57bab311fd857af27c782cb7548f902b.ppt
- Количество слайдов: 103
 The Cardiovascular System
The Cardiovascular System
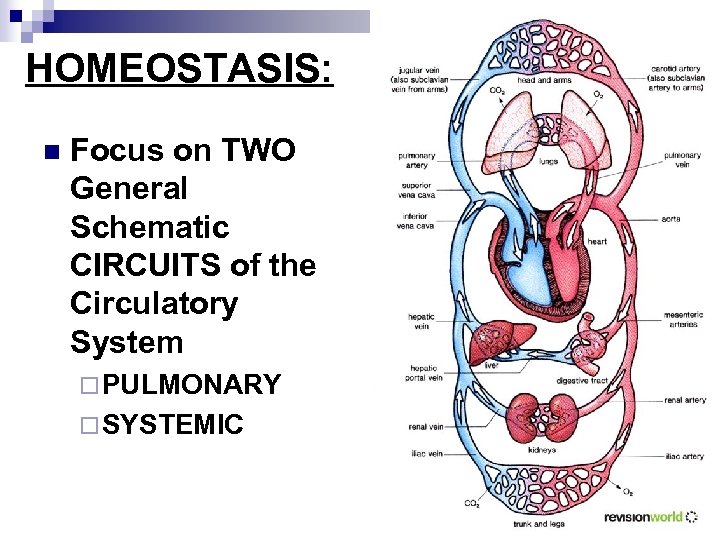 HOMEOSTASIS: n Focus on TWO General Schematic CIRCUITS of the Circulatory System ¨ PULMONARY ¨ SYSTEMIC
HOMEOSTASIS: n Focus on TWO General Schematic CIRCUITS of the Circulatory System ¨ PULMONARY ¨ SYSTEMIC
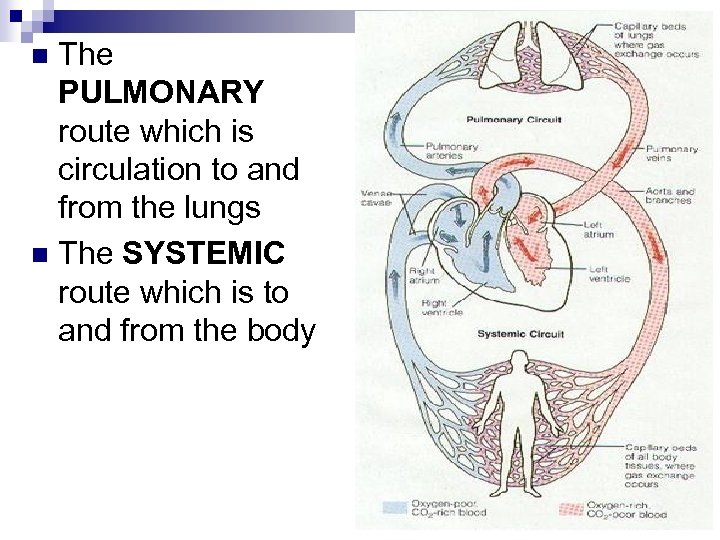 The PULMONARY route which is circulation to and from the lungs n The SYSTEMIC route which is to and from the body n
The PULMONARY route which is circulation to and from the lungs n The SYSTEMIC route which is to and from the body n
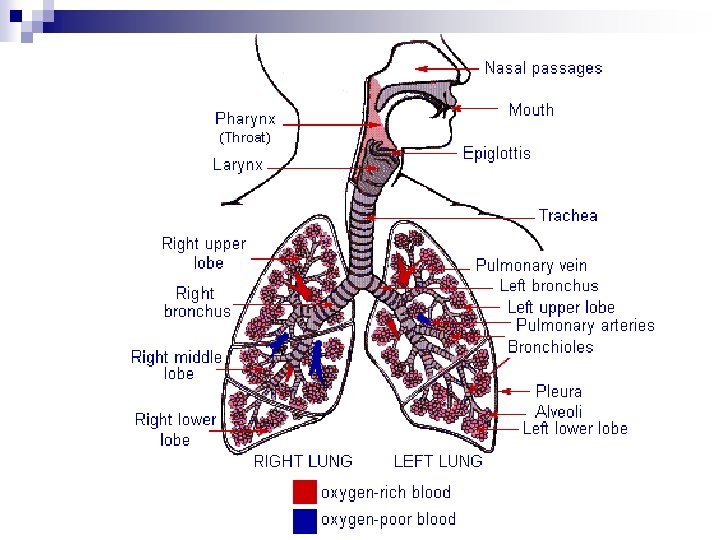
 PULMONARY ROUTE: RESPIRATORY CIRCUIT: n Pulmonary arteries – heart to the lungs. ¨ In the lungs gas exchange occurs. Pulmonary veins – lungs to heart. n HOMEOSTASIS: the maintenance of oxygen for cellular respiration and removal of carbon dioxide, a byproduct of respiration. n
PULMONARY ROUTE: RESPIRATORY CIRCUIT: n Pulmonary arteries – heart to the lungs. ¨ In the lungs gas exchange occurs. Pulmonary veins – lungs to heart. n HOMEOSTASIS: the maintenance of oxygen for cellular respiration and removal of carbon dioxide, a byproduct of respiration. n
 Respiration The physiological process by which organisms supply oxygen to their cells 1. 2. 3. External Respiration – exchange between body & environment (inhale/exhale) Internal Respiration – exchange between internal body fluids (blood and cells) Cellular Respiration – oxidation of glucose and synthesis of ATP
Respiration The physiological process by which organisms supply oxygen to their cells 1. 2. 3. External Respiration – exchange between body & environment (inhale/exhale) Internal Respiration – exchange between internal body fluids (blood and cells) Cellular Respiration – oxidation of glucose and synthesis of ATP
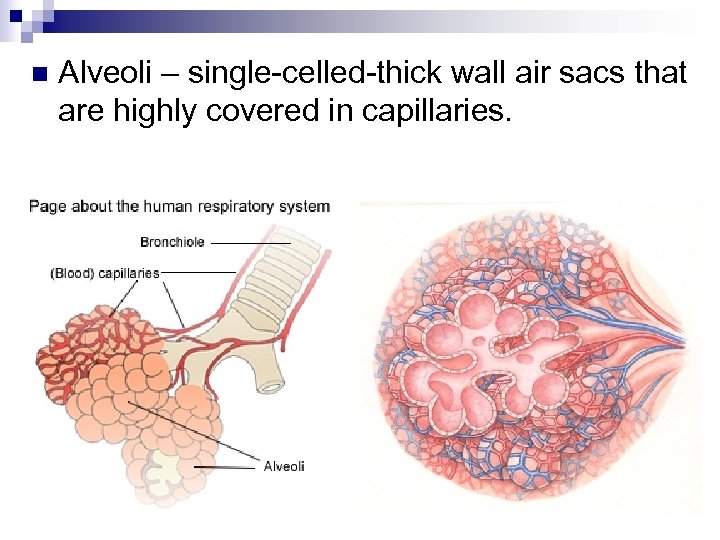 n Alveoli – single-celled-thick wall air sacs that are highly covered in capillaries.
n Alveoli – single-celled-thick wall air sacs that are highly covered in capillaries.
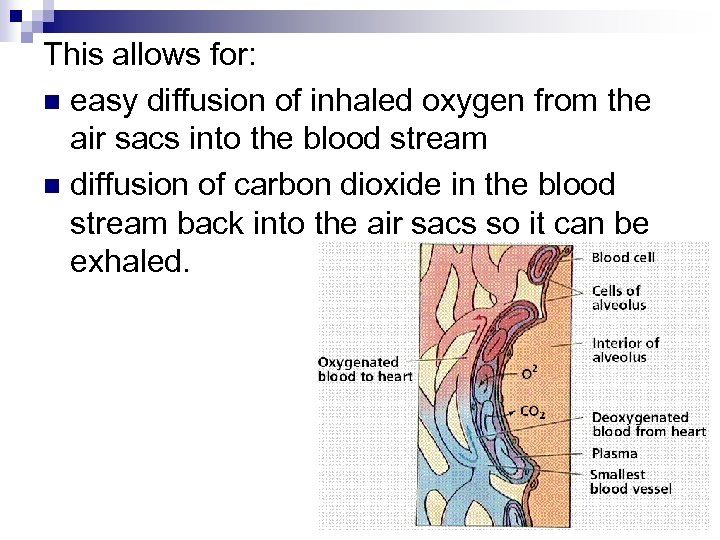 This allows for: n easy diffusion of inhaled oxygen from the air sacs into the blood stream n diffusion of carbon dioxide in the blood stream back into the air sacs so it can be exhaled.
This allows for: n easy diffusion of inhaled oxygen from the air sacs into the blood stream n diffusion of carbon dioxide in the blood stream back into the air sacs so it can be exhaled.
 n Our cellular reactions require oxygen.
n Our cellular reactions require oxygen.
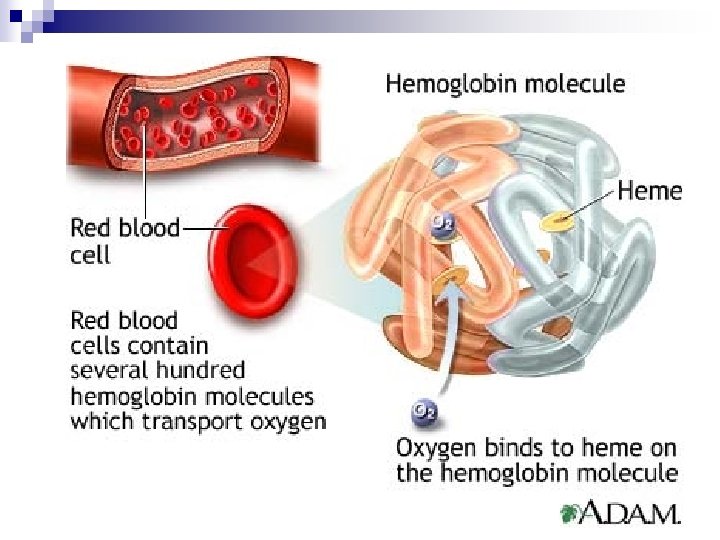
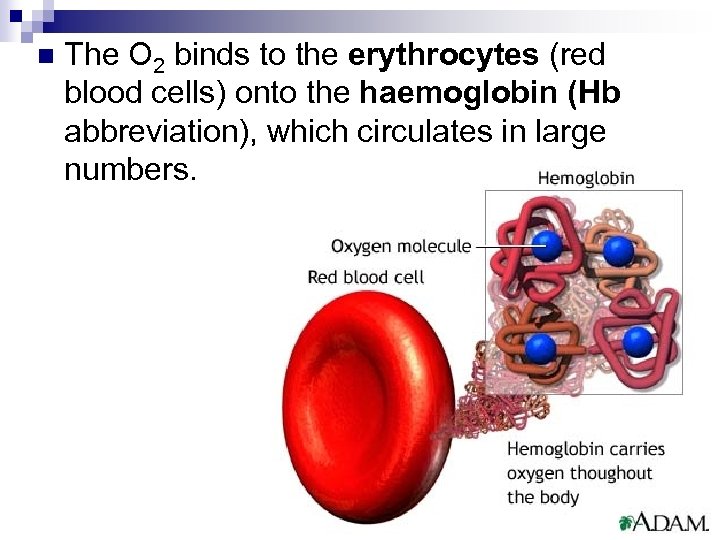 n The O 2 binds to the erythrocytes (red blood cells) onto the haemoglobin (Hb abbreviation), which circulates in large numbers.
n The O 2 binds to the erythrocytes (red blood cells) onto the haemoglobin (Hb abbreviation), which circulates in large numbers.
 From the lungs, the oxygenated blood is pumped back to the heart where O 2 is then pumped into the systemic route—to all tissues of the body. n O 2 diffuses across the capillary wall into the body cells where mitochondria use it to carry out respiration for energy production. n
From the lungs, the oxygenated blood is pumped back to the heart where O 2 is then pumped into the systemic route—to all tissues of the body. n O 2 diffuses across the capillary wall into the body cells where mitochondria use it to carry out respiration for energy production. n
 This releases CO 2 into the blood stream by diffusion n The CO 2 dissolves into the blood plasma and becomes carbonic acid (H 2 CO 3) n n n i. e. H 2 O + CO 2 H 2 CO 3 Hb (now low in oxygen) binds an H+ which prevents our blood from becoming too acidic. ¨ This is what buffers our blood – keeps the p. H around 7. 4.
This releases CO 2 into the blood stream by diffusion n The CO 2 dissolves into the blood plasma and becomes carbonic acid (H 2 CO 3) n n n i. e. H 2 O + CO 2 H 2 CO 3 Hb (now low in oxygen) binds an H+ which prevents our blood from becoming too acidic. ¨ This is what buffers our blood – keeps the p. H around 7. 4.
 The now deoxygenated (oxygen poor) blood is high in CO 2 n it returns to the heart in large veins called the vena cava ¨superior – from the head; ¨inferior – from the rest of the body) n The blood is now pumped back to the lungs for gas exchange to start over. n
The now deoxygenated (oxygen poor) blood is high in CO 2 n it returns to the heart in large veins called the vena cava ¨superior – from the head; ¨inferior – from the rest of the body) n The blood is now pumped back to the lungs for gas exchange to start over. n
 HOMEOSTASIS and the Metabolic Circuit The aorta is the main artery of systemic circuit. n The vena cava are the main veins of the systemic circuit. n Blood from the heart that is well oxygenated but nutrient poor travels through the aorta to the digestive tract. n
HOMEOSTASIS and the Metabolic Circuit The aorta is the main artery of systemic circuit. n The vena cava are the main veins of the systemic circuit. n Blood from the heart that is well oxygenated but nutrient poor travels through the aorta to the digestive tract. n
 n Capillaries in the villi of the intestines and the stomach lining allow the diffusion of essential nutrients into the blood steam ¨ proteins, amino acids, sugars, fats (into the lacteals of the lymphatic system). Oxygen is delivered to these cells as well. n These digestion products are carried to the liver (HEPATIC PORTAL SYSTEM) where the blood is filtered and toxins metabolized. n
n Capillaries in the villi of the intestines and the stomach lining allow the diffusion of essential nutrients into the blood steam ¨ proteins, amino acids, sugars, fats (into the lacteals of the lymphatic system). Oxygen is delivered to these cells as well. n These digestion products are carried to the liver (HEPATIC PORTAL SYSTEM) where the blood is filtered and toxins metabolized. n
 n The blood stream then carries these nutrients to all body cells ¨ where they diffuse across the cell membranes while cell wastes from metabolism diffuse out (carbon dioxide and N-containing wastes of protein metabolism).
n The blood stream then carries these nutrients to all body cells ¨ where they diffuse across the cell membranes while cell wastes from metabolism diffuse out (carbon dioxide and N-containing wastes of protein metabolism).
 The “polluted” blood is eventually transported to the kidneys (RENAL SYSTEM) where the wastes in the blood are filtered out and concentrated into urine. n The “cleaned” blood that is both nutrient poor and oxygen poor then streams back to the heart. n
The “polluted” blood is eventually transported to the kidneys (RENAL SYSTEM) where the wastes in the blood are filtered out and concentrated into urine. n The “cleaned” blood that is both nutrient poor and oxygen poor then streams back to the heart. n
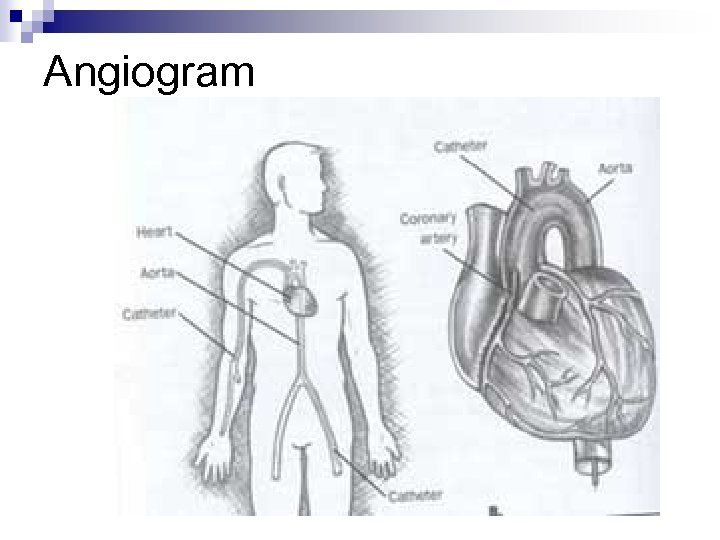 Angiogram
Angiogram
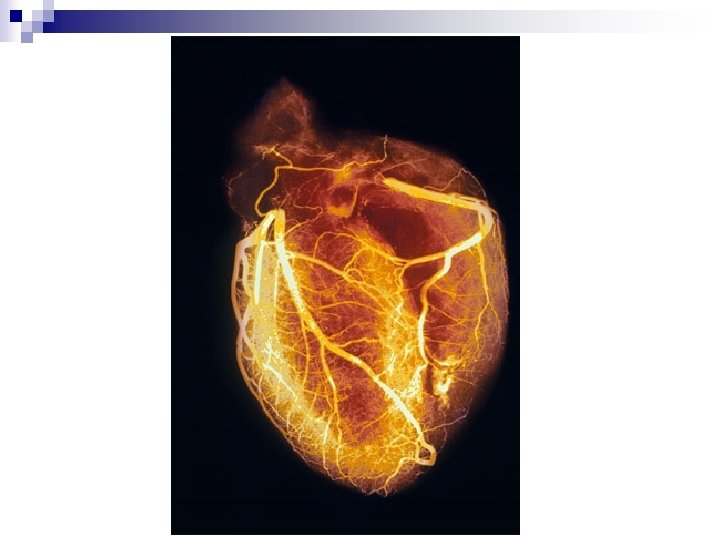

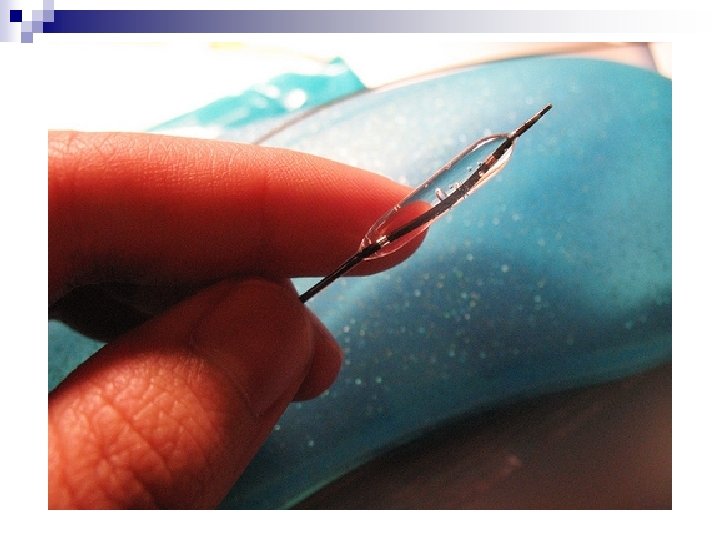
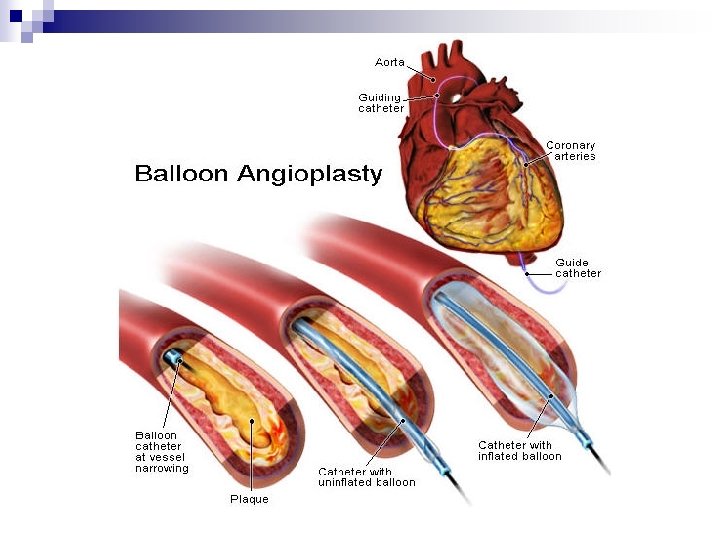
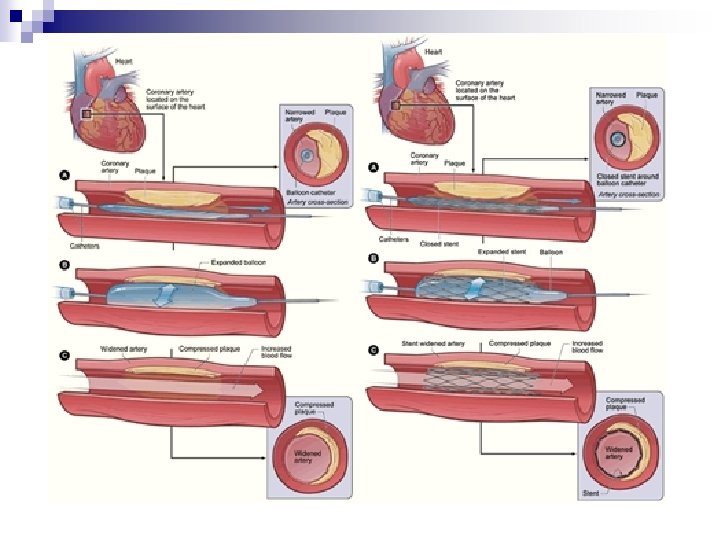
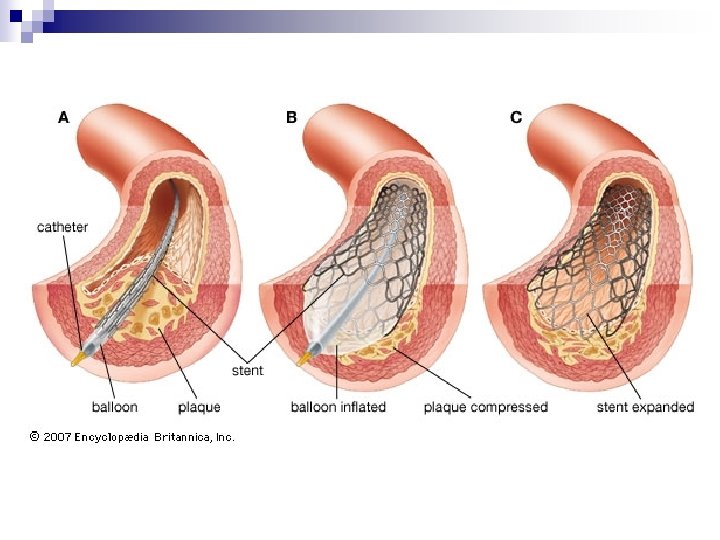
 Angioplasty
Angioplasty
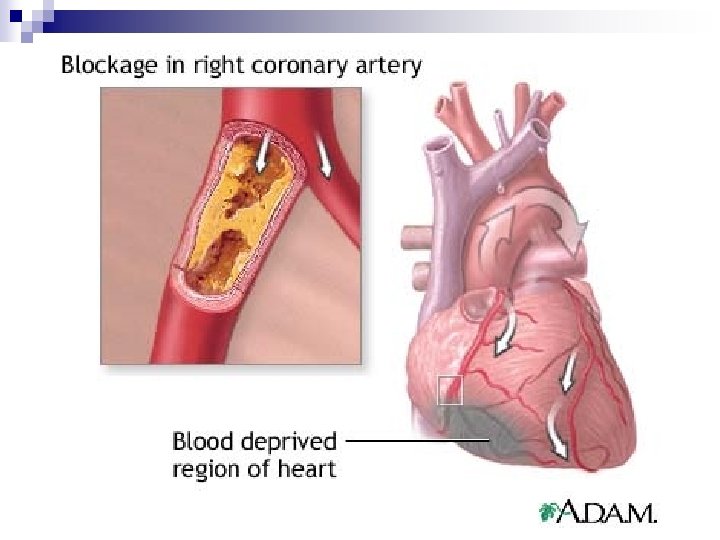
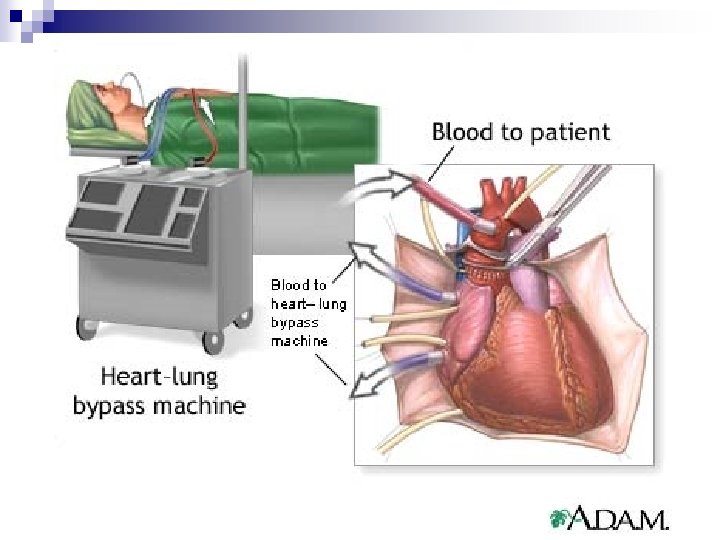
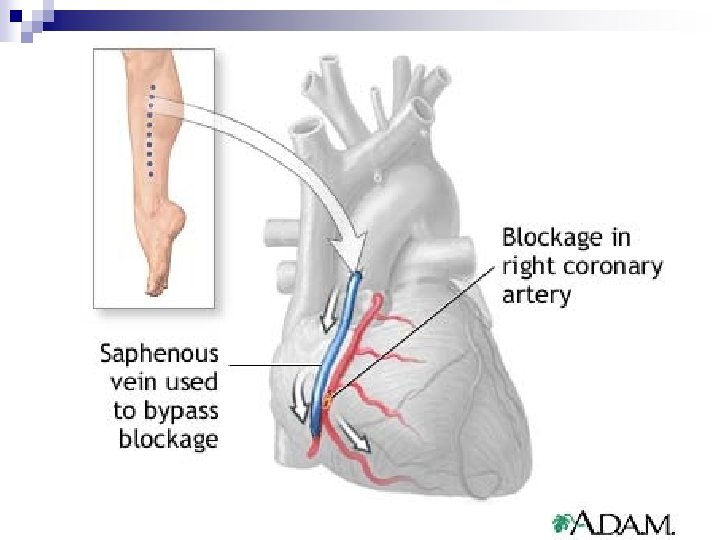
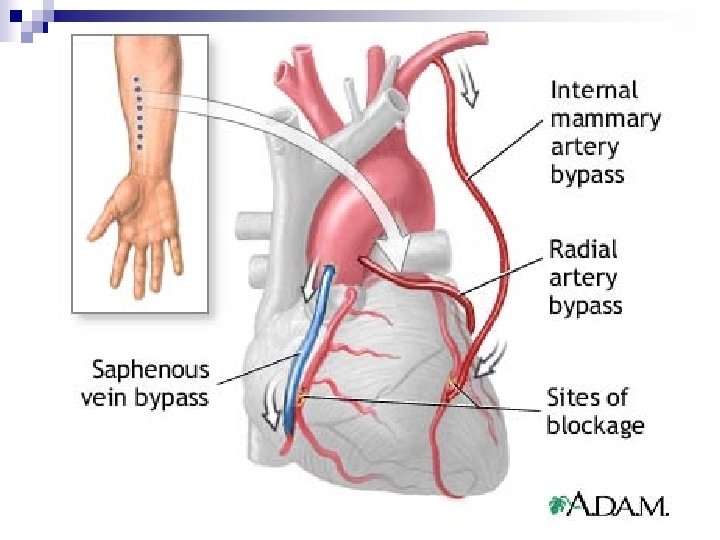
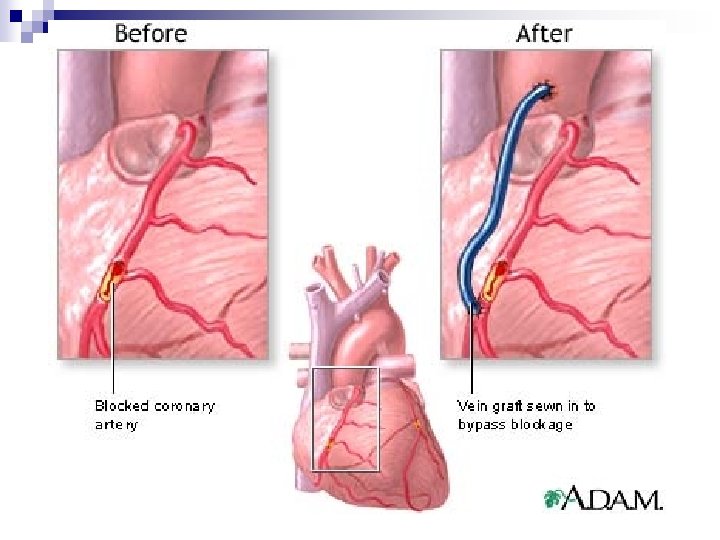
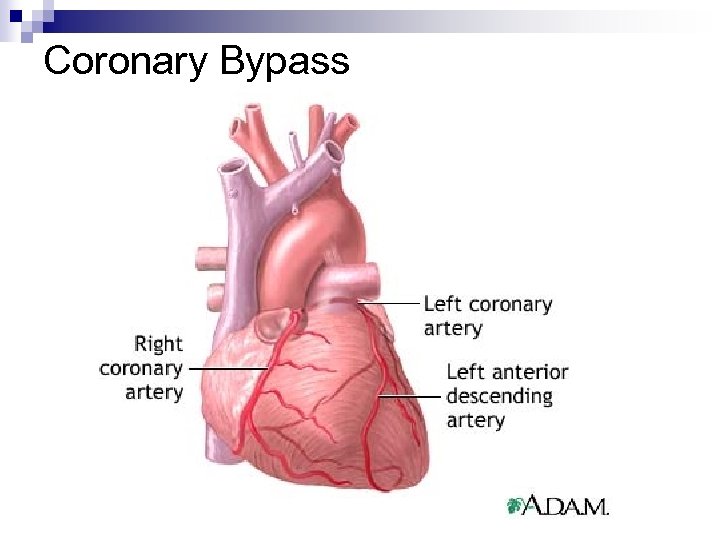 Coronary Bypass
Coronary Bypass
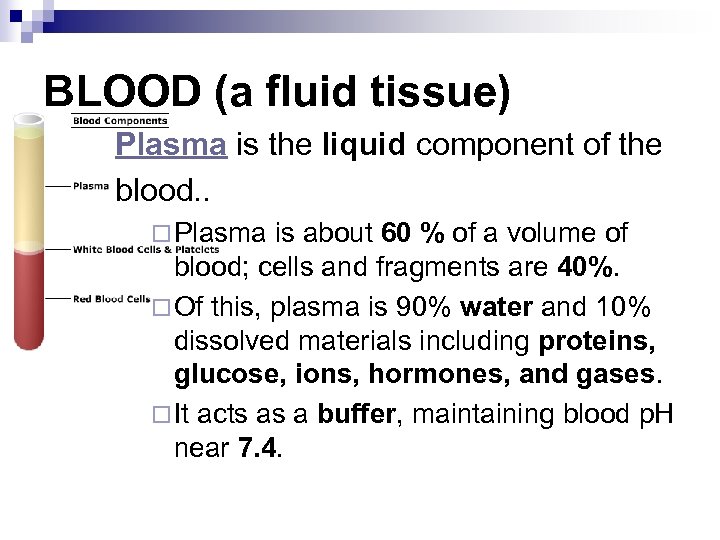 BLOOD (a fluid tissue) Plasma is the liquid component of the blood. . ¨ Plasma is about 60 % of a volume of blood; cells and fragments are 40%. ¨ Of this, plasma is 90% water and 10% dissolved materials including proteins, glucose, ions, hormones, and gases. ¨ It acts as a buffer, maintaining blood p. H near 7. 4.
BLOOD (a fluid tissue) Plasma is the liquid component of the blood. . ¨ Plasma is about 60 % of a volume of blood; cells and fragments are 40%. ¨ Of this, plasma is 90% water and 10% dissolved materials including proteins, glucose, ions, hormones, and gases. ¨ It acts as a buffer, maintaining blood p. H near 7. 4.
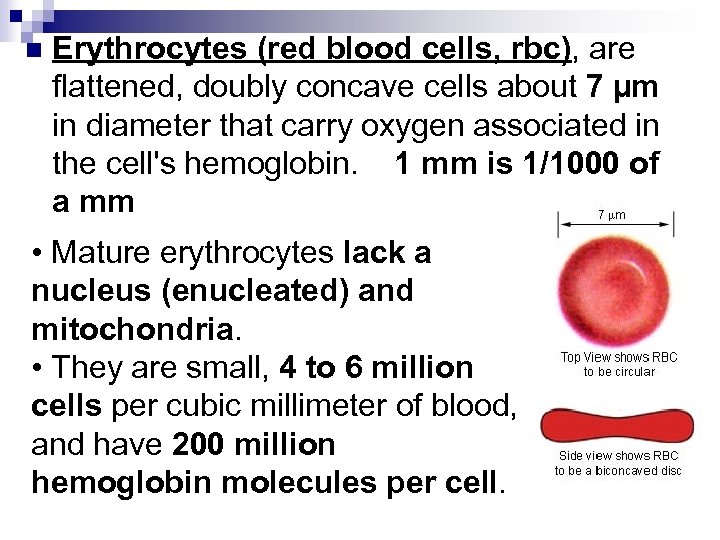 n Erythrocytes (red blood cells, rbc), are flattened, doubly concave cells about 7 µm in diameter that carry oxygen associated in the cell's hemoglobin. 1 mm is 1/1000 of a mm • Mature erythrocytes lack a nucleus (enucleated) and mitochondria. • They are small, 4 to 6 million cells per cubic millimeter of blood, and have 200 million hemoglobin molecules per cell.
n Erythrocytes (red blood cells, rbc), are flattened, doubly concave cells about 7 µm in diameter that carry oxygen associated in the cell's hemoglobin. 1 mm is 1/1000 of a mm • Mature erythrocytes lack a nucleus (enucleated) and mitochondria. • They are small, 4 to 6 million cells per cubic millimeter of blood, and have 200 million hemoglobin molecules per cell.
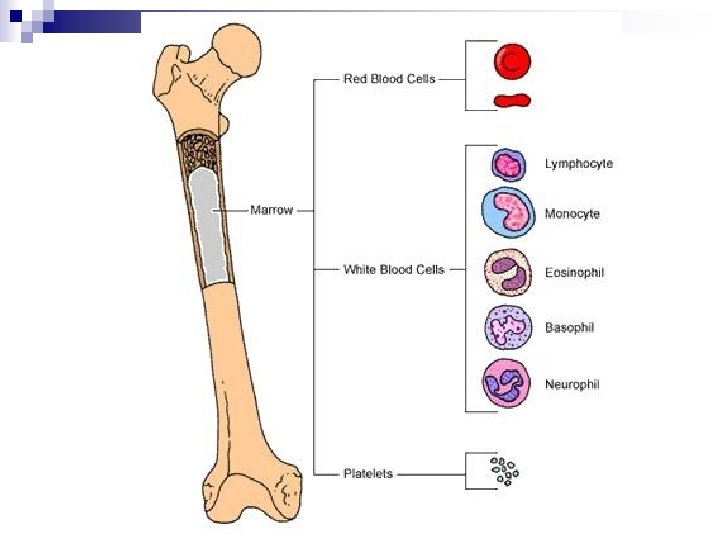
 We have a total of 25 trillion rbc (about 1/3 of all the cells in the body). n Red blood cells are continuously manufactured in red marrow of long bones, ribs, skull, and vertebrae. n Life-span of an erythrocyte is only 120 days, after which they are destroyed in liver and spleen. n
We have a total of 25 trillion rbc (about 1/3 of all the cells in the body). n Red blood cells are continuously manufactured in red marrow of long bones, ribs, skull, and vertebrae. n Life-span of an erythrocyte is only 120 days, after which they are destroyed in liver and spleen. n
 Iron from hemoglobin is recovered and reused by red marrow. The liver degrades the heme units and secretes them as pigment in the bile, responsible for the color of feces. n Each second two million red blood cells are produced to replace those thus taken out of circulation. n Cannot move independently and rely on the heart to move them n
Iron from hemoglobin is recovered and reused by red marrow. The liver degrades the heme units and secretes them as pigment in the bile, responsible for the color of feces. n Each second two million red blood cells are produced to replace those thus taken out of circulation. n Cannot move independently and rely on the heart to move them n
 Leukocytes (white blood cells, wbc), are larger than erythrocytes, have a nucleus and mitochondria, and lack hemoglobin. n White blood cells are best known for their ability to help fight off infection and illness. n When the body creates additional white blood cells, it runs a fever. n
Leukocytes (white blood cells, wbc), are larger than erythrocytes, have a nucleus and mitochondria, and lack hemoglobin. n White blood cells are best known for their ability to help fight off infection and illness. n When the body creates additional white blood cells, it runs a fever. n
 White blood cells propel themselves in an amoebic fashion. n White blood cells are able to seek out an infection site outside of the blood stream thanks to their ability to move independently. n They are able to make their way through the pores within the walls of the capillaries in order to fight infections that are not within the blood stream. n This action of movement through the walls of the capillaries is known as diapedesis. n
White blood cells propel themselves in an amoebic fashion. n White blood cells are able to seek out an infection site outside of the blood stream thanks to their ability to move independently. n They are able to make their way through the pores within the walls of the capillaries in order to fight infections that are not within the blood stream. n This action of movement through the walls of the capillaries is known as diapedesis. n
 n n n 1. White blood cells (leukocytes) are less than 1% of the blood's volume. They are made from stem cells in bone marrow. There are five types of leukocytes, important components of the immune system. Neutrophils enter the tissue fluid by squeezing through capillary walls and phagocytozing foreign substances.
n n n 1. White blood cells (leukocytes) are less than 1% of the blood's volume. They are made from stem cells in bone marrow. There are five types of leukocytes, important components of the immune system. Neutrophils enter the tissue fluid by squeezing through capillary walls and phagocytozing foreign substances.
 2. 3. Eosinophils also fight infection, they are acid loving and will secrete a harmful toxin into parasites to kill them. They also are responsible in our allergy responses. Although they are not suppose to accumulate in the lungs, in asthmatics they do—this is being studied. Macrophages release white blood cell growth factors, causing a population increase for white blood cells.
2. 3. Eosinophils also fight infection, they are acid loving and will secrete a harmful toxin into parasites to kill them. They also are responsible in our allergy responses. Although they are not suppose to accumulate in the lungs, in asthmatics they do—this is being studied. Macrophages release white blood cell growth factors, causing a population increase for white blood cells.
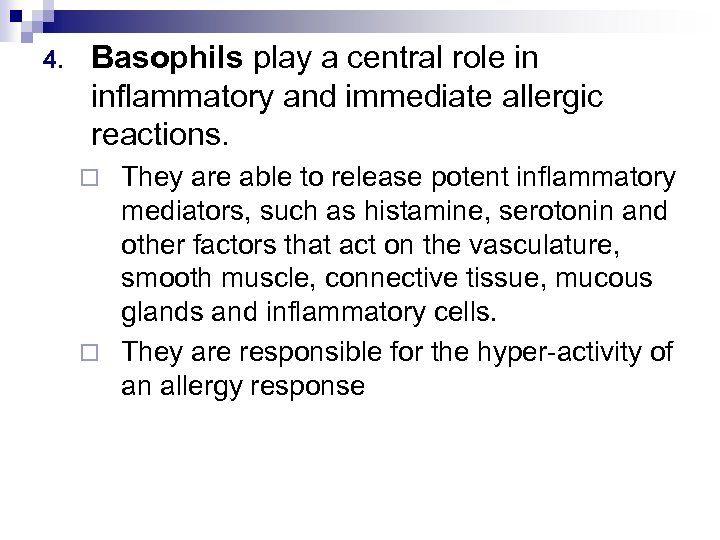 4. Basophils play a central role in inflammatory and immediate allergic reactions. They are able to release potent inflammatory mediators, such as histamine, serotonin and other factors that act on the vasculature, smooth muscle, connective tissue, mucous glands and inflammatory cells. ¨ They are responsible for the hyper-activity of an allergy response ¨
4. Basophils play a central role in inflammatory and immediate allergic reactions. They are able to release potent inflammatory mediators, such as histamine, serotonin and other factors that act on the vasculature, smooth muscle, connective tissue, mucous glands and inflammatory cells. ¨ They are responsible for the hyper-activity of an allergy response ¨
 5. Lymphocytes and MONOCYTES fight infection. ¨ T-cells attack cells containing viruses. ¨ B-cells produce antibodies.
5. Lymphocytes and MONOCYTES fight infection. ¨ T-cells attack cells containing viruses. ¨ B-cells produce antibodies.
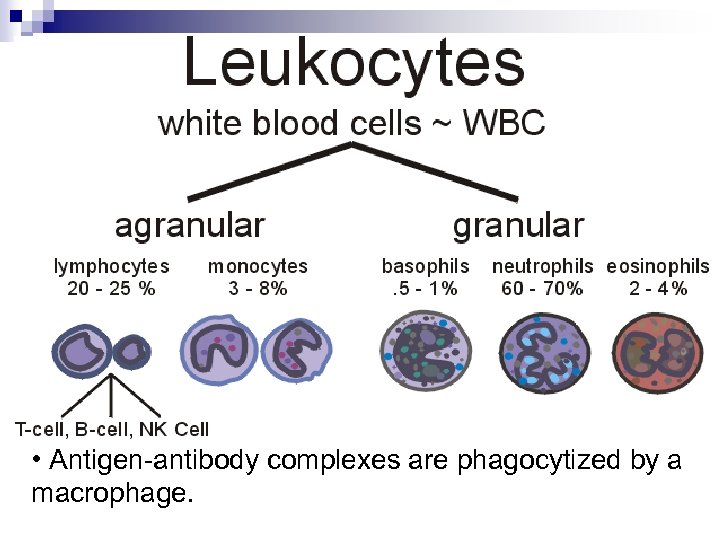 • Antigen-antibody complexes are phagocytized by a macrophage.
• Antigen-antibody complexes are phagocytized by a macrophage.
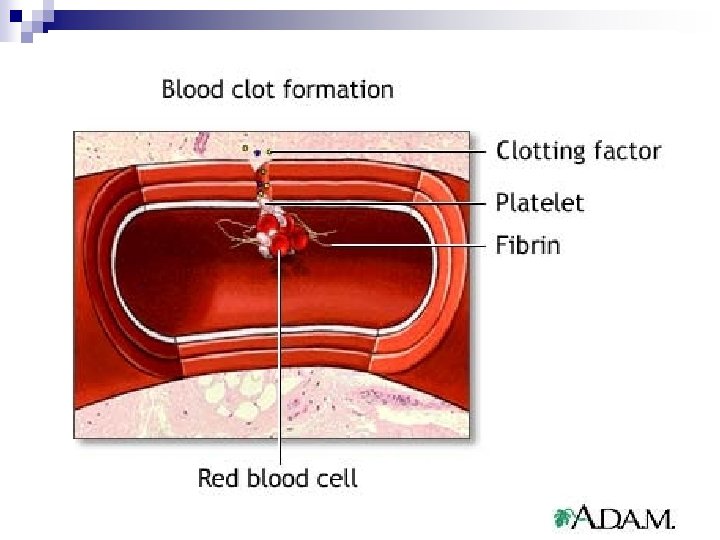
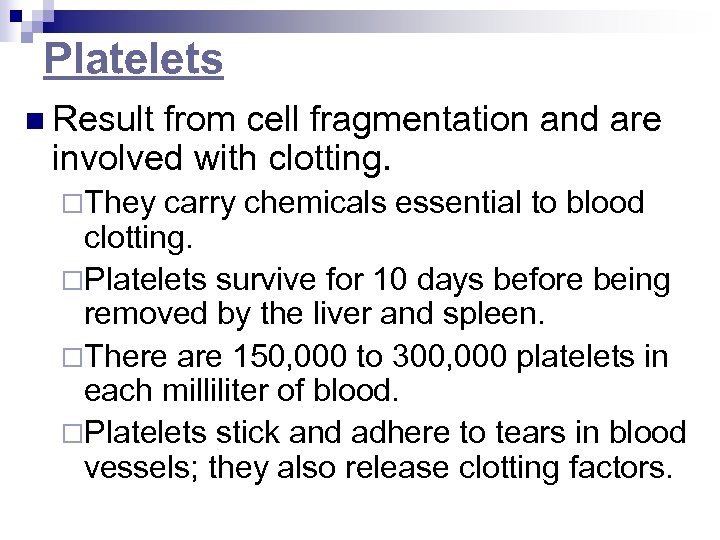 Platelets n Result from cell fragmentation and are involved with clotting. ¨They carry chemicals essential to blood clotting. ¨Platelets survive for 10 days before being removed by the liver and spleen. ¨There are 150, 000 to 300, 000 platelets in each milliliter of blood. ¨Platelets stick and adhere to tears in blood vessels; they also release clotting factors.
Platelets n Result from cell fragmentation and are involved with clotting. ¨They carry chemicals essential to blood clotting. ¨Platelets survive for 10 days before being removed by the liver and spleen. ¨There are 150, 000 to 300, 000 platelets in each milliliter of blood. ¨Platelets stick and adhere to tears in blood vessels; they also release clotting factors.
 Hemophilia A hemophiliac's blood cannot clot. n Providing correct proteins (clotting factors) has been a common method of treating hemophiliacs. n It has also led to HIV transmission due to the use of transfusions and use of contaminated blood products. n http: //www. funsci. com/fun 3_en/blood. htm
Hemophilia A hemophiliac's blood cannot clot. n Providing correct proteins (clotting factors) has been a common method of treating hemophiliacs. n It has also led to HIV transmission due to the use of transfusions and use of contaminated blood products. n http: //www. funsci. com/fun 3_en/blood. htm
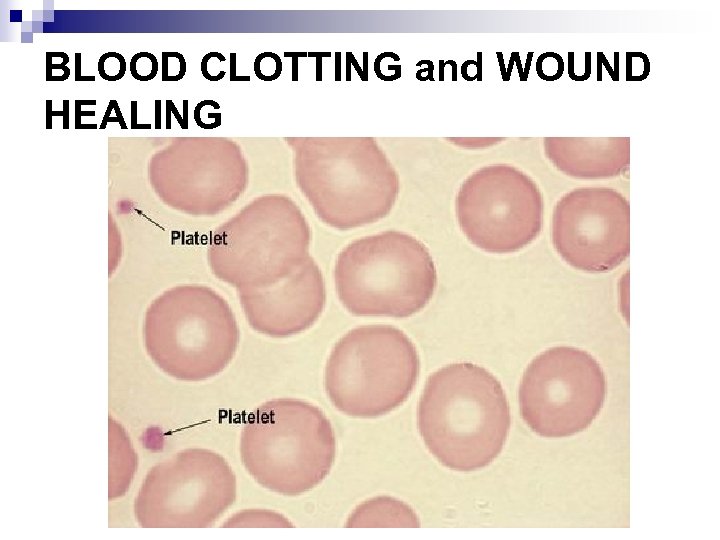 BLOOD CLOTTING and WOUND HEALING
BLOOD CLOTTING and WOUND HEALING
 Platelets are vital to the blood clotting process. n For a clot to form, the platelets make up nearly the entire blood clot. n The platelet plug is reinforced by the threads of fibrin which is activated by the phospholipids in the cell. n These phospholipids activate the plasma’s blood clotting factors, creating what is commonly seen on the outside of the body as a scab. n
Platelets are vital to the blood clotting process. n For a clot to form, the platelets make up nearly the entire blood clot. n The platelet plug is reinforced by the threads of fibrin which is activated by the phospholipids in the cell. n These phospholipids activate the plasma’s blood clotting factors, creating what is commonly seen on the outside of the body as a scab. n
 The action of the platelets forming the plug release serotonin into the blood stream. n The serotonin encourages the body to restrict the flow of blood. n This constraint of the blood vessels reduces blood flow at the injury site, allowing the platelets to clot, form a secure plug, and ceases the flow of blood to outside the site of injury. n
The action of the platelets forming the plug release serotonin into the blood stream. n The serotonin encourages the body to restrict the flow of blood. n This constraint of the blood vessels reduces blood flow at the injury site, allowing the platelets to clot, form a secure plug, and ceases the flow of blood to outside the site of injury. n
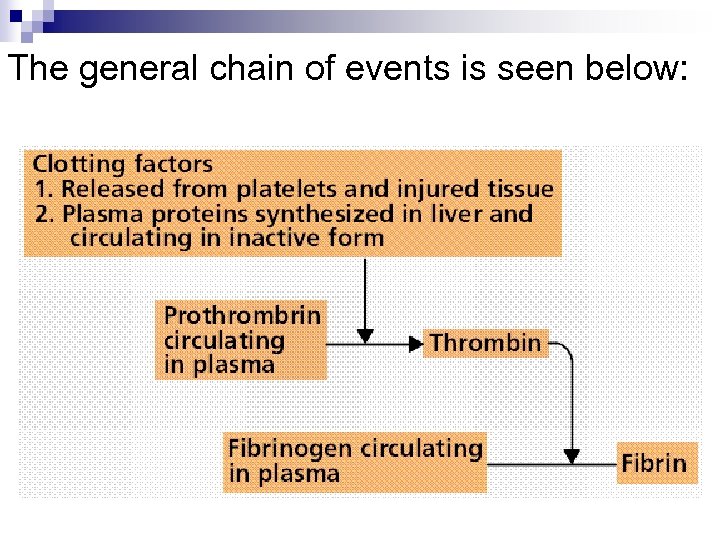 The general chain of events is seen below:
The general chain of events is seen below:
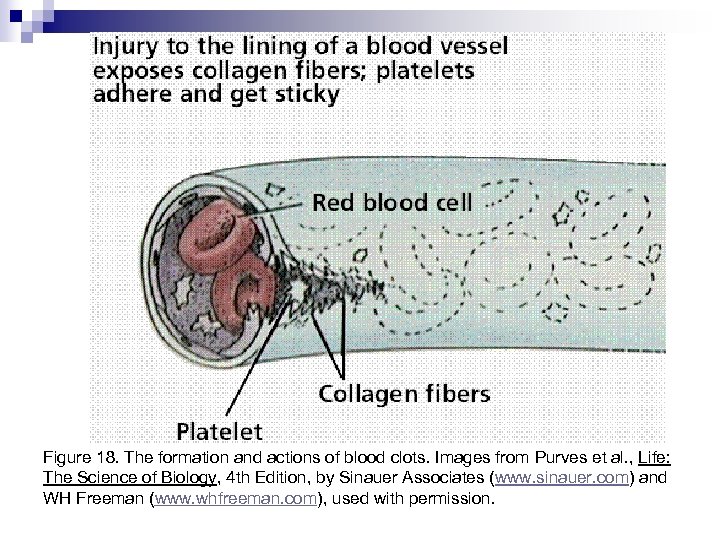 Figure 18. The formation and actions of blood clots. Images from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.
Figure 18. The formation and actions of blood clots. Images from Purves et al. , Life: The Science of Biology, 4 th Edition, by Sinauer Associates (www. sinauer. com) and WH Freeman (www. whfreeman. com), used with permission.

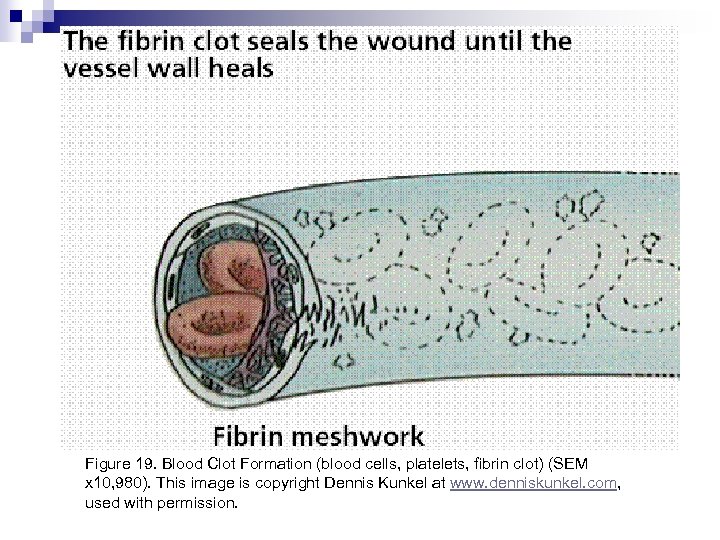 Figure 19. Blood Clot Formation (blood cells, platelets, fibrin clot) (SEM x 10, 980). This image is copyright Dennis Kunkel at www. denniskunkel. com, used with permission.
Figure 19. Blood Clot Formation (blood cells, platelets, fibrin clot) (SEM x 10, 980). This image is copyright Dennis Kunkel at www. denniskunkel. com, used with permission.
 Interactive Web Sites Progression of Atherosclerosis n Deep Vein Thrombosis (DVT) n
Interactive Web Sites Progression of Atherosclerosis n Deep Vein Thrombosis (DVT) n
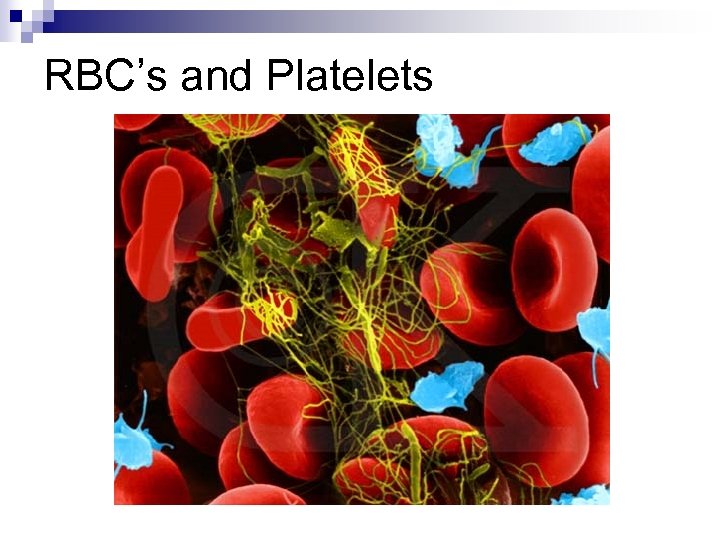 RBC’s and Platelets
RBC’s and Platelets
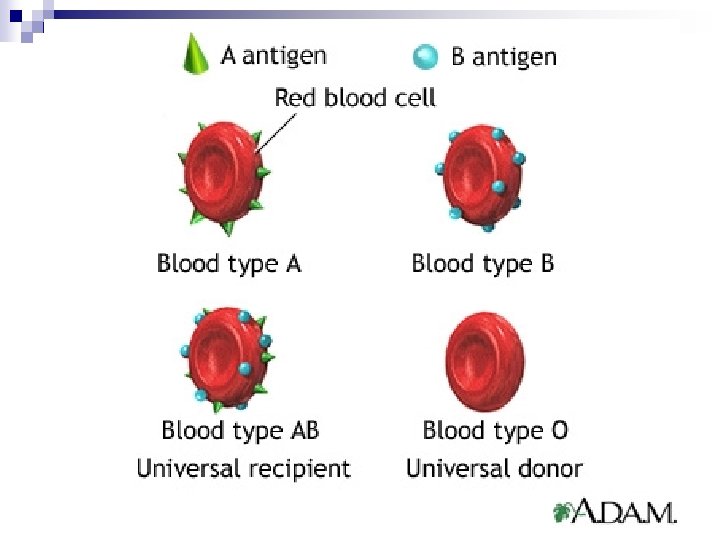
 Blood Types n Antigen ¨ Protein on the surface of cells. (in blood, Allele A makes A antigen. ¨ Allele B makes B antigen. Allele O makes no antigens. )
Blood Types n Antigen ¨ Protein on the surface of cells. (in blood, Allele A makes A antigen. ¨ Allele B makes B antigen. Allele O makes no antigens. )
 Antibody: n Protein in plasma that reacts with specific antigens that enter the blood (usually something that isn't supposed to be there!). n (Ex. : Anti-A is an antibody that recognizes A-antigen, binds to it (lock & key), then causes clumping together or clotting of similar A-antigens. ) n These are often depicted Y-shaped.
Antibody: n Protein in plasma that reacts with specific antigens that enter the blood (usually something that isn't supposed to be there!). n (Ex. : Anti-A is an antibody that recognizes A-antigen, binds to it (lock & key), then causes clumping together or clotting of similar A-antigens. ) n These are often depicted Y-shaped.
 n Agglutination: clumping of blood cells n Genotype: type of gene present (or allele) n Phenotype: the expression of the gene we observe
n Agglutination: clumping of blood cells n Genotype: type of gene present (or allele) n Phenotype: the expression of the gene we observe
 Everybody has a blood type. n There are several classifications possible. n The most common blood type classification system is the ABO system discovered by Karl Landsteiner in the early 1900 s. n There is also the Rh (Rhesus factor) as well, especially important for childbirth. n There are four types of blood in the ABO system: A, B, AB, and O. n There are two types of blood in the Rh system: Rh+ and Rh-
Everybody has a blood type. n There are several classifications possible. n The most common blood type classification system is the ABO system discovered by Karl Landsteiner in the early 1900 s. n There is also the Rh (Rhesus factor) as well, especially important for childbirth. n There are four types of blood in the ABO system: A, B, AB, and O. n There are two types of blood in the Rh system: Rh+ and Rh-
 Your blood type is established before you are born, by specific genes inherited from your parents. n You receive one gene from your mother and one from your father; these two combine to establish your blood type. n These genes can appear in different versions or ALLELES. There are three alleles of the blood type gene: A, B, and O. n
Your blood type is established before you are born, by specific genes inherited from your parents. n You receive one gene from your mother and one from your father; these two combine to establish your blood type. n These genes can appear in different versions or ALLELES. There are three alleles of the blood type gene: A, B, and O. n
 These two genes determine your blood type by causing proteins called ANTIGENS to exist on the surface of all of your red blood cells. n Since everybody has two copies of these genes, there are six possible combinations; AA, BB, OO, AB, AO, and BO. n In genetic terms, these combinations are called genotypes, and they describe the genes you got from your parents. n
These two genes determine your blood type by causing proteins called ANTIGENS to exist on the surface of all of your red blood cells. n Since everybody has two copies of these genes, there are six possible combinations; AA, BB, OO, AB, AO, and BO. n In genetic terms, these combinations are called genotypes, and they describe the genes you got from your parents. n
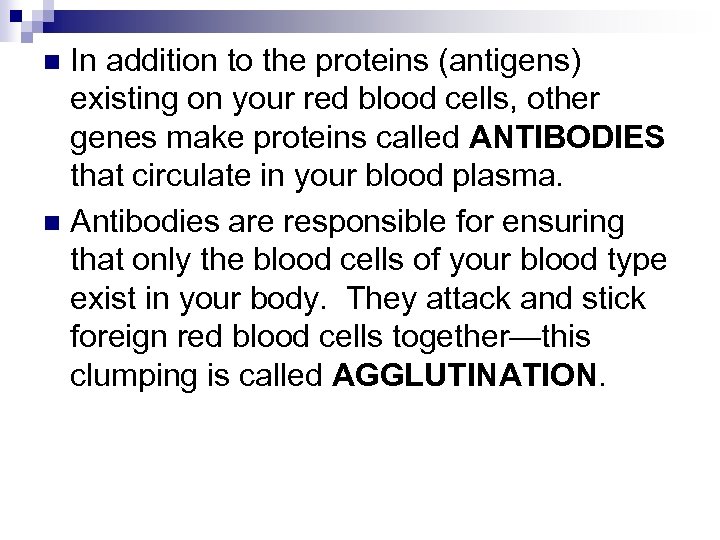 In addition to the proteins (antigens) existing on your red blood cells, other genes make proteins called ANTIBODIES that circulate in your blood plasma. n Antibodies are responsible for ensuring that only the blood cells of your blood type exist in your body. They attack and stick foreign red blood cells together—this clumping is called AGGLUTINATION. n
In addition to the proteins (antigens) existing on your red blood cells, other genes make proteins called ANTIBODIES that circulate in your blood plasma. n Antibodies are responsible for ensuring that only the blood cells of your blood type exist in your body. They attack and stick foreign red blood cells together—this clumping is called AGGLUTINATION. n
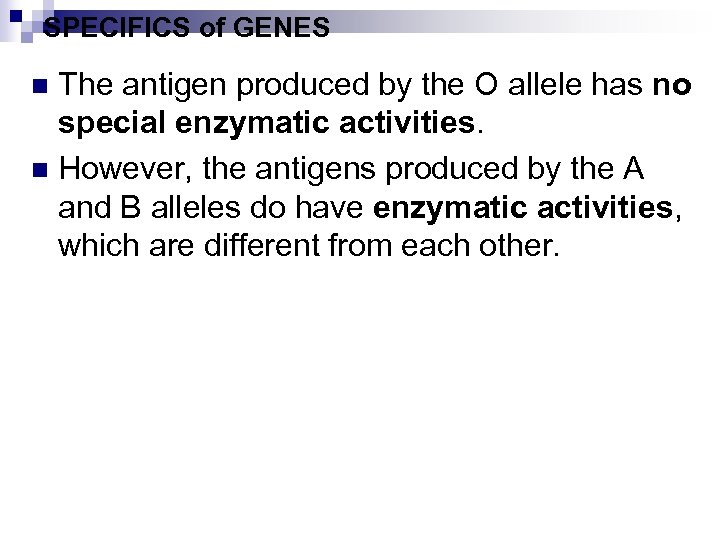 SPECIFICS of GENES The antigen produced by the O allele has no special enzymatic activities. n However, the antigens produced by the A and B alleles do have enzymatic activities, which are different from each other. n
SPECIFICS of GENES The antigen produced by the O allele has no special enzymatic activities. n However, the antigens produced by the A and B alleles do have enzymatic activities, which are different from each other. n
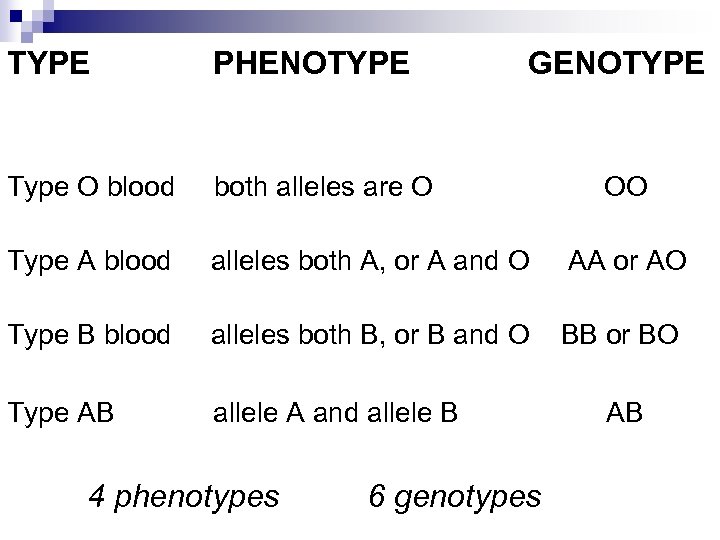 TYPE PHENOTYPE Type O blood both alleles are O Type A blood alleles both A, or A and O AA or AO Type B blood alleles both B, or B and O BB or BO Type AB allele A and allele B 4 phenotypes GENOTYPE 6 genotypes OO AB
TYPE PHENOTYPE Type O blood both alleles are O Type A blood alleles both A, or A and O AA or AO Type B blood alleles both B, or B and O BB or BO Type AB allele A and allele B 4 phenotypes GENOTYPE 6 genotypes OO AB
 People with Type A blood have Antibody. B (anti-B) in their blood plasma. n Anti-B helps the body destroy any type B blood cells that might enter the circulation system. n Likewise, people with the BB and the BO genotypes are said to have type B blood. These people have antibody-A (anti-A) in their blood plasma. n Anti-A helps the body destroy any type A blood cells that might enter the circulation system. n
People with Type A blood have Antibody. B (anti-B) in their blood plasma. n Anti-B helps the body destroy any type B blood cells that might enter the circulation system. n Likewise, people with the BB and the BO genotypes are said to have type B blood. These people have antibody-A (anti-A) in their blood plasma. n Anti-A helps the body destroy any type A blood cells that might enter the circulation system. n
 People who have the AB genotype have the enzyme activity associated with both the A and B alleles. n These people have no anti-A nor anti-B in their blood plasma. n
People who have the AB genotype have the enzyme activity associated with both the A and B alleles. n These people have no anti-A nor anti-B in their blood plasma. n
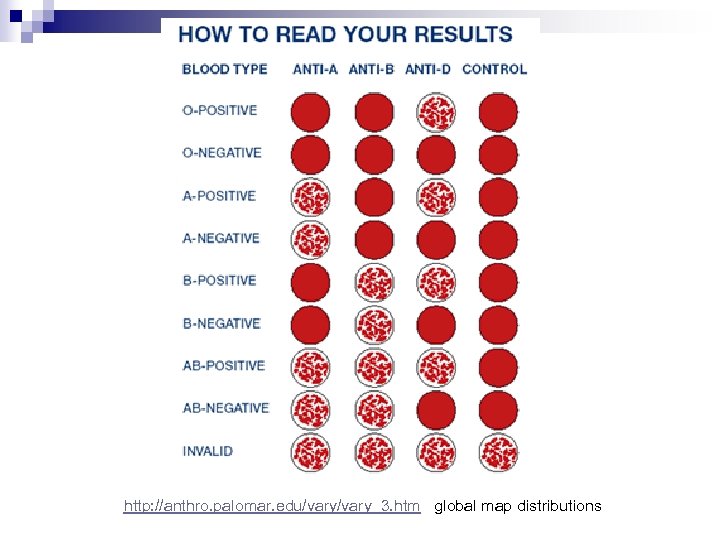
 SPECIFICS of TYPING BLOOD The ABO blood typing is done by taking two drops of blood on two slides. n Anti-A serum(antibody A) is added to one slide. Anti-B serum is added to the other slide. n The antibodies will attack and agglutinate blood cells that have the antigen-A and antigen-B present on their surfaces. n
SPECIFICS of TYPING BLOOD The ABO blood typing is done by taking two drops of blood on two slides. n Anti-A serum(antibody A) is added to one slide. Anti-B serum is added to the other slide. n The antibodies will attack and agglutinate blood cells that have the antigen-A and antigen-B present on their surfaces. n
 THUS the antibodies are used to type the same blood. n Sometimes, Rh is also tested using anti-D. n If there is clumping with anti-D the blood is Rh+. If there is no clumping, it is Rh-. n
THUS the antibodies are used to type the same blood. n Sometimes, Rh is also tested using anti-D. n If there is clumping with anti-D the blood is Rh+. If there is no clumping, it is Rh-. n
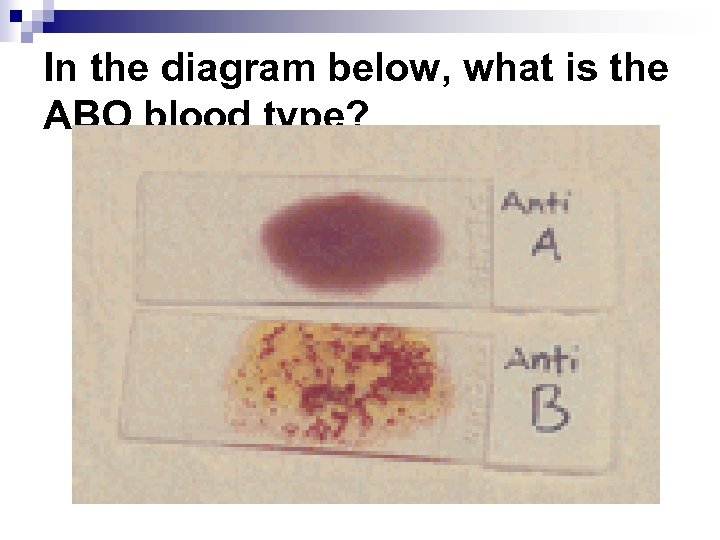 In the diagram below, what is the ABO blood type?
In the diagram below, what is the ABO blood type?
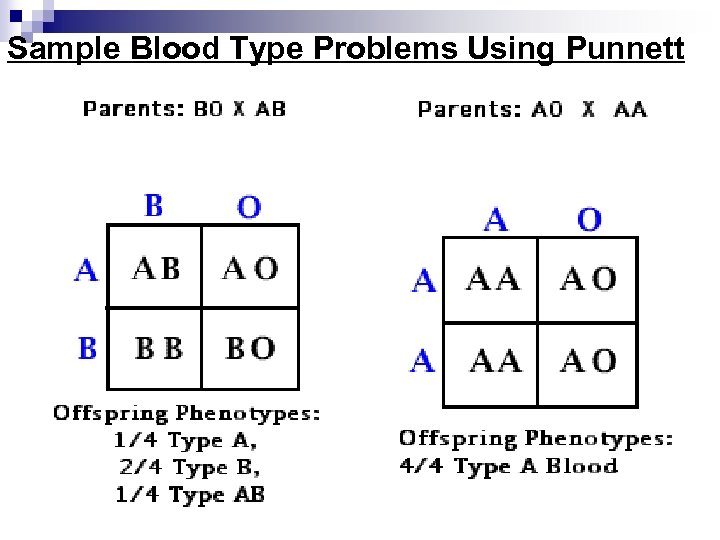 Sample Blood Type Problems Using Punnett
Sample Blood Type Problems Using Punnett
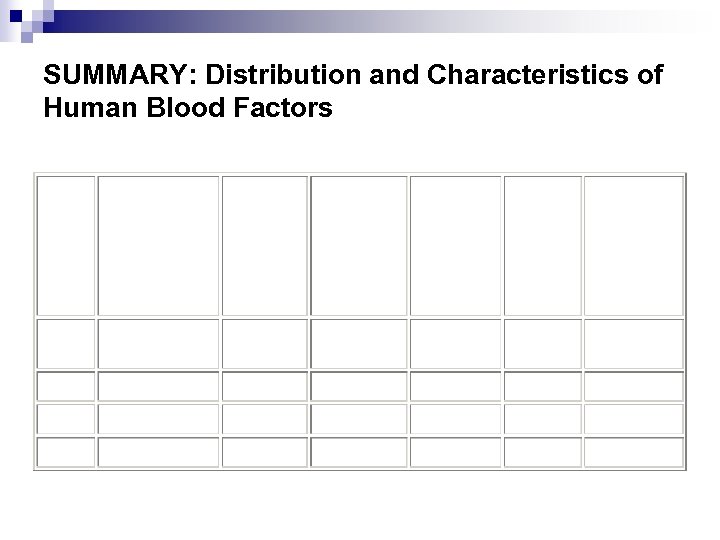 SUMMARY: Distribution and Characteristics of Human Blood Factors
SUMMARY: Distribution and Characteristics of Human Blood Factors
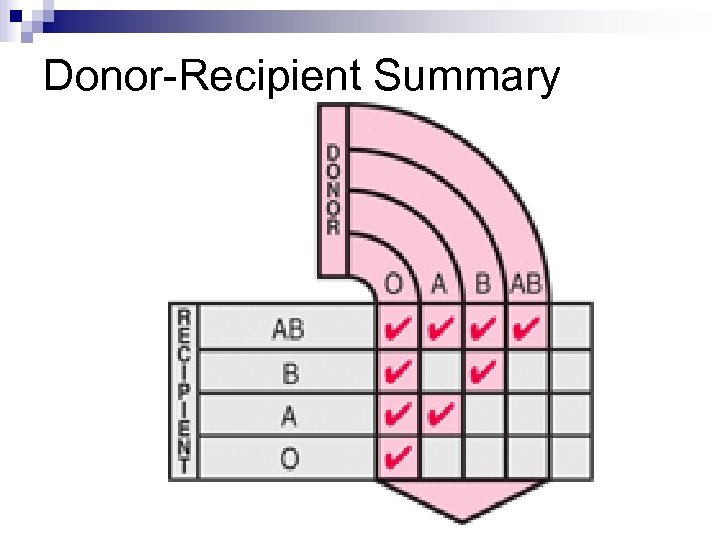 Donor-Recipient Summary
Donor-Recipient Summary
 Type O Blood: Universal Donor as it contains no A or B antigens, so the receivers' blood will not clot when given the O blood. n Type AB Blood: Universal Receiver, as it contains no Anti-A or Anti-B antibodies in its plasma. It can receive all blood types. n http: //ghs. gresham. k 12. or. us/science/ps/sci/soph/genetics/notes/bloodtype. htm
Type O Blood: Universal Donor as it contains no A or B antigens, so the receivers' blood will not clot when given the O blood. n Type AB Blood: Universal Receiver, as it contains no Anti-A or Anti-B antibodies in its plasma. It can receive all blood types. n http: //ghs. gresham. k 12. or. us/science/ps/sci/soph/genetics/notes/bloodtype. htm
 http: //anthro. palomar. edu/vary_3. htm global map distributions
http: //anthro. palomar. edu/vary_3. htm global map distributions
 BLOOD TYPING WORKSHEET Directions: n Given the alleles, genotypes and phenotypes for human blood typing ABO, solve the following multiple allele problems. n Other blood type systems are used in paternity cases and crime scene analysis. n The ABO is always the first to be performed. n Probability is reduced from there. n Use your notes and text as needed.
BLOOD TYPING WORKSHEET Directions: n Given the alleles, genotypes and phenotypes for human blood typing ABO, solve the following multiple allele problems. n Other blood type systems are used in paternity cases and crime scene analysis. n The ABO is always the first to be performed. n Probability is reduced from there. n Use your notes and text as needed.
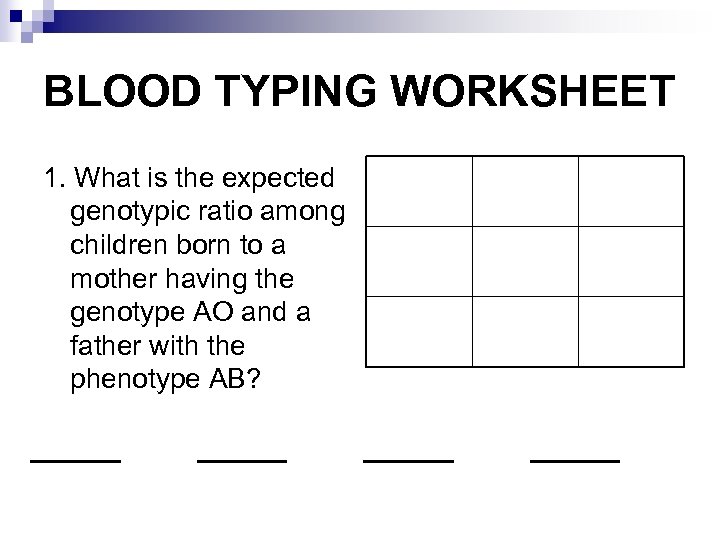 BLOOD TYPING WORKSHEET 1. What is the expected genotypic ratio among children born to a mother having the genotype AO and a father with the phenotype AB? ____
BLOOD TYPING WORKSHEET 1. What is the expected genotypic ratio among children born to a mother having the genotype AO and a father with the phenotype AB? ____
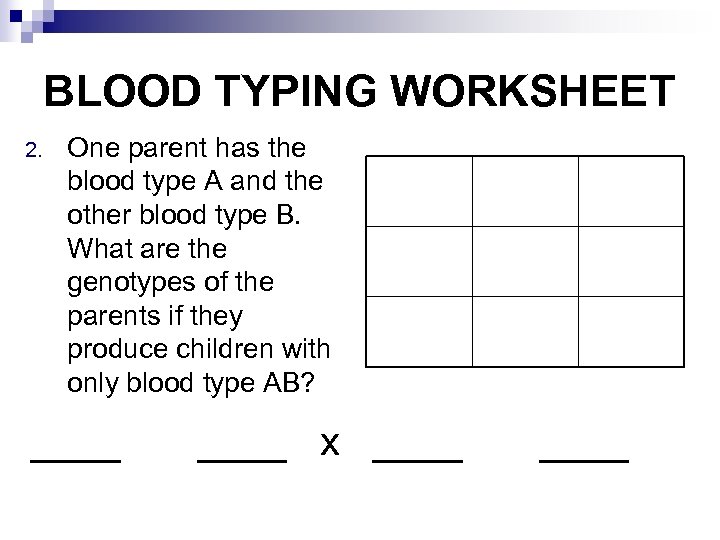 BLOOD TYPING WORKSHEET 2. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if they produce children with only blood type AB? ____ x ____
BLOOD TYPING WORKSHEET 2. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if they produce children with only blood type AB? ____ x ____
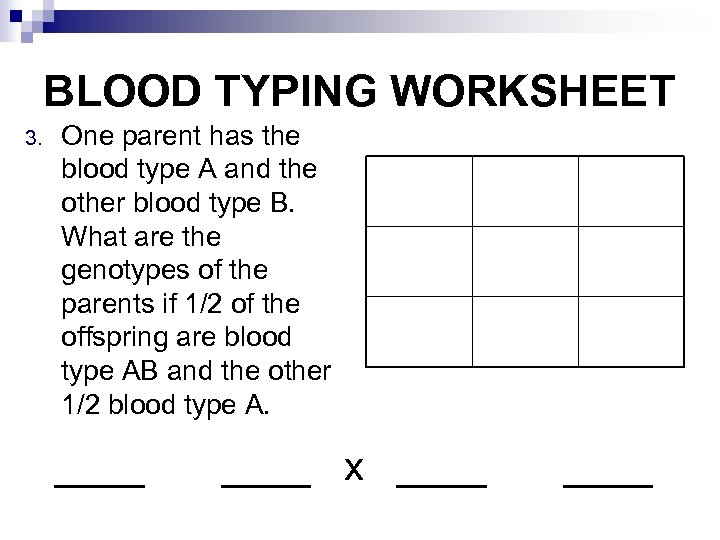 BLOOD TYPING WORKSHEET 3. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if 1/2 of the offspring are blood type AB and the other 1/2 blood type A. ____ x ____
BLOOD TYPING WORKSHEET 3. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if 1/2 of the offspring are blood type AB and the other 1/2 blood type A. ____ x ____
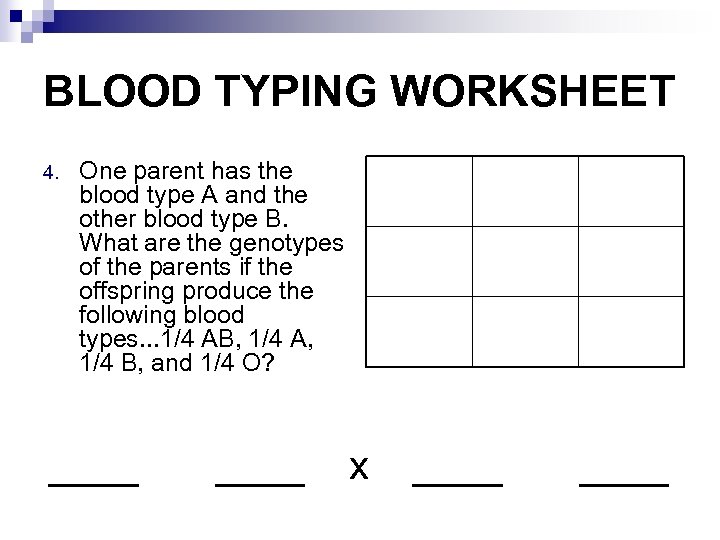 BLOOD TYPING WORKSHEET 4. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if the offspring produce the following blood types. . . 1/4 AB, 1/4 A, 1/4 B, and 1/4 O? ____ x ____
BLOOD TYPING WORKSHEET 4. One parent has the blood type A and the other blood type B. What are the genotypes of the parents if the offspring produce the following blood types. . . 1/4 AB, 1/4 A, 1/4 B, and 1/4 O? ____ x ____
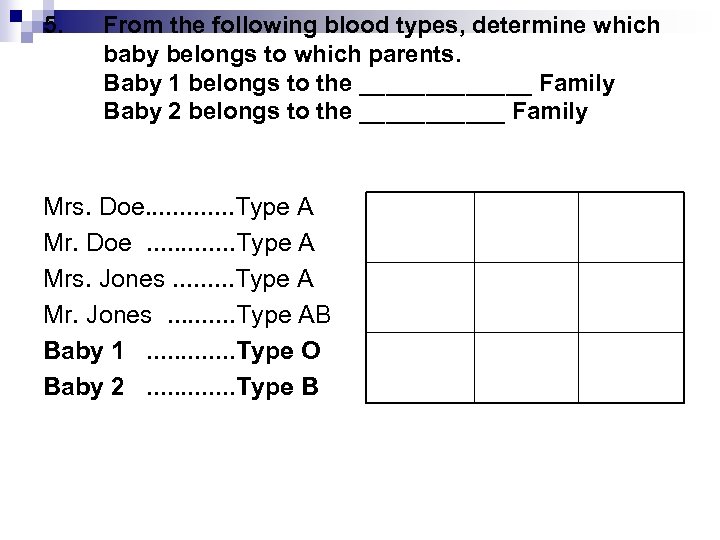 5. From the following blood types, determine which baby belongs to which parents. Baby 1 belongs to the _______ Family Baby 2 belongs to the ______ Family Mrs. Doe. . . Type A Mrs. Jones. . Type A Mr. Jones. . Type AB Baby 1. . . Type O Baby 2. . . Type B
5. From the following blood types, determine which baby belongs to which parents. Baby 1 belongs to the _______ Family Baby 2 belongs to the ______ Family Mrs. Doe. . . Type A Mrs. Jones. . Type A Mr. Jones. . Type AB Baby 1. . . Type O Baby 2. . . Type B
 BLOOD TYPING WORKSHEET
BLOOD TYPING WORKSHEET
 Rh Factor and Erythroblastosis Fetalis n In addition to the blood group (A, B, O, AB), the Rh factor is written as either positive (Rh+ means antigen present) or negative (Rh- means antigen absent). Most people are Rh+ (85% in Canada). eg. A- (means blood type A, Rh negative) AB+ (means blood type AB, with Rh factor)
Rh Factor and Erythroblastosis Fetalis n In addition to the blood group (A, B, O, AB), the Rh factor is written as either positive (Rh+ means antigen present) or negative (Rh- means antigen absent). Most people are Rh+ (85% in Canada). eg. A- (means blood type A, Rh negative) AB+ (means blood type AB, with Rh factor)
 This factor does not effect your health except if you are an Rh+ fetus in an Rhmother, rarely also with blood transfusions. n RISK: A woman’s baby is at risk when she has a negative Rh factor and her partner has a positive Rh factor. n See page 979 n
This factor does not effect your health except if you are an Rh+ fetus in an Rhmother, rarely also with blood transfusions. n RISK: A woman’s baby is at risk when she has a negative Rh factor and her partner has a positive Rh factor. n See page 979 n
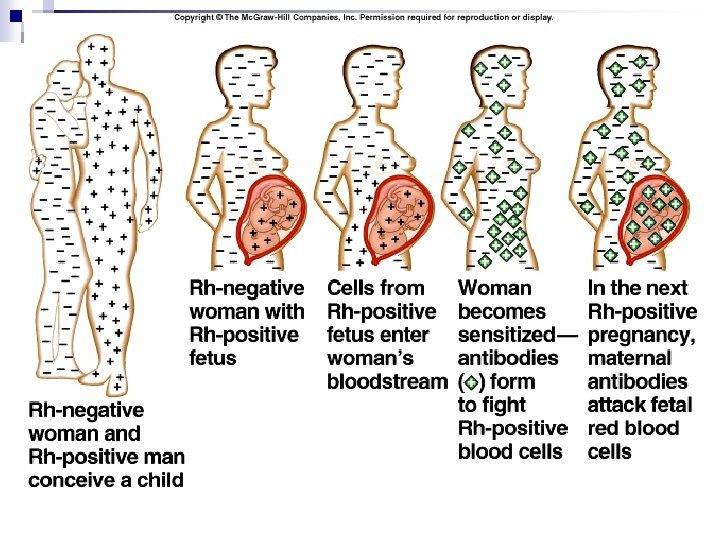
 The mother’s antibodies begin clumping the baby’s hemoglobin molecules so that they cannot attach oxygen, breaking them down. n This causes a severe anemia called “Hemolytic disease of the Newborn” or Erythroblastosis fetalis. n The result is massive swelling of the newborn and can cause illness, brain damage and even death. n It may also be mild (jaundice) or absent. n
The mother’s antibodies begin clumping the baby’s hemoglobin molecules so that they cannot attach oxygen, breaking them down. n This causes a severe anemia called “Hemolytic disease of the Newborn” or Erythroblastosis fetalis. n The result is massive swelling of the newborn and can cause illness, brain damage and even death. n It may also be mild (jaundice) or absent. n
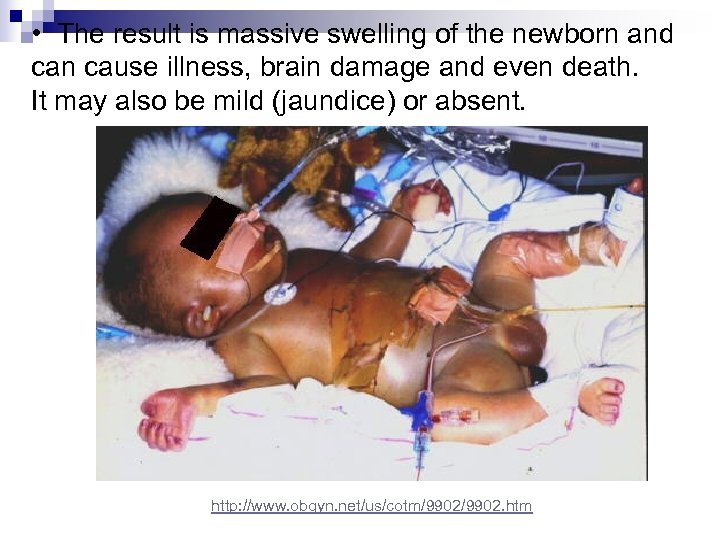 • The result is massive swelling of the newborn and can cause illness, brain damage and even death. It may also be mild (jaundice) or absent. http: //www. obgyn. net/us/cotm/9902. htm
• The result is massive swelling of the newborn and can cause illness, brain damage and even death. It may also be mild (jaundice) or absent. http: //www. obgyn. net/us/cotm/9902. htm
 Hemolytic disease can be prevented for many infants, if their mother is not already sensitized. n This disease used to adversely affect 1 in 16 000 babies. n Research at the University of Manitoba throughout the 50 s and 60 s produced a treatment that has become the world standard for preventing this type of anemia in infants. n
Hemolytic disease can be prevented for many infants, if their mother is not already sensitized. n This disease used to adversely affect 1 in 16 000 babies. n Research at the University of Manitoba throughout the 50 s and 60 s produced a treatment that has become the world standard for preventing this type of anemia in infants. n
 Rh immunoglobulin (Rh. Ig) is a blood product given via injection to help the Rh negative mother by suppressing her ability to react to the Rh positive red cells from her baby. n Reactions to the medication are generally minor, including soreness at the injection sight and sometimes a slight fever. n
Rh immunoglobulin (Rh. Ig) is a blood product given via injection to help the Rh negative mother by suppressing her ability to react to the Rh positive red cells from her baby. n Reactions to the medication are generally minor, including soreness at the injection sight and sometimes a slight fever. n
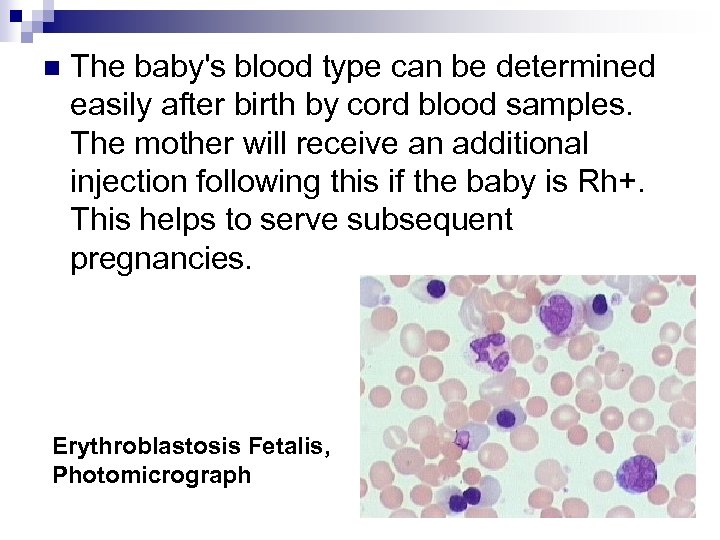 n The baby's blood type can be determined easily after birth by cord blood samples. The mother will receive an additional injection following this if the baby is Rh+. This helps to serve subsequent pregnancies. Erythroblastosis Fetalis, Photomicrograph
n The baby's blood type can be determined easily after birth by cord blood samples. The mother will receive an additional injection following this if the baby is Rh+. This helps to serve subsequent pregnancies. Erythroblastosis Fetalis, Photomicrograph
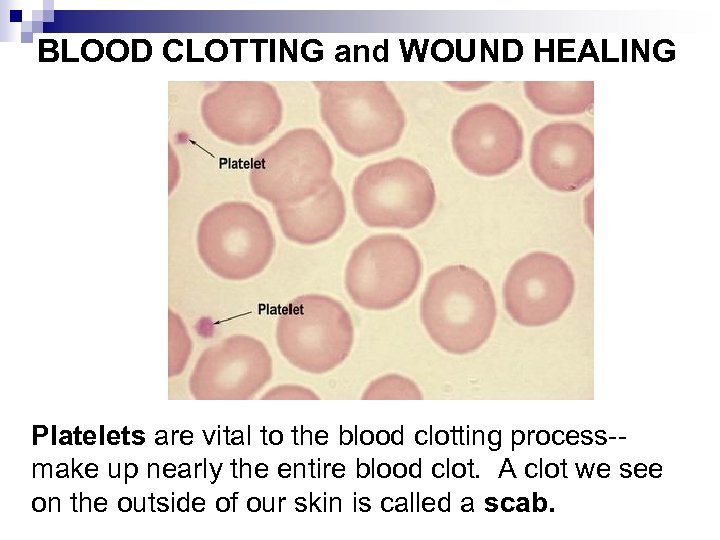 BLOOD CLOTTING and WOUND HEALING Platelets are vital to the blood clotting process-make up nearly the entire blood clot. A clot we see on the outside of our skin is called a scab.
BLOOD CLOTTING and WOUND HEALING Platelets are vital to the blood clotting process-make up nearly the entire blood clot. A clot we see on the outside of our skin is called a scab.
 Clotting: The complex chain of chemical events that produces a plug (clot) at the site of bleeding. n Certain medications may interfere with clotting, such as aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs; anticoagulants (such as Coumadin); vitamin E; and herbal preparations containing garlic or ginkgo biloba. n
Clotting: The complex chain of chemical events that produces a plug (clot) at the site of bleeding. n Certain medications may interfere with clotting, such as aspirin, ibuprofen, and other nonsteroidal anti-inflammatory drugs; anticoagulants (such as Coumadin); vitamin E; and herbal preparations containing garlic or ginkgo biloba. n
 BLOOD / LYMPH DISORDERS A few definitions: n hematocrit – fraction percentage of red blood cells in blood n CBC – complete blood count: red, white and platelets n Hemophilia – a bleeding disorder (many) caused by lack of one or more clotting factors. Treatment includes injection of clotting factors.
BLOOD / LYMPH DISORDERS A few definitions: n hematocrit – fraction percentage of red blood cells in blood n CBC – complete blood count: red, white and platelets n Hemophilia – a bleeding disorder (many) caused by lack of one or more clotting factors. Treatment includes injection of clotting factors.
 From a bruise
From a bruise
 n From an injection in the buttocks
n From an injection in the buttocks
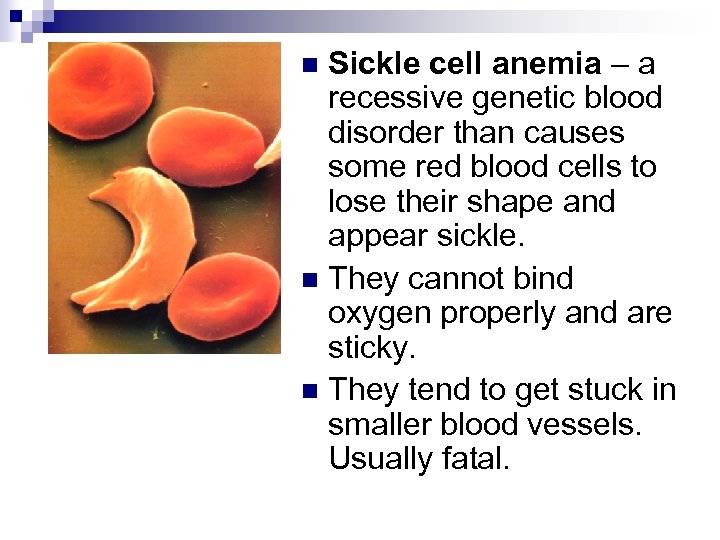 Sickle cell anemia – a recessive genetic blood disorder than causes some red blood cells to lose their shape and appear sickle. n They cannot bind oxygen properly and are sticky. n They tend to get stuck in smaller blood vessels. Usually fatal. n
Sickle cell anemia – a recessive genetic blood disorder than causes some red blood cells to lose their shape and appear sickle. n They cannot bind oxygen properly and are sticky. n They tend to get stuck in smaller blood vessels. Usually fatal. n
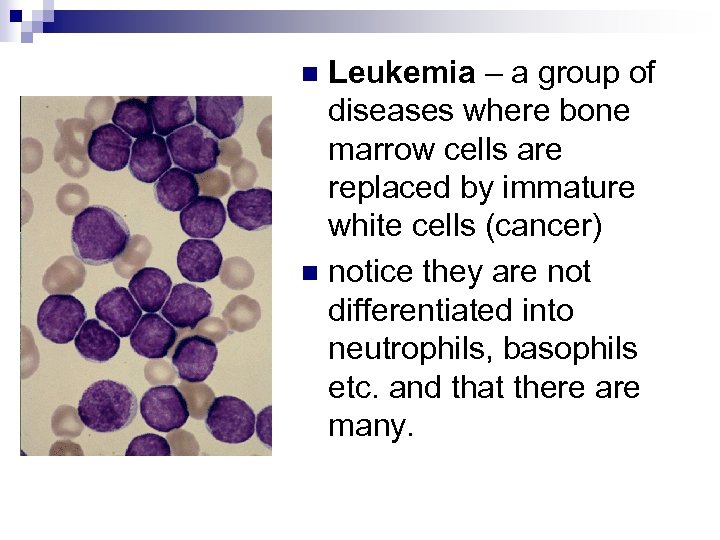 Leukemia – a group of diseases where bone marrow cells are replaced by immature white cells (cancer) n notice they are not differentiated into neutrophils, basophils etc. and that there are many. n
Leukemia – a group of diseases where bone marrow cells are replaced by immature white cells (cancer) n notice they are not differentiated into neutrophils, basophils etc. and that there are many. n
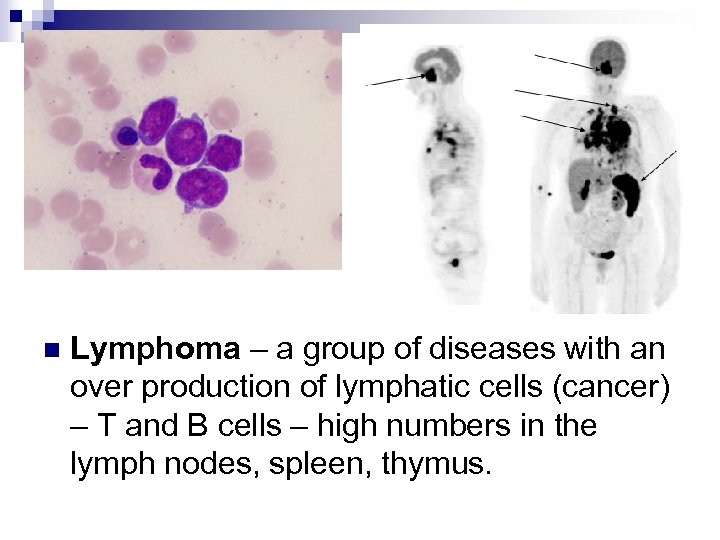 n Lymphoma – a group of diseases with an over production of lymphatic cells (cancer) – T and B cells – high numbers in the lymph nodes, spleen, thymus.
n Lymphoma – a group of diseases with an over production of lymphatic cells (cancer) – T and B cells – high numbers in the lymph nodes, spleen, thymus.
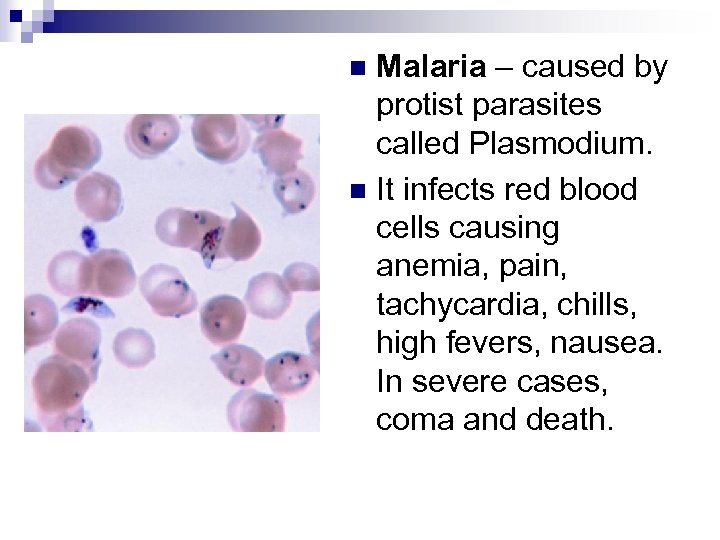 Malaria – caused by protist parasites called Plasmodium. n It infects red blood cells causing anemia, pain, tachycardia, chills, high fevers, nausea. In severe cases, coma and death. n
Malaria – caused by protist parasites called Plasmodium. n It infects red blood cells causing anemia, pain, tachycardia, chills, high fevers, nausea. In severe cases, coma and death. n
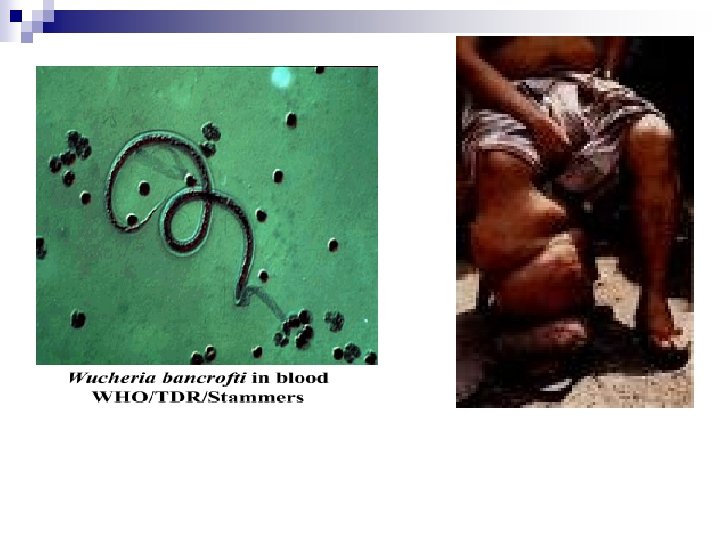
 Lymphatic filariasis (elephant man syndrome) n The thread-like, parasitic filarial worms Wuchereria bancrofti and Brugia malayi that cause lymphatic filariasis live almost exclusively in humans. These worms lodge in the lymphatic system, the network of nodes and vessels that maintain the delicate fluid balance between the tissues and blood and are an essential component for the body's immune defence system. n
Lymphatic filariasis (elephant man syndrome) n The thread-like, parasitic filarial worms Wuchereria bancrofti and Brugia malayi that cause lymphatic filariasis live almost exclusively in humans. These worms lodge in the lymphatic system, the network of nodes and vessels that maintain the delicate fluid balance between the tissues and blood and are an essential component for the body's immune defence system. n