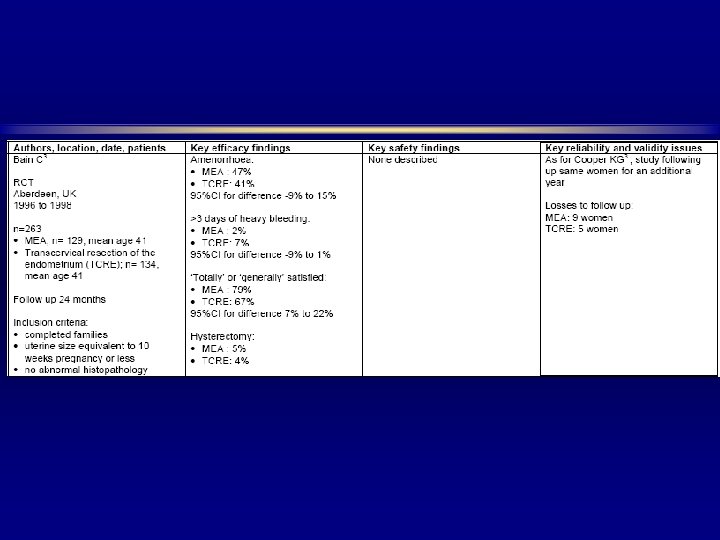
Microwave Endometrial Ablation amenorrhoea rate of 37. 2% patient satisfaction rates of 83. 7% at 3 years Hodgson DA, Feldberg IB, Sharp N, et al. . Microwave Endometrial Ablation: Development, clinical trial and outcomes at three years. Br J Obstet Gynaecol. 1999; 106: 684 -694.

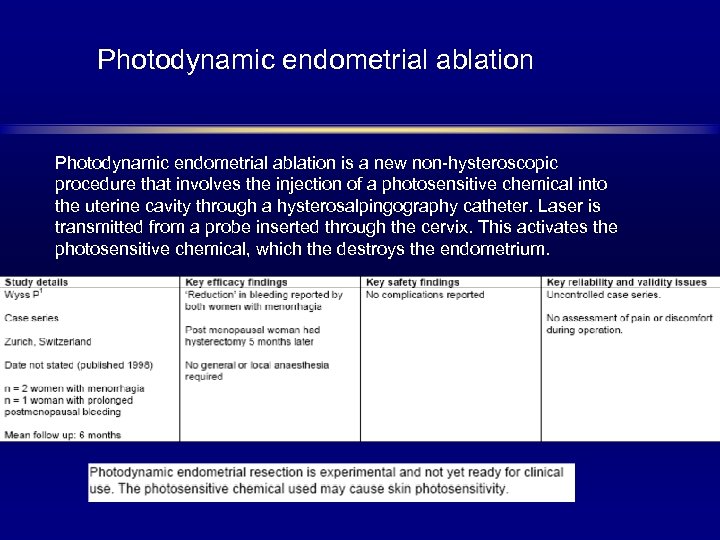
Photodynamic endometrial ablation is a new non-hysteroscopic procedure that involves the injection of a photosensitive chemical into the uterine cavity through a hysterosalpingography catheter. Laser is transmitted from a probe inserted through the cervix. This activates the photosensitive chemical, which the destroys the endometrium.
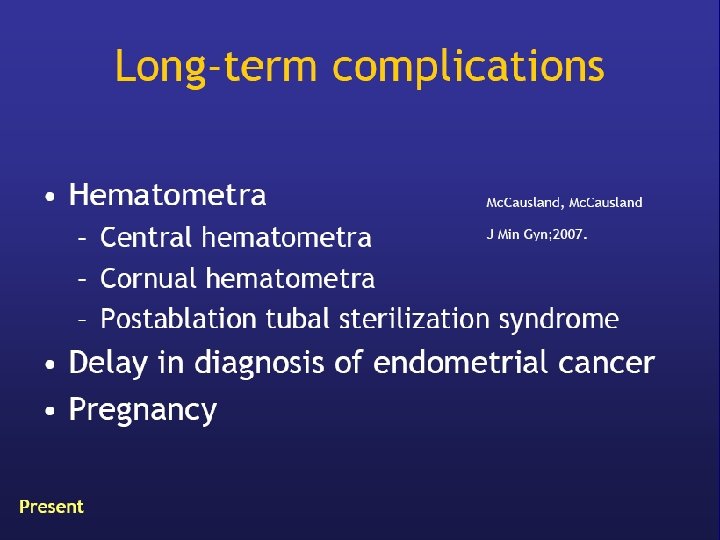
KEY POINTS üThese techniques are easy to learn and use, and offer results comparable to rollerball procedures. Selected patients can be treated successfully in the office setting. üIt is is vital that the patient have a reliable and permanent form of contraception, such as tubal ligation or vasectomy. üLong-term complications, though rare, include endometrial hyperplasia and occult endometrial carcinoma.





Thank You
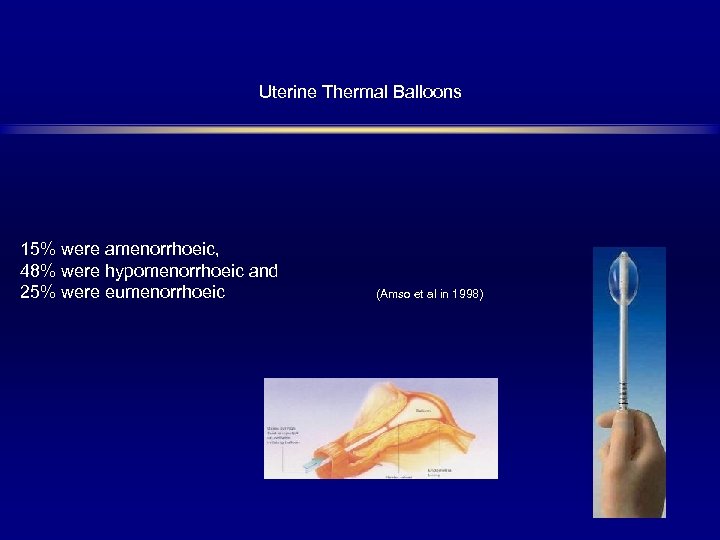
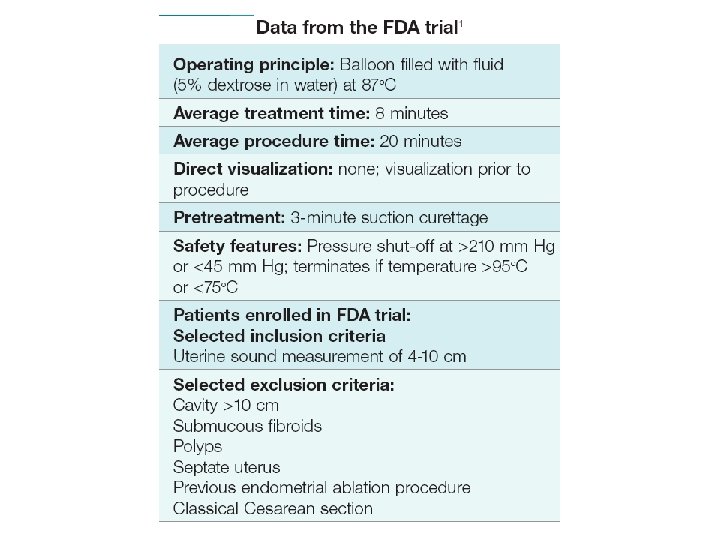
Uterine Thermal Balloons 15% were amenorrhoeic, 48% were hypomenorrhoeic and 25% were eumenorrhoeic (Amso et al in 1998)



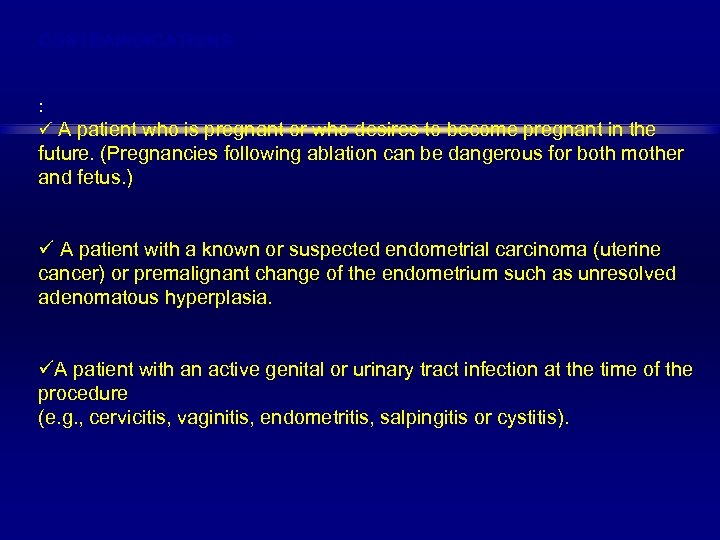
CONTRAINDICATIONS : ü A patient who is pregnant or who desires to become pregnant in the future. (Pregnancies following ablation can be dangerous for both mother and fetus. ) ü A patient with a known or suspected endometrial carcinoma (uterine cancer) or premalignant change of the endometrium such as unresolved adenomatous hyperplasia. üA patient with an active genital or urinary tract infection at the time of the procedure (e. g. , cervicitis, vaginitis, endometritis, salpingitis or cystitis).
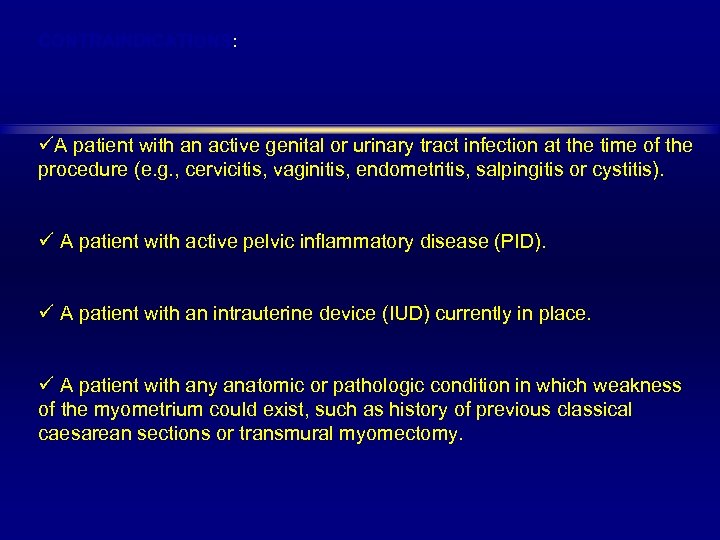
CONTRAINDICATIONS: üA patient with an active genital or urinary tract infection at the time of the procedure (e. g. , cervicitis, vaginitis, endometritis, salpingitis or cystitis). ü A patient with active pelvic inflammatory disease (PID). ü A patient with an intrauterine device (IUD) currently in place. ü A patient with any anatomic or pathologic condition in which weakness of the myometrium could exist, such as history of previous classical caesarean sections or transmural myomectomy.
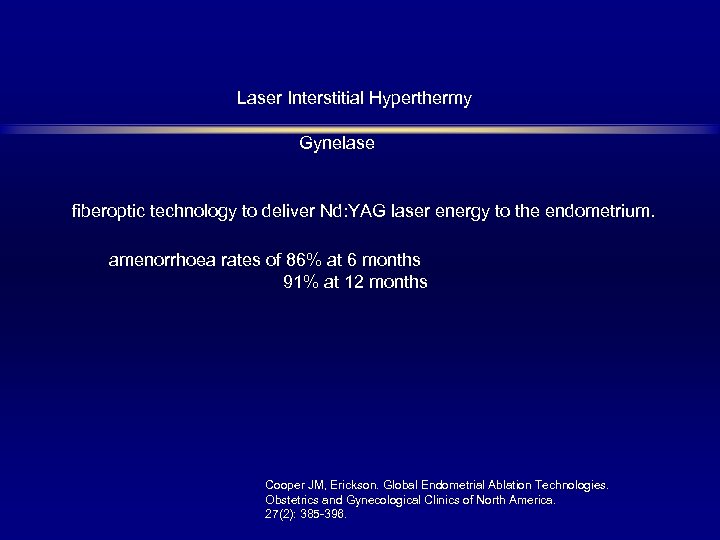
Laser Interstitial Hyperthermy Gynelase fiberoptic technology to deliver Nd: YAG laser energy to the endometrium. amenorrhoea rates of 86% at 6 months 91% at 12 months Cooper JM, Erickson. Global Endometrial Ablation Technologies. Obstetrics and Gynecological Clinics of North America. 27(2): 385 -396.
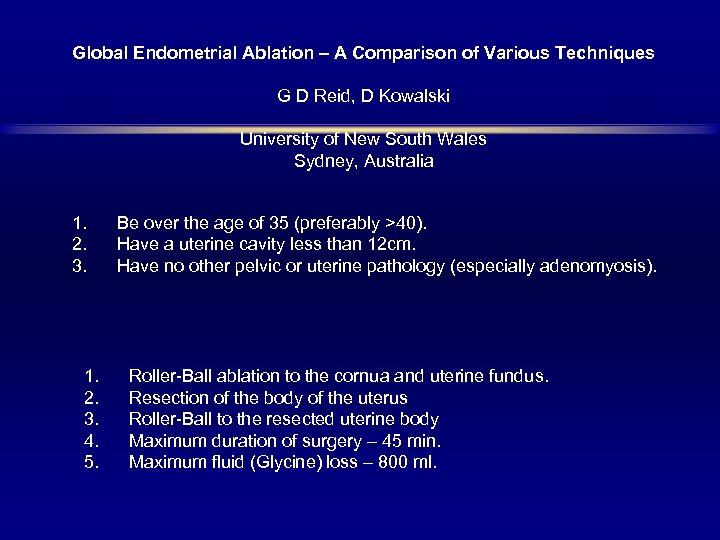
Global Endometrial Ablation – A Comparison of Various Techniques G D Reid, D Kowalski University of New South Wales Sydney, Australia 1. Be over the age of 35 (preferably >40). 2. Have a uterine cavity less than 12 cm. 3. Have no other pelvic or uterine pathology (especially adenomyosis). 1. Roller-Ball ablation to the cornua and uterine fundus. 2. Resection of the body of the uterus 3. Roller-Ball to the resected uterine body 4. Maximum duration of surgery – 45 min. 5. Maximum fluid (Glycine) loss – 800 ml.
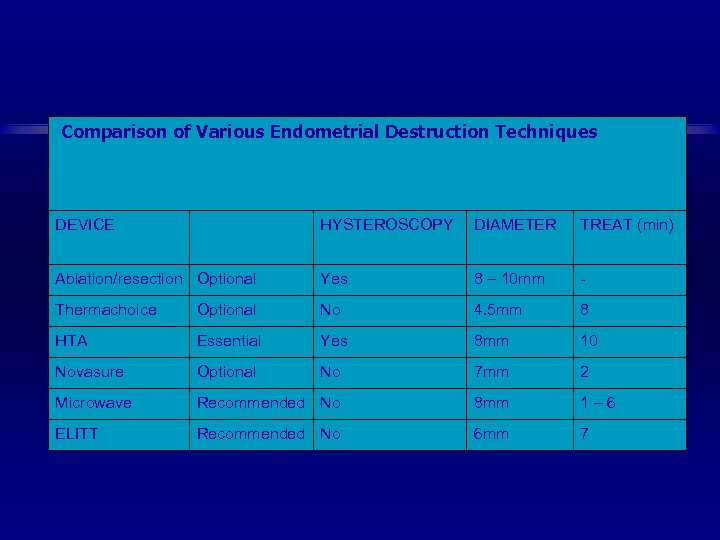
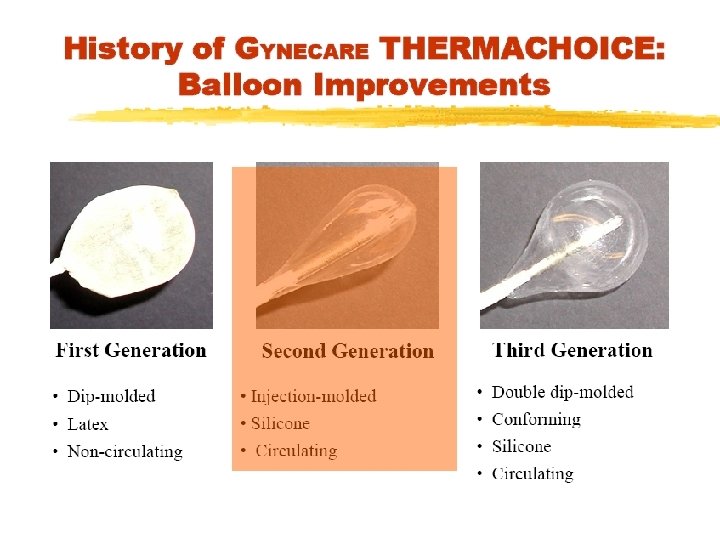
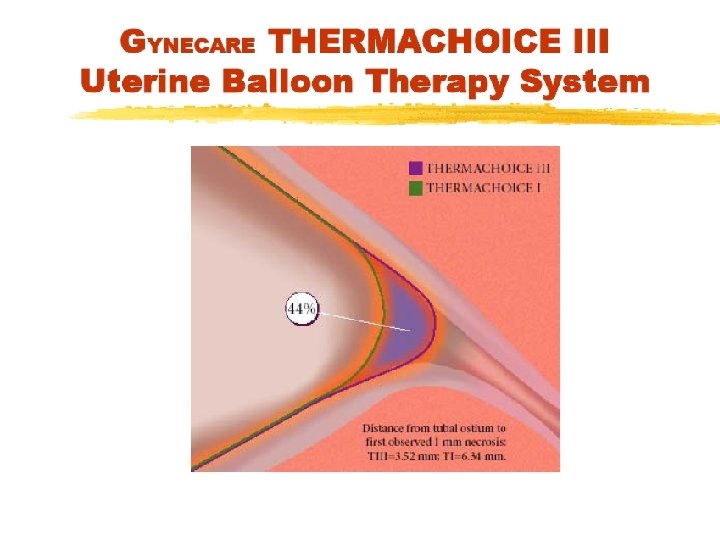
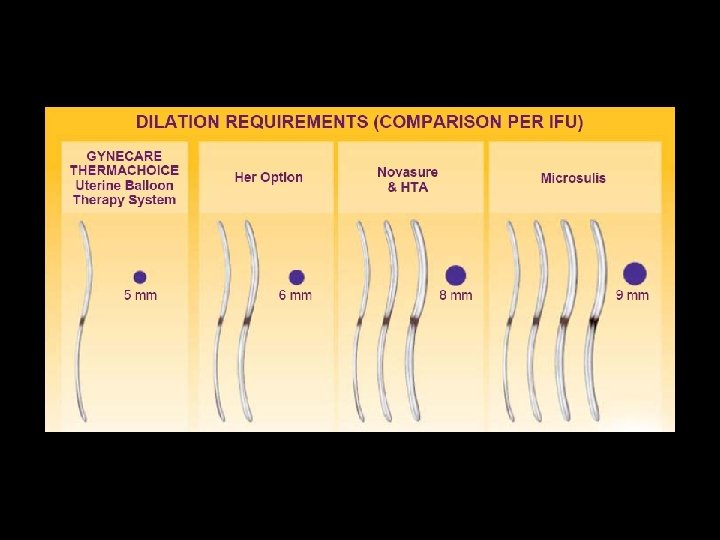
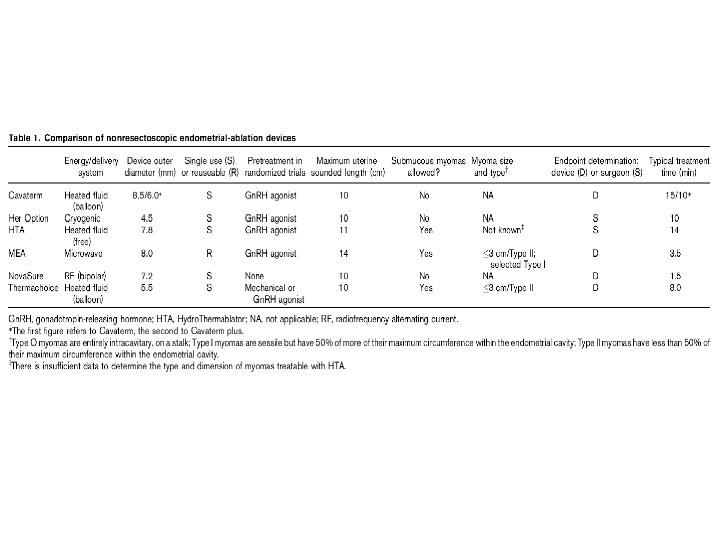
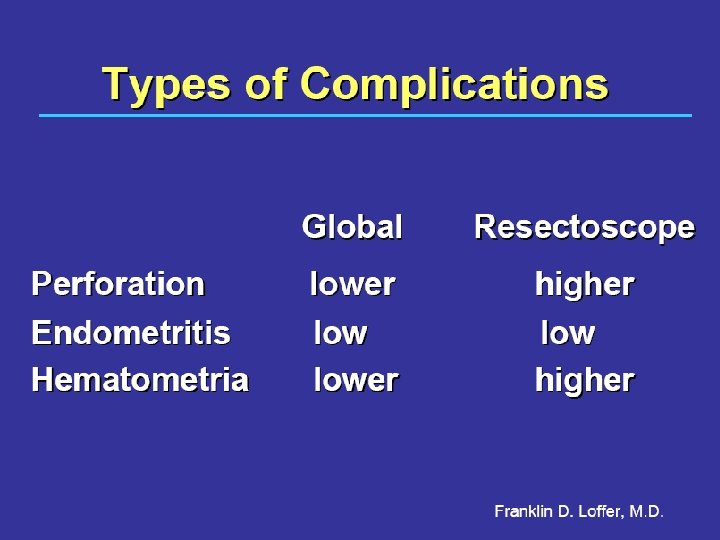
Comparison of Various Endometrial Destruction Techniques DEVICE HYSTEROSCOPY DIAMETER TREAT (min) Ablation/resection Optional Yes 8 – 10 mm - Thermachoice Optional No 4. 5 mm 8 HTA Essential Yes 8 mm 10 Novasure Optional No 7 mm 2 Microwave Recommended No 8 mm 1 – 6 ELITT Recommended No 6 mm 7
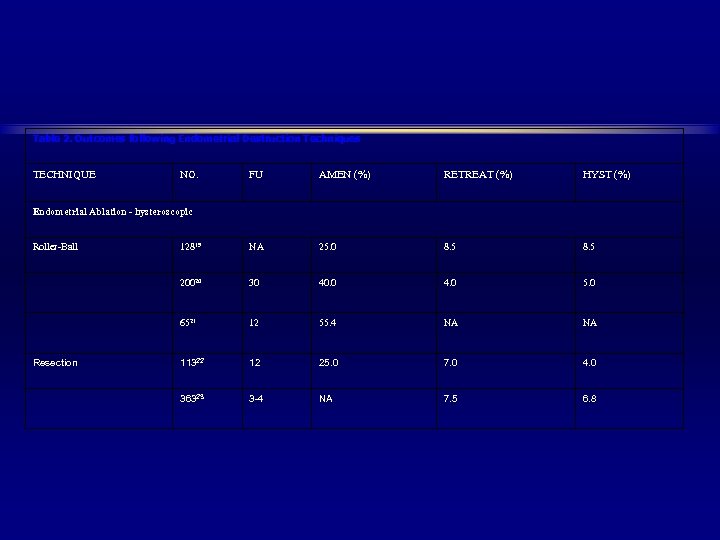
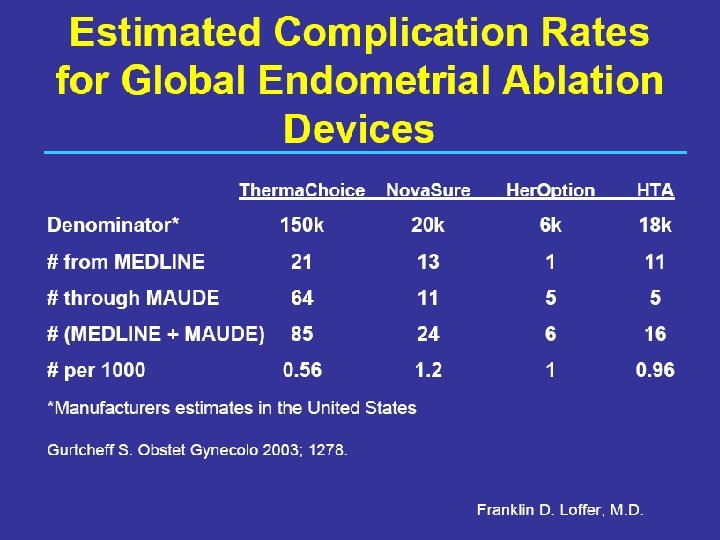
Table 2. Outcomes following Endometrial Destruction Techniques TECHNIQUE NO. FU AMEN (%) RETREAT (%) HYST (%) Endometrial Ablation - hysteroscopic Roller-Ball 12819 NA 25. 0 8. 5 20020 30 40. 0 4. 0 5. 0 6521 12 55. 4 NA NA Resection 11322 12 25. 0 7. 0 4. 0 36323 3 -4 NA 7. 5 6. 8
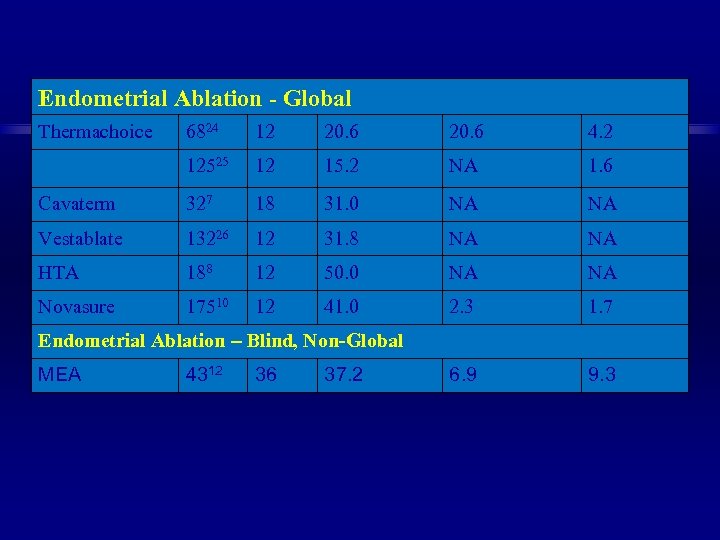
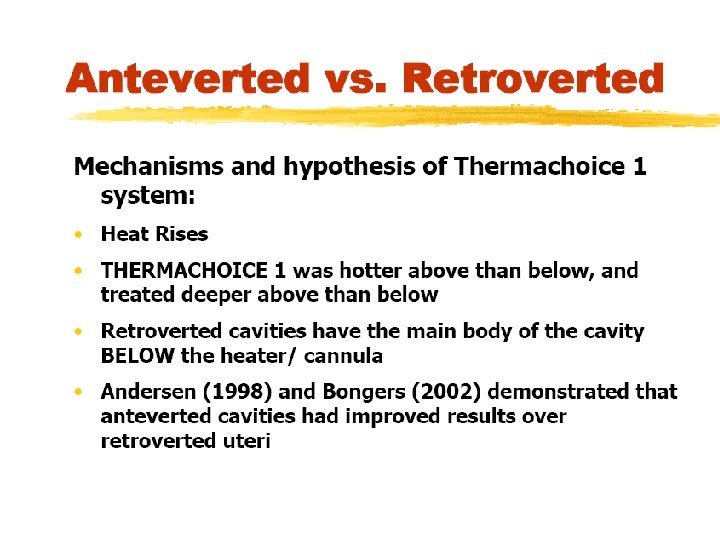
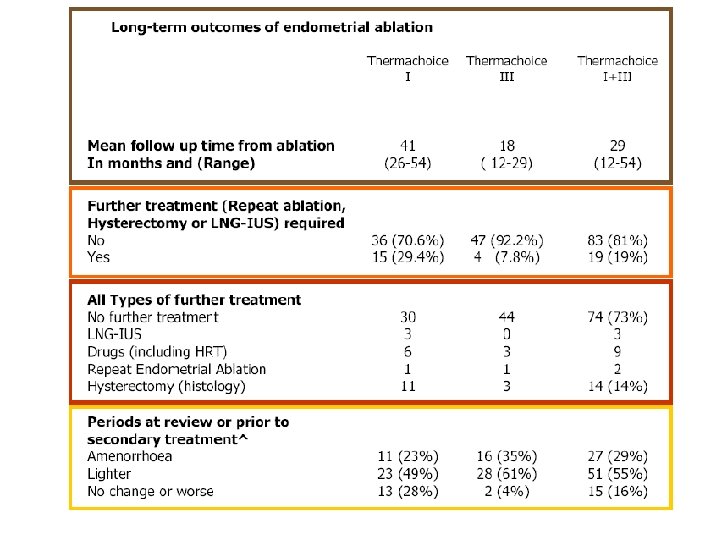
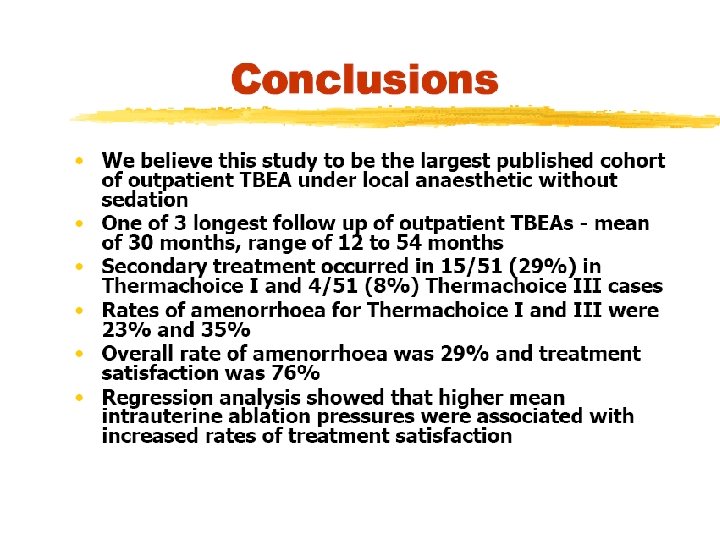
Endometrial Ablation - Global Thermachoice 6824 12 20. 6 4. 2 12525 12 15. 2 NA 1. 6 Cavaterm 327 18 31. 0 NA NA Vestablate 13226 12 31. 8 NA NA HTA 188 12 50. 0 NA NA Novasure 17510 12 41. 0 2. 3 1. 7 6. 9 9. 3 Endometrial Ablation – Blind, Non-Global MEA 4312 36 37. 2
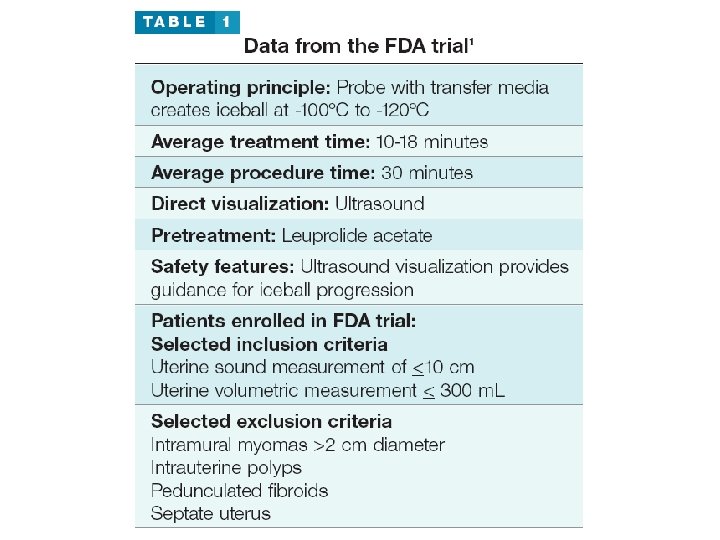
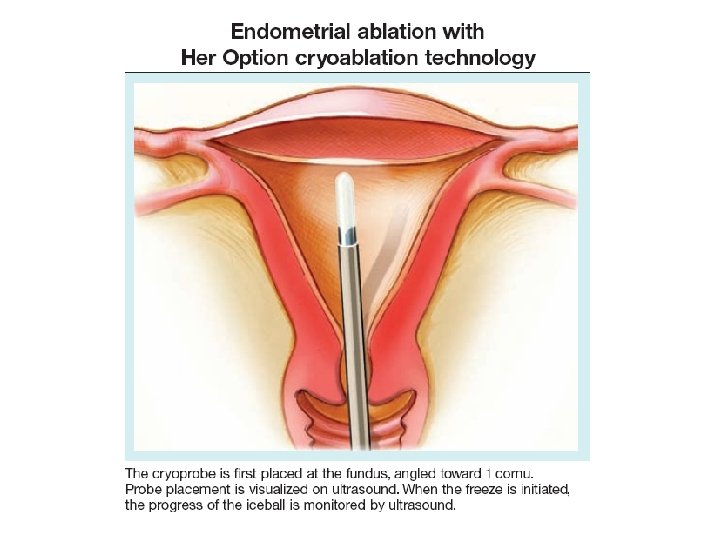
Key points üGlobal ablation methods involve destroying the endometrium using specialized devices that do not require an operative hysteroscope or resectoscope. üThe endometrium should be destroyed or resected to the level of the basalis, which is approximately 4 to 6 mm deep. üIn cryoablation, freezing the tissue causes less pain than the heat energy associated with other ablation devices. The procedure typically takes 10 to 20 minutes. üNot only is bipolar desiccation quick and simple, no endometrial pretreatment is required because the system allows for consistent depths of ablation regardless of endometrial thickness. üThe advantage of hydrothermal ablation is that the circulating hot saline solution contacts the entire endometrial surface regardless of the shape or size of the cavity.
The thinner the endometrial lining, the more likely ablation will be successful
Patient selection INDICATIONS • Women with menorrhagia/metrorrhagia due to benign disease who have not responded to medical therapy, e. g. , non-steroidal anti-inflammatory drugs, oral contraceptives, and antifibrinolytic agents, or dilatation and curettage and who do not desire future fertility or a hysterectomy CONTRAINDICATIONS • Abnormal uterine bleeding due to endometrial polyps, submucous and intramural myomata, or adenomyosis • Endometrial cancer • History of endometrial cancer or hyperplasia • A desire of amenorrhea for social reasons
Cryoablation 54% of 222 patients experienced amenorrhea
430151292d48805d1d1aa1541e7ac841.ppt