bbbef5684e682da1f3d9ac3310b126f1.ppt
- Количество слайдов: 52

THE COMMONWEALTH FUND Why Not the Best? How States Can Lead Us Toward a High Performance Health System Karen Davis President, The Commonwealth Fund National Academy for State Health Policy Annual Policy Conference October 16, 2006

2 The Commonwealth Fund Commission on a High Performance Health System Objective: Commission Members, including James J. Mongan, MD, Chairman; Alan Weil, JD; and others • Move the U. S. toward a higher-performing health care system that achieves better access, improved quality, and greater efficiency, with particular focus on the most vulnerable due to income, gaps in insurance coverage, race/ethnicity, health, or age THE COMMONWEALTH FUND
3 Vision: What Constitutes a High Performance Health System? THE COMMONWEALTH FUND
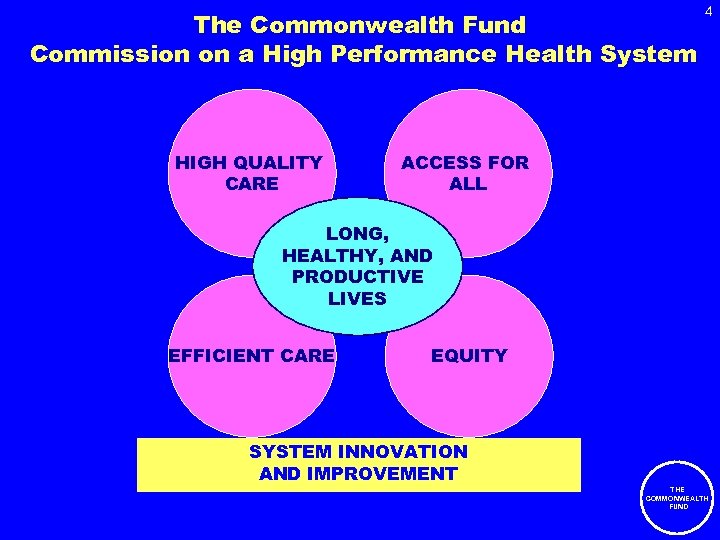
The Commonwealth Fund Commission on a High Performance Health System HIGH QUALITY CARE 4 ACCESS FOR ALL LONG, HEALTHY, AND PRODUCTIVE LIVES EFFICIENT CARE EQUITY SYSTEM INNOVATION AND IMPROVEMENT THE COMMONWEALTH FUND
5 Achieving a High Performance Health System Requires: • Committing to a clear national strategy and establishing a process to implement and refine that strategy • Delivering care through models that emphasize coordination and integration • Establishing and tracking metrics for health outcomes, quality of care, access, disparities, and efficiency THE COMMONWEALTH FUND
6 State Performance: Where We Are Now and Achievable Benchmarks THE COMMONWEALTH FUND
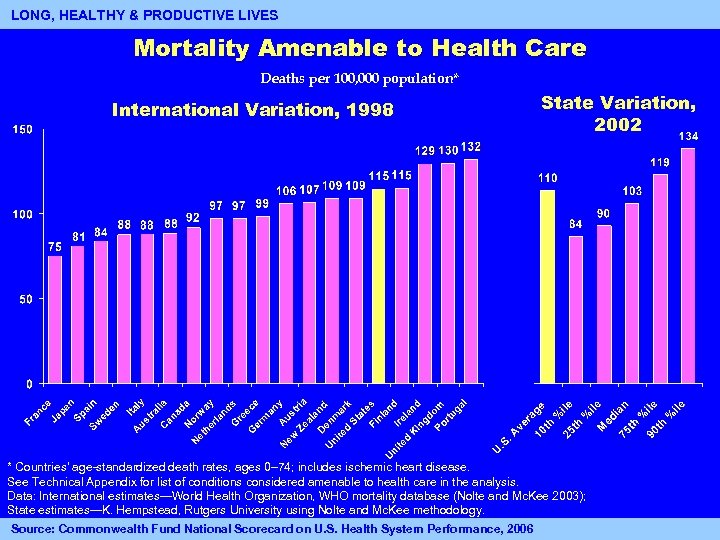
7 LONG, HEALTHY & PRODUCTIVE LIVES Mortality Amenable to Health Care Deaths per 100, 000 population* International Variation, 1998 State Variation, 2002 * Countries’ age-standardized death rates, ages 0– 74; includes ischemic heart disease. See Technical Appendix for list of conditions considered amenable to health care in the analysis. Data: International estimates—World Health Organization, WHO mortality database (Nolte and Mc. Kee 2003); State estimates—K. Hempstead, Rutgers University using Nolte and Mc. Kee methodology. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006
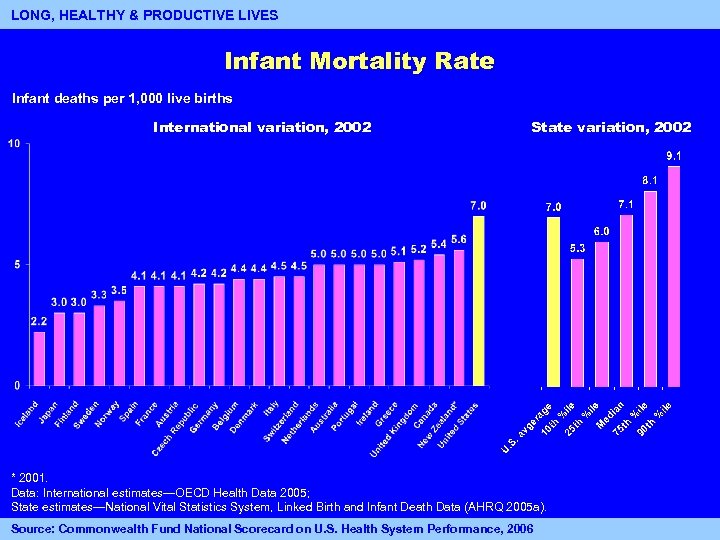
8 LONG, HEALTHY & PRODUCTIVE LIVES Infant Mortality Rate Infant deaths per 1, 000 live births International variation, 2002 State variation, 2002 * 2001. Data: International estimates—OECD Health Data 2005; State estimates—National Vital Statistics System, Linked Birth and Infant Death Data (AHRQ 2005 a). Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006
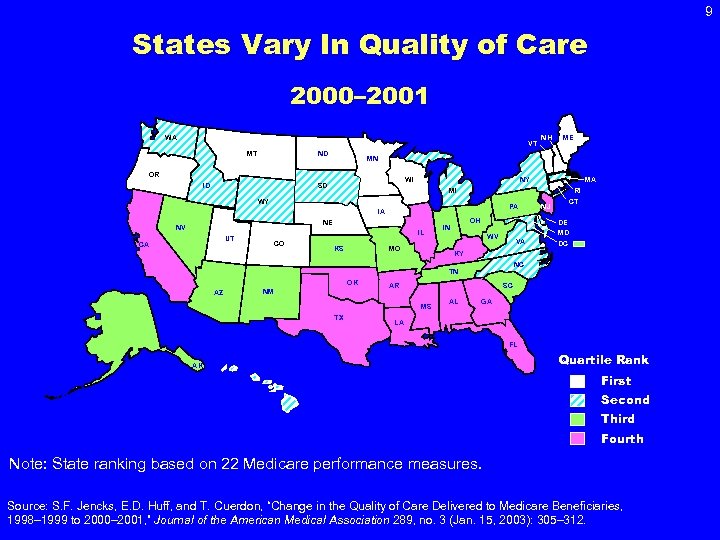
9 States Vary In Quality of Care 2000– 2001 WA VT MT ND WI SD NY RI PA IA NE IL UT CA CO KS MO OH IN OK NM MD VA DC KY NC AR SC MS TX CT NJ DE WV TN AZ MA MI WY NV ME MN OR ID NH AL GA LA FL AK Quartile Rank First Second Third Fourth Note: State ranking based on 22 Medicare performance measures. Source: S. F. Jencks, E. D. Huff, and T. Cuerdon, “Change in the Quality of Care Delivered to Medicare Beneficiaries, 1998– 1999 to 2000– 2001, ” Journal of the American Medical Association 289, no. 3 (Jan. 15, 2003): 305– 312.
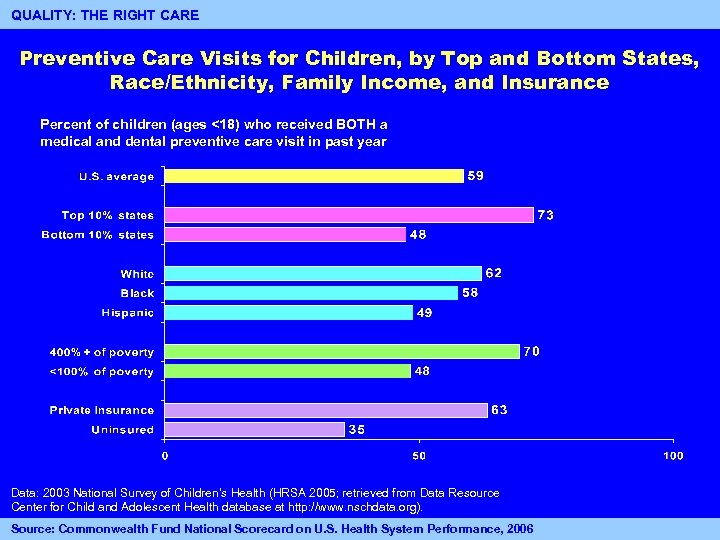
QUALITY: THE RIGHT CARE 10 Preventive Care Visits for Children, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance Percent of children (ages <18) who received BOTH a medical and dental preventive care visit in past year Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http: //www. nschdata. org). Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006
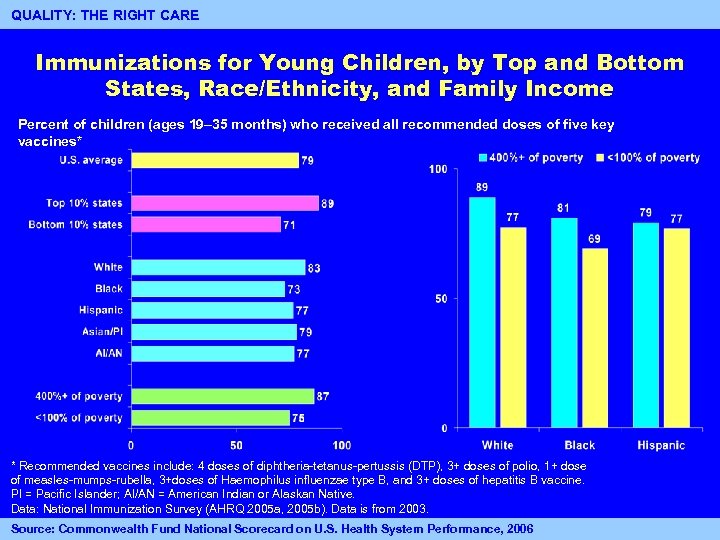
QUALITY: THE RIGHT CARE Immunizations for Young Children, by Top and Bottom States, Race/Ethnicity, and Family Income Percent of children (ages 19– 35 months) who received all recommended doses of five key vaccines* * Recommended vaccines include: 4 doses of diphtheria-tetanus-pertussis (DTP), 3+ doses of polio, 1+ dose of measles-mumps-rubella, 3+doses of Haemophilus influenzae type B, and 3+ doses of hepatitis B vaccine. PI = Pacific Islander; AI/AN = American Indian or Alaskan Native. Data: National Immunization Survey (AHRQ 2005 a, 2005 b). Data is from 2003. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006 11
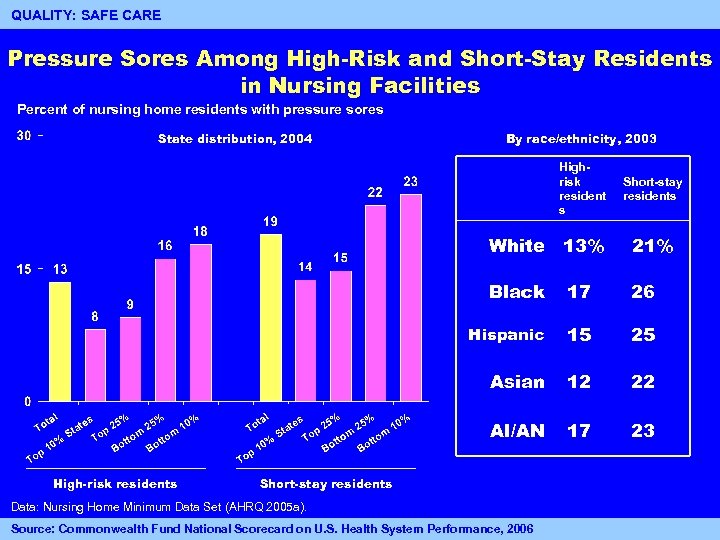
12 QUALITY: SAFE CARE Pressure Sores Among High-Risk and Short-Stay Residents in Nursing Facilities Percent of nursing home residents with pressure sores State distribution, 2004 By race/ethnicity, 2003 Highrisk resident s White 13% 21% Black 17 26 Hispanic 15 25 Asian 12 22 AI/AN High-risk residents Short-stay residents 17 23 Short-stay residents Data: Nursing Home Minimum Data Set (AHRQ 2005 a). Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006
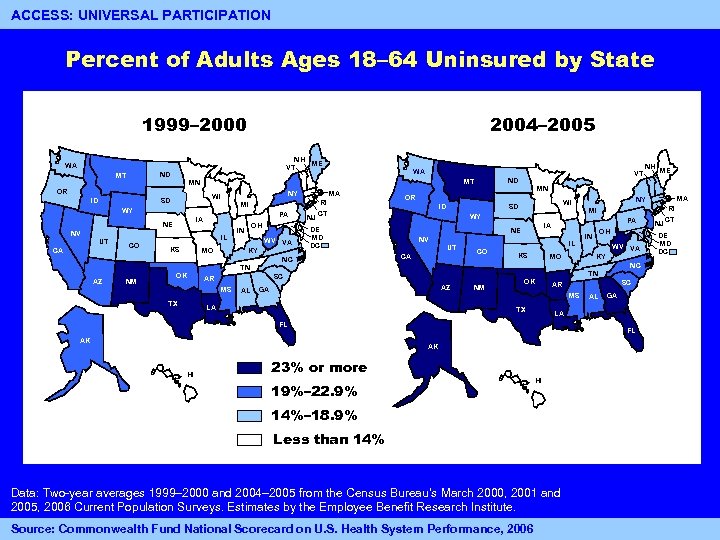
13 ACCESS: UNIVERSAL PARTICIPATION Percent of Adults Ages 18– 64 Uninsured by State 1999– 2000 2004– 2005 NH NH ME VT WA ND MT ID NY WI SD MI WY PA IA NE NV CA IL CO KS MO OH IN WV VA KY NM OK ID AL MI PA IA NE NV UT CA IL CO KS MO AZ LA NM OK WV VA NC SC AR AL GA LA FL FL AK HI IN KY MS TX AK OH TN GA MA NY WI SD WY DE MD DC NH ME MN OR SC AR MS TX NJ RI CT NC TN AZ MA VT ND MT MN OR UT WA 23% or more 19%– 22. 9% HI 14%– 18. 9% Less than 14% Data: Two-year averages 1999– 2000 and 2004– 2005 from the Census Bureau’s March 2000, 2001 and 2005, 2006 Current Population Surveys. Estimates by the Employee Benefit Research Institute. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006 NJ RI CT DE MD DC
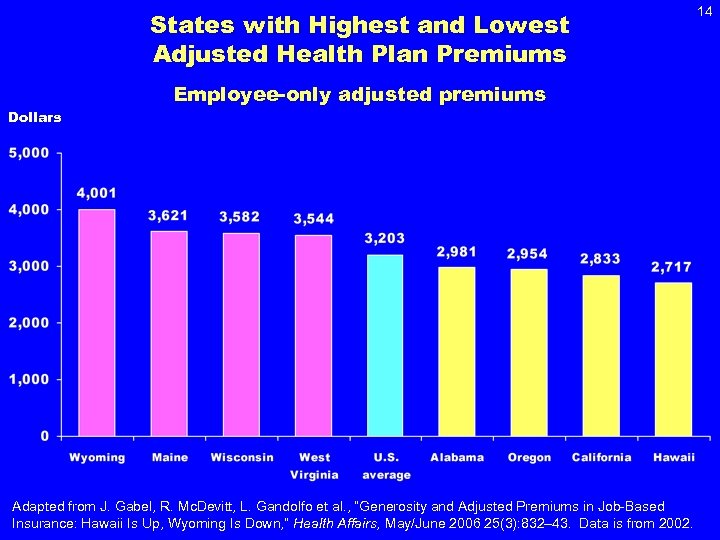
States with Highest and Lowest Adjusted Health Plan Premiums Dollars Employee-only adjusted premiums Adapted from J. Gabel, R. Mc. Devitt, L. Gandolfo et al. , “Generosity and Adjusted Premiums in Job-Based Insurance: Hawaii Is Up, Wyoming Is Down, ” Health Affairs, May/June 2006 25(3): 832– 43. Data is from 2002. 14
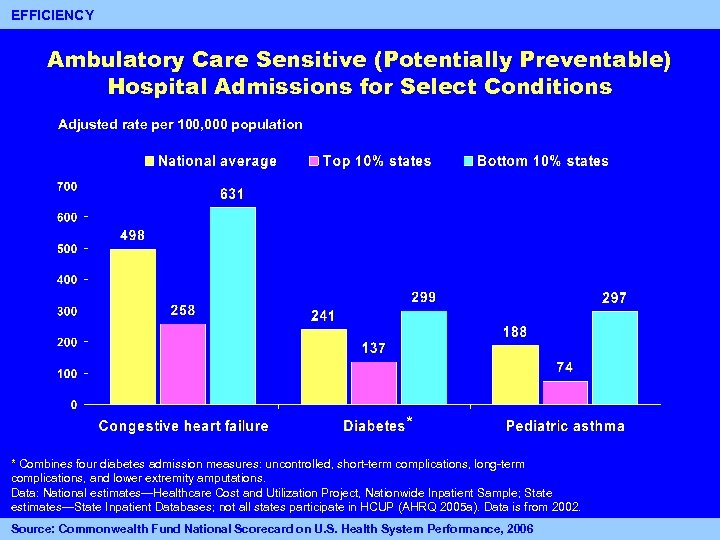
15 EFFICIENCY Ambulatory Care Sensitive (Potentially Preventable) Hospital Admissions for Select Conditions Adjusted rate per 100, 000 population * * Combines four diabetes admission measures: uncontrolled, short-term complications, long-term complications, and lower extremity amputations. Data: National estimates—Healthcare Cost and Utilization Project, Nationwide Inpatient Sample; State estimates—State Inpatient Databases; not all states participate in HCUP (AHRQ 2005 a). Data is from 2002. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006
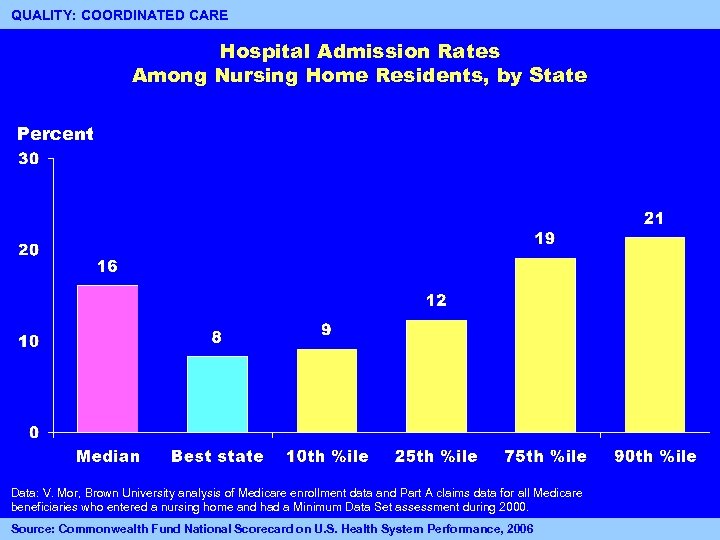
QUALITY: COORDINATED CARE 16 Hospital Admission Rates Among Nursing Home Residents, by State Percent Data: V. Mor, Brown University analysis of Medicare enrollment data and Part A claims data for all Medicare beneficiaries who entered a nursing home and had a Minimum Data Set assessment during 2000. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006 16
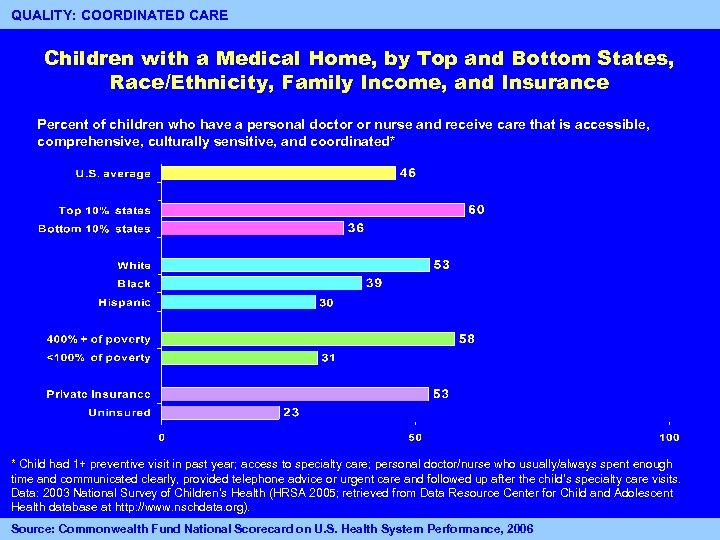
QUALITY: COORDINATED CARE Children with a Medical Home, by Top and Bottom States, Race/Ethnicity, Family Income, and Insurance Percent of children who have a personal doctor or nurse and receive care that is accessible, comprehensive, culturally sensitive, and coordinated* * Child had 1+ preventive visit in past year; access to specialty care; personal doctor/nurse who usually/always spent enough time and communicated clearly, provided telephone advice or urgent care and followed up after the child’s specialty care visits. Data: 2003 National Survey of Children’s Health (HRSA 2005; retrieved from Data Resource Center for Child and Adolescent Health database at http: //www. nschdata. org). Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006 17
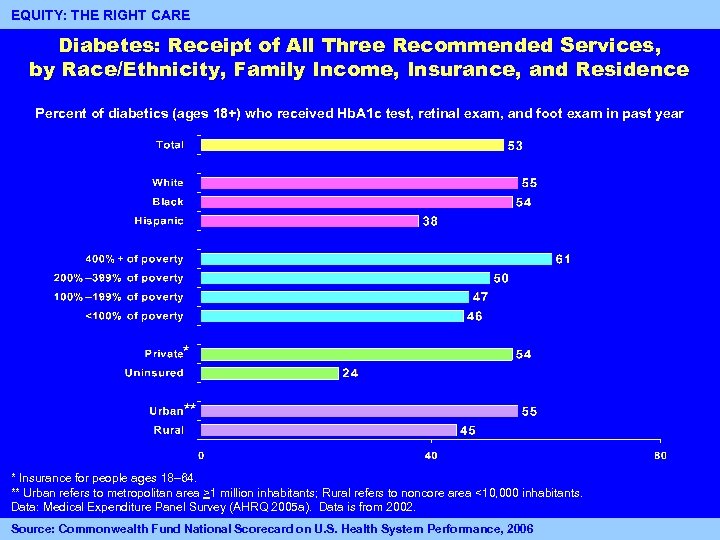
EQUITY: THE RIGHT CARE Diabetes: Receipt of All Three Recommended Services, by Race/Ethnicity, Family Income, Insurance, and Residence Percent of diabetics (ages 18+) who received Hb. A 1 c test, retinal exam, and foot exam in past year * ** * Insurance for people ages 18– 64. ** Urban refers to metropolitan area >1 million inhabitants; Rural refers to noncore area <10, 000 inhabitants. Data: Medical Expenditure Panel Survey (AHRQ 2005 a). Data is from 2002. Source: Commonwealth Fund National Scorecard on U. S. Health System Performance, 2006 18
State Health Policies Aimed at Promoting Excellent Systems (SHAPES) • Environmental scan of state-level policies that promote or impede high performance – Qualitative companion to Commission's quantitative National Scorecard – Mechanism for identifying innovative states for future Commission site visits – Four Commission members serve on advisory committee • Products to date – Data information collection plan completed – Survey drafted -- will probe broadly the policy domains of coverage, quality/efficiency/value, and infrastructure supports – Data collection to begin September 2006 – Health policy community notified at Academy Health June 25, 2006 Alan Weil, NASHP Catherine Hess, NASHP 19

Keys to Transforming the U. S. Health Care System 1. 2. 3. 4. 5. 6. 7. Guarantee affordable health insurance coverage Implement major quality and safety improvements Work toward a more organized delivery system that emphasizes patient-centered primary and preventive care Increase transparency and reporting on quality and costs Expand the use of interoperable information technology Reward performance for quality and efficiency Encourage public-private collaboration to achieve simplification, more effective change 20

Guarantee Affordable Health Insurance Coverage 21 1. Guarantee Affordable Health Insurance Coverage THE COMMONWEALTH FUND
22 Massachusetts Health Plan • Mass. Health expansion for children up to 300% FPL; adults up to 100% poverty • Individual mandate, with affordability provision; subsidies between 100% and 300% of poverty • Employer mandatory offer, employee mandatory take-up • Employer assessment ($295 if employer doesn’t provide health insurance) • Connector to organize affordable insurance offerings through a group pool Source: John Holahan, “The Basics of Massachusetts Health Reform, ” Presentation to United Hospital Fund, April 2006. THE COMMONWEALTH FUND
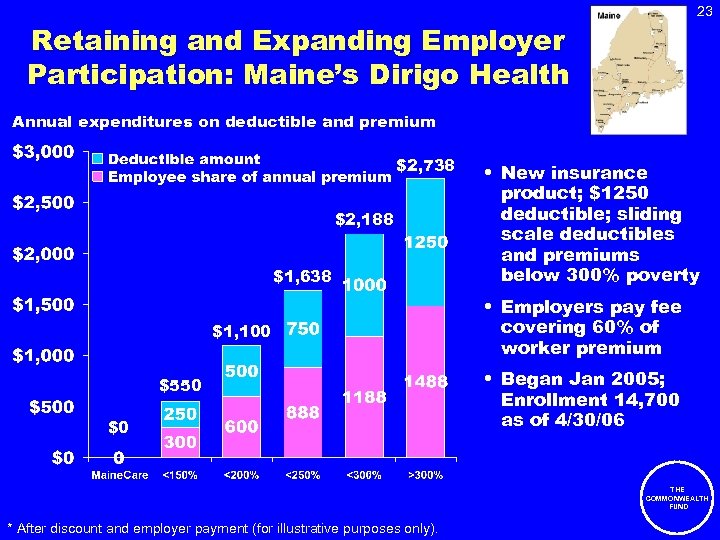
23 Retaining and Expanding Employer Participation: Maine’s Dirigo Health Annual expenditures on deductible and premium $2, 738 $2, 188 $1, 638 $1, 100 $550 $0 • New insurance product; $1250 deductible; sliding scale deductibles and premiums below 300% poverty • Employers pay fee covering 60% of worker premium • Began Jan 2005; Enrollment 14, 700 as of 4/30/06 THE COMMONWEALTH FUND * After discount and employer payment (for illustrative purposes only).
Vermont Health Care Affordability Act Enacted May 2006 24 • Coverage expansion – Catamount Health Plans • Targets those w/o access to work-based coverage • Premium subsidies based on sliding scale up to 300% FPL • Comprehensive benefit package including primary, chronic, acute care & other services • No patient cost-sharing for preventive or chronic care • Builds upon Wagner’s Chronic Care Model • Financing – Employer assessment – Increase in tobacco taxes – Federal matching funds from Medicaid waiver • Quality improvement initiatives – Public-private collaboration – Collection of health care data from all payers – Rules to publicly report price & quality information THE COMMONWEALTH FUND
25 Illinois All-Kids • • • Effective July 1, 2006 Available to any child uninsured for 6 months or more Cost to family determined on a sliding scale Linked to other public programs - Family. Care & Kid. Care Federal and state funds – Children <200% of FPL covered by federal funds – Children 200%+ of FPL funded by state savings from Medicaid Primary Care Case Management Program • All-Kids Training Tour – Public outreach program to highlight new and expanded healthcare programs THE COMMONWEALTH FUND
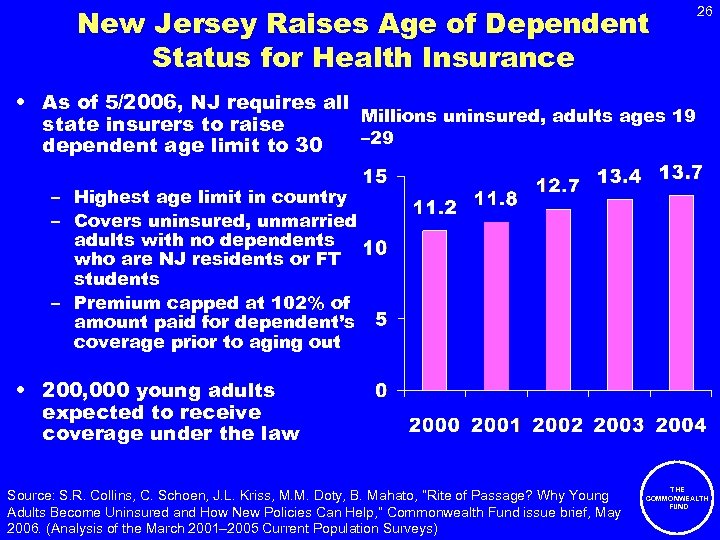
New Jersey Raises Age of Dependent Status for Health Insurance 26 • As of 5/2006, NJ requires all Millions uninsured, adults ages 19 state insurers to raise – 29 dependent age limit to 30 – Highest age limit in country – Covers uninsured, unmarried adults with no dependents who are NJ residents or FT students – Premium capped at 102% of amount paid for dependent’s coverage prior to aging out • 200, 000 young adults expected to receive coverage under the law Source: S. R. Collins, C. Schoen, J. L. Kriss, M. M. Doty, B. Mahato, “Rite of Passage? Why Young Adults Become Uninsured and How New Policies Can Help, ” Commonwealth Fund issue brief, May 2006. (Analysis of the March 2001– 2005 Current Population Surveys) THE COMMONWEALTH FUND

27 Implement Major Quality and Safety Improvements 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements THE COMMONWEALTH FUND
Rhode Island: Five-Point Strategy 1. 2. 3. 4. 5. • Creating affordable plans for small businesses & individuals Increasing wellness programs Investing in health care technology Developing centers of excellence Leveraging the state’s purchasing power RI Quality Institute – – • 28 Non-profit coalition -- hospitals, providers, insurers, consumers, business, academia & government Partnered with “Sure. Scripts” to implement state-wide electronic connectivity between all retail pharmacies and prescribers in the state Health Information Exchange Initiative – – – Statewide public/private effort AHRQ contract 5 yr/ $5 M Connecting information from physicians, hospitals, labs, imaging & other community providers THE COMMONWEALTH FUND
Work Toward a More Organized Delivery System that Emphasizes Patient-Centered Primary and Preventive Care 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements 29 3. Emphasize Patient. Centered Primary, and Preventive Care THE COMMONWEALTH FUND
30 Helping Patients Become Informed and Active Partners in Their Care Patient-centered care: • www. howsyourhealth. org • PCDC – advanced access collaborative • Shared decision-making • Resident-centered care in nursing homes • Family-centered care in Healthy Steps & ABCD THE COMMONWEALTH FUND
31 Resident-Centered Nursing Home Care for Frail Elders • Green House in Tupelo, Mississippi, featured in New York Times and AARP Bulletin; Commonwealth supported evaluation in progress • Ohio project finds high correlation between resident and family satisfaction and nursing home clinical quality • New York state – analysis of use of hospitals by nursing home residents
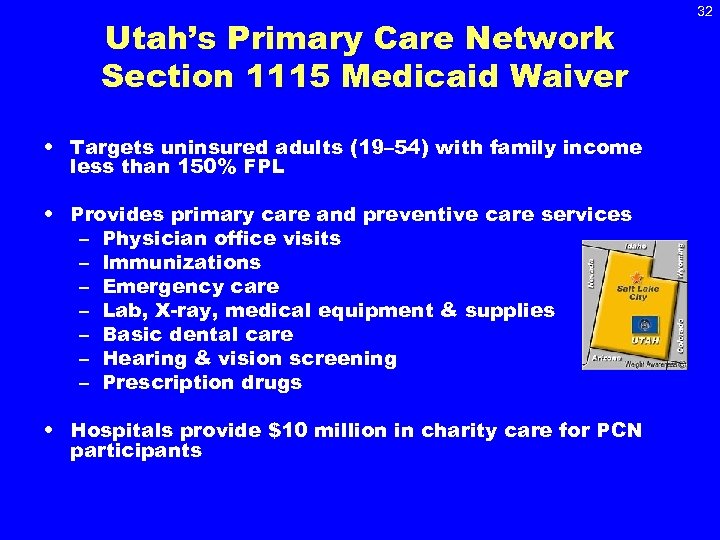
Utah’s Primary Care Network Section 1115 Medicaid Waiver • Targets uninsured adults (19– 54) with family income less than 150% FPL • Provides primary care and preventive care services – Physician office visits – Immunizations – Emergency care – Lab, X-ray, medical equipment & supplies – Basic dental care – Hearing & vision screening – Prescription drugs • Hospitals provide $10 million in charity care for PCN participants 32
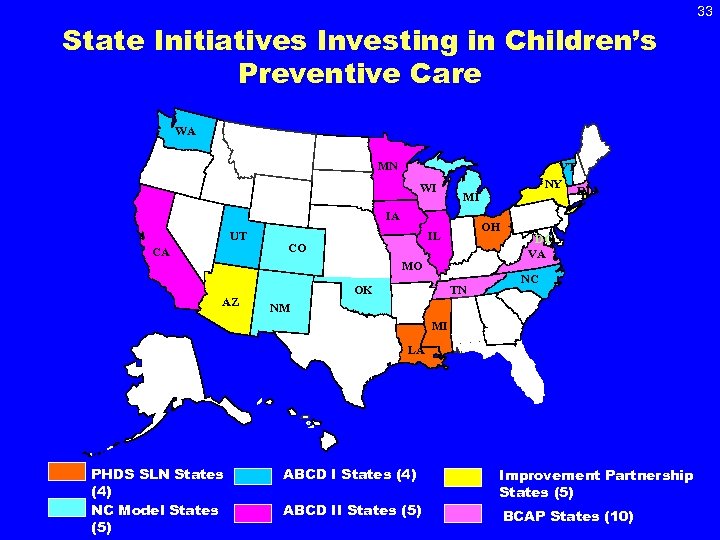
State Initiatives Investing in Children’s Preventive Care WA MN MN WI NV UT CA MI IA NE OH IL CO VT NY DC VA MO AZ OK NM MI TX NC TN AR RI SC GA LA FL PHDS SLN States (4) NC Model States (5) ABCD I States (4) ABCD II States (5) Improvement Partnership States (5) BCAP States (10)) 33
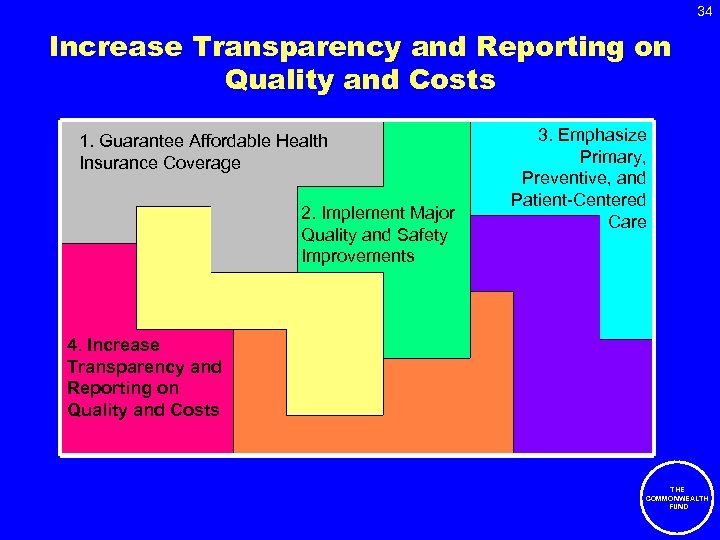
34 Increase Transparency and Reporting on Quality and Costs 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements 3. Emphasize Primary, Preventive, and Patient-Centered Care 4. Increase Transparency and Reporting on Quality and Costs THE COMMONWEALTH FUND
35 Wisconsin • Wisconsin Collaborative for Healthcare Quality – Voluntary consortium formed in 2003 -- physician groups, hospitals, health plans, employers & labor – Develops & publicly reports comparative performance information on physician practices, hospitals & health plans – Includes measures assessing ambulatory care, IT capacity, patient satisfaction & access • Wisconsin Health Information Organization – Coalition formed in 2005 to create a centralized health data repository based on voluntary sharing of private health insurance claims, including pharmacy & laboratory data – Wisconsin Dept of Health & Family Services and Dept of Employee Trust Funds will add data on costs of publicly paid health care through Medicaid THE COMMONWEALTH FUND
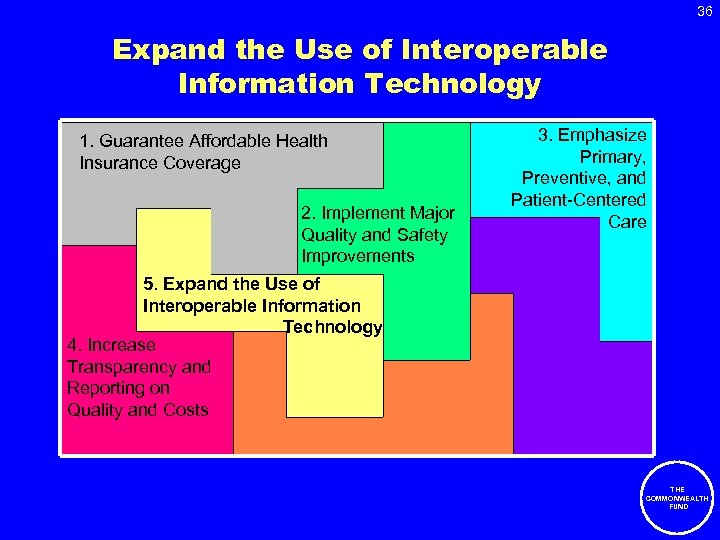
36 Expand the Use of Interoperable Information Technology 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements 3. Emphasize Primary, Preventive, and Patient-Centered Care 5. Expand the Use of Interoperable Information Technology 4. Increase Transparency and Reporting on Quality and Costs THE COMMONWEALTH FUND
Value of Electronic Medical Records and Information Systems • Reduce duplicate tests • Reduce hospital admissions by having information accessible to ER physicians • Improve patient care • Decision support for physicians and patients • Facilitate “referrals”, secure transfer of responsibility • Reduce medical errors • Better management of chronic conditions and care coordination – Registries – Performance information – Facilitated by interoperability 37 THE COMMONWEALTH FUND
38 Information Exchange: States Leading the Way • Rhode Island Quality Institute Information Exchange – Provide access to patient data (as permitted) to all providers initially through secure web-based portal – future integration into EHRs – Create the ability to aggregate and utilize data for public health purposes (e. g. , population-based analysis, biosurveillance) • Mid. South e-health Alliance: Memphis, TN – State-wide data exchange with initial focus on EDs • Utah Health Information Network – Secure exchange of health care data using standardized transactions through a single portal • New York State Health Information Technology (HIT) initiative – Under the Health Care Efficiency and Affordability Law for New Yorkers, $52. 9 million awarded to 26 regional health networks to expand technology in NY health care system and support clinical data THE COMMONWEALTH exchange; Commonwealth Fund-supported evaluation underway FUND Source: Evolution of State Health Information Exchange, AHRQ, Publication No. 06 -0057, January 2006.
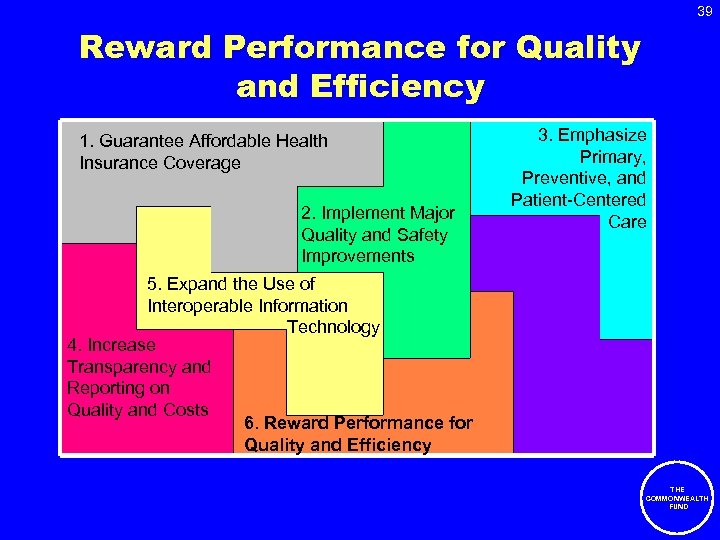
39 Reward Performance for Quality and Efficiency 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements 3. Emphasize Primary, Preventive, and Patient-Centered Care 5. Expand the Use of Interoperable Information Technology 4. Increase Transparency and Reporting on Quality and Costs 6. Reward Performance for Quality and Efficiency THE COMMONWEALTH FUND
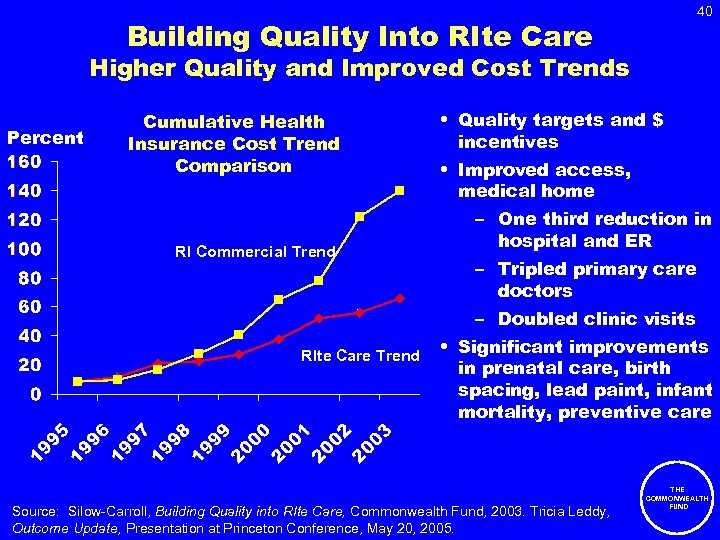
40 Building Quality Into RIte Care Higher Quality and Improved Cost Trends Percent Cumulative Health Insurance Cost Trend Comparison RI Commercial Trend • Quality targets and $ incentives • Improved access, medical home – One third reduction in hospital and ER – Tripled primary care doctors – Doubled clinic visits RIte Care Trend • Significant improvements in prenatal care, birth spacing, lead paint, infant mortality, preventive care Source: Silow-Carroll, Building Quality into RIte Care, Commonwealth Fund, 2003. Tricia Leddy, Outcome Update, Presentation at Princeton Conference, May 20, 2005. THE COMMONWEALTH FUND
41 New York State Medicaid Pay-for-Performance • 1997 — NYS began transition to mandatory statewide Medicaid managed care. Currently > 2. 5 million enrollees (including Family Health Plus) • 2002 — NYS DOH incorporated quality incentive into computation of Medicaid managed care capitation rates – Incentive tied to performance on 10 quality of care measures and 5 consumer satisfaction measures – Initial incentive up to an additional 1% of monthly premium; as of April 2005, maximum incentive increased to 3% • 2005 — incentive payments totaled $40 million • Commonwealth Fund supporting Dr. Robert Berenson (Urban Institute) to evaluate impact of quality incentive program — qualitative analysis (interviews/site visits of participating plans) and quantitative analysis of measures THE COMMONWEALTH FUND
Assisting States in the Design of Medicaid Pay-for-Performance Programs 42 CHCS/Stephen Somers, Jul 06–Jun 08 Overview • Develop Pay-for-Performance Purchasing Institute Technical Assistance Series for 6 state Medicaid teams – Two in-person training institutes – Follow-up technical assistance • Conduct environmental scan on P 4 P lessons learned in the public/private sectors focusing on the provider level – Draft report expected Sep 2006 • Synthesis of lessons learned and best practices – Draft report expected May 2008 Status • 1 st training institute scheduled for October 12– 13, 2006 • State Participants: Arizona, Connecticut, Idaho, Massachusetts, Missouri, Ohio, & West Virginia THE COMMONWEALTH FUND
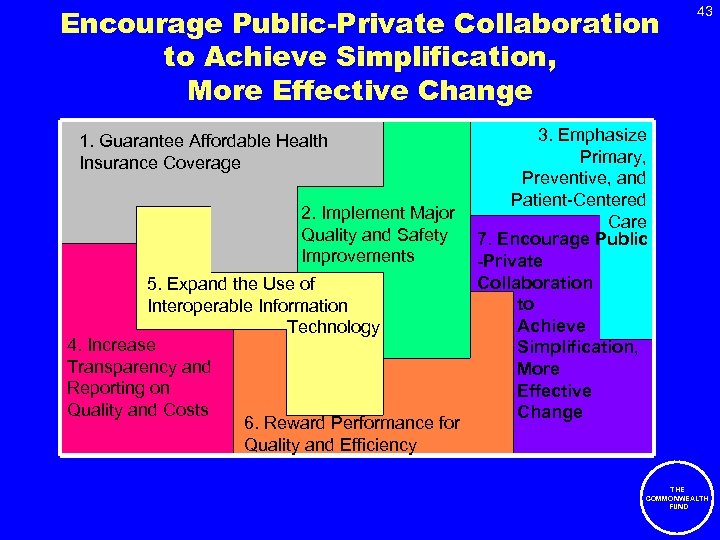
Encourage Public-Private Collaboration to Achieve Simplification, More Effective Change 1. Guarantee Affordable Health Insurance Coverage 2. Implement Major Quality and Safety Improvements 5. Expand the Use of Interoperable Information Technology 4. Increase Transparency and Reporting on Quality and Costs 6. Reward Performance for Quality and Efficiency 43 3. Emphasize Primary, Preventive, and Patient-Centered Care 7. Encourage Public -Private Collaboration to Achieve Simplification, More Effective Change THE COMMONWEALTH FUND

44 Minnesota Smart-Buy Alliance • Initiated in 2004 – alliance between state, private businesses & labor groups • Purchase health insurance for 70% of state residents ~3. 5 million people • Pool purchasing power to drive value in health care delivery system • Set uniform performance standards, cost/quality reporting requirements & technology demands • Four key strategies: 1. Reward or require “best in class” certification 2. Adopt and utilize uniform measures of quality and results 3. Empower consumers with easy access to information 4. Require use of information technology THE COMMONWEALTH FUND
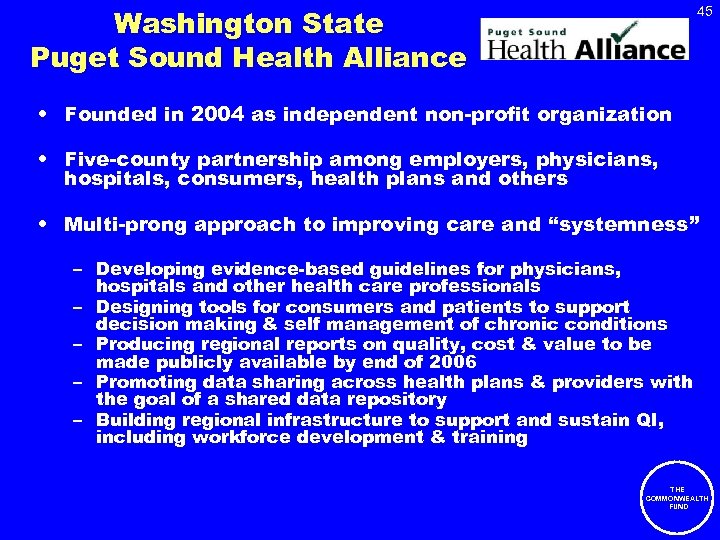
Washington State Puget Sound Health Alliance 45 • Founded in 2004 as independent non-profit organization • Five-county partnership among employers, physicians, hospitals, consumers, health plans and others • Multi-prong approach to improving care and “systemness” – Developing evidence-based guidelines for physicians, hospitals and other health care professionals – Designing tools for consumers and patients to support decision making & self management of chronic conditions – Producing regional reports on quality, cost & value to be made publicly available by end of 2006 – Promoting data sharing across health plans & providers with the goal of a shared data repository – Building regional infrastructure to support and sustain QI, including workforce development & training THE COMMONWEALTH FUND

West Virginia Small Business Plan Leveraging Purchasing Power 46 • West Virginia (WV) Small Business Plan – Enacted March 2004 – Partnership between WV Public Employees Insurance Agency (PEIA) & private market insurers – Small business insurers pay providers at same rates negotiated by PEIA THE COMMONWEALTH FUND

47 Moving Forward
What States Can Do to Promote a High Performance Health System: Strategies to Expand Coverage • Expand public programs • Provide financial assistance to workers and employers to afford coverage • Promote partnerships with employers • Pool purchasing power and promote new benefit designs to make coverage more affordable • Mandate that employers offer, and/or individuals purchase, coverage; subsidize those with low incomes • Develop reinsurance programs to make coverage more affordable in the small group and individual markets 48 THE COMMONWEALTH FUND

What States Can Do to Promote a High Performance Health System: Strategies to Improve Quality and Efficiency • • • 49 Promote evidence-based medicine Promote effective chronic care management Promote transitional care post-hospital discharge Encourage data transparency and reporting on performance Promote/practice value-based purchasing Promote the use of health information technology Promote wellness and healthy living Encourage selection of medical home and improved access to primary care and preventive services Simplify and streamline public program eligibility and redetermination THE COMMONWEALTH FUND
50 Continue to Lead the Way to Achieving a High Performance Health System! THE COMMONWEALTH FUND
51 Selected Commonwealth Fund Publications • The Commonwealth Fund Commission on a High Performance Health System, Framework for a High Performance Health System for the United States, The Commonwealth Fund, August 2006 • C. Schoen et al. , “U. S. Health System Performance: A National Scorecard, ” Health Affairs Web Exclusive, September 20, 2006. • S. Silow-Carroll and F. Pervez, States in Action: A Quarterly Look at Innovations in Health Policy, The Commonwealth Fund, Summer 2006, Vol. 5. • Forthcoming – – State Scorecard on Health System Performance THE COMMONWEALTH FUND
52 Thank You! Stephen C. Schoenbaum, M. D. , Executive Vice President and Executive Director, Commission on a High Performance Health System Karen B. Adams, Program Officer, State Innovations Program Cathy Schoen, Senior Vice President for Research and Evaluation Alyssa L. Holmgren, Research Associate Anne Gauthier, Senior Policy Director, Commission on a High Performance Health System Jennifer L. Kriss, Program Assistant Sign up for States in Action newsletter and forward to colleagues – www. cmwf. org THE COMMONWEALTH FUND
bbbef5684e682da1f3d9ac3310b126f1.ppt