f377a28c15fb69611e3097b2fc2d3a04.ppt
- Количество слайдов: 25
 Teaching prenatal care through group visits: learning from experience Jessica Gamboa MS 3, Jordan White MD, Sara Shields MD MS, Susanna Magee MD MPH Alpert Medical School of Brown University of Massachusetts
Teaching prenatal care through group visits: learning from experience Jessica Gamboa MS 3, Jordan White MD, Sara Shields MD MS, Susanna Magee MD MPH Alpert Medical School of Brown University of Massachusetts
 Objectives n Discuss the state of prenatal care in Family Medicine today n Describe how prenatal care is taught in residency n Describe Brown’s Group Prenatal Care Intervention n Describe UMass’ Group Prenatal Care Intervention n Future implications
Objectives n Discuss the state of prenatal care in Family Medicine today n Describe how prenatal care is taught in residency n Describe Brown’s Group Prenatal Care Intervention n Describe UMass’ Group Prenatal Care Intervention n Future implications
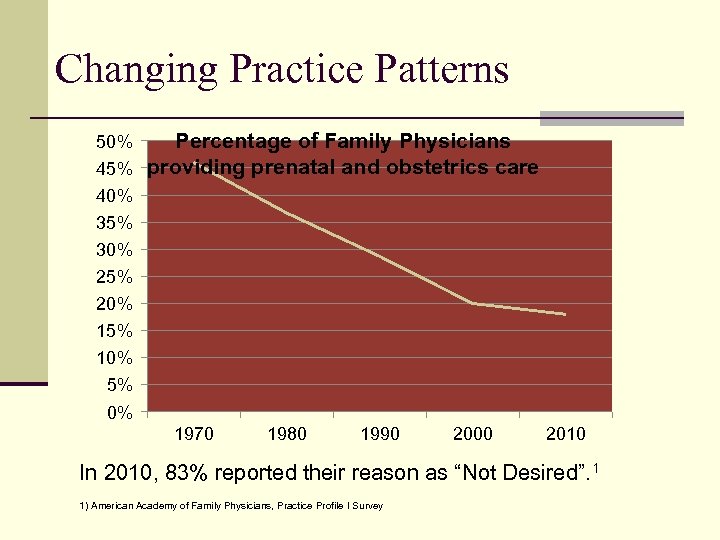 Changing Practice Patterns Percentage of Family Physicians 45% providing prenatal and obstetrics care 50% 40% 35% 30% 25% 20% 15% 10% 5% 0% 1970 1980 1990 2000 2010 In 2010, 83% reported their reason as “Not Desired”. 1 1) American Academy of Family Physicians, Practice Profile I Survey
Changing Practice Patterns Percentage of Family Physicians 45% providing prenatal and obstetrics care 50% 40% 35% 30% 25% 20% 15% 10% 5% 0% 1970 1980 1990 2000 2010 In 2010, 83% reported their reason as “Not Desired”. 1 1) American Academy of Family Physicians, Practice Profile I Survey
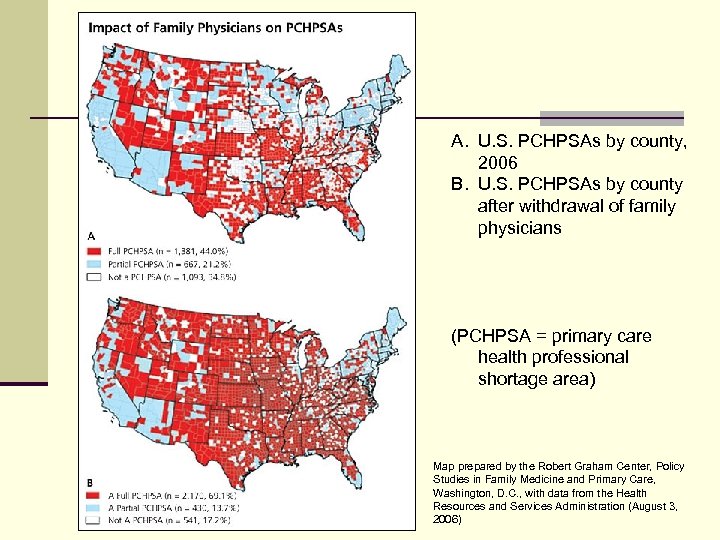 A. U. S. PCHPSAs by county, 2006 B. U. S. PCHPSAs by county after withdrawal of family physicians (PCHPSA = primary care health professional shortage area) Map prepared by the Robert Graham Center, Policy Studies in Family Medicine and Primary Care, Washington, D. C. , with data from the Health Resources and Services Administration (August 3, 2006)
A. U. S. PCHPSAs by county, 2006 B. U. S. PCHPSAs by county after withdrawal of family physicians (PCHPSA = primary care health professional shortage area) Map prepared by the Robert Graham Center, Policy Studies in Family Medicine and Primary Care, Washington, D. C. , with data from the Health Resources and Services Administration (August 3, 2006)
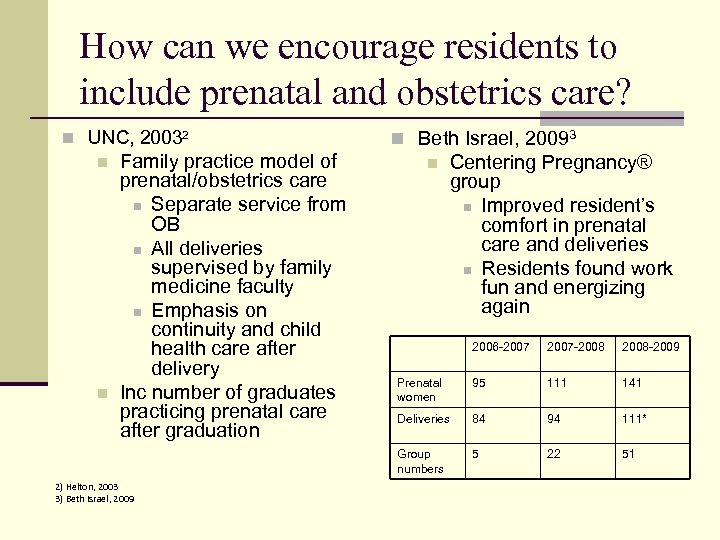 How can we encourage residents to include prenatal and obstetrics care? n UNC, 20032 n Family practice model of prenatal/obstetrics care n Separate service from OB n All deliveries supervised by family medicine faculty n Emphasis on continuity and child health care after delivery Inc number of graduates practicing prenatal care after graduation n Beth Israel, 20093 n Centering Pregnancy® group n Improved resident’s comfort in prenatal care and deliveries n Residents found work fun and energizing again 2) Helton, 2003 3) Beth Israel, 2009 2007 -2008 -2009 Prenatal women 95 111 141 Deliveries 84 94 111* Group numbers n 2006 -2007 5 22 51
How can we encourage residents to include prenatal and obstetrics care? n UNC, 20032 n Family practice model of prenatal/obstetrics care n Separate service from OB n All deliveries supervised by family medicine faculty n Emphasis on continuity and child health care after delivery Inc number of graduates practicing prenatal care after graduation n Beth Israel, 20093 n Centering Pregnancy® group n Improved resident’s comfort in prenatal care and deliveries n Residents found work fun and energizing again 2) Helton, 2003 3) Beth Israel, 2009 2007 -2008 -2009 Prenatal women 95 111 141 Deliveries 84 94 111* Group numbers n 2006 -2007 5 22 51
 Why group care? n Successfully implemented in over 100 sites 4 n Increased patient-provider time n Facilitative vs. didactic teaching n Patient-centered care n Associated with positive outcomes n Increased birth weight n Increased gestational age at delivery n Increased rate of breastfeeding n Better satisfaction with care 4) Baldwin, 2006
Why group care? n Successfully implemented in over 100 sites 4 n Increased patient-provider time n Facilitative vs. didactic teaching n Patient-centered care n Associated with positive outcomes n Increased birth weight n Increased gestational age at delivery n Increased rate of breastfeeding n Better satisfaction with care 4) Baldwin, 2006
 How can residents benefit from group care? n Increase fund of knowledge on basic prenatal care topics n Learn common concerns and questions during pregnancy n Improve confidence in caring for prenatal women n Provide more opportunities for practicing prenatal care
How can residents benefit from group care? n Increase fund of knowledge on basic prenatal care topics n Learn common concerns and questions during pregnancy n Improve confidence in caring for prenatal women n Provide more opportunities for practicing prenatal care
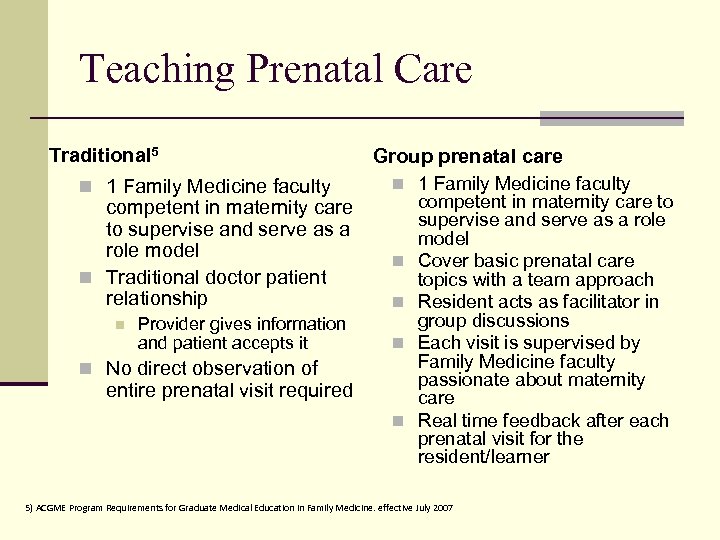 Teaching Prenatal Care Traditional 5 n 1 Family Medicine faculty competent in maternity care to supervise and serve as a role model n Traditional doctor patient relationship n Provider gives information and patient accepts it Group prenatal care n 1 Family Medicine faculty n n No direct observation of entire prenatal visit required n competent in maternity care to supervise and serve as a role model Cover basic prenatal care topics with a team approach Resident acts as facilitator in group discussions Each visit is supervised by Family Medicine faculty passionate about maternity care Real time feedback after each prenatal visit for the resident/learner 5) ACGME Program Requirements for Graduate Medical Education in Family Medicine. effective July 2007
Teaching Prenatal Care Traditional 5 n 1 Family Medicine faculty competent in maternity care to supervise and serve as a role model n Traditional doctor patient relationship n Provider gives information and patient accepts it Group prenatal care n 1 Family Medicine faculty n n No direct observation of entire prenatal visit required n competent in maternity care to supervise and serve as a role model Cover basic prenatal care topics with a team approach Resident acts as facilitator in group discussions Each visit is supervised by Family Medicine faculty passionate about maternity care Real time feedback after each prenatal visit for the resident/learner 5) ACGME Program Requirements for Graduate Medical Education in Family Medicine. effective July 2007
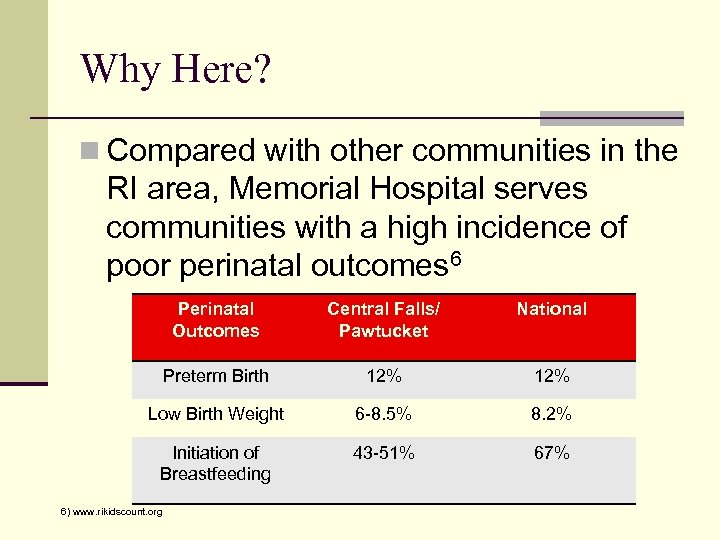 Why Here? n Compared with other communities in the RI area, Memorial Hospital serves communities with a high incidence of poor perinatal outcomes 6 Perinatal Outcomes Central Falls/ Pawtucket National Preterm Birth 12% Low Birth Weight 6 -8. 5% 8. 2% Initiation of Breastfeeding 43 -51% 67% 6) www. rikidscount. org
Why Here? n Compared with other communities in the RI area, Memorial Hospital serves communities with a high incidence of poor perinatal outcomes 6 Perinatal Outcomes Central Falls/ Pawtucket National Preterm Birth 12% Low Birth Weight 6 -8. 5% 8. 2% Initiation of Breastfeeding 43 -51% 67% 6) www. rikidscount. org
 Brown’s Pilot Program n 3 Family Medicine resident facilitators- (2)PGY-1 and (1) PGY-2 n Women recruited by residents, nurses and faculty with posters/brochures placed in waiting rooms n Attempts to recruit 8 -10 women n Age 18+ n Similar gestational ages at presentation n Goal: diversity in terms of racial and ethnic background, G/P, family dynamic, etc. n Supported by one faculty member trained in Maternal Child Health, one fellow in Preventive Medicine and third year medical student.
Brown’s Pilot Program n 3 Family Medicine resident facilitators- (2)PGY-1 and (1) PGY-2 n Women recruited by residents, nurses and faculty with posters/brochures placed in waiting rooms n Attempts to recruit 8 -10 women n Age 18+ n Similar gestational ages at presentation n Goal: diversity in terms of racial and ethnic background, G/P, family dynamic, etc. n Supported by one faculty member trained in Maternal Child Health, one fellow in Preventive Medicine and third year medical student.
 Brown’s Pilot Program n Of 5 women agreeing to participate, 4 women participated n n Ages 21 -33 GA at first visit from 12 -28 weeks G 1 P 0 to G 5 P 4 2 women included their partners in the group
Brown’s Pilot Program n Of 5 women agreeing to participate, 4 women participated n n Ages 21 -33 GA at first visit from 12 -28 weeks G 1 P 0 to G 5 P 4 2 women included their partners in the group
 Brown’s Pilot Program n 5 monthly sessions, supplemented by individual visits with their PCP n Residents rotated as the facilitator for group discussion on various topics n Diet, exercise, common complaints of pregnancy, infant care, and labor/pain management n Preparation for group visits and follow up visits scheduled by Dr. White as well as monthly chart review
Brown’s Pilot Program n 5 monthly sessions, supplemented by individual visits with their PCP n Residents rotated as the facilitator for group discussion on various topics n Diet, exercise, common complaints of pregnancy, infant care, and labor/pain management n Preparation for group visits and follow up visits scheduled by Dr. White as well as monthly chart review
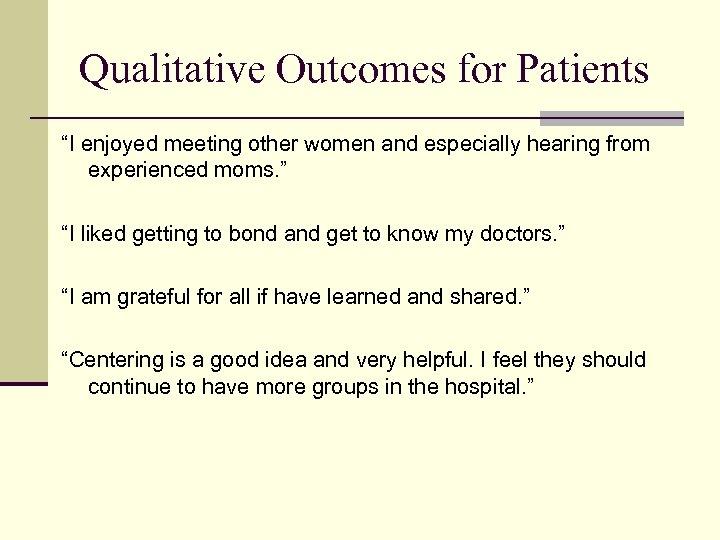 Qualitative Outcomes for Patients “I enjoyed meeting other women and especially hearing from experienced moms. ” “I liked getting to bond and get to know my doctors. ” “I am grateful for all if have learned and shared. ” “Centering is a good idea and very helpful. I feel they should continue to have more groups in the hospital. ”
Qualitative Outcomes for Patients “I enjoyed meeting other women and especially hearing from experienced moms. ” “I liked getting to bond and get to know my doctors. ” “I am grateful for all if have learned and shared. ” “Centering is a good idea and very helpful. I feel they should continue to have more groups in the hospital. ”
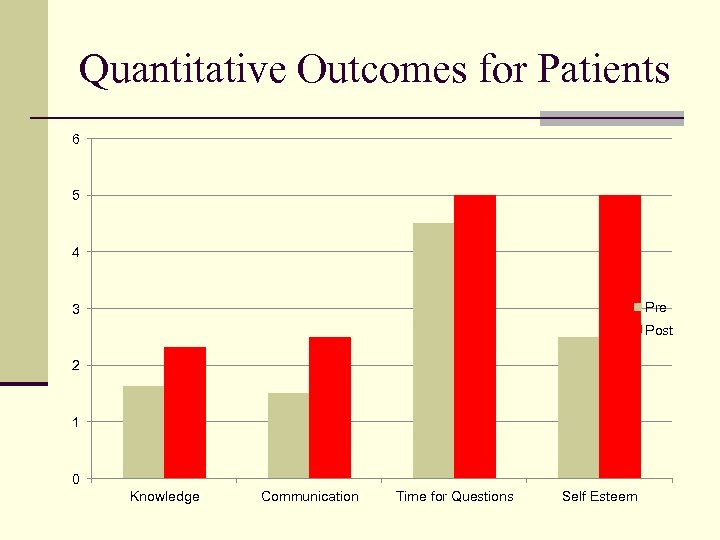 Quantitative Outcomes for Patients 6 5 4 Pre 3 Post 2 1 0 Knowledge Communication Time for Questions Self Esteem
Quantitative Outcomes for Patients 6 5 4 Pre 3 Post 2 1 0 Knowledge Communication Time for Questions Self Esteem
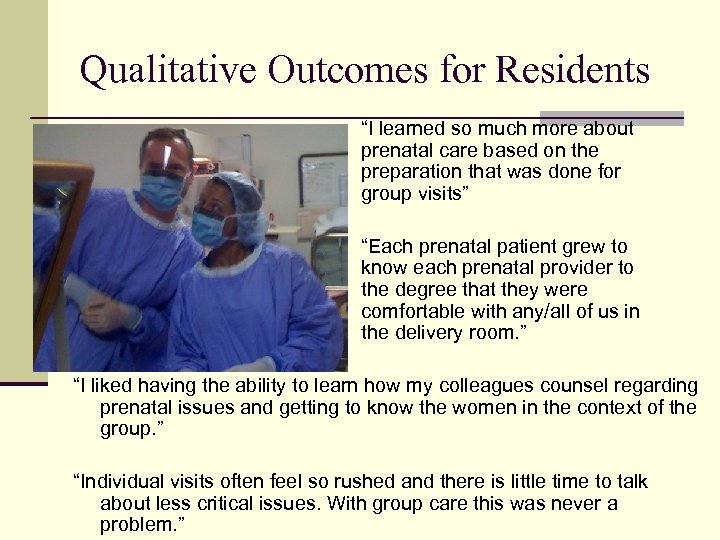 Qualitative Outcomes for Residents “I learned so much more about prenatal care based on the preparation that was done for group visits” “Each prenatal patient grew to know each prenatal provider to the degree that they were comfortable with any/all of us in the delivery room. ” “I liked having the ability to learn how my colleagues counsel regarding prenatal issues and getting to know the women in the context of the group. ” “Individual visits often feel so rushed and there is little time to talk about less critical issues. With group care this was never a problem. ”
Qualitative Outcomes for Residents “I learned so much more about prenatal care based on the preparation that was done for group visits” “Each prenatal patient grew to know each prenatal provider to the degree that they were comfortable with any/all of us in the delivery room. ” “I liked having the ability to learn how my colleagues counsel regarding prenatal issues and getting to know the women in the context of the group. ” “Individual visits often feel so rushed and there is little time to talk about less critical issues. With group care this was never a problem. ”
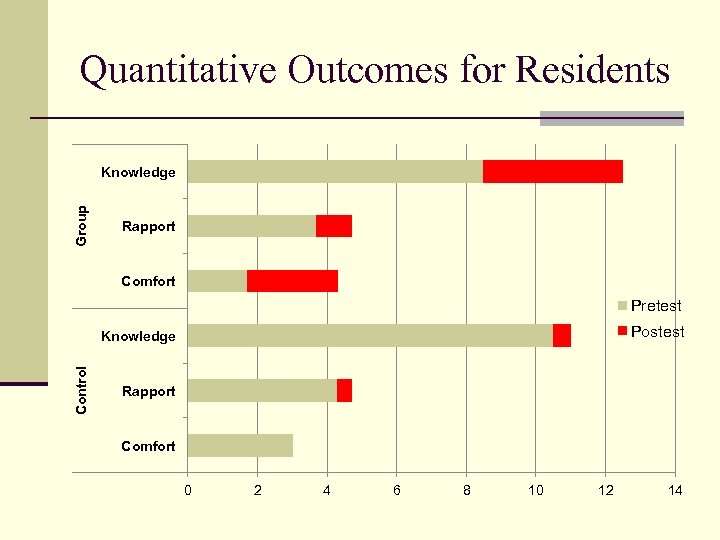 Quantitative Outcomes for Residents Group Knowledge Rapport Comfort Pretest Postest Control Knowledge Rapport Comfort 0 2 4 6 8 10 12 14
Quantitative Outcomes for Residents Group Knowledge Rapport Comfort Pretest Postest Control Knowledge Rapport Comfort 0 2 4 6 8 10 12 14
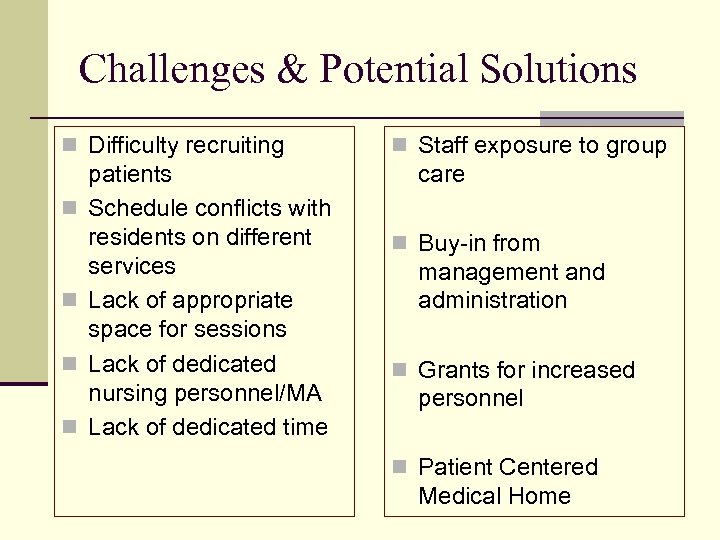 Challenges & Potential Solutions n Difficulty recruiting n n patients Schedule conflicts with residents on different services Lack of appropriate space for sessions Lack of dedicated nursing personnel/MA Lack of dedicated time n Staff exposure to group care n Buy-in from management and administration n Grants for increased personnel n Patient Centered Medical Home
Challenges & Potential Solutions n Difficulty recruiting n n patients Schedule conflicts with residents on different services Lack of appropriate space for sessions Lack of dedicated nursing personnel/MA Lack of dedicated time n Staff exposure to group care n Buy-in from management and administration n Grants for increased personnel n Patient Centered Medical Home
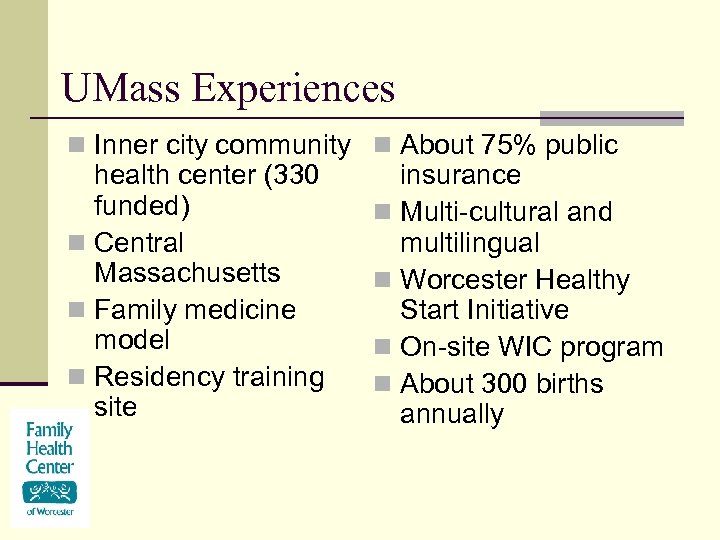 UMass Experiences n Inner city community n About 75% public health center (330 funded) n Central Massachusetts n Family medicine model n Residency training site insurance n Multi-cultural and multilingual n Worcester Healthy Start Initiative n On-site WIC program n About 300 births annually
UMass Experiences n Inner city community n About 75% public health center (330 funded) n Central Massachusetts n Family medicine model n Residency training site insurance n Multi-cultural and multilingual n Worcester Healthy Start Initiative n On-site WIC program n About 300 births annually
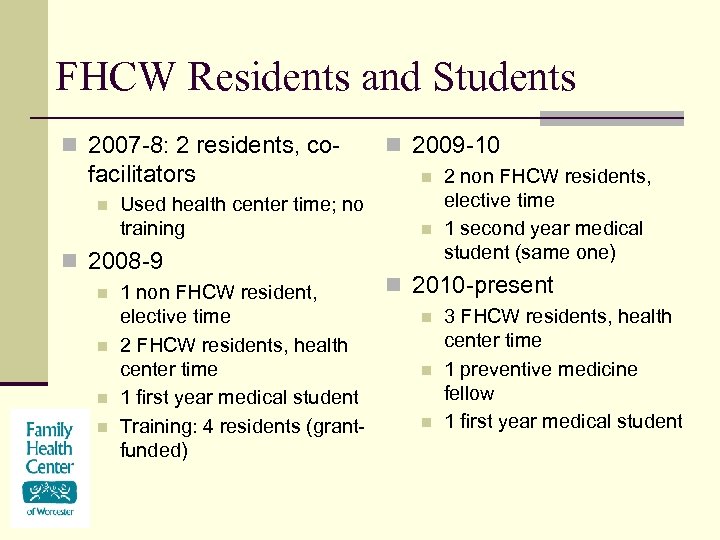 FHCW Residents and Students n 2007 -8: 2 residents, co- facilitators n Used health center time; no training n 2008 -9 n n 1 non FHCW resident, elective time 2 FHCW residents, health center time 1 first year medical student Training: 4 residents (grantfunded) n 2009 -10 n n 2 non FHCW residents, elective time 1 second year medical student (same one) n 2010 -present n n n 3 FHCW residents, health center time 1 preventive medicine fellow 1 first year medical student
FHCW Residents and Students n 2007 -8: 2 residents, co- facilitators n Used health center time; no training n 2008 -9 n n 1 non FHCW resident, elective time 2 FHCW residents, health center time 1 first year medical student Training: 4 residents (grantfunded) n 2009 -10 n n 2 non FHCW residents, elective time 1 second year medical student (same one) n 2010 -present n n n 3 FHCW residents, health center time 1 preventive medicine fellow 1 first year medical student
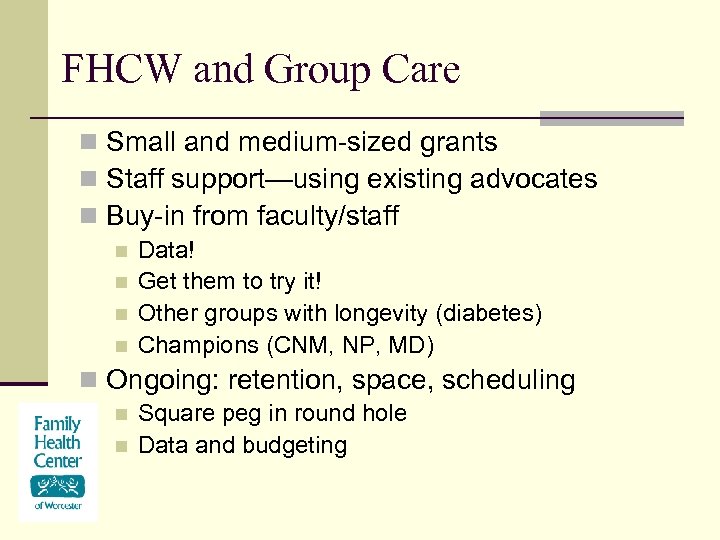 FHCW and Group Care n Small and medium-sized grants n Staff support—using existing advocates n Buy-in from faculty/staff n n Data! Get them to try it! Other groups with longevity (diabetes) Champions (CNM, NP, MD) n Ongoing: retention, space, scheduling n n Square peg in round hole Data and budgeting
FHCW and Group Care n Small and medium-sized grants n Staff support—using existing advocates n Buy-in from faculty/staff n n Data! Get them to try it! Other groups with longevity (diabetes) Champions (CNM, NP, MD) n Ongoing: retention, space, scheduling n n Square peg in round hole Data and budgeting
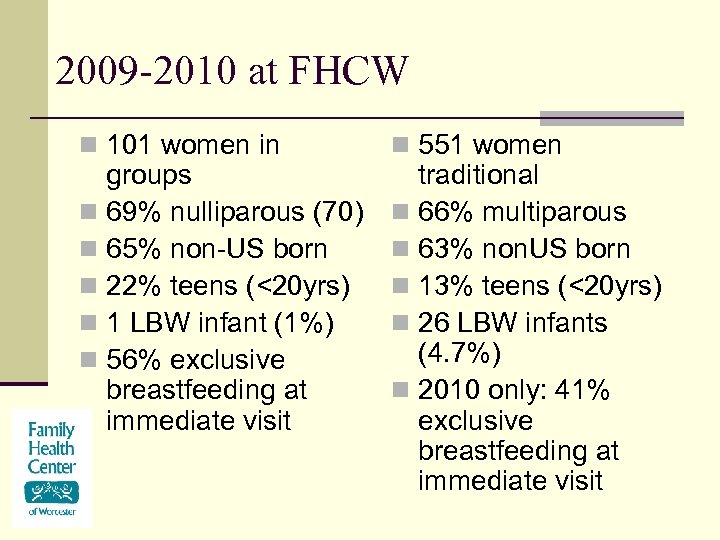 2009 -2010 at FHCW n 101 women in groups n 69% nulliparous (70) n 65% non-US born n 22% teens (<20 yrs) n 1 LBW infant (1%) n 56% exclusive breastfeeding at immediate visit n 551 women traditional n 66% multiparous n 63% non. US born n 13% teens (<20 yrs) n 26 LBW infants (4. 7%) n 2010 only: 41% exclusive breastfeeding at immediate visit
2009 -2010 at FHCW n 101 women in groups n 69% nulliparous (70) n 65% non-US born n 22% teens (<20 yrs) n 1 LBW infant (1%) n 56% exclusive breastfeeding at immediate visit n 551 women traditional n 66% multiparous n 63% non. US born n 13% teens (<20 yrs) n 26 LBW infants (4. 7%) n 2010 only: 41% exclusive breastfeeding at immediate visit
 The Future n Can group prenatal care be a tool to increase the number of graduating residents including prenatal care in their practice? Comfort n Knowledge n Empowerment n Experience n
The Future n Can group prenatal care be a tool to increase the number of graduating residents including prenatal care in their practice? Comfort n Knowledge n Empowerment n Experience n
 Acknowledgements n Women’s Reproductive Health Freedom and Rights Scholarly Concentration and the Braufman Fund at Brown University
Acknowledgements n Women’s Reproductive Health Freedom and Rights Scholarly Concentration and the Braufman Fund at Brown University
 References ACGME Program Requirements for Graduate Medical Education in Family Medicine. effective July 2007 Baldwin, Karen Comparison of Selected Outcomes of Centering Pregnancy versus Traditional Prenatal Care Journal of Midwifery and Women’s Health 51 (2006): 266272 Barr, Wendy Using Centering Pregnancy to Teach Prenatal Care: Implementing Group Prenatal Care in a Family Medicine Residency. Beth Israel Residency in Urban Family Medicine presentation: 2009 Dresden, Graham et al Influence of Obstetrics Practice on Workload and Practice Patterns of Family Medicine Physicians and Obstetrician-Gynecologists Ann Fam Med 2008; 6(suppl 1): s 5 -s 11 Helton, Margaret MD et al A Maternal and Child Health Curriculum for Family Practice Residents: Results of an Intervention at University of North Carolina Fam Med 2003; 35(3): 174 -180 Robert Graham Center, Policy Studies in Family Medicine and Primary Care, Washington, D. C. , with data from the Health Resources and Services Administration (August 3, 2006) Ringdahl, Erika MD et al Changing Practice Patterns of Family Medicine Graduates: A Comparison of Alumni Surveys from 1998 -2004 J Am Board FM 2006; 19: 404 -412 Rhode Island Kids Count http: //www. rikidscount. org
References ACGME Program Requirements for Graduate Medical Education in Family Medicine. effective July 2007 Baldwin, Karen Comparison of Selected Outcomes of Centering Pregnancy versus Traditional Prenatal Care Journal of Midwifery and Women’s Health 51 (2006): 266272 Barr, Wendy Using Centering Pregnancy to Teach Prenatal Care: Implementing Group Prenatal Care in a Family Medicine Residency. Beth Israel Residency in Urban Family Medicine presentation: 2009 Dresden, Graham et al Influence of Obstetrics Practice on Workload and Practice Patterns of Family Medicine Physicians and Obstetrician-Gynecologists Ann Fam Med 2008; 6(suppl 1): s 5 -s 11 Helton, Margaret MD et al A Maternal and Child Health Curriculum for Family Practice Residents: Results of an Intervention at University of North Carolina Fam Med 2003; 35(3): 174 -180 Robert Graham Center, Policy Studies in Family Medicine and Primary Care, Washington, D. C. , with data from the Health Resources and Services Administration (August 3, 2006) Ringdahl, Erika MD et al Changing Practice Patterns of Family Medicine Graduates: A Comparison of Alumni Surveys from 1998 -2004 J Am Board FM 2006; 19: 404 -412 Rhode Island Kids Count http: //www. rikidscount. org
 Questions?
Questions?


