Systemic Lupus Erythematosus.ppt 2012.ppt
- Количество слайдов: 62
 SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) 2/11/2018
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) 2/11/2018
 DEFINITION • Inflammatory disease • Multi-system disease • Autoimmune disease – Autoantibodies – Immune complexes 2/11/2018
DEFINITION • Inflammatory disease • Multi-system disease • Autoimmune disease – Autoantibodies – Immune complexes 2/11/2018
 EPIDEMIOLOGY OF SLE • • • Frequency: 14. 6/100, 000 to 50. 8/100, 000 Incidence: 1. 8 -7. 6/100, 000 per year Internationally: worldwide Age: 15 -45 years Gender: F/M = 9/1 Race: blacks: whites = 4: 1 2/11/2018
EPIDEMIOLOGY OF SLE • • • Frequency: 14. 6/100, 000 to 50. 8/100, 000 Incidence: 1. 8 -7. 6/100, 000 per year Internationally: worldwide Age: 15 -45 years Gender: F/M = 9/1 Race: blacks: whites = 4: 1 2/11/2018
 SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) • Prototypic autoimmune disease • Loss of tolerance to self leads to immune system mediated damage to self • Etiology of SLE unknown • Each patient unique 2/11/2018
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) • Prototypic autoimmune disease • Loss of tolerance to self leads to immune system mediated damage to self • Etiology of SLE unknown • Each patient unique 2/11/2018
 Pathogenesis of SLE • Genetic Factors – Autoimmunity genes on chromosome 16 – Increased frequency in close relatives – Ethnic susceptibility – HLA-DR 2 and –DR 3 associations – Inherited complement deficiencies (C 1 q, C 2, C 4) 2/11/2018
Pathogenesis of SLE • Genetic Factors – Autoimmunity genes on chromosome 16 – Increased frequency in close relatives – Ethnic susceptibility – HLA-DR 2 and –DR 3 associations – Inherited complement deficiencies (C 1 q, C 2, C 4) 2/11/2018
 Pathogenesis of SLE • Environmental factors – Ultraviolet light (flares in 70%) • Increased apoptosis of skin cells • Altering of DNA and intracellular proteins – Ag – Drug-induced lupus – Infectious triggers • EBV • Hormonal factors – Female, pregnancy, delivery – Oral contraceptives, HRT (estradiol receptors on Ly) 2/11/2018
Pathogenesis of SLE • Environmental factors – Ultraviolet light (flares in 70%) • Increased apoptosis of skin cells • Altering of DNA and intracellular proteins – Ag – Drug-induced lupus – Infectious triggers • EBV • Hormonal factors – Female, pregnancy, delivery – Oral contraceptives, HRT (estradiol receptors on Ly) 2/11/2018
 SLE - Pathogenesis Susceptibility genes (usually multiple) + Triggering factors (probably environmental) ABNORMAL IMMUNE RESPONSE 2/11/2018
SLE - Pathogenesis Susceptibility genes (usually multiple) + Triggering factors (probably environmental) ABNORMAL IMMUNE RESPONSE 2/11/2018
 SLE - Pathogenesis • Activation of innate immunity (dendritic cells) – By DNA in IC – By RNA in RNA/self-antigens • Lowered activation thresholds of adaptive immunity (antigen specific T-ly and B-ly) • Ineffective regulatory CD 4+ and inhibitory CD 8+ • Abnormal function of T-reg • Reduced clearance of apoptotic cells and IC 2/11/2018
SLE - Pathogenesis • Activation of innate immunity (dendritic cells) – By DNA in IC – By RNA in RNA/self-antigens • Lowered activation thresholds of adaptive immunity (antigen specific T-ly and B-ly) • Ineffective regulatory CD 4+ and inhibitory CD 8+ • Abnormal function of T-reg • Reduced clearance of apoptotic cells and IC 2/11/2018
 Pathogenesis SLE • Apoptosis – programmed cells death – Blebs contain self-antigens • DNA • RNA • Phospholipids • Excess of proinflammatory cytokines – TNF , IFN -γ, BLy. S – B lymphocyte stimulator, IL-10 • Inadequate secretion by T-ly and NK regulatory cytokines – IL-2 and TGF – Deficit of Reg CD 4+ and Inh CD 8+ 2/11/2018
Pathogenesis SLE • Apoptosis – programmed cells death – Blebs contain self-antigens • DNA • RNA • Phospholipids • Excess of proinflammatory cytokines – TNF , IFN -γ, BLy. S – B lymphocyte stimulator, IL-10 • Inadequate secretion by T-ly and NK regulatory cytokines – IL-2 and TGF – Deficit of Reg CD 4+ and Inh CD 8+ 2/11/2018
 Pathogenesis SLE • Sustain production of pathogenic autoantibodies directed against self-antigens and IC • Binding of IC to target tissues • Activation of complement system and phagocytic cells that recognize Ig-coating circulation blood cells • Tissue damage - release of chemotoxins, cytokines, chemokines, vasoactive peptides, destructive enzymes 2/11/2018
Pathogenesis SLE • Sustain production of pathogenic autoantibodies directed against self-antigens and IC • Binding of IC to target tissues • Activation of complement system and phagocytic cells that recognize Ig-coating circulation blood cells • Tissue damage - release of chemotoxins, cytokines, chemokines, vasoactive peptides, destructive enzymes 2/11/2018
 Pathology SLE • Skin: Ig deposition in DEJ, injury to keratinocytes, T-ly induced inflammation • Renal: 6 types with active /chronic changes • Vasculitis- leukocytoclasis • Lymph nodes – nonspecific inflammtion 2/11/2018
Pathology SLE • Skin: Ig deposition in DEJ, injury to keratinocytes, T-ly induced inflammation • Renal: 6 types with active /chronic changes • Vasculitis- leukocytoclasis • Lymph nodes – nonspecific inflammtion 2/11/2018
 TYPES OF LUPUS • • • Discoid LE Subacute cutaneous LE Systemic LE Drug-induced LE Overlap syndrome 2/11/2018
TYPES OF LUPUS • • • Discoid LE Subacute cutaneous LE Systemic LE Drug-induced LE Overlap syndrome 2/11/2018
 Clinical Features of SLE • • Constitutional symptoms – nonspecific but can be profound. Fatigue Appetite loss Weight loss Fever 2/11/2018
Clinical Features of SLE • • Constitutional symptoms – nonspecific but can be profound. Fatigue Appetite loss Weight loss Fever 2/11/2018
 Cutaneous manifestations • Malar rash in 50% – – • • Photosensitive Transient or chronic Photosensitivity (50%) – usually to UV-B Discoid Lupus – annular, scaly hyperpigmented erythematous plaques; scarring; atrophic centers – – SLE – 25% have DLE 10% with DLE will develop SLE 25% ANA pos Most anti Ro (SS-A) pos 2/11/2018
Cutaneous manifestations • Malar rash in 50% – – • • Photosensitive Transient or chronic Photosensitivity (50%) – usually to UV-B Discoid Lupus – annular, scaly hyperpigmented erythematous plaques; scarring; atrophic centers – – SLE – 25% have DLE 10% with DLE will develop SLE 25% ANA pos Most anti Ro (SS-A) pos 2/11/2018
 Cutaneous manifestations • Subacute cutaneous lupus – small erythematous papules that coalesce into patterns, non scarring – – • Upper torso, next, arms Ro (SS-A) association 10% of SLE patients have it May have this alone without systemic disease Lupus profundus/panniculitis – Nodules in dermis or subcutaneous tissue – Nodules may be under skin lesions or under normal skin (panniculitis) • Oral ulcers 2/11/2018
Cutaneous manifestations • Subacute cutaneous lupus – small erythematous papules that coalesce into patterns, non scarring – – • Upper torso, next, arms Ro (SS-A) association 10% of SLE patients have it May have this alone without systemic disease Lupus profundus/panniculitis – Nodules in dermis or subcutaneous tissue – Nodules may be under skin lesions or under normal skin (panniculitis) • Oral ulcers 2/11/2018
 Cutaneous manifestations • Alopecia – 70% – Scarring, discoid lesion – Non scarring • Vascular – – – Periangular erythema Livido reticularis Telangiectasias Raynaud’s phenomenon Vasculitis • Rare subcutaneous nodule 2/11/2018
Cutaneous manifestations • Alopecia – 70% – Scarring, discoid lesion – Non scarring • Vascular – – – Periangular erythema Livido reticularis Telangiectasias Raynaud’s phenomenon Vasculitis • Rare subcutaneous nodule 2/11/2018
 2/11/2018
2/11/2018
 2/11/2018
2/11/2018
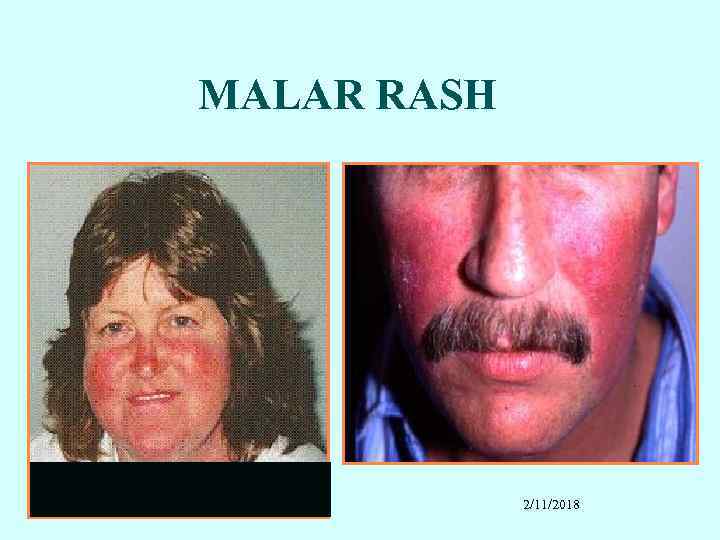 MALAR RASH 2/11/2018
MALAR RASH 2/11/2018
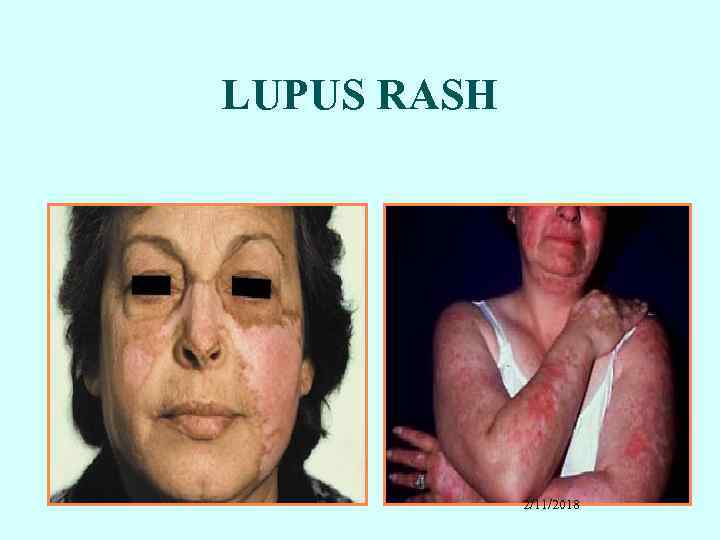 LUPUS RASH 2/11/2018
LUPUS RASH 2/11/2018
 2/11/2018
2/11/2018
 DISCOID LUPUS 2/11/2018
DISCOID LUPUS 2/11/2018
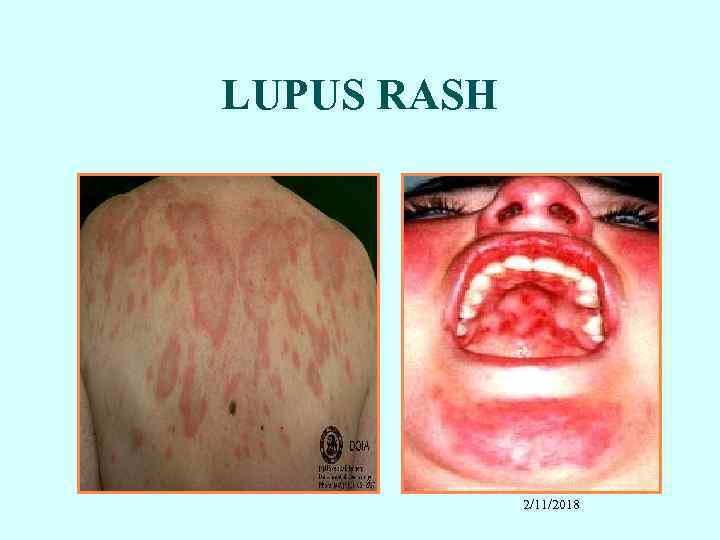 LUPUS RASH 2/11/2018
LUPUS RASH 2/11/2018
 VASCULAR SKIN CHANGES RAYNAUD’S PHENOMENON 2/11/2018 LIVEDO RETICULARIS
VASCULAR SKIN CHANGES RAYNAUD’S PHENOMENON 2/11/2018 LIVEDO RETICULARIS
 SLE SKIN PATHOLOGY 2/11/2018
SLE SKIN PATHOLOGY 2/11/2018
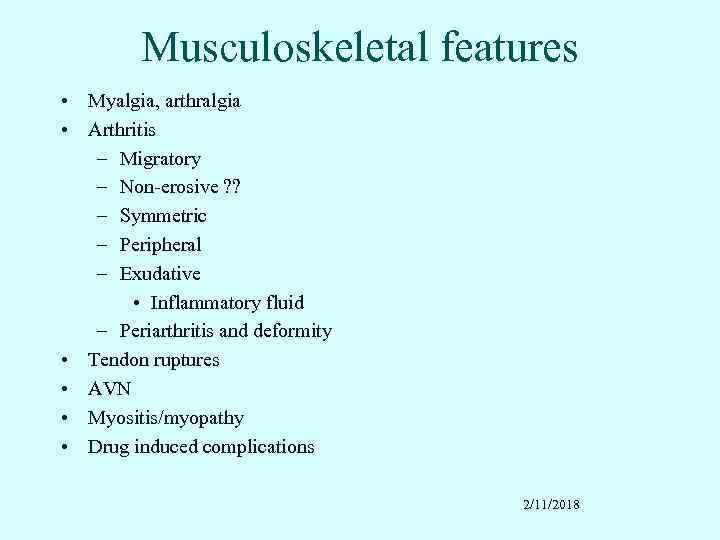 Musculoskeletal features • Myalgia, arthralgia • Arthritis – Migratory – Non-erosive ? ? – Symmetric – Peripheral – Exudative • Inflammatory fluid – Periarthritis and deformity • Tendon ruptures • AVN • Myositis/myopathy • Drug induced complications 2/11/2018
Musculoskeletal features • Myalgia, arthralgia • Arthritis – Migratory – Non-erosive ? ? – Symmetric – Peripheral – Exudative • Inflammatory fluid – Periarthritis and deformity • Tendon ruptures • AVN • Myositis/myopathy • Drug induced complications 2/11/2018
 2/11/2018
2/11/2018
 Pulmonary manifestations • Pleurisy and pleuritis – Exudate – ANA pos, low complement – Normal glucose • Acute pneumonitis • Chronic pneumonitis, ILD, fibrosis • Pulmonary hypertension • “Shrinking lung” • Isolated diffusing capacity impairment • PE (APLA) --------------Infections always to be excluded !!!!! 2/11/2018
Pulmonary manifestations • Pleurisy and pleuritis – Exudate – ANA pos, low complement – Normal glucose • Acute pneumonitis • Chronic pneumonitis, ILD, fibrosis • Pulmonary hypertension • “Shrinking lung” • Isolated diffusing capacity impairment • PE (APLA) --------------Infections always to be excluded !!!!! 2/11/2018
 SEROSITIS IN SLE PLEURITIS PERICARDITIS 2/11/2018
SEROSITIS IN SLE PLEURITIS PERICARDITIS 2/11/2018
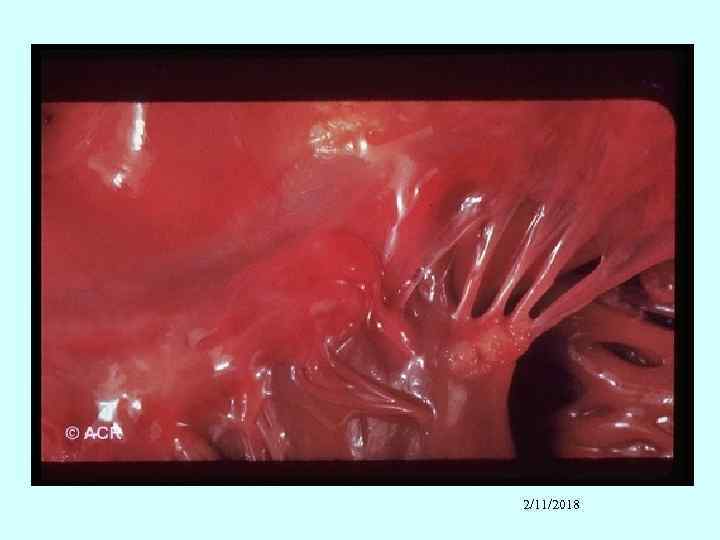
 Cardiac manifestations • Pericardial involvement – Pleurisy – Pleuritis – Tamponade • Myocardial involvement – acute or chronic • Endocardial involvement - Libman-Sacks (verrucous endocarditis) - Diffuse valvular thickening • Coronary artery disease - premature 2/11/2018
Cardiac manifestations • Pericardial involvement – Pleurisy – Pleuritis – Tamponade • Myocardial involvement – acute or chronic • Endocardial involvement - Libman-Sacks (verrucous endocarditis) - Diffuse valvular thickening • Coronary artery disease - premature 2/11/2018
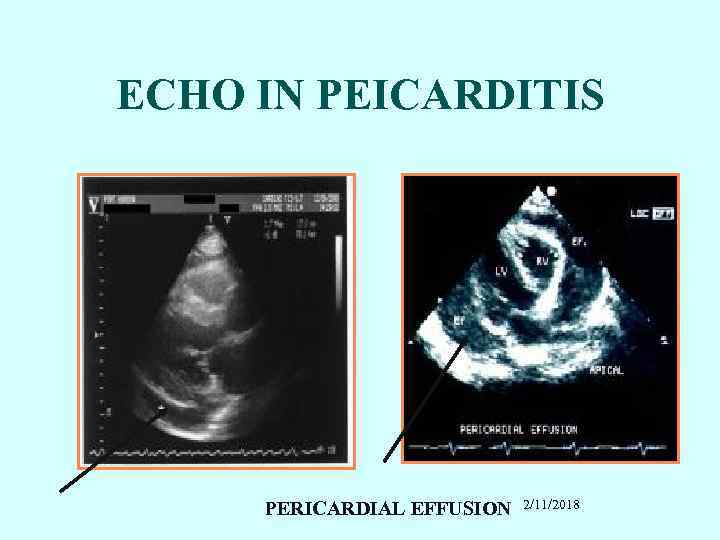 ECHO IN PEICARDITIS PERICARDIAL EFFUSION 2/11/2018
ECHO IN PEICARDITIS PERICARDIAL EFFUSION 2/11/2018
 Hematologic manifestations • Anemia – “Chronic disease” – Hemolytic • Leukopenia – lymphopenia • Thrombocytopenia – Early ITP • Hypercoagulable state - associated with antiphospholipid antibodies 2/11/2018
Hematologic manifestations • Anemia – “Chronic disease” – Hemolytic • Leukopenia – lymphopenia • Thrombocytopenia – Early ITP • Hypercoagulable state - associated with antiphospholipid antibodies 2/11/2018
 Gastrointestinal manifestations • Dyspepsia, dysphagia – common • Acute abdomen – Vasculitis – Serositis (peritonitis) • Pancreatitis – usually mild, subclinical • Autoimmune (lupoid) hepatitis 2/11/2018
Gastrointestinal manifestations • Dyspepsia, dysphagia – common • Acute abdomen – Vasculitis – Serositis (peritonitis) • Pancreatitis – usually mild, subclinical • Autoimmune (lupoid) hepatitis 2/11/2018
 Neuropsychiatric • Diffuse CNS lupus • • • Cognitive dysfunction Headache Psychosis Seizures – can be any kind, usually grand mal Meningitis Focal cerebral dysfunction - Associated with antiphospholipid antibodies - Stroke (5%) 2/11/2018
Neuropsychiatric • Diffuse CNS lupus • • • Cognitive dysfunction Headache Psychosis Seizures – can be any kind, usually grand mal Meningitis Focal cerebral dysfunction - Associated with antiphospholipid antibodies - Stroke (5%) 2/11/2018
 Other neural system features • • • Peripheral neuropathy Cranial neuropathy – usually affects eyes Transverse myelitis Neuromyelitis optica Myelopathy Eye – cytoid bodies (vasculitis of retinal capillaries) _______________ Infection always must be excluded!!!!!! 2/11/2018
Other neural system features • • • Peripheral neuropathy Cranial neuropathy – usually affects eyes Transverse myelitis Neuromyelitis optica Myelopathy Eye – cytoid bodies (vasculitis of retinal capillaries) _______________ Infection always must be excluded!!!!!! 2/11/2018
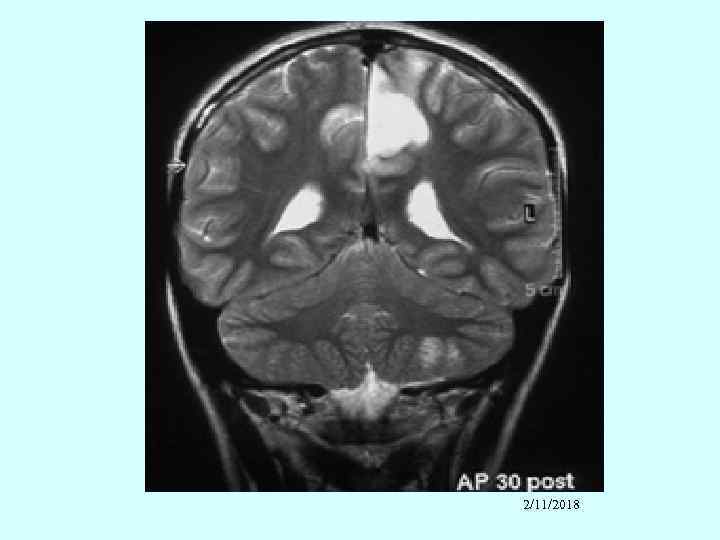 2/11/2018
2/11/2018
 2/11/2018
2/11/2018
 (Lupus nephritis (50% • The most morbid manifestation of SLE • Nearly all patients have EM and immunofluorescent renal abnormalities; 50% have clinically apparent disease • Occurs early in the course of the disease. • If not present within 1 year it probably won’t occur. • Pathology – immune complexes and complement deposit in glomeruli, in capillary wall, subepithelium, subendothelium and mesangium • Untreated class IV and III– ESRD in 2 years • Concomitant accelerated atherosclerosis 2/11/2018
(Lupus nephritis (50% • The most morbid manifestation of SLE • Nearly all patients have EM and immunofluorescent renal abnormalities; 50% have clinically apparent disease • Occurs early in the course of the disease. • If not present within 1 year it probably won’t occur. • Pathology – immune complexes and complement deposit in glomeruli, in capillary wall, subepithelium, subendothelium and mesangium • Untreated class IV and III– ESRD in 2 years • Concomitant accelerated atherosclerosis 2/11/2018
 Lupus Nephritis – clinical presentation • • • Hypertension – new onset Peripheral edema, weight gain Renal insufficiency or failure (elevated creatinine) Nephrotic syndrome Asymptomatic urinary findings - Proteinuria - RBC, less commonly WBC - Casts – RBC casts ominous 2/11/2018
Lupus Nephritis – clinical presentation • • • Hypertension – new onset Peripheral edema, weight gain Renal insufficiency or failure (elevated creatinine) Nephrotic syndrome Asymptomatic urinary findings - Proteinuria - RBC, less commonly WBC - Casts – RBC casts ominous 2/11/2018
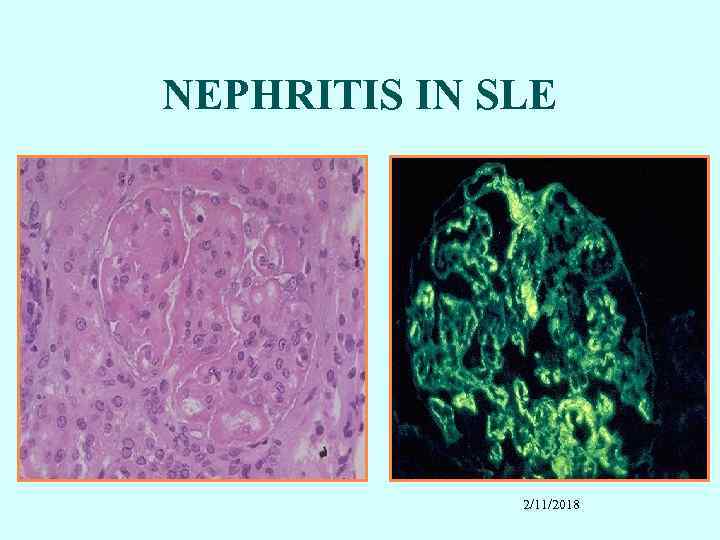 NEPHRITIS IN SLE 2/11/2018
NEPHRITIS IN SLE 2/11/2018
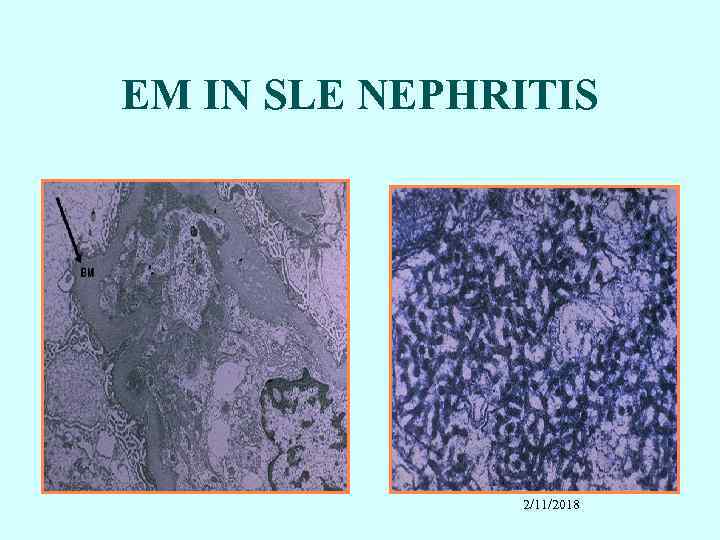 EM IN SLE NEPHRITIS 2/11/2018
EM IN SLE NEPHRITIS 2/11/2018
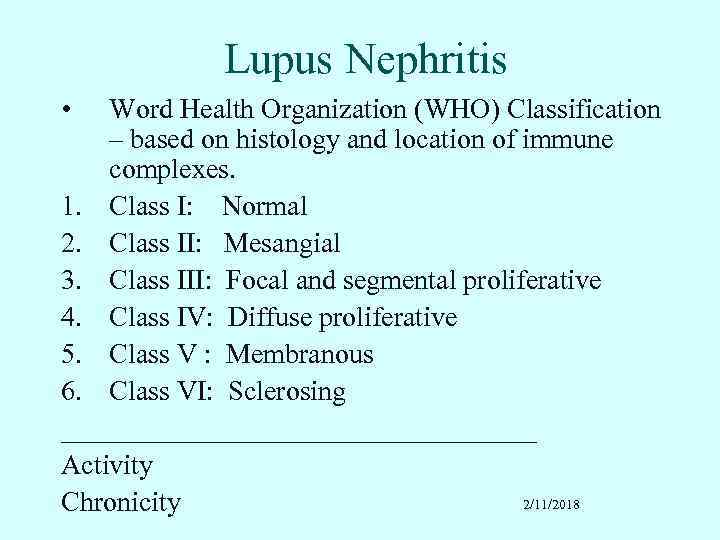 Lupus Nephritis • Word Health Organization (WHO) Classification – based on histology and location of immune complexes. 1. Class I: Normal 2. Class II: Mesangial 3. Class III: Focal and segmental proliferative 4. Class IV: Diffuse proliferative 5. Class V : Membranous 6. Class VI: Sclerosing _________________ Activity 2/11/2018 Chronicity
Lupus Nephritis • Word Health Organization (WHO) Classification – based on histology and location of immune complexes. 1. Class I: Normal 2. Class II: Mesangial 3. Class III: Focal and segmental proliferative 4. Class IV: Diffuse proliferative 5. Class V : Membranous 6. Class VI: Sclerosing _________________ Activity 2/11/2018 Chronicity
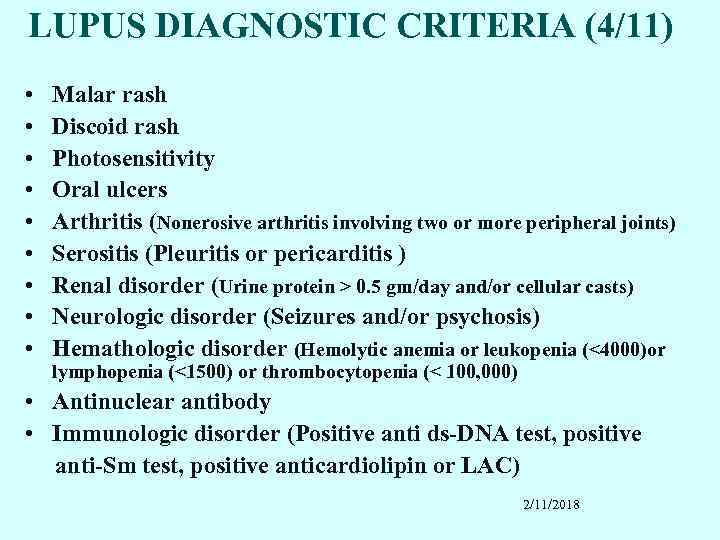 LUPUS DIAGNOSTIC CRITERIA (4/11) • • • Malar rash Discoid rash Photosensitivity Oral ulcers Arthritis (Nonerosive arthritis involving two or more peripheral joints) Serositis (Pleuritis or pericarditis ) Renal disorder (Urine protein > 0. 5 gm/day and/or cellular casts) Neurologic disorder (Seizures and/or psychosis) Hemathologic disorder (Hemolytic anemia or leukopenia (<4000)or lymphopenia (<1500) or thrombocytopenia (< 100, 000) • Antinuclear antibody • Immunologic disorder (Positive anti ds-DNA test, positive anti-Sm test, positive anticardiolipin or LAC) 2/11/2018
LUPUS DIAGNOSTIC CRITERIA (4/11) • • • Malar rash Discoid rash Photosensitivity Oral ulcers Arthritis (Nonerosive arthritis involving two or more peripheral joints) Serositis (Pleuritis or pericarditis ) Renal disorder (Urine protein > 0. 5 gm/day and/or cellular casts) Neurologic disorder (Seizures and/or psychosis) Hemathologic disorder (Hemolytic anemia or leukopenia (<4000)or lymphopenia (<1500) or thrombocytopenia (< 100, 000) • Antinuclear antibody • Immunologic disorder (Positive anti ds-DNA test, positive anti-Sm test, positive anticardiolipin or LAC) 2/11/2018
 LABORATORY TESTS SLE • Urine – sediment: RBC or Granular casts, protein • ESR – elevated • CBC – Leukopenia, lymphopenia - Anemia - Thrombocytopenia • Liver and Kidney function tests 2/11/2018
LABORATORY TESTS SLE • Urine – sediment: RBC or Granular casts, protein • ESR – elevated • CBC – Leukopenia, lymphopenia - Anemia - Thrombocytopenia • Liver and Kidney function tests 2/11/2018
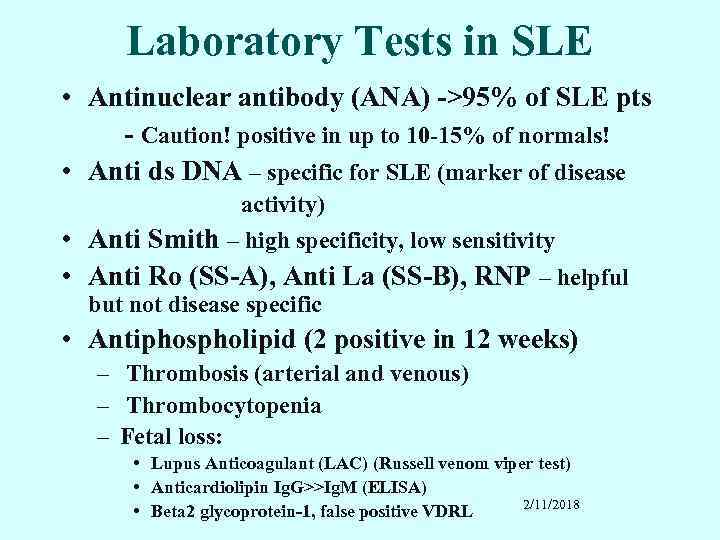 Laboratory Tests in SLE • Antinuclear antibody (ANA) ->95% of SLE pts - Caution! positive in up to 10 -15% of normals! • Anti ds DNA – specific for SLE (marker of disease activity) • Anti Smith – high specificity, low sensitivity • Anti Ro (SS-A), Anti La (SS-B), RNP – helpful but not disease specific • Antiphospholipid (2 positive in 12 weeks) – Thrombosis (arterial and venous) – Thrombocytopenia – Fetal loss: • Lupus Anticoagulant (LAC) (Russell venom viper test) • Anticardiolipin Ig. G>>Ig. M (ELISA) 2/11/2018 • Beta 2 glycoprotein-1, false positive VDRL
Laboratory Tests in SLE • Antinuclear antibody (ANA) ->95% of SLE pts - Caution! positive in up to 10 -15% of normals! • Anti ds DNA – specific for SLE (marker of disease activity) • Anti Smith – high specificity, low sensitivity • Anti Ro (SS-A), Anti La (SS-B), RNP – helpful but not disease specific • Antiphospholipid (2 positive in 12 weeks) – Thrombosis (arterial and venous) – Thrombocytopenia – Fetal loss: • Lupus Anticoagulant (LAC) (Russell venom viper test) • Anticardiolipin Ig. G>>Ig. M (ELISA) 2/11/2018 • Beta 2 glycoprotein-1, false positive VDRL
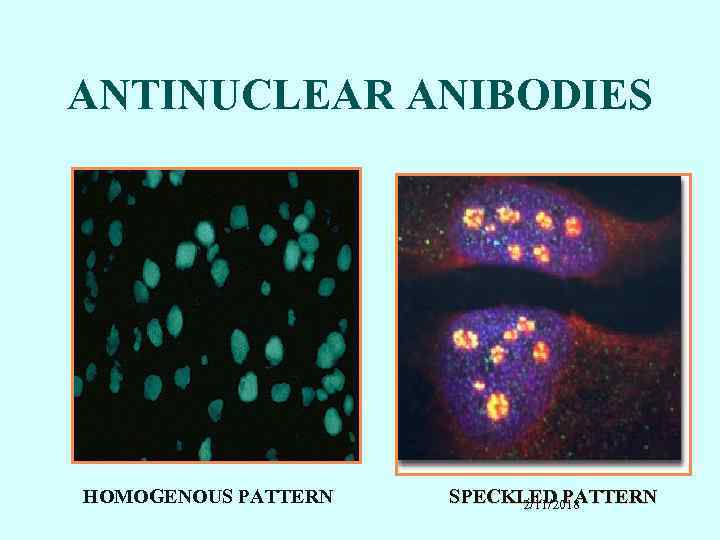 ANTINUCLEAR ANIBODIES HOMOGENOUS PATTERN SPECKLED PATTERN 2/11/2018
ANTINUCLEAR ANIBODIES HOMOGENOUS PATTERN SPECKLED PATTERN 2/11/2018
 PROGNOSIS • Mortality: – 10 -year survival rates ranging from 75 -85% – > 90% of patients surviving more than 5 years • Early deaths: – Infection – Active disease – Thrombosis – Renal failure • Late complications: – Atherosclerosis – Osteoporosis – Avascular bone necrosis – Dementia 2/11/2018
PROGNOSIS • Mortality: – 10 -year survival rates ranging from 75 -85% – > 90% of patients surviving more than 5 years • Early deaths: – Infection – Active disease – Thrombosis – Renal failure • Late complications: – Atherosclerosis – Osteoporosis – Avascular bone necrosis – Dementia 2/11/2018
 Treatment of lupus nephritis NIH data • Cyclophosphamide significantly reduced the risk of renal failure at 9+ years compared to corticosteroids alone • Azathioprine had intermediate efficacy • Pulse IV cyclophosphamide superior to pulse IV methylprednisolone in preventing 2 X increase in creatinine in severe nephritis • Chronisity index of prognostic importance • Dyalisis • Transplantation 2/11/2018
Treatment of lupus nephritis NIH data • Cyclophosphamide significantly reduced the risk of renal failure at 9+ years compared to corticosteroids alone • Azathioprine had intermediate efficacy • Pulse IV cyclophosphamide superior to pulse IV methylprednisolone in preventing 2 X increase in creatinine in severe nephritis • Chronisity index of prognostic importance • Dyalisis • Transplantation 2/11/2018
 PREGNANCY AND LUPUS • Increased risk of disease activity during or immediately after (3 to 4 weeks) pregnancy • Antiphospholipid antibodies pose a particular risk of miscarriages • Congenital SLE (positive a. Ro/a. La mothers): – Congenital heart block – Rash/Photosensitivity – Thrombocytopenia 2/11/2018
PREGNANCY AND LUPUS • Increased risk of disease activity during or immediately after (3 to 4 weeks) pregnancy • Antiphospholipid antibodies pose a particular risk of miscarriages • Congenital SLE (positive a. Ro/a. La mothers): – Congenital heart block – Rash/Photosensitivity – Thrombocytopenia 2/11/2018
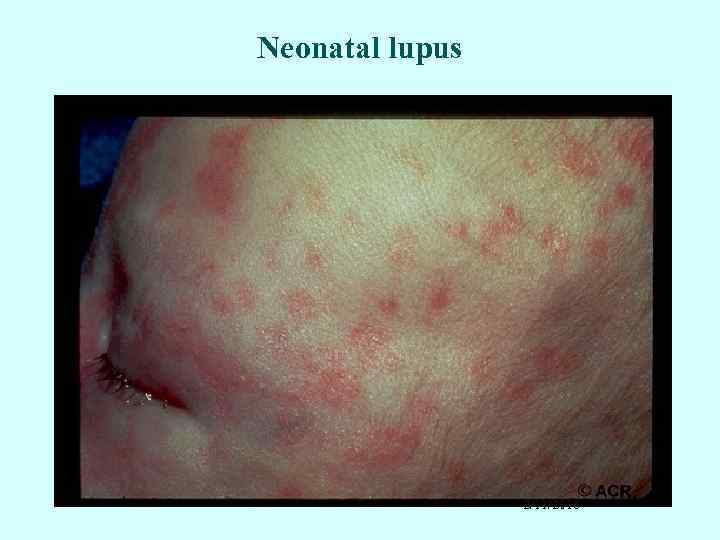 Neonatal lupus 2/11/2018
Neonatal lupus 2/11/2018
 2/11/2018
2/11/2018
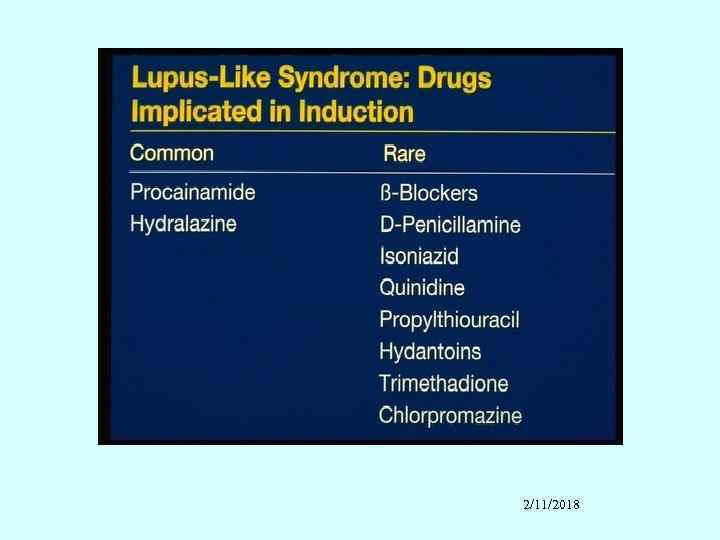
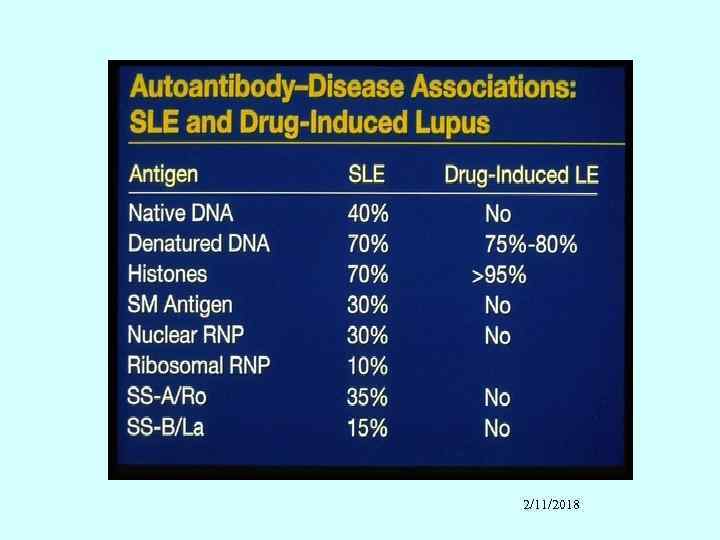
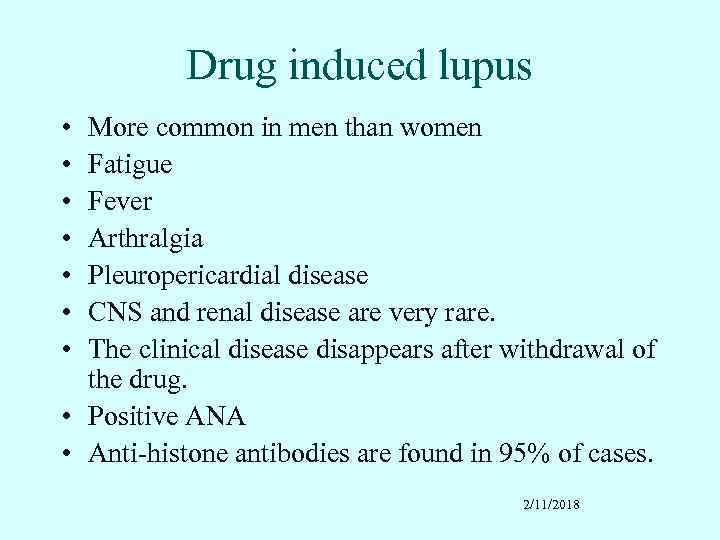 Drug induced lupus • • More common in men than women Fatigue Fever Arthralgia Pleuropericardial disease CNS and renal disease are very rare. The clinical disease disappears after withdrawal of the drug. • Positive ANA • Anti-histone antibodies are found in 95% of cases. 2/11/2018
Drug induced lupus • • More common in men than women Fatigue Fever Arthralgia Pleuropericardial disease CNS and renal disease are very rare. The clinical disease disappears after withdrawal of the drug. • Positive ANA • Anti-histone antibodies are found in 95% of cases. 2/11/2018
 2/11/2018
2/11/2018
 2/11/2018
2/11/2018
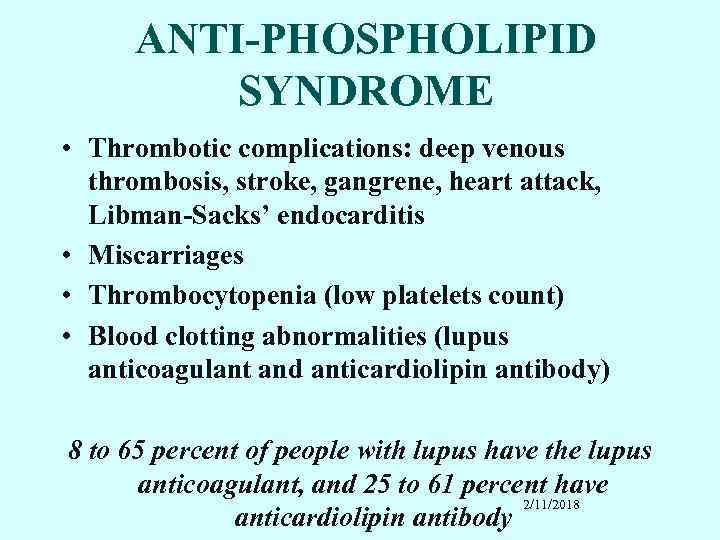 ANTI-PHOSPHOLIPID SYNDROME • Thrombotic complications: deep venous thrombosis, stroke, gangrene, heart attack, Libman-Sacks’ endocarditis • Miscarriages • Thrombocytopenia (low platelets count) • Blood clotting abnormalities (lupus anticoagulant and anticardiolipin antibody) 8 to 65 percent of people with lupus have the lupus anticoagulant, and 25 to 61 percent have 2/11/2018 anticardiolipin antibody
ANTI-PHOSPHOLIPID SYNDROME • Thrombotic complications: deep venous thrombosis, stroke, gangrene, heart attack, Libman-Sacks’ endocarditis • Miscarriages • Thrombocytopenia (low platelets count) • Blood clotting abnormalities (lupus anticoagulant and anticardiolipin antibody) 8 to 65 percent of people with lupus have the lupus anticoagulant, and 25 to 61 percent have 2/11/2018 anticardiolipin antibody
 2/11/2018
2/11/2018
 2/11/2018
2/11/2018
 2/11/2018
2/11/2018
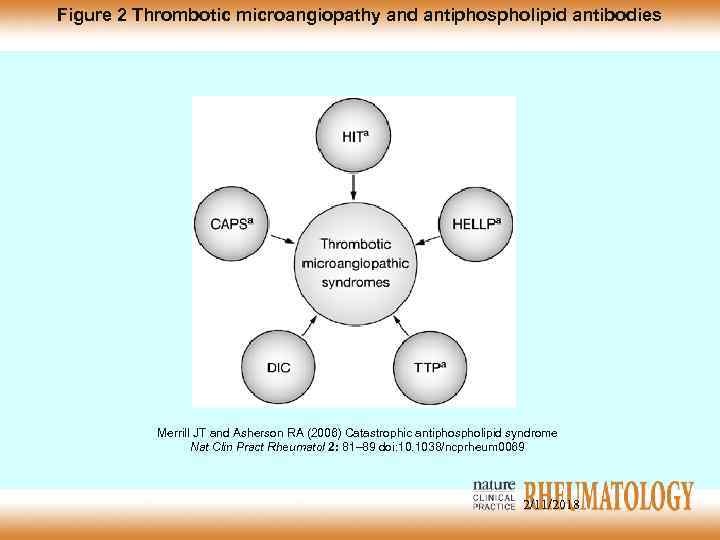 Figure 2 Thrombotic microangiopathy and antiphospholipid antibodies Merrill JT and Asherson RA (2006) Catastrophic antiphospholipid syndrome Nat Clin Pract Rheumatol 2: 81– 89 doi: 10. 1038/ncprheum 0069 2/11/2018
Figure 2 Thrombotic microangiopathy and antiphospholipid antibodies Merrill JT and Asherson RA (2006) Catastrophic antiphospholipid syndrome Nat Clin Pract Rheumatol 2: 81– 89 doi: 10. 1038/ncprheum 0069 2/11/2018
 TREATMENT • Non-steroidal Anti-inflammatory Drugs (NSAID’s) including COX 2 • Corticosteroids (Prednisone, Solu. Medrol) • Antimalarial (Hydroxychloroquine) • Immunomodulating Drugs – Azathioprine – Methotrexate – Cyclophosphamide – Mycophenolate mofetil • Anticoagulants (Aspirin, Coumadine) 2/11/2018
TREATMENT • Non-steroidal Anti-inflammatory Drugs (NSAID’s) including COX 2 • Corticosteroids (Prednisone, Solu. Medrol) • Antimalarial (Hydroxychloroquine) • Immunomodulating Drugs – Azathioprine – Methotrexate – Cyclophosphamide – Mycophenolate mofetil • Anticoagulants (Aspirin, Coumadine) 2/11/2018
 Preventive therapies • • • Influenza vaccination Pneumovax Prophylaxis UTI Osteoporosis Atherosclerosis Obesity, DM, hypertension 2/11/2018
Preventive therapies • • • Influenza vaccination Pneumovax Prophylaxis UTI Osteoporosis Atherosclerosis Obesity, DM, hypertension 2/11/2018
 New strategies • • • Mycophenolate mofetil (MMF) – Celcept Abatacept Mabthera BLy. S APRIL TACi 2/11/2018
New strategies • • • Mycophenolate mofetil (MMF) – Celcept Abatacept Mabthera BLy. S APRIL TACi 2/11/2018


