a933de45089e0f92f1061050b56f011d.ppt
- Количество слайдов: 149

Team-Based Care in the Management of People with Pain SOUTHERN OREGON PAIN CONFERENCE MAY 4, 2017 PRESENTED BY KIM SWANSON, PH. D. & SCOTT SAFFORD, PH. D. ST. CHARLES FAMILY CARE –REDMOND & BEND

Disclosures Kim Swanson, Ph. D. is a full time salaried employee at St. Charles Health System. Dr. Kimberly Swanson has disclosed that within the past 12 months, she has not had financial interest with any manufacturers of medical commercial products pertaining to the presented topics. Scott Safford, Ph. D. is a full time salaried employee at St. Charles Health System. Dr. Scott Safford has disclosed that within the past 12 months, he has not had financial interest with any manufacturers of medical commercial products pertaining to the presented topics.
How to Contact Us Please email: Kim Swanson, Ph. D. www. copainguide. org under “contact us” Scott Safford, Ph. D. smsafford@stcharleshealthcare. org
Team-Based Care in the Management of People with Pain

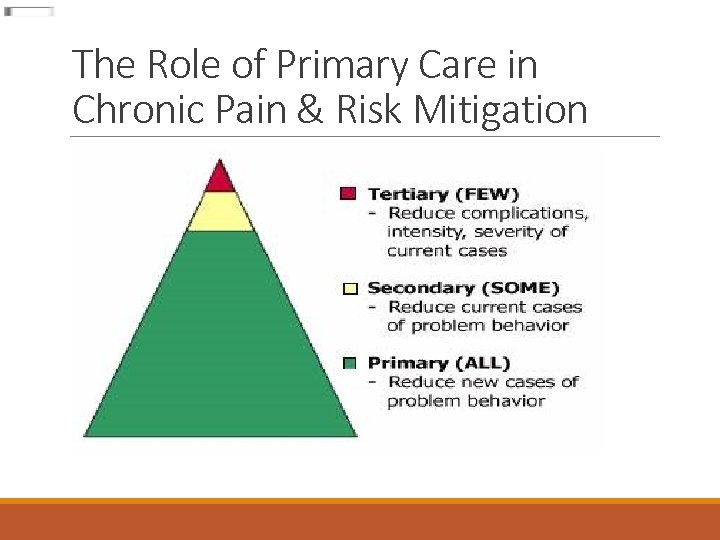
Course Outline 1) Background 2) Team Based Care ◦ Primary Prevention ◦ Secondary Prevention ◦ Tertiary Prevention 3) Stepped-care approach for chronic pain management 4) Self-management education: Pain School 5) Current outcomes and lessons learned 6) Future Directions 7) Getting Involved 8) Questions & Answers
Course Objectives 1) Develop understanding of importance of systemized chronic pain treatment in primary care. 2) Conceptualize team based, stepped care, clinical pathways for adopting comprehensive chronic pain management treatment algorithms in primary care. 3) Identify key team member’s roles and responsibilities for efficacious implementation of holistic chronic pain management treatment algorithms in primary care
Team-Based Care in the Management of People with Pain

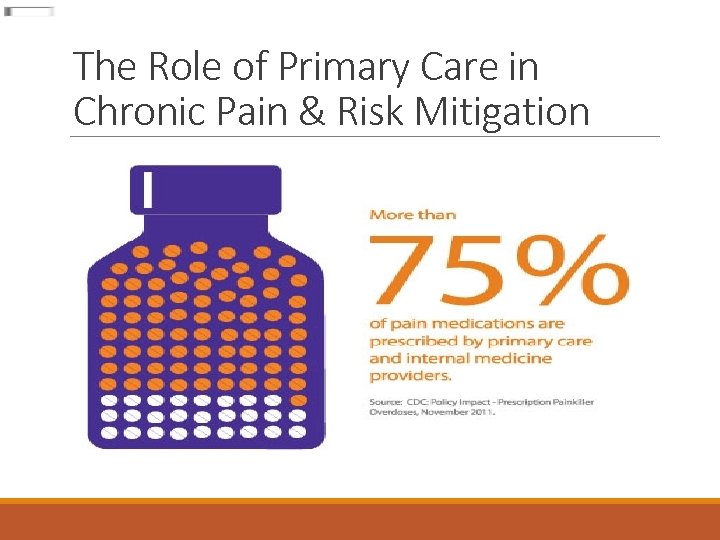
Team-Based Care in the Management of People with Pain Why should primary care providers become better with managing chronic pain? Ø Most chronic pain conditions present and are managed in primary care. Ø 79% of elderly patients with chronic pain were treated in primary care while only 5% saw a specialist. Ø Primary care is the point of entry to the medical delivery system Ø Moderate to severe pain is still one of the most common reasons for primary care visits in the United States Ø Primary care providers are the top prescribers for opioids in Oregon
Team-Based Care in the Management of People with Pain

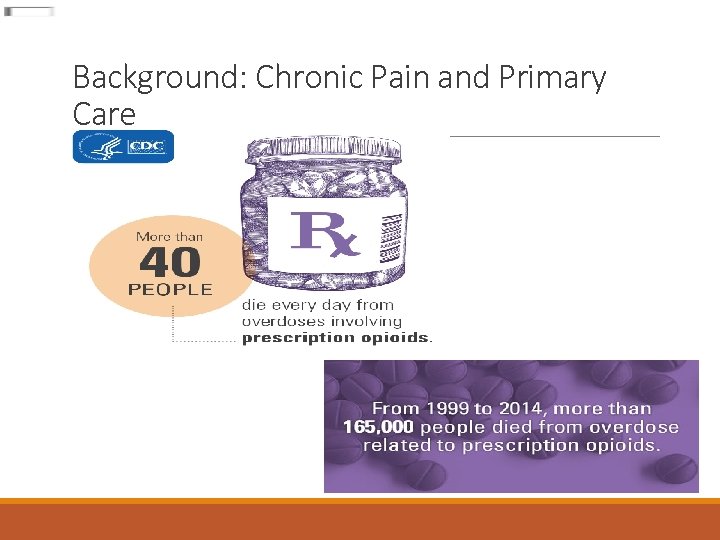
Background: Chronic Pain and Primary Care Chronic pain is a common health problem Low back pain is the leading cause of disability for Americans under the age of 45 Reference: American Academy of Pain Medicine, http: //www. painmed. org/Patient. Center/Facts_on_Pain. aspx

Background: Chronic Pain and Primary Care Statewide Information from PDMP 2013 ◦ “ 760, 000 Oregonians live with chronic pain (20%). ◦ 100, 000 are treated within the emergency department annually. ◦ More than 918, 00 Oregonians (24%) received at least one prescription opioid where the median number of prescription opioids per patient was four opioids. ◦ More than 211, 000 Oregonians received prescriptions for both an opioid and a benzodiazepine. ◦ 5943 patients filled prescriptions from at least 4 different providers and at least 4 different pharmacies. ” (p. 6) ◦ Reference: Oregon PDMP January, 2013 -December, 2013 Annual Report http: //www. orpdmp. com/orpdmpfiles/PDF_Files/Reports/Statewide 2013. pdf
Background: Chronic Pain and Primary Care
Background: Chronic Pain and Primary Care

Background: Chronic Pain and Primary Care S (Strengths) W (Weaknesses) O (Opportunities) T (Threats) Analysis S W Chronic pain Is common PCPs are reluctant to treat chronic Pain Chronic pain & its multiple morbidities are frequently treated in primary care Complex care Gaps in primary care in interdisciplinary team Innovation Quadruple Aim Gaps in coordination of care O Reduced cost Access to skilled interdisciplinary team Identification & treatment of social determinants of health Primary care team building Payer reform T Lack of etiology Paucity of specialty providers Time Agile leadership changes Inconsistencies in reimbursement
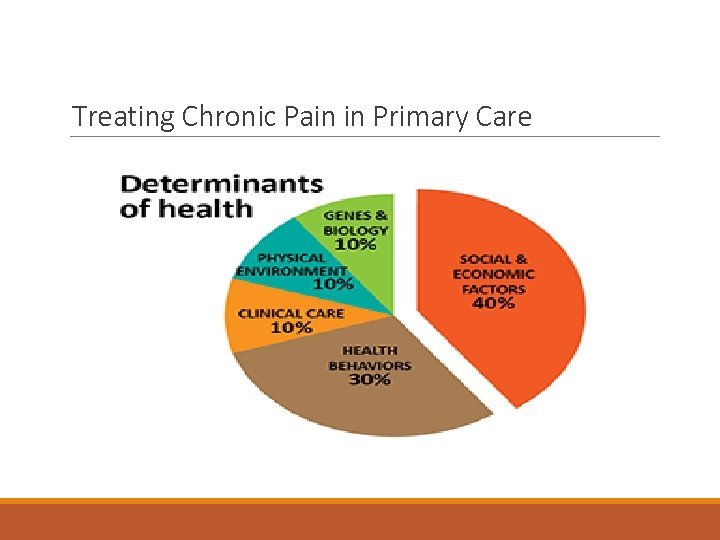
Treating Chronic Pain in Primary Care • With chronic pain, comorbidity is the rule, not the exception, for both mental and physical health conditions • Why is it important? ◦ The historical division of mind and body must give way to the reality that we cannot contain healthcare costs and improve patient care as long as we structure health and mental health care as separate and discrete enterprises

Treating Chronic Pain in Primary Care Why primary care versus specialty care? ◦ Only about 20% of individuals with mental health issues are seen by mental health professionals (Medicaid. gov) ◦ Only 30 -50% of patients follow through with PCP referrals to any service outside of primary care ◦ Paucity of Resources ◦ There a paucity of specialists who treat chronic pain ◦ There is a greater paucity of mental health and substance use specialists who treat chronic pain
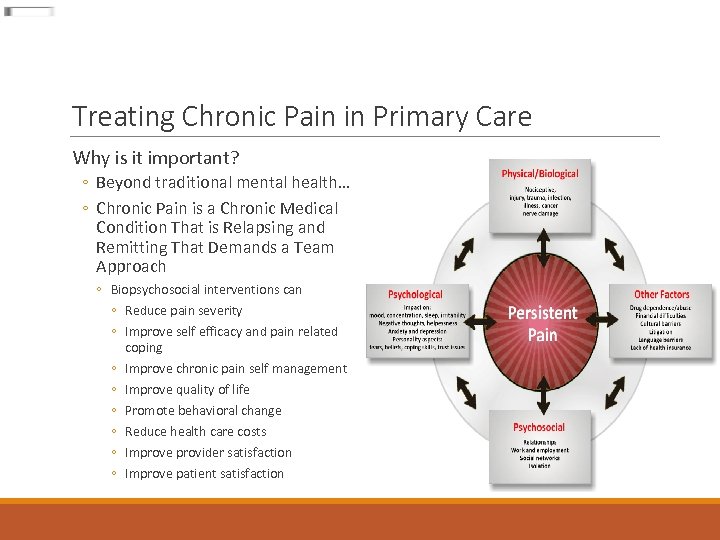
Treating Chronic Pain in Primary Care Why is it important? ◦ Beyond traditional mental health… ◦ Chronic Pain is a Chronic Medical Condition That is Relapsing and Remitting That Demands a Team Approach ◦ Biopsychosocial interventions can ◦ Reduce pain severity ◦ Improve self efficacy and pain related coping ◦ Improve chronic pain self management ◦ Improve quality of life ◦ Promote behavioral change ◦ Reduce health care costs ◦ Improve provider satisfaction ◦ Improve patient satisfaction
Treating Chronic Pain in Primary Care
Chronic Pain & Complex Care

Chronic Pain & Complex Care What is Complex Care? Ø Multiple (2 or more) chronic medical conditions Why is it important to treat chronic pain in primary care as complex care? ØPatients who present with chronic pain often have multi-morbid chronic conditions ØA condition-centric view underestimates the implications of chronic conditions ØReference: Cohen C. J. , Flaks-Manov, N. , Low M. , Balicer R. D. , & Shadmi, E. (2015). High-risk case identification for use in comprehensive complex care management. Population Health Management, 18, 15 -22. doi: 10. 1089/pop. 2014. 0011.

Chronic Pain & Complex Care Why is it important to treat chronic pain in primary care as complex? ØAt the level of individual patients, several issues are apparent: Ø How are multiple and duplicate interventions avoided? Ø How must care protocols be adjusted to take co-morbidities into account? ØAt a systems level, how can physicians best participate in increasingly complex health care that must be both systematic and individualized? Ø Integrating the management of multi-morbid conditions into primary care overwhelms even the most energetic physician without adequate support from other members of the health care team. Reference: Macleod, J. , & Smith, G. D. (2003). Psychosocial factors in public health treatment? Journal of Epidemiology and Community Health; 57, 565 -570.

Chronic Pain & Complex Care Reference: http: //www. improvingchroniccare. org/index. php? p=The_Chronic_Care. Model&s=2
Chronic Pain & Complex Care

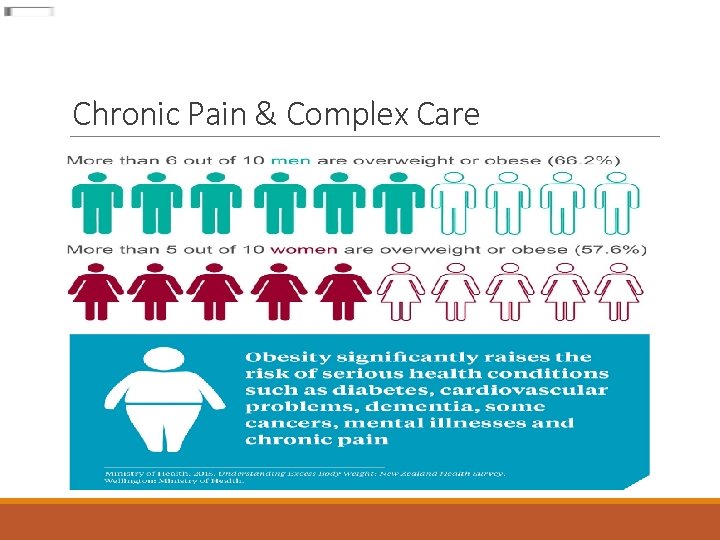
Chronic Pain & Complex Care Obesity and Chronic Pain Obesity is a modifiable risk factor in chronic pain treatment. ◦ Four out of ten obese individuals reported chronic pain ◦ 90% of them suffer from moderate-to-severe pain. ◦ Overweight and obesity have the strongest association with seeking care for low back pain and chronic low back pain. ◦ Overweight and obese twins were more likely to report low back pain, tension-type or migraine headache, fibromyalgia, abdominal pain, and chronic widespread pain than normal-weight twins References: Coaccioli S, Masia F, Celi G, Grandone I, Crapa ME, & Fatati G. (2014). Chronic pain in the obese: a quali-quantitative observational study. Recenti Progressi in Medicina, 105, 151– 154. [Medline] Hooper, MN. (2006). Tending to the musculoskeletal problems of obesity. Cleveland Clinic Journal of Medicine, 739, 839 -845 American Pain Society, news release, July 19, 2010

Chronic Pain & Complex Care Diabetes and Chronic Pain ◦ Individuals with diabetes report higher rates of chronic pain than those without diabetes, up to 40% of diabetic patients (Mantyselka et al, 2008) ◦ Chronic pain hampers diabetes self management. Reference: Mantyselka, P. , Miettoa, J. , Niskanen, L. , & Kumpusalo, E. (2008). Chronic pain, impaired glucose tolerance and diabetes: A community based study. Pain, 137, 34 -40.
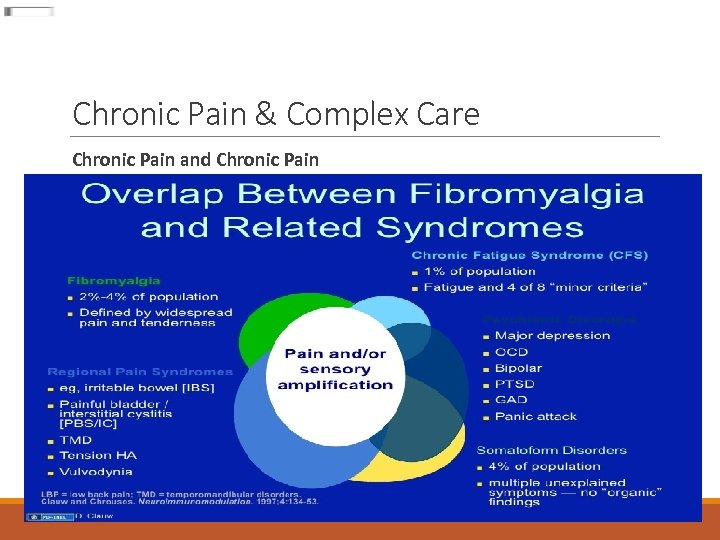
Chronic Pain & Complex Care Chronic Pain and Chronic Pain
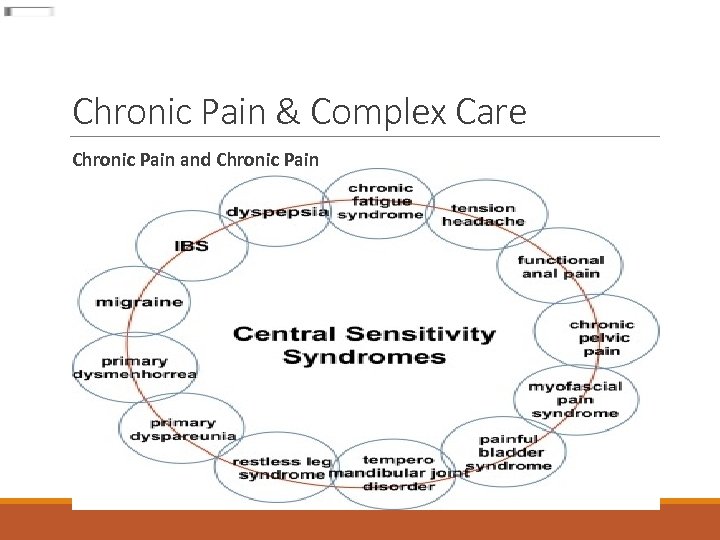
Chronic Pain & Complex Care Chronic Pain and Chronic Pain

Chronic Pain & Complex Care
Chronic Pain & Complex Care Depression & Chronic Pain ◦ On average, 65% of depressed individuals also complain of pain symptoms ◦ 3/4 ths of chronic pain patients report depressive symptoms ◦ 40 -60% of chronic pain patients meet criteria for depression ◦ (Surah et al, 2013) ◦ Depression Chronic Pain ◦ (Currie & Wang, 2005) ◦ References: Surah, A, Baranidharan, G, & Morley, S. (2013). Chronic pain and depression. Continuing Education in Anaesthesia, Critical Care, & Pain. Advance Access Publication, October 8, 2013. Curry, SR & Wang, J. (2005). More data on major depression as an antecedent risk factor first onset of chronic back pain. Psychological Medicine, 35, 1275 -1282.

Chronic Pain & Complex Care Depression & Chronic Pain ◦ Those who suffer with both depression and chronic pain report: ◦ There is a neuroanatomical ◦ More intense pain link between depression and chronic pain via the ◦ Less control of their lives hypothalamus, amygdala and ◦ More unhealthy coping strategies anterior cingulate gyrus ◦ Reduced analgesic response to opiate medications pathway ◦ Negative thinking is a common feature of depression ◦ Reduced serotonin and ◦ Catastrophic thinking, helplessness-hopelessness, norepinephrine associated and negative expectations negatively impact how a with both depression and person might respond to pain treatment increased pain sensation interventions ◦ (Surah et al, 2013) ◦ Reverse placebo/nocebo effect ◦ “Nothing works for me”

Chronic Pain & Complex Care
Chronic Pain & Complex Care Anxiety & Chronic Pain ◦ Up to 45% of chronic pain patients will screen positive for an anxiety disorder, with up to 20% meeting diagnostic criteria ◦ (Pederson, 2015) ◦ Chronic pain associated with generalized anxiety disorder, panic disorder and PTSD ◦ (Mc. Williams et al. , 2003; https: //www. adaa. org/understandinganxiety/related-illnesses/other-related -conditions/chronic-pain) ◦ References: Pederson, T. (2015). Anxiety symptoms often accompany chronic pain. Psych Central. https: //psychcentral. com/news/2013/05/11/anxiety -symptoms-often-accompany-chronicpain/54716. html Mc. Williams, L. A. , Cox, B. J. , & Enns, M. W. (2003). Mood anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain, 106, 127 -133.

Chronic Pain & Complex Care Anxiety & Chronic Pain ◦ Research has shown a link between pre-surgical anxiety and worse post-surgical outcomes, including increased reported pain ◦ (Kain et al, 2006) ◦ Chronic pain patients with comorbid anxiety may have a lower pain tolerance, be more prone to medication side-effects or fearful of having side effects, and more fearful of pain itself ◦ Anxiety management strategies (relaxation, CBT, exercise, sleep hygiene, SSRIs) can also be helpful for managing chronic pain ◦ (https: //www. adaa. org/understanding-anxiety/related-illnesses/other-relatedconditions/chronic-pain) Reference: Kain, Z. N. , Sevarino, F. , Alexander, G. M. , Pincus, S. , & Mayes, L. C. (2006). Preoperative anxiety and postoperative pain in women undergoing hysterectomy: A repeated-measures design. Journal of Psychosomatic Research, 49, 417 -422.
Chronic Pain & Complex Care Panic Disorder & Chronic Pain ◦ One study indicated 40% of Panic disorder patients also had chronic pain, particularly head, shoulder, and lower back pain ◦ Panic disorder involves a hyper-focus on somatic sensations that might increase subjective pain sensation ◦ Patients with both chronic pain and panic may engage in more “illness behaviors” ◦ (Kuch et al, 1991) Reference: Kuch, K. , Cox, B. J. , Woszczyna, C. B. , Swinson, R. P. , & Shulman, I. (1991). Chronic pain in panic disorder. Journal of Behavior Therapy and Experimental Psychiatry, 22, 255 -259.
Chronic Pain & Complex Care
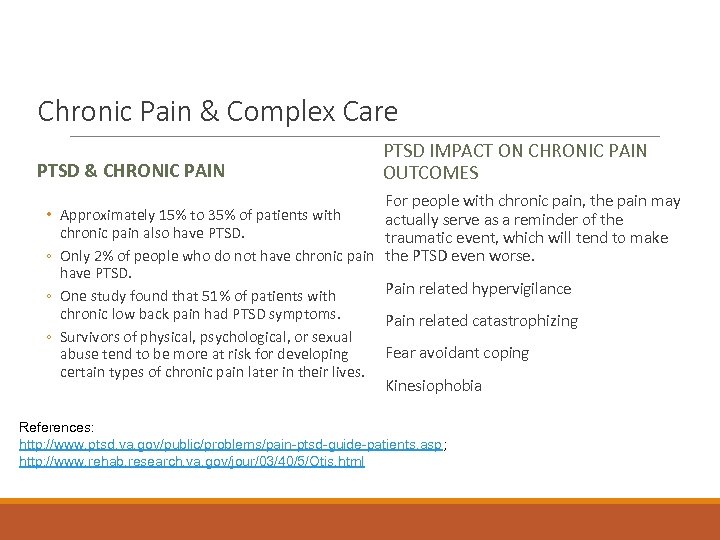
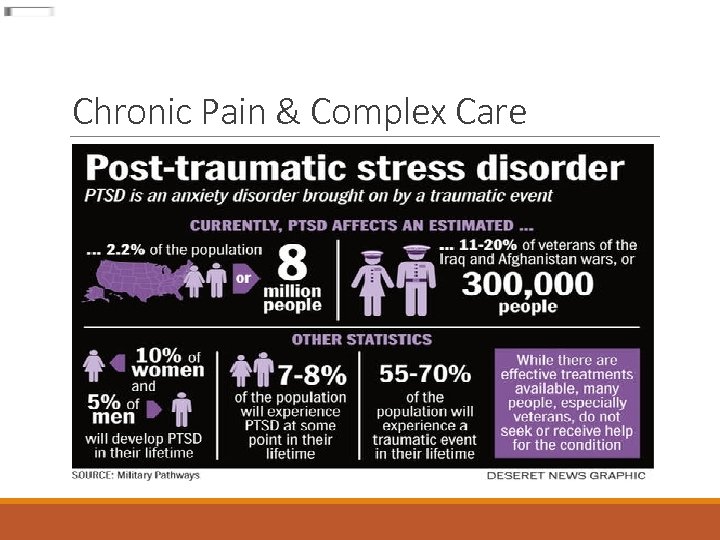
Chronic Pain & Complex Care PTSD & CHRONIC PAIN PTSD IMPACT ON CHRONIC PAIN OUTCOMES For people with chronic pain, the pain may • Approximately 15% to 35% of patients with actually serve as a reminder of the chronic pain also have PTSD. traumatic event, which will tend to make ◦ Only 2% of people who do not have chronic pain the PTSD even worse. have PTSD. Pain related hypervigilance ◦ One study found that 51% of patients with chronic low back pain had PTSD symptoms. Pain related catastrophizing ◦ Survivors of physical, psychological, or sexual Fear avoidant coping abuse tend to be more at risk for developing certain types of chronic pain later in their lives. Kinesiophobia References: http: //www. ptsd. va. gov/public/problems/pain-ptsd-guide-patients. asp; http: //www. rehab. research. va. gov/jour/03/40/5/Otis. html
Chronic Pain & Complex Care Substance Abuse & Chronic Pain
Chronic Pain & Complex Care Substance Use/Misuse/Dependence ◦ Prevalence rates of opioid misuse among chronic pain patients in primary care clinics have ranged between 20% and 40% based on urine drug screening results. ◦ Prevalence rates of opioid dependence at 2 primary care clinics was between 24% and 31%. References: ◦ Katz N, & Fanciullo GJ. (2002). Role of urine toxicology testing in the management of chronic opioid therapy. Clinical Journal of Pain, 18(supplement), S 76– 82. ◦ Reid MC, Engles-Horton LL, Weber MB, et al. (2002). Use of opioid medications for chronic non-cancer pain syndromes in primary care. Journal of General Internal Medicine, 173– 179.
Chronic Pain & Complex Care Substance Abuse & Chronic Pain References: Rates of current substance use disorders among chronic pain patients varies from 3 -48% across studies (Morasco et al, 2011) Morasco, B. J. , Gritzner, S. , Lewis, L. , Oldham, R. , Turk, D. C. , & Dobscha, S. K. (2011). Systematic review of prevalence, correlates, and treatment outcomes for chronic non-cancer pain in patients with comorbid substance use disorder. Pain, 152, 488 -497. SUD often precedes onset of chronic pain (Ilgen et al, 2010) Pain patients identified with SUD that result in discontinuation of their opioid medication will often withdraw from integrated treatment programs (Chelminski et al, 2005) Ilgen, M. A. , Perron, B. , Czyz, E. K. , Mc. Cammon, R. J. , & Trafton, J. (2010). The timing of onset of pain and substance use disorders. American Journal of Addiction, 19, 409 -415. Chelminski, P. R. , Ives, T. J. , Felix, K. M. , Prakken, S. D. , Miller, T. M. et al. (2005). A primary care, multidisciplinary disease management program for opioidtreated patients with chronic non-cancer pain amdn a high burden of psychiatric comorbidity. BMC Health Services Research, 13, 3.
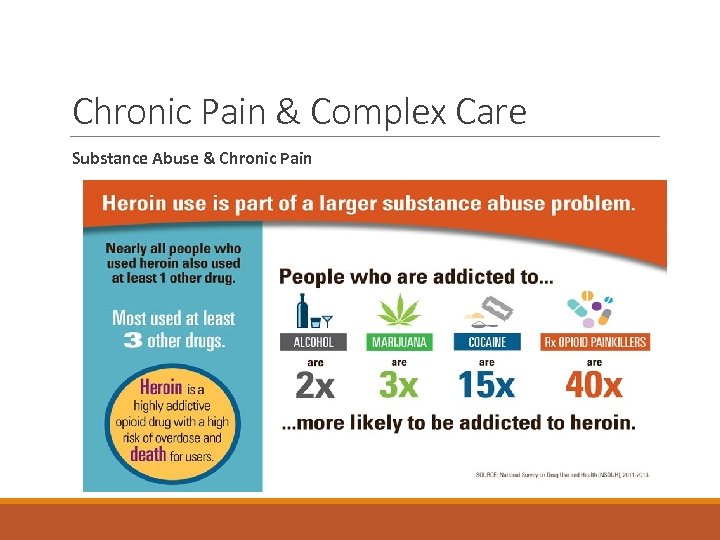
Chronic Pain & Complex Care Substance Abuse & Chronic Pain
Primary Care Comprehensive Chronic Pain Management Program o. Nuts and bolts of developing an integrated care team intervention protocol o Policies o Procedures o Who is involved? o Buy-in o Role of the EHR

Primary Care Comprehensive Chronic Pain Management Program o. Let’s start with… Mitigating Risk in Chronic Pain Patients
The Role of Primary Care in Chronic Pain & Risk Mitigation

The Role of Primary Care in Chronic Pain & Risk Mitigation America’s opioid epidemic is worsening ◦ 52, 000 Americans died from overdose in 2015
The Role of Primary Care in Chronic Pain & Risk Mitigation

The Role of Primary Care in Chronic Pain & Risk Mitigation Physician Factors In Risk Mitigation ◦ Research indicates physician’s “hunch” on patient’s use/misuse of prescription opioids is worse than chance. Reference: ◦ Michna E, Jamison RN, Pham LD, et al. (2007). Urine toxicology screening among chronic pain patients on opioid therapy: frequency and predictability of abnormal findings. Clinical Journal of Pain, 23, 173– 179.
The Role of Primary Care in Chronic Pain & Risk Mitigation Physician Factors In Risk Mitigation “Whether or not GPs prescribe opioids for persistent non-cancer pain is mainly determined by their personal beliefs about appropriateness of opioids for this problem. Neither training nor guidelines influenced prescribing” (p. 93). Reference: o Hutchinson, K. , Moreland, A. M. , Wiliams, A. C. , Weinman, J. , & Horne, R. (2007), Exploring beliefs and practice of opioid prescribing for persistent non-cancer pain by general practitioners. European Journal of Pain, 11, 93 -98.
The Role of Primary Care in Chronic Pain & Risk Mitigation Physician Factors In Risk Mitigation February 16, 2017 “Doctors Prescribe More Antibiotics When Expectations are High, Study Says” Reference: Sirota, M. , Round, T. , Samaranayaka, S. , & Kostopouou, O. (2017). Expectations for Antibiotics Increase Their Prescribing: Causal Evidence About Localized Impact. Health Psychology, published online Feb. 16, 2017.
The Role of Primary Care in Chronic Pain & Risk Mitigation Physician Factors In Risk Mitigation o Let us pause for a moment and entertain an uncomfortable conversation. . . o What influences your prescribing practices? (for the prescribing providers in the room) o What influences your clinical interventions? (for the non-prescribing providers and the prescribing providers) o How do you think an integrated primary care team could influence prescribing practices?

The Role of Primary Care in Chronic Pain & Risk Mitigation Patient Factors
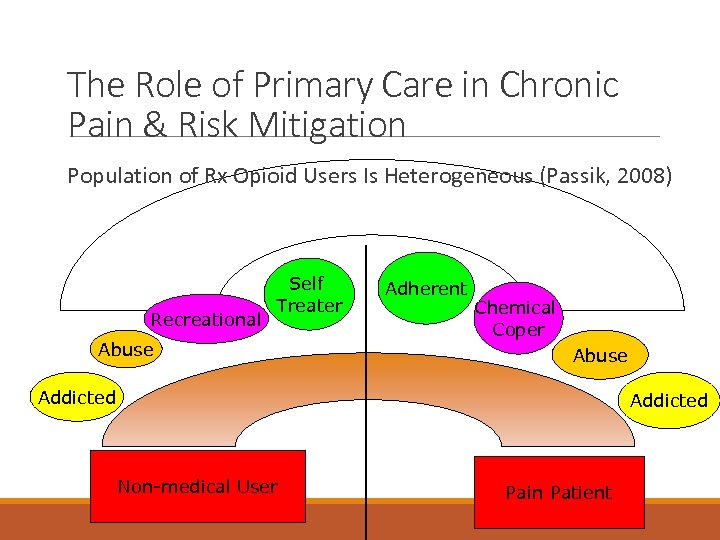
The Role of Primary Care in Chronic Pain & Risk Mitigation Population of Rx Opioid Users Is Heterogeneous (Passik, 2008) Recreational Self Treater Abuse Adherent Chemical Coper Abuse Addicted Non-medical User Pain Patient

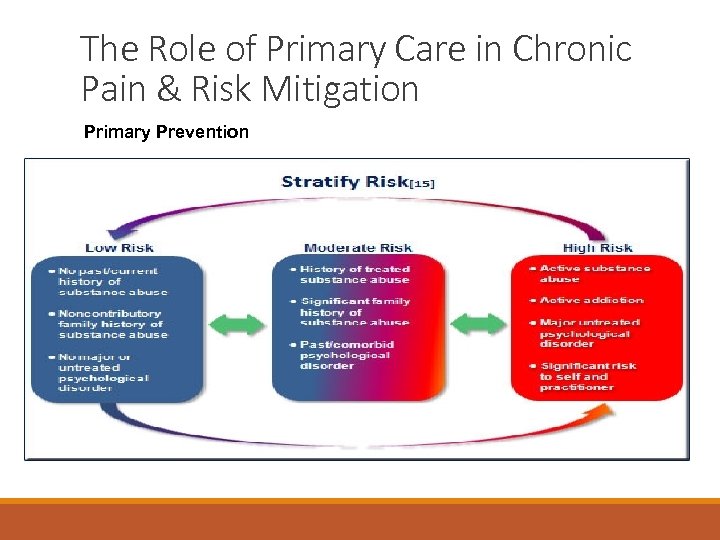
The Role of Primary Care in Chronic Pain & Risk Mitigation Patient Factors Predictive of Aberrance ◦ ◦ ◦ ◦ ◦ Personal history of drug and alcohol abuse/dependence Family history of drug and alcohol abuse/dependence Personal or family history of psychiatric disorders Male History of childhood trauma/sexual abuse History of DUII/drug convictions History of legal issues Smoking cigarettes first thing in the morning Age (16 - 45)
The Role of Primary Care in Chronic Pain & Risk Mitigation

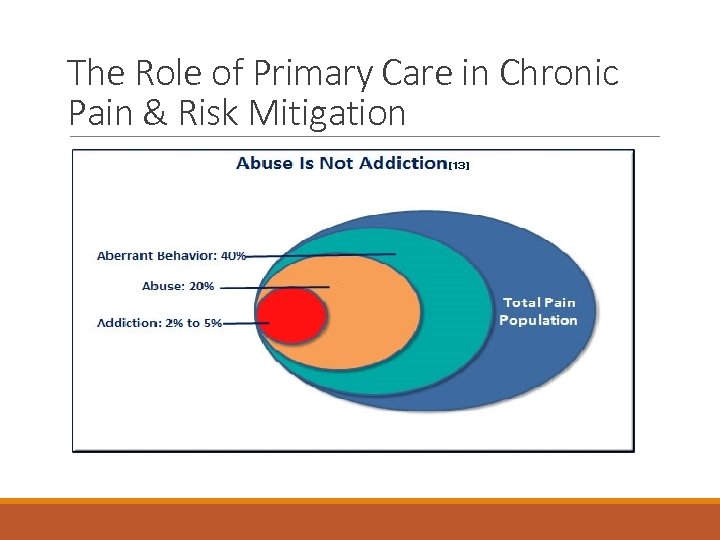
The Role of Primary Care in Chronic Pain & Risk Mitigation Definitions ◦ Misuse ◦ Use of a medication for non-medical use, or for reasons other than prescribed. ◦ Aberrant Behaviors ◦ Any medication-related behaviors that depart from strict adherence to the prescribed therapeutic plan of care. ◦ Diversion ◦ The intentional transfer of a controlled substance from legitimate distribution and dispensing channels.

The Role of Primary Care in Chronic Pain & Risk Mitigation Definitions ◦ Pseudo-addiction ◦ A drug-seeking behavior that simulates true addiction, which occurs in patients with pain who are receiving inadequate pain medication. ◦ Tolerance ◦ A higher dose of the drug is needed to achieve the same level of response achieved initially ◦ Withdrawal ◦ Symptoms that occur when drug use is discontinued or reduced in dosage
The Role of Primary Care in Chronic Pain & Risk Mitigation Definitions ◦ Physical Dependence ◦ Substance dependence in which there is evidence of tolerance, withdrawal, or both ◦ Often normal consequence of long term use of controlled substance ◦ Psychological Dependence ◦ The drug is used to obtain relief from tension or emotional discomfort

The Role of Primary Care in Chronic Pain & Risk Mitigation Definitions o The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), no longer uses the terms substance abuse and substance dependence, rather it refers to substance use disorders determined by the number of diagnostic criteria met by an individual. o Defined by severity o mild, o moderate o severe American Psychiatric Association. (2013). Substance-related and addictive disorders. Diagnostic and statistical manual of mental disorders, 5 th Ed. American Psychiatric Publishing: Washington, DC. 481 -590.

The Role of Primary Care in Chronic Pain & Risk Mitigation Definitions Opioid Use Disorder o Symptoms of opioid use disorders include o strong desire for opioids o inability to control or reduce use o continued use despite interference with major obligations or social functioning o use of larger amounts over time o development of tolerance o spending a great deal of time to obtain and use opioids o withdrawal symptoms that occur after stopping or reducing use
The Role of Primary Care in Chronic Pain & Risk Mitigation
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Checklist ØClinical interview ØPhysical examination ØClinic/Health system policies and procedures with regard to controlled substance prescribing ØReview of previous medical records and obtain signed releases of information ØPaper and pencil risk screening ØPDMP monitoring ØUrine drug screening
The Role of Primary Care in Chronic Pain & Risk Mitigation Should patients establishing care in your clinic who have previously been prescribed opioids for chronic non-cancer pain undergo risk assessment?
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention o. Clinic/Health system policies and procedures o Increases administrative buy-in and creates avenues for enforcement. o Provides an avenue for prescribing providers to say “no” with more ease when medically and clinically appropriate. o Creates a universal standard of care in a clinic/health system. o Helps clinics align with Federal and State safe prescribing guidelines o References: See www. cdc. gov/drugoverdose/prescribing/guideline. html for CDC guidelines See https: //public. health. oregon. gov/Prevention. Wellness/Substance. Use/Opioids/ Documents/taskforce/oregon-opioid-prescribing-guidelines. pdf for Oregon Prescribing Guidelines
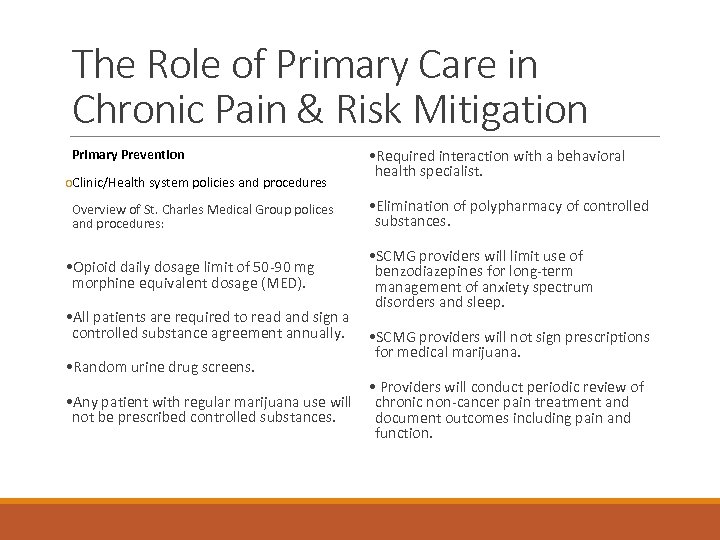
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention o. Clinic/Health system policies and procedures • Required interaction with a behavioral health specialist. Overview of St. Charles Medical Group polices and procedures: • Elimination of polypharmacy of controlled substances. • Opioid daily dosage limit of 50 -90 mg morphine equivalent dosage (MED). • SCMG providers will limit use of benzodiazepines for long-term management of anxiety spectrum disorders and sleep. • All patients are required to read and sign a controlled substance agreement annually. • SCMG providers will not sign prescriptions for medical marijuana. • Random urine drug screens. • Providers will conduct periodic review of • Any patient with regular marijuana use will chronic non-cancer pain treatment and not be prescribed controlled substances. document outcomes including pain and function.
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention

The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Method Sensitivity Psychologist Clinical Interview 77% Screener and Opioid Assessment for Patients with Pain (SOAPP) 73% Opioid Risk Tool (ORT) 45% Which method is the best way to predict opioid misuse or abuse? ◦ In a study of 48 chronic pain patients, the sensitivity of predicting aberrant behavior was compared using three different methods: Reference: ◦ https: //www. capc. org/fast-facts/244 -screeningopioid-misuse-and-abuse/
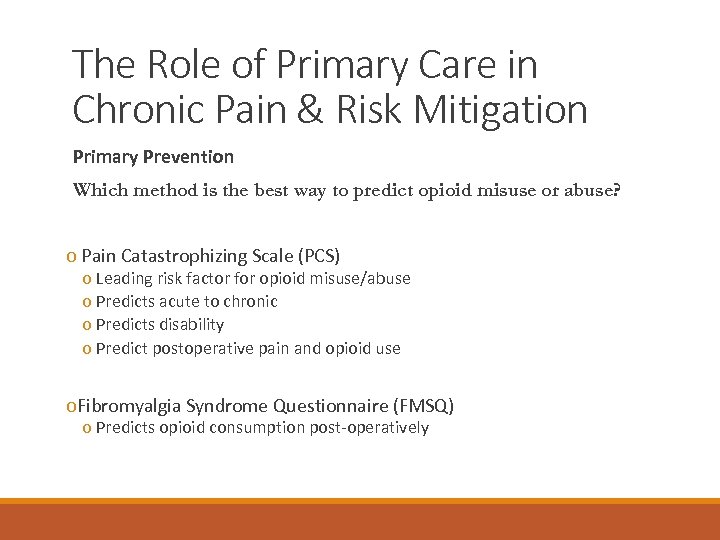
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Which method is the best way to predict opioid misuse or abuse? o Pain Catastrophizing Scale (PCS) o Leading risk factor for opioid misuse/abuse o Predicts acute to chronic o Predicts disability o Predict postoperative pain and opioid use o. Fibromyalgia Syndrome Questionnaire (FMSQ) o Predicts opioid consumption post-operatively

The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention ◦ Systematic screening conducted by Behavioral Health Consultant ◦ ◦ ◦ Clinical interview Opioid Risk Tool PHQ-9 GAD-7 Adult ADHD Self Report Screening Test ◦ Mood Disorder Questionnaire ◦ Primary Care Posttraumatic Stress Disorder Questionnaire ◦ ◦ ◦ ◦ Pain Catastrophizing Scale Numeric Pain Rating Scale Pain Disability Index Insomnia Severity Index STOP-BANG Epworth Sleepiness Scale Alcohol Use Disorder Identification Test (AUDIT) ◦ Drug Abuse Screening Test (DAST) ◦ Cannabis Use Disorder Test – Revised (CUDIT-R)

The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Urine Drug Screening Review of Medical Records Conduct urine drug testing before starting opioid therapy Prior to prescribing opioids, review the patient’s medical records and, if possible, consult with the patient’s previous prescriber. Reference: https: //www. cdc. gov/drugoverdose/pdf /guidelines_factsheet-a. pdf http: //www. ago. wv. gov/Documents/ 2016. 08. 19%20 BP%20 Prescribing. P DF
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Prescription Drug Monitoring Program (PDMP) Maximize efficiency and improve patient care by using a PDMP Clinicians should review PDMP data when starting opioid therapy for chronic pain o Helps providers by increasing awareness of all active controlled substance medications on file for a patient. o Helps providers safely and effectively treat chronic pain. o Alerts prescribers to patients obtaining prescriptions from multiple providers. o Prescribers can use PDMP data as a tool to monitor compliance and increase confidence in prescribing decisions. If you have not signed up as a prescribing provider or a delegate go to this website: http: //www. orpdmp. com/ References: https: //www. cdc. gov/drugoverdose/pdf/guidelines_factsheet-a. pdf https: //www. cms. gov/Medicare-Medicaid-Coordination/Fraud-Prevention/Medicaid-Integrity. Education/Downloads/drugdiversion-drugmonitoring-factsheet. pdf

The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Prescription Drug Monitoring Program (PDMP) o What is your clinic’s workflow in using PDMP for primary prevention?
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention o Refer for alternative safer treatments first o American College of Physicians Guidelines for Low Back Pain (2017) ◦ For pain lasting up to 12 weeks, nondrug treatments are preferred, with the strongest evidence for applying heat. There is also evidence for massage, acupuncture, and spinal manipulation. Evidence does support nonsteroidal anti-inflammatory drugs (NSAIDs, such as aspirin and ibuprofen) and muscle relaxants. ◦ Chronic lower back pain (more than 12 weeks) should initially be treated with practices like exercise, multidisciplinary rehabilitation, acupuncture, and mindfulness-based stress reduction. There is also evidence for practices ranging from tai chi and yoga to biofeedback and cognitive behavioral therapy. ◦ Chronic back pain that did not respond to nondrug treatments should first be treated with NSAIDs. Tramadol (a short-acting opioid) or duloxetine (an antidepressant) would be secondline treatments. Other opioids should be a last resort. References: http: //www. aafp. org/afp/2008/0601/p 1607. html http: //annals. org/aim/article/2603228/noninvasive -treatments-acute-subacute-chronic-low-backpain-clinical-practice
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention o Refer for alternative safer treatments first “HERC Updated Policy to Treat Back Pain The May meeting of the HERC (Health Evidence Review Commission) announced the release of updated guidelines for the treatment of chronic non-cancer back pain. These changes became effective 7/1/16. The back conditions technical changes reflects the priority to reduce the number of opiate prescriptions that are given for chronic non-cancer pain. The guidelines include a bio-psycho-social model designed to help people with back problems resume normal activities. This model aims to help people manage their pain with less reliance on medication and utilization of different modalities including acupuncture, cognitive behavioral therapy and otherapies based in evidence. ” http: //www. ccooregon. org/2016/05/23/herc-updated-policy-treat-back-pain/

The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention All patients with chronic pain should be referred to courses in self management.
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Several contraindications exist for treating with a controlled substance ◦ ◦ Opiate risk score: >90% chance of developing problematic behaviors. History of suicide attempts within the past 2 years Patient currently on Suboxone/Methadone maintenance No functional improvement noted after a trial or chronic use as determined by the provider
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Several contraindications exist for treating with a controlled substance ◦ No medical work-up or incomplete work up of pain condition ◦ History of misuse, overuse, or diversion ◦ Receiving multiple prescriptions from multiple different providers/clinics/sites ◦ Frequent ER use to obtain controlled substances ◦ Active substance abuse as defined by any illicit or non-prescribed medication use within the past 12 -months
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention Several circumstances exist where it is strongly cautioned against prescribing a controlled substance: ◦ ◦ Diagnosis is not clear or defined Previous dismissal and/or controlled substance agreement violation Patient concomitantly taking long term benzodiazepines Under-treated or inadequately treated psychiatric health conditions as evidenced by a Patient Health Questionnaire – 9 (PHQ-9) score > 15 or a Generalized Anxiety Disorder – 7 (GAD-7) score > 12
The Role of Primary Care in Chronic Pain & Risk Mitigation Primary Prevention o Case Study of BHC Consultation to PCP
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Checklist ØMaterials Risk Notice ØPatient education about risk/benefits ØControlled Substance Agreement ØPDMP Monitoring ØUrine Drug Screen ØCo-Prescription of Naloxone

The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention ◦ Prescribing providers should respond to every violation of the controlled substance agreement including no-shows and document in the patient’s medical record. ◦ 85% of all patients who are prescribed a controlled substance will not demonstrate aberrant drug related behavior. ◦ all violations of the controlled substance agreement should be addressed ◦ careful reassessment of appropriateness of continuation of a controlled medication prescription should be considered.
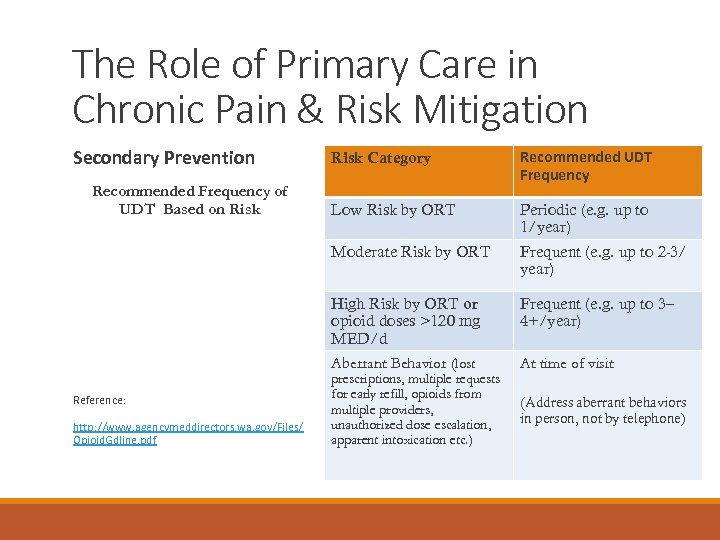
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention http: //www. agencymeddirectors. wa. gov/Files/ Opioid. Gdline. pdf Low Risk by ORT Periodic (e. g. up to 1/year) Frequent (e. g. up to 2 -3/ year) High Risk by ORT or opioid doses >120 mg MED/d Aberrant Behavior (lost Reference: Recommended UDT Frequency Moderate Risk by ORT Recommended Frequency of UDT Based on Risk Category Frequent (e. g. up to 3– 4+/year) prescriptions, multiple requests for early refill, opioids from multiple providers, unauthorized dose escalation, apparent intoxication etc. ) At time of visit (Address aberrant behaviors in person, not by telephone)
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Behavioral Characteristics of Aberrance ◦ Diversion ◦ ◦ Selling prescription drugs Forging prescriptions Stealing or borrowing drugs Multiple episodes of loss or theft of prescription drugs ◦ Insist on a written police report ◦ Preference for high street value drugs (e. g. oxycodone) ◦ Not following prescribed dose and schedule on several occasions Reference: http: //www. agencymeddirectors. wa. gov/Files/Opioid. Gdline. pdf
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Behavioral Characteristics of Aberrance ◦ Most likely to predict substance misuse/abuse: ◦ ◦ ◦ Steeling or borrowing controlled substances Obtaining controlled substances from a non-medical source Concurrent use/abuse of illicit drugs Injecting controlled substances meant for oral use Multiple unsanctioned dose escalations Recurrent (more than once) loss or theft of controlled substance prescriptions and requests for early refills Reference: http: //www. agencymeddirectors. wa. gov/Files/Opioid. Gdline. pdf
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Behavioral Characteristics of Aberrance ◦ Less likely to predict misuse/abuse: ◦ ◦ ◦ Aggressive complaining about the need for higher doses Drug hoarding during periods of reduced symptoms Requests for specific drugs Unsanctioned dose escalations Unapproved use of the controlled substance for other symptoms Patient report of unexpected central nervous system effects (e. g. euphoria) Reference: http: //www. agencymeddirectors. wa. gov/Files/Opioid. Gdline. pdf

The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Materials Risk Notice “When prescribing opioids for chronic pain, the law requires health care professionals to provide careful assessment and documentation of the medical condition causing pain as well as comorbid medical and mental health conditions. Goals for treatment should be established with the patient before prescribing opioids. Patients must be informed of the risks and sign a Material Risk Notice. ” Reference: http: //www. oregon. gov/omb/OMBForms 1/material-risk-notice. pdf
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Materials Risk Notice
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Controlled substance agreement o o o The written agreement shall include: The patient’s agreement to provide biological samples for urine/serum medical level when requested by the provider The patient’s agreement to take medications at the dose and frequency prescribed A requirement that all controlled substances are provided by a single prescriber/medical group, and dispensed by a single pharmacy system The patient’s agreement to not abuse alcohol or other illicit or medically unauthorized substances
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Controlled substance agreement o The written agreement shall include: ◦ Written authorization for: ◦ The physician to release the agreement for treatment to all local emergency room departments, urgent care facilities, and pharmacies ◦ Other practitioners to report violations of the agreement back to the physician ◦ Regular access to the Oregon Prescription Drug Monitoring Program
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Controlled substance agreement o The written agreement shall include: ◦ Acknowledgement that ◦ The provider may notify the proper authorities if he or she has reason to believe the patient has engaged in illegal activity ◦ Violation of the agreement will result in a tapering or discontinuation of the controlled substance ◦ It is the patient’s responsibility to safeguard all medications and keep them in a secure location ◦ The patient will not request early refills or call after 5 pm or over the weekend for refills of their controlled substance ◦ If the patient violates the terms of the agreement, the violation and the provider’s response will be documented, as well as the rationale for the changes in the treatment plan ◦ Required attendance at Pain School or an equivalent behavioral program to learn behavioral management of chronic pain
Primary Care Comprehensive Chronic Pain Management Program Secondary Prevention Ongoing Assessment & Provider Education (PCP) ◦ Implementation of education and educational standards regarding chronic pain management ◦ Physician documentation and ongoing assessment to demonstrate best practices in chronic pain management ◦ Is the patient adhering to treatment including engagement with behavioral health and self management? ◦ Are the treatment interventions working? ◦ The 4 A’s ◦ Adequate analgesia ◦ Adverse side effects ◦ Activities of daily living ◦ Aberrant drug-related behaviors
Primary Care Comprehensive Chronic Pain Management Program Secondary Prevention PDMP Monitoring Once you have started a patient on an opioid, tell me about your best practices for PDMP monitoring?
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Teach Patients Medication Home Safety These simple steps can help reduce the risk of their misuse and abuse by people who have access to your patient’s home and medicine cabinet o Monitor: Do patients know what medications they have in the home? o Secure: Are controlled substances kept in a secure location? o Dispose: Do patients get rid of expired and unused medications and where do they go to do so? Reference: https: //www. cdc. gov/medicationsafety/
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Teach Patients Medication Home Safety Medication Safes o. Here are some websites where patients can purchase medication safes to store all of their medications securely in one locked location. o http: //medicinesafe. com/ o http: //medixsafe. com/products/ o http: //www. knoxbox. com/store/Knox. Med. Vault. cfm? utm_source=bing&utm_campaign=medvault_s_drug_locker&utm_me dium=cpc&utm_term=safe o http: //medguardsafes. com
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Co-Prescription of Naloxone as Universal Precautions o Early access to the opioid reversal agent Naloxone through communitybased models has demonstrated positive outcomes during its use in the last decade. o Pain patients and their loved ones can be educated on overdose symptoms and administration of intranasal naloxone in the community setting Reference: https: //www. ihs. gov/odm/overdose-prevention-treatment/naloxone-prescribing/
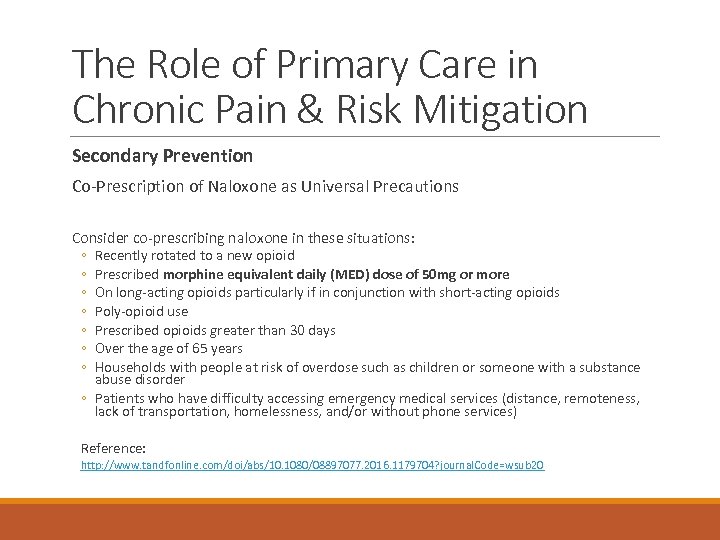
The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Co-Prescription of Naloxone as Universal Precautions Consider co-prescribing naloxone in these situations: ◦ ◦ ◦ ◦ Recently rotated to a new opioid Prescribed morphine equivalent daily (MED) dose of 50 mg or more On long-acting opioids particularly if in conjunction with short-acting opioids Poly-opioid use Prescribed opioids greater than 30 days Over the age of 65 years Households with people at risk of overdose such as children or someone with a substance abuse disorder ◦ Patients who have difficulty accessing emergency medical services (distance, remoteness, lack of transportation, homelessness, and/or without phone services) Reference: http: //www. tandfonline. com/doi/abs/10. 1080/08897077. 2016. 1179704? journal. Code=wsub 20

The Role of Primary Care in Chronic Pain & Risk Mitigation Secondary Prevention Co-Prescription of Naloxone as Universal Precautions Consider co-prescribing naloxone in these situations ◦ Concurrent prescription or over-the-counter medications ◦ ◦ ◦ Benzodiazepines Antipsychotics Antiepileptics Muscle relaxers Hypnotics Antihistamines Reference: http: //www. tandfonline. com/doi/abs/10. 1080/08897077. 2016. 1179704? journal. Code=wsub 20

The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention Checklist ØEngagement with integrated Health Care Team (Clinical Pharmacist, RNCC, CHE) ØOpioid Tapering ØReferral to Mental Health Treatment ØReferral to Chemical Dependency Treatment ØMedication Assisted Treatment in Primary Care after Stable ØER Diversion ØThe role of the Electronic Health Record
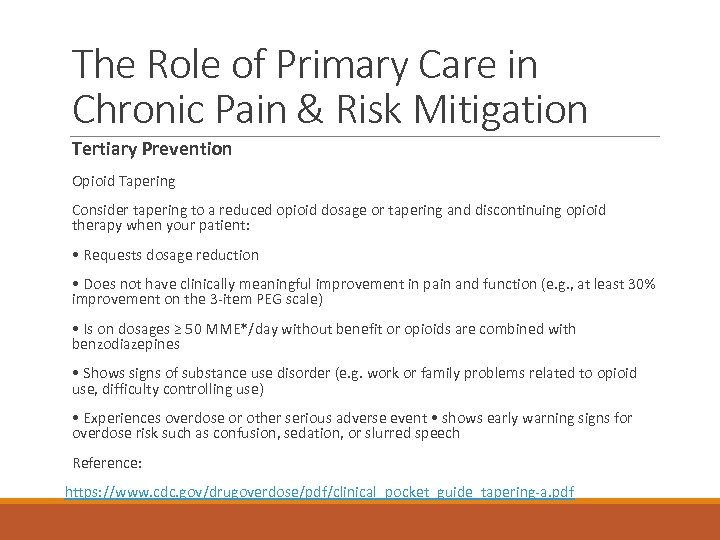
The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention Opioid Tapering Consider tapering to a reduced opioid dosage or tapering and discontinuing opioid therapy when your patient: • Requests dosage reduction • Does not have clinically meaningful improvement in pain and function (e. g. , at least 30% improvement on the 3 -item PEG scale) • Is on dosages ≥ 50 MME*/day without benefit or opioids are combined with benzodiazepines • Shows signs of substance use disorder (e. g. work or family problems related to opioid use, difficulty controlling use) • Experiences overdose or other serious adverse event • shows early warning signs for overdose risk such as confusion, sedation, or slurred speech Reference: https: //www. cdc. gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a. pdf

The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention Opioid Tapering The role of an embedded Clinical Pharmacist in tapering
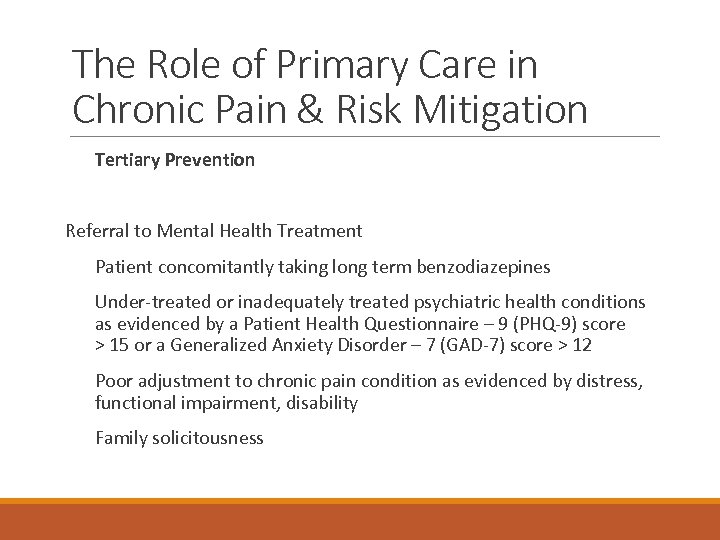
The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention Referral to Mental Health Treatment Patient concomitantly taking long term benzodiazepines Under-treated or inadequately treated psychiatric health conditions as evidenced by a Patient Health Questionnaire – 9 (PHQ-9) score > 15 or a Generalized Anxiety Disorder – 7 (GAD-7) score > 12 Poor adjustment to chronic pain condition as evidenced by distress, functional impairment, disability Family solicitousness

The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention Referral to Chemical Dependency Treatment Do you refer to medication assisted treatment or abstinence only programs?

The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention
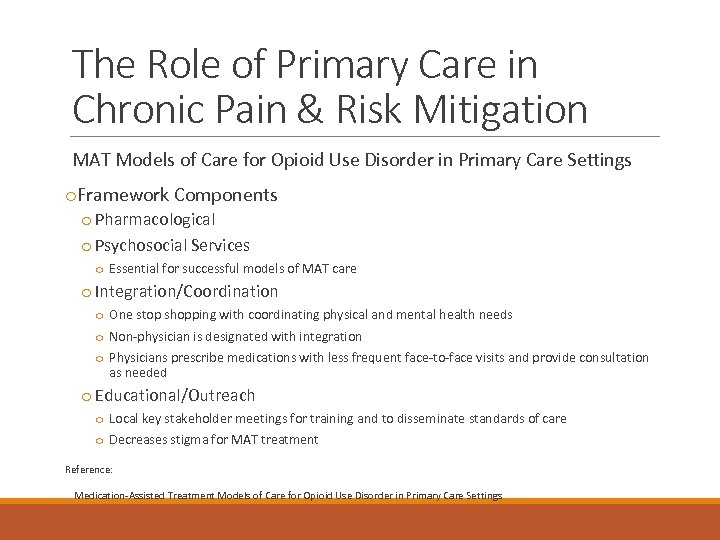
The Role of Primary Care in Chronic Pain & Risk Mitigation MAT Models of Care for Opioid Use Disorder in Primary Care Settings o. Framework Components o Pharmacological o Psychosocial Services o Essential for successful models of MAT care o Integration/Coordination o One stop shopping with coordinating physical and mental health needs o Non-physician is designated with integration o Physicians prescribe medications with less frequent face-to-face visits and provide consultation as needed o Educational/Outreach o Local key stakeholder meetings for training and to disseminate standards of care o Decreases stigma for MAT treatment Reference: Medication-Assisted Treatment Models of Care for Opioid Use Disorder in Primary Care Settings

The Role of Primary Care in Chronic Pain & Risk Mitigation MAT Models of Care for Opioid Use Disorder in Primary Care Settings o. Hub and Spoke Model o. Collaborative Opioid Prescribing Model o. Office Based Opioid Treatment o. Massachusetts Nurse Care Manager Model o. Project Extension for Community Healthcare Outcomes Reference: Medication-Assisted Treatment Models of Care for Opioid Use Disorder in Primary Care Settings

The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention o. The role of an embedded Nurse Care Coordinator (RNCC) in tracking Emergency Department utilization (ED Diversion) o Tracking ED visits: If frequent (≥ 6 x/year), activate team-based intervention o Informing PCP of suspected inappropriate utilization; possible violations of controlled substance agreement o Informing patient of the need to engage in primary care for managing chronic health conditions o Informing BHC if a patient needs behavioral health intervention to address inappropriate health care behaviors (opiate seeking) or to initiate Pain School
The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention o. The role of an embedded Community Health Educator (CHE) in managing chronic pain patients o Assisting with psychosocial barriers to engagement in health care o Discussing barriers to attending appointments (for those with frequent no-shows, late cancellations, and late arrivals) o Transportation assistance (Dial-a-ride, bus passes) o Same-day reminder calls o Insurance enrollment o Housing options o Employment resources (Vocational Rehabilitation, Temp agencies) o Food boxes/food resources o Walking Club o Weekly or bi-weekly walking group
The Role of Primary Care in Chronic Pain & Risk Mitigation Tertiary Prevention o. The role of your Electronic Health Record (EHR) in managing chronic pain patients o Are you able to easily identify and track: o Chronic pain patients in your clinic? o Chronic pain patients who are on opiates? o Chronic pain patients who are engaged with your integrated care team? o Changes in pain level and functional capacity? o Chronic pain patients who have a history of aberrant behavior? o UDS history? o Chronic pain outcome measures? o It is difficult to manage what you can’t track!

Patient Engagement

Managing Patient’s Expectations “Naïve theory” of health ◦ “I go to my PCP to get medicine for my health issues” ◦ “Pain pills [opiates] treat pain” ◦ “Why would you give me an antidepressant for pain? ” ◦ “Why would you send me to a psychologist/behavioral health specialist? ” ◦ “I’m not stressed so stress management has nothing to do with pain management” ◦ “Exercise makes my pain worse, not better” Potential sources of health (mis-)information ◦ Friends, family, television, the internet, on-line support groups, “Dr. Google”

Managing Patient’s Expectations Seeing behavioral health does not mean pain is “all in your head” “Selling” the biopsychosocial model Physician buy-in: support for the integrated care model and support for behavioral health as important component of treatment are VITAL ◦ The patient’s primary health care contact is their PCP ◦ If PCP espouses biopsychosocial intervention, patient more likely to listen ◦ Helps reduce physician-patient battle of “pills vs. skills” Administrator buy-in AND enforcement is also VITAL (or at least VERY helpful!) ◦ Who enforces policies and procedures? ◦ Who enforces utilization of the integrated care team? ◦ What does “enforcement” mean? What does it look like?

Managing Patient’s Expectations The role of insurance Insurance coverage for integrated care interventions and behavioral health is VITAL ◦ If patients have to fight insurance or pay out of pocket, makes it difficult to get patient buy-in and engagement ◦ Requires: ◦ Administrator negotiation with health insurance companies to cover Health and Behavior (H&B) CPT codes ◦ Working with your local Coordinated Care Organization to cover integrated care interventions

Expectations for Pain Patients on Opiates

Expectations for Pain Patients on Opiates Do’s Do sign the clinic pain contract/controlled substances agreement form Don’ts Do not request early refills Do provide copies of your previous medical records to verify treatment history Do not get controlled medications from other health care providers without checking with your primary care provider to make sure it is okay Do take your medications as prescribed by your health care provider Do not wait until the last minute or late in the day to request immediate refills Do complete random drug screens when requested Do not take more than one prescribed controlled medication, unless approved by your health care provider Do bring in medications for pill counts when requested Do not use other people’s medications or take non-prescribed controlled substances (including marijuana) Do keep your medications in a secure place where they will not be lost or stolen Do not yell at our front staff, medical assistants, or health care providers If your medications are stolen, Do file a police report Do not no-show appointments Do engage in non-medication treatments recommended by your health care provider or the clinic behavioral health consultant Do not late-cancel appointments (giving less than 24 -hour’s notice)

Stepped Care and Chronic Pain

Stepped Care and Chronic Pain Originated in the Veteran’s Health Administration
Stepped Care and Chronic Pain Aims ◦ ◦ Equitable access to health care for all chronic pain patients Effective use of resources Timely, cost-effective care consistent with level of patient need Implementation of routine first-line care with a gateway provider to a highly skilled interdisciplinary primary care team ◦ Detection of individuals who have responded sub-optimally
Chronic Pain & Self Management The role of self-management in complex pain management ◦ Helping patients understand: ◦ Health care providers can’t “fix” or “cure” their chronic pain ◦ Managing their chronic pain requires a collaborative effort between health care providers and the patient (and patient’s social support system) ◦ Most of pain management happens outside the medical office ◦ Patients CAN learn skills to better manage, and cope with, their pain

Chronic Pain & Self Management The role of self-management in complex pain management ◦ Barriers to patient engagement ◦ Non-opiate treatment rejecting: “It won’t help”; “only pain meds will help my pain” ◦ Low locus of control/ low self-efficacy: “health care providers need to fix me”; “there’s nothing I can do to change my pain" ◦ Time: “I don’t have time to attend classes or work on behavior change” ◦ Finances: “I can’t afford to pay for classes”

Chronic Pain & Self Management The role of self-management in complex pain management ◦ Self-management requires learning: ◦ ◦ ◦ ◦ Relaxation strategies Exercise and stretching Distraction Diverting attention away from their body Pacing oneself and taking breaks when needed Counteracting negative thinking Social engagement and effective communication Behavioral sleep management strategies

Chronic Pain & Self Management The role of self-management in complex pain management What role do physicians play in promoting patient selfmanagement? ◦ Not one and done. Requires: ◦ On-going discussion with patients ◦ On-going assessment of patient engagement in self-management
Chronic Pain & Self Management The role of self-management in complex pain management BHC’s role : ◦ Teaching providers to teach patient adherence to selfmanagement. ◦ Evidenced Based Treatment Adherence Strategies ◦ Consistency/Specificity ◦ Self Reminders ◦ Keeping Track (“What is monitored is changed”) ◦ Social Support ◦ Rewards for following through Reference: Atreja, A. , Bellam, N. Levy, S. (2005), Strategies to enhance patient adherence: making it simple, Medscape General Medicine, 7, PMC 16 g 370
Chronic Pain & Self Management The role of self-management in complex pain management ◦ Barriers to physician promotion of patient engagement in selfcare: ◦ ◦ ◦ (Listen + Patience + Celebrate) Don’t think it will change patient behavior Limited time to discuss with patient ◦ Too busy working in the medical record, placing orders, documenting Over-focus on medication prescribing as treatment strategy Approval seeking/conflict avoidance; accommodating patient ambivalence or rejection of the idea Lack of support resources or referral options

Chronic Pain Self Management: Pain School Required of all patients prescribed chronic opioid therapy for pain management Optional for any chronic pain patients not on opioid medications Pain Management Course ◦ Attendance ◦ Four 1 -hour weekly evidenced-based group interventions ◦ Designed to promote ◦ Chronic pain self management ◦ Self efficacy ◦ Health literacy regarding chronic pain
Chronic Pain Self Management: Pain School 4 -session group psychoeducational intervention: ◦ Why 4 classes? ◦ Realities of operating in the world of insurance coverage ◦ Fee for service clinic vs “closed system” or bundled payment models ◦ Each class includes: ◦ Providing information about chronic pain ◦ Working on applied skills to help patients manage their chronic pain ◦ Teaching various relaxation strategies
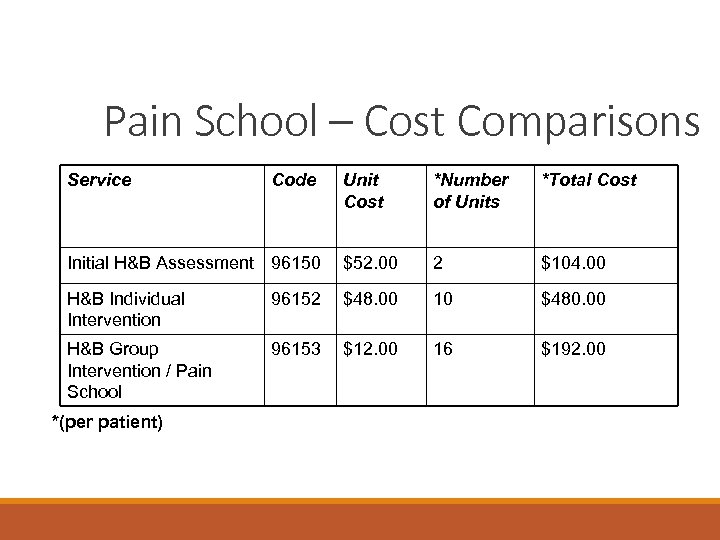
Pain School – Cost Comparisons Service Unit Cost *Number of Units *Total Cost Initial H&B Assessment 96150 $52. 00 2 $104. 00 H&B Individual Intervention 96152 $48. 00 10 $480. 00 H&B Group Intervention / Pain School 96153 $12. 00 16 $192. 00 *(per patient) Code
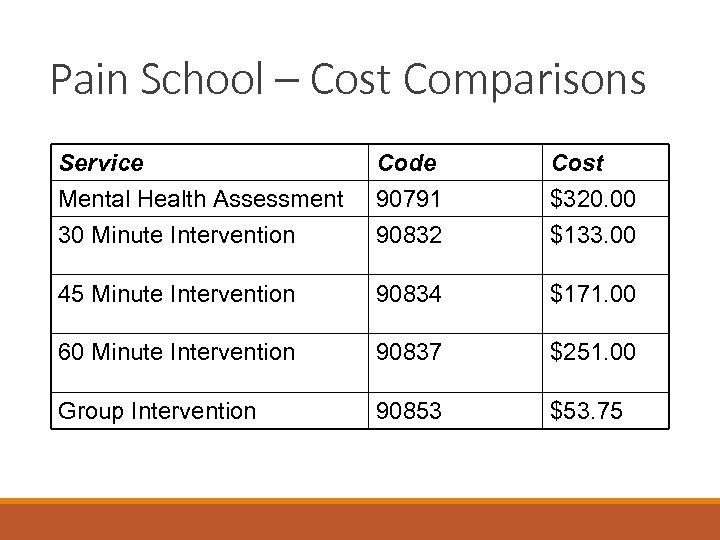
Pain School – Cost Comparisons Service Mental Health Assessment 30 Minute Intervention Code 90791 90832 Cost $320. 00 $133. 00 45 Minute Intervention 90834 $171. 00 60 Minute Intervention 90837 $251. 00 Group Intervention 90853 $53. 75

Chronic Pain Self Management: Pain School Class 1: ◦ ◦ Acute versus chronic pain Pain diary and pain scale Pacing Diaphragmatic Breathing Too little Too much

Chronic Pain Self Management: Pain School Class 2: ◦ Current theories of chronic pain (Gate Control Theory, Central Sensitization Theory) ◦ Maladaptive thinking patterns and coping strategies for addressing them ◦ Progressive Muscle Relaxation

Chronic Pain Self Management: Pain School Class 3 ◦ ◦ ◦ Interpersonal relationships Non-verbal pain behaviors Communication styles and effective communication strategies Improving patient-provider communication/interactions Pain control visualization guided imagery
Chronic Pain Self Management: Pain School Class 4 ◦ ◦ ◦ Balancing productive activities, enjoyable activities, and rest Problem-solving/Goal-setting Exercise and stretching Sleep hygiene / behavioral strategies for managing sleep Guided Imagery Providing community resources (local, websites, etc. )
Current Outcomes

Current Outcomes: Demographics and Payer Source Jan 2012 – Dec 2016 Completers 320 Age (Mean) 52 Sex (F/M) 218 / 102 Insurance Carrier BCBS = (N) Medicaid/OHP = Medicare = MODA/ODS = Self Pay = 10 162 104 10 9 Other Private Ins = 25
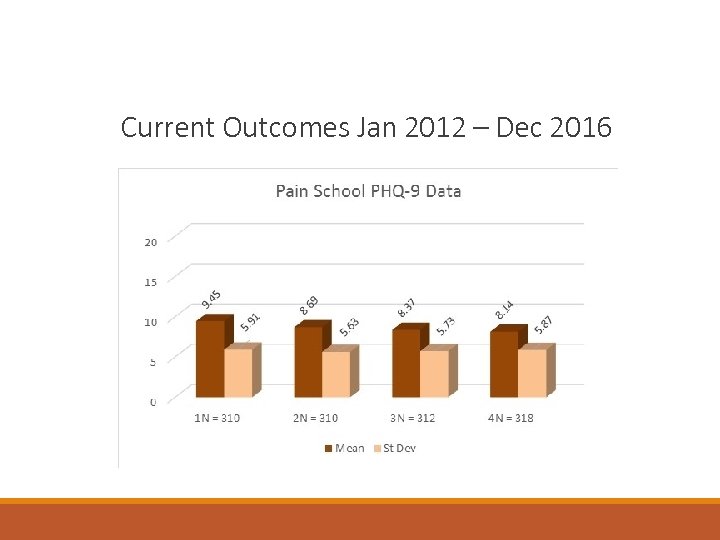
Current Outcomes Jan 2012 – Dec 2016

Current Outcomes Claims Data PCSC/OHP Date Range 1/1/20127/30/2012 N = 26 Total Costs Before First Appointment Date Total Costs after last appointment date $159, 345. 45 Savings $31, 236. 19 $128, 109. 26

Current Outcomes Anecdotal Physician Satisfaction ◦ “It is nice to have a ‘program/standard of care” ◦ “I feel less anxious about treating pain patients because I feel more supported” Physician Adherence (N = 14) ◦ Controlled substance agreement = 85% ◦ Urine Toxicology Screening = 85% ◦ Oregon Prescription Drug Monitoring Program = 85% ◦ Evaluation for Risk Stratification and Comorbidities = 64% ◦ Documentation to Best Practices = 0%
Lessons Learned
Lessons Learned Ideal intervention (described above) versus realities of practicing in a busy primary care clinic ◦ Practicing in a fee for service clinic versus capitated payment or “closed” system (like VA or university setting) EHR limitations: data collection/extraction and patient tracking difficulties; population-based health: identifying who needs treatment Expect negative impact on Press-Ganey evaluations Administrative support or lack there of? Top-down vs bottom up development/support for model
Lessons Learned Physician resistance/lack of participation ◦ Barriers: Personality style factors, conflict avoidant/need to be liked by patients, lack of time during appointments, don’t think coordinated care/BH will be helpful/alter patient behavior BHC limitations ◦ Barriers: what makes it difficult to institute the program? Personality style factors? BHC role identity: “consultant”/helper to physicians in patient care vs clinic leader/requiring physician participation ◦ Educating physicians on best practices and why we do what we do (on-going process) Exploring Your Communication Style o Complete Communication Styles Questionnaire
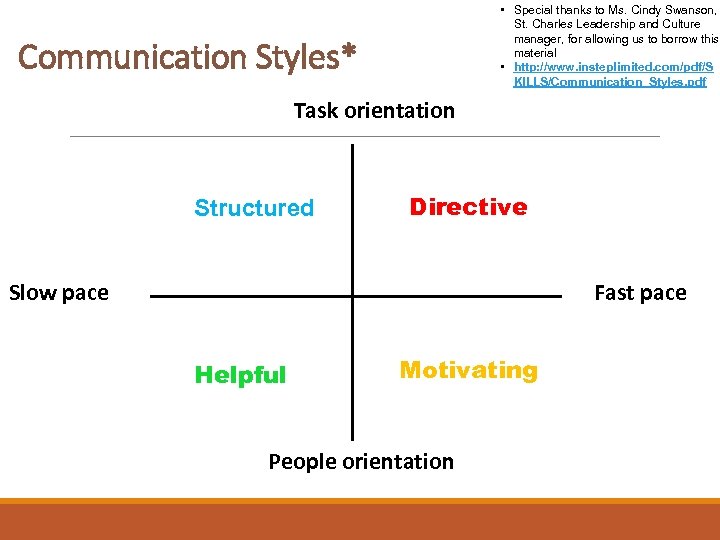
• Special thanks to Ms. Cindy Swanson, St. Charles Leadership and Culture manager, for allowing us to borrow this material • http: //www. insteplimited. com/pdf/S KILLS/Communication_Styles. pdf Communication Styles* Task orientation Structured Directive Fast pace Slow pace Helpful Motivating People orientation
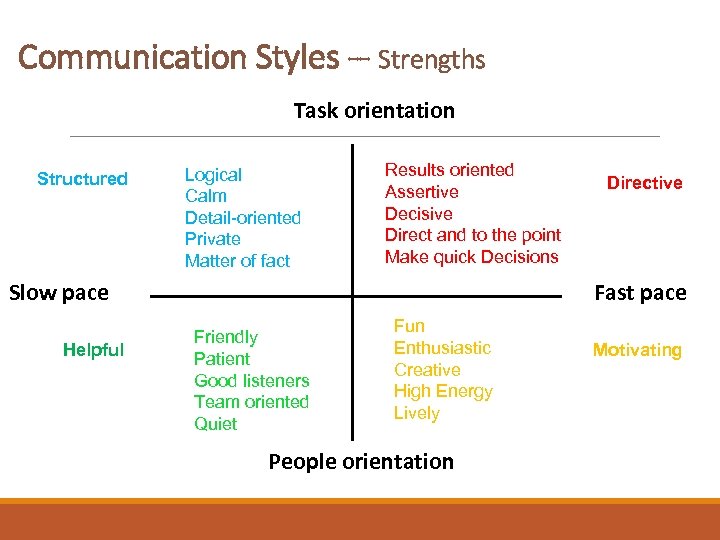
Communication Styles -- Strengths Task orientation Structured Logical Calm Detail-oriented Private Matter of fact Results oriented Assertive Decisive Direct and to the point Make quick Decisions Fast pace Slow pace Helpful Directive Friendly Patient Good listeners Team oriented Quiet Fun Enthusiastic Creative High Energy Lively People orientation Motivating

Communication Styles – Value to the team Task orientation Structured Slow pace Helpful Maintain high standards Conscientious Defines, clarifies, verifies Objective Comprehensive problem solver Dependable Work for a leader and a cause Patient & empathetic Logical thinker Service-oriented Bottom line organizer Forward-thinking Challenge-oriented Initiates activity Innovative Directive Fast pace Optimism and enthusiasm Motivating Creative problem solving Motivates others toward goals Team player Negotiates conflicts People orientation
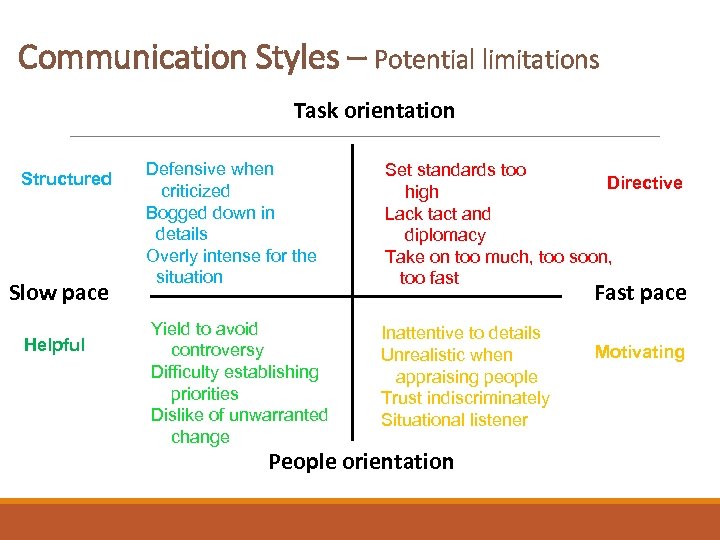
Communication Styles – Potential limitations Task orientation Structured Slow pace Helpful Defensive when criticized Bogged down in details Overly intense for the situation Set standards too Directive high Lack tact and diplomacy Take on too much, too soon, too fast Yield to avoid controversy Difficulty establishing priorities Dislike of unwarranted change Inattentive to details Unrealistic when appraising people Trust indiscriminately Situational listener Fast pace People orientation Motivating

Communication Styles – Performance under Stress Structured Task orientation Demanding Nervy Aggressive Egotistical Pessimistic Picky Fussy Overly critical Fast pace Slow pace Helpful Directive Non-demonstrative Unconcerned Hesitant Inflexible Self-promoting Overly optimistic Gabby Unrealistic People orientation Motivating
Future Directions
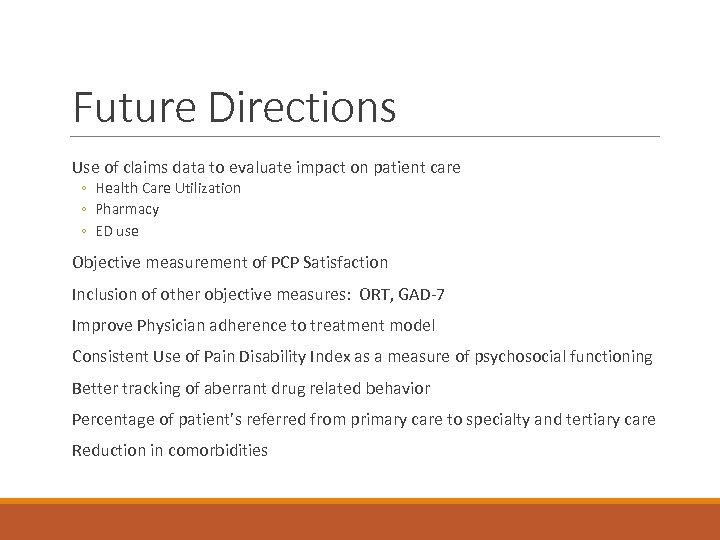
Future Directions Use of claims data to evaluate impact on patient care ◦ Health Care Utilization ◦ Pharmacy ◦ ED use Objective measurement of PCP Satisfaction Inclusion of other objective measures: ORT, GAD-7 Improve Physician adherence to treatment model Consistent Use of Pain Disability Index as a measure of psychosocial functioning Better tracking of aberrant drug related behavior Percentage of patient’s referred from primary care to specialty and tertiary care Reduction in comorbidities

Future Directions Development of secondary / follow up pain management education program ◦ Monthly expanded pain school, tied to obtaining opiate Rx for high risk patients ◦ Funding issues / Need for administrative support Patients repeating pain school? Patients following up with 1: 1 BHC intervention Expanding Pain School (more sessions? ) ◦ Adding in ACT strategies/concepts to Pain School ◦ Addressing Pain Catastrophizing in more detail (outside of current focus on cognitive distortions)
Getting Involved
Getting Involved If you are already working as embedded BHC in a primary care setting, we’d be happy to share our materials If you are in private practice, it is important that you collaborate closely with PCPs. ◦ Show me the data! Provide presentation on benefits of behavioral interventions for pain management ◦ How can you help them do their job better? ◦ How can you help make their job less frustrating? ◦ Rent office space in/near medical office/hospital ◦ Frequent contact/feedback to PCPs. No silo-ing! ◦ Assist PCPs with controlled substance policy development

Questions & Answers Thank you for your time and attention
Pain Management and Safe Opioid Therapy in Primary Care Six Building Blocks with Laura Heesacker, LCSW ØBuilding Block #1: Ø Leadership, goals, and assigned responsibilities ØBuilding Block #2: Ø Produce/revise policies, workflows, treatment agreements, and patient education materials ØBuilding Block 3: ØIdentify the patient population and develop ways to track progress ØBuilding Block 4: ØPlanned, patient-centered visits ØBuilding Block 5: ØCaring for complex patients ØBuilding Block 6: ØMeasuring Success
a933de45089e0f92f1061050b56f011d.ppt