TB treatment.pptx
- Количество слайдов: 48
TB treatment by Konrad T Juszkiewicz, MD, MPH Donald Burgess, Ph. D DRK Biomedical Research and Development LLC Almaty, December, 2013 1
Fundamental Responsibility and Approach in TB Treatment Assure that appropriate regimen is prescribed Ensure successful completion of therapy (adherence) Utilize directly observed therapy (DOT) as standard-of-care
Aims in Treatment To cure the patient of TB To prevent death from active TB or its late effects To prevent relapse of TB To decrease transmission of TB to others
Adherence Non adherence is a major problem in TB control • Patient education is the most effective • tool to prevent default • Use case management and directly • observed therapy (DOT) to ensure • patients complete treatment
Why Do Patients Default? As their condition improves they may feel better and decide they don’t need meds They may experience side effects Forgetfulness/lack of a reminder! Travel to cattle posts without refills Difficulty getting to clinic b/c of work/distance
What is Case Management? • Assignment of responsibility within • clinic to oversee patient monitoring -bacteriology -DOT -side effects • Systematic regular review of patient • data • Plans in place to address barriers to • adherence before default occurs
Directly Observed Therapy (DOT) • Health care worker watches patient • swallow each -Dose of medication -Every pill, every day -Self-administered is NOT DOT REMEMBER DOT for all patients on all regimens NO exceptions
Factors Guiding Treatment Initiation Epidemiologic information ◦ e. g. , circulating strains, resistance patterns Clinical, pathological, chest x-ray findings Microscopic examination of acid-fast bacilli (AFB) in sputum smears Culture and drug resistance results
Basic Principles of Treatment Ø Provide safest, most effective therapy in shortest time • Multiple drugs to which the organisms are susceptible • Never add single drug to failing regimen • Ensure adherence to therapy (DOT) • Determine the patient’s HIV status- this could save their life!
Main Activities of Anti-TB Drugs: Early bactericidal activity – ◦ the ability of a drug to decrease the number of tubercle bacilli in sputum during the initial period of therapy in actively multiplying subpopulations (= fast decrease of bacterial load) Sterilizing activity – ◦ the ability to eliminate or substantially decrease the numberof bacilli in (semi) dormant subpopulations (= ultimate elimination of all bacilli)
Anti-TB Drugs Mechanisms of Action Rifampicin A bactericidal drug active against ALL populations of TB bacilli Semi-synthetic, macrocyclic antibiotic inhibiting nucleic acid synthesis Potent bactericidal action and potent sterilizing effect against tubercle bacilli
Anti-TB Drugs Mechanisms of Action Isoniazid A bactericidal drug active against ALL populations of TB bacilli Highly bactericidal against replicating tubercle bacilli Kills 90% during first few days of treatment
Anti-TB Drugs Mechanisms of Action Pyrazinamide A bactericidal drug active against certain populations of TB bacilli Particularly active in acid intra-cellular environment and in areas of acute inflammation Active in acid environment against bacilli inside macrophages Synthetic analogue of nicotinamide with weak bactericidal, but potent sterilizing activity against M. tuberculosis
Anti-TB Drugs Mechanisms of Action Streptomycin A bactericidal drug active against certain populations of TB bacilli Active against rapidly multiplying extracellular TB bacilli
Anti-TB Drugs Mechanisms of Action Ethambutol A synthetic, bacteriostatic drug active against M. tuberculosis and other mycobacteria Used in combination with other more powerful drugs to prevent emergence of resistant bacilli
Rifampicin (R) Forms- 150 mg and 300 mg capsules Administration remarks ◦ Must always be administered in combination withother anti-mycobacterial agents ◦ Should be given at least 30 minutes before meals, since absorption is reduced when taken with food
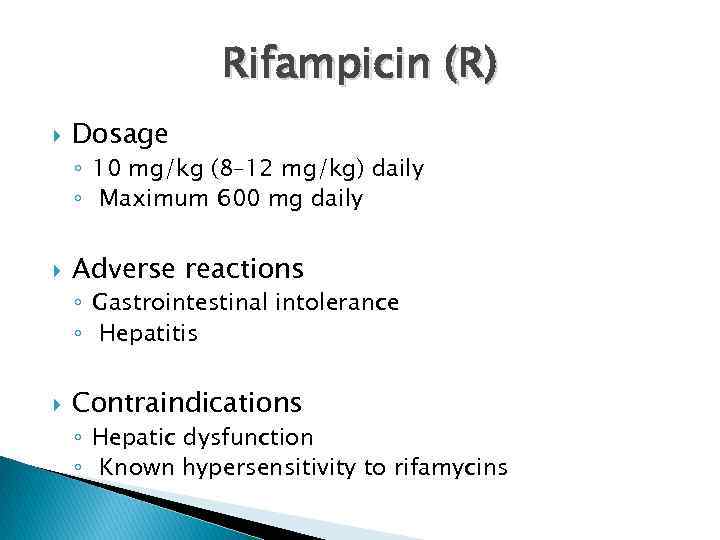
Rifampicin (R) Dosage ◦ 10 mg/kg (8– 12 mg/kg) daily ◦ Maximum 600 mg daily Adverse reactions ◦ Gastrointestinal intolerance ◦ Hepatitis Contraindications ◦ Hepatic dysfunction ◦ Known hypersensitivity to rifamycins
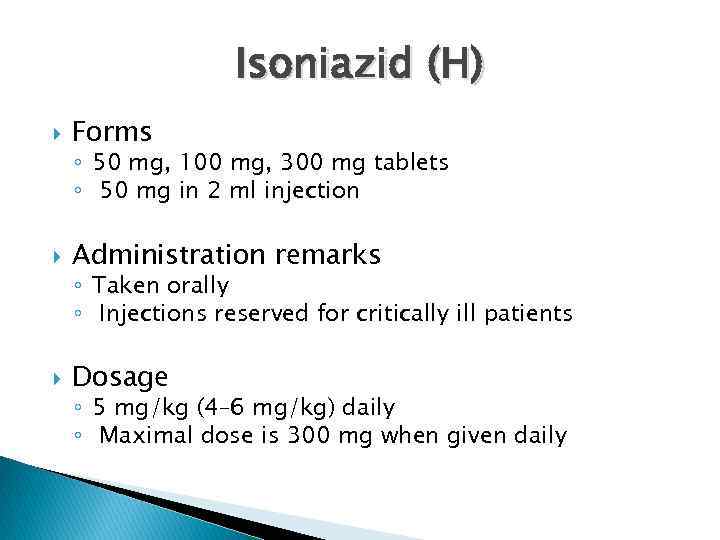
Isoniazid (H) Forms ◦ 50 mg, 100 mg, 300 mg tablets ◦ 50 mg in 2 ml injection Administration remarks ◦ Taken orally ◦ Injections reserved for critically ill patients Dosage ◦ 5 mg/kg (4– 6 mg/kg) daily ◦ Maximal dose is 300 mg when given daily
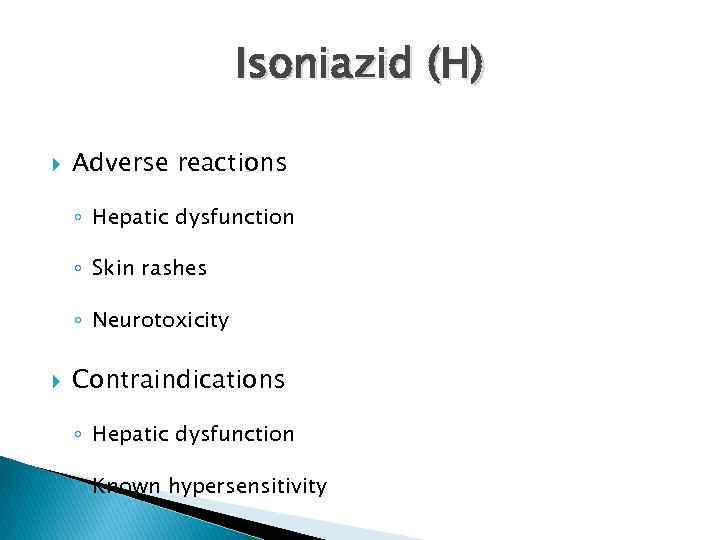
Isoniazid (H) Adverse reactions ◦ Hepatic dysfunction ◦ Skin rashes ◦ Neurotoxicity Contraindications ◦ Hepatic dysfunction ◦ Known hypersensitivity
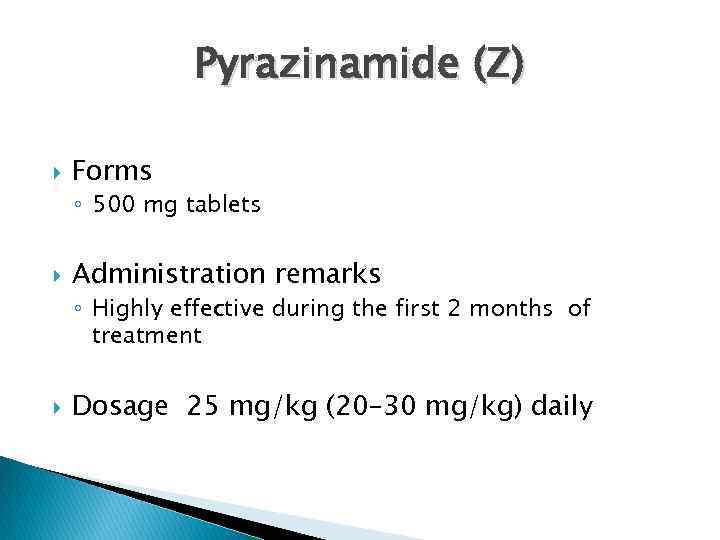
Pyrazinamide (Z) Forms ◦ 500 mg tablets Administration remarks ◦ Highly effective during the first 2 months of treatment Dosage 25 mg/kg (20– 30 mg/kg) daily
Pyrazinamide (Z) Adverse reactions ◦ Hepatitis ◦ Hyperuricaemia ◦ Rash Contraindications ◦ Hepatic dysfunction ◦ Known hypersensitivity
Streptomycin (S) Forms ◦ 1. 0 g ampoule injections Administration remarks ◦ Streptomycin is an aminoglicoside antibiotic withbactericidal activity against TB bacilli Dosage ◦ 15 mg/kg (12– 18 mg/kg) daily ◦ In patients over age 60, 500 -750 mg daily
Streptomycin (S) Adverse reactions ◦ Vestibular damage ◦ Hypersensitivity ◦ Nephrotoxicity Contraindications ◦ ◦ ◦ Pre-existing auditory nerve impairment Renal impairment Myasthenia gravis Pregnancy Known hypersensitivity
Ethambutol (E) Forms ◦ 100 mg, 250 mg, 400 mg tablets Administration remarks ◦ Used in combination with other anti-TB drugs to prevent the emergence of resistant strains Dosage ◦ 15 mg/kg (15 -20 mg/kg) daily
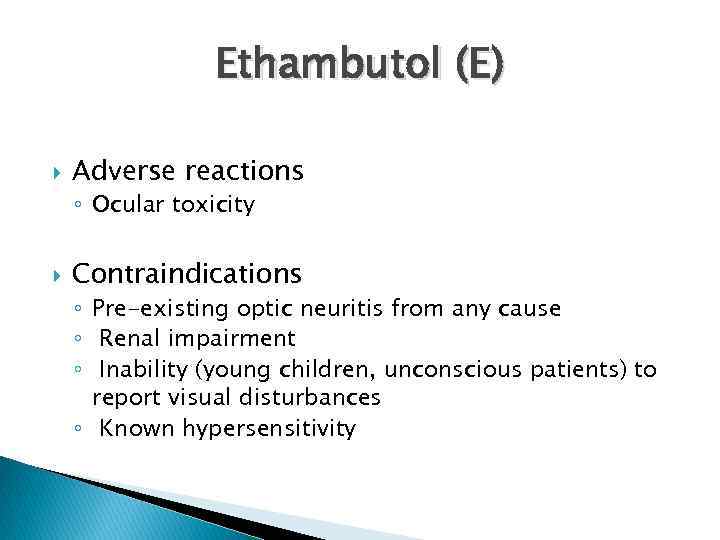
Ethambutol (E) Adverse reactions ◦ Ocular toxicity Contraindications ◦ Pre-existing optic neuritis from any cause ◦ Renal impairment ◦ Inability (young children, unconscious patients) to report visual disturbances ◦ Known hypersensitivity
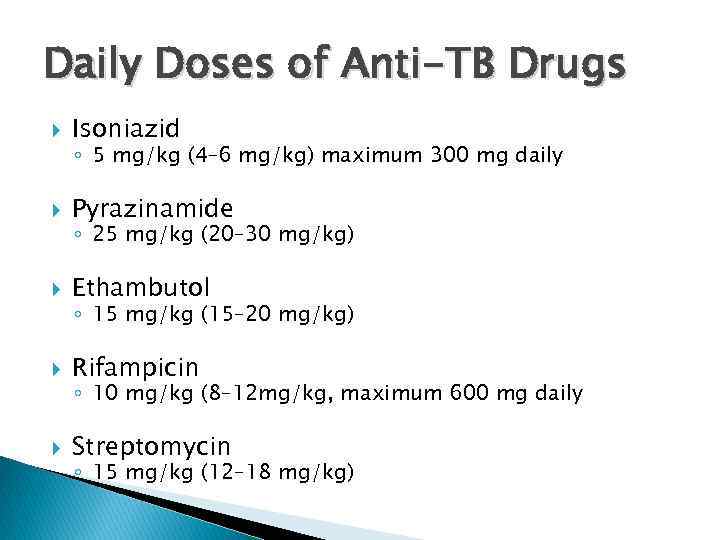
Daily Doses of Anti-TB Drugs Isoniazid Pyrazinamide Ethambutol Rifampicin Streptomycin ◦ 5 mg/kg (4– 6 mg/kg) maximum 300 mg daily ◦ 25 mg/kg (20– 30 mg/kg) ◦ 15 mg/kg (15– 20 mg/kg) ◦ 10 mg/kg (8– 12 mg/kg, maximum 600 mg daily ◦ 15 mg/kg (12– 18 mg/kg)
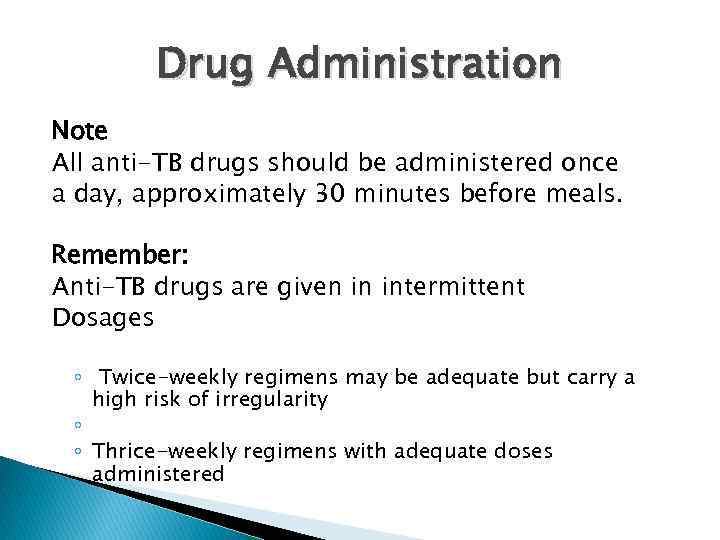
Drug Administration Note All anti-TB drugs should be administered once a day, approximately 30 minutes before meals. Remember: Anti-TB drugs are given in intermittent Dosages ◦ Twice-weekly regimens may be adequate but carry a high risk of irregularity ◦ ◦ Thrice-weekly regimens with adequate doses administered
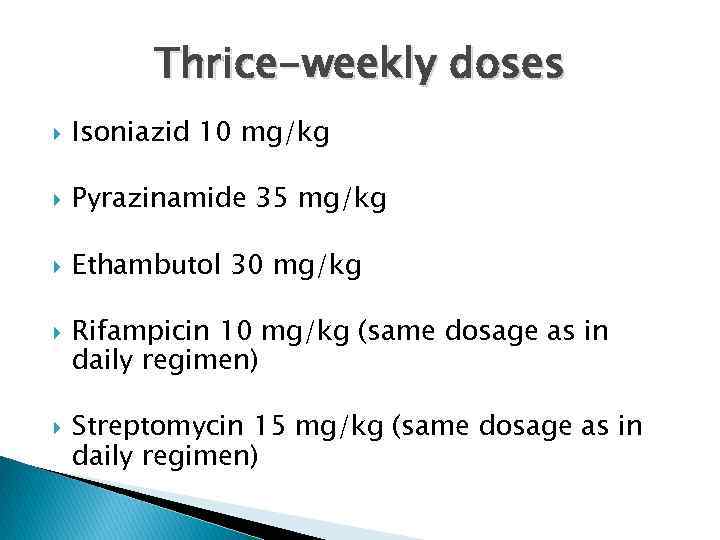
Thrice-weekly doses Isoniazid 10 mg/kg Pyrazinamide 35 mg/kg Ethambutol 30 mg/kg Rifampicin 10 mg/kg (same dosage as in daily regimen) Streptomycin 15 mg/kg (same dosage as in daily regimen)
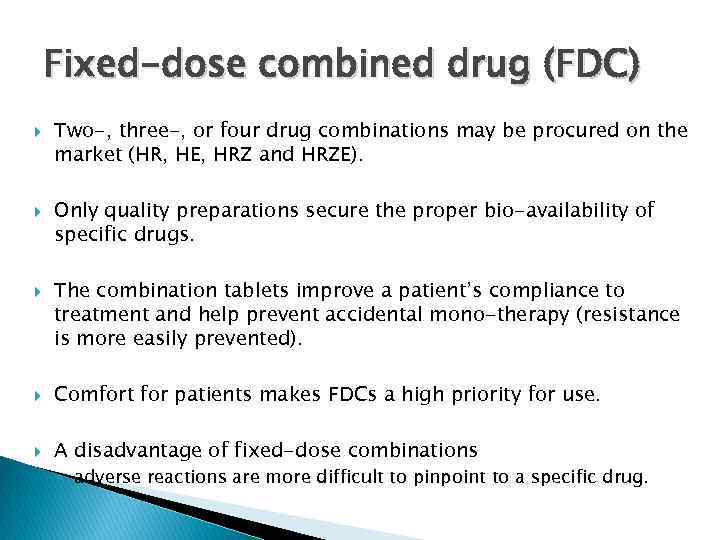
Fixed-dose combined drug (FDC) Two-, three-, or four drug combinations may be procured on the market (HR, HE, HRZ and HRZE). Only quality preparations secure the proper bio-availability of specific drugs. The combination tablets improve a patient’s compliance to treatment and help prevent accidental mono-therapy (resistance is more easily prevented). Comfort for patients makes FDCs a high priority for use. A disadvantage of fixed-dose combinations ◦ adverse reactions are more difficult to pinpoint to a specific drug.
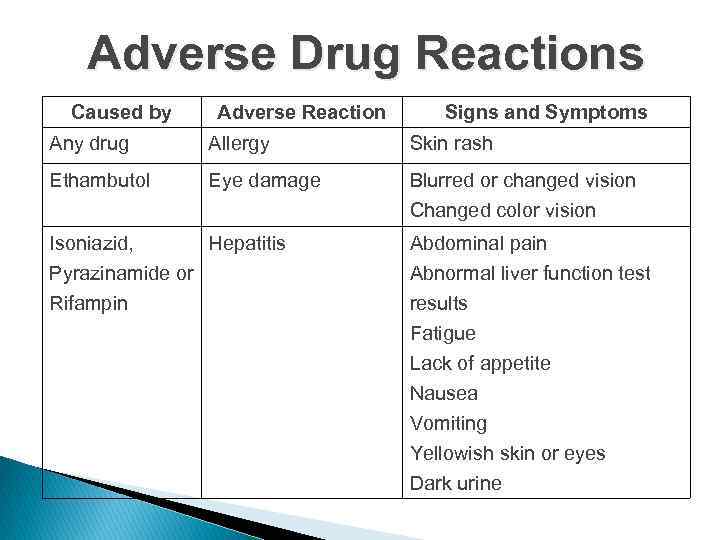
Adverse Drug Reactions Caused by Adverse Reaction Signs and Symptoms Any drug Allergy Skin rash Ethambutol Eye damage Blurred or changed vision Changed color vision Isoniazid, Hepatitis Pyrazinamide or Abdominal pain Abnormal liver function test Rifampin results Fatigue Lack of appetite Nausea Vomiting Yellowish skin or eyes Dark urine
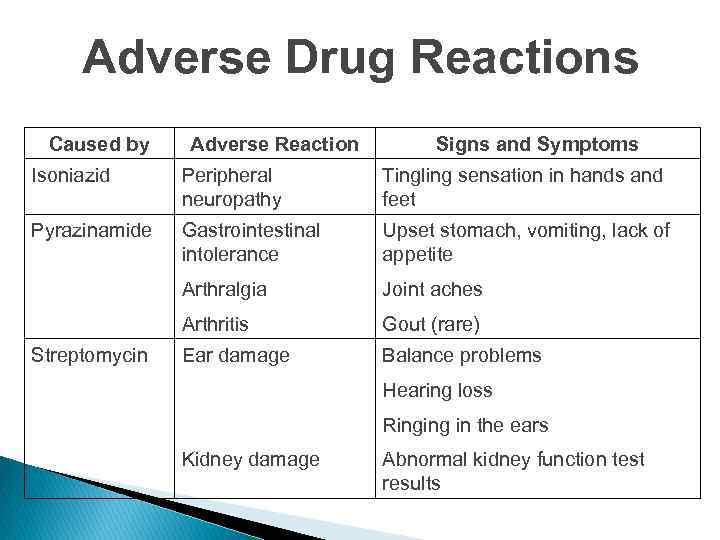
Adverse Drug Reactions Caused by Adverse Reaction Signs and Symptoms Isoniazid Peripheral neuropathy Tingling sensation in hands and feet Pyrazinamide Gastrointestinal intolerance Upset stomach, vomiting, lack of appetite Arthralgia Joint aches Arthritis Gout (rare) Ear damage Balance problems Streptomycin Hearing loss Ringing in the ears Kidney damage Abnormal kidney function test results
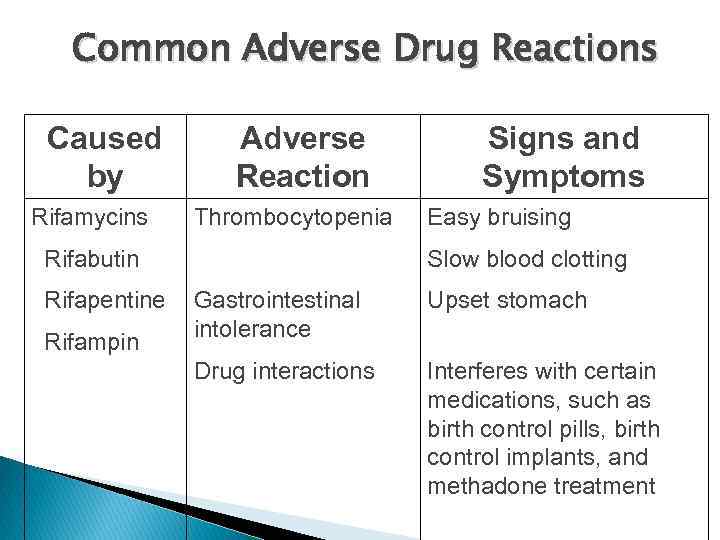
Common Adverse Drug Reactions Caused by Rifamycins Adverse Reaction Thrombocytopenia • Rifabutin • Rifapentine • Rifampin Signs and Symptoms Easy bruising Slow blood clotting Gastrointestinal intolerance Upset stomach Drug interactions Interferes with certain medications, such as birth control pills, birth control implants, and methadone treatment
Drug Interactions Relatively few drug interactions substantially change concentrations of antituberculosis drugs Antituberculosis drugs sometimes change concentrations of other drugs Rifamycins can decrease serum concentrations of many drugs, (e. g. , most of the HIV-1 protease inhibitors), to subtherapeutic levels Isoniazid increases concentrations of some drugs (e. g. , phenytoin) to toxic levels
Treatment Monitoring Sputum smear microscopy for AFB at 2 months and 6 months ◦ If positive at two months, repeat at 3 If still smear positive at 3 months, continuation phase (4 HR) is still started while awaiting DST results Continue drug-susceptibility tests if smear -positive after 3 months of treatment
Treatment Categories Overview 4 categories of anti-TB treatment depending on Localization of disease Severity of TB Sputum smear result History of previous treatment
Treatment categories Category I: New smear-positive pulmonary TB Category II: Recurrent smearpositive pulmonary TB Category III: All smear-negative pulmonary TB Category III: All extra-pulmonary TB Category IV: Chronic cases (sputum-positive after supervised retreatment)
Treatment regimen Regimen I (new smear-positive regimen) Regimen II (smear-positive retreatment regimen) Regimen III (smear-negative regimen) Treatment regimen administered in specialized centres
Note All smear-positive cases identified as “failures”, “treatment after default” and “relapses” should be classified as “retreatment” cases. These patients should be put on treatment Regimen II. A drug susceptibility test should be performed. When results are known, the regimen may need to be adapted according to the susceptibility test results
Treatment regiment All smear-negative cases that are severely ill may be treated with Regimen I or II depending on the patient’s clinical history and record “Treatment after default” smear-negative cases that return after interruption of treatment should, depending on physician’s decision, continue with the previously prescribed regimen or start it again “Transferred-out” cases should continue with their previously prescribed treatment in the new district “Chronic” cases should be treated according to drug susceptibility test results

Standard Treatment Regimen Initial phase: ◦ standard four drug regimens (INH, RIF, PZA, EMB), for 2 months Continuation phase: ◦ additional 4 months
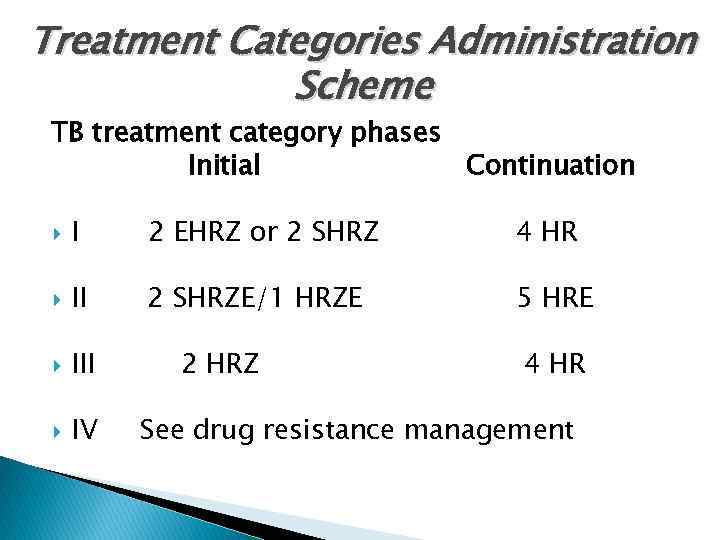
Treatment Categories Administration Scheme TB treatment category phases Initial Continuation I 2 EHRZ or 2 SHRZ 4 HR II 2 SHRZE/1 HRZE 5 HRE III IV 2 HRZ 4 HR See drug resistance management
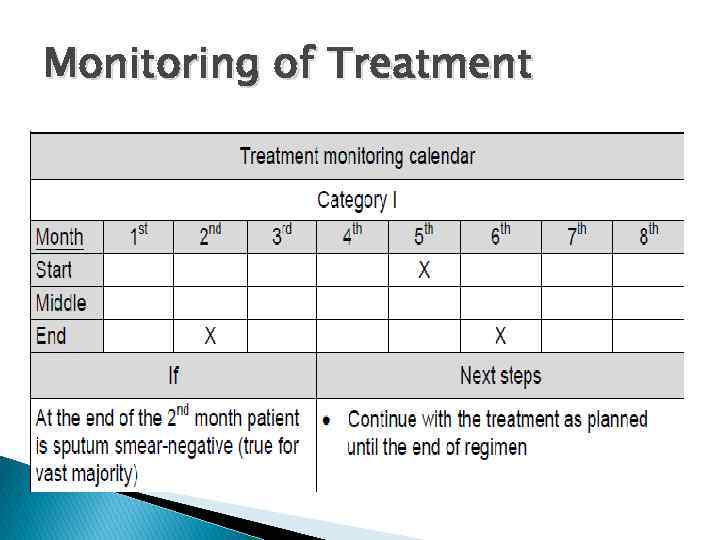
Monitoring of Treatment
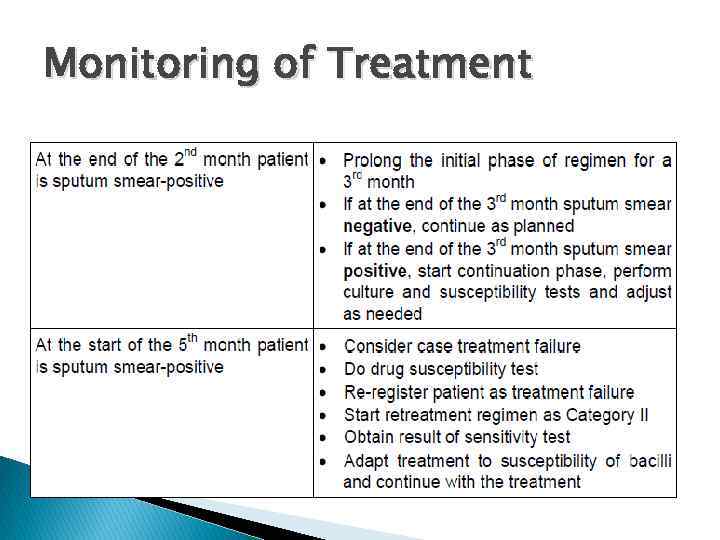
Monitoring of Treatment
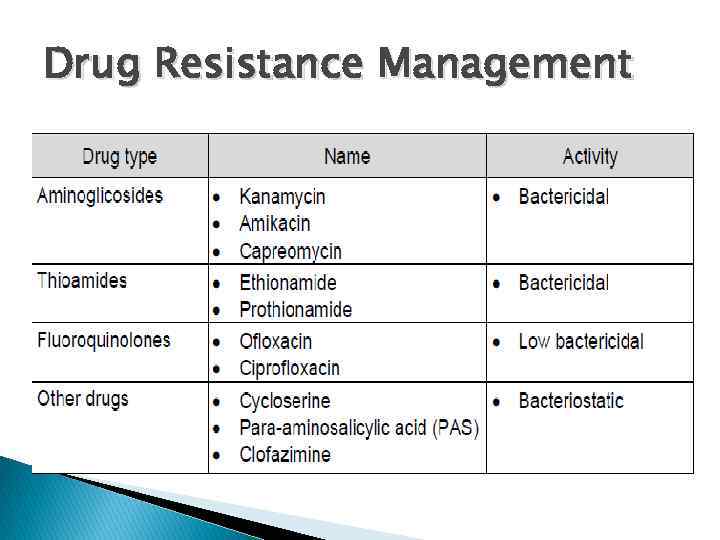
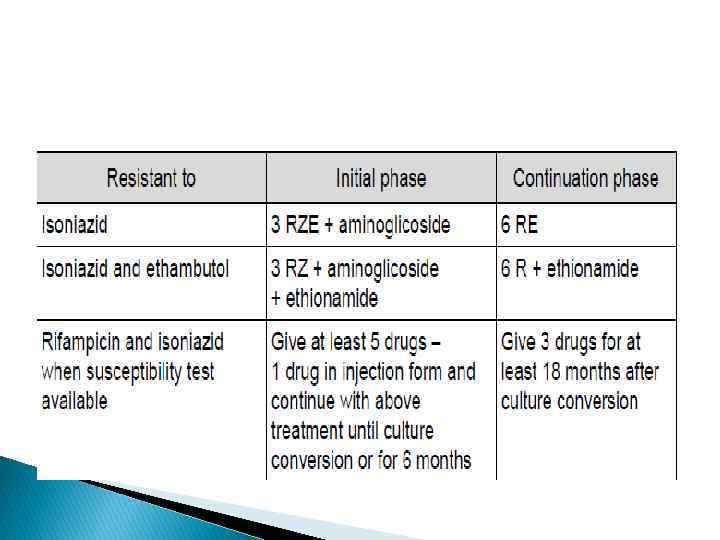
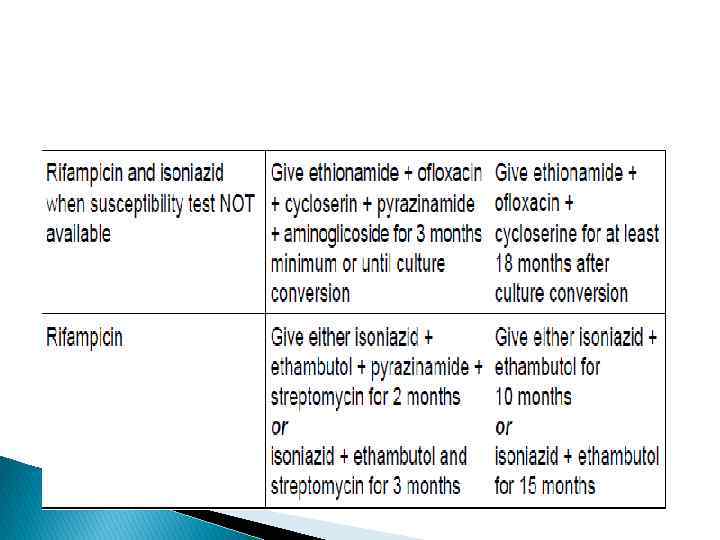
Drug Resistance Management
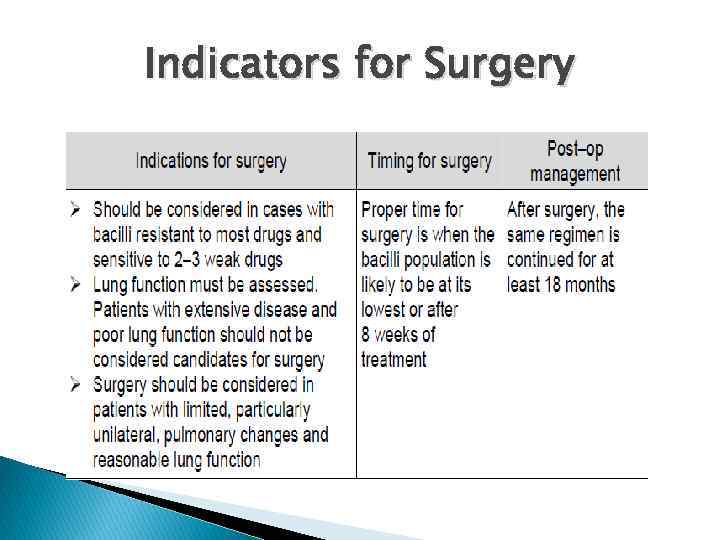
Indicators for Surgery

Thanks Spasiba Rakhmet Deburgess@drkbiomed. org Kjuszkiewicz@drkbiomed. org Cell. : +7 701 218 2377
TB treatment.pptx