4f21bdb4d1eb419653644a70e4ff218d.ppt
- Количество слайдов: 45
 The Elderly Patient and Peritoneal Dialysis Fredric O. Finkelstein Clinical Professor of Medicine Yale University New Haven, CT USA
The Elderly Patient and Peritoneal Dialysis Fredric O. Finkelstein Clinical Professor of Medicine Yale University New Haven, CT USA
 Points to be Covered • Increasing number of elderly patients with ESRD • Need to be clear about the goals and objectives of therapies • PD has certain advantages as well as disadvantages in the elderly • Certain issues need to be kept in mind in discussing PD utilization in the elderly
Points to be Covered • Increasing number of elderly patients with ESRD • Need to be clear about the goals and objectives of therapies • PD has certain advantages as well as disadvantages in the elderly • Certain issues need to be kept in mind in discussing PD utilization in the elderly
 Questions to be Answered • Why are so few elderly patients on PD? • Is there a higher mortality or complication rate in elderly patients on PD compared to HD? • Is there a higher technique failure and/or peritonitis rate in the elderly PD patient compared to younger patients? • Is the quality of life worse in the elderly patient on PD than on HD? • What can we do to improve the quality of life of the elderly patient maintained on PD?
Questions to be Answered • Why are so few elderly patients on PD? • Is there a higher mortality or complication rate in elderly patients on PD compared to HD? • Is there a higher technique failure and/or peritonitis rate in the elderly PD patient compared to younger patients? • Is the quality of life worse in the elderly patient on PD than on HD? • What can we do to improve the quality of life of the elderly patient maintained on PD?
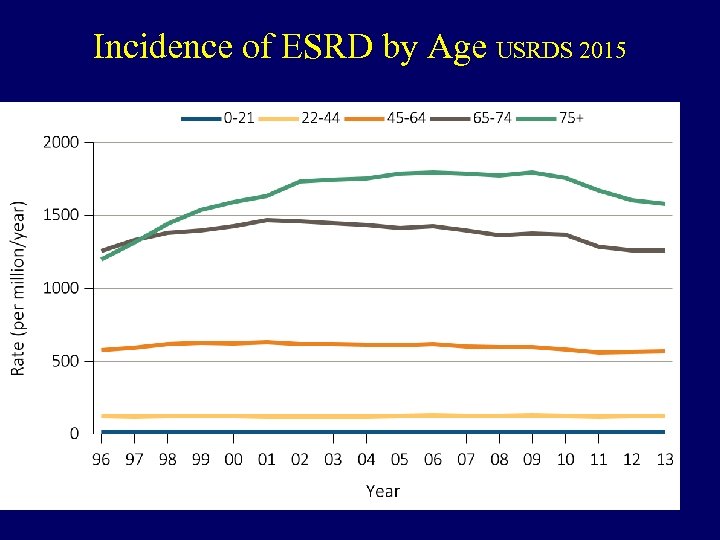 Incidence of ESRD by Age USRDS 2015
Incidence of ESRD by Age USRDS 2015
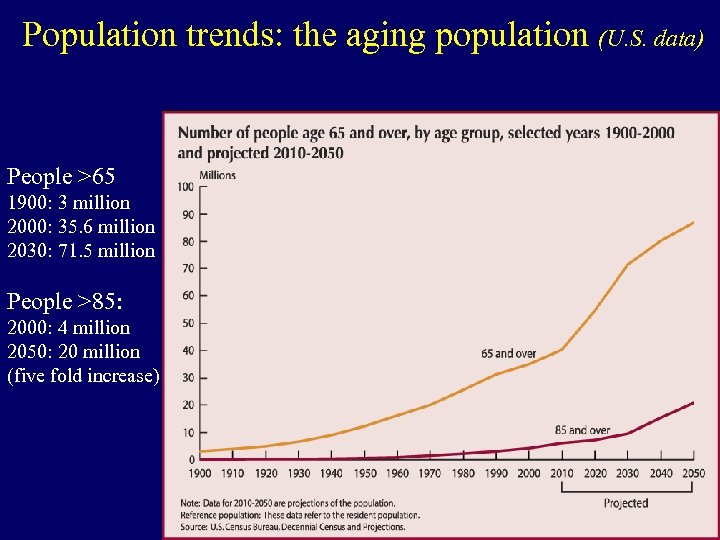 Population trends: the aging population (U. S. data) People >65 1900: 3 million 2000: 35. 6 million 2030: 71. 5 million People >85: 2000: 4 million 2050: 20 million (five fold increase)
Population trends: the aging population (U. S. data) People >65 1900: 3 million 2000: 35. 6 million 2030: 71. 5 million People >85: 2000: 4 million 2050: 20 million (five fold increase)
 Lucas Cranach: The Fountain of Youth, 1546, Berlin Gemalderie
Lucas Cranach: The Fountain of Youth, 1546, Berlin Gemalderie
 Thomas Cole: Voyage of Life: Youth, 1842, National Gallery, Washington
Thomas Cole: Voyage of Life: Youth, 1842, National Gallery, Washington
 Thomas Cole: The Voyage of Life: Old Age, 1842, National Gallery, Washington, DC
Thomas Cole: The Voyage of Life: Old Age, 1842, National Gallery, Washington, DC
 What Is the Goal of Treatment? • • Alleviate symptoms? Prevent development of symptoms? Maximize longevity? Conform to standard guidelines?
What Is the Goal of Treatment? • • Alleviate symptoms? Prevent development of symptoms? Maximize longevity? Conform to standard guidelines?
 Indications to Start Dialysis Urgent Indications “Uremic” symptoms • • • Pericarditis Acute neurological problems Metabolic problems Unmanageable fluid overload Fatigue Lethargy Cognitive impairment Neuropathy Uremic pruritus Sleep disorders Anorexia, nausea Restless leg syndrome
Indications to Start Dialysis Urgent Indications “Uremic” symptoms • • • Pericarditis Acute neurological problems Metabolic problems Unmanageable fluid overload Fatigue Lethargy Cognitive impairment Neuropathy Uremic pruritus Sleep disorders Anorexia, nausea Restless leg syndrome
 Symptom Burden in CKD/ESRD • • • Pain (proprioceptive or neuropathic, nociceptive) Pruritis • GI symptoms: anorexia, nausea, constipation, Sleep disorders diarrhea Restless legs • Cardiac symptoms: chest Depression pain, edema, DOE, etc Anxiety Impaired physical functioning Loss of energy, vitality Key Question: to what Sexual dysfunction extent are the symptoms Cognitive dysfunction impacting on the patient’s Impact of the dialysis regimen (e. g. post hemodialysis recovery time) quality of life? Risks of treatment vs the benefits
Symptom Burden in CKD/ESRD • • • Pain (proprioceptive or neuropathic, nociceptive) Pruritis • GI symptoms: anorexia, nausea, constipation, Sleep disorders diarrhea Restless legs • Cardiac symptoms: chest Depression pain, edema, DOE, etc Anxiety Impaired physical functioning Loss of energy, vitality Key Question: to what Sexual dysfunction extent are the symptoms Cognitive dysfunction impacting on the patient’s Impact of the dialysis regimen (e. g. post hemodialysis recovery time) quality of life? Risks of treatment vs the benefits
 How Does the Initiation of Dialysis Impact On These Symptoms: CHOICE Study Wu et al JASN 2004 15: 743 -53 • Changes were examined over 1 yr using the CHEK questionnaire includes the SF-36 and 14 dialysis specific domains • On the 8 SF-36 domains, 20 to 31% of patients had a worsening, 42 to 60% had no change, and 19 to 28% had an improvement • In the dialysis specific domains, 19 to 30% had a worsening, 50 to 65% had no change, and 16 to 24% had an improvement
How Does the Initiation of Dialysis Impact On These Symptoms: CHOICE Study Wu et al JASN 2004 15: 743 -53 • Changes were examined over 1 yr using the CHEK questionnaire includes the SF-36 and 14 dialysis specific domains • On the 8 SF-36 domains, 20 to 31% of patients had a worsening, 42 to 60% had no change, and 19 to 28% had an improvement • In the dialysis specific domains, 19 to 30% had a worsening, 50 to 65% had no change, and 16 to 24% had an improvement
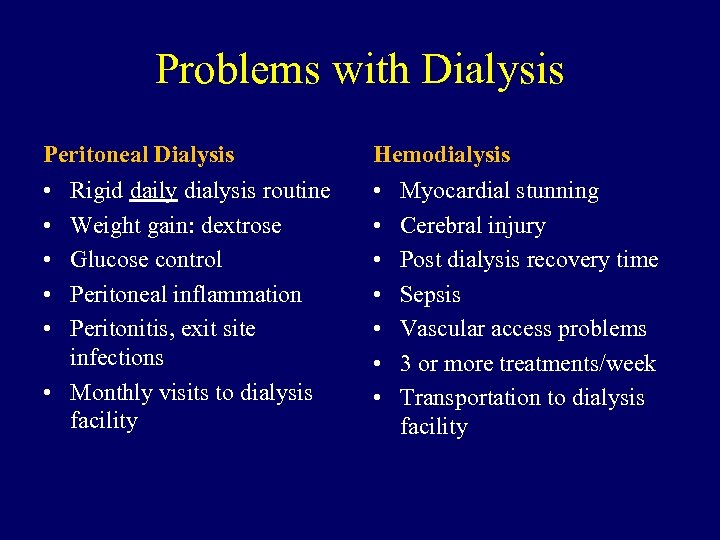 Problems with Dialysis Peritoneal Dialysis Hemodialysis • • • Rigid daily dialysis routine Weight gain: dextrose Glucose control Peritoneal inflammation Peritonitis, exit site infections • Monthly visits to dialysis facility Myocardial stunning Cerebral injury Post dialysis recovery time Sepsis Vascular access problems 3 or more treatments/week Transportation to dialysis facility
Problems with Dialysis Peritoneal Dialysis Hemodialysis • • • Rigid daily dialysis routine Weight gain: dextrose Glucose control Peritoneal inflammation Peritonitis, exit site infections • Monthly visits to dialysis facility Myocardial stunning Cerebral injury Post dialysis recovery time Sepsis Vascular access problems 3 or more treatments/week Transportation to dialysis facility
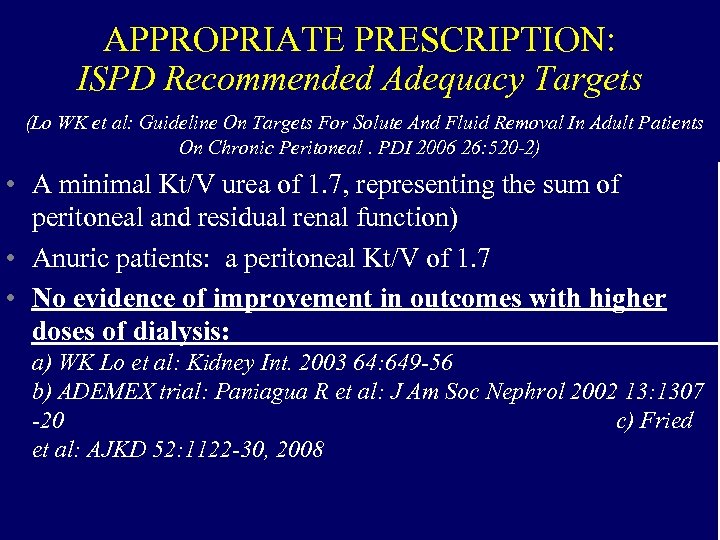 APPROPRIATE PRESCRIPTION: ISPD Recommended Adequacy Targets (Lo WK et al: Guideline On Targets For Solute And Fluid Removal In Adult Patients On Chronic Peritoneal. PDI 2006 26: 520 -2) • A minimal Kt/V urea of 1. 7, representing the sum of peritoneal and residual renal function) • Anuric patients: a peritoneal Kt/V of 1. 7 • No evidence of improvement in outcomes with higher doses of dialysis: a) WK Lo et al: Kidney Int. 2003 64: 649 -56 b) ADEMEX trial: Paniagua R et al: J Am Soc Nephrol 2002 13: 1307 -20 c) Fried et al: AJKD 52: 1122 -30, 2008 14
APPROPRIATE PRESCRIPTION: ISPD Recommended Adequacy Targets (Lo WK et al: Guideline On Targets For Solute And Fluid Removal In Adult Patients On Chronic Peritoneal. PDI 2006 26: 520 -2) • A minimal Kt/V urea of 1. 7, representing the sum of peritoneal and residual renal function) • Anuric patients: a peritoneal Kt/V of 1. 7 • No evidence of improvement in outcomes with higher doses of dialysis: a) WK Lo et al: Kidney Int. 2003 64: 649 -56 b) ADEMEX trial: Paniagua R et al: J Am Soc Nephrol 2002 13: 1307 -20 c) Fried et al: AJKD 52: 1122 -30, 2008 14
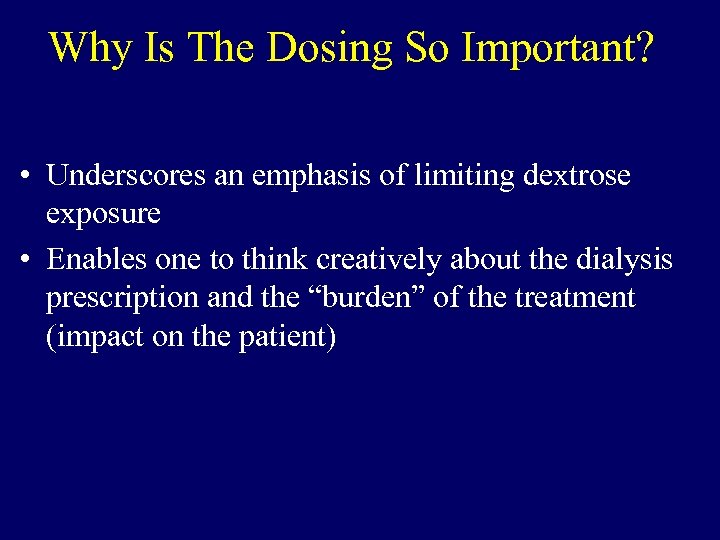 Why Is The Dosing So Important? • Underscores an emphasis of limiting dextrose exposure • Enables one to think creatively about the dialysis prescription and the “burden” of the treatment (impact on the patient)
Why Is The Dosing So Important? • Underscores an emphasis of limiting dextrose exposure • Enables one to think creatively about the dialysis prescription and the “burden” of the treatment (impact on the patient)
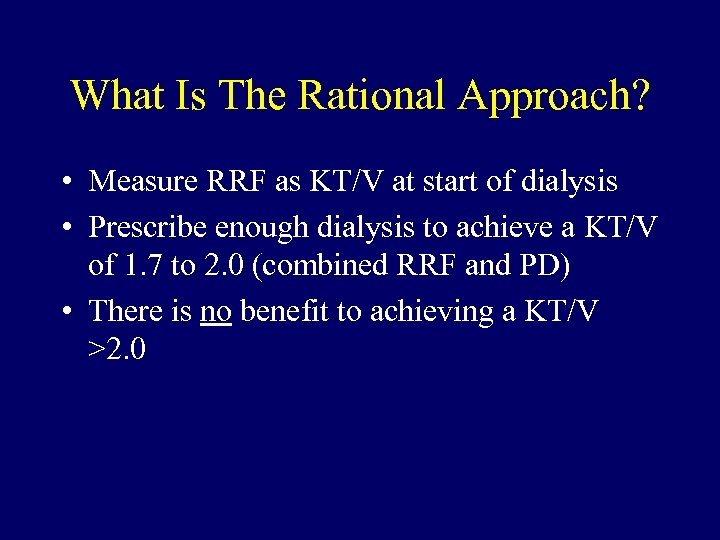 What Is The Rational Approach? • Measure RRF as KT/V at start of dialysis • Prescribe enough dialysis to achieve a KT/V of 1. 7 to 2. 0 (combined RRF and PD) • There is no benefit to achieving a KT/V >2. 0
What Is The Rational Approach? • Measure RRF as KT/V at start of dialysis • Prescribe enough dialysis to achieve a KT/V of 1. 7 to 2. 0 (combined RRF and PD) • There is no benefit to achieving a KT/V >2. 0
 New Haven Protocol • Patient is going to start PD: measure a 24 hour urine for KT/V urea • Model dose of PD necessary to achieve a KT/V >1. 7 but <2. 0 • Preferred model: 2 exchanges per day for those with endogenous KT/V of 1 or higher • Discuss with patient the need to increase dose if RRF declines
New Haven Protocol • Patient is going to start PD: measure a 24 hour urine for KT/V urea • Model dose of PD necessary to achieve a KT/V >1. 7 but <2. 0 • Preferred model: 2 exchanges per day for those with endogenous KT/V of 1 or higher • Discuss with patient the need to increase dose if RRF declines
 Other Options • Dialysis 5 or 6 days/week • Low dose cycler therapy with a dry day • 2 exchanges per day – with part of the day dry
Other Options • Dialysis 5 or 6 days/week • Low dose cycler therapy with a dry day • 2 exchanges per day – with part of the day dry
 Assisted PD • Nurses or trained individual attaches patients to cycler and disconnects in the morning (French model) • Trained individual sets machine up during day and patient makes connections and disconnections (Canadian and UK model) • Family member(s) assist (U. S. and other countries model) • Nursing home or rehabilitation facility does PD
Assisted PD • Nurses or trained individual attaches patients to cycler and disconnects in the morning (French model) • Trained individual sets machine up during day and patient makes connections and disconnections (Canadian and UK model) • Family member(s) assist (U. S. and other countries model) • Nursing home or rehabilitation facility does PD
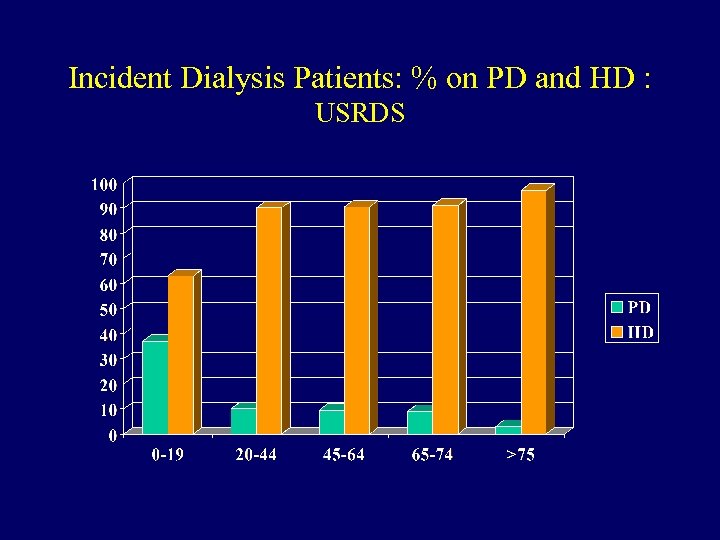 Incident Dialysis Patients: % on PD and HD : USRDS
Incident Dialysis Patients: % on PD and HD : USRDS
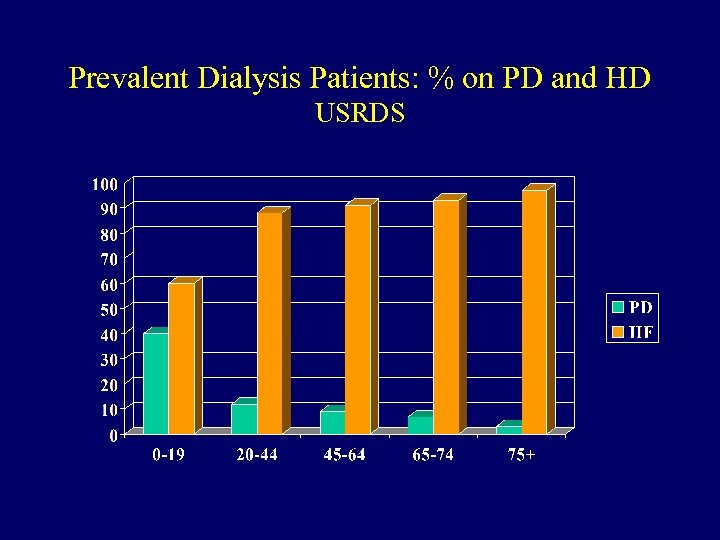 Prevalent Dialysis Patients: % on PD and HD USRDS
Prevalent Dialysis Patients: % on PD and HD USRDS
 Potential problems associated with elderly PD patients • High frequency of co-morbid diseases, including vascular disease and arthritis • Impaired mobility • Cognitive difficulties • Living environment: potential problem • Nutrition • Compliance with home regimen
Potential problems associated with elderly PD patients • High frequency of co-morbid diseases, including vascular disease and arthritis • Impaired mobility • Cognitive difficulties • Living environment: potential problem • Nutrition • Compliance with home regimen
 But What Does the Data Show for Elderly Patients on PD? • No difference in mortality rates compared to HD patients • Higher mortality rate compared to younger patients • No difference in overall peritonitis rates compared to younger patients • No difference (or lower) technique failure rate compared to younger patients
But What Does the Data Show for Elderly Patients on PD? • No difference in mortality rates compared to HD patients • Higher mortality rate compared to younger patients • No difference in overall peritonitis rates compared to younger patients • No difference (or lower) technique failure rate compared to younger patients
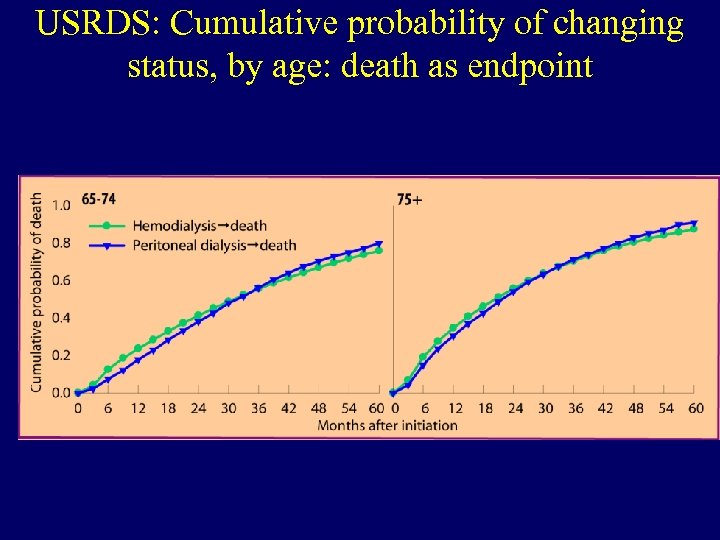 USRDS: Cumulative probability of changing status, by age: death as endpoint illi lla
USRDS: Cumulative probability of changing status, by age: death as endpoint illi lla
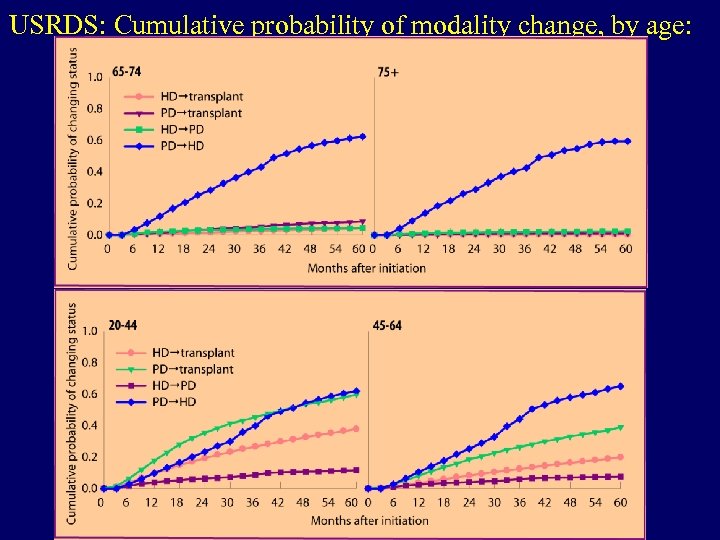 USRDS: Cumulative probability of modality change, by age:
USRDS: Cumulative probability of modality change, by age:
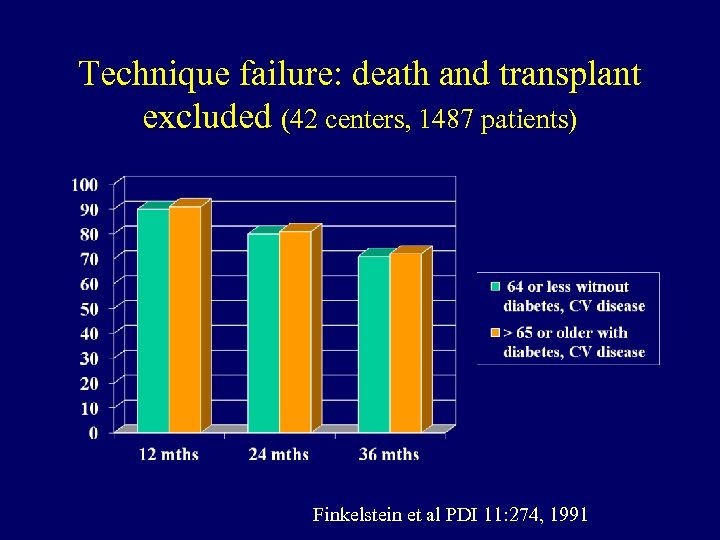 Technique failure: death and transplant excluded (42 centers, 1487 patients) Finkelstein et al PDI 11: 274, 1991
Technique failure: death and transplant excluded (42 centers, 1487 patients) Finkelstein et al PDI 11: 274, 1991
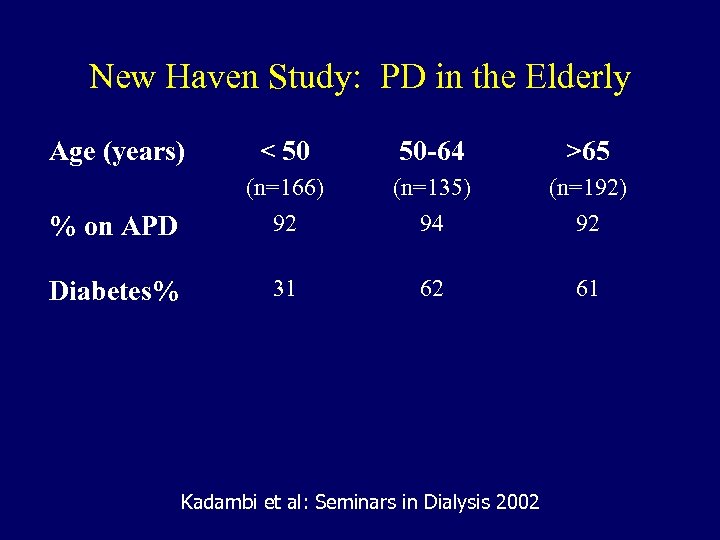 New Haven Study: PD in the Elderly Age (years) < 50 50 -64 >65 % on APD (n=166) 92 (n=135) 94 (n=192) 92 Diabetes% 31 62 61 Kadambi et al: Seminars in Dialysis 2002
New Haven Study: PD in the Elderly Age (years) < 50 50 -64 >65 % on APD (n=166) 92 (n=135) 94 (n=192) 92 Diabetes% 31 62 61 Kadambi et al: Seminars in Dialysis 2002
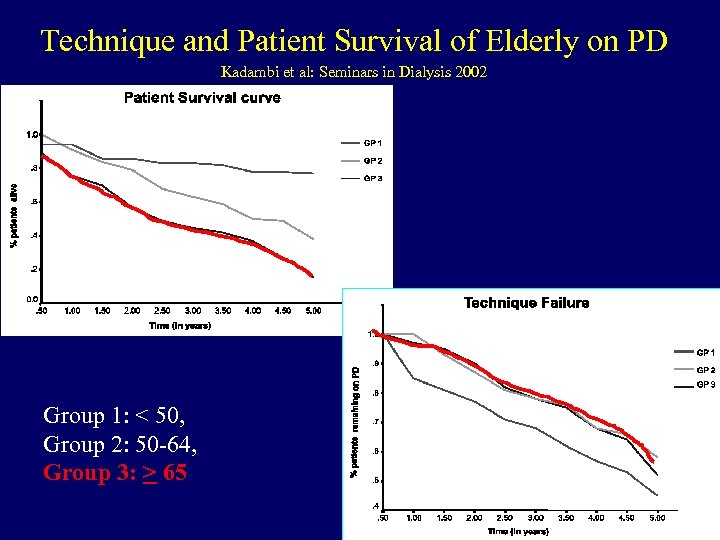 Technique and Patient Survival of Elderly on PD Kadambi et al: Seminars in Dialysis 2002 Group 1: < 50, Group 2: 50 -64, Group 3: > 65
Technique and Patient Survival of Elderly on PD Kadambi et al: Seminars in Dialysis 2002 Group 1: < 50, Group 2: 50 -64, Group 3: > 65
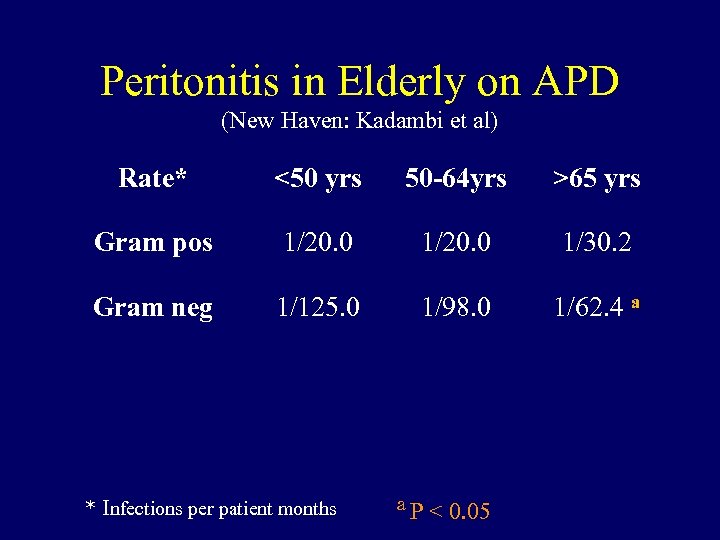 Peritonitis in Elderly on APD (New Haven: Kadambi et al) Rate* <50 yrs 50 -64 yrs >65 yrs Gram pos 1/20. 0 1/30. 2 Gram neg 1/125. 0 1/98. 0 1/62. 4 a * Infections per patient months a. P < 0. 05
Peritonitis in Elderly on APD (New Haven: Kadambi et al) Rate* <50 yrs 50 -64 yrs >65 yrs Gram pos 1/20. 0 1/30. 2 Gram neg 1/125. 0 1/98. 0 1/62. 4 a * Infections per patient months a. P < 0. 05
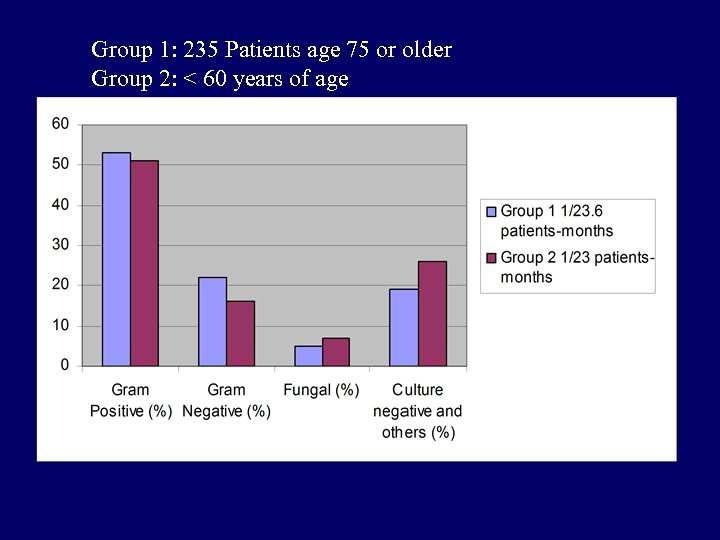 Group 1: 235 Patients age 75 or older Group 2: < 60 years of age
Group 1: 235 Patients age 75 or older Group 2: < 60 years of age
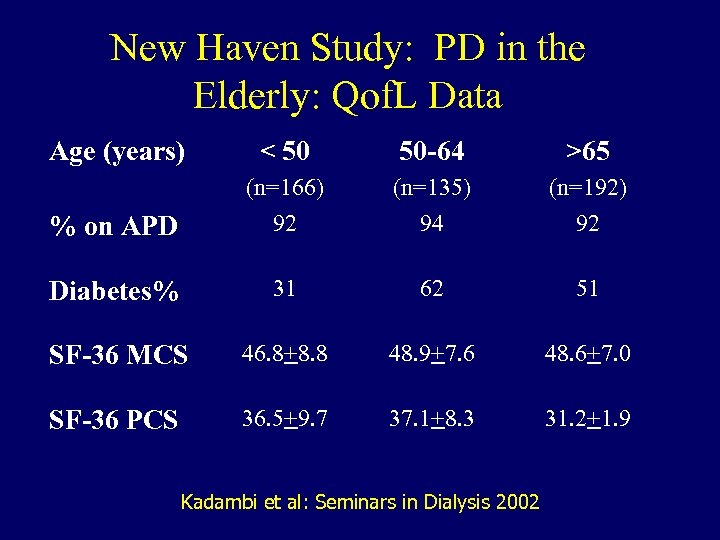 New Haven Study: PD in the Elderly: Qof. L Data Age (years) < 50 50 -64 >65 % on APD (n=166) 92 (n=135) 94 (n=192) 92 Diabetes% 31 62 51 SF-36 MCS 46. 8+8. 8 48. 9+7. 6 48. 6+7. 0 SF-36 PCS 36. 5+9. 7 37. 1+8. 3 31. 2+1. 9 Kadambi et al: Seminars in Dialysis 2002
New Haven Study: PD in the Elderly: Qof. L Data Age (years) < 50 50 -64 >65 % on APD (n=166) 92 (n=135) 94 (n=192) 92 Diabetes% 31 62 51 SF-36 MCS 46. 8+8. 8 48. 9+7. 6 48. 6+7. 0 SF-36 PCS 36. 5+9. 7 37. 1+8. 3 31. 2+1. 9 Kadambi et al: Seminars in Dialysis 2002
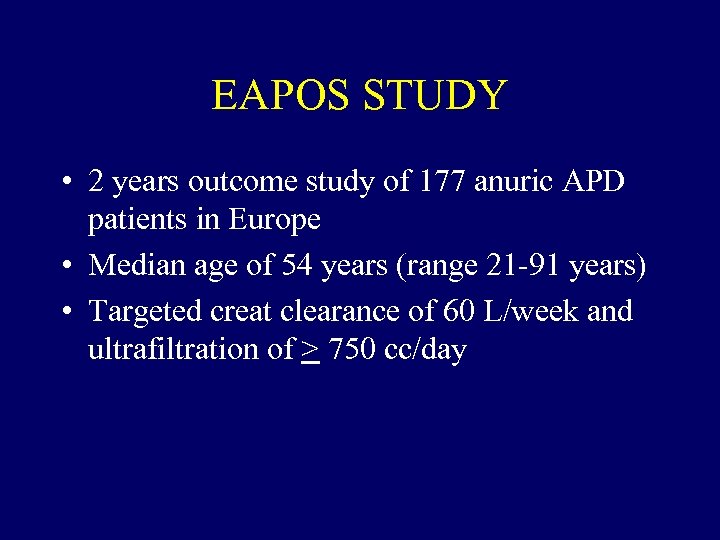 EAPOS STUDY • 2 years outcome study of 177 anuric APD patients in Europe • Median age of 54 years (range 21 -91 years) • Targeted creat clearance of 60 L/week and ultrafiltration of > 750 cc/day
EAPOS STUDY • 2 years outcome study of 177 anuric APD patients in Europe • Median age of 54 years (range 21 -91 years) • Targeted creat clearance of 60 L/week and ultrafiltration of > 750 cc/day
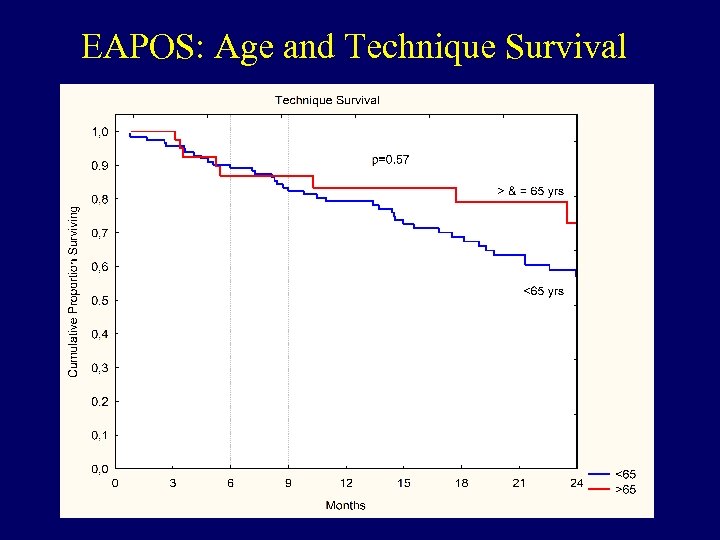 EAPOS: Age and Technique Survival
EAPOS: Age and Technique Survival
 North Thames Dialysis Study (NTDS) • 12 month prospective cohort study to evaluate clinical outcomes, quality of life (QOL) and costs in elderly dialysis patients • Elderly defined as > 70 years old at start of dialysis • Chronic dialysis defined according to the USRDS 90 day rule • All eligible patients from 4 centers included in study Lamping et al, Lancet 2000; Harris S et al, PDI 2002
North Thames Dialysis Study (NTDS) • 12 month prospective cohort study to evaluate clinical outcomes, quality of life (QOL) and costs in elderly dialysis patients • Elderly defined as > 70 years old at start of dialysis • Chronic dialysis defined according to the USRDS 90 day rule • All eligible patients from 4 centers included in study Lamping et al, Lancet 2000; Harris S et al, PDI 2002
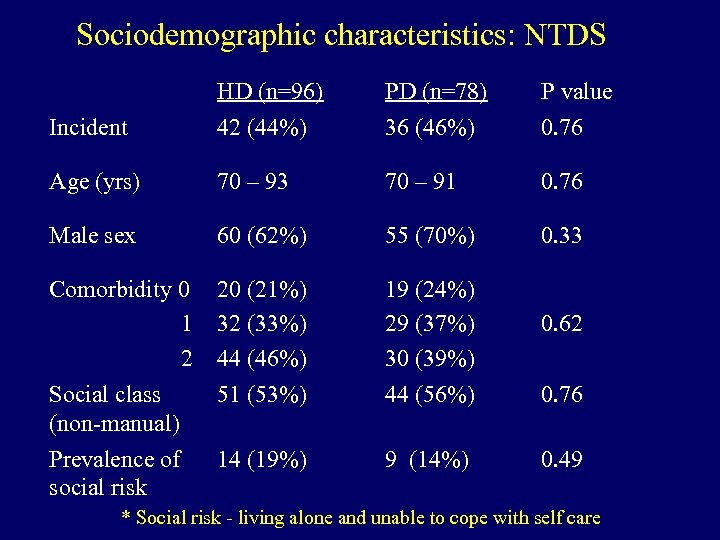 Sociodemographic characteristics: NTDS Incident HD (n=96) 42 (44%) PD (n=78) 36 (46%) P value 0. 76 Age (yrs) 70 – 93 70 – 91 0. 76 Male sex 60 (62%) 55 (70%) 0. 33 Comorbidity 0 1 2 Social class (non-manual) 20 (21%) 32 (33%) 44 (46%) 51 (53%) 19 (24%) 29 (37%) 30 (39%) 44 (56%) Prevalence of social risk 14 (19%) 9 (14%) 0. 62 0. 76 0. 49 * Social risk - living alone and unable to cope with self care
Sociodemographic characteristics: NTDS Incident HD (n=96) 42 (44%) PD (n=78) 36 (46%) P value 0. 76 Age (yrs) 70 – 93 70 – 91 0. 76 Male sex 60 (62%) 55 (70%) 0. 33 Comorbidity 0 1 2 Social class (non-manual) 20 (21%) 32 (33%) 44 (46%) 51 (53%) 19 (24%) 29 (37%) 30 (39%) 44 (56%) Prevalence of social risk 14 (19%) 9 (14%) 0. 62 0. 76 0. 49 * Social risk - living alone and unable to cope with self care
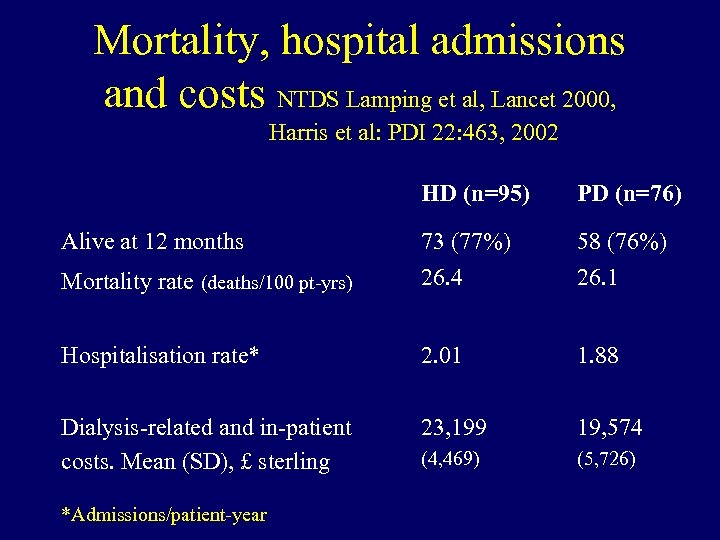 Mortality, hospital admissions and costs NTDS Lamping et al, Lancet 2000, Harris et al: PDI 22: 463, 2002 HD (n=95) PD (n=76) Mortality rate (deaths/100 pt-yrs) 73 (77%) 26. 4 58 (76%) 26. 1 Hospitalisation rate* 2. 01 1. 88 Dialysis-related and in-patient costs. Mean (SD), £ sterling 23, 199 19, 574 (4, 469) (5, 726) Alive at 12 months *Admissions/patient-year
Mortality, hospital admissions and costs NTDS Lamping et al, Lancet 2000, Harris et al: PDI 22: 463, 2002 HD (n=95) PD (n=76) Mortality rate (deaths/100 pt-yrs) 73 (77%) 26. 4 58 (76%) 26. 1 Hospitalisation rate* 2. 01 1. 88 Dialysis-related and in-patient costs. Mean (SD), £ sterling 23, 199 19, 574 (4, 469) (5, 726) Alive at 12 months *Admissions/patient-year
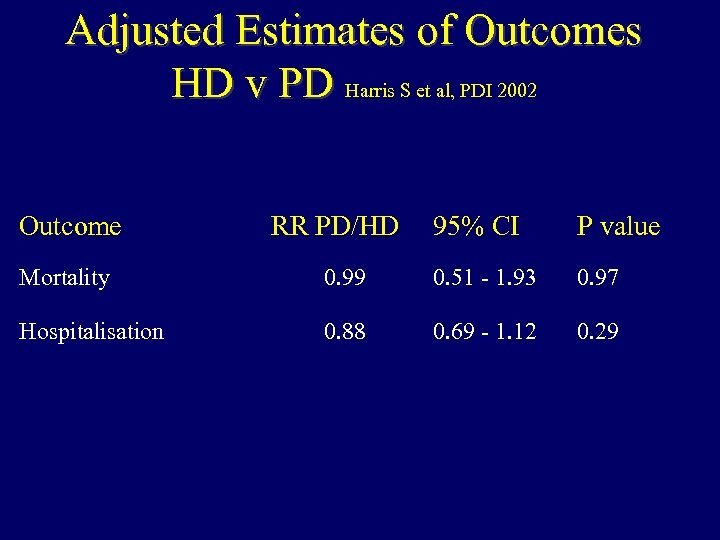 Adjusted Estimates of Outcomes HD v PD Harris S et al, PDI 2002 Outcome RR PD/HD 95% CI P value Mortality 0. 99 0. 51 - 1. 93 0. 97 Hospitalisation 0. 88 0. 69 - 1. 12 0. 29
Adjusted Estimates of Outcomes HD v PD Harris S et al, PDI 2002 Outcome RR PD/HD 95% CI P value Mortality 0. 99 0. 51 - 1. 93 0. 97 Hospitalisation 0. 88 0. 69 - 1. 12 0. 29
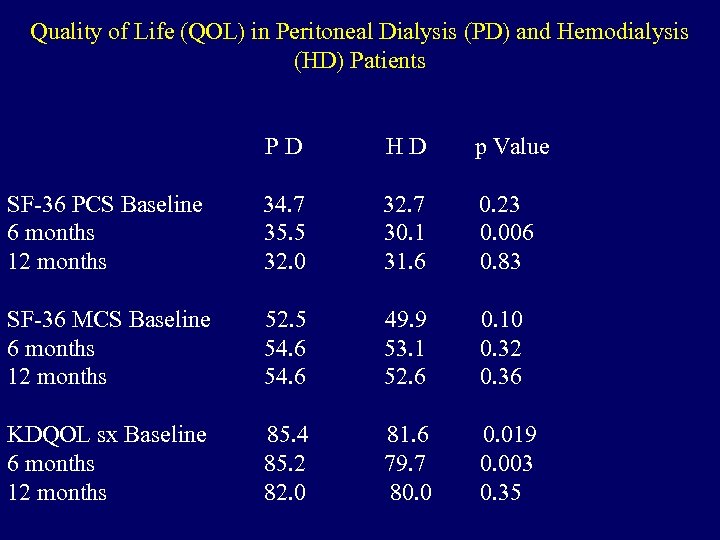 Quality of Life (QOL) in Peritoneal Dialysis (PD) and Hemodialysis (HD) Patients PD HD p Value SF-36 PCS Baseline 6 months 12 months 34. 7 35. 5 32. 0 32. 7 30. 1 31. 6 0. 23 0. 006 0. 83 SF-36 MCS Baseline 6 months 12 months 52. 5 54. 6 49. 9 53. 1 52. 6 0. 10 0. 32 0. 36 KDQOL sx Baseline 6 months 12 months 85. 4 85. 2 82. 0 81. 6 79. 7 80. 019 0. 003 0. 35
Quality of Life (QOL) in Peritoneal Dialysis (PD) and Hemodialysis (HD) Patients PD HD p Value SF-36 PCS Baseline 6 months 12 months 34. 7 35. 5 32. 0 32. 7 30. 1 31. 6 0. 23 0. 006 0. 83 SF-36 MCS Baseline 6 months 12 months 52. 5 54. 6 49. 9 53. 1 52. 6 0. 10 0. 32 0. 36 KDQOL sx Baseline 6 months 12 months 85. 4 85. 2 82. 0 81. 6 79. 7 80. 019 0. 003 0. 35
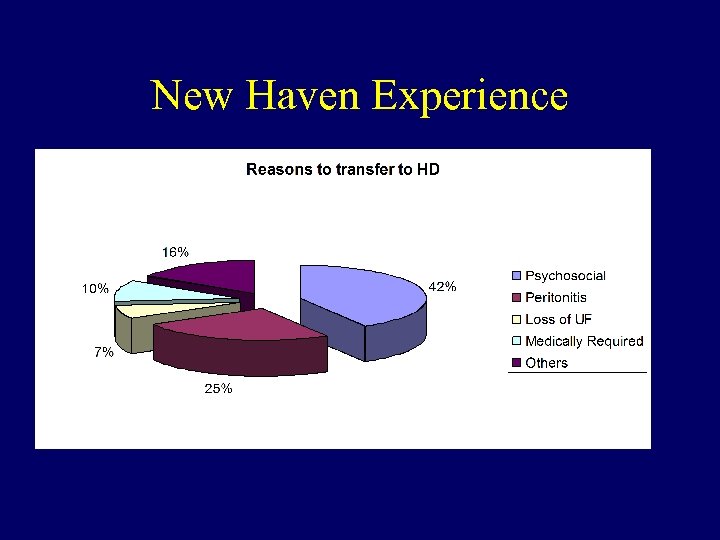 New Haven Experience
New Haven Experience
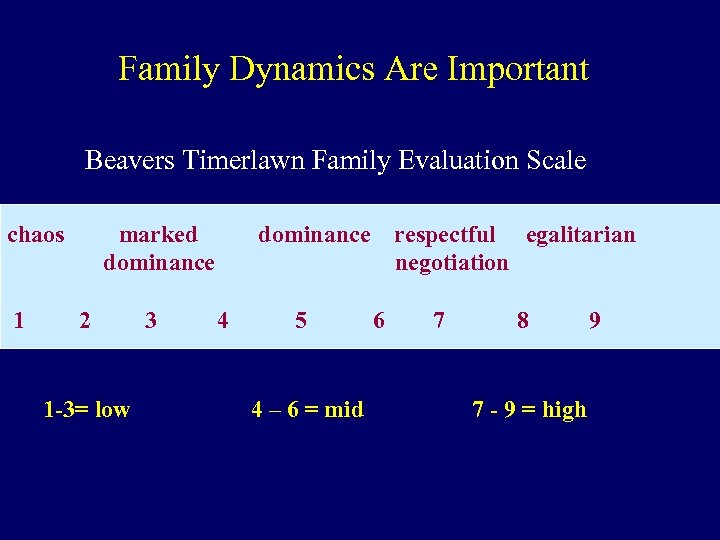 Family Dynamics Are Important Beavers Timerlawn Family Evaluation Scale chaos 1 marked dominance 2 1 -3= low 3 dominance 4 5 4 – 6 = mid respectful egalitarian negotiation 6 7 8 7 - 9 = high 9
Family Dynamics Are Important Beavers Timerlawn Family Evaluation Scale chaos 1 marked dominance 2 1 -3= low 3 dominance 4 5 4 – 6 = mid respectful egalitarian negotiation 6 7 8 7 - 9 = high 9
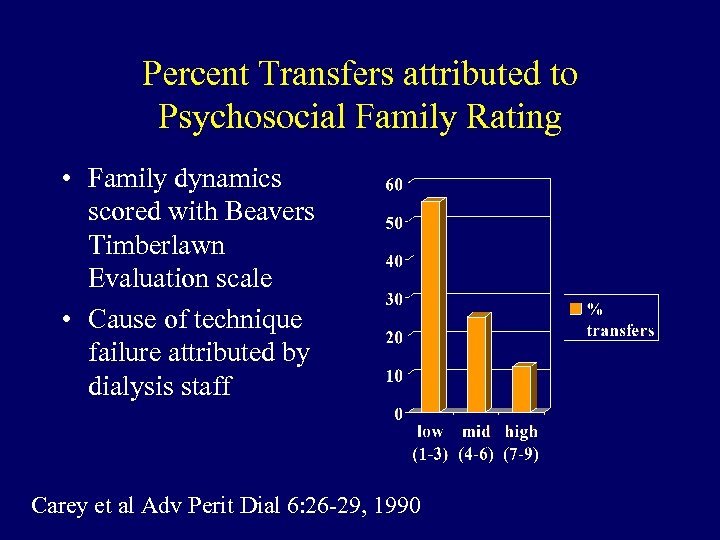 Percent Transfers attributed to Psychosocial Family Rating • Family dynamics scored with Beavers Timberlawn Evaluation scale • Cause of technique failure attributed by dialysis staff Carey et al Adv Perit Dial 6: 26 -29, 1990
Percent Transfers attributed to Psychosocial Family Rating • Family dynamics scored with Beavers Timberlawn Evaluation scale • Cause of technique failure attributed by dialysis staff Carey et al Adv Perit Dial 6: 26 -29, 1990
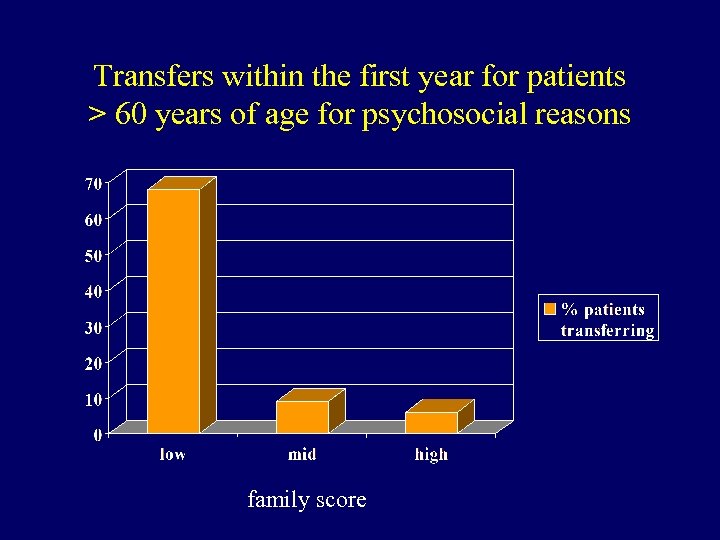 Transfers within the first year for patients > 60 years of age for psychosocial reasons family score
Transfers within the first year for patients > 60 years of age for psychosocial reasons family score
 EXTENDED CARE FACILITIES AND CPD • Reasonable option for elderly patients on dialysis • Markedly reduced global costs • We have trained over 10 ECFs and have cared for over 350 patients since 1993 • Peritonitis rate of 1 per 24 patient months • Useful for both short and long term stays
EXTENDED CARE FACILITIES AND CPD • Reasonable option for elderly patients on dialysis • Markedly reduced global costs • We have trained over 10 ECFs and have cared for over 350 patients since 1993 • Peritonitis rate of 1 per 24 patient months • Useful for both short and long term stays
 CONCLUSIONS • PD is a reasonable treatment for elderly patients with ESRD • It is important to keep in mind the goals of therapy and be flexible about the dose of dialysis • Mortality in elderly patients on PD is higher than in younger patients, but not higher than in HD patients of comparable age • Technique failure rates and peritonitis rates are not higher in elderly patients (? lower) • Quality of life measures are similar in elderly HD and PD patients • Mental Qof. L scores are similar in elderly and younger patients
CONCLUSIONS • PD is a reasonable treatment for elderly patients with ESRD • It is important to keep in mind the goals of therapy and be flexible about the dose of dialysis • Mortality in elderly patients on PD is higher than in younger patients, but not higher than in HD patients of comparable age • Technique failure rates and peritonitis rates are not higher in elderly patients (? lower) • Quality of life measures are similar in elderly HD and PD patients • Mental Qof. L scores are similar in elderly and younger patients
 ISSUES THAT NEED SPECIAL ATTENTION IN THE ELDERLY • • • Assessment of cognitive function Assessment of family dynamics Attention to GI problems, bowels Ongoing assessment of quality of life issues Support and availability to patient, family
ISSUES THAT NEED SPECIAL ATTENTION IN THE ELDERLY • • • Assessment of cognitive function Assessment of family dynamics Attention to GI problems, bowels Ongoing assessment of quality of life issues Support and availability to patient, family


