c16066a48efd6d4328a940e2b6cb0aeb.ppt
- Количество слайдов: 87

The 5 Best Trials from 2011 that may Impact my Practice CRT 2012 Washington, DC February 2012 David R. Holmes, MD Mayo Clinic Rochester, MN

David R. Holmes, MD I have no real or apparent conflicts of interest to report.

So much data, so little time…


TAVR

Clinical Documents in Development • Societal Overview of TVT by ACCF and STS (July 2011) • ACCF, STS, AATS, SCAI led expert consensus document on pre- and post-procedural issues, including patient selection (Jan 2012) • SCAI, AATS, ACCF, STS led competence statement addressing institutional and operator requirements (First Quarter 2012) • ACCF led update guideline on Valvular Heart Disease (TBD) All multi-societal efforts involving physician stakeholders

Consensus Recommendations ACC and STS • Focus TAVR Programs • Specialized Heart Centers • Multidisciplinary teams • Expert surgeons and interventionalists and • imagers • Expertise with high risk and structural heart disease patients • Ancillary personnel • Optimal facilities Protocol development • Patient selection • Procedural details • Complication management

Consensus Recommendations ACC and STS • TAVR Programs • Participate in TVT Registry • Track appropriate use • Patient selection • Outcomes – risk benefit ratio • Development of post procedural protocols • Development of communication strategies


• 2007: STS Quality Measurement Task Force developed a multidimensional composite quality measure for isolated CABG – 11 process and outcome measures in 4 quality domains • 2010 -11: In collaboration with Consumers Union, STS published isolated CABG composite’s cores. Public Reporting Initiative • Rating system: • Below average • Above average Shahian DM et al: Ann Thorac Surg 92: S 12 -S 23, 2011

Other Performance Metrics • Safety – fewer adverse hospital events and medical errors • Timeliness – reduced waiting time • Equity – reduce racial and ethnic disparities • Effectiveness – treatment results are superior to alternatives, including no treatment • Efficiency – minimize waste, maximize quality/ cost ratio • Patient-centricity – respect patient preferences and goals Shahian DM et al: Ann Thorac Surg 92: S 12 -S 23, 2011

ACC Website(s) Consumer Reports Hospital/Compare USNWR


Moderate Bleeding Depends on whether you are the one bleeding or not

Cumulative hazard rates Major Bleeding Warfarin Dabigatran 150 Dabigatran 110 Follow-up (yr) No. at risk 6, 015 6, 076 6, 022 5, 835 5, 839 5, 801 5, 640 5, 638 5, 600 4, 510 4, 557 4, 474 2, 872 2, 928 2, 797 1, 349 1, 366 1, 269 3016128 -30

Major Bleeding ISTH Definition Warfarin Event (%) 31% RRR Apixaban 327 patients, 2. 13% per year Warfarin 462 patients, 3. 09% per year HR 0. 69 (95% CI, 0. 60 -0. 80); P<0. 001 No. at risk Apixaban Warfarin Month 9088 9052 8103 7910 7564 7335 5365 5196 3048 2956 1515 1491 3140487 -31

Medication Safety Alert Dabigatran January 12, 2012 • Launched in 2010 • First quarter 2011 • 932 serious adverse events reported • 120 deaths • 25 permanent disability • 543 repeat hospitalization • 505/932 involved hemorrhage • 120 of which indicted hemorrhagic stroke+ + Warfarin ranked second – 176 episodes of hemorrhage

Disappearing LAA Thrombus Resulting in Stroke Parekh A, Ezekowitz M et al: Circ 114: e 513, 2006

Left Atrial Function • Single-center study of 150 patients undergoing Maze procedure using radiofrequency and cryo-ablation for AF • Sustained Sinus rhythm during follow-up • Goal: assess LA mechanical contraction post-op and determine if it imposes increased risk of stroke • Endpoint: ischemic stroke felt secondary to T/E event Buber J, J Am Coll Cardiol 58: 1614 -21, 2011

Left Atrial Function 3 Months 1 Year Absent LAMC 31% 69% Present LAMC Buber J, J Am Coll Cardiol 58: 1614 -21, 2011

Left Atrial Function Buber J, J Am Coll Cardiol 58: 1614 -21, 2011 Survival Free of Stroke by LAMC


Intent-to-Treat: All Stroke Cohort WATCHMAN Control Rate (95% CI) Rel risk (95% CI) Posterior probabilities* Noninferiority Superiority 600 pt-yr 3. 4 (1. 9 -5. 5) 3. 6 (1. 5 -6. 3) 0. 96 (0. 43 -2. 57) 0. 927 0. 488 900 pt-yr 2. 6 (1. 5 -4. 1) 3. 5 (1. 7 -5. 7) 0. 74 (0. 36 -1. 76) 0. 998 0. 731 1, 065 pt-yr 2. 3 (1. 3 -2. 6) 3. 2 (1. 6 -5. 2) 0. 71 (0. 35 -1. 64) 0. 993 0. 769 1, 350 pt-yr 2. 1 (1. 3 -3. 3) 2. 7 (1. 4 -4. 3) 0. 78 (0. 41 -1. 75) 0. 989 0. 685 1, 500 pt-yr 2. 0 (1. 3 -3. 1) 2. 7 (1. 5 -4. 1) 0. 77 (0. 42 -1. 62) 0. 995 0. 728 • 23% lower relative risk in WATCHMAN group *No adjustment made for multiple comparisons

LAA Occlusion What Do We Know? • There is a strong relationship between atrial fibrillation, increasing age, increasing stroke • In patients with atrial non-valvular atrial fibrillation, embolus arises in LAA • Even with new drugs, bleeding remains an issue and increases with time • Satisfactory closure of LAA is noninferior to chronic anticoagulation in preventing stroke

CABG PCI

MACCE to 4 Years by SYNTAX Score Tercile Low Scores (0 -22) CABG (N=275) TAXUS (N=299) CABG Cumulative Event Rate (%) 25 0. 77 4. 0% 1. 4% 0. 059 4. 2% 6. 6% 0. 25 Death, CVA or MI 14. 6% 14. 4% 0. 87 Revasc 28. 6% 26. 1% 8. 3% MI P=0. 57 8. 9% CVA 50 P Death Overall PCI 13. 6% 20. 0% 0. 04 0 0 12 24 36 Months Since Allocation 48 Cumulative KM Event Rate ± 1. 5 SE; log-rank P value Site-reported Data; ITT population

MACCE to 4 Years by SYNTAX Score Tercile Intermediate Scores (23 -32) CABG (N=300) TAXUS (N=310) PCI P Death 9. 3% 11. 1% 0. 49 CVA 3. 6% 2. 0% 0. 25 MI 3. 6% 9. 0% 0. 009 Death, CVA or MI 14. 9% 17. 3% 0. 44 Revasc 10. 9% 20. 7% 0. 002 Overall 50 Cumulative Event Rate (%) CABG P=0. 006 32. 0% 25 21. 5% 0 0 12 24 36 Months Since Allocation 48 Cumulative KM Event Rate ± 1. 5 SE; log-rank P value Site-reported Data; ITT population

MACCE to 4 Years by SYNTAX Score Tercile High Scores ( 33) CABG (N=315) TAXUS (N=290) CABG Cumulative Event Rate (%) P<0. 001 40. 1% 25 23. 6% Death 8. 4% 16. 1% 0. 004 CVA 3. 7% 3. 5% 0. 80 3. 9% 9. 3% 0. 01 Death, CVA or MI 14. 6% 22. 7% 0. 01 Revasc 50 P MI Overall PCI 11. 4% 28. 8% <0. 001 0 0 12 24 36 Months Since Allocation 48 Cumulative KM Event Rate ± 1. 5 SE; log-rank P value Site-reported Data; ITT population

Drug-Eluting Stents vs CABG Repeat Revascularization Meta-Analysis EES vs PES HR=0. 51, 95% CI 0. 39 -0. 66 TLR at 1 Year Trials EES PES RR (95% CI) SPIRIT II 4/223 5/77 22/669 18/333 0. 61 (0. 33, 1. 12) SPIRIT IV 61/2458 55/1229 15/897 40/903 EES vs CABG? 0. 55 (0. 39, 0. 79) COMPARE HR=2. 3, 95% CI 1. 7 -3. 1 0. 28 (0. 08, 1. 00) SPIRIT III SYNTAX 0. 38 (0. 21, 0. 68) PES Overall (I-squared = 0. 0%, p = 0. 491) EES 6. 9 0. 51 (0. 39, 0. 66) NOTE: Weights are from random effects analysis. 1 . 2 Favors EES . 5 1 Risk ratio 2 5 10 Favors PES Kalesan, Juni – Updated 8/2011 Serruys PW et al: NEJM 2009





System Delay and Long-Term Mortality System Delay (min) 0 -60 61 -120 121 -180 181 -360 Long-term Mortality 15. 4% 23. 3% 28. 1% 30. 8% Terkelsen CJ et al: JAMA 304: 763 -771, 2010

Care Processes RACE Initiatives • Hospital specific reperfusion protocol • ED activation of catheterization laboratory single call • Provide EMS equipment for pre-hospital ECG Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011

Care Processes RACE Initiatives • 55 non PCI hospitals, 436 patients • Evaluate association of EMS, ED and Hospital setting with door-in-door-out time Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011

Care Processes Recommendations to Improve Door-In-Door-Out Times % of Hospitals (n=55) Before After Intervention P Hospital processes Dedicated STEMI reperfusion team with committed leadership Hospital-specific reperfusion protocol ED processes System for obtaining ECGs within 10 min. of ED arrival Single call No. to activate PCI center cardiac catheterization lab 25. 5 65. 4 <0. 001 20. 0 89. 1 <0. 001 27. 3 36. 4 0. 41 16. 4 96. 2 <0. 001 Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011

Care Processes Recommendations to Improve Door-In-Door-Out Times % of Hospitals (n=55) Before After Intervention P EMS processes EMS has equipment to perform prehospital ECGs Program for paramedics to recognize STEMI on 12 -lead ECGs Use local ambulance to transport patients within 50 miles Keep patient on local stretcher as part of AMI 74. 5 88. 2 0. 12 45. 4 80. 4 <0. 001 34. 2 56. 0 0. 07 3. 9 27. 5 0. 02 Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011

Care Processes Door-In-Door-Out Time (minutes) Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011 RACE Initiatives Pre-Intervention Post-Intervention Changes in door-in-door-out times with the RACE intervention. Among the 436 patients in this study, median door-in-door-out times improved significantly with the RACE intervention (before: 97. 0 min. [interquartile range 56 -160]; after 58. 0 min. [interquartile range 35 -90]; p<0. 0001).
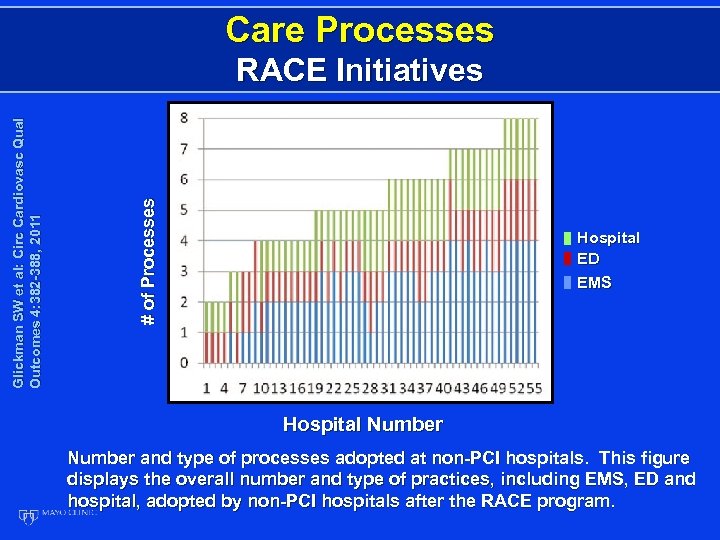
Care Processes # of Processes Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011 RACE Initiatives Hospital ED EMS Hospital Number and type of processes adopted at non-PCI hospitals. This figure displays the overall number and type of practices, including EMS, ED and hospital, adopted by non-PCI hospitals after the RACE program.

Care Processes EMS Processes Number Mi n u te s Number ED Processes Total Processes Number Glickman SW et al: Circ Cardiovasc Qual Outcomes 4: 382 -388, 2011 Hospital Processes Mi n u te s Median Door-in-Door Out Times

Conclusions – Prehospital, ED, and hospital processes of care were independently associated with shorter door-in-door-out times for STEMI patients requiring transfer. Adoption of several EMS processes was associated with the largest reduction in treatment times. These findings highlight the need for an integrated, system-based approach to improving STEMI care.

Emergency Medical Service Transport GWTG • 37, 634 STEMI patients enrolled in GWTG from 2007 -2009 • Evaluate use of EMS transport vs self transport to ED Self EMS 40% 60% Mathews R et al: Circulation 124: 154 -163, 2011

Emergency Medical Service Transport GWTG Self-Transport (n=15, 049), min EMS Transport (n=22, 585), min P 120 (60 -285) 89 (57 -163) <0. 0001 8 (4 -14) 5 (2 -10) <0. 0001 Door-to-balloon time 76 (61 -93) 63 (48 -80) <0. 0001 Door-to-needle time 29 (18 -51) 23 (13 -36) <0. 0001 Symptom-onset-tohospital-arrival time Time to ECG Mathews R et al: Circulation 124: 154 -163, 2011

Emergency Medical Service Transport GWTG EMS • Older • Live further from hospital • Hemodynamic compromise Self • • Younger Male Hispanic Private insurance Race, income, educational level – no significant association Mathews R et al: Circulation 124: 154 -163, 2011

Conclusions – Emergency medical services transportation to the hospital is underused among contemporary ST-segmentelevation myocardial infarction patients. Nevertheless, use of EMS transportation is associated with substantial reductions in ischemic time and treatment delays. Community education efforts are needed to improve the use of emergency transport as part of system-wide strategies to improve ST-segment-elevation myocardial infarction reperfusion care.

EMT Activation of Cath Labs False Positives False Negatives Door to Balloon Time

EMT Activation Approaches • Monitor vital signs and transport • Obtain ECGs • Transmit • Local ER • Regional clearing house • ED • Interventional cardiologist • Participate in interpretation • Provide in the field lytic therapy under supervision

Pre hospital ECG Programs “The central challenge for health care providers is not to simply perform PH ECG, but to use and integrate the diagnostic information from a PH ECG with systems of care. ” AHA

EMT Activation of Cath Labs Issues • False positives • University hospital in Michigan: 30% to • • 50% false positive activations Acceptable ceiling in private practice? Mayo Clinic: 15% Washington State: 15% North Carolina: 20% (ED physicians: 5%)

EMT Activation of Cath Labs Issues • False negatives

Pre hospital ECG Protocol • Prospective observational study of systems of care • Evaluate implementation of pre hospital ECG program on patients with STEMI Nestler DM. Circ Cardiovasc Qual Outcomes. 4: 640 -46, 2011

Pre hospital ECG Protocol System 1. PH ECG acquisition 2. Emergency medical service, interpretation without PHECG transmission 3. Pre hospital activation of cardiac cath team 4. Bypass ED Nestler DM. Circ Cardiovasc Qual Outcomes. 4: 640 -46, 2011

Nestler DM et al: Circ Cardiovasc Qual Outcomes 4: 640 -646, 2011 Prehospital ECGs & Activation Protocol

Prehospital ECGs & Activation Pre-implementation (n=50) Post-implementation (n=82) PH STEMI Activation (n=38) Minutes Nestler DM et al: Circ Cardiovasc Qual Outcomes 4: 640 -646, 2011

Prehospital ECGs & Activation All Preimplementation (n=50) All Postimplementation (n=82) P Postimplementation PH STEMI Activation (n=38) P Median DTB, min (interquartile range) 59 (47, 76) 57 (36, 72) 0. 28 32 (27, 55) <0. 001 Median FMCTB, min (interquartile range) 90 (78, 111) 88 (63, 114) 0. 87 58 (51, 87) 0. 001 Nestler DM et al: Circ Cardiovasc Qual Outcomes 4: 640 -646, 2011

Prehospital ECGs & Activation Conclusions An EMS-based PH ECG protocol involving prehospital interpretation without physician oversight, direct cardiac catheterization laboratory activation, and ED bypass resulted in significant reductions in median DTB and FMCTB intervals for those identified as STEMI in the prehospital setting. Nestler DM et al: Circ Cardiovasc Qual Outcomes 4: 640 -646, 2011


Futility versus Frailty

Futility versus Frailty All who drink of this remedy recover in a short time, except those whom it does not help, who all die. Therefore, it is obvious that it fails only in incurable cases…. Galen • Futility: treatment that does not accomplish its intended goal. May result from several factors – • Lack of medical efficacy • Lack of meaningful survival (patient) • Despite absolute 20% survival advantage with TAVR in PARTNER B, there is still a 30% mortality rate at one year

All-cause mortality (%) Primary Endpoint at 1 yr = 20. 0% NNT = 5. 0 pt HR (95% CI) = 0. 51 (0. 38, 0. 68) Log rank P<0. 001 50. 7% Std Rx TAVR 30. 7% Months Std Rx TAVR 179 121 138 85 124 56 103 24 60 3135558 -85

Cardiac Death to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 2. 1% vs 3. 7% P=0. 0503 50 1 -2 years* 0. 6% vs 0. 8% P=0. 62 2 -3 years* 0. 9% vs 1. 6% P=0. 22 3 -4 years* 0. 8% vs 1. 6% P=0. 13 P=0. 004 25 7. 6% 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 4. 3% 48 ITT population

Myocardial Infarction to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 3. 3% vs 4. 8% P=0. 11 50 1 -2 years* 0. 1% vs 1. 2% P=0. 008 2 -3 years* 0. 3% vs 1. 2% P=0. 03 3 -4 years* 0. 3% vs 1. 5% P=0. 01 P<0. 001 25 8. 3% 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 3. 8% 48 ITT population

CVA to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 2. 2% vs 0. 6% P=0. 003 50 1 -2 years* 0. 6% vs 0. 7% P=0. 82 2 -3 years* 0. 5% vs 0. 6% P=1. 00 3 -4 years* 0. 4% vs 0. 2% P=0. 68 P=0. 06 25 3. 7% 2. 3% 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 48 ITT population

All-Cause Death/CVA/MI to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 7. 7% vs 7. 6% P=0. 98 50 1 -2 years* 2. 2% vs 3. 5% P=0. 11 2 -3 years* 2. 5% vs 3. 8% P=0. 14 3 -4 years* 2. 7% vs 4. 6% P=0. 051 P=0. 07 25 18. 0% 14. 6% 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 48 ITT population

Repeat Revascularization to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 5. 9% vs 13. 5% P<0. 001 50 1 -2 years* 3. 7% vs 5. 6% P=0. 06 2 -3 years* 2. 5% vs 3. 4% P=0. 33 3 -4 years* 1. 6% vs 4. 2% P=0. 002 P<0. 001 23. 0% 25 11. 9% 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 48 ITT population

MACCE to 4 Years TAXUS (N=903) Cumulative Event Rate (%) CABG (N=897) Before 1 year* 12. 4% vs 17. 8% P=0. 002 50 1 -2 years* 5. 7% vs 8. 3% P=0. 03 2 -3 years* 4. 8% vs 6. 7% P=0. 10 3 -4 years* 4. 2% vs 7. 9% P=0. 002 P<0. 001 33. 5% 23. 6% 25 0 0 12 24 Months Since Allocation Cumulative KM Event Rate ± 1. 5 SE; log-rank P value; *Binary rates 36 48 ITT population

Summary and Conclusions • Four-year MACCE rates in the overall randomized • • cohort were significantly higher for PCI than CABG Significant increase of cardiac death, MI and repeat revascularization in PCI vs CABG-treated patients Composite safety (death/stroke/MI) remains not significantly different between arms at 4 years (P=0. 07) MACCE rates at 4 years were not significantly different for patients with a low baseline SYNTAX Score; for patients with intermediate or high SYNTAX Scores, MACCE was increased at 4 years in patients treated with PCI The 4 -year SYNTAX results suggest that PCI may be an acceptable alternative revascularization method to CABG when treating patients with less complex (lower SYNTAX Score) disease including LM disease

Summary: II • The 4 -year SYNTAX results suggest that CABG remains the standard of care for patients with complex disease (intermediate or high SYNTAX Scores); however, PCI may be an acceptable alternative revascularization method to CABG when treating patients with less complex (lower SYNTAX Score) disease including LM disease • The 4 -year MACCE rates for the CABG and PCI registry were 19. 9% and 42. 2% respectively • SYNTAX patients will continue to be followed for 5 years

Summary: I • In the SYNTAX randomized patients, 4 -year MACCE rates (all-cause death, stroke, repeat revascularization) were significantly higher for PCI than CABG • Significant increase of cardiac death, MI and repeat revascularization in PCI vs CABG-treated patients • Composite safety (death/stroke/MI) remains not significantly different between arms at 4 years (P=0. 07) • MACCE rates at 4 years were not significantly different for patients with a low (0 -22) baseline SYNTAX Score • For patients with intermediate (23 -32) or high SYNTAX Scores ( 33), MACCE was increased at 4 years in patients treated with PCI

Rates of Death or MI Outcomes Death or MI rate at 1 yr (%) Low risk Medium risk High risk Classic SYNTAX score P<0. 01 Functional SYNTAX score Nam et al: J Am Coll Cardiol 2011; 58: 1211 -8 3153901 -95

Rates of Major Adverse Cardiac Events (MACE) Outcomes MACE rate at 1 yr (%) Low risk Medium risk High risk P<0. 001 P<0. 01 Classic SYNTAX score Functional SYNTAX score Nam et al: J Am Coll Cardiol 2011; 58: 1211 -8 3153901 -96

FAME : “Downgrading” Multivessel Disease with FFR 3 Vessel Disease 0 -VD 2 Vessel Disease 3 -VD 1 -VD 0 -VD 2 -VD 1 -VD 2 -VD 86% 3 VD and 57% 2 VD reclassified >1 vessel Tonino et al, JACC 2010; 55: 2816 -21

ROC Analysis Death or MI FSS Sensitivity P=0. 02 SS AUC (95% CI) P FSS 0. 677 (0. 61 -0. 75) <0. 001 SS 0. 630 (0. 55 -0. 71) 0. 001 Sensitivity Nam et al: J Am Coll Cardiol 2011; 58: 1211 -8 3153901 -98

ROC Analysis Any Revascularization FSS SS Sensitivity P=0. 017 AUC (95% CI) P FSS 0. 676 (0. 59 -0. 76) <0. 001 SS 0. 621 (0. 52 -0. 72) 0. 013 Sensitivity Nam et al: J Am Coll Cardiol 2011; 58: 1211 -8 3153901 -99

ROC Analysis Death/MI/MACE at One Year FSS P=0. 329 Sensitivity SS AUC (95% CI) FSS 0. 657 (0. 56 -0. 76) SS 0. 627 (0. 52 -0. 74) P 0. 004 0. 020 Sensitivity Nam et al: J Am Coll Cardiol 2011; 58: 1211 -8 3153901 -100

Conclusions Recalculating SS by only incorporating ischemiaproducing lesions as determined by FFR decreases the number of higher-risk patients and better discriminates risk for adverse events in patients with multivessel CAD undergoing PCI. (Fractional Flow Reserve versus Angiography for Multivessel Evaluations [FAME]; NCT 00237774) 3153901 -101







Time Passes By


c16066a48efd6d4328a940e2b6cb0aeb.ppt