7a556b11dcd5da9ff37311efc8c80f94.ppt
- Количество слайдов: 52
Team Building in Primary Care Mi. PCT Kick Off—March 2012 Kevin Taylor MD, MS Associate Medical Director Mi. PCT
The Good, the Bad, The Ugly of Primary Care • http: //www. youtube. com/watch? v=p. Oy 5 Lmp 3 q l. Q&feature=related
Research on Structure and Culture in Modern Primary Care • Practices are highly individual and personality driven enterprises ▫ Split deeply between physicians and staff • Embracing Radical Changes (PCMH or EMR) ▫ No fundamental redefining of roles or creating different hierarchy within practice Health Affairs 29, No. 5 (2010) 874 -879
Field Study of Three Primary Care Practices-2010 • Observations and Structured Interviews by Professional Anthropologist ▫ A solo Practice ▫ A certified PCMH ▫ A multi-physician academic practice How Teams Work-Or don’t-In Primary Care Benjamin J. Chesluk and Eric S. Holmboe Health Affairs 29, No. 5 (2010) 874 -879
Study Results • Practice team operates in separate social silos ▫ Different experience of time, space, and work within the practice ▫ Isolates Physicians from staff ▫ Disorients patients Health Affairs 29, No. 5 (2010) 874 -879
Physicians—The Frantic Bubble • Series of non-stop, one-on-one interactions with a stream of patients, • “Fictive Schedule” ▫ The”real” schedule in physicians’ heads was informed by their knowledge of the actual patients. • Not nearly enough time during office schedule to do routine documentation ▫ Several hours in evening to catch up • Extraordinary diversity of patients and complaints ▫ Physicians presented calm, friendly faces to all patients • Handled each visit essentially alone ▫ Minimal Verbal exchange between physician and staff Health Affairs 29, No. 5 (2010) 874 -879
Practice Staff—The Flexible Team • Practice Staff work in more flexible and collaborative manner ▫ Collective work ebbed and flowed • Staff would “team up” in groups ▫ Handle a host of jobs Greeting patients Answering phones Scheduling visits Preparing charts Rooming patients Health Affairs 29, No. 5 (2010) 874 -879
Patients—In Limbo • Even more isolated than the physicians • Long wait times ▫ Unpredictable, open-ended periods of waiting In designated public areas, In cold, sparse exam rooms, Sometimes partially clad in thin gowns • Left confused and disoriented at the end of visit ▫ Left to sort things out for themselves ▫ “Where do I go now? ” Health Affairs 29, No. 5 (2010) 874 -879
Meetings • Physician meetings ▫ Discuss practice from clinical and business standpoint ▫ How to tweak flow of patients and information ▫ Non-physicians absent from meeting • No regular meetings with staff and physicians Health Affairs 29, No. 5 (2010) 874 -879
Implications for Primary Care • Scarcest resources are: ▫ TIME ▫ TEAMWORK Health Affairs 29, No. 5 (2010) 874 -879
A simple definition of “team” “A team is a group with a specific task or tasks, the accomplishment of which requires the interdependent and collaborative efforts of its members. ” California Health. Care Foundation Building Teams in Primary Care: Lessons Learned
Why Teams? • Providing all of the evidence-based preventive and chronic illness care to an average panel of patients would take a single primary care provider 18 hours a day. • Most physicians only deliver 55% of recommended care and 42% report not having enough time with their patients • Providers spend 13% of their day on care coordination activities and only 50% of their time on activities using their medical knowledge. • Physicians spending 49% of the visit time at the computer and only 13% talking with the patient Safety Net Medical Home Initiative August 2011 Issue

Chronic Care Model Community Health System Resources and Improvements Policies come from redesign of basic Selfcare Management delivery Support Informed Activated Patient Health Care Organization Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared Proactive Practice Team Outcomes Improved Outcomes
Benefits of Teams in Primary Care Clinical Outcomes Multidisciplinary clinical teams produce clinical outcomes superior to those achieved by “usual care” arrangements. § § § Performance in diabetes care Overall patient satisfaction Continuity of care Access to care Better control of Chronic conditions (Hypertension, diabetes and hyperlipidemia) California Health. Care Foundation Building Teams in Primary Care: Lessons Learned
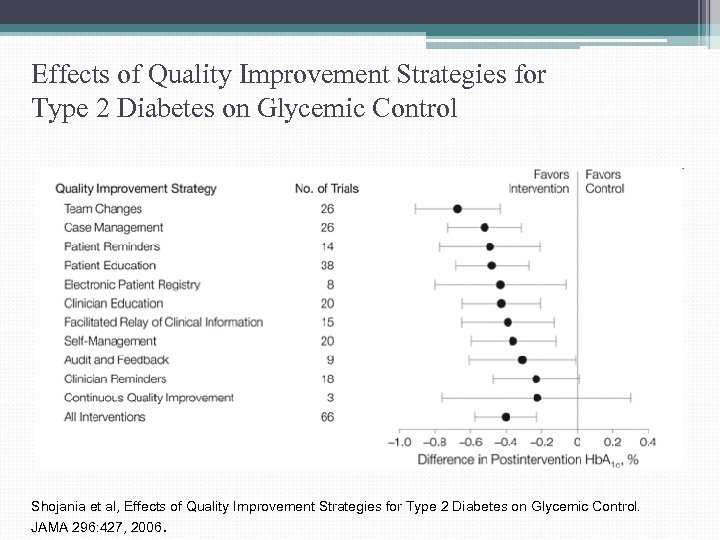
Effects of Quality Improvement Strategies for Type 2 Diabetes on Glycemic Control Shojania et al, Effects of Quality Improvement Strategies for Type 2 Diabetes on Glycemic Control. JAMA 296: 427, 2006.
What do they mean by Team Changes? Changes to the structure or organization of the primary health care team, defined as present if any of the following applied: § Adding a team member or "shared care, " § Use of multidisciplinary teams, ie, active participation of professionals from more than 1 discipline (eg, medicine, nursing, pharmacy, nutrition) in the primary, ongoing management of patients. § Expansion or revision of professional roles The most effective team changes included routine visits with personnel other than the physician and expansion of professional roles (e. g. RN, pharmacy) to include an active role in patient monitoring or adjustment. Shojania et al, JAMA 296: 427, 2006
17 Redesigning of primary care for patients with chronic conditions • Chronic Care team (Santa Clara Valley Health System) ▫ RN and Pharmacist Focus on patients with chronic illness, use registry, establish and conduct planned visits and provide medical management for HTN, DM and Hyperlipidemia following physician protocols. • Team Nursing Pilot Project (Palo Alto Foundation) ▫ In this pilot project, RN has responsibility for assisting with the care of a distinct panel of patients. ▫ By doing so, the nursing team fosters continuity of care no only with the physician but also with the RN ▫ More efficient and effective than Advice Pool RN program
Think about your favorite team…
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication California Health. Care Foundation Building Teams in Primary Care: Lessons Learned
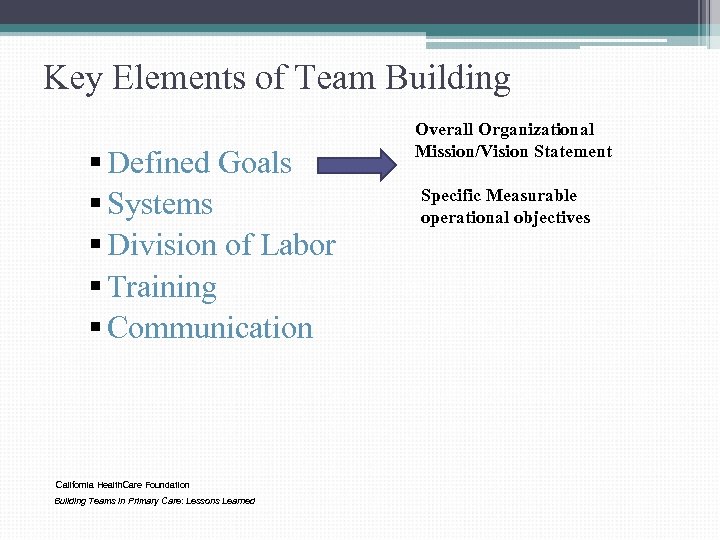
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication California Health. Care Foundation Building Teams in Primary Care: Lessons Learned Overall Organizational Mission/Vision Statement Specific Measurable operational objectives
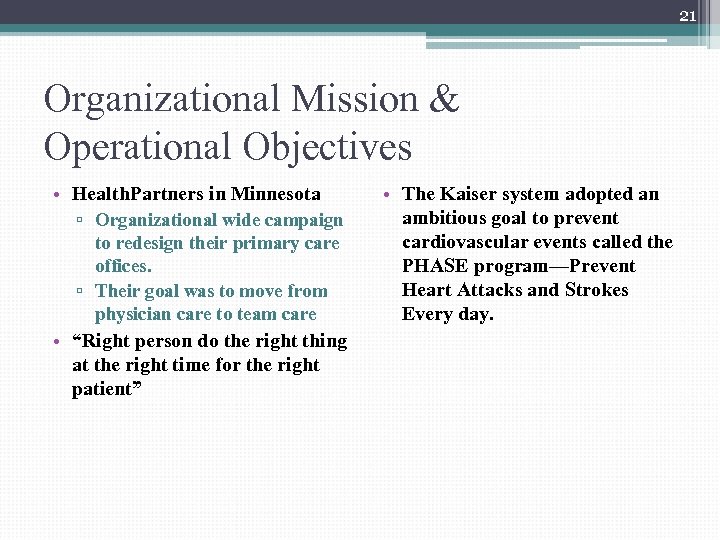
21 Organizational Mission & Operational Objectives • Health. Partners in Minnesota ▫ Organizational wide campaign to redesign their primary care offices. ▫ Their goal was to move from physician care to team care • “Right person do the right thing at the right time for the right patient” • The Kaiser system adopted an ambitious goal to prevent cardiovascular events called the PHASE program—Prevent Heart Attacks and Strokes Every day.
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication Clinical systems • Procedures for providing prescription refills Administrative systems • Procedures for making patient appointments “Standard Office Process” (SOP) California Health. Care Foundation Building Teams in Primary Care: Lessons Learned
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication California Health. Care Foundation Building Teams in Primary Care: Lessons Learned • We need to determine which people on the team perform which tasks within the clinical and administrative systems of practice. • Clear definition of tasks • Clear assignment of roles
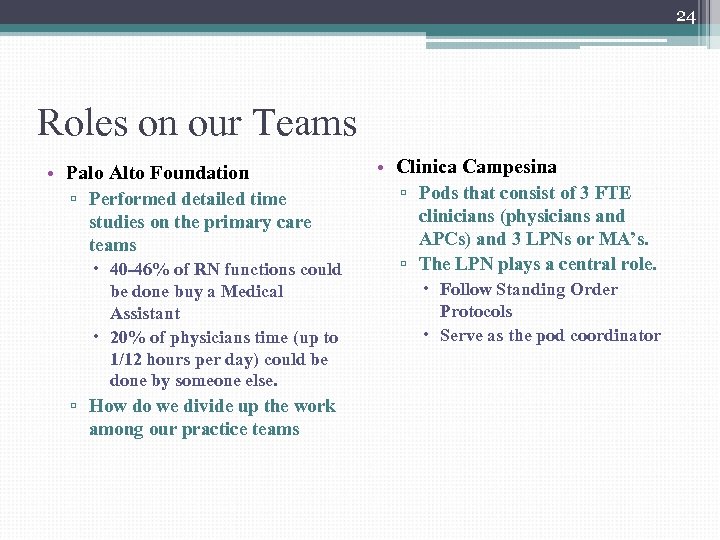
24 Roles on our Teams • Palo Alto Foundation ▫ Performed detailed time studies on the primary care teams 40 -46% of RN functions could be done buy a Medical Assistant 20% of physicians time (up to 1/12 hours per day) could be done by someone else. ▫ How do we divide up the work among our practice teams • Clinica Campesina ▫ Pods that consist of 3 FTE clinicians (physicians and APCs) and 3 LPNs or MA’s. ▫ The LPN plays a central role. Follow Standing Order Protocols Serve as the pod coordinator
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication California Health. Care Foundation Building Teams in Primary Care: Lessons Learned Training and Cross. Training for the functions that each team member regularly performs
26 St. Peter Family Medicine Residency Program Olympia WA • Medical Assistants become diabetes care managers: ▫ Follow Registry, Order appropriate labs, schedule planned visits, Draw blood, Provide MA planned visit and Followup Phone call. ▫ Require 40 hours of training 8 hours are for basic orientation to diabetes including pathophysiology, complications, treatment, practice guidelines. Also include training in behavior change, goal setting with action plans, use of the registry, conducting planned visits and SMAs
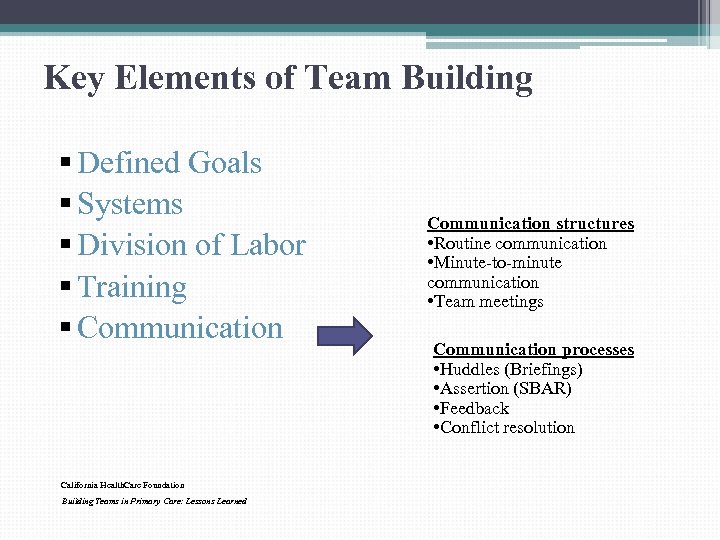
Key Elements of Team Building § Defined Goals § Systems § Division of Labor § Training § Communication California Health. Care Foundation Building Teams in Primary Care: Lessons Learned Communication structures • Routine communication • Minute-to-minute communication • Team meetings Communication processes • Huddles (Briefings) • Assertion (SBAR) • Feedback • Conflict resolution
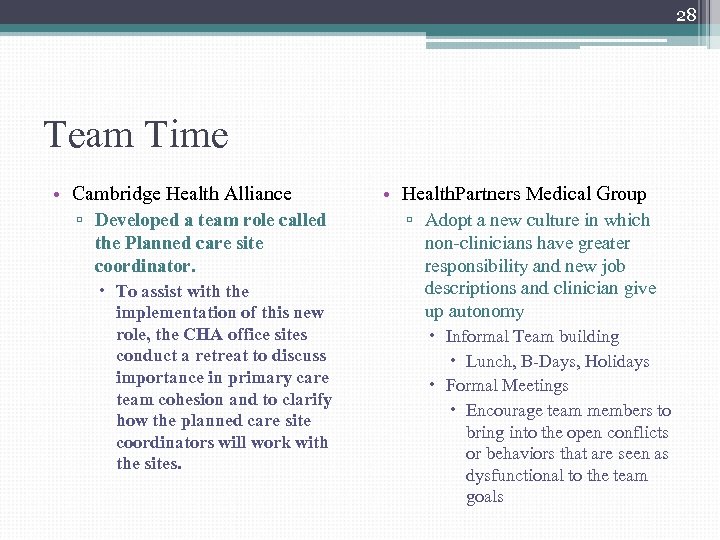
28 Team Time • Cambridge Health Alliance ▫ Developed a team role called the Planned care site coordinator. To assist with the implementation of this new role, the CHA office sites conduct a retreat to discuss importance in primary care team cohesion and to clarify how the planned care site coordinators will work with the sites. • Health. Partners Medical Group ▫ Adopt a new culture in which non-clinicians have greater responsibility and new job descriptions and clinician give up autonomy Informal Team building Lunch, B-Days, Holidays Formal Meetings Encourage team members to bring into the open conflicts or behaviors that are seen as dysfunctional to the team goals
Team Building Tools Team Building
http: //va. gov/ (search TDM) www. teammeasure. org
TEAM DEVELOPMENT MEASURE© § How do you know whether you are working as a team or not? § How much “teamness” is present in your clinic or workgroup? § What are the attributes of effective teamwork and how can you improve them?
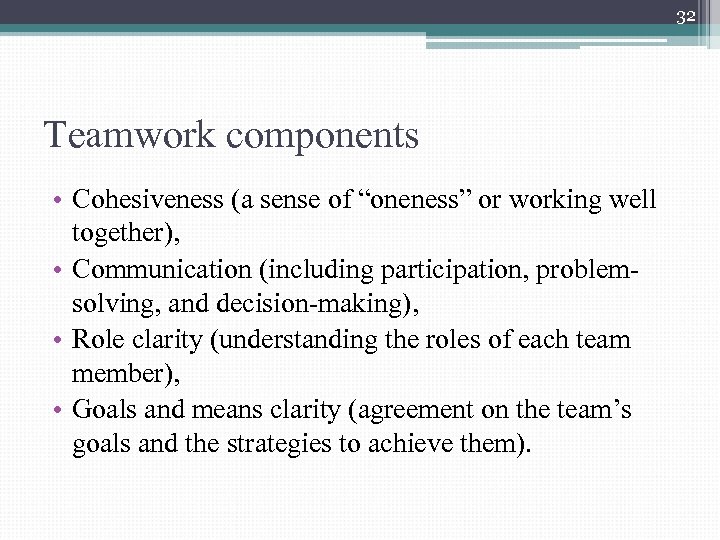
32 Teamwork components • Cohesiveness (a sense of “oneness” or working well together), • Communication (including participation, problemsolving, and decision-making), • Role clarity (understanding the roles of each team member), • Goals and means clarity (agreement on the team’s goals and the strategies to achieve them).
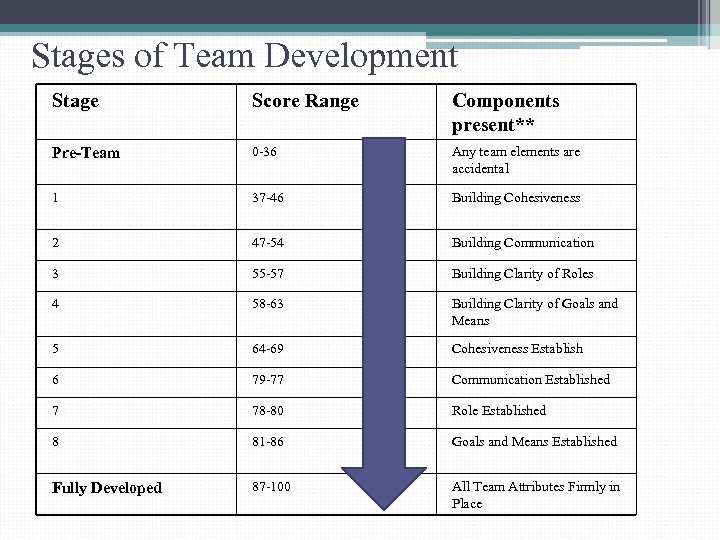
Stages of Team Development Stage Score Range Components present** Pre-Team 0 -36 Any team elements are accidental 1 37 -46 Building Cohesiveness 2 47 -54 Building Communication 3 55 -57 Building Clarity of Roles 4 58 -63 Building Clarity of Goals and Means 5 64 -69 Cohesiveness Establish 6 79 -77 Communication Established 7 78 -80 Role Established 8 81 -86 Goals and Means Established Fully Developed 87 -100 All Team Attributes Firmly in Place
34 IMPLEMENTING THE TEAM DEVELOPMENT MEASURE SURVEY • STEP 1. INITIATE THE TEAM DEVELOPMENT SURVEY (10 Minutes, 31 questions) ▫ Online www. teammeasure. og or http: //va. gov/ • STEP 2. DISTRIBUTE TEAM REPORT IN PREPARATION FOR MEETING • STEP 3. HOLD A MEETING TO REVIEW TDM REPORT (60 -90 minutes) ▫ Use Facilitator Guide http: //va. gov/ • Step 4. CONDUCTING A BRIEF TEAM REVIEW ▫ What do you consider to be the team's two or three greatest strengths? ▫ What are two or three things that the team should change or improve immediately that will make it more effective?
35 TIPS FOR SUCCESSFUL TEAMWORK Tips for Improving: • Cohesion • Communication • Roles • Goals & Means http: //va. gov/ Adapted from The Team Handbook®, Third Edition, Scholted, Joiner and Streible, Oriel Incorporated, 2003
Change Management DANGER OPPORTUNITY CRISIS
37 Transfor. MED Recommendations • Medical home requires more than just the four pillars and technological support ▫ (four pillars: access, comprehensive care, coordination of care, relationships over time) • In addition, it requires a strong organizational core (material and human resources, organizational structure, clinical process) and adaptive reserve (healthy relationship infrastructure, an aligned management model, facilitative leadership). Crabtree et al, Summary of the National Demonstration Project and Recommendations for Patient-Centered Medical Home. Ann Fam Med 2010: 8 (Suppl 1) S 80 – S 90
38 What have we learned? • Practices that never get started have leadership that is either ineffective or opposed to change. • Practices that transformed have Adaptive Reserve – the ability to learn and change. • Key feature of adaptive reserve is unified leadership that can: ▫ ▫ envision a future, have a strategy for getting there, facilitate staff involvement, and devote time to make and evaluate changes Crabtree et al, Summary of the National Demonstration Project and Recommendations for Patient-Centered Medical Home. Ann Fam Med 2010: 8 (Suppl 1) S 80 – S 90
39 Set Up for Change—Clarify the Vision “The culture of an organization is a reflection of the values of its leaders. Thus, cultural transformation begins with the personal transformation of the leaders” From “Building a values-driven organization” Richard Barrett • Communicate to all staff-- make a compelling case • Describe how it will be better • Describe the plan for making the change happen • Contributions and expectations from all • Welcome open and constructive “resistance” • Create a solid and realistic plan
40 Is There Alignment in Vision? ▫ It is easy to create a vision ▫ It is harder to create a shared vision that individuals actively engage in. ▫ It is harder still to have deep shared understanding of what the vision means for the future. ▫ It is even harder to move individuals from compliance (will do what’s expected) to commitment (will do all they can to make it happen)
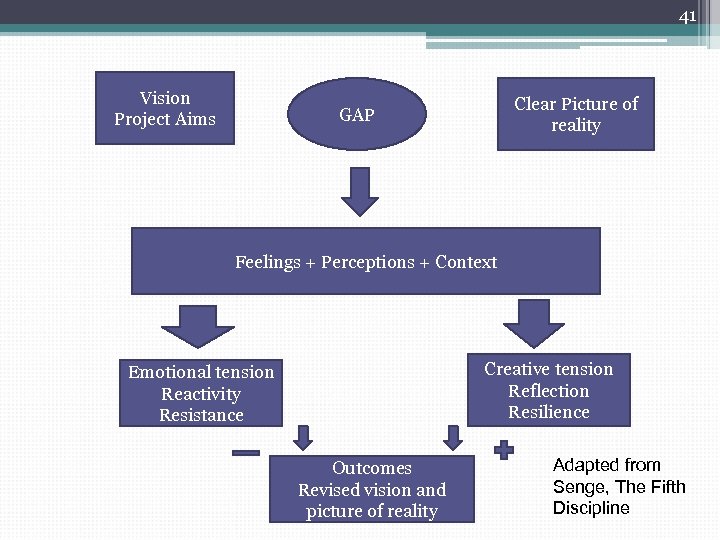
41 Vision Project Aims Clear Picture of reality GAP Feelings + Perceptions + Context Creative tension Reflection Resilience Emotional tension Reactivity Resistance Outcomes Revised vision and picture of reality Adapted from Senge, The Fifth Discipline
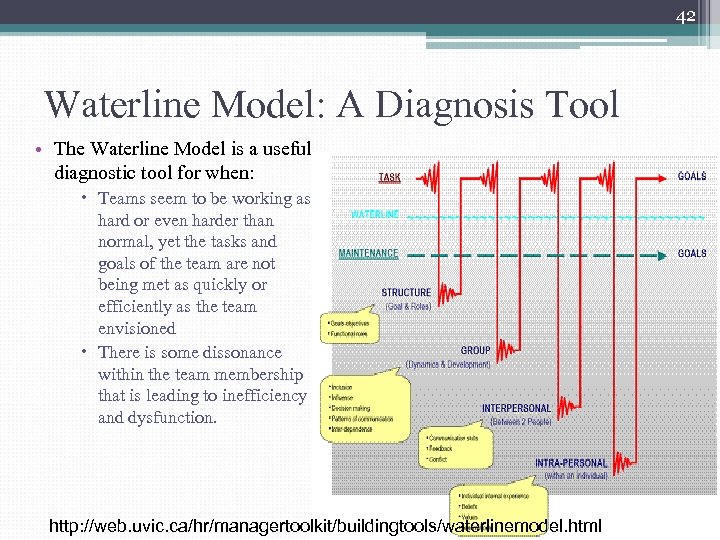
42 Waterline Model: A Diagnosis Tool • The Waterline Model is a useful diagnostic tool for when: Teams seem to be working as hard or even harder than normal, yet the tasks and goals of the team are not being met as quickly or efficiently as the team envisioned There is some dissonance within the team membership that is leading to inefficiency and dysfunction. http: //web. uvic. ca/hr/managertoolkit/buildingtools/waterlinemodel. html
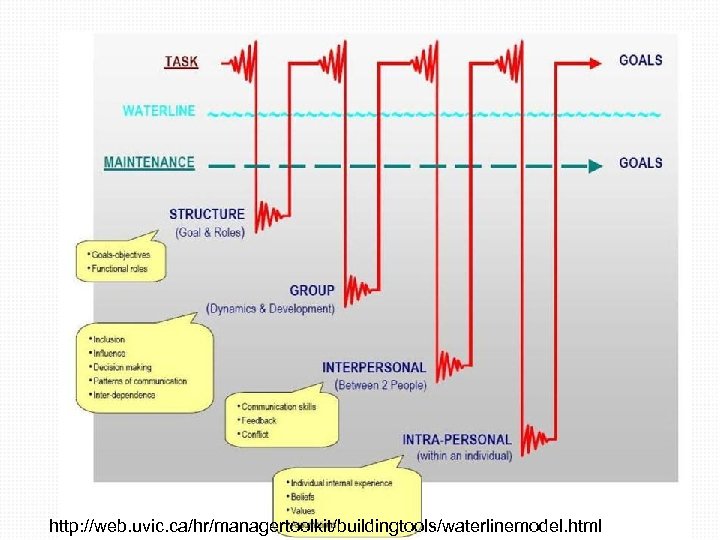
43 http: //web. uvic. ca/hr/managertoolkit/buildingtools/waterlinemodel. html
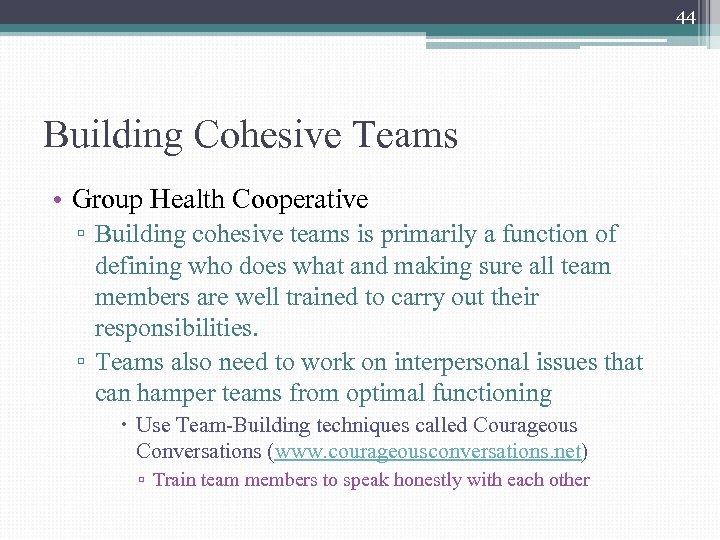
44 Building Cohesive Teams • Group Health Cooperative ▫ Building cohesive teams is primarily a function of defining who does what and making sure all team members are well trained to carry out their responsibilities. ▫ Teams also need to work on interpersonal issues that can hamper teams from optimal functioning Use Team-Building techniques called Courageous Conversations (www. courageousconversations. net) ▫ Train team members to speak honestly with each other
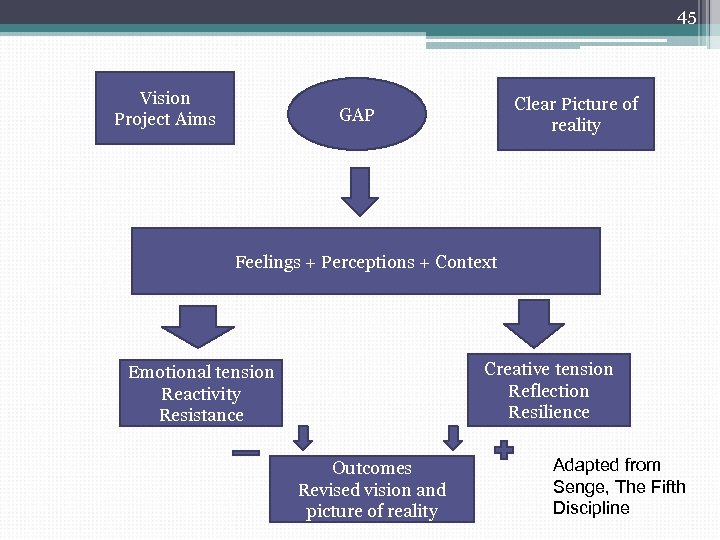
45 Vision Project Aims Clear Picture of reality GAP Feelings + Perceptions + Context Creative tension Reflection Resilience Emotional tension Reactivity Resistance Outcomes Revised vision and picture of reality Adapted from Senge, The Fifth Discipline
46 Responding Skillfully to Resistance • Establish understanding: their view ▫ Use active listening and empathy to understand the resistance (and confirm it) ▫ Get in their shoes • Establish understanding: alternative views ▫ Bring in new data and alternative views as information for consideration ▫ As indicated, assert authority or explain leadership decisions • Find mutual goals ▫ Find the connection between the vision and what is important to the person/group ▫ Elicit pros/cons of doing and not doing the change • Stay in Dialogue ▫ Free flow of information dependent on: Mutual Purpose and Mutual Respect
47 Motivational Model 1. It’s possible to do. (Yes or No) 2. I have the capability. (high, medium, low) ▫ ▫ Capability means skills, time and resources Are you capable now? Can you learn it in time? 3. It’s worthwhile for me personally? ▫ “What is most important to me personally in this situation”? Copyright 2010 Mindtech, Inc. Manny Elkind
48 Kenmore Site—Harvard Vanguard Redesigning Teams—Toyota Management Approach Essence of Toyota Method “Respectfully seeing employees as quality improvement experts and creative front line employees to improve their own work process” Three Principles in Team Formation ▫ Respect each other and the patients ▫ The management team supports the staff “What resources and training do you need to achieve your job? ” ▫ Set Expectations for excellence!
49 Kenmore Leadership—“Operationalzing” Respect • Team members meet regularly to listen to their colleagues describe • Clinical team felt their workday in detail empowered to change the way they worked ▫ Stimulate listening, understanding and coordination • Team members are encouraged to • Clinicians and staff talk about what they believe in, how members began to embrace they feel helping their patients and change what challenges come up during their day • Team members ask patients “What does it feel like to receive care here? ” ▫ Share these stories at the team meetings
Successful Practice Transformation For Mi. PCT Practices—Embrace Change! § Recognizes its difficulty and prepares practices for it. § Assure that routine care delivery is different. § Involve staff and patients in continuous process of change. WE ARE Mi. PCT! WE CAN DO IT! WE CAN MAKE CARE BETTER!
http: //www. youtube. com/watch? v=SII 1 EU 3 huu. E&feature=related
52 Tools • Clinical Microsystems http: //www. clinicalmicrosystem. org/ The Dartmouth-Hitchcock Medical Center offers free tools, including a great quick team assessment, to help pinpoint areas of improvement in team functioning. • Improving Chronic Illness Care http: //www. improvingchroniccare. org/downloads/I CIC_Toolkit_Full_FINAL. pdf ICIC developed a free, step-by-step toolkit called “Integrating Chronic Care and Business Strategies in the Safety Net” that provides tools for practices as they work to improve quality. • Institute for Healthcare Improvement http: //www. ihi. org/Pages/default. aspx IHI provides free guidance an tools around forming the team and using team huddles to improve communication. • Iowa Chronic Care Consortium http: //www. iowaccc. com/programs-andprojects/clinical-health-coach/index. aspx This group offers training for health professionals interested in becoming leaders in improving chronic illness care in their practice. Training focuses on self-management support and panel management skills among others. • Integrating Chronic Care and Business Strategies in the Safety Net http: //www. safetynetmedicalhome. org/safetynet/empanelment. cfm Group Health’s Mac. Coll Institute for Healthcare Innovation, RAND and the California Health Care Safety Net Institute have published a toolkit which provides a step-by-step practical approach to guide teams through quality improvement, focused on the chronically ill in safety net populations.
7a556b11dcd5da9ff37311efc8c80f94.ppt