Hypertension-W.ppt
- Количество слайдов: 82
Systemic Arterial Hypertension Hussein Amrat MD
Objective • Describe the signs, symptoms, etiologies, treatments and complications of hypertension.
Introduction • 25 % of population > 18 have HTN • Usually asymptomatic • Readily detectable • Usually easily treatable • Lethal if not treated
Introduction • Hypertension is the most common primary diagnosis in the U. S. with 35 million office visits as the primary diagnosis. • 50 million Americans have hypertension; 30% are still unaware they have HTN.
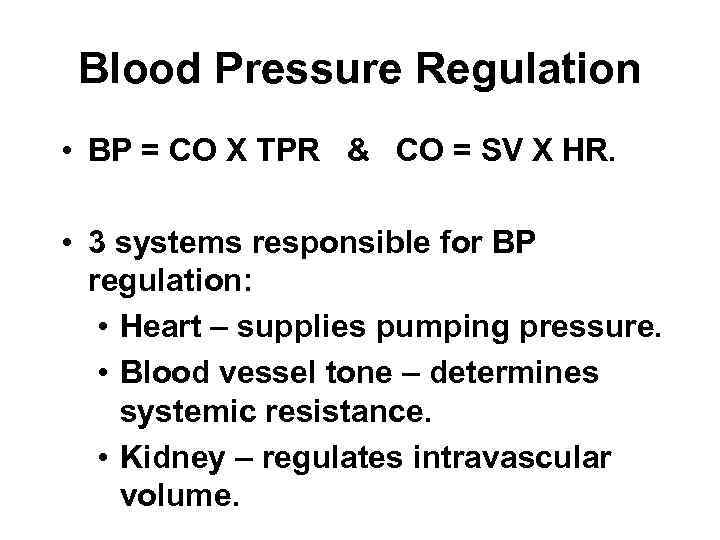
Blood Pressure Regulation • BP = CO X TPR & CO = SV X HR. • 3 systems responsible for BP regulation: • Heart – supplies pumping pressure. • Blood vessel tone – determines systemic resistance. • Kidney – regulates intravascular volume.
Blood Pressure Reflexes • Baroreceptor reflex mediated by receptors in walls of aortic arch and carotid sinuses; • Stimulation inhibits sympathetic nervous system outflow and excites parasympathetic effects. • Main effect is to reduce moment-bymoment variation in systemic BP; does not prevent development of chronic hypertension.
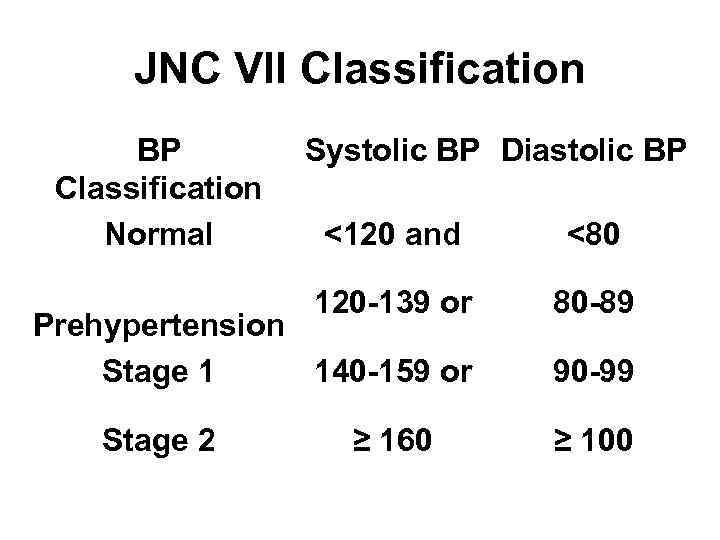
JNC VII Classification BP Classification Normal Systolic BP Diastolic BP <120 and <80 120 -139 or 80 -89 Prehypertension Stage 1 140 -159 or Stage 2 ≥ 160 90 -99 ≥ 100
Diagnosis of HTN • Values must be obtained on at least two separate occasions UNLESS end organ damage already exists. • Must R/O any possible secondary causes at initial workup.
Essential vs. Secondary • Essential – 95%, Secondary – 5%. • Assess for historical clues. • PE findings suggest 2º etiology. • New onset < 30 y. o. or > 50 y. o. . • Poor control despite multiple meds. • Sudden change in stable HTN.
Factors Affecting HTN • Nonreversible: Age Race Gender Hereditary • Reversible: Salt Sensitivity (blacks & elderly) Alcohol Emotional stress Low physical activity Obesity Tobacco
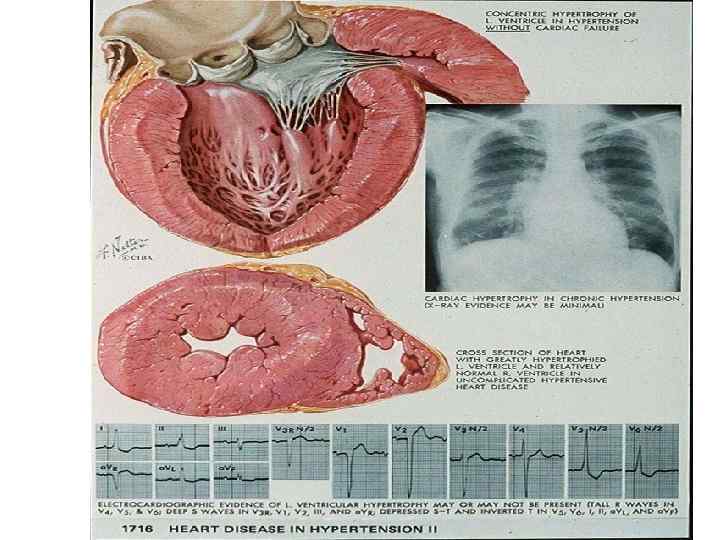
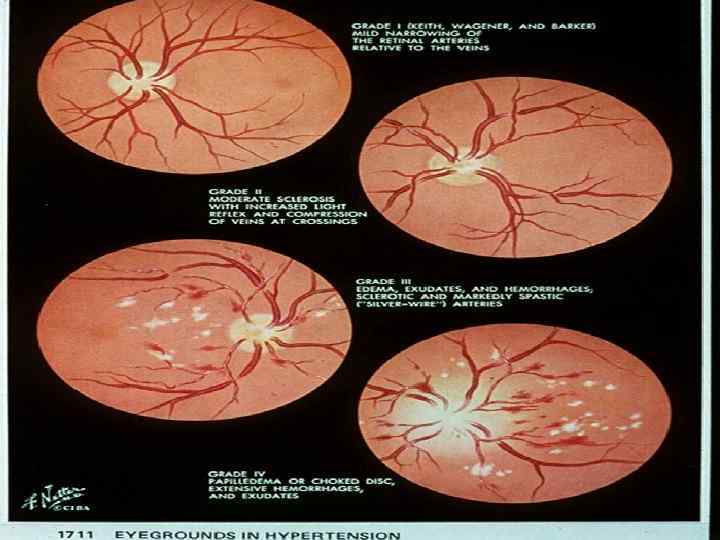
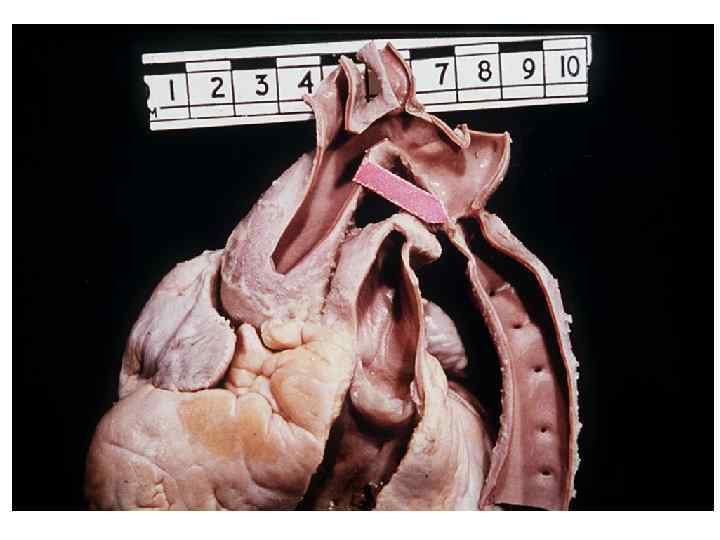
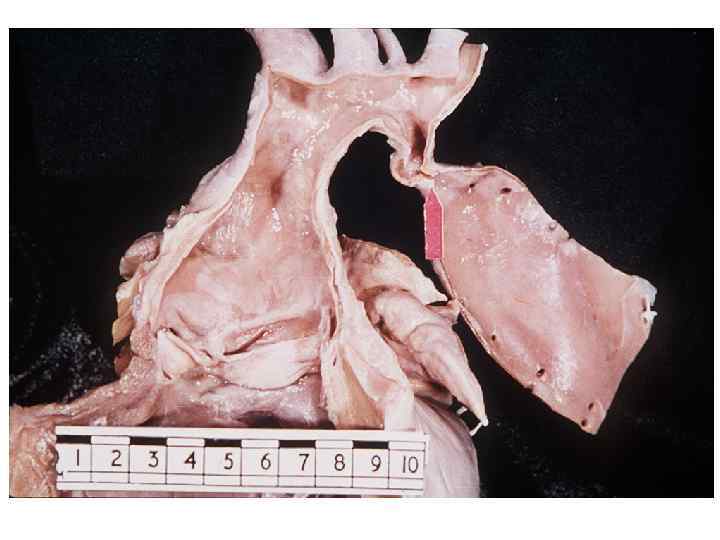
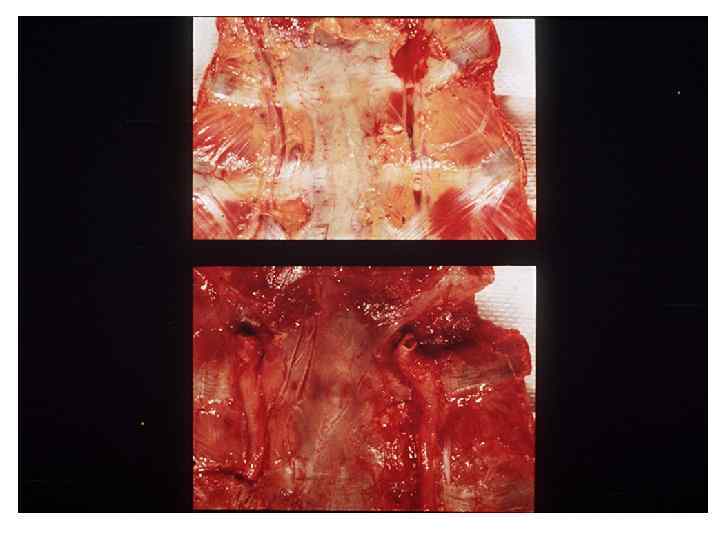
Detrimental Effects of HTN • Cardiac Complications – LVH, diastolic dysfunction, systolic dysfunction, CAD. • CNS – hemorrhagic and / or thrombotic strokes. • Hypertensive retinopathy – acute/chronic. • Renal Disease. • Peripheral Vascular Disease (PVD).

Evaluation • Goals: • Determine if etiology is primary or secondary. • Identify & treat other correctable RF. • Identify end organ damage. • Determine factors that may influence drug choice.
Evaluation • History: • Generally asymptomatic. • Symptoms w/o vascular damage: • Occipital headache • Vertigo/tinnitus • Nose bleeds • Palpitations • Nervousness
Evaluation • History: • Symptoms with vascular damage: • Blurring vision • Hematuria/proteinuria • Transient ischemic attack (TIA) • Angina • Dyspnea • Pain (from dissecting aorta)
Hypertensive Emergency • • Violent headaches Vomiting Visual impairment Drowsiness Transient neurological deficits Catastrophic CNS complications Often associated with acute retinopathy: hemorrhage, exudates, papilledema
Physical Exam • Ideally, pt seated for 5 min, feet flat on floor, arm supported at heart level. • Appropriate sized cuff for arm. • At least two measurements (both arms initial evaluation). • Provide readings verbally and in writing to the pt.
Physical Exam • Funduscopic exam: • Arteriolar narrowing. • Keith-Wagener-Baker Classification. • Neck: • Thyroid. • Bruits. • JVD. • Cardiac exam including extremities. • Abdomen for masses, kidneys, bruits, AAA. • Calculation of BMI. • Neurologic exam.
Screening Labs • Urine • Calcium • Creatinine/BUN • Lipid profile • Potassium • CBC • Uric acid • TSH • Fasting glucose • ECG
Ambulatory BP Monitoring • White-coat syndrome. • Drug resistance. • Episodic HTN. • Autonomic dysfunction. • Correlates better with target organ injury. • Info about night reductions (↑ CV risk if not reduced by 10 -20% @ night).
Secondary HTN • Clinical Clues: • Age - <20 or >50. • Severity – often Stage 2. • Onset – abrupt. • Associated Signs/Symptoms. • FH – sporadic.
Causes of Secondary HTN • Primary renal parenchymal disease. • Renovascular hypertension. • Pheochromocytoma. • Primary Aldosteronism. • Oral contraceptives.
Causes of Secondary HTN • Coarctation of the Aorta. • Hyperthyroidism. • CNS disorders. • Toxemia of pregnancy. • Tobacco. • Alcohol excess.
Renal Parenchymal Disease (2 -4%) • Mechanism: • Salt and water retention (↑ intravascular volume). • Renin/angiotensin mediated. • HTN (most frequent complication): • Vicious cycle. • Most renal failure patients die from vascular complications. • Treatment of hypertension delays ESRF.
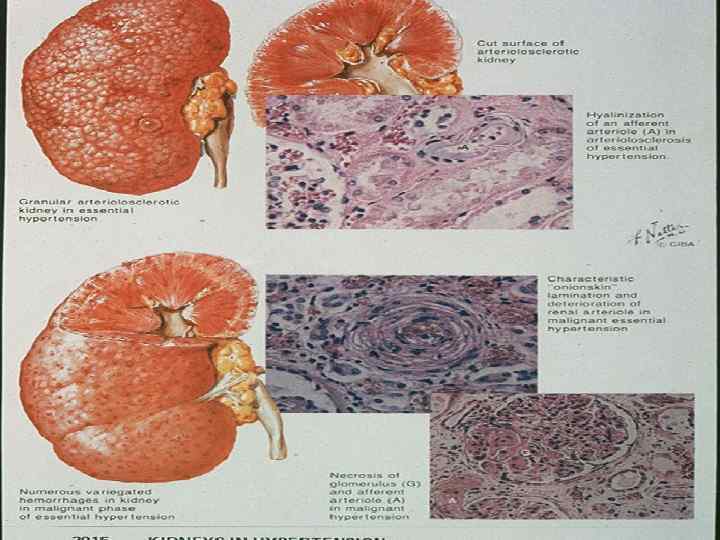
Renal Parenchymal Disease • Presentation: • Elevated BUN. • Elevated Creatinine. • Treatment: • ACE inhibitor. • Lasix.
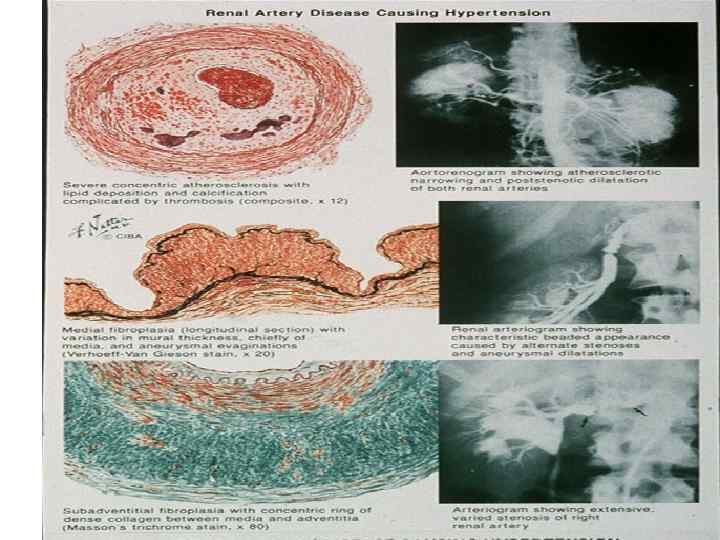
Renovascular Hypertension (1%) • Mechanism - ↑ renin levels. • Etiology: • Vascular obstruction. • Atherosclerotic plaque – older males. • Fibromuscular dysplasia – young women. • Arteritis.
Clinical Clues to RV HTN • Onset < 30 w/o family history or recent onset > 55. • Abdominal bruit. • Accelerated or resistant HTN. • Recurrent pulmonary edema. • Coexisting vascular disease. • Acute renal failure precipitated by antihypertensives (ACEI or Angiotensin II blockers).
Evaluation RV HTN • Rapid sequence IVP • Difference in kidney size by 1. 5 cm. • Captopril enhanced radionuclide renal scan. • Renal Flow Scan. • Use if renal failure or dye allergy. • Renal arteriography. • Selective renal vein renins.
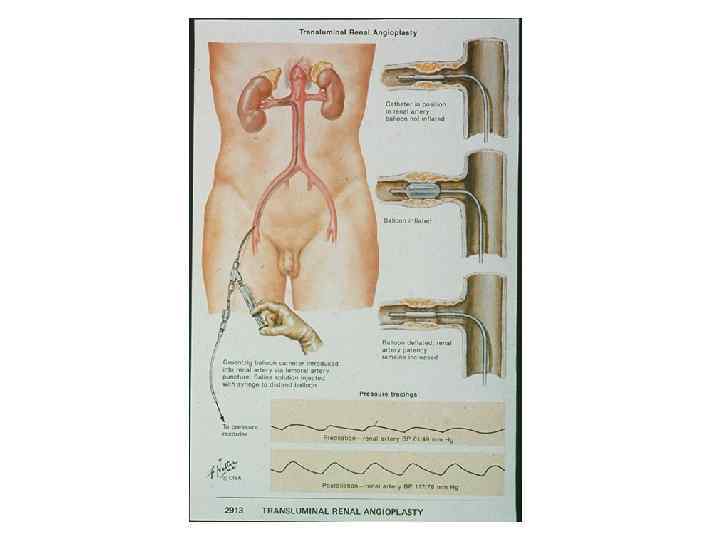
Treatment of RV HTN • ACE inhibitors: • Not in bilateral renal stenosis or • Unilateral renal stenosis with one kidney. • Monitor renal function closely. • Consider angioplasty. • Consider surgery.
Pheochromocytoma (0. 2%) • Adrenal tumor: • Medulla secretes NE and Epinephrine. • Metabolized to metanephrine or VMA. • May be familial. • 90 % benign. • 10 % multiple, ectopic, and malignant.
Clinical Presentation - Pheo • Moderate - severe paroxysms of HTN: • Headache. • Palpitations. • Sweating. • Nausea, vomiting. • Tachycardia. • Weight loss. • Hyperglycemia.
PE/Lab Pheo • EKG – LVH. • UA – proteinuria. • 24 h urine for metanephrines. • Adrenal CT or MRI. • Arteriography.
Treatment for HTN 2º Pheo • Medications: • Combination of alpha and beta blockers. • Phentolamine, phenoxybenzamine first, then beta blocker. • Surgical excision.
Primary Aldosteronism • Hyperaldosteronism leads to retention of Na+ and excretion of K+. • Renin release is suppressed. • Suggested if HTN & • Unprovoked hypokalemia. • Symptoms of hypokalemia.
Primary Aldosteronism • Treatment: Don’t use potassium wasting diuretics. • Aldosterone blockade: • Spironolactone. • Amiloride. • Surgery - Generally 2º adrenal adenoma (Conn’s syndrome).
Cushing Syndrome (. 1 %) • Excessive corticosteroids – pituitary or adrenal adenoma. • History: • Sexual dysfunction. • Weakness. • Backache.
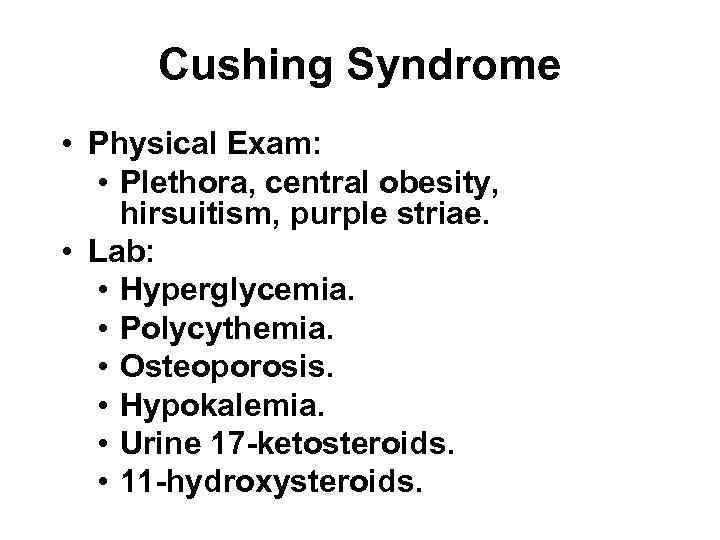
Cushing Syndrome • Physical Exam: • Plethora, central obesity, hirsuitism, purple striae. • Lab: • Hyperglycemia. • Polycythemia. • Osteoporosis. • Hypokalemia. • Urine 17 -ketosteroids. • 11 -hydroxysteroids.
Cushing Syndrome • Diagnosis: • 24 hour urine test for cortisol; • <2750 nmol r/o Cushing’s. • Dexamethasone suppression test: • give 1 mg at bedtime. • measure am serum cortisol level between 0700 -1000 hours.
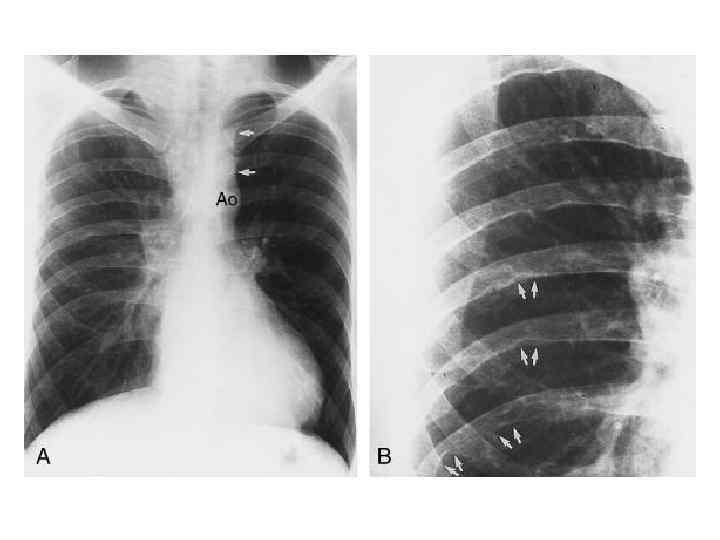
Coarctation of the Aorta • Congenital narrowing of thoracic aorta – generally distal to L subclavian: • ↓ perfusion of kidneys. • ↑ renin, Na+, H 2 O retention.
Coarctation of the Aorta • Presentation: • Young patient with HTN • UE but not LE • RA pressure > LA • + Claudication • Systolic murmur • CXR • rib notching • 3 sign
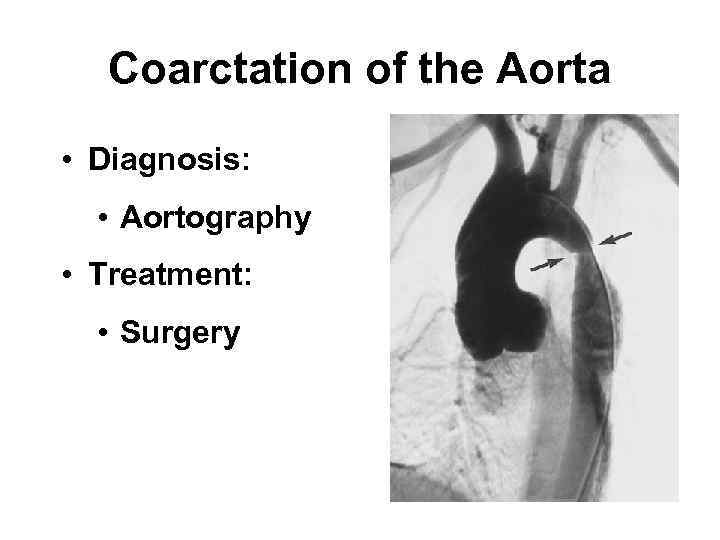
Coarctation of the Aorta • Diagnosis: • Aortography • Treatment: • Surgery
Miscellaneous Etiologies HTN • Oral Contraceptives: • increase renin and angiotensin I • D/C if other CRF or severe HTN. • Hyperthyroidism, Hypothyroidism. • CNS disorder. • Toxemia of pregnancy. • Tobacco. • Alcohol excess.
JNC VII Key Points • In pts > 50 y. o. , SBP > 140 mm. Hg is a much more important CVD risk factor than DBP. • The risk of CVD beginning at 115/75 mm. Hg doubles with each increment of 20/10 mm. Hg. • Individuals who are normotensive at age 55 have a 90% lifetime risk for developing HTN.
JNC VII Key Points • Thiazide type diuretics should be used in Rx for most pts with HTN, either alone or combined with drugs from other classes. • Most pts will require 2 or more antihypertensive meds to achieve goal (<140/90 mm. Hg, or <130/80 mm. Hg if DM or CRF). • If BP >20/10 mm. Hg above goal, consider initiating Rx with 2 agents, one should be a thiazide.
Treatment of Essential HTN • Non-pharmacologic Rx measures: • Weight reduction. • Decrease sodium intake. • Decrease alcohol. • Stop smoking. • Low cholesterol / low fat diet. • Increase exercise. • Stress avoidance.
Why use Drugs? • Decrease morbidity and mortality. • High risk groups: • Men. • Blacks. • Young age. • Other risk factors. • End organ damage present.
Why use Drugs? • Rx mild HTN: • Mortality decreases 20%. • Prevent severe HTN. • Protect from: • LVH. • Renal disease. • Eye complications.
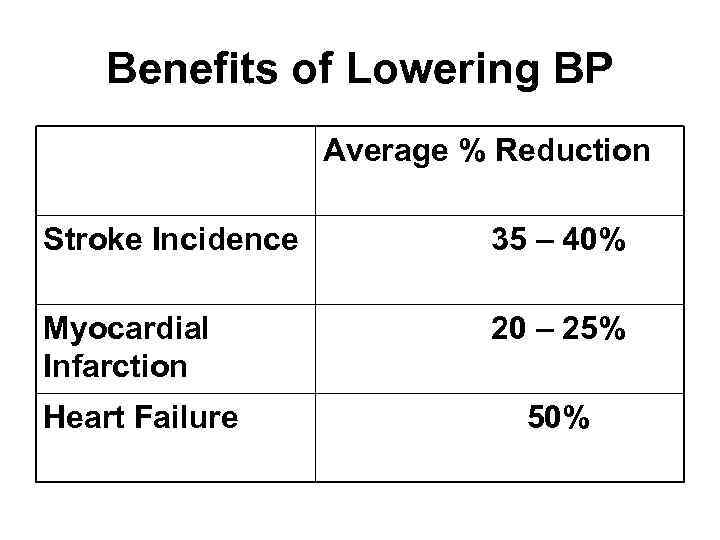
Benefits of Lowering BP Average % Reduction Stroke Incidence 35 – 40% Myocardial Infarction 20 – 25% Heart Failure 50%
4 Classes of Drugs • Diuretics. • Sympatholytics. • Vasodilators. • Renin-angiotensin system antagonists.
Diuretics • Thiazide: • Hydrochlorothiazide (HCTZ). • Loop: • Lasix. • Potassium sparing diuretics: • Spironolactone.
Thiazide Diuretics • Mechanism: • Sodium depletion. • Indication: • Mild HTN. • Combination. • Contraindications: • Hyperuricemia. • Primary Aldosteronism.
Thiazide Diuretics • Side effects: • Hypokalemia. • Hyperglycemia. • Hyperuricemia. • Hypercalcemia. • Dehydration. • Dermatitis. • Depression.
Loop Diuretics • Indication: • HTN with renal insufficiency. • Contraindications: • Hyperuricemia. • Primary Aldosteronism.
Loop Diuretics • Side effects: • Hypokalemia. • Hyperuricemia. • Hyperglycemia. • Hypercalcemia. • Volume depletion. • Rash.
Potassium Sparing Diuretics • Indications: • HTN secondary to ↑ mineralcorticoids and as adjuvant to thiazides (Maxzide). • Contraindications: • Renal failure. • Use with caution in combo with ACEI. • Side effects: • Hyperkalemia, diarrhea, gynecomastia.
Sympatholytics • Beta blockers. • Combined alpha-beta blockers. • Central alpha antagonists. • Peripheral alpha blockers.
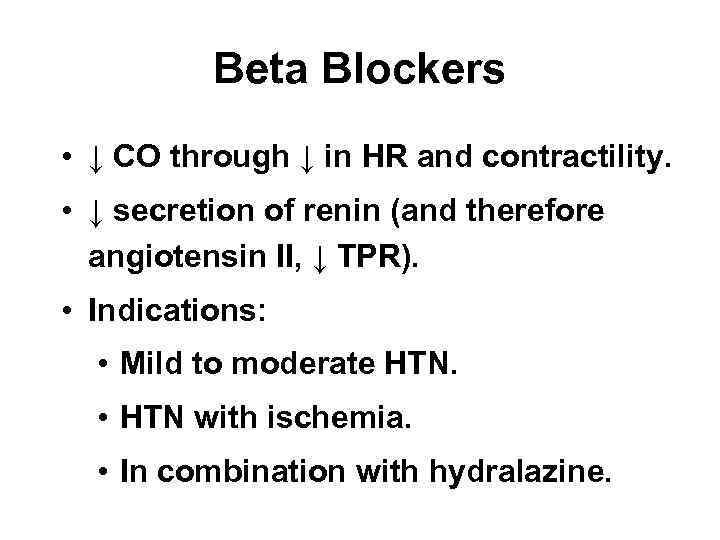
Beta Blockers • ↓ CO through ↓ in HR and contractility. • ↓ secretion of renin (and therefore angiotensin II, ↓ TPR). • Indications: • Mild to moderate HTN. • HTN with ischemia. • In combination with hydralazine.
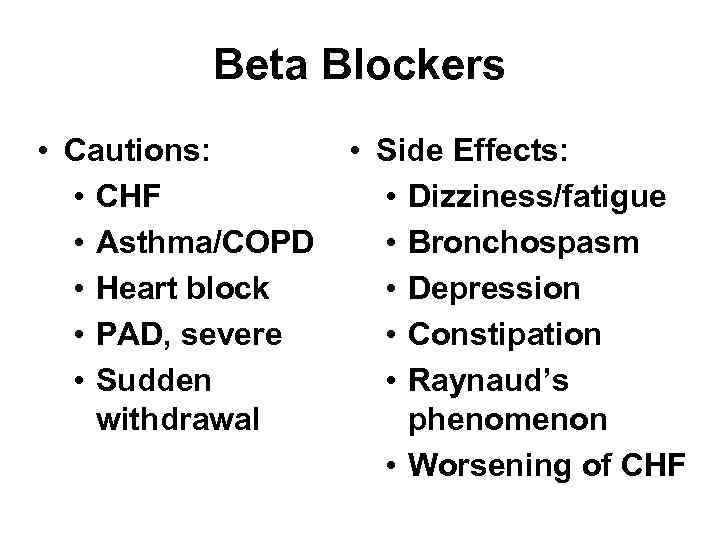
Beta Blockers • Cautions: • CHF • Asthma/COPD • Heart block • PAD, severe • Sudden withdrawal • Side Effects: • Dizziness/fatigue • Bronchospasm • Depression • Constipation • Raynaud’s phenomenon • Worsening of CHF
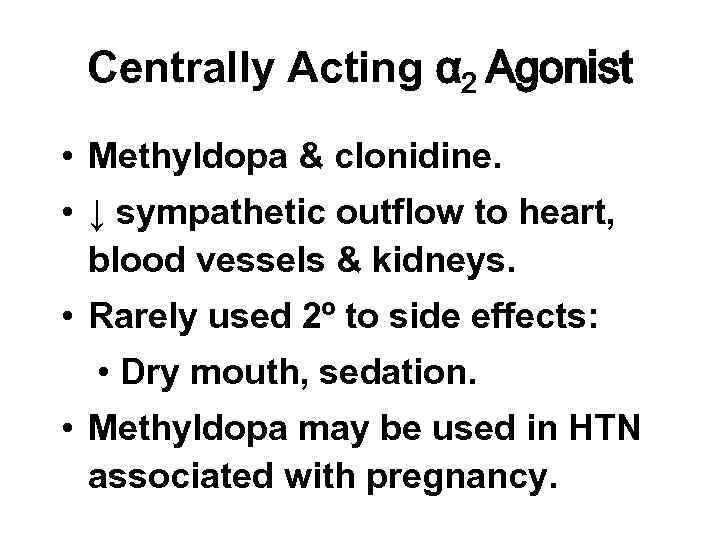
Centrally Acting α 2 Agonist • Methyldopa & clonidine. • ↓ sympathetic outflow to heart, blood vessels & kidneys. • Rarely used 2º to side effects: • Dry mouth, sedation. • Methyldopa may be used in HTN associated with pregnancy.
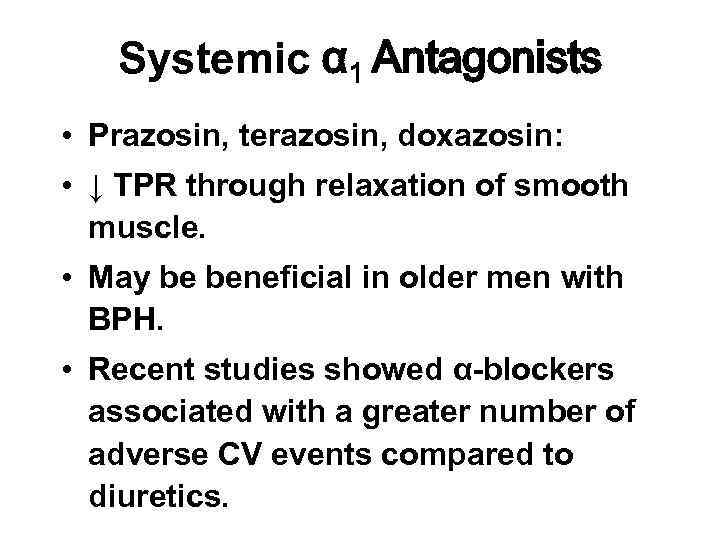
Systemic α 1 Antagonists • Prazosin, terazosin, doxazosin: • ↓ TPR through relaxation of smooth muscle. • May be beneficial in older men with BPH. • Recent studies showed α-blockers associated with a greater number of adverse CV events compared to diuretics.
Vasodilators • Direct vasodilators: hydralazine & minoxidil: • Act by relaxing vascular smooth muscle of precapillary resistance vessels. • Causes reflex ↑ in HR, therefore often given with a β-blocker.
Vasodilators • Ca++ Channel blockers: • ↓ cardiac contractility and TPR. • Marked differences in drugs in this class: • Dihydropyridines: nifedipine, amlodipine, felodipine, etc. • Marked vasodilation with little negative inotropic effect.
Ca++ Channel Blockers • Nondihydropyridines with potent negative inotropic (esp. Verapamil) effects. • Niche uses: • Mod HTN, peripheral vasospasm– dihydropyridine. • SVT – verapamil. • Vasospastic angina – diltiazem.
Ca++ Channel Blockers • Cautions: • Dihydropyridines – reflex tachy, so not good with ischemic heart disease. • Nondihydropyridines – potent negative inotropism (trigger CHF), suppression of AV node so do not give with AV block. • Avoid if possible in peri-myocardial infarct period as ↑ mortality noted.
Renin-angiotensin System Antagonists • Angiotensin Converting Enzyme Inhibitors (ACEI). • Block conversion angiotensin I to angiotensin II. • ↓ in TPR and Na+ retention. • Indicated for mild-severe HTN and unilateral renal artery stenosis.
ACE Inhibitors • Contraindications: • Renal failure. • Pregnancy – teratogenic. • Bilateral renal artery stenosis or solitary kidney with stenosis.
ACE Inhibitors • Side effects: • Dry cough 2º ↑ in circulating bradykinin. • Acute renal failure. • Angioedema. • Urticarial rash. • Hyperkalemia. • Hypotension.
Renin-angiotensin System Antagonists • Angiotensin receptor blockers (ARBs): • Losartan, Valsartan, Telmisartan, candesartan. • Block binding of angiotensin II to its receptors in blood vessels resulting in vasodilation and ↓ secretion of aldosterone. • Similar to ACEI in efficacy, well tolerated.
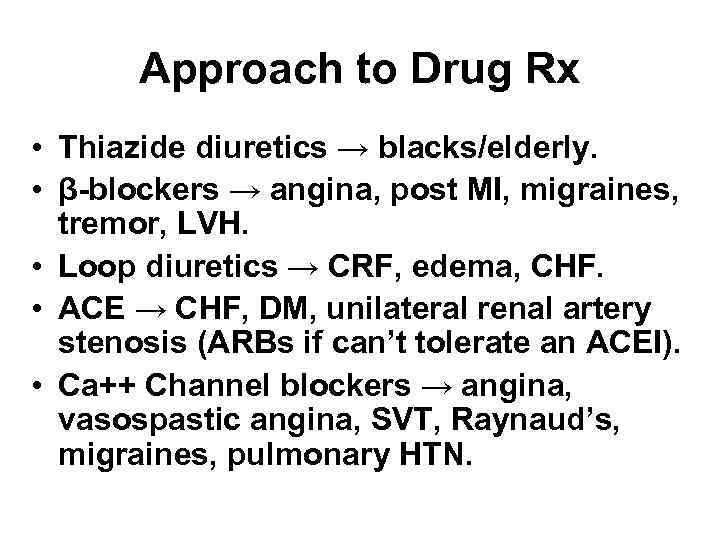
Approach to Drug Rx • Thiazide diuretics → blacks/elderly. • β-blockers → angina, post MI, migraines, tremor, LVH. • Loop diuretics → CRF, edema, CHF. • ACE → CHF, DM, unilateral renal artery stenosis (ARBs if can’t tolerate an ACEI). • Ca++ Channel blockers → angina, vasospastic angina, SVT, Raynaud’s, migraines, pulmonary HTN.
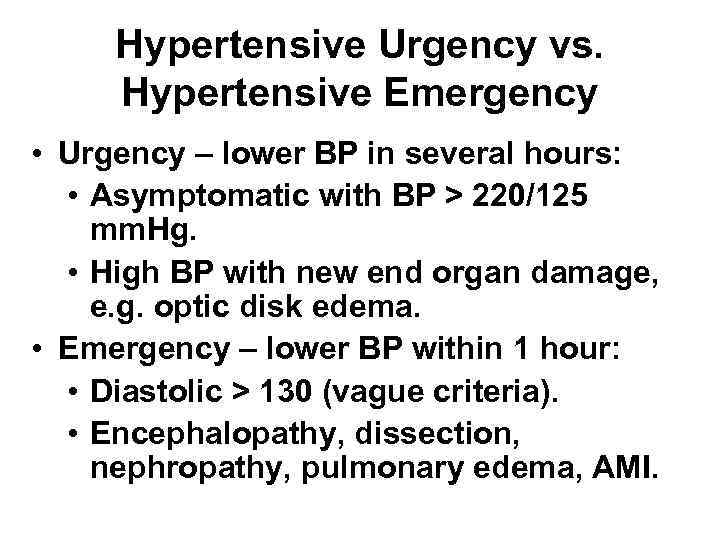
Hypertensive Urgency vs. Hypertensive Emergency • Urgency – lower BP in several hours: • Asymptomatic with BP > 220/125 mm. Hg. • High BP with new end organ damage, e. g. optic disk edema. • Emergency – lower BP within 1 hour: • Diastolic > 130 (vague criteria). • Encephalopathy, dissection, nephropathy, pulmonary edema, AMI.
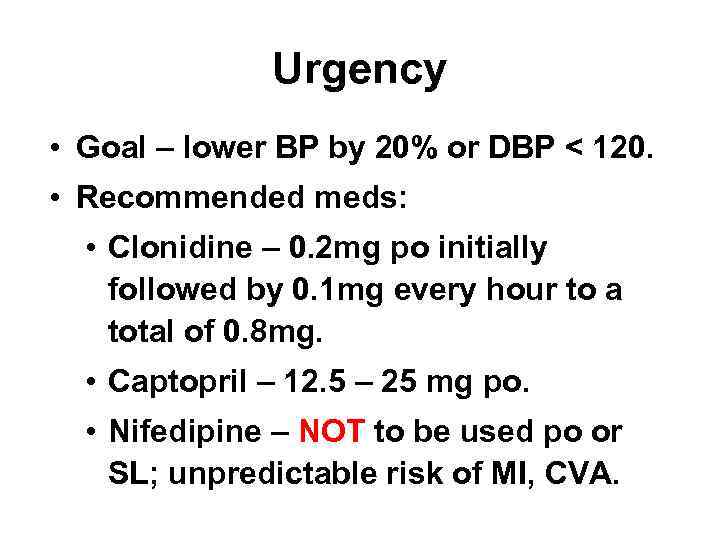
Urgency • Goal – lower BP by 20% or DBP < 120. • Recommended meds: • Clonidine – 0. 2 mg po initially followed by 0. 1 mg every hour to a total of 0. 8 mg. • Captopril – 12. 5 – 25 mg po. • Nifedipine – NOT to be used po or SL; unpredictable risk of MI, CVA.
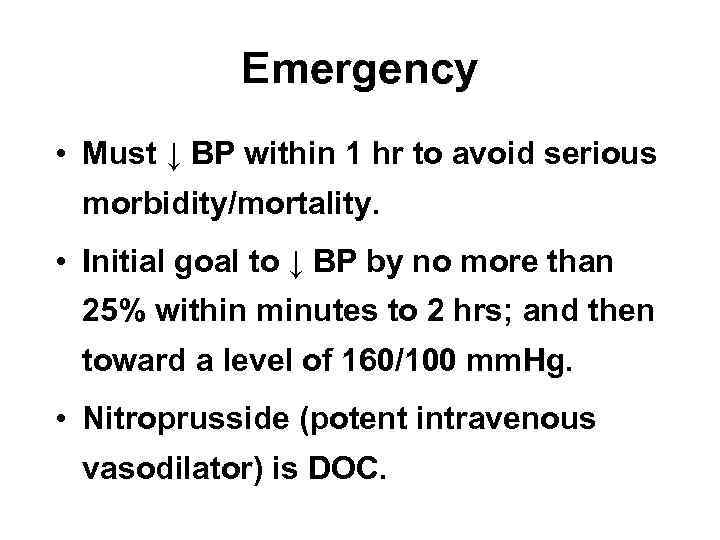
Emergency • Must ↓ BP within 1 hr to avoid serious morbidity/mortality. • Initial goal to ↓ BP by no more than 25% within minutes to 2 hrs; and then toward a level of 160/100 mm. Hg. • Nitroprusside (potent intravenous vasodilator) is DOC.
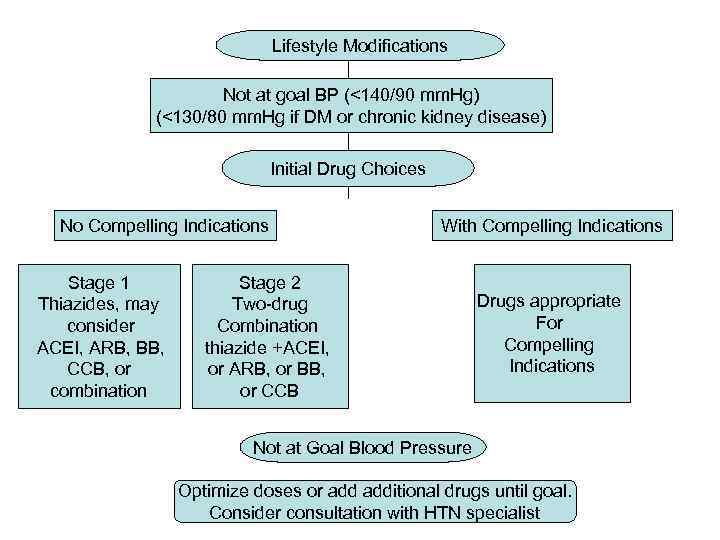
Lifestyle Modifications Not at goal BP (<140/90 mm. Hg) (<130/80 mm. Hg if DM or chronic kidney disease) Initial Drug Choices No Compelling Indications Stage 1 Thiazides, may consider ACEI, ARB, BB, CCB, or combination With Compelling Indications Stage 2 Two-drug Combination thiazide +ACEI, or ARB, or BB, or CCB Drugs appropriate For Compelling Indications Not at Goal Blood Pressure Optimize doses or additional drugs until goal. Consider consultation with HTN specialist
Hypertension-W.ppt