e8e64161d17d55345b8d6192c49d5306.ppt
- Количество слайдов: 70
The Agitated Patient Wild and Crazy Randall Berlin, MD
Learning Objectives Review the toxic causes of agitated delirium. Recognize and treat life threatening complications. Sedation of the agitated patient. Recognize and treat rhabdomyolysis.
Case 1 - Form 10 • Police attended the house of patient X after complaints from the neighbors that he was screaming all night. Neighbors and his live in landlord stated that he had not slept at all and was not making any sense. Pt X followed one of his neighbors home and pushed him on his lawn.
Form 10 (cont’d) • Pt X is currently on medication, however has not been taking his medications. Pt X’s landlord said that he has been selling his valium and filled all his meds - no other meds available to pt X for 3 weeks. Pt X threatened to kill everyone/have them murdered/shot/poisoned. He is a danger to himself and others. • Your thoughts?
• Schizophrenia • Drug withdrawal – Benzodiazepines • Personality Disorder • Illicit Drug Use
In the ED • • Pt yelling and aggressive. Security required to restrain. BP 113/59; P 79; T 37 C; 94% RA Pharmacologic sedation – Versed 5 mg IM – Olanzapine 10 mg IM
Old chart • Schizoaffective • Marijuana and cocaine abuse • Antisocial personality disorder • Dispostion – Admit to psychiatry
Patient 2 30 year old, 100 kg male bodybuilder is brought to the Emergency Department. He was arrested by the police after running naked down the middle of a major road. Two paramedics and four police are having trouble holding him down on the stretcher. Earlier that day the patient had a major motor seizure. What are some causes of agitation?
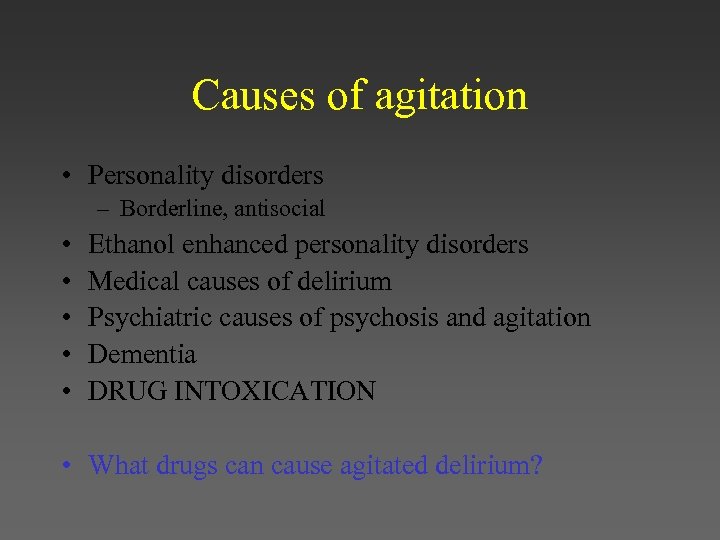
Causes of agitation • Personality disorders – Borderline, antisocial • • • Ethanol enhanced personality disorders Medical causes of delirium Psychiatric causes of psychosis and agitation Dementia DRUG INTOXICATION • What drugs can cause agitated delirium?
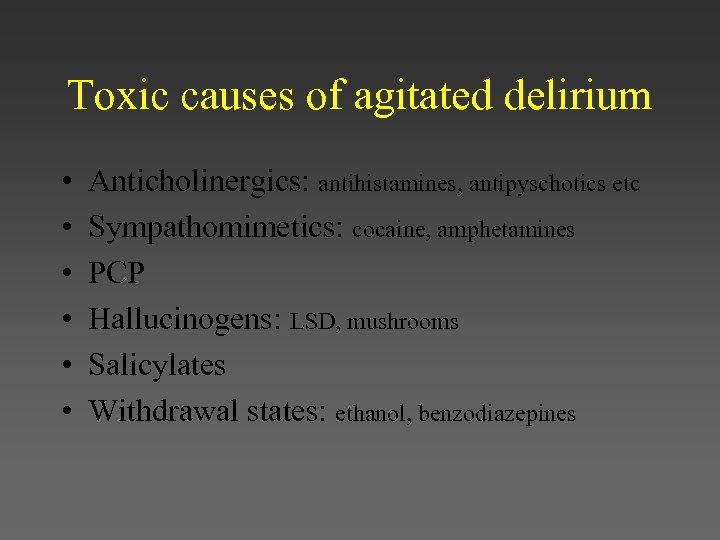
Toxic causes of agitated delirium • • • Anticholinergics: antihistamines, antipyschotics etc Sympathomimetics: cocaine, amphetamines PCP Hallucinogens: LSD, mushrooms Salicylates Withdrawal states: ethanol, benzodiazepines
Back to the Case • P: 140; BP 150/95; RR 24; Sa. O 2 98%; T 39. 5 C • Agitated • Pupils 7 mm, reactive • Diaphoretic • Life threats?
Life threats • Sudden cardiac death • Hyperthermia
Sudden cardiac death Typical scenario • 29 yo male pulled over by police for driving erratically. He was agitated and confused and resisted arrest. He was pepper sprayed and continued to resist. He was physically subdued and continued to struggle despite being placed in 4 -point restraints on the ambulance stretcher and suddenly stopped moving.
Typical scenario (cont’d) • As he was being loaded into the ambulance, he was found to be pulseless and apneic. His passenger reported that he had been sniffing cocaine just prior to being stopped.
Sudden Cardiac Death Associated with Agitated Delirium • “Sudden In-Custody Death” • “Restraint Associated Cardiac Arrest”
Sudden Cardiac Death Similarities with most cases • Presence of excited delirium • Continued maximal struggle despite attempts at maximal restraint • Clear association exists between illicit drug use and the syndrome but not universal. • Non-drug related causes are almost always psychotic (schizophrenia, bipolar)
Sudden Cardiac Death Mechanism of Death • No definite etiology usually found at autopsy • Profound metabolic acidosis likely leading to cardiac arrest • Hyperthermia often contributory • Convulsions often contributory • Hyperkalemia often contributory • Restraint asphyxia unlikely explanation
Sudden Cardiac Death Summary • Dr. Chris Linden: – “I constantly and emphatically remind our residents and fellows that the patient with agitated delirium, particularly one who is actively and persistently struggling against restraint, should be treated as a true emergency - a cardiac arrest waiting to happen. ”
Back to the Case • P: 140; BP 150/95; RR 24; Sa. O 2 98%; T 39. 5 C • Agitated • Pupils 7 mm, reactive • Diaphoretic • Life threats?
Life threats • Sudden cardiac death • Hyperthermia
Recognize the life threat! (not the drug) How important is hyperthermia?
Hyperthermia • 75% of drug overdose patients with a temperature greater than 40. 5 C for greater than one hour die or have permanent neurologic sequelae

Back to the case • Wildly agitated Movie Trivia: “If you cut their tendons, even the largest elephant will fall. ”
Movie Trivia • The Protector (2006) • Tony Jaa How can we control our wildly, agitated patient?
Control of the patient • Physical restraints • Chemical sedation • Intubation and paralysis
Code Black • Standardized approach • Standardized team
Physical restraints • Short term solution to gain IV access and treat with pharmaceutical agents • 5 or more people • Monitoring protocol • Documentation
Chemical sedation • Control psychomotor agitation while minimizing drug related complications • Identify and treat life threats What drugs can we use?
• Benzodiazepines – Lorazepam – Diazepam – Midazolam • Antipsychotics • Paralytics – Succinylcholine – Rocuronium
Benzodiazepines • Advantages – Treats hyperthermia – Prevents or treats seizures – Decreases mortality in animal studies of cocaine intoxication

Benzodiazepines • Disadvantages – Respiratory depression
Midazolam • Onset: IV - 1 -5 minutes • Dose: 2. 5 -5. 0 mg IV/IM q 3 -5 min • Elderly: reduce dose
Midazolam Boxed Warning • May cause severe resp depression, resp. arrest or apnea • Initial doses in the elderly or debilitated should be conservative • Parental form contains benzyl alcohol; avoid rapid injection in neonates or prolonged infusions
Antipsychotics • Advantages – No respiratory depression
Antipsychotics • Disadvantages – Anticholinergic side effects • Impair heat dissipation – – Lower the seizure threshold Prolong the QT interval Dystonic reactions Increased mortality in animal studies of cocaine intoxication
Haloperidol • • Peak: 10 -20 minutes Duration: days Dose: 2 -5 mg IV/IM q 20 min Elderly: reduce dose
Haloperidol Boxed Warning • None • However, DROPERIDOL – Cases of QT prolongation and torsades de pointes, including some fatal cases, have been reported
Olanzapine • • Peak: 15 -45 minutes Duration: days Dose: 5 -10 mg IM/SL q 2 -4 h Elderly: Reduced doses
Olanzapine Boxed Warning • Increased risk of death in pts with dementia related behavioral disorders • Increased risk of CVAs in elderly pts with dementia related psychosis
Intubation and Paralysis • Ultimate control • Consider in patients with – Risk of C-spine injury – Hyperthermia
Succinylcholine • In most cases it will be safe • Hyperkalemia is a risk in the patient with a protracted and fulminant course
Hyperthermia
Treatment of Hyperthermia • Mist and fan • Ice packs to groin and axilla
Back to the Case • P: 140; BP 150/95; RR 24; Sa. O 2 98%; T 39. 5 C • Agitated • Pupils 7 mm, reactive • Diaphoretic • What toxidrome is this?
Sympathomimetic Toxidrome • • Hyperdynamic vitals Agitated mental status Dilated pupils Diaphoresis
What are the causes of death in cocaine intoxication?
Cocaine related deaths • • • Seizures CVA MI Aortic dissection Dysrhythmias HYPERTHERMIA How does cocaine cause hyperthermia?
How does cocaine cause hyperthermia? • Psychomotor agitation --> increased heat production • Vasoconstriction-->decreased heat dissipation • A direct central effect • A metabolic effect
Back to the Case • The patient is physically restrained, an IV is started and midazolam is titrated. • Thirty minutes later, 30 mg of midazolam has been given, the patient is still agitated and his temp is 40 C • A RSI is done and the patient is paralyzed.
My approach • Midazolam 2. 5 - 5. 0 mg IV q 3 -5 min • Endpoints – Control of patient – Control of hyperthermia • Ativan 2 mg IV
That should be the worst of it • Review differential diagnosis • Look for complications
History • Collateral history from police, paramedics, friends or family – Medical and psych history, alcohol and drug usage, medications • Previous medical records
Physical • Toxidromes • Signs of infection – Meningismus, cellulitis, pneumonia, etc • Trauma • Thyroid disease
Labs • CBC, electrolytes, renal function, CK, EKG, urine dip • When indicated – LFTs, Ca, Mg, Phos, TSH, T 4, – CXR, – LP, – head CT
Back to the case • A Foley catheter is inserted and tea colored urine comes out. • How do we explain this finding.
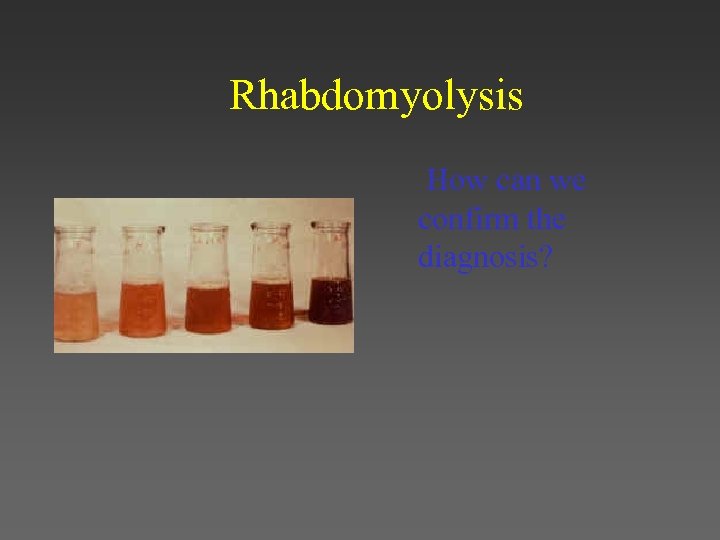
Rhabdomyolysis How can we confirm the diagnosis?
Rhabdomyolysis • Urine – Urine dipstick – Urine for myoglobin Treatment? • Blood – Myoglobin – Creatine Kinase
Rhabdomyolysis • Treatment – Hydration and electrolyte management – ? Alkalinization – ? Mannitol
Rhabdomyolysis • Hydration – Goal: urine output: 1 -2 cc/kg/hr • Alkalinization – – – Implement when CK greater than 5000 1 amp bicarb IV push 1 L of D 5 W (remove 150 cc) and add 3 amps of bicarb Run at 100 -150 cc/hr Goal: urine p. H > 6 • Monitor serial CK – If still rising look for a compartment syndrome
Re-assessments • Drain the bladder • Look and treat for causes of pain • Re-assess need for restraints and document progress
Summary of Approach • • Control Life threats Differential Diagnosis Complications
Summary of Drug Therapy • • • Drug induced: benzodiazepines Drug withdrawal: benzodiazepines Psychiatric: antipsychotic Dementia: antipsychotic Unknown: benzodiazepines

Tox Trivia Name the Movie • Tagline for this 1994 movie – Girls like me don't make invitations like this to just anyone! • Directed by Quentin Tarratino • Starred John Travolta, Uma Thurman, Samuel L. Jackson • The stories of two mob hit men, a boxer and a pair of diner bandits intertwine in four tales of violence and redemption.
Uma Thurman overdoses on what drug and how do they revive her?
Heroin Adrenaline
e8e64161d17d55345b8d6192c49d5306.ppt