ff987a2714f127b5783d2d6486195a0b.ppt
- Количество слайдов: 27
 The Advance and Emergency Care Pathway for Children and Young People with Life-limiting or Lifethreatening illness C&V UHB Child Health Advance and Emergency Care Pathway Focus Group
The Advance and Emergency Care Pathway for Children and Young People with Life-limiting or Lifethreatening illness C&V UHB Child Health Advance and Emergency Care Pathway Focus Group
 Overview • What is an AECP? • When to introduce an AECP • Ethical & legal frameworks for practice • The AECP process • The AECP form
Overview • What is an AECP? • When to introduce an AECP • Ethical & legal frameworks for practice • The AECP process • The AECP form
 The AECP • Is an expression of wishes • Is not the same as a DNAR directive • Aims to facilitate open and effective communication within the multiagency team and between the team and the patient/family
The AECP • Is an expression of wishes • Is not the same as a DNAR directive • Aims to facilitate open and effective communication within the multiagency team and between the team and the patient/family
 AECP- A framework of care • Multi Agency • Travels with the child • Seamless communication • Decisions should be made within a trusting relationship and an ethos of shared decision-making* • Professionals should be led by the needs of the patient/family • takes place over a number of weeks, months or years • Advance care planning may evolve over time* *Brook et al. A Plan for Living and a Plan for Dying: Advance Care Planning for Children. Arch Dis Child 2008; 93(suppl): A 61 -66
AECP- A framework of care • Multi Agency • Travels with the child • Seamless communication • Decisions should be made within a trusting relationship and an ethos of shared decision-making* • Professionals should be led by the needs of the patient/family • takes place over a number of weeks, months or years • Advance care planning may evolve over time* *Brook et al. A Plan for Living and a Plan for Dying: Advance Care Planning for Children. Arch Dis Child 2008; 93(suppl): A 61 -66
 AECP- transparent procedure • For children/young people who die at home the AECP aims to: – Ensure that families understand the multiagency response to death – Ensure that agencies are appropriately informed to prevent additional distress to families
AECP- transparent procedure • For children/young people who die at home the AECP aims to: – Ensure that families understand the multiagency response to death – Ensure that agencies are appropriately informed to prevent additional distress to families
 Advance Decisions in Adults • Advance decisions concern the refusal of treatment • Can be made only by mentally capable people aged 18 and over • Can be oral or written (unless relating to life-saving treatment, in which case they must be in writing and meet further criteria) • Must specify the treatment being refused • Healthcare professionals are bound by advance decisions to refuse treatment • So an AECP cannot be an advance decision, unless it meets these basic criteria.
Advance Decisions in Adults • Advance decisions concern the refusal of treatment • Can be made only by mentally capable people aged 18 and over • Can be oral or written (unless relating to life-saving treatment, in which case they must be in writing and meet further criteria) • Must specify the treatment being refused • Healthcare professionals are bound by advance decisions to refuse treatment • So an AECP cannot be an advance decision, unless it meets these basic criteria.
 When to create an AECP? Would you be surprised if this child died prematurely due • to Predicting illness? life is challenging* a life-limiting end of Would you be surprised if this child died within a year? • Families benefit from the opportunity to Would you be surprised if this child died during this make informed decisions about the care of episode of care? their child* Do you know what the patient’s and family’s wishes are for end of life care? If the answer to any of these questions is ‘NO’ it may be worth considering the value of pediatric terminal **Vickers JL, Carlisle C. Choices and control: parental experiences in an AECP home care. J Pediatr Oncol Nurs 2000; 17: 12 -21 *Brook L, Hain R. Predicting death in children. Arch Dis Child 2008; 93: 1067 -70
When to create an AECP? Would you be surprised if this child died prematurely due • to Predicting illness? life is challenging* a life-limiting end of Would you be surprised if this child died within a year? • Families benefit from the opportunity to Would you be surprised if this child died during this make informed decisions about the care of episode of care? their child* Do you know what the patient’s and family’s wishes are for end of life care? If the answer to any of these questions is ‘NO’ it may be worth considering the value of pediatric terminal **Vickers JL, Carlisle C. Choices and control: parental experiences in an AECP home care. J Pediatr Oncol Nurs 2000; 17: 12 -21 *Brook L, Hain R. Predicting death in children. Arch Dis Child 2008; 93: 1067 -70
 When to create an AECP? • Child/YP receiving end of life care • Child/YP’s condition is such that death may occur at any point (reasonable risk of life threatening event) • ‘PICU/HDU route into AECP’ triggered during a recent PICU/HDU admission • Professionals, child/YP or family identifying a deterioration in the patient • Knowledge of the natural history of the child/YP’s condition suggests that he/she may be approaching the terminal phase
When to create an AECP? • Child/YP receiving end of life care • Child/YP’s condition is such that death may occur at any point (reasonable risk of life threatening event) • ‘PICU/HDU route into AECP’ triggered during a recent PICU/HDU admission • Professionals, child/YP or family identifying a deterioration in the patient • Knowledge of the natural history of the child/YP’s condition suggests that he/she may be approaching the terminal phase
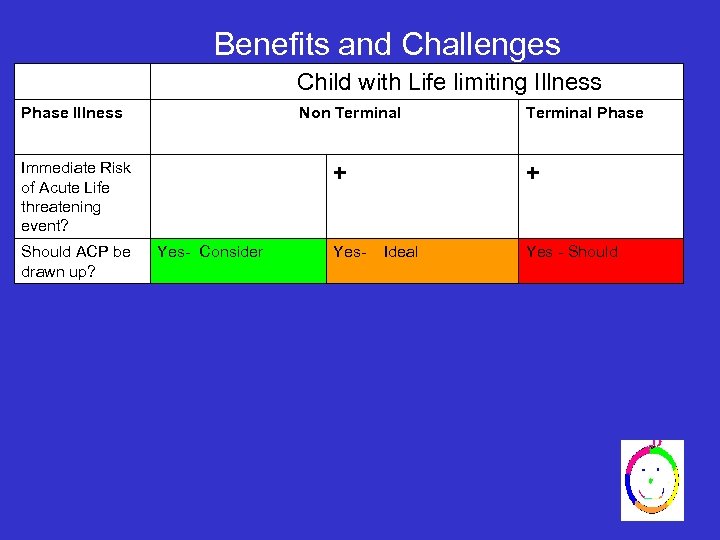 Benefits and Challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should
Benefits and Challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should
 Benefits and Challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? Focus + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should • Comfort and support • Symptom Control Purpose • Inform • Advocate Comfort and Support Challenges • Recognition of End of life phase. • Uncertainty
Benefits and Challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? Focus + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should • Comfort and support • Symptom Control Purpose • Inform • Advocate Comfort and Support Challenges • Recognition of End of life phase. • Uncertainty
 Benefits and challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should • Plan life sustaining treatment (Modify Risk factors) • Symptom Control • likely request for invasive ventilation • Comfort and support Purpose • Inform • Advocate for active measures • Potential considerations for invasive ventilation • Inform • Advocate Comfort and Support Challenges • Conveying Not without hope /not on slippery slope yet but uncertainty of illness trajectory and ALTE makes ACP reasonable • Parents may not want ACP • Recognition of End of life phase. • Uncertainty Focus • Symptom Control
Benefits and challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? Should ACP be drawn up? + Yes- Consider Yes- Terminal Phase + Ideal Yes - Should • Plan life sustaining treatment (Modify Risk factors) • Symptom Control • likely request for invasive ventilation • Comfort and support Purpose • Inform • Advocate for active measures • Potential considerations for invasive ventilation • Inform • Advocate Comfort and Support Challenges • Conveying Not without hope /not on slippery slope yet but uncertainty of illness trajectory and ALTE makes ACP reasonable • Parents may not want ACP • Recognition of End of life phase. • Uncertainty Focus • Symptom Control
 Benefits and challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? + Terminal Phase + Should ACP be drawn up? Yes- Consider Yes- Ideal Yes - Should Focus • Plan life sustaining treatment (Modify Risk factors) • Symptom Control • likely request for invasive ventilation • Comfort and support Purpose • Inform • Advocate for active measures • Potential considerations for invasive ventilation • Inform • Advocate Comfort and Support Challenges • Disclosure of life limiting illness • Discuss uncertainty illness trajectory • Conveying Not without hope /not on slippery slope yet but uncertainty of illness trajectory and ALTE makes ACP reasonable • Parents may not want ACP • Recognition of End of life phase. • Uncertainty • Symptom Control
Benefits and challenges Child with Life limiting Illness Phase Illness Non Terminal Immediate Risk of Acute Life threatening event? + Terminal Phase + Should ACP be drawn up? Yes- Consider Yes- Ideal Yes - Should Focus • Plan life sustaining treatment (Modify Risk factors) • Symptom Control • likely request for invasive ventilation • Comfort and support Purpose • Inform • Advocate for active measures • Potential considerations for invasive ventilation • Inform • Advocate Comfort and Support Challenges • Disclosure of life limiting illness • Discuss uncertainty illness trajectory • Conveying Not without hope /not on slippery slope yet but uncertainty of illness trajectory and ALTE makes ACP reasonable • Parents may not want ACP • Recognition of End of life phase. • Uncertainty • Symptom Control
 Ethical & legal frameworks - Data Protection Act 1998 -Mental Capacity Act 2005, -Equalities Act 2010 -Good practice in consent implementation guide WAG 2008
Ethical & legal frameworks - Data Protection Act 1998 -Mental Capacity Act 2005, -Equalities Act 2010 -Good practice in consent implementation guide WAG 2008
 Who do you need to discuss and agree the AECP with? • AECP is not a consent form, but you need to be clear who is the client! • For example, no point agreeing an AECP with parents, if it’s the child/young person’s consent you need when implementing the AECP, by providing treatment, etc
Who do you need to discuss and agree the AECP with? • AECP is not a consent form, but you need to be clear who is the client! • For example, no point agreeing an AECP with parents, if it’s the child/young person’s consent you need when implementing the AECP, by providing treatment, etc
 from whom must consent be obtained? Capacity to consent – Understand, – retain, – weigh & use information
from whom must consent be obtained? Capacity to consent – Understand, – retain, – weigh & use information
 is it…? – At 16 -17 years a young person is presumed to have the capacity to consent( MCA 2005) – for a 16/17 year old with impaired capacity? A best interests decision (MCA 2005) must be followed – Under 16 yrs a young person may have the capacity to consent if they are Gillick/ Frazer Competent – A person with parental responsibility , if <16 and not Gillick competent – Or is there a court decision or is one needed?
is it…? – At 16 -17 years a young person is presumed to have the capacity to consent( MCA 2005) – for a 16/17 year old with impaired capacity? A best interests decision (MCA 2005) must be followed – Under 16 yrs a young person may have the capacity to consent if they are Gillick/ Frazer Competent – A person with parental responsibility , if <16 and not Gillick competent – Or is there a court decision or is one needed?
 Sharing the AECP • It is essential that you obtain and record consent from the appropriate person, before you share the AECP with other people, agencies! • Do not rely on parental consent for this if the child is competent • If a 16/17 year old lacks capacity to consent to this, sharing AECP must be a best interests decision (MCA 2005)
Sharing the AECP • It is essential that you obtain and record consent from the appropriate person, before you share the AECP with other people, agencies! • Do not rely on parental consent for this if the child is competent • If a 16/17 year old lacks capacity to consent to this, sharing AECP must be a best interests decision (MCA 2005)
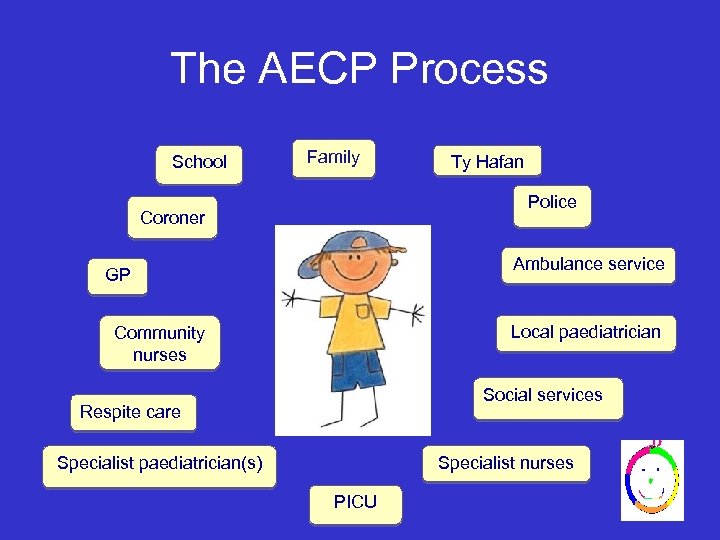 The AECP Process School Family Ty Hafan Police Coroner Ambulance service GP Local paediatrician Community nurses Social services Respite care Specialist nurses Specialist paediatrician(s) PICU
The AECP Process School Family Ty Hafan Police Coroner Ambulance service GP Local paediatrician Community nurses Social services Respite care Specialist nurses Specialist paediatrician(s) PICU
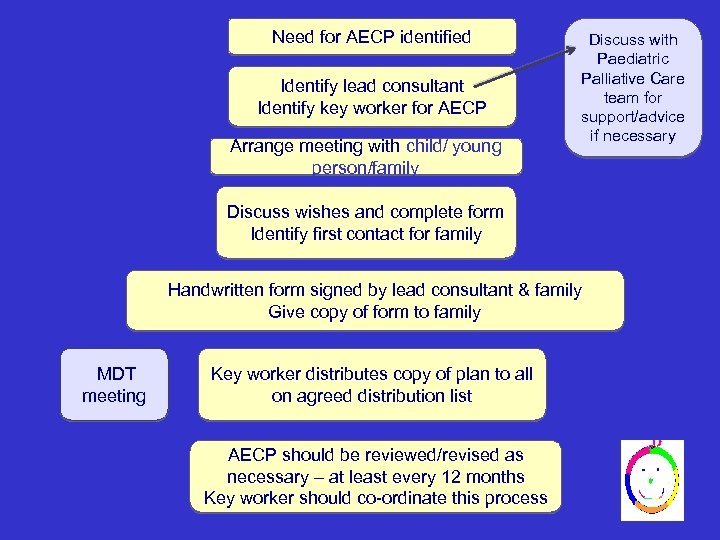 Need for AECP identified Identify lead consultant Identify key worker for AECP Arrange meeting with child/ young person/family Discuss with Paediatric Palliative Care team for support/advice if necessary Discuss wishes and complete form Identify first contact for family Handwritten form signed by lead consultant & family Give copy of form to family MDT meeting Key worker distributes copy of plan to all on agreed distribution list AECP should be reviewed/revised as necessary – at least every 12 months Key worker should co-ordinate this process
Need for AECP identified Identify lead consultant Identify key worker for AECP Arrange meeting with child/ young person/family Discuss with Paediatric Palliative Care team for support/advice if necessary Discuss wishes and complete form Identify first contact for family Handwritten form signed by lead consultant & family Give copy of form to family MDT meeting Key worker distributes copy of plan to all on agreed distribution list AECP should be reviewed/revised as necessary – at least every 12 months Key worker should co-ordinate this process
 Child dies at home Parents call agreed 1 st contact Worker will offer telephone support or go to home depending on family’s preferences IF AT ANY STAGE ANY PROFESSIONAL HAS CONCERNS THAT THE CHILD’S DEATH MAY Worker phones GP, if available, to certify death If GP unavailable OOH doctor contacted to OR NOT HAVE OCCURRED NATURALLYverify AS death and GP requested to complete death certificate ASAP EXPECTED THE POLICE MUST BE INFORMED IMMEDIATELY Next working day: 1 st contact to inform Detective Inspector in local Public Protection Unit of child’s death then hands over if appropriate to key worker. Team to assist family with their wishes for saying goodbye to the child and funeral arrangements. Key worker to inform all agencies and holders of the plan.
Child dies at home Parents call agreed 1 st contact Worker will offer telephone support or go to home depending on family’s preferences IF AT ANY STAGE ANY PROFESSIONAL HAS CONCERNS THAT THE CHILD’S DEATH MAY Worker phones GP, if available, to certify death If GP unavailable OOH doctor contacted to OR NOT HAVE OCCURRED NATURALLYverify AS death and GP requested to complete death certificate ASAP EXPECTED THE POLICE MUST BE INFORMED IMMEDIATELY Next working day: 1 st contact to inform Detective Inspector in local Public Protection Unit of child’s death then hands over if appropriate to key worker. Team to assist family with their wishes for saying goodbye to the child and funeral arrangements. Key worker to inform all agencies and holders of the plan.
 The AECP form • 12 pages long • Contact details – Family – Professionals • Treatment plans – Acute deterioration – Slow deterioration – Symptom care • Clarity of documented wishes • Consent to information sharing
The AECP form • 12 pages long • Contact details – Family – Professionals • Treatment plans – Acute deterioration – Slow deterioration – Symptom care • Clarity of documented wishes • Consent to information sharing
 Completing the form • Ensure form is dated (first completion, amendment & planned review) • Current form should be filed at the front of the child’s medical case-notes • Non-current forms should not be destroyed • Send completed audit form to Dr Sian Moynihan, St David’s Children’s Centre
Completing the form • Ensure form is dated (first completion, amendment & planned review) • Current form should be filed at the front of the child’s medical case-notes • Non-current forms should not be destroyed • Send completed audit form to Dr Sian Moynihan, St David’s Children’s Centre
 Supporting documentation • To be found on the clinical portal: – Background information – Guidance on the process and form-completion – Information sheet for families and for patient – Example covering letter to professionals – Additional guidance: • Actions to take when a child dies • Involving the Coroner, Police & Ambulance – Audit form
Supporting documentation • To be found on the clinical portal: – Background information – Guidance on the process and form-completion – Information sheet for families and for patient – Example covering letter to professionals – Additional guidance: • Actions to take when a child dies • Involving the Coroner, Police & Ambulance – Audit form
 Conclusions • AECPs should replace DNAR orders • AECPs support and evidence discussions taking place in different settings • AECPs are transportable, visible and consistent • AECPs facilitate multiagency support from point of diagnosis through to death and into bereavement
Conclusions • AECPs should replace DNAR orders • AECPs support and evidence discussions taking place in different settings • AECPs are transportable, visible and consistent • AECPs facilitate multiagency support from point of diagnosis through to death and into bereavement
 One last thing • The document cannot predict all eventualities • A valid document will contribute information to decision making • The responsibility of interpreting a AECP lies with most senior available professional at time of treatment • Professional judgement must be used when interpreting the document • If under the AECP, the child/young person needs treatment, ENSURE you obtain consent from the right person!
One last thing • The document cannot predict all eventualities • A valid document will contribute information to decision making • The responsibility of interpreting a AECP lies with most senior available professional at time of treatment • Professional judgement must be used when interpreting the document • If under the AECP, the child/young person needs treatment, ENSURE you obtain consent from the right person!
 For support/advice please contact: • • • Dr Richard Hain, Consultant in Paediatric Palliative Medicine, UHW Dr Sian Moynihan, Consultant Community Paediatrician, Dr Michelle Jardine PICU Consultant Dr Jennifer Evans Consultant Paediatrician Dr Joan Bongili Associate Specialist/ Dr Cath Norton Consultant, CD Dr Victoria Lidstone Consultant Adult and transition Palliative Care Julia Barrell Mental Capacity Act Manager SNHV, Special School nurse leads Ty Hafan Cath Thompson Assistant Director of Care Police DCI Richard Jones Ambulance Andrew Jenkins Consultant Paramedic
For support/advice please contact: • • • Dr Richard Hain, Consultant in Paediatric Palliative Medicine, UHW Dr Sian Moynihan, Consultant Community Paediatrician, Dr Michelle Jardine PICU Consultant Dr Jennifer Evans Consultant Paediatrician Dr Joan Bongili Associate Specialist/ Dr Cath Norton Consultant, CD Dr Victoria Lidstone Consultant Adult and transition Palliative Care Julia Barrell Mental Capacity Act Manager SNHV, Special School nurse leads Ty Hafan Cath Thompson Assistant Director of Care Police DCI Richard Jones Ambulance Andrew Jenkins Consultant Paramedic
 Acknowledgements • • • • • • Dr Charlotte Mellor, Sp. R Palliative Care , Bristol Dr Sian Moynihan, Lead Consultant Community Paediatrician Dr Michelle Jardine, Consultant Paediatric Intensive Care Dr Cath Norton, Consultant Community Paedaitrician Dr Helen Fardy, Consultant Paediatric Intensive Care Dr Louise Hartley, Consultant Paediatric Neurologist Dr Richard Hain, Consultant Paediatric Palliative Medicine Dr Graham Shortland, Consultant Paediatrician Cath Thompson, Assistant Director of Care, Ty Hafan Children’s Hospice Mrs Hilary Valle, Parent representative Liz Pendleton, Lead Nurse, Children’s Community Nursing, Cardiff Carys Davies, Special Needs Health Visitor Wendy Herbert, Lead Health Visitor Dr Rhodri Lewis, General Practitioner Chris Horrocks, Team Manager, Child Health and Disability Team, Cardiff Janet Stroud, Assistant Team Manager, Child Health and Disability Team, The Vale of Glamorgan Ms ME Hassell, HM Coroner for Cardiff and The Vale of Glamorgan Rhiannon Beaumont-Wood, Welsh Ambulance Services NHS Trust Diane Rogers, Lead for Paediatric Physiotherapy, UHW Sue King, Parent Counseling Service, UHW Nuala Mahon, Lead Nurse for School Health DCI Richard Jones, Major Crime Investigation Unit Dr Jo Griffiths, Consultant Community Child Health, ABMU Neath/Port Talbot Children’s Safeguarding Management Board
Acknowledgements • • • • • • Dr Charlotte Mellor, Sp. R Palliative Care , Bristol Dr Sian Moynihan, Lead Consultant Community Paediatrician Dr Michelle Jardine, Consultant Paediatric Intensive Care Dr Cath Norton, Consultant Community Paedaitrician Dr Helen Fardy, Consultant Paediatric Intensive Care Dr Louise Hartley, Consultant Paediatric Neurologist Dr Richard Hain, Consultant Paediatric Palliative Medicine Dr Graham Shortland, Consultant Paediatrician Cath Thompson, Assistant Director of Care, Ty Hafan Children’s Hospice Mrs Hilary Valle, Parent representative Liz Pendleton, Lead Nurse, Children’s Community Nursing, Cardiff Carys Davies, Special Needs Health Visitor Wendy Herbert, Lead Health Visitor Dr Rhodri Lewis, General Practitioner Chris Horrocks, Team Manager, Child Health and Disability Team, Cardiff Janet Stroud, Assistant Team Manager, Child Health and Disability Team, The Vale of Glamorgan Ms ME Hassell, HM Coroner for Cardiff and The Vale of Glamorgan Rhiannon Beaumont-Wood, Welsh Ambulance Services NHS Trust Diane Rogers, Lead for Paediatric Physiotherapy, UHW Sue King, Parent Counseling Service, UHW Nuala Mahon, Lead Nurse for School Health DCI Richard Jones, Major Crime Investigation Unit Dr Jo Griffiths, Consultant Community Child Health, ABMU Neath/Port Talbot Children’s Safeguarding Management Board


