b6d61e688e660121051a91a5fa091e14.ppt
- Количество слайдов: 63
 Tackling NCDs in Pakistan: the Policy Makers Perspective in Khyber Pakhtunkhwa Dr Shabina Raza Health Department Government of Khyber Pakhtunkhwa
Tackling NCDs in Pakistan: the Policy Makers Perspective in Khyber Pakhtunkhwa Dr Shabina Raza Health Department Government of Khyber Pakhtunkhwa
 INVESTING IN HEALTH DECREASING VIOLENCE REDUCING POVERTY
INVESTING IN HEALTH DECREASING VIOLENCE REDUCING POVERTY
 Khyber Pakhtunkhwa
Khyber Pakhtunkhwa
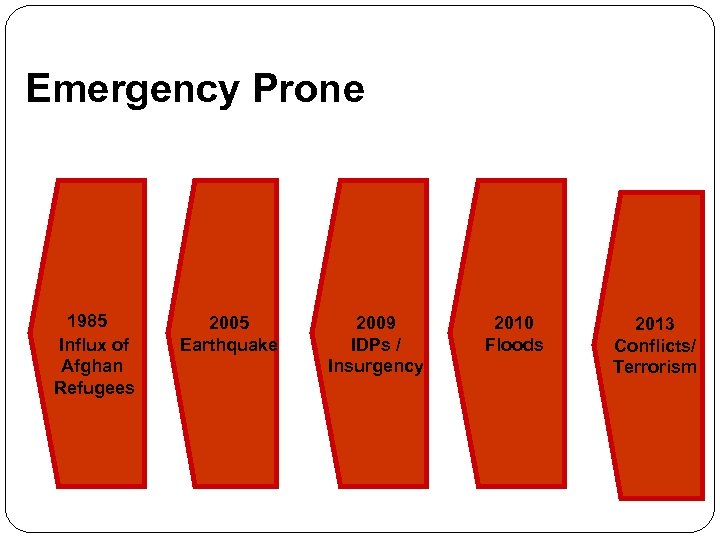 Emergency Prone 1985 Influx of Afghan Refugees 2005 Earthquake 2009 IDPs / Insurgency 2010 Floods 2013 Conflicts/ Terrorism
Emergency Prone 1985 Influx of Afghan Refugees 2005 Earthquake 2009 IDPs / Insurgency 2010 Floods 2013 Conflicts/ Terrorism
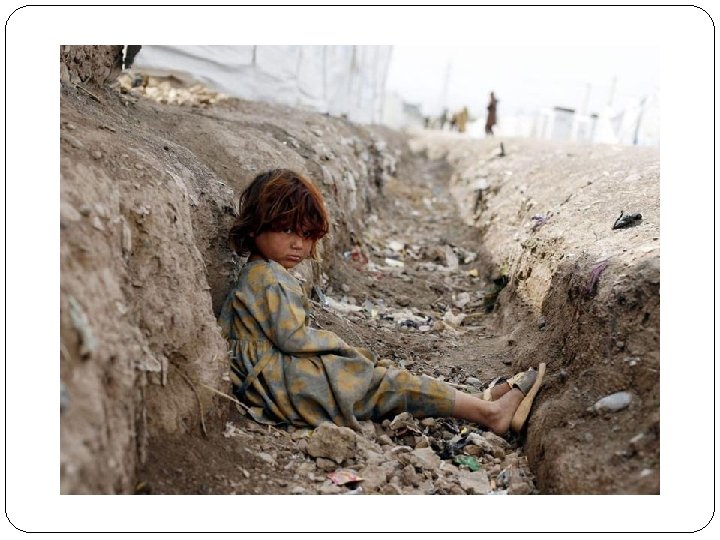
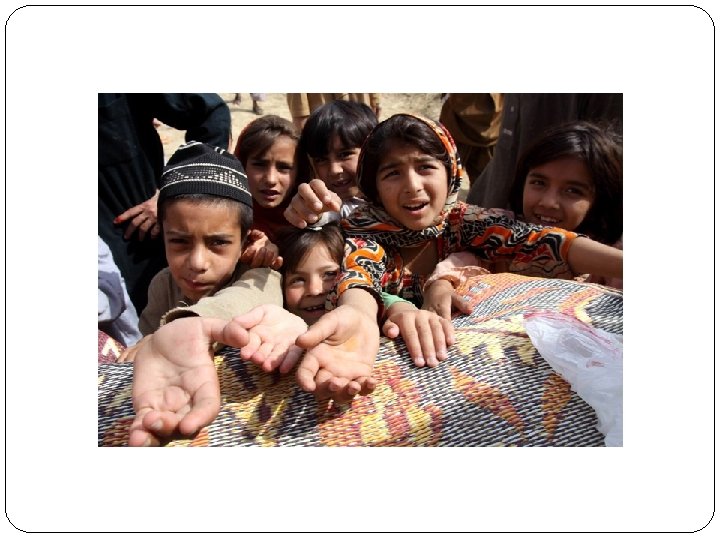


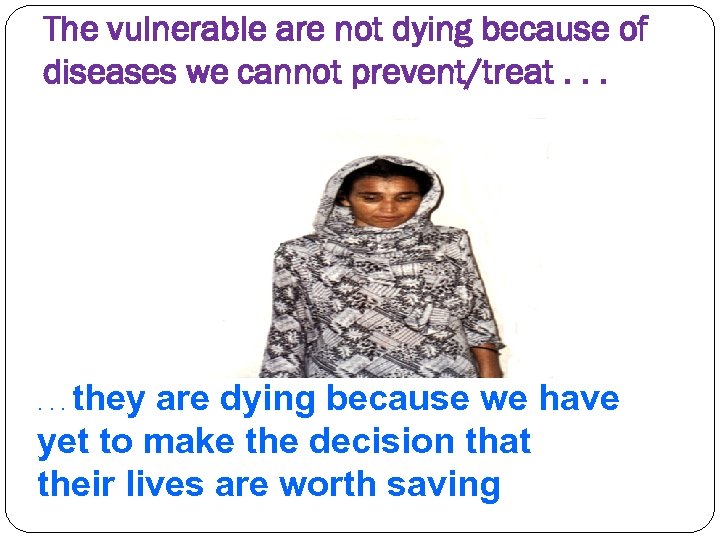 The vulnerable are not dying because of diseases we cannot prevent/treat. . . they are dying because we have yet to make the decision that their lives are worth saving. . .
The vulnerable are not dying because of diseases we cannot prevent/treat. . . they are dying because we have yet to make the decision that their lives are worth saving. . .
 No more poor options for poor people
No more poor options for poor people
 miles to go…. .
miles to go…. .
 Health Sector in KP Health being acknowledged as an important mean for Human Development & accepted as prerequisite for social & economic development Goal for Health Department is to improve the health status of the population in the province through ensuring access to a high quality, responsive healthcare delivery system, which provides acceptable and affordable services in an equitable manner.
Health Sector in KP Health being acknowledged as an important mean for Human Development & accepted as prerequisite for social & economic development Goal for Health Department is to improve the health status of the population in the province through ensuring access to a high quality, responsive healthcare delivery system, which provides acceptable and affordable services in an equitable manner.
 Objectives Following six strategic objectives identified for health sector: i. Improved governance & strengthened management ii. Institutionalized informed decision making iii. Improved regulation & quality assurance iv. Effective & efficient management of human resource v. Improved accessibility to preventive & curative services vi. Disaster risk reduction & management
Objectives Following six strategic objectives identified for health sector: i. Improved governance & strengthened management ii. Institutionalized informed decision making iii. Improved regulation & quality assurance iv. Effective & efficient management of human resource v. Improved accessibility to preventive & curative services vi. Disaster risk reduction & management
 OUR PERFORMANCE How will we succeed? Plan our business around our Outcomes Set our key strategic directions for each financial year in the Health Budget of Go. KP, which guide our business and operational plans Provide our service deliverers with systems [package of services], tools [protocols and procedures] and information [DHIS] needed to achieve these goals Anticipate opportunities & what might go wrong, and manage risk Evaluate our progress to measure our success Seek to continuously improve the performance of our health programs and the way we use our resources.
OUR PERFORMANCE How will we succeed? Plan our business around our Outcomes Set our key strategic directions for each financial year in the Health Budget of Go. KP, which guide our business and operational plans Provide our service deliverers with systems [package of services], tools [protocols and procedures] and information [DHIS] needed to achieve these goals Anticipate opportunities & what might go wrong, and manage risk Evaluate our progress to measure our success Seek to continuously improve the performance of our health programs and the way we use our resources.
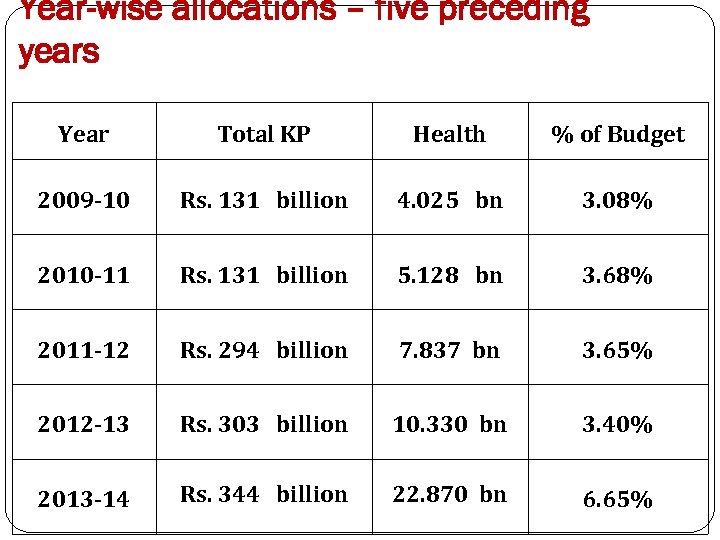 Year-wise allocations – five preceding years Year Total KP Health % of Budget 2009 -10 Rs. 131 billion 4. 025 bn 3. 08% 2010 -11 Rs. 131 billion 5. 128 bn 3. 68% 2011 -12 Rs. 294 billion 7. 837 bn 3. 65% 2012 -13 Rs. 303 billion 10. 330 bn 3. 40% 2013 -14 Rs. 344 billion 22. 870 bn 6. 65%
Year-wise allocations – five preceding years Year Total KP Health % of Budget 2009 -10 Rs. 131 billion 4. 025 bn 3. 08% 2010 -11 Rs. 131 billion 5. 128 bn 3. 68% 2011 -12 Rs. 294 billion 7. 837 bn 3. 65% 2012 -13 Rs. 303 billion 10. 330 bn 3. 40% 2013 -14 Rs. 344 billion 22. 870 bn 6. 65%
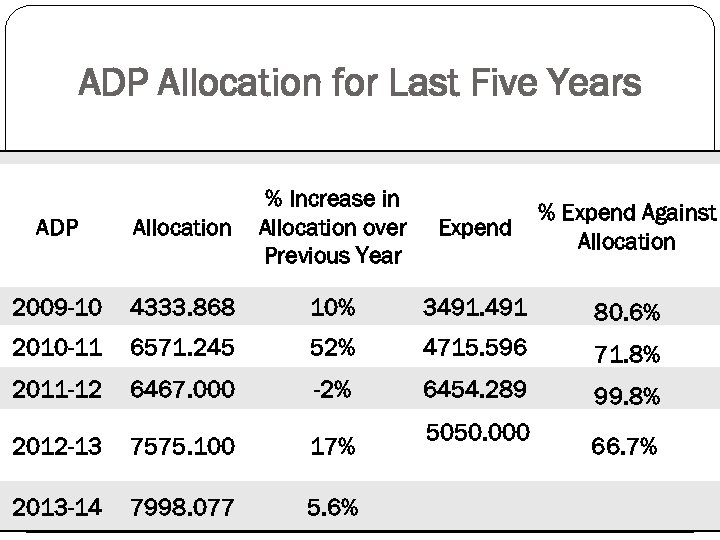 ADP Allocation for Last Five Years ADP Allocation % Increase in Allocation over Previous Year 2009 -10 4333. 868 10% 3491. 491 80. 6% 2010 -11 6571. 245 52% 4715. 596 71. 8% 2011 -12 6467. 000 -2% 6454. 289 2012 -13 7575. 100 17% 2013 -14 7998. 077 5. 6% Expend Against Allocation 5050. 000 Contd. 99. 8% 66. 7%
ADP Allocation for Last Five Years ADP Allocation % Increase in Allocation over Previous Year 2009 -10 4333. 868 10% 3491. 491 80. 6% 2010 -11 6571. 245 52% 4715. 596 71. 8% 2011 -12 6467. 000 -2% 6454. 289 2012 -13 7575. 100 17% 2013 -14 7998. 077 5. 6% Expend Against Allocation 5050. 000 Contd. 99. 8% 66. 7%
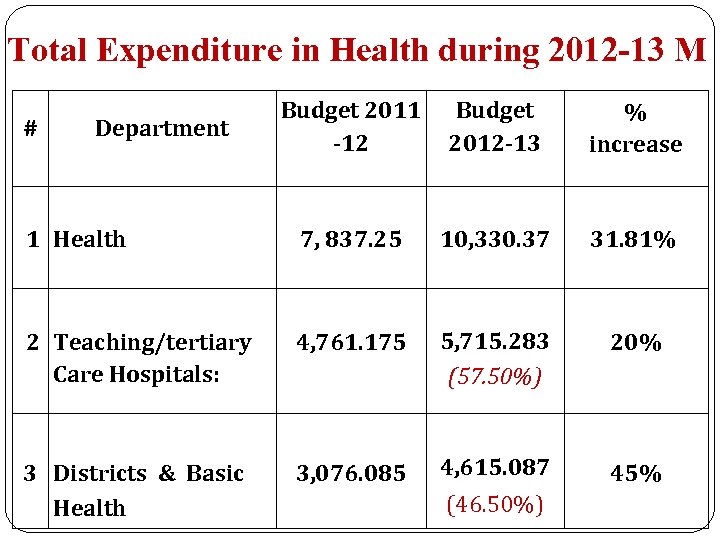 Total Expenditure in Health during 2012 -13 M # Department 1 Health Budget 2011 -12 Budget 2012 -13 % increase 7, 837. 25 10, 330. 37 31. 81% 2 Teaching/tertiary Care Hospitals: 4, 761. 175 5, 715. 283 (57. 50%) 20% 3 Districts & Basic Health 3, 076. 085 4, 615. 087 45% (46. 50%)
Total Expenditure in Health during 2012 -13 M # Department 1 Health Budget 2011 -12 Budget 2012 -13 % increase 7, 837. 25 10, 330. 37 31. 81% 2 Teaching/tertiary Care Hospitals: 4, 761. 175 5, 715. 283 (57. 50%) 20% 3 Districts & Basic Health 3, 076. 085 4, 615. 087 45% (46. 50%)
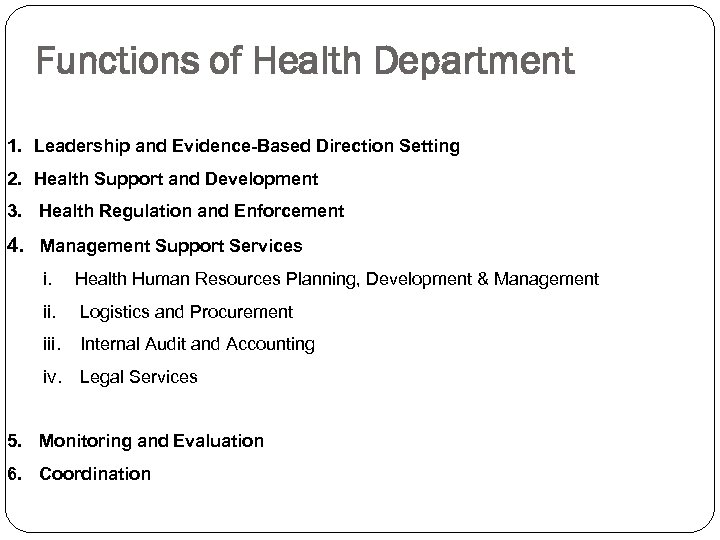 Functions of Health Department 1. Leadership and Evidence-Based Direction Setting 2. Health Support and Development 3. Health Regulation and Enforcement 4. Management Support Services i. Health Human Resources Planning, Development & Management ii. Logistics and Procurement iii. Internal Audit and Accounting iv. Legal Services 5. Monitoring and Evaluation 6. Coordination
Functions of Health Department 1. Leadership and Evidence-Based Direction Setting 2. Health Support and Development 3. Health Regulation and Enforcement 4. Management Support Services i. Health Human Resources Planning, Development & Management ii. Logistics and Procurement iii. Internal Audit and Accounting iv. Legal Services 5. Monitoring and Evaluation 6. Coordination
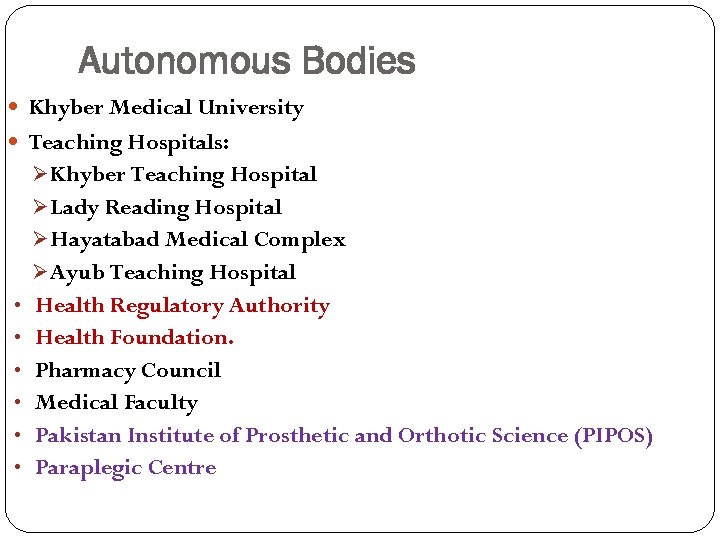 Autonomous Bodies Khyber Medical University Teaching Hospitals: Ø Khyber Teaching Hospital Ø Lady Reading Hospital Ø Hayatabad Medical Complex Ø Ayub Teaching Hospital • Health Regulatory Authority • Health Foundation. • Pharmacy Council • Medical Faculty • Pakistan Institute of Prosthetic and Orthotic Science (PIPOS) • Paraplegic Centre
Autonomous Bodies Khyber Medical University Teaching Hospitals: Ø Khyber Teaching Hospital Ø Lady Reading Hospital Ø Hayatabad Medical Complex Ø Ayub Teaching Hospital • Health Regulatory Authority • Health Foundation. • Pharmacy Council • Medical Faculty • Pakistan Institute of Prosthetic and Orthotic Science (PIPOS) • Paraplegic Centre
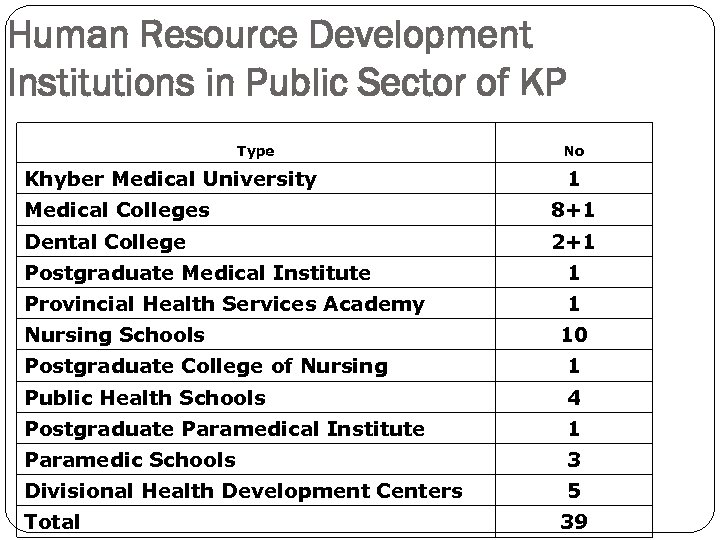 Human Resource Development Institutions in Public Sector of KP Type Khyber Medical University No 1 Medical Colleges 8+1 Dental College 2+1 Postgraduate Medical Institute 1 Provincial Health Services Academy 1 Nursing Schools 10 Postgraduate College of Nursing 1 Public Health Schools 4 Postgraduate Paramedical Institute 1 Paramedic Schools 3 Divisional Health Development Centers 5 Total 39
Human Resource Development Institutions in Public Sector of KP Type Khyber Medical University No 1 Medical Colleges 8+1 Dental College 2+1 Postgraduate Medical Institute 1 Provincial Health Services Academy 1 Nursing Schools 10 Postgraduate College of Nursing 1 Public Health Schools 4 Postgraduate Paramedical Institute 1 Paramedic Schools 3 Divisional Health Development Centers 5 Total 39
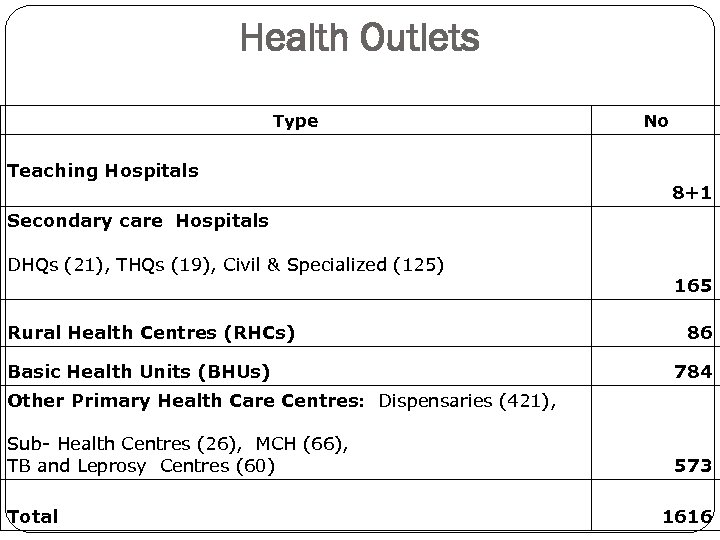 Health Outlets Type Teaching Hospitals No 8+1 Secondary care Hospitals DHQs (21), THQs (19), Civil & Specialized (125) Rural Health Centres (RHCs) Basic Health Units (BHUs) 165 86 784 Other Primary Health Care Centres: Dispensaries (421), Sub- Health Centres (26), MCH (66), TB and Leprosy Centres (60) Total 573 1616
Health Outlets Type Teaching Hospitals No 8+1 Secondary care Hospitals DHQs (21), THQs (19), Civil & Specialized (125) Rural Health Centres (RHCs) Basic Health Units (BHUs) 165 86 784 Other Primary Health Care Centres: Dispensaries (421), Sub- Health Centres (26), MCH (66), TB and Leprosy Centres (60) Total 573 1616
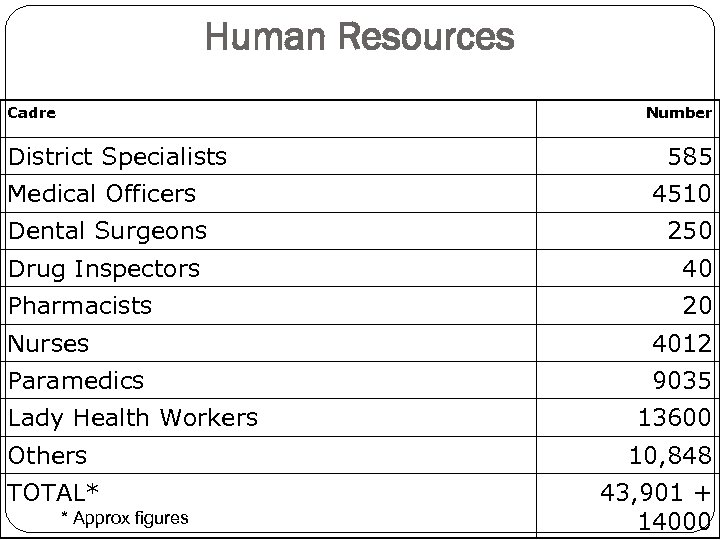 Human Resources Cadre Number District Specialists Medical Officers 585 4510 Dental Surgeons 250 Drug Inspectors 40 Pharmacists 20 Nurses 4012 Paramedics 9035 Lady Health Workers Others TOTAL* * Approx figures 13600 10, 848 43, 901 + 14000
Human Resources Cadre Number District Specialists Medical Officers 585 4510 Dental Surgeons 250 Drug Inspectors 40 Pharmacists 20 Nurses 4012 Paramedics 9035 Lady Health Workers Others TOTAL* * Approx figures 13600 10, 848 43, 901 + 14000
 How are the Services Delivered? Public sector services are delivered by: Provincial Health Department delivers *health promotive, preventive, curative, and rehabilitative services to all population *through community based LHW services & CMWs, first level care facilities, secondary healthcare facilities and tertiary healthcare hospitals Federal Government through PSDP provides *financial supports to provincial health department in implementation of vertical programs 24
How are the Services Delivered? Public sector services are delivered by: Provincial Health Department delivers *health promotive, preventive, curative, and rehabilitative services to all population *through community based LHW services & CMWs, first level care facilities, secondary healthcare facilities and tertiary healthcare hospitals Federal Government through PSDP provides *financial supports to provincial health department in implementation of vertical programs 24
 Service Delivery - cont’d…. Private sector services are delivered by: Private for profit sector is the second largest provider in the province. Major focus is curative services and their distribution is widespread across the province. Majority of people in the province utilize private facilities, e. g. more than 90% had their first contact with a private practitioner at primary healthcare level
Service Delivery - cont’d…. Private sector services are delivered by: Private for profit sector is the second largest provider in the province. Major focus is curative services and their distribution is widespread across the province. Majority of people in the province utilize private facilities, e. g. more than 90% had their first contact with a private practitioner at primary healthcare level
 Healthcare Financing Public sector health services are financed by Government of Khyber Pakhtunkhwa Out Of Pocket expenditure in KP is 2/3 rd of Total Health Expenditure (THE) and highest in Pakistan Federal Government contributes 0. 5 – 0. 8% of provincial budget Development partners support provincial budget 0. 2 -0. 3% of
Healthcare Financing Public sector health services are financed by Government of Khyber Pakhtunkhwa Out Of Pocket expenditure in KP is 2/3 rd of Total Health Expenditure (THE) and highest in Pakistan Federal Government contributes 0. 5 – 0. 8% of provincial budget Development partners support provincial budget 0. 2 -0. 3% of
 Human Resource Health Department has the second largest health workforce in the province. Medical education delivered through public sector medical colleges, postgraduate medical institute, nursing schools & college, public health schools, paramedical schools and postgraduate paramedical institute. Medical education delivered through private sector medical colleges, nursing school, paramedical schools
Human Resource Health Department has the second largest health workforce in the province. Medical education delivered through public sector medical colleges, postgraduate medical institute, nursing schools & college, public health schools, paramedical schools and postgraduate paramedical institute. Medical education delivered through private sector medical colleges, nursing school, paramedical schools
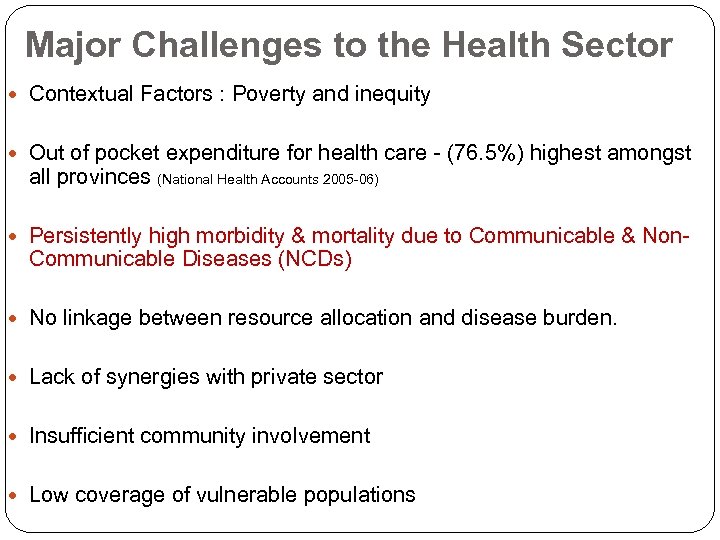 Major Challenges to the Health Sector Contextual Factors : Poverty and inequity Out of pocket expenditure for health care - (76. 5%) highest amongst all provinces (National Health Accounts 2005 -06) Persistently high morbidity & mortality due to Communicable & Non- Communicable Diseases (NCDs) No linkage between resource allocation and disease burden. Lack of synergies with private sector Insufficient community involvement Low coverage of vulnerable populations
Major Challenges to the Health Sector Contextual Factors : Poverty and inequity Out of pocket expenditure for health care - (76. 5%) highest amongst all provinces (National Health Accounts 2005 -06) Persistently high morbidity & mortality due to Communicable & Non- Communicable Diseases (NCDs) No linkage between resource allocation and disease burden. Lack of synergies with private sector Insufficient community involvement Low coverage of vulnerable populations
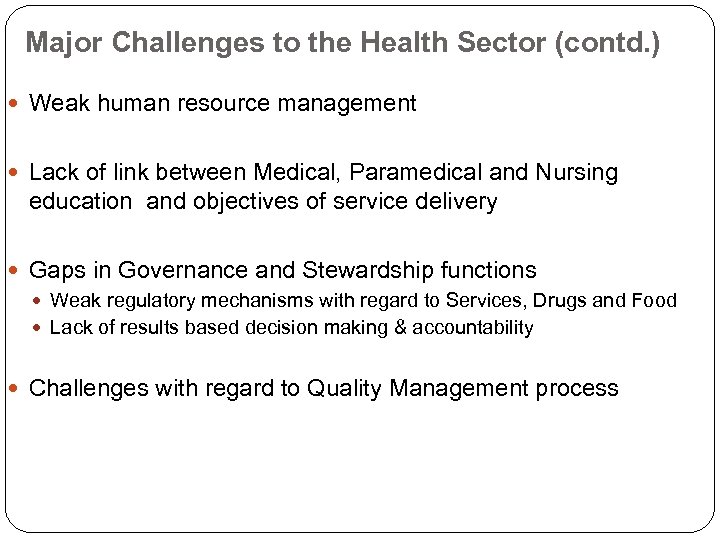 Major Challenges to the Health Sector (contd. ) Weak human resource management Lack of link between Medical, Paramedical and Nursing education and objectives of service delivery Gaps in Governance and Stewardship functions Weak regulatory mechanisms with regard to Services, Drugs and Food Lack of results based decision making & accountability Challenges with regard to Quality Management process
Major Challenges to the Health Sector (contd. ) Weak human resource management Lack of link between Medical, Paramedical and Nursing education and objectives of service delivery Gaps in Governance and Stewardship functions Weak regulatory mechanisms with regard to Services, Drugs and Food Lack of results based decision making & accountability Challenges with regard to Quality Management process
 Introducing Institutionalized Community Participation: Health Management Committees Contributions: 1. Support for human resources 2. Improved access 3. Infrastructure for quality services 4. Increased demand
Introducing Institutionalized Community Participation: Health Management Committees Contributions: 1. Support for human resources 2. Improved access 3. Infrastructure for quality services 4. Increased demand
 Learning by doing
Learning by doing
 Quality Standards as “job-aids”
Quality Standards as “job-aids”
 “Champions for Change”
“Champions for Change”
 Regular Performance Assessment
Regular Performance Assessment
 Quality Services can be provided for BETTER HEALTH!
Quality Services can be provided for BETTER HEALTH!
 Priority Reform Areas: Identified since June 2013 Creating Institutions for the Future 1. a) Khyber Pakhtunkhwa Health Foundation b) Khyber Pakhtunkhwa Health Regulatory Authority c) Medical and Health Institutions Law (Autonomy Act) d) Drug and Food Regulation e) District Health Coordination Boards f) Public Private Partnership Law /Policy 1. Primary Health Care 2. Health Workforce 3. E - Health 36
Priority Reform Areas: Identified since June 2013 Creating Institutions for the Future 1. a) Khyber Pakhtunkhwa Health Foundation b) Khyber Pakhtunkhwa Health Regulatory Authority c) Medical and Health Institutions Law (Autonomy Act) d) Drug and Food Regulation e) District Health Coordination Boards f) Public Private Partnership Law /Policy 1. Primary Health Care 2. Health Workforce 3. E - Health 36
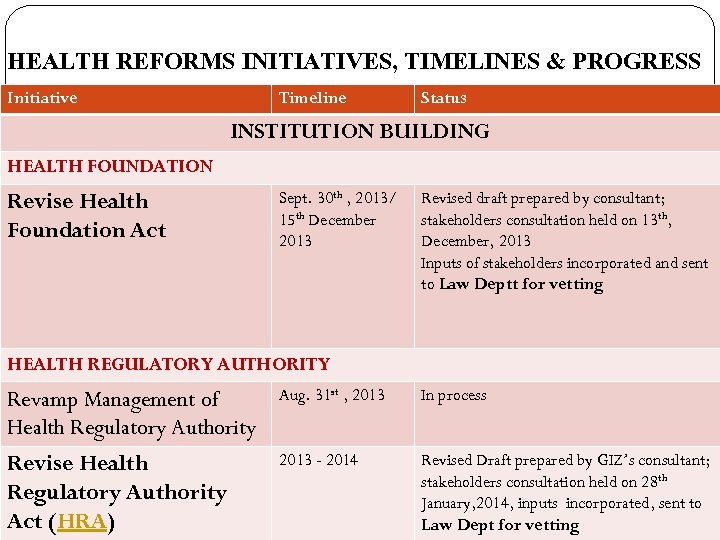 HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS Initiative Timeline Status INSTITUTION BUILDING HEALTH FOUNDATION Revise Health Foundation Act Sept. 30 th , 2013/ 15 th December 2013 Revised draft prepared by consultant; stakeholders consultation held on 13 th, December, 2013 Inputs of stakeholders incorporated and sent to Law Deptt for vetting HEALTH REGULATORY AUTHORITY Revamp Management of Health Regulatory Authority Aug. 31 st , 2013 In process Revise Health Regulatory Authority Act (HRA) 2013 - 2014 Revised Draft prepared by GIZ’s consultant; stakeholders consultation held on 28 th January, 2014, inputs incorporated, sent to 4 Law Dept for vetting
HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS Initiative Timeline Status INSTITUTION BUILDING HEALTH FOUNDATION Revise Health Foundation Act Sept. 30 th , 2013/ 15 th December 2013 Revised draft prepared by consultant; stakeholders consultation held on 13 th, December, 2013 Inputs of stakeholders incorporated and sent to Law Deptt for vetting HEALTH REGULATORY AUTHORITY Revamp Management of Health Regulatory Authority Aug. 31 st , 2013 In process Revise Health Regulatory Authority Act (HRA) 2013 - 2014 Revised Draft prepared by GIZ’s consultant; stakeholders consultation held on 28 th January, 2014, inputs incorporated, sent to 4 Law Dept for vetting
 HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS Initiative Timeline Status INSTITUTION BUILDING MEDICAL & HEALTH INSTITUTIONS Revamp management of Health Institutions Sept. 30 th , 2013 Done/Institution Management Committees for 4 teaching hospitals notified Revise Medical & Health Institution Act (MHI) Sept. 30 th , 2013 Draft prepared by consultant GIZ; inputs of stakeholders incorporated; Submitted to Law Deptt. Reply on the observations of Law Deptt , sent back to Law Deptt DISTRICT HEALTH COORDINATION BOARD District Health Coordination Board (DHCB) Is dependent on new Local Govt. Act 2013 Approved by the Department; will be notified once local governments are in place 5
HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS Initiative Timeline Status INSTITUTION BUILDING MEDICAL & HEALTH INSTITUTIONS Revamp management of Health Institutions Sept. 30 th , 2013 Done/Institution Management Committees for 4 teaching hospitals notified Revise Medical & Health Institution Act (MHI) Sept. 30 th , 2013 Draft prepared by consultant GIZ; inputs of stakeholders incorporated; Submitted to Law Deptt. Reply on the observations of Law Deptt , sent back to Law Deptt DISTRICT HEALTH COORDINATION BOARD District Health Coordination Board (DHCB) Is dependent on new Local Govt. Act 2013 Approved by the Department; will be notified once local governments are in place 5
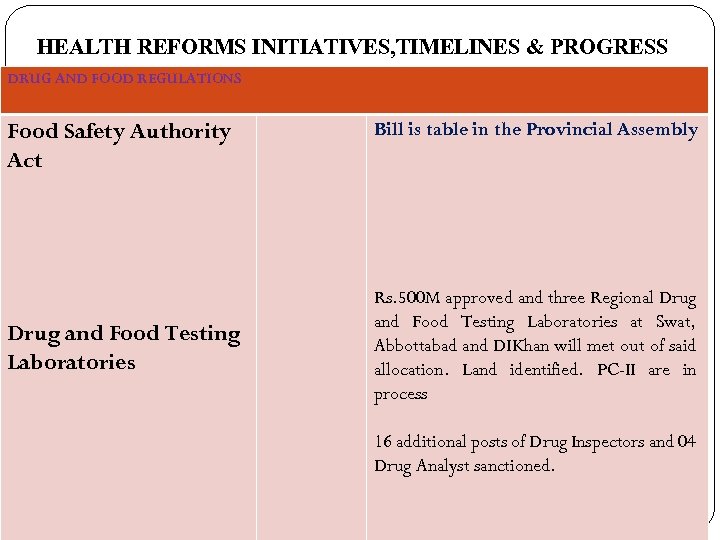 HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS DRUG AND FOOD REGULATIONS Food Safety Authority Act Drug and Food Testing Laboratories Bill is table in the Provincial Assembly Rs. 500 M approved and three Regional Drug and Food Testing Laboratories at Swat, Abbottabad and DIKhan will met out of said allocation. Land identified. PC-II are in process 16 additional posts of Drug Inspectors and 04 Drug Analyst sanctioned. 39
HEALTH REFORMS INITIATIVES, TIMELINES & PROGRESS DRUG AND FOOD REGULATIONS Food Safety Authority Act Drug and Food Testing Laboratories Bill is table in the Provincial Assembly Rs. 500 M approved and three Regional Drug and Food Testing Laboratories at Swat, Abbottabad and DIKhan will met out of said allocation. Land identified. PC-II are in process 16 additional posts of Drug Inspectors and 04 Drug Analyst sanctioned. 39
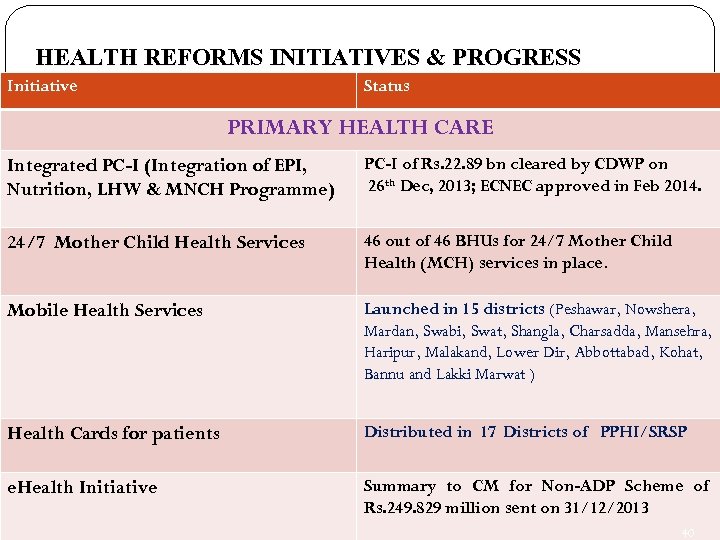 HEALTH REFORMS INITIATIVES & PROGRESS Initiative Status PRIMARY HEALTH CARE Integrated PC-I (Integration of EPI, Nutrition, LHW & MNCH Programme) PC-I of Rs. 22. 89 bn cleared by CDWP on 26 th Dec, 2013; ECNEC approved in Feb 2014. 24/7 Mother Child Health Services 46 out of 46 BHUs for 24/7 Mother Child Health (MCH) services in place. Mobile Health Services Launched in 15 districts (Peshawar, Nowshera, Mardan, Swabi, Swat, Shangla, Charsadda, Mansehra, Haripur, Malakand, Lower Dir, Abbottabad, Kohat, Bannu and Lakki Marwat ) Health Cards for patients Distributed in 17 Districts of PPHI/SRSP e. Health Initiative Summary to CM for Non-ADP Scheme of Rs. 249. 829 million sent on 31/12/2013 40
HEALTH REFORMS INITIATIVES & PROGRESS Initiative Status PRIMARY HEALTH CARE Integrated PC-I (Integration of EPI, Nutrition, LHW & MNCH Programme) PC-I of Rs. 22. 89 bn cleared by CDWP on 26 th Dec, 2013; ECNEC approved in Feb 2014. 24/7 Mother Child Health Services 46 out of 46 BHUs for 24/7 Mother Child Health (MCH) services in place. Mobile Health Services Launched in 15 districts (Peshawar, Nowshera, Mardan, Swabi, Swat, Shangla, Charsadda, Mansehra, Haripur, Malakand, Lower Dir, Abbottabad, Kohat, Bannu and Lakki Marwat ) Health Cards for patients Distributed in 17 Districts of PPHI/SRSP e. Health Initiative Summary to CM for Non-ADP Scheme of Rs. 249. 829 million sent on 31/12/2013 40

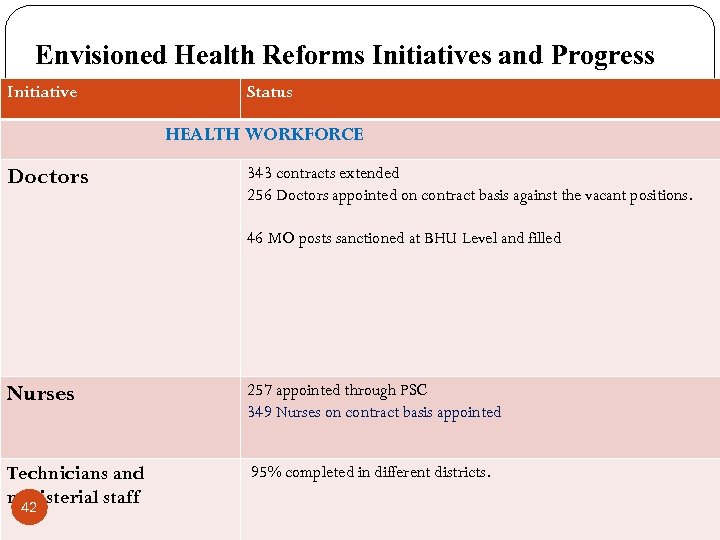 Envisioned Health Reforms Initiatives and Progress Initiative Status HEALTH WORKFORCE Doctors 343 contracts extended 256 Doctors appointed on contract basis against the vacant positions. 46 MO posts sanctioned at BHU Level and filled Nurses 257 appointed through PSC 349 Nurses on contract basis appointed Technicians and ministerial staff 42 95% completed in different districts.
Envisioned Health Reforms Initiatives and Progress Initiative Status HEALTH WORKFORCE Doctors 343 contracts extended 256 Doctors appointed on contract basis against the vacant positions. 46 MO posts sanctioned at BHU Level and filled Nurses 257 appointed through PSC 349 Nurses on contract basis appointed Technicians and ministerial staff 42 95% completed in different districts.
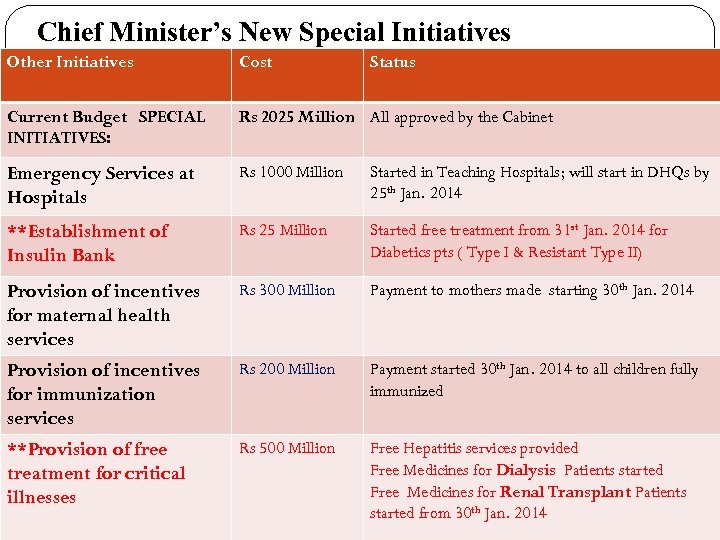 Chief Minister’s New Special Initiatives Other Initiatives Cost Status Current Budget SPECIAL INITIATIVES: Rs 2025 Million All approved by the Cabinet Emergency Services at Hospitals Rs 1000 Million Started in Teaching Hospitals; will start in DHQs by 25 th Jan. 2014 **Establishment of Insulin Bank Rs 25 Million Started free treatment from 31 st Jan. 2014 for Diabetics pts ( Type I & Resistant Type II) Provision of incentives for maternal health services Rs 300 Million Payment to mothers made starting 30 th Jan. 2014 Provision of incentives for immunization services Rs 200 Million Payment started 30 th Jan. 2014 to all children fully immunized **Provision of free treatment for critical illnesses Rs 500 Million Free Hepatitis services provided Free Medicines for Dialysis Patients started Free Medicines for Renal Transplant Patients started from 30 th Jan. 2014 10
Chief Minister’s New Special Initiatives Other Initiatives Cost Status Current Budget SPECIAL INITIATIVES: Rs 2025 Million All approved by the Cabinet Emergency Services at Hospitals Rs 1000 Million Started in Teaching Hospitals; will start in DHQs by 25 th Jan. 2014 **Establishment of Insulin Bank Rs 25 Million Started free treatment from 31 st Jan. 2014 for Diabetics pts ( Type I & Resistant Type II) Provision of incentives for maternal health services Rs 300 Million Payment to mothers made starting 30 th Jan. 2014 Provision of incentives for immunization services Rs 200 Million Payment started 30 th Jan. 2014 to all children fully immunized **Provision of free treatment for critical illnesses Rs 500 Million Free Hepatitis services provided Free Medicines for Dialysis Patients started Free Medicines for Renal Transplant Patients started from 30 th Jan. 2014 10
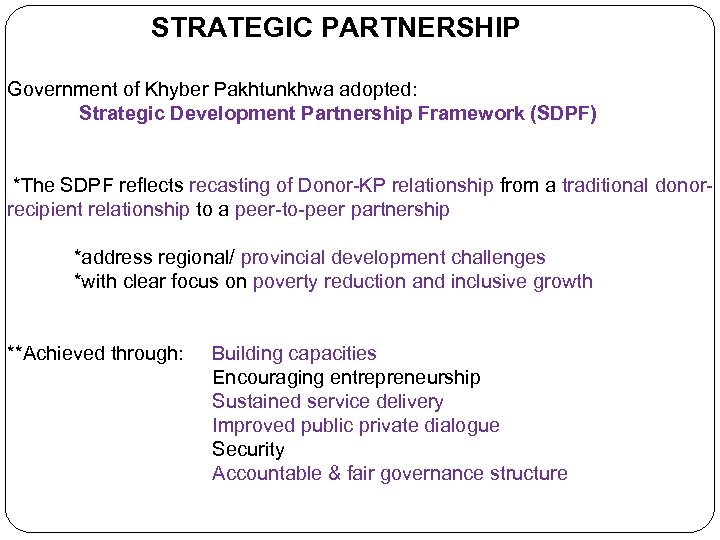 STRATEGIC PARTNERSHIP Government of Khyber Pakhtunkhwa adopted: Strategic Development Partnership Framework (SDPF) *The SDPF reflects recasting of Donor-KP relationship from a traditional donorrecipient relationship to a peer-to-peer partnership *address regional/ provincial development challenges *with clear focus on poverty reduction and inclusive growth **Achieved through: Building capacities Encouraging entrepreneurship Sustained service delivery Improved public private dialogue Security Accountable & fair governance structure
STRATEGIC PARTNERSHIP Government of Khyber Pakhtunkhwa adopted: Strategic Development Partnership Framework (SDPF) *The SDPF reflects recasting of Donor-KP relationship from a traditional donorrecipient relationship to a peer-to-peer partnership *address regional/ provincial development challenges *with clear focus on poverty reduction and inclusive growth **Achieved through: Building capacities Encouraging entrepreneurship Sustained service delivery Improved public private dialogue Security Accountable & fair governance structure
 Strategic Partnership in Health Sector Challenges Low level health status. High poverty and Inequity – adversely affects health status of the population Access to Basic Health Services Risk Adequate Financing Security Human Resource Opportunities Provincial Independence Political commitment Development partners’ international commitments to align with government strategies
Strategic Partnership in Health Sector Challenges Low level health status. High poverty and Inequity – adversely affects health status of the population Access to Basic Health Services Risk Adequate Financing Security Human Resource Opportunities Provincial Independence Political commitment Development partners’ international commitments to align with government strategies
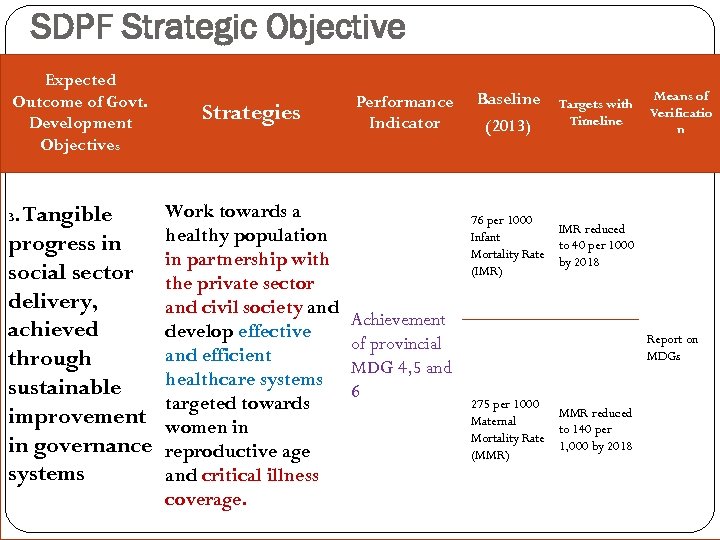 SDPF Strategic Objective Expected Outcome of Govt. Development Objectives Tangible progress in social sector delivery, achieved through sustainable improvement in governance systems 3. Strategies Work towards a healthy population in partnership with the private sector and civil society and develop effective and efficient healthcare systems targeted towards women in reproductive age and critical illness coverage. Performance Indicator Baseline (2013) Targets with Timeline Means of Verificatio n 76 per 1000 IMR reduced Infant to 40 per 1000 Mortality Rate by 2018 (IMR) Achievement of provincial MDG 4, 5 and 6 Report on MDGs 275 per 1000 MMR reduced Maternal to 140 per Mortality Rate 1, 000 by 2018 (MMR)
SDPF Strategic Objective Expected Outcome of Govt. Development Objectives Tangible progress in social sector delivery, achieved through sustainable improvement in governance systems 3. Strategies Work towards a healthy population in partnership with the private sector and civil society and develop effective and efficient healthcare systems targeted towards women in reproductive age and critical illness coverage. Performance Indicator Baseline (2013) Targets with Timeline Means of Verificatio n 76 per 1000 IMR reduced Infant to 40 per 1000 Mortality Rate by 2018 (IMR) Achievement of provincial MDG 4, 5 and 6 Report on MDGs 275 per 1000 MMR reduced Maternal to 140 per Mortality Rate 1, 000 by 2018 (MMR)
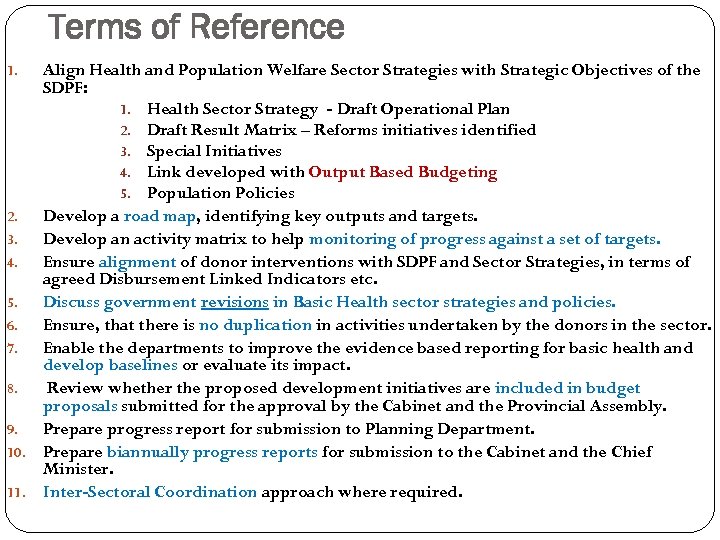 Terms of Reference Align Health and Population Welfare Sector Strategies with Strategic Objectives of the SDPF: 1. Health Sector Strategy - Draft Operational Plan 2. Draft Result Matrix – Reforms initiatives identified 3. Special Initiatives 4. Link developed with Output Based Budgeting 5. Population Policies 2. Develop a road map, identifying key outputs and targets. 3. Develop an activity matrix to help monitoring of progress against a set of targets. 4. Ensure alignment of donor interventions with SDPF and Sector Strategies, in terms of agreed Disbursement Linked Indicators etc. 5. Discuss government revisions in Basic Health sector strategies and policies. 6. Ensure, that there is no duplication in activities undertaken by the donors in the sector. 7. Enable the departments to improve the evidence based reporting for basic health and develop baselines or evaluate its impact. 8. Review whether the proposed development initiatives are included in budget proposals submitted for the approval by the Cabinet and the Provincial Assembly. 9. Prepare progress report for submission to Planning Department. 10. Prepare biannually progress reports for submission to the Cabinet and the Chief Minister. 11. Inter-Sectoral Coordination approach where required. 1.
Terms of Reference Align Health and Population Welfare Sector Strategies with Strategic Objectives of the SDPF: 1. Health Sector Strategy - Draft Operational Plan 2. Draft Result Matrix – Reforms initiatives identified 3. Special Initiatives 4. Link developed with Output Based Budgeting 5. Population Policies 2. Develop a road map, identifying key outputs and targets. 3. Develop an activity matrix to help monitoring of progress against a set of targets. 4. Ensure alignment of donor interventions with SDPF and Sector Strategies, in terms of agreed Disbursement Linked Indicators etc. 5. Discuss government revisions in Basic Health sector strategies and policies. 6. Ensure, that there is no duplication in activities undertaken by the donors in the sector. 7. Enable the departments to improve the evidence based reporting for basic health and develop baselines or evaluate its impact. 8. Review whether the proposed development initiatives are included in budget proposals submitted for the approval by the Cabinet and the Provincial Assembly. 9. Prepare progress report for submission to Planning Department. 10. Prepare biannually progress reports for submission to the Cabinet and the Chief Minister. 11. Inter-Sectoral Coordination approach where required. 1.
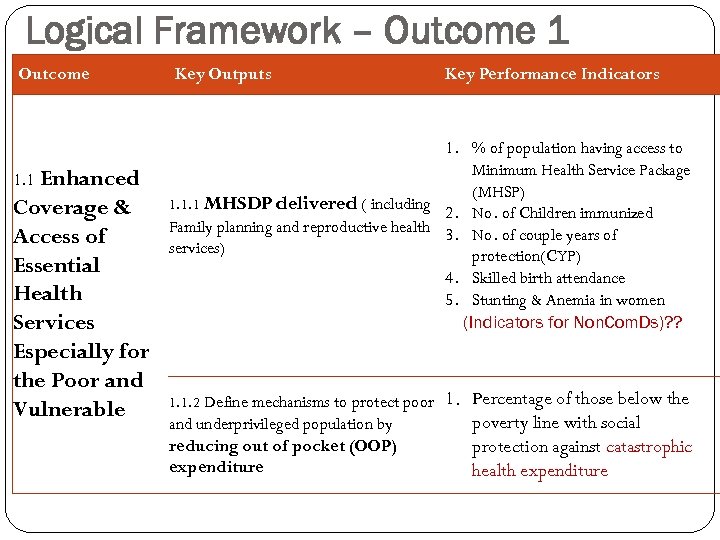 Logical Framework – Outcome 1 Outcome Enhanced Coverage & Access of Essential Health Services Especially for the Poor and Vulnerable 1. 1 Key Outputs Key Performance Indicators 1. % of population having access to Minimum Health Service Package (MHSP) 1. 1. 1 MHSDP delivered ( including 2. No. of Children immunized Family planning and reproductive health 3. No. of couple years of services) protection(CYP) 4. Skilled birth attendance 5. Stunting & Anemia in women (Indicators for Non. Com. Ds)? ? 1. 1. 2 Define mechanisms to protect poor and underprivileged population by reducing out of pocket (OOP) expenditure 1. Percentage of those below the poverty line with social protection against catastrophic health expenditure
Logical Framework – Outcome 1 Outcome Enhanced Coverage & Access of Essential Health Services Especially for the Poor and Vulnerable 1. 1 Key Outputs Key Performance Indicators 1. % of population having access to Minimum Health Service Package (MHSP) 1. 1. 1 MHSDP delivered ( including 2. No. of Children immunized Family planning and reproductive health 3. No. of couple years of services) protection(CYP) 4. Skilled birth attendance 5. Stunting & Anemia in women (Indicators for Non. Com. Ds)? ? 1. 1. 2 Define mechanisms to protect poor and underprivileged population by reducing out of pocket (OOP) expenditure 1. Percentage of those below the poverty line with social protection against catastrophic health expenditure
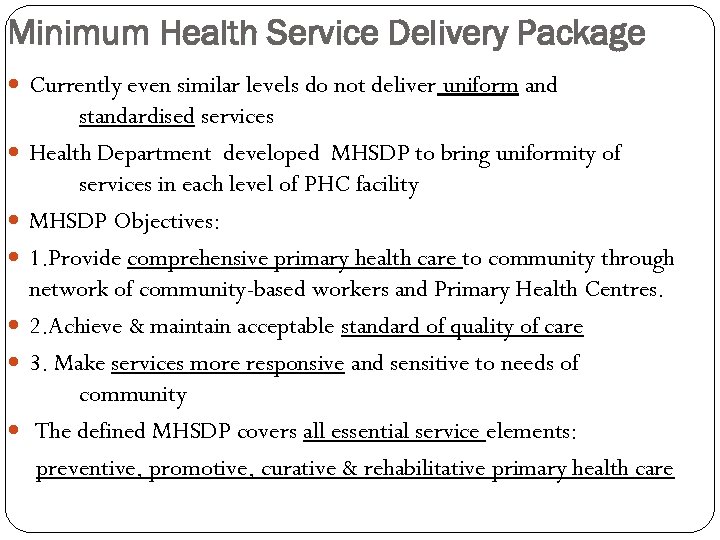 Minimum Health Service Delivery Package Currently even similar levels do not deliver uniform and standardised services Health Department developed MHSDP to bring uniformity of services in each level of PHC facility MHSDP Objectives: 1. Provide comprehensive primary health care to community through network of community-based workers and Primary Health Centres. 2. Achieve & maintain acceptable standard of quality of care 3. Make services more responsive and sensitive to needs of community The defined MHSDP covers all essential service elements: preventive, promotive, curative & rehabilitative primary health care
Minimum Health Service Delivery Package Currently even similar levels do not deliver uniform and standardised services Health Department developed MHSDP to bring uniformity of services in each level of PHC facility MHSDP Objectives: 1. Provide comprehensive primary health care to community through network of community-based workers and Primary Health Centres. 2. Achieve & maintain acceptable standard of quality of care 3. Make services more responsive and sensitive to needs of community The defined MHSDP covers all essential service elements: preventive, promotive, curative & rehabilitative primary health care
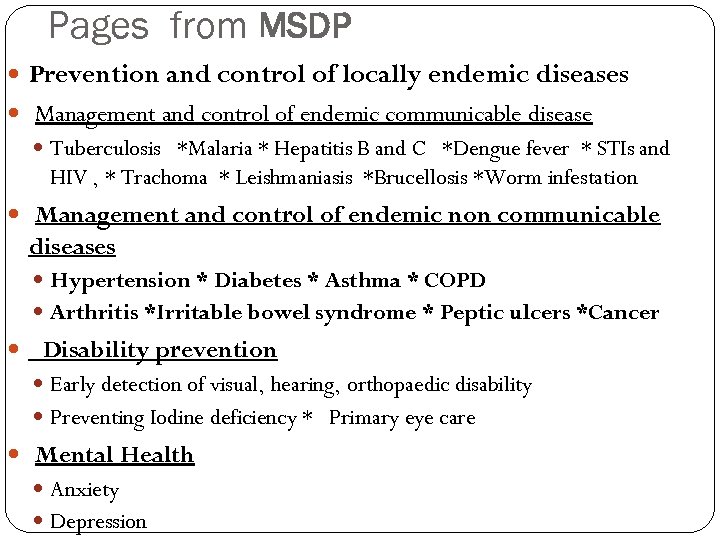 Pages from MSDP Prevention and control of locally endemic diseases Management and control of endemic communicable disease Tuberculosis *Malaria * Hepatitis B and C *Dengue fever * STIs and HIV , * Trachoma * Leishmaniasis *Brucellosis *Worm infestation Management and control of endemic non communicable diseases Hypertension * Diabetes * Asthma * COPD Arthritis *Irritable bowel syndrome * Peptic ulcers *Cancer Disability prevention Early detection of visual, hearing, orthopaedic disability Preventing Iodine deficiency * Primary eye care Mental Health Anxiety Depression
Pages from MSDP Prevention and control of locally endemic diseases Management and control of endemic communicable disease Tuberculosis *Malaria * Hepatitis B and C *Dengue fever * STIs and HIV , * Trachoma * Leishmaniasis *Brucellosis *Worm infestation Management and control of endemic non communicable diseases Hypertension * Diabetes * Asthma * COPD Arthritis *Irritable bowel syndrome * Peptic ulcers *Cancer Disability prevention Early detection of visual, hearing, orthopaedic disability Preventing Iodine deficiency * Primary eye care Mental Health Anxiety Depression
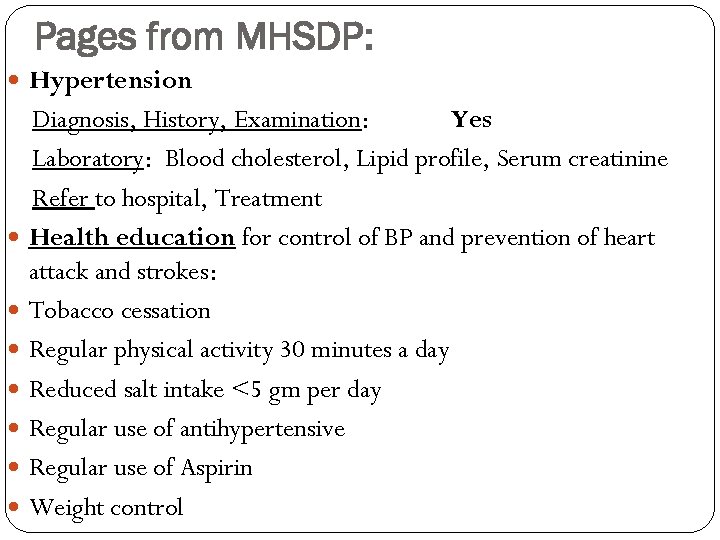 Pages from MHSDP: Hypertension Diagnosis, History, Examination: Yes Laboratory: Blood cholesterol, Lipid profile, Serum creatinine Refer to hospital, Treatment Health education for control of BP and prevention of heart attack and strokes: Tobacco cessation Regular physical activity 30 minutes a day Reduced salt intake <5 gm per day Regular use of antihypertensive Regular use of Aspirin Weight control
Pages from MHSDP: Hypertension Diagnosis, History, Examination: Yes Laboratory: Blood cholesterol, Lipid profile, Serum creatinine Refer to hospital, Treatment Health education for control of BP and prevention of heart attack and strokes: Tobacco cessation Regular physical activity 30 minutes a day Reduced salt intake <5 gm per day Regular use of antihypertensive Regular use of Aspirin Weight control
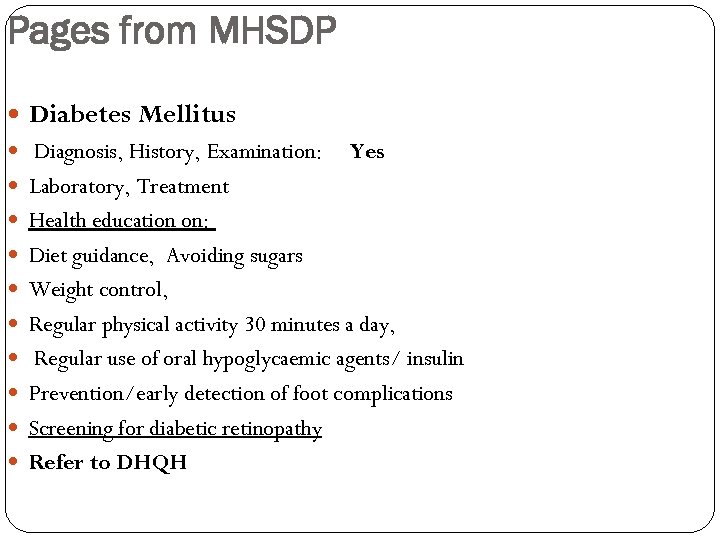 Pages from MHSDP Diabetes Mellitus Diagnosis, History, Examination: Yes Laboratory, Treatment Health education on: Diet guidance, Avoiding sugars Weight control, Regular physical activity 30 minutes a day, Regular use of oral hypoglycaemic agents/ insulin Prevention/early detection of foot complications Screening for diabetic retinopathy Refer to DHQH
Pages from MHSDP Diabetes Mellitus Diagnosis, History, Examination: Yes Laboratory, Treatment Health education on: Diet guidance, Avoiding sugars Weight control, Regular physical activity 30 minutes a day, Regular use of oral hypoglycaemic agents/ insulin Prevention/early detection of foot complications Screening for diabetic retinopathy Refer to DHQH
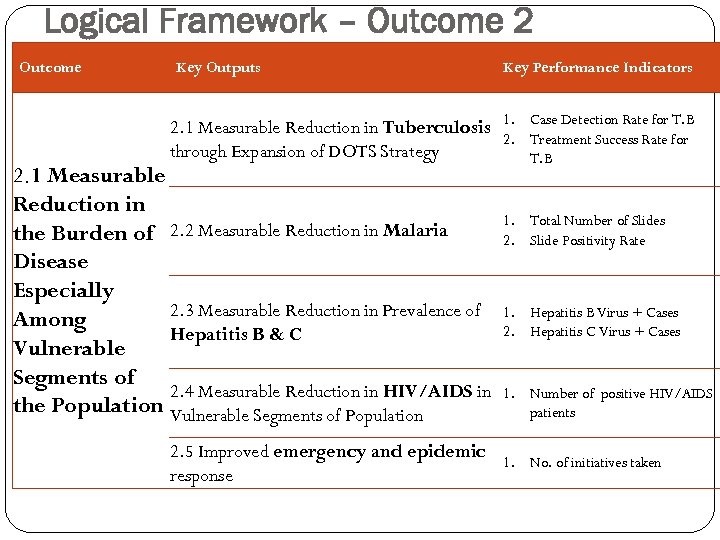 Logical Framework – Outcome 2 Outcome Key Outputs Key Performance Indicators 2. 1 Measurable Reduction in Tuberculosis 1. 2. through Expansion of DOTS Strategy 2. 1 Measurable Reduction in the Burden of 2. 2 Measurable Reduction in Malaria Disease Especially 2. 3 Measurable Reduction in Prevalence of Among Hepatitis B & C Vulnerable Segments of 2. 4 Measurable Reduction in HIV/AIDS in the Population Vulnerable Segments of Population Case Detection Rate for T. B Treatment Success Rate for T. B 1. Total Number of Slides 2. Slide Positivity Rate 1. Hepatitis B Virus + Cases 2. Hepatitis C Virus + Cases 1. Number of positive HIV/AIDS patients 2. 5 Improved emergency and epidemic 1. response No. of initiatives taken
Logical Framework – Outcome 2 Outcome Key Outputs Key Performance Indicators 2. 1 Measurable Reduction in Tuberculosis 1. 2. through Expansion of DOTS Strategy 2. 1 Measurable Reduction in the Burden of 2. 2 Measurable Reduction in Malaria Disease Especially 2. 3 Measurable Reduction in Prevalence of Among Hepatitis B & C Vulnerable Segments of 2. 4 Measurable Reduction in HIV/AIDS in the Population Vulnerable Segments of Population Case Detection Rate for T. B Treatment Success Rate for T. B 1. Total Number of Slides 2. Slide Positivity Rate 1. Hepatitis B Virus + Cases 2. Hepatitis C Virus + Cases 1. Number of positive HIV/AIDS patients 2. 5 Improved emergency and epidemic 1. response No. of initiatives taken
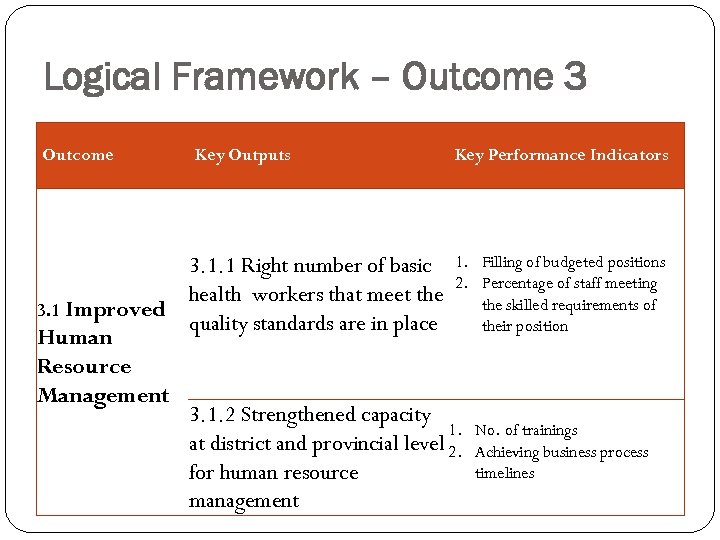 Logical Framework – Outcome 3 Outcome Key Outputs Key Performance Indicators 3. 1. 1 Right number of basic 1. Filling of budgeted positions 2. Percentage of staff meeting health workers that meet the skilled requirements of 3. 1 Improved quality standards are in place their position Human Resource Management 3. 1. 2 Strengthened capacity 1. No. of trainings at district and provincial level 2. Achieving business process timelines for human resource management
Logical Framework – Outcome 3 Outcome Key Outputs Key Performance Indicators 3. 1. 1 Right number of basic 1. Filling of budgeted positions 2. Percentage of staff meeting health workers that meet the skilled requirements of 3. 1 Improved quality standards are in place their position Human Resource Management 3. 1. 2 Strengthened capacity 1. No. of trainings at district and provincial level 2. Achieving business process timelines for human resource management
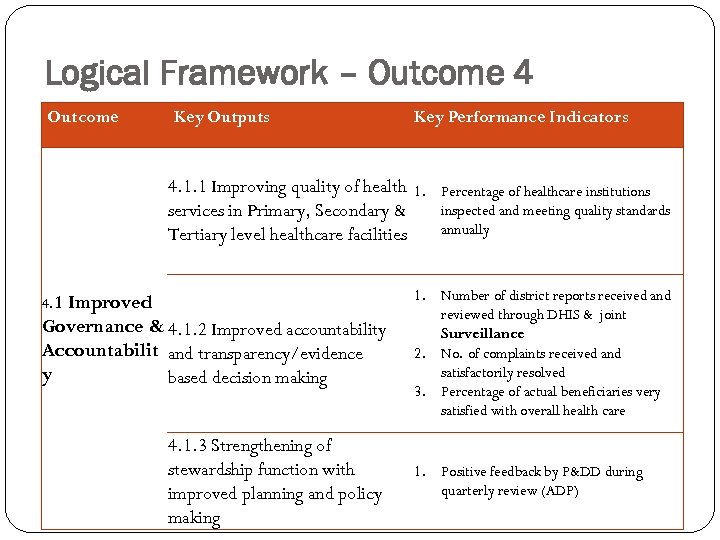 Logical Framework – Outcome 4 Outcome Key Outputs Key Performance Indicators 4. 1. 1 Improving quality of health 1. services in Primary, Secondary & Tertiary level healthcare facilities 4. 1 Improved Governance & 4. 1. 2 Improved accountability Accountabilit and transparency/evidence y based decision making 4. 1. 3 Strengthening of stewardship function with improved planning and policy making Percentage of healthcare institutions inspected and meeting quality standards annually 1. Number of district reports received and reviewed through DHIS & joint Surveillance 2. No. of complaints received and satisfactorily resolved 3. Percentage of actual beneficiaries very satisfied with overall health care 1. Positive feedback by P&DD during quarterly review (ADP)
Logical Framework – Outcome 4 Outcome Key Outputs Key Performance Indicators 4. 1. 1 Improving quality of health 1. services in Primary, Secondary & Tertiary level healthcare facilities 4. 1 Improved Governance & 4. 1. 2 Improved accountability Accountabilit and transparency/evidence y based decision making 4. 1. 3 Strengthening of stewardship function with improved planning and policy making Percentage of healthcare institutions inspected and meeting quality standards annually 1. Number of district reports received and reviewed through DHIS & joint Surveillance 2. No. of complaints received and satisfactorily resolved 3. Percentage of actual beneficiaries very satisfied with overall health care 1. Positive feedback by P&DD during quarterly review (ADP)
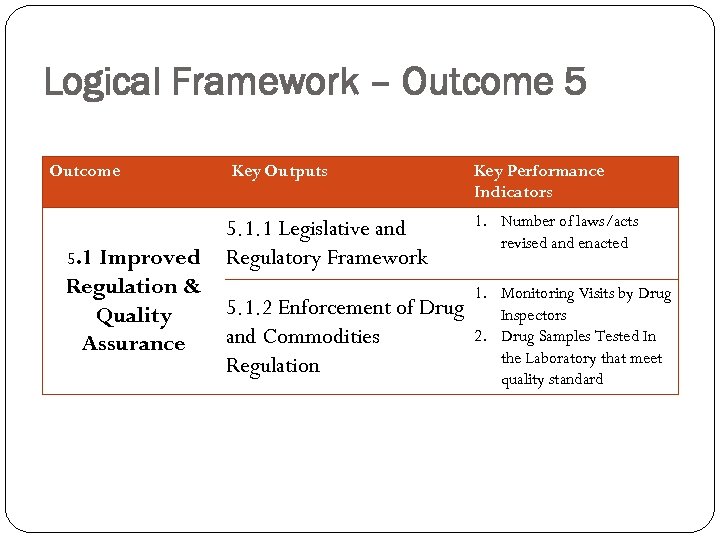 Logical Framework – Outcome 5. 1 Improved Key Outputs 5. 1. 1 Legislative and Regulatory Framework Regulation & 5. 1. 2 Enforcement of Drug Quality and Commodities Assurance Regulation Key Performance Indicators 1. Number of laws/acts revised and enacted 1. Monitoring Visits by Drug Inspectors 2. Drug Samples Tested In the Laboratory that meet quality standard
Logical Framework – Outcome 5. 1 Improved Key Outputs 5. 1. 1 Legislative and Regulatory Framework Regulation & 5. 1. 2 Enforcement of Drug Quality and Commodities Assurance Regulation Key Performance Indicators 1. Number of laws/acts revised and enacted 1. Monitoring Visits by Drug Inspectors 2. Drug Samples Tested In the Laboratory that meet quality standard
 NON COMMUNICABLE DISEASES
NON COMMUNICABLE DISEASES
 BACKGROUND FACTS q Increasing burden of Non Communicable Diseases (Heart diseases, cancer, diabetes, chronic pulmonary & mental diseases) q High prevalence of risk factors ( Tobacco, alcohol, obesity, blood pressure, diet and inactivity) q Lack of public awareness q Poor health seeking behavior q Non availability/ inadequate availability of treatments q Low level of service provision, equipment & availability of staff Lack of robust laboratory services at district level q Opportunities of treatment: Contrasts between poor /rich, urban/ rural , men/women
BACKGROUND FACTS q Increasing burden of Non Communicable Diseases (Heart diseases, cancer, diabetes, chronic pulmonary & mental diseases) q High prevalence of risk factors ( Tobacco, alcohol, obesity, blood pressure, diet and inactivity) q Lack of public awareness q Poor health seeking behavior q Non availability/ inadequate availability of treatments q Low level of service provision, equipment & availability of staff Lack of robust laboratory services at district level q Opportunities of treatment: Contrasts between poor /rich, urban/ rural , men/women
 Preventable Risk Factors Changing Lifestyle can potentially avoid: Coronary heart ds cases: Up to 80% Diabetes types 2 case: Upto 90% Cancers: one third cases avoided by eating healthily, maintaining normal weight & exercising throughout life. In high-risk populations, an optimum fish consumption of 40– 60 grams per day leads to 50% reduction in death from coronary heart disease Daily intake of fresh fruit and vegetables : 400– 500 grams/day)recommended to reduce risk of coronary heart disease, stroke and high blood pressure
Preventable Risk Factors Changing Lifestyle can potentially avoid: Coronary heart ds cases: Up to 80% Diabetes types 2 case: Upto 90% Cancers: one third cases avoided by eating healthily, maintaining normal weight & exercising throughout life. In high-risk populations, an optimum fish consumption of 40– 60 grams per day leads to 50% reduction in death from coronary heart disease Daily intake of fresh fruit and vegetables : 400– 500 grams/day)recommended to reduce risk of coronary heart disease, stroke and high blood pressure
 Pragmatic decisions: Prohibit smoking in public areas Control alcohol abusers Encourage physical activity Promote healthy diet Improve primary health care for screening and early detection of chronic diseases Overcome tendency to rely on disjointed set of Initiatives: Factor “integration” Development & implementation of NCD Prevention Strategy : Integrate actions with existing public health system, combine prevention and health promotion and harness potential within PPP partnerships
Pragmatic decisions: Prohibit smoking in public areas Control alcohol abusers Encourage physical activity Promote healthy diet Improve primary health care for screening and early detection of chronic diseases Overcome tendency to rely on disjointed set of Initiatives: Factor “integration” Development & implementation of NCD Prevention Strategy : Integrate actions with existing public health system, combine prevention and health promotion and harness potential within PPP partnerships
 Limitations Political Commitment : Clear, strong and sustained Successful implementation of plan: Setting up of appropriate infrastructure & public health workforce with adequate capacity for core public health functions Has implications for need to build capacity and related infrastructure as a parallel process. ‘Development policy framework’ encourages private- sector participation in state activities Has its own challenges: KP has been lessons learnt in PPP undertakings
Limitations Political Commitment : Clear, strong and sustained Successful implementation of plan: Setting up of appropriate infrastructure & public health workforce with adequate capacity for core public health functions Has implications for need to build capacity and related infrastructure as a parallel process. ‘Development policy framework’ encourages private- sector participation in state activities Has its own challenges: KP has been lessons learnt in PPP undertakings
 Policy Direction of Khyber Pakhtunkhwa Provincial Health Department shall aim to develop an integrated approach to chronic diseases at several levels, capitalize on strengths of partnerships, build on existing efforts & bring focus of primary health care on chronic disease prevention Life Course Approach : Seek to integrate strategies with communicable disease control Enable development of sustainable public health system for all diseases
Policy Direction of Khyber Pakhtunkhwa Provincial Health Department shall aim to develop an integrated approach to chronic diseases at several levels, capitalize on strengths of partnerships, build on existing efforts & bring focus of primary health care on chronic disease prevention Life Course Approach : Seek to integrate strategies with communicable disease control Enable development of sustainable public health system for all diseases
 THANK YOU
THANK YOU


