SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) 8 December 2017 DEFINITION

SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) 8 December 2017
DEFINITION Inflammatory disease Multi-system disease Autoimmune disease Autoantibodies Immune complexes 8 December 2017
EPIDEMIOLOGY OF SLE Frequency: 14.6/100,000 to 50.8/100,000 Incidence: 1.8-7.6/100,000 per year Internationally: worldwide Age: 15-45 years Gender: F/M = 9/1 Race: blacks: whites = 4:1 8 December 2017
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) Prototypic autoimmune disease Loss of tolerance to self leads to immune system mediated damage to self Etiology of SLE unknown Each patient unique 8 December 2017
Pathogenesis of SLE Genetic Factors Autoimmunity genes on chromosome 16 Increased frequency in close relatives Ethnic susceptibility HLA-DR2 and –DR3 associations Inherited complement deficiencies (C1q, C2, C4) 8 December 2017
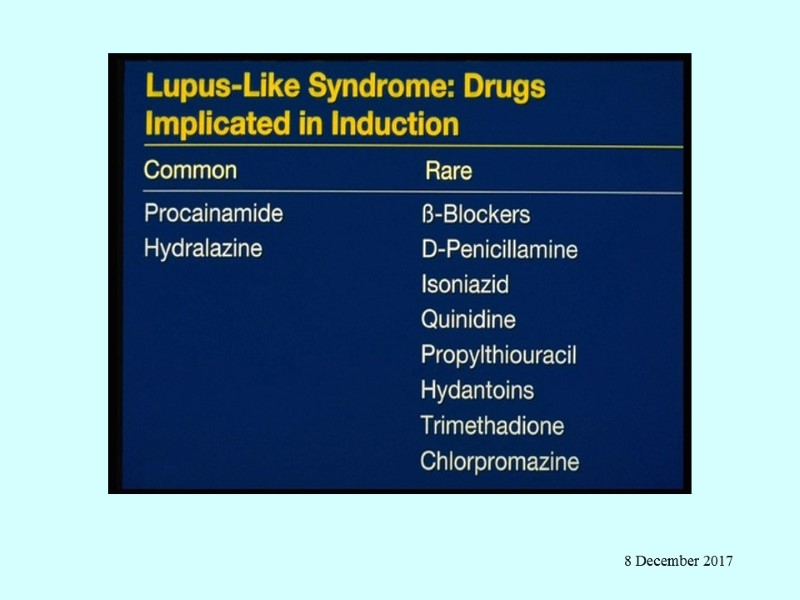
Pathogenesis of SLE Environmental factors Ultraviolet light (flares in 70%) Increased apoptosis of skin cells Altering of DNA and intracellular proteins – Ag Drug-induced lupus Infectious triggers EBV Hormonal factors Female, pregnancy, delivery Oral contraceptives, HRT (estradiol receptors on Ly) 8 December 2017
SLE - Pathogenesis Susceptibility genes (usually multiple) + Triggering factors (probably environmental) ABNORMAL IMMUNE RESPONSE 8 December 2017
SLE - Pathogenesis Activation of innate immunity (dendritic cells) By DNA By DNA in IC By RNA in RNA/self-antigens Lowered activation thresholds of adaptive immunity (antigen specific T-ly and B-ly) Ineffective regulatory CD4+ and inhibitory CD8+ Abnormal function of T-reg Reduced clearance of apoptotic cells and IC 8 December 2017
Pathogenesis SLE Apoptosis – programmed cells death Blebs contain self-antigens DNA RNA Phospholipids Excess of proinflammatory cytokines TNF, IFN -γ, BLyS – B lymphocyte stimulator, IL-10 Inadequate secretion by T-ly and NK regulatory cytokines IL-2 and TGF Deficit of Reg CD4+ and Inh CD8+ 8 December 2017
Pathogenesis SLE Sustain production of pathogenic autoantibodies directed against self-antigens and IC Binding of IC to target tissues Activation of complement system and phagocytic cells that recognize Ig-coating circulation blood cells Tissue damage - release of chemotoxins, cytokines, chemokines, vasoactive peptides, destructive enzymes 8 December 2017
Pathology SLE Skin: Ig deposition in DEJ, injury to keratinocytes, T-ly induced inflammation Renal: 6 types with active /chronic changes Vasculitis- leukocytoclasis Lymph nodes – nonspecific inflammtion 8 December 2017
TYPES OF LUPUS Discoid LE Subacute cutaneous LE Systemic LE Drug-induced LE Overlap syndrome 8 December 2017
Clinical Features of SLE Constitutional symptoms – nonspecific but can be profound. Fatigue Appetite loss Weight loss Fever 8 December 2017
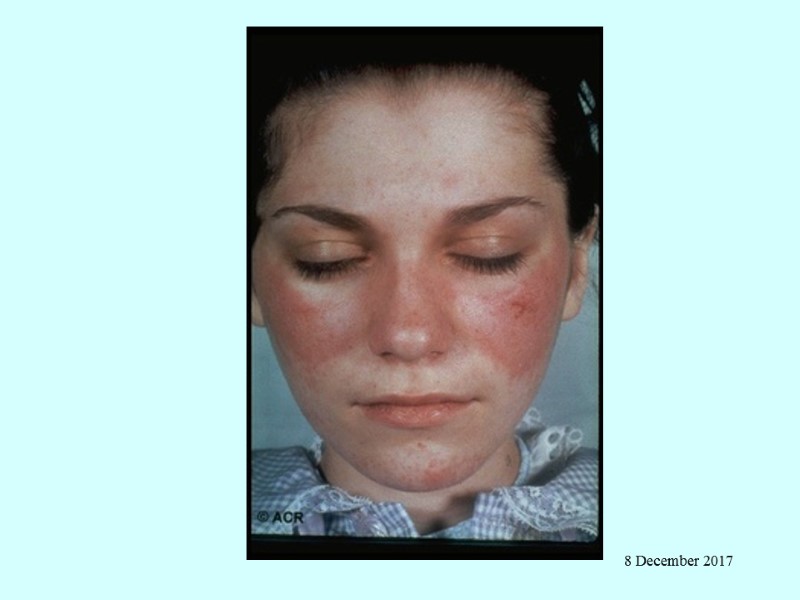
Cutaneous manifestations Malar rash in 50% Photosensitive Transient or chronic Photosensitivity (50%) – usually to UV-B Discoid Lupus annular, scaly hyperpigmented erythematous plaques; scarring; atrophic centers SLE – 25% have DLE 10% with DLE will develop SLE 25% ANA pos Most anti Ro (SS-A) pos 8 December 2017
Cutaneous manifestations Subacute cutaneous lupus – small erythematous papules that coalesce into patterns, non scarring Upper torso, next, arms Ro (SS-A) association 10% of SLE patients have it May have this alone without systemic disease Lupus profundus/panniculitis Nodules in dermis or subcutaneous tissue Nodules may be under skin lesions or under normal skin (panniculitis) Oral ulcers 8 December 2017
Cutaneous manifestations Alopecia – 70% Scarring, discoid lesion Non scarring Vascular Periangular erythema Livido reticularis Telangiectasias Raynaud’s phenomenon Vasculitis Rare subcutaneous nodule 8 December 2017
8 December 2017

8 December 2017
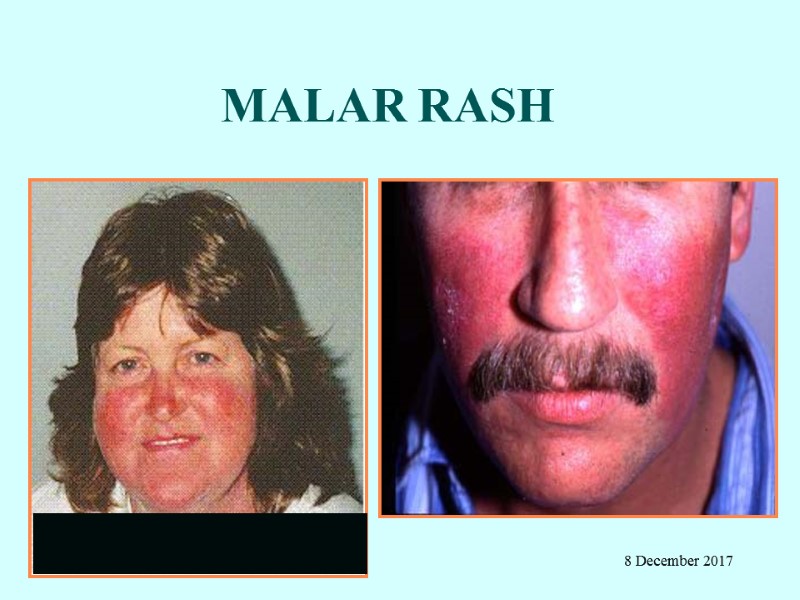
MALAR RASH 8 December 2017
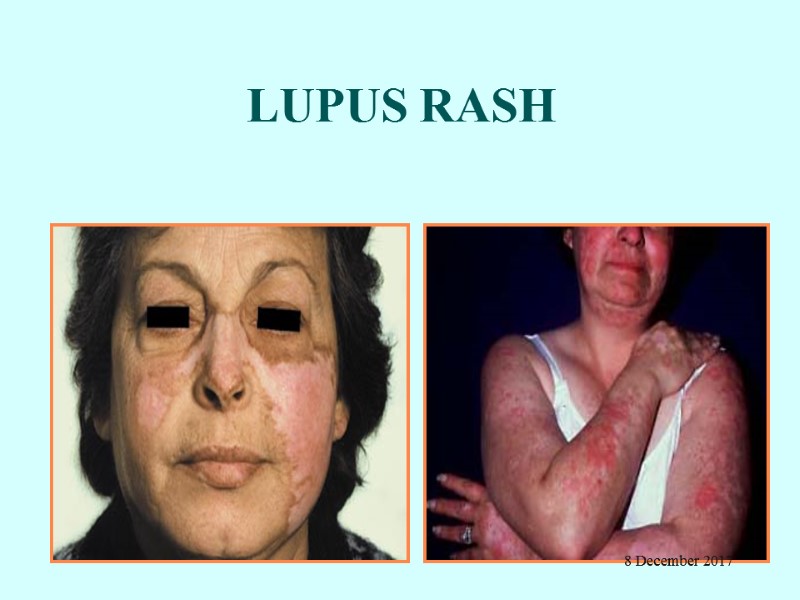
LUPUS RASH 8 December 2017

8 December 2017
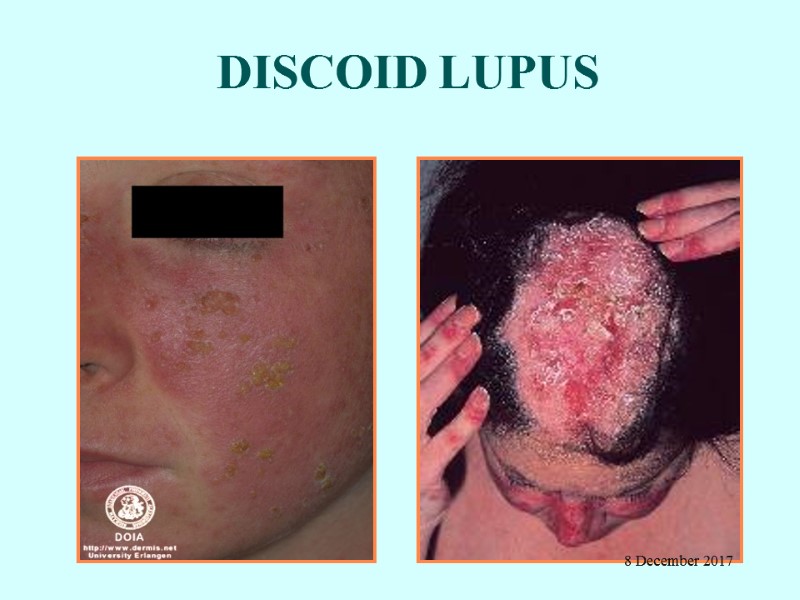
DISCOID LUPUS 8 December 2017
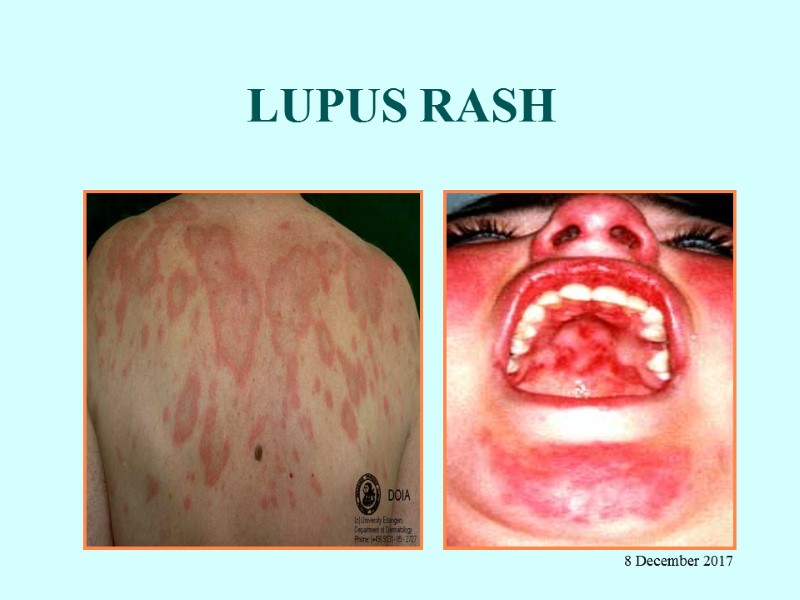
LUPUS RASH 8 December 2017

VASCULAR SKIN CHANGES RAYNAUD’S PHENOMENON LIVEDO RETICULARIS 8 December 2017

SLE SKIN PATHOLOGY 8 December 2017
Musculoskeletal features Myalgia, arthralgia Arthritis Migratory Non-erosive ?? Symmetric Peripheral Exudative Inflammatory fluid Periarthritis and deformity Tendon ruptures AVN Myositis/myopathy Drug induced complications 8 December 2017

8 December 2017
Pulmonary manifestations Pleurisy and pleuritis Exudate ANA pos, low complement Normal glucose Acute pneumonitis Chronic pneumonitis, ILD, fibrosis Pulmonary hypertension “Shrinking lung” Isolated diffusing capacity impairment PE (APLA) ---------------------------- Infections always to be excluded !!!!!!!!! 8 December 2017
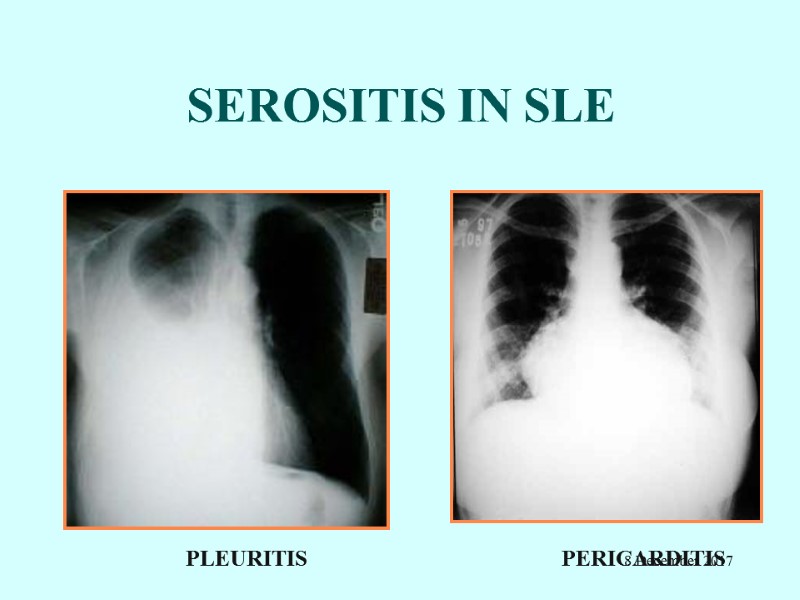
SEROSITIS IN SLE PLEURITIS PERICARDITIS 8 December 2017
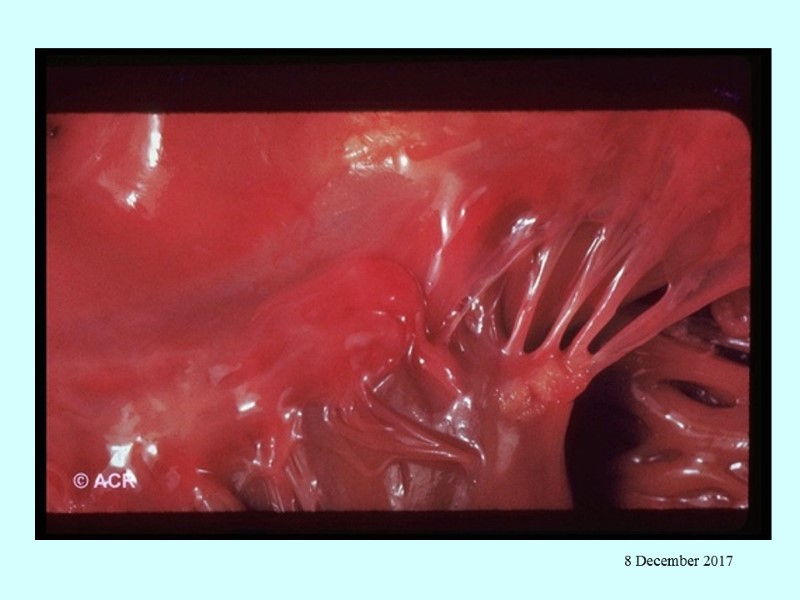
Cardiac manifestations Pericardial involvement Pleurisy Pleuritis Tamponade Myocardial involvement – acute or chronic Endocardial involvement - Libman-Sacks (verrucous endocarditis) - Diffuse valvular thickening Coronary artery disease - premature 8 December 2017
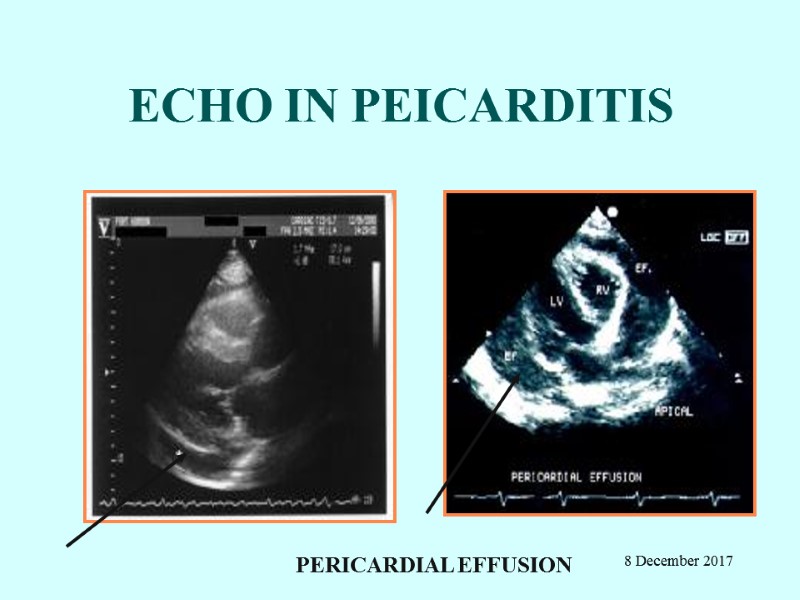
ECHO IN PEICARDITIS PERICARDIAL EFFUSION 8 December 2017
Hematologic manifestations Anemia “Chronic disease” Hemolytic Leukopenia lymphopenia Thrombocytopenia Early ITP Hypercoagulable state - associated with antiphospholipid antibodies 8 December 2017
Gastrointestinal manifestations Dyspepsia, dysphagia – common Acute abdomen Vasculitis Serositis (peritonitis) Pancreatitis – usually mild, subclinical Autoimmune (lupoid) hepatitis 8 December 2017
Neuropsychiatric Diffuse CNS lupus Cognitive dysfunction Headache Psychosis Seizures – can be any kind, usually grand mal Meningitis Focal cerebral dysfunction - Associated with antiphospholipid antibodies - Stroke (5%) 8 December 2017
Other neural system features Peripheral neuropathy Cranial neuropathy – usually affects eyes Transverse myelitis Neuromyelitis optica Myelopathy Eye – cytoid bodies (vasculitis of retinal capillaries) ______________________________ Infection always must be excluded!!!!!!!!!!! 8 December 2017
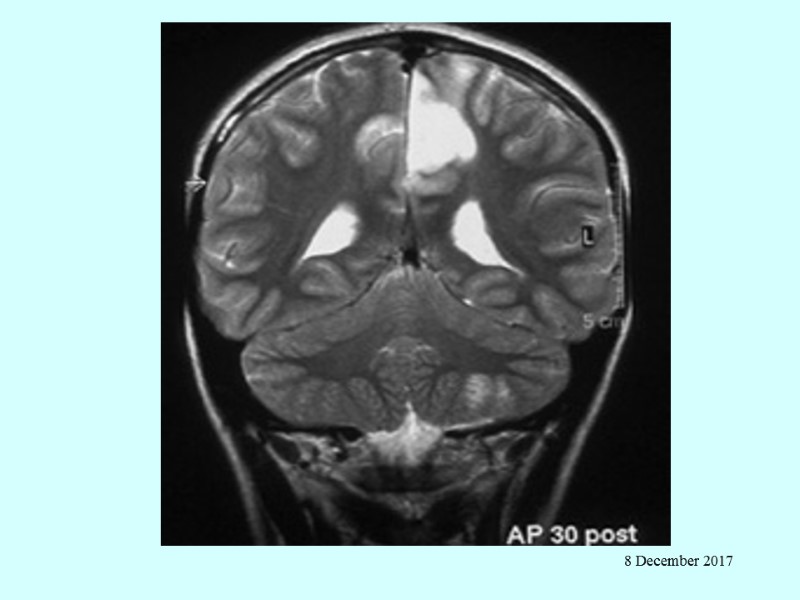
8 December 2017
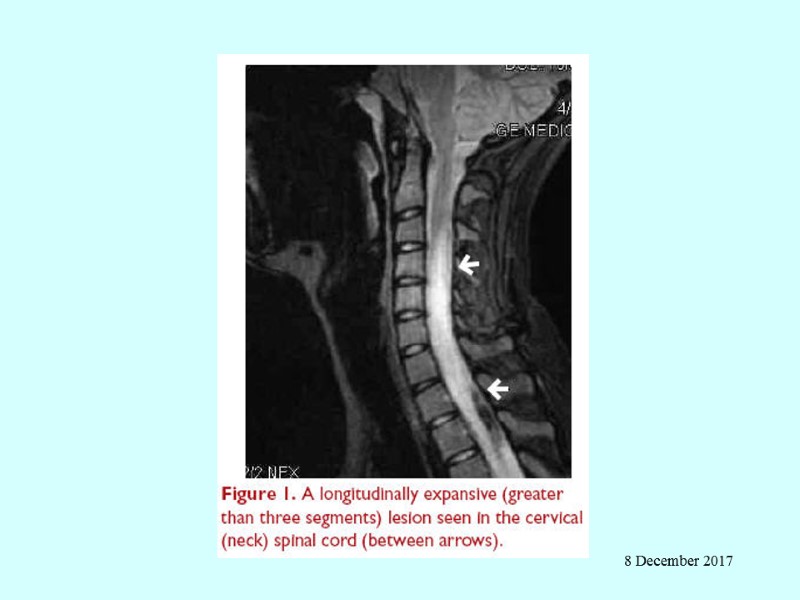
8 December 2017
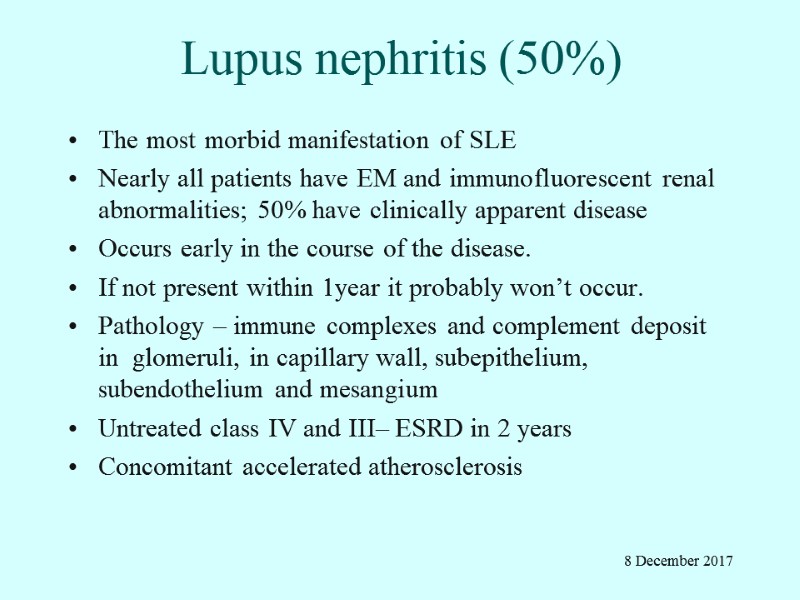
Lupus nephritis (50%) The most morbid manifestation of SLE Nearly all patients have EM and immunofluorescent renal abnormalities; 50% have clinically apparent disease Occurs early in the course of the disease. If not present within 1year it probably won’t occur. Pathology – immune complexes and complement deposit in glomeruli, in capillary wall, subepithelium, subendothelium and mesangium Untreated class IV and III– ESRD in 2 years Concomitant accelerated atherosclerosis 8 December 2017
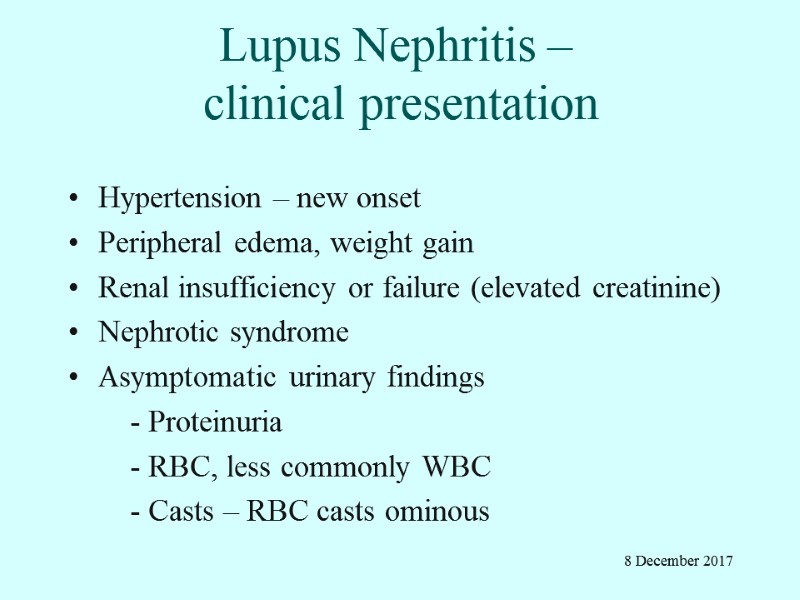
Lupus Nephritis – clinical presentation Hypertension – new onset Peripheral edema, weight gain Renal insufficiency or failure (elevated creatinine) Nephrotic syndrome Asymptomatic urinary findings - Proteinuria - RBC, less commonly WBC - Casts – RBC casts ominous 8 December 2017
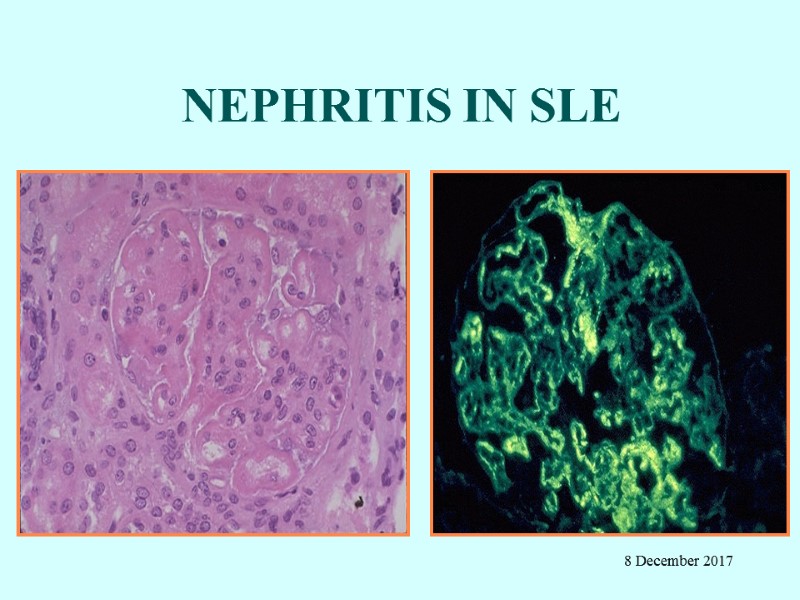
NEPHRITIS IN SLE 8 December 2017
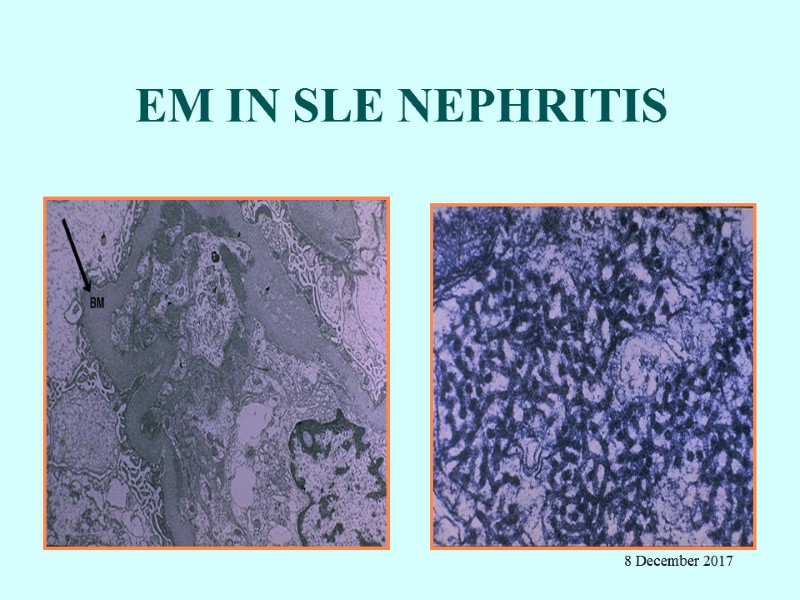
EM IN SLE NEPHRITIS 8 December 2017
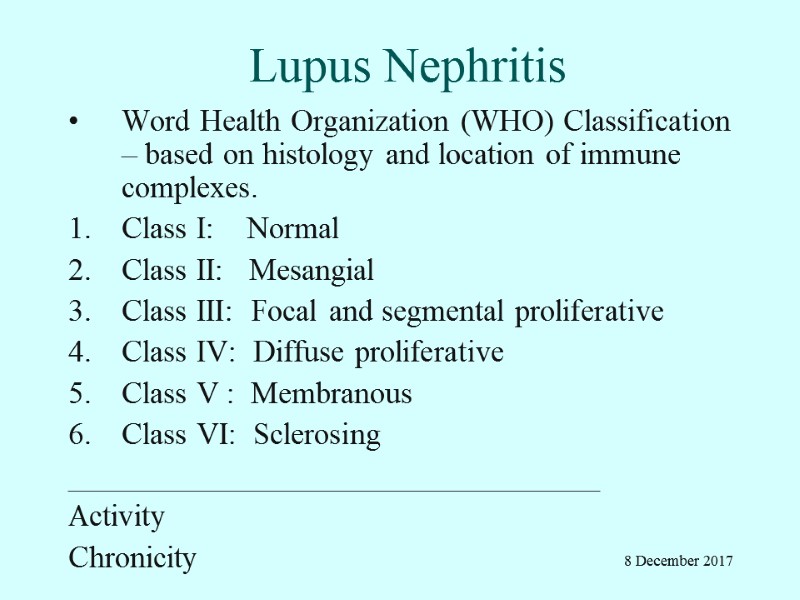
Lupus Nephritis Word Health Organization (WHO) Classification – based on histology and location of immune complexes. Class I: Normal Class II: Mesangial Class III: Focal and segmental proliferative Class IV: Diffuse proliferative Class V : Membranous Class VI: Sclerosing __________________________________ Activity Chronicity 8 December 2017
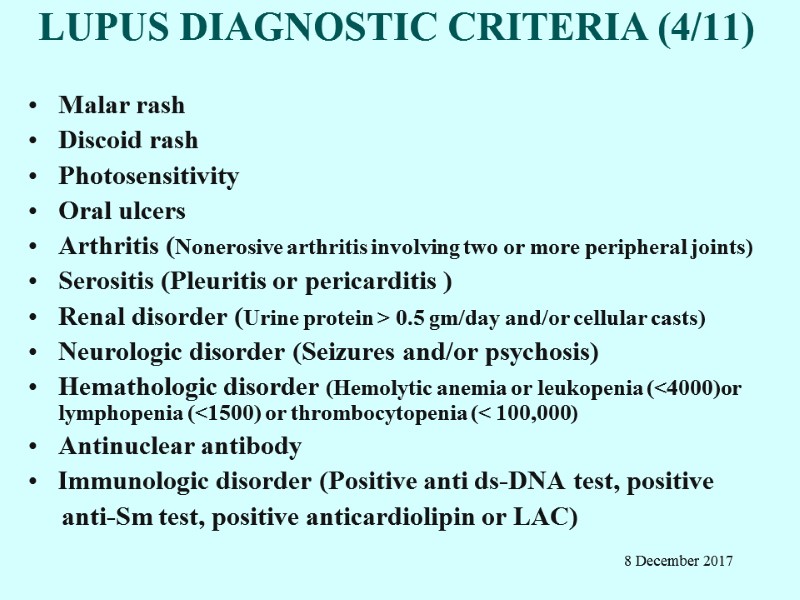
LUPUS DIAGNOSTIC CRITERIA (4/11) Malar rash Discoid rash Photosensitivity Oral ulcers Arthritis (Nonerosive arthritis involving two or more peripheral joints) Serositis (Pleuritis or pericarditis ) Renal disorder (Urine protein > 0.5 gm/day and/or cellular casts) Neurologic disorder (Seizures and/or psychosis) Hemathologic disorder (Hemolytic anemia or leukopenia (<4000)or lymphopenia (<1500) or thrombocytopenia (< 100,000) Antinuclear antibody Immunologic disorder (Positive anti ds-DNA test, positive anti-Sm test, positive anticardiolipin or LAC) 8 December 2017
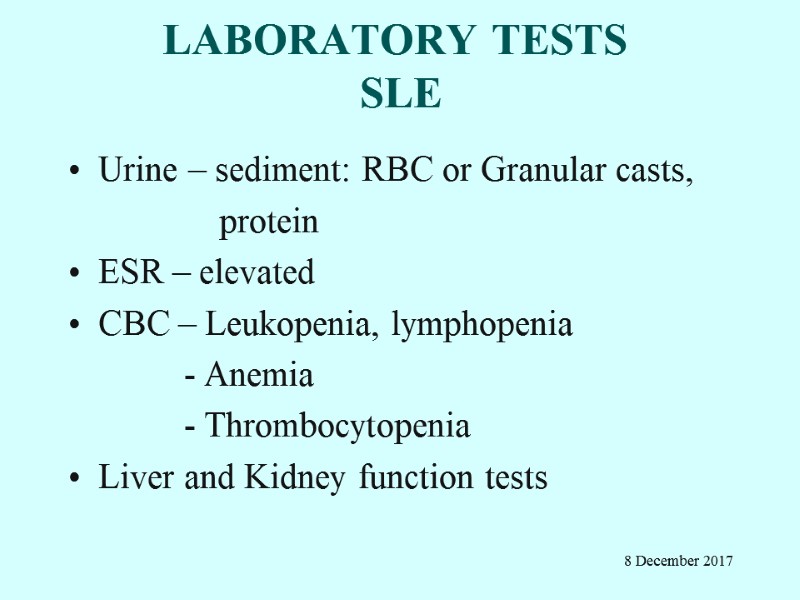
LABORATORY TESTS SLE Urine – sediment: RBC or Granular casts, protein ESR – elevated CBC – Leukopenia, lymphopenia - Anemia - Thrombocytopenia Liver and Kidney function tests 8 December 2017
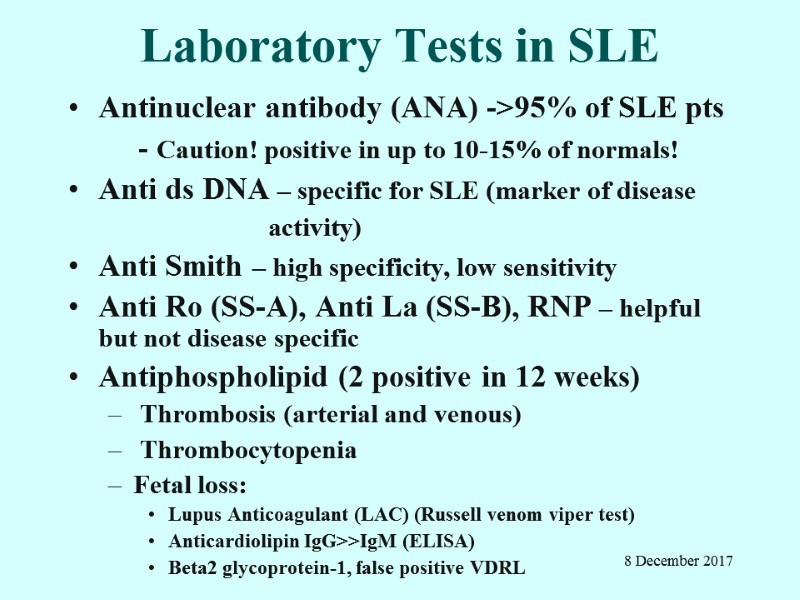
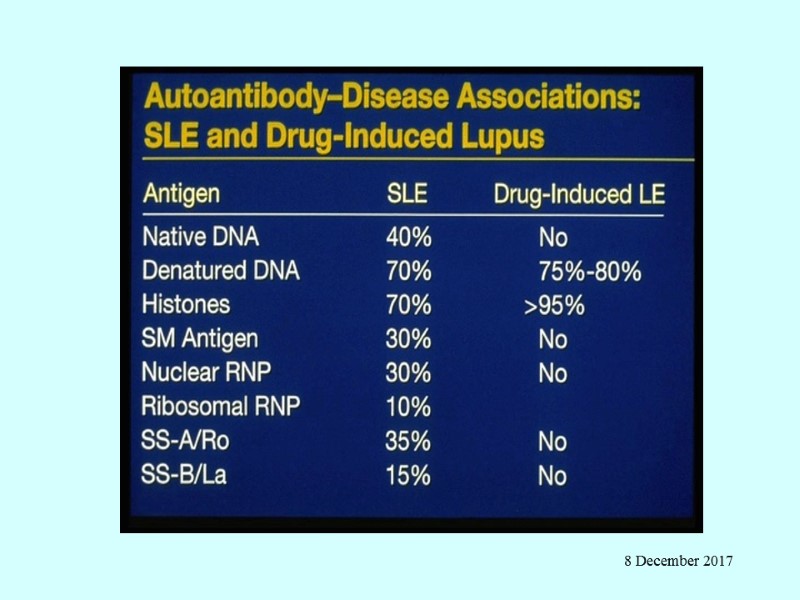
Laboratory Tests in SLE Antinuclear antibody (ANA) ->95% of SLE pts - Caution! positive in up to 10-15% of normals! Anti ds DNA – specific for SLE (marker of disease activity) Anti Smith – high specificity, low sensitivity Anti Ro (SS-A), Anti La (SS-B), RNP – helpful but not disease specific Antiphospholipid (2 positive in 12 weeks) Thrombosis (arterial and venous) Thrombocytopenia Fetal loss: Lupus Anticoagulant (LAC) (Russell venom viper test) Anticardiolipin IgG>>IgM (ELISA) Beta2 glycoprotein-1, false positive VDRL 8 December 2017
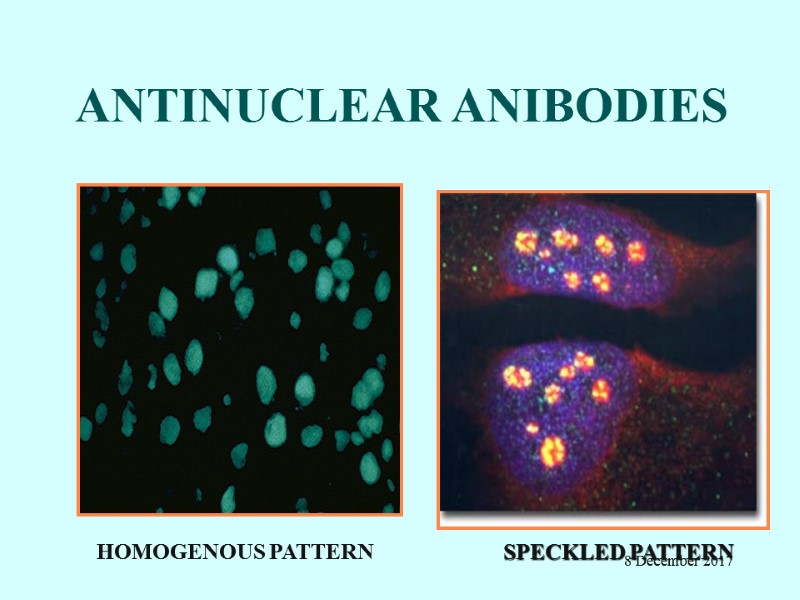
ANTINUCLEAR ANIBODIES HOMOGENOUS PATTERN SPECKLED PATTERN 8 December 2017
PROGNOSIS Mortality: 10-year survival rates ranging from 75-85% > 90% of patients surviving more than 5 years Early deaths: Infection Active disease Thrombosis Renal failure Late complications: Atherosclerosis Osteoporosis Avascular bone necrosis Dementia 8 December 2017
Treatment of lupus nephritis -NIH data Cyclophosphamide significantly reduced the risk of renal failure at 9+ years compared to corticosteroids alone Azathioprine had intermediate efficacy Pulse IV cyclophosphamide superior to pulse IV methylprednisolone in preventing 2X increase in creatinine in severe nephritis Chronisity index of prognostic importance Dyalisis Transplantation 8 December 2017
PREGNANCY AND LUPUS Increased risk of disease activity during or immediately after (3 to 4 weeks) pregnancy Antiphospholipid antibodies pose a particular risk of miscarriages Congenital SLE (positive aRo/aLa mothers): Congenital heart block Rash/Photosensitivity Thrombocytopenia 8 December 2017

Neonatal lupus 8 December 2017
8 December 2017
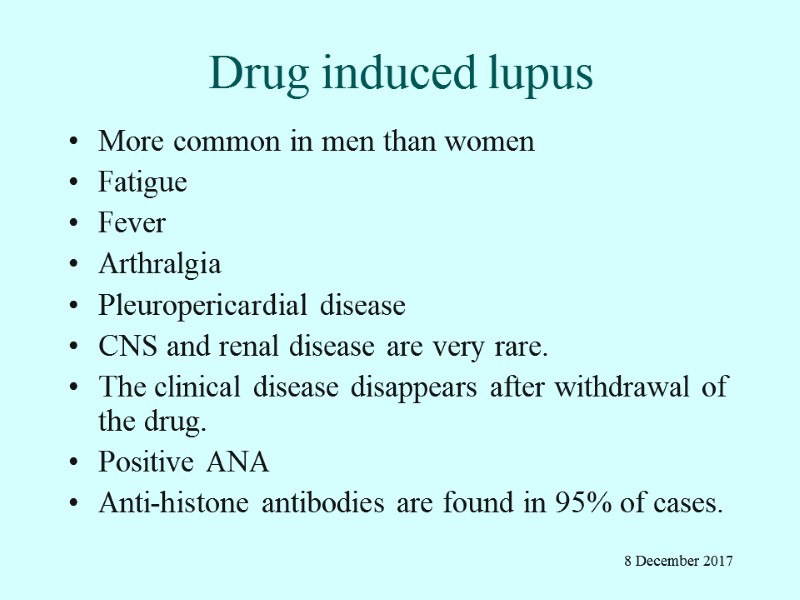
Drug induced lupus More common in men than women Fatigue Fever Arthralgia Pleuropericardial disease CNS and renal disease are very rare. The clinical disease disappears after withdrawal of the drug. Positive ANA Anti-histone antibodies are found in 95% of cases. 8 December 2017
8 December 2017
8 December 2017
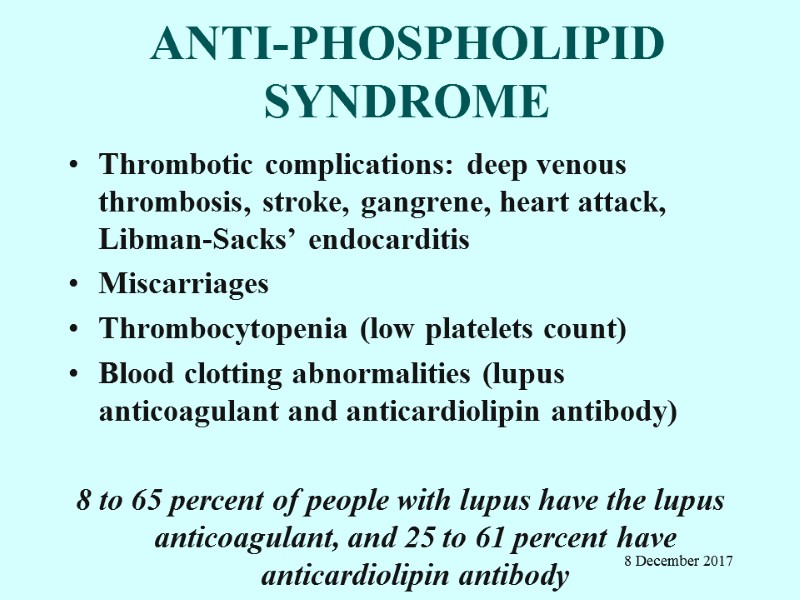
ANTI-PHOSPHOLIPID SYNDROME Thrombotic complications: deep venous thrombosis, stroke, gangrene, heart attack, Libman-Sacks’ endocarditis Miscarriages Thrombocytopenia (low platelets count) Blood clotting abnormalities (lupus anticoagulant and anticardiolipin antibody) 8 to 65 percent of people with lupus have the lupus anticoagulant, and 25 to 61 percent have anticardiolipin antibody 8 December 2017

8 December 2017

8 December 2017
8 December 2017
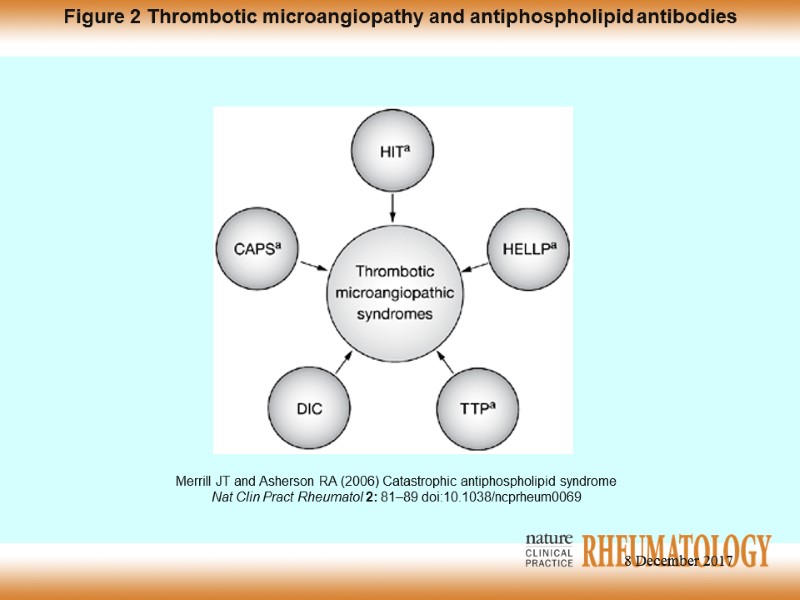
Merrill JT and Asherson RA (2006) Catastrophic antiphospholipid syndrome Nat Clin Pract Rheumatol 2: 81–89 doi:10.1038/ncprheum0069 Figure 2 Thrombotic microangiopathy and antiphospholipid antibodies 8 December 2017

TREATMENT Non-steroidal Anti-inflammatory Drugs (NSAID’s) including COX 2 Corticosteroids (Prednisone, SoluMedrol) Antimalarial (Hydroxychloroquine) Immunomodulating Drugs Azathioprine Methotrexate Cyclophosphamide Mycophenolate mofetil Anticoagulants (Aspirin, Coumadine) 8 December 2017
Preventive therapies Influenza vaccination Pneumovax Prophylaxis UTI Osteoporosis Atherosclerosis Obesity, DM, hypertension 8 December 2017

New strategies Mycophenolate mofetil (MMF) – Celcept Abatacept Mabthera BLyS APRIL TACi 8 December 2017
5430-systemic_lupus_erythematosus.ppt_2012.ppt
- Количество слайдов: 62

