c845cb893f0db3daa059d7b384beb6c6.ppt
- Количество слайдов: 35
 Tanzania’s Health Financing Strategy 2014 -2025 towards Universal Health Coverage JAHSR November 2014
Tanzania’s Health Financing Strategy 2014 -2025 towards Universal Health Coverage JAHSR November 2014
 Universal Health Coverage - UHC Ensures that all people can use quality health services they need without suffering financial hardship (WHO) Social Health Protection - SHP A series of public or private measures against social distress and economic loss that can result from paying the cost of seeking treatment during episodes of ill health (ILO)
Universal Health Coverage - UHC Ensures that all people can use quality health services they need without suffering financial hardship (WHO) Social Health Protection - SHP A series of public or private measures against social distress and economic loss that can result from paying the cost of seeking treatment during episodes of ill health (ILO)
 Process & Situational Analysis
Process & Situational Analysis
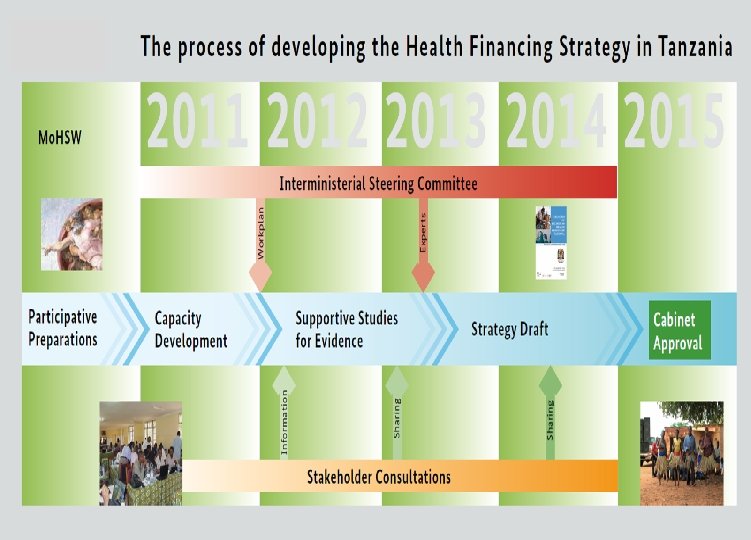
 HFS Rationale and Process • Health Policy-2007 vision to move towards UHC via SHP mechanisms • Goal of Health Sector Strategic Plan III (2009 -2015) • Inter-Ministerial Steering Committee (ISC) created in August 2012 to oversee the HFS development • 11 policy papers informing the strategy development process (2013)
HFS Rationale and Process • Health Policy-2007 vision to move towards UHC via SHP mechanisms • Goal of Health Sector Strategic Plan III (2009 -2015) • Inter-Ministerial Steering Committee (ISC) created in August 2012 to oversee the HFS development • 11 policy papers informing the strategy development process (2013)
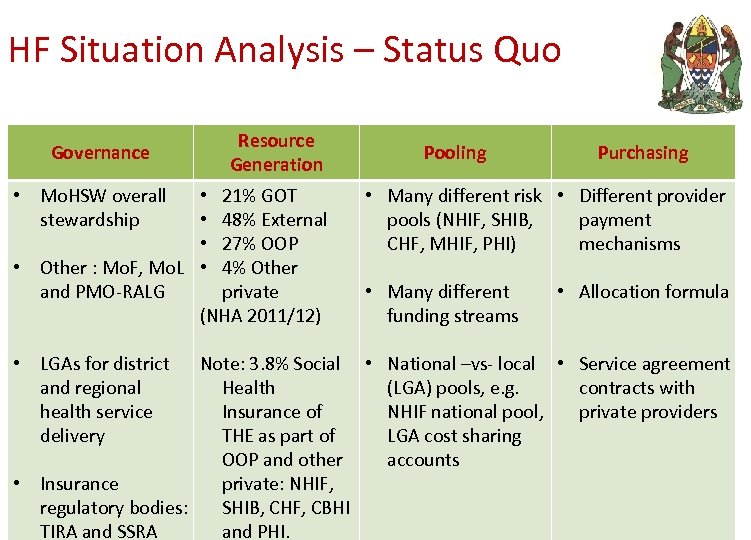 HF Situation Analysis – Status Quo Governance • Mo. HSW overall stewardship Resource Generation • 21% GOT • 48% External • 27% OOP • Other : Mo. F, Mo. L • 4% Other and PMO-RALG private (NHA 2011/12) • LGAs for district and regional health service delivery Pooling Purchasing • Many different risk • Different provider pools (NHIF, SHIB, payment CHF, MHIF, PHI) mechanisms • Many different funding streams • Allocation formula Note: 3. 8% Social • National –vs- local • Service agreement Health (LGA) pools, e. g. contracts with Insurance of NHIF national pool, private providers THE as part of LGA cost sharing OOP and other accounts • Insurance private: NHIF, regulatory bodies: SHIB, CHF, CBHI TIRA and SSRA and PHI.
HF Situation Analysis – Status Quo Governance • Mo. HSW overall stewardship Resource Generation • 21% GOT • 48% External • 27% OOP • Other : Mo. F, Mo. L • 4% Other and PMO-RALG private (NHA 2011/12) • LGAs for district and regional health service delivery Pooling Purchasing • Many different risk • Different provider pools (NHIF, SHIB, payment CHF, MHIF, PHI) mechanisms • Many different funding streams • Allocation formula Note: 3. 8% Social • National –vs- local • Service agreement Health (LGA) pools, e. g. contracts with Insurance of NHIF national pool, private providers THE as part of LGA cost sharing OOP and other accounts • Insurance private: NHIF, regulatory bodies: SHIB, CHF, CBHI TIRA and SSRA and PHI.
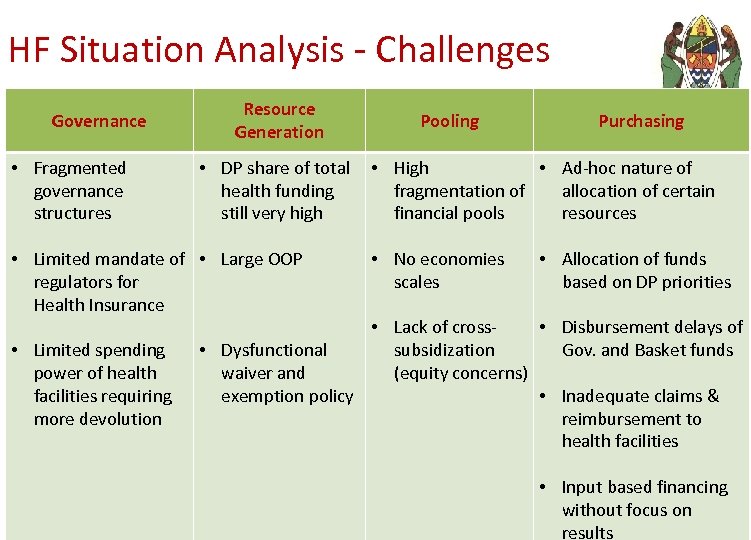 HF Situation Analysis - Challenges Governance • Fragmented governance structures Resource Generation • DP share of total health funding still very high • Limited mandate of • Large OOP regulators for Health Insurance • Limited spending power of health facilities requiring more devolution Pooling Purchasing • High • Ad-hoc nature of fragmentation of allocation of certain financial pools resources • No economies scales • Allocation of funds based on DP priorities • Lack of cross • Disbursement delays of • Dysfunctional subsidization Gov. and Basket funds waiver and (equity concerns) exemption policy • Inadequate claims & reimbursement to health facilities • Input based financing without focus on results
HF Situation Analysis - Challenges Governance • Fragmented governance structures Resource Generation • DP share of total health funding still very high • Limited mandate of • Large OOP regulators for Health Insurance • Limited spending power of health facilities requiring more devolution Pooling Purchasing • High • Ad-hoc nature of fragmentation of allocation of certain financial pools resources • No economies scales • Allocation of funds based on DP priorities • Lack of cross • Disbursement delays of • Dysfunctional subsidization Gov. and Basket funds waiver and (equity concerns) exemption policy • Inadequate claims & reimbursement to health facilities • Input based financing without focus on results
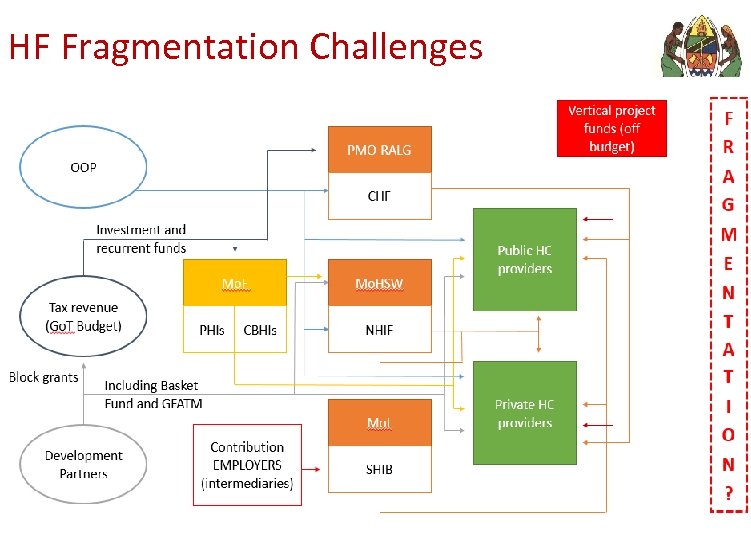 HF Fragmentation Challenges
HF Fragmentation Challenges
 HF Strategy - Content • VISION: achieve Universal Health Coverage • MISSION: A comprehensive SHP System for all Tanzanian residents exists providing a high degree of UHC • GOAL: enable equitable access to affordable & cost -effective quality care & financial protection in case of ill health, according to a nationally defined essential health services package
HF Strategy - Content • VISION: achieve Universal Health Coverage • MISSION: A comprehensive SHP System for all Tanzanian residents exists providing a high degree of UHC • GOAL: enable equitable access to affordable & cost -effective quality care & financial protection in case of ill health, according to a nationally defined essential health services package
 HF Strategy - Content Objectives 1. Develop a sound, responsive and adequate health financing legal and regulatory framework 2. Implement a reformed SHP institutional structure 3. Develop a health financing system which responsive to the poor and vulnerable 4. Strengthen the revenue collection system for the health
HF Strategy - Content Objectives 1. Develop a sound, responsive and adequate health financing legal and regulatory framework 2. Implement a reformed SHP institutional structure 3. Develop a health financing system which responsive to the poor and vulnerable 4. Strengthen the revenue collection system for the health
 HF Strategy - Content Objectives 5. Improve financial and risk pooling mechanisms within the sector 6. Ensure appropriate resources allocations and expenditures 7. Continuously adapt and shape the purchasing structure within the health system with particular focus on RBF for improved services delivery 8. Strengthen the overall public financial and resource data management
HF Strategy - Content Objectives 5. Improve financial and risk pooling mechanisms within the sector 6. Ensure appropriate resources allocations and expenditures 7. Continuously adapt and shape the purchasing structure within the health system with particular focus on RBF for improved services delivery 8. Strengthen the overall public financial and resource data management
 HF Strategy - Content GUIDING PRINCIPLES AND VALUES: Implementation of the HFS will adhere to the following principles: o Equity o Progressivity in financial contributions o Access to needed health services (financial and geographic) o Solidarity o Transparency and Accountability o Sustainability o Efficiency and value for money. • The HFS is geared towards providing financial protection to the population and will focus its efforts on the inclusion of the poor into the envisaged Social Health Protection System.
HF Strategy - Content GUIDING PRINCIPLES AND VALUES: Implementation of the HFS will adhere to the following principles: o Equity o Progressivity in financial contributions o Access to needed health services (financial and geographic) o Solidarity o Transparency and Accountability o Sustainability o Efficiency and value for money. • The HFS is geared towards providing financial protection to the population and will focus its efforts on the inclusion of the poor into the envisaged Social Health Protection System.
 Main Reforms Creation of a Single National Health Insurer (SNHI).
Main Reforms Creation of a Single National Health Insurer (SNHI).
 Strategic Interventions – Governance Strategy 1: Provide adequate legal/regulatory framework & institutional set up for reformed health financing system • Legislate the mandatory SNHI with entitlement to a MBP for all. • Policy level: Defragment current governance landscape and establish a unified command over SNHI. • Regulatory level: creation of clear regulation and auditing structures for SNHI. • SNHI as main purchaser in the public health system, with national and sub-national institutional structures. • Private health insurances: duplicative and supplementary functions to the SNHI; cover non-MBP benefits. No opting out of the SNHI (premium).
Strategic Interventions – Governance Strategy 1: Provide adequate legal/regulatory framework & institutional set up for reformed health financing system • Legislate the mandatory SNHI with entitlement to a MBP for all. • Policy level: Defragment current governance landscape and establish a unified command over SNHI. • Regulatory level: creation of clear regulation and auditing structures for SNHI. • SNHI as main purchaser in the public health system, with national and sub-national institutional structures. • Private health insurances: duplicative and supplementary functions to the SNHI; cover non-MBP benefits. No opting out of the SNHI (premium).
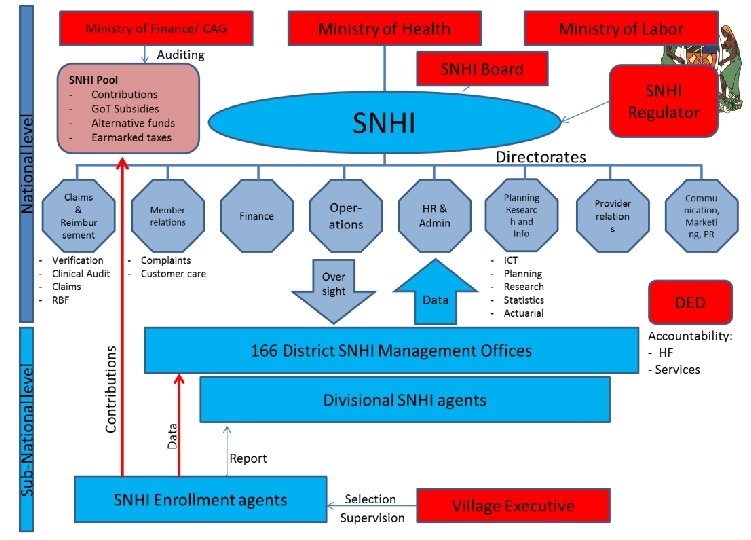
 Strategic Interventions – Governance plus Enhance stakeholder engagement for accountability • RBF: country wide performance based incentive system at health service delivery level (potentially managed by SNHI in the long-term). • Population involvement and the community: appropriate community representation structures are established. • Exploiting the political constituency: involvement of the political constituency in matters of SNHI.
Strategic Interventions – Governance plus Enhance stakeholder engagement for accountability • RBF: country wide performance based incentive system at health service delivery level (potentially managed by SNHI in the long-term). • Population involvement and the community: appropriate community representation structures are established. • Exploiting the political constituency: involvement of the political constituency in matters of SNHI.
 Strategic Interventions – Revenue Collection Strategy 2: Increase public revenues for health • Advocacy for larger sectorial share of existing resources to health. • Identification of additional government resources for health (e. g. VAT, earmarked taxes, proportion of profits made through public investment, etc. ). • Creating fiscal space through efficiency gains (e. g. effective gate keeping and referral mechanisms, HRH distribution, etc. ). plus mobilize additional resources from the private corporate sector • Engage private sector in HF and efficient service delivery. • Implement fiscal and financing mechanisms to promote private sector growth in the private sector.
Strategic Interventions – Revenue Collection Strategy 2: Increase public revenues for health • Advocacy for larger sectorial share of existing resources to health. • Identification of additional government resources for health (e. g. VAT, earmarked taxes, proportion of profits made through public investment, etc. ). • Creating fiscal space through efficiency gains (e. g. effective gate keeping and referral mechanisms, HRH distribution, etc. ). plus mobilize additional resources from the private corporate sector • Engage private sector in HF and efficient service delivery. • Implement fiscal and financing mechanisms to promote private sector growth in the private sector.
 Main Reforms Creation of a Mandatory Nature Insurance Enrolment
Main Reforms Creation of a Mandatory Nature Insurance Enrolment
 Strategic Interventions – Revenue Collection Strategy 3: Implement the mandatory contribution system. • Shared SNHI contributions between employer and employee (formal sector) – employer share never lower than the employee share • Subsidization (full or partial) for those with limited financial means • Establishment of mechanisms for populations enrolment into the SNHI (making access to certain essential public services dependent on HI membership card)
Strategic Interventions – Revenue Collection Strategy 3: Implement the mandatory contribution system. • Shared SNHI contributions between employer and employee (formal sector) – employer share never lower than the employee share • Subsidization (full or partial) for those with limited financial means • Establishment of mechanisms for populations enrolment into the SNHI (making access to certain essential public services dependent on HI membership card)
 Main Reforms Methods for Targeting the Poor
Main Reforms Methods for Targeting the Poor
 Strategic Interventions – Revenue Collection Strategy 4: Identify and ensure coverage of the poor. • SHP coverage of the entire population (UHC principles). • Prioritizing the inclusion of the poor and most vulnerable. • Establishment of targeting mechanisms for the poor (identification of the poor aligned with TASAF approach). • Full government subsidy in health coverage of the poor (28% of the population, starting with the food poor 9. 7%), partial subsidies according to poverty identification formula.
Strategic Interventions – Revenue Collection Strategy 4: Identify and ensure coverage of the poor. • SHP coverage of the entire population (UHC principles). • Prioritizing the inclusion of the poor and most vulnerable. • Establishment of targeting mechanisms for the poor (identification of the poor aligned with TASAF approach). • Full government subsidy in health coverage of the poor (28% of the population, starting with the food poor 9. 7%), partial subsidies according to poverty identification formula.
 Strategic Intervention - Pooling Strategy 5: Decrease the fragmentation of risk pools. • Increase redistributive capacity of prepaid funds and align different revenue sources. • Decrease number of financial and risk pools. • Enable cross-subsidization with the health system through the creation of a single national insurer.
Strategic Intervention - Pooling Strategy 5: Decrease the fragmentation of risk pools. • Increase redistributive capacity of prepaid funds and align different revenue sources. • Decrease number of financial and risk pools. • Enable cross-subsidization with the health system through the creation of a single national insurer.
 Strategic Interventions – Health Purchasing Strategy 6: Implement a standard Minimum Benefit Package (MBP) • MBP: all services at the dispensary and health center levels and services at district hospital level. • Strengthen referral mechanisms & introduce copayments for non- compliance with the referral system. • Public health activities run in parallel of the MBP directly delivered by the government (e. g. vector control, general sanitation).
Strategic Interventions – Health Purchasing Strategy 6: Implement a standard Minimum Benefit Package (MBP) • MBP: all services at the dispensary and health center levels and services at district hospital level. • Strengthen referral mechanisms & introduce copayments for non- compliance with the referral system. • Public health activities run in parallel of the MBP directly delivered by the government (e. g. vector control, general sanitation).
 Strategic Interventions – Health Purchasing Strategy 6: Implement a standard Minimum Benefit Package (MBP) • Division into MBP (whole population) & current NHIF package (MBP +, current NHIF members + those classified as extremely poor). • Over time, the entire population will access MBP + as minimum entitlement. • Upgrades from MBP to MBP + will be possible for additional premium. • MBP will be delivered primarily by the public health system and accredited/ contracted private providers.
Strategic Interventions – Health Purchasing Strategy 6: Implement a standard Minimum Benefit Package (MBP) • Division into MBP (whole population) & current NHIF package (MBP +, current NHIF members + those classified as extremely poor). • Over time, the entire population will access MBP + as minimum entitlement. • Upgrades from MBP to MBP + will be possible for additional premium. • MBP will be delivered primarily by the public health system and accredited/ contracted private providers.
 Strategic Interventions – Health Purchasing Plus Improve purchasing for areas outside MBP pool • Purchasing of Public Health and Capital Investment will continue to be managed by LGAs • Medical Education and hi-tech capital investment to be funded by Mo. HSW and Mo. EVT.
Strategic Interventions – Health Purchasing Plus Improve purchasing for areas outside MBP pool • Purchasing of Public Health and Capital Investment will continue to be managed by LGAs • Medical Education and hi-tech capital investment to be funded by Mo. HSW and Mo. EVT.
 Main Reforms Changing Purchasing Methods
Main Reforms Changing Purchasing Methods
 Strategic Interventions – Health Purchasing Strategy 7: Establish effective provider payment systems • Establishment of a combination of provider payment mechanisms • Creation of appropriate incentive mechanisms (e. g. RBF) to enhance performance of providers and CHMT and RHMT. The incentives will be used for staff incentives, strengthening health facilities (e. g. purchasing essential inputs) and enhancing management performance.
Strategic Interventions – Health Purchasing Strategy 7: Establish effective provider payment systems • Establishment of a combination of provider payment mechanisms • Creation of appropriate incentive mechanisms (e. g. RBF) to enhance performance of providers and CHMT and RHMT. The incentives will be used for staff incentives, strengthening health facilities (e. g. purchasing essential inputs) and enhancing management performance.
 Strategic Interventions – Health Purchasing Strategy 8: Improve resource allocation and expenditures • Review and adjustment of LGA allocation formulae in consultation with Mo. F and PMO-RALG • Review existing pay and incentive structures for health workers and explore the possibility to channel addition PE funding through RBF and SNHI. • Development of an equalization mechanism between LGAs to enable individual and geographic crosssubsidization.
Strategic Interventions – Health Purchasing Strategy 8: Improve resource allocation and expenditures • Review and adjustment of LGA allocation formulae in consultation with Mo. F and PMO-RALG • Review existing pay and incentive structures for health workers and explore the possibility to channel addition PE funding through RBF and SNHI. • Development of an equalization mechanism between LGAs to enable individual and geographic crosssubsidization.
 Main Reforms Provider Autonomy
Main Reforms Provider Autonomy
 Strategic Interventions – Health Purchasing Strategy 9: Improve public financial management • Focus on efficient and cost-effective resource management, • Fiscal Decentralization to health facilities, • Effective claim and reimbursement systems have to be established for SNHI, • PFM structure should be revised to guide budgeting and planning of the health sector in line with suggested reforms, • SNHI data sets need to be available to all formal bodies (planning and budgeting department, PMO-RALG etc)
Strategic Interventions – Health Purchasing Strategy 9: Improve public financial management • Focus on efficient and cost-effective resource management, • Fiscal Decentralization to health facilities, • Effective claim and reimbursement systems have to be established for SNHI, • PFM structure should be revised to guide budgeting and planning of the health sector in line with suggested reforms, • SNHI data sets need to be available to all formal bodies (planning and budgeting department, PMO-RALG etc)
 Strategic Interventions – Health Purchasing Strategy 10: improve use of information for evidence-based policy • Development linkages with HMIS by data systems • Link vital national databases to the Social Health Insurance. • Regular supportive research. • Solid social health insurance database.
Strategic Interventions – Health Purchasing Strategy 10: improve use of information for evidence-based policy • Development linkages with HMIS by data systems • Link vital national databases to the Social Health Insurance. • Regular supportive research. • Solid social health insurance database.
 Fiscal Space Analysis for Health in TZ • NHA 2012 calculates current health expenditure (Gov&DP) of 46 USD per capita – difference to international average to supply minimum health needs package (USD 84 per capita) is large. • If gradually expands budget allocation to health over next ten years to meet the 15% Abuja target, this can provide extra revenues, which could cover 11% of the minimum financial gap • If there were major policy prioritizations to reform and improve health insurance the study projects it could account for almost 50% of THE by 2024/25 if health insurance coverage could be raised to above 50% of the population
Fiscal Space Analysis for Health in TZ • NHA 2012 calculates current health expenditure (Gov&DP) of 46 USD per capita – difference to international average to supply minimum health needs package (USD 84 per capita) is large. • If gradually expands budget allocation to health over next ten years to meet the 15% Abuja target, this can provide extra revenues, which could cover 11% of the minimum financial gap • If there were major policy prioritizations to reform and improve health insurance the study projects it could account for almost 50% of THE by 2024/25 if health insurance coverage could be raised to above 50% of the population
 Fiscal Space Analysis for Health in TZ • Potential revenues raised from alternative resources (earmarked taxes, airtime or airline levies etc) are estimated to cover only up to 4% of the financing gap • Efficiency savings: if we improve efficiency, the study estimates a potential of closing the gap by 10% (if it reduced its inefficiency to 18% less efficient from 30% less efficient than most efficient countries)
Fiscal Space Analysis for Health in TZ • Potential revenues raised from alternative resources (earmarked taxes, airtime or airline levies etc) are estimated to cover only up to 4% of the financing gap • Efficiency savings: if we improve efficiency, the study estimates a potential of closing the gap by 10% (if it reduced its inefficiency to 18% less efficient from 30% less efficient than most efficient countries)
 The Way Forward • Incorporate comments from JAHSR, finalize strategy and its costing (Nov. 2014) • Final presentation to ISC end of November 2014 • Presentation of the HFS to the Cabinet Secretariat, (January 2015)
The Way Forward • Incorporate comments from JAHSR, finalize strategy and its costing (Nov. 2014) • Final presentation to ISC end of November 2014 • Presentation of the HFS to the Cabinet Secretariat, (January 2015)
 ASANTENI KWA KUNISIKILIZA
ASANTENI KWA KUNISIKILIZA


