283c97e1e0563acd65d55aefe084cfd0.ppt
- Количество слайдов: 13
Team. STEPPS Executive Briefing Drawn from the Agency for Healthcare Research and Quality AHRQ 19 March 2018 A partnership of the Healthcare Association of New York State and the Greater New York Hospital Association
NYS PARTNERSHIP FOR PATIENTS What is Team. STEPPS? o o An evidence-based teamwork system Designed to improve: o o o 2 Quality Safety Efficiency of health care Practical and adaptable Provides ready-to-use materials for training and ongoing teamwork 19 March 2018
NYS PARTNERSHIP FOR PATIENTS Why Use Team. STEPPS? o Goal: Produce highly effective medical teams that optimize the use of information, people, and resources to achieve the best clinical outcomes o Teams of individuals who communicate effectively and back each other up dramatically reduce the consequences of human error o Team skills are not innate; people must be trained 3 19 March 2018
NYS PARTNERSHIP FOR PATIENTS Importance of Communication o Communication failure has been identified as the leading root cause of sentinel events over the past 10 years (The Joint Commission) o Communication failure is a primary contributing factor in almost 80% of more than 6, 000 root cause analyses of adverse events and close calls (VA Center for Patient Safety) 4 19 March 2018
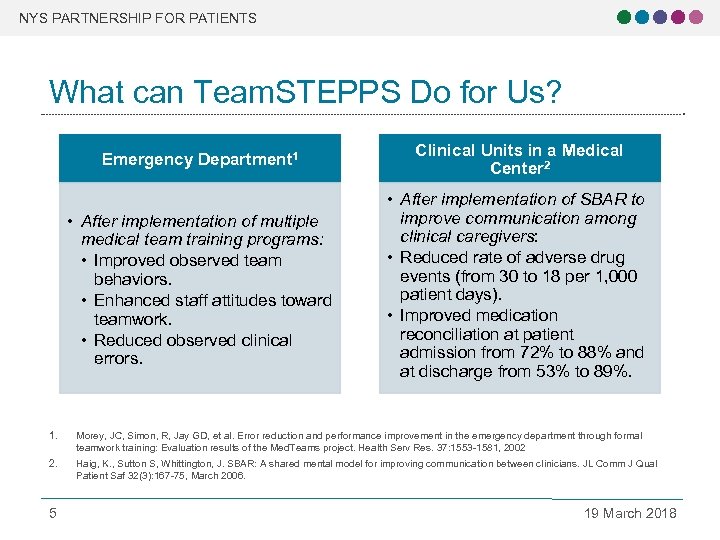
NYS PARTNERSHIP FOR PATIENTS What can Team. STEPPS Do for Us? Emergency Department 1 Clinical Units in a Medical Center 2 • After implementation of multiple medical team training programs: • Improved observed team behaviors. • Enhanced staff attitudes toward teamwork. • Reduced observed clinical errors. • After implementation of SBAR to improve communication among clinical caregivers: • Reduced rate of adverse drug events (from 30 to 18 per 1, 000 patient days). • Improved medication reconciliation at patient admission from 72% to 88% and at discharge from 53% to 89%. 1. Morey, JC, Simon, R, Jay GD, et al. Error reduction and performance improvement in the emergency department through formal teamwork training: Evaluation results of the Med. Teams project. Health Serv Res. 37: 1553 -1581, 2002 2. Haig, K. , Sutton S, Whittington, J. SBAR: A shared mental model for improving communication between clinicians. JL Comm J Qual Patient Saf 32(3): 167 -75, March 2006. 5 19 March 2018
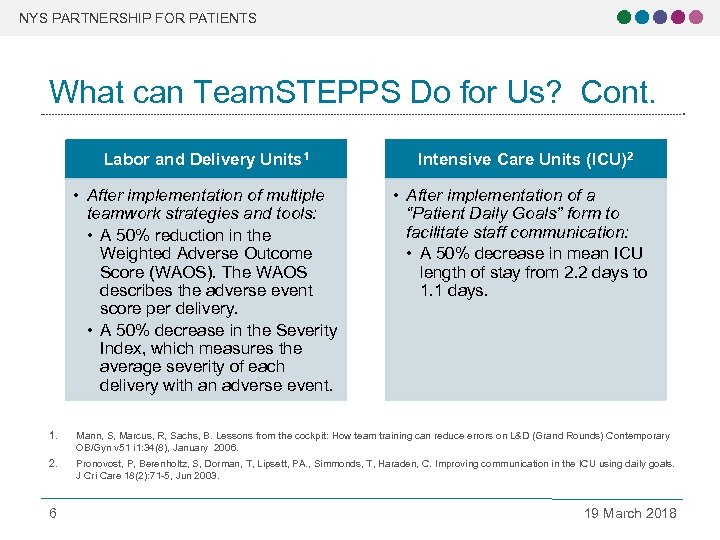
NYS PARTNERSHIP FOR PATIENTS What can Team. STEPPS Do for Us? Cont. Labor and Delivery Units 1 • After implementation of multiple teamwork strategies and tools: • A 50% reduction in the Weighted Adverse Outcome Score (WAOS). The WAOS describes the adverse event score per delivery. • A 50% decrease in the Severity Index, which measures the average severity of each delivery with an adverse event. Intensive Care Units (ICU)2 • After implementation of a “Patient Daily Goals” form to facilitate staff communication: • A 50% decrease in mean ICU length of stay from 2. 2 days to 1. 1 days. 1. Mann, S, Marcus, R, Sachs, B. Lessons from the cockpit: How team training can reduce errors on L&D (Grand Rounds) Contemporary OB/Gyn v 51 i 1: 34(8), January 2006. 2. Pronovost, P, Berenholtz, S, Dorman, T, Lipsett, PA. , Simmonds, T, Haraden, C. Improving communication in the ICU using daily goals. J Cri Care 18(2): 71 -5, Jun 2003. 6 19 March 2018
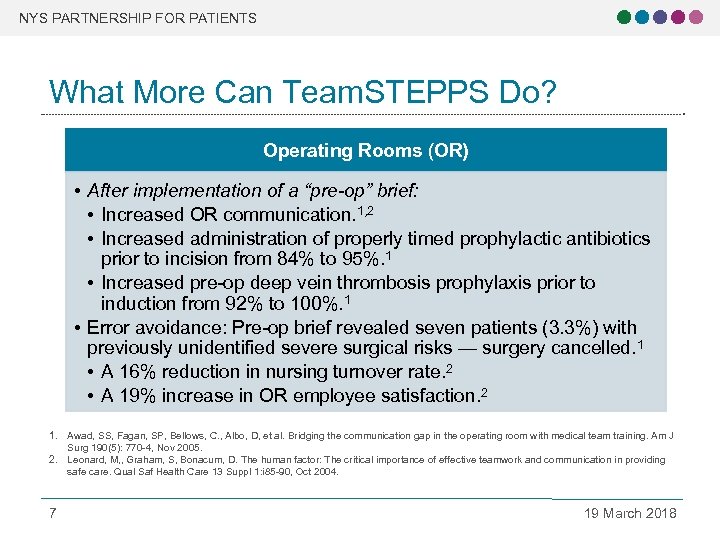
NYS PARTNERSHIP FOR PATIENTS What More Can Team. STEPPS Do? Operating Rooms (OR) • After implementation of a “pre-op” brief: • Increased OR communication. 1, 2 • Increased administration of properly timed prophylactic antibiotics prior to incision from 84% to 95%. 1 • Increased pre-op deep vein thrombosis prophylaxis prior to induction from 92% to 100%. 1 • Error avoidance: Pre-op brief revealed seven patients (3. 3%) with previously unidentified severe surgical risks — surgery cancelled. 1 • A 16% reduction in nursing turnover rate. 2 • A 19% increase in OR employee satisfaction. 2 1. Awad, SS, Fagan, SP, Bellows, C. , Albo, D, et al. Bridging the communication gap in the operating room with medical team training. Am J Surg 190(5): 770 -4, Nov 2005. 2. Leonard, M, , Graham, S, Bonacum, D. The human factor: The critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 13 Suppl 1: i 85 -90, Oct 2004. 7 19 March 2018
NYS PARTNERSHIP FOR PATIENTS What Makes Team. STEPPS Different? o o o 8 Evidence-based and field-tested Comprehensive Customizable Easy-to-use teamwork tools and strategies Publicly available 19 March 2018
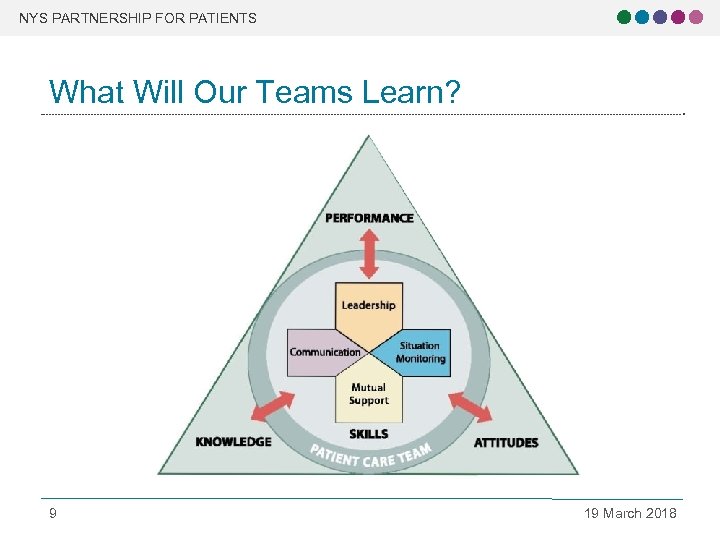
NYS PARTNERSHIP FOR PATIENTS What Will Our Teams Learn? 9 19 March 2018
NYS PARTNERSHIP FOR PATIENTS How Does Team. STEPPS Work? o I. Assessment Clearly define the need o II. Planning, Training, and Implementation o Plan to sustain the effort o Train individuals o Implement and test the strategies o III. Sustainment o Integrate into daily practice o Monitor and measure programs o 10 19 March 2018
NYS PARTNERSHIP FOR PATIENTS What Do We Need to Make This Work? o o o 11 Clearly define the need Focus on enhancing teamwork and establishing a teamwork and safety culture Support from senior leadership Allocate sufficient resources o Personnel o Time o Resources Measure success Reward and reinforce teamwork 19 March 2018
NYS PARTNERSHIP FOR PATIENTS How Do We Start? 1. 2. 3. 4. 5. 6. 7. 12 Create a sense of urgency Pull together the guiding team Formulate a change vision and strategy Communicate your vision for understanding and buy-in Attend a NYSPFP training Contact your NYSPFP Project Manager with questions More resources on Team. STEPPS available at: http: //teamstepps. ahrq. gov/ 19 March 2018
NYS PARTNERSHIP FOR PATIENTS Resources Available Team. STEPPS resources include: o o o 13 Three teamwork training curricula Course Management Guide Multimedia course materials Team. STEPPS Implementation Guide Measurement tools More resources on Team. STEPPS available at: http: //teamstepps. ahrq. gov/ 19 March 2018
283c97e1e0563acd65d55aefe084cfd0.ppt