c85985fa904e75b8ab5713cca17eb8ec.ppt
- Количество слайдов: 83
SYNCOPE EVALUATION AND MANAGEMENT Jayne Barr, MD Clinical Assistant Professor The Ohio State University
Case #1 • 42 year old female • Chief complaint: passing out at work • Works in a pharmaceutical lab. Was sitting at her desk, felt nauseated and knew she was going to pass out. • Per witnesses, was slump over chair and was unconscious for a few seconds.
Case continues • No chest pain, palpitations, shortness of breath • Similar episodes 10 years ago. • No family history of sudden cardiac death • No medications. • No smoking. No alcohol. No drugs.
Case #2 • • • 82 year old male. Found unresponsive by his son Past medical history—HTN Medications—HCTZ Exam—BP 160/98. P 70. Now alert and oriented. Facial contusions. Otherwise normal exam. Q: How would you manage these 2 patients?
Syncope: Definition • Abrupt and self-limited loss of consciousness associated with absence of postural tone • Relatively rapid onset. Variable warning symptoms. • Followed by rapid and complete recovery. Last only a few minutes. • Absence of prolonged confusion • Presyncope---prodromal symptom of fainting and typically has the same work up as syncope.
Significance of Syncope • “The only difference between syncope and sudden death is that in one you wake up”. [1] • --anonomymous
Syncope: Epidemiology • 20 -50% of adults experience at least one episode of syncope during their lifetime. • Explained 53 -62% • Infrequent, unexplained 38 -47% • • 500, 000 new syncope patients each year. 3 -5% of ER visits. 6% of hospital visits. More common in the elderly. • Up to 23% in age >70 years.
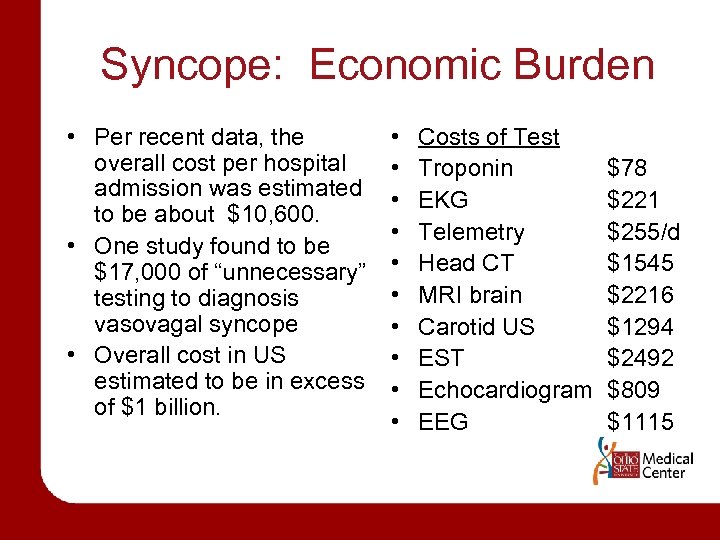
Syncope: Economic Burden • Per recent data, the overall cost per hospital admission was estimated to be about $10, 600. • One study found to be $17, 000 of “unnecessary” testing to diagnosis vasovagal syncope • Overall cost in US estimated to be in excess of $1 billion. • • • Costs of Test Troponin EKG Telemetry Head CT MRI brain Carotid US EST Echocardiogram EEG $78 $221 $255/d $1545 $2216 $1294 $2492 $809 $1115
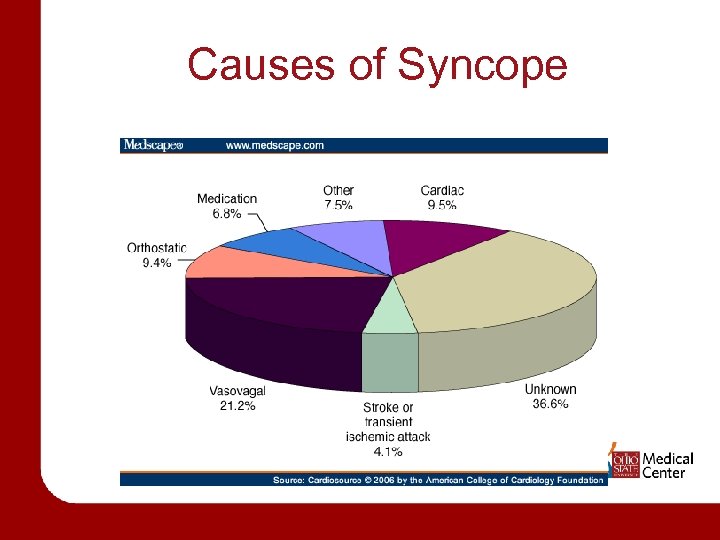
Causes of Syncope
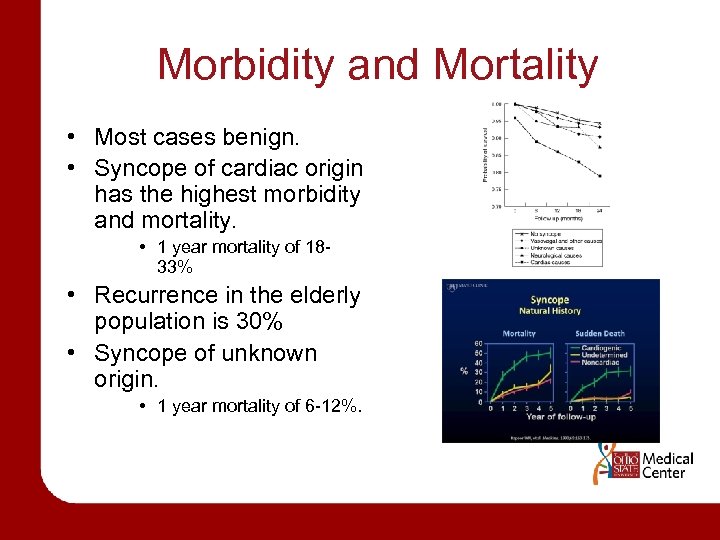
Morbidity and Mortality • Most cases benign. • Syncope of cardiac origin has the highest morbidity and mortality. • 1 year mortality of 1833% • Recurrence in the elderly population is 30% • Syncope of unknown origin. • 1 year mortality of 6 -12%.
Syncope in Children • Generally a benign event. • Rare but serious • Most common causes – – Vasovagal (40%) Simple faint (29%) Breathholding (4%) Unknown (15%) causes of syncope in children – Hypertrophic cardiomyopathy – Anomalous origin of left coronary artery – Myocarditis – Long QT syndrome – Cystic medial necrosis – WPW
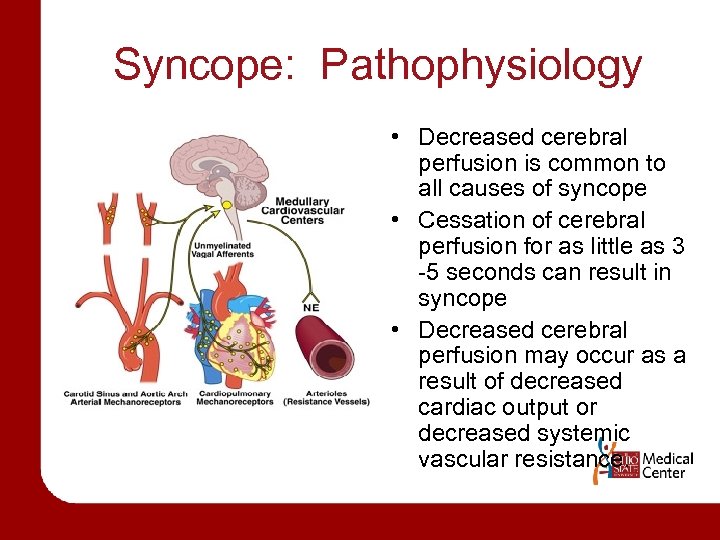
Syncope: Pathophysiology • Decreased cerebral perfusion is common to all causes of syncope • Cessation of cerebral perfusion for as little as 3 -5 seconds can result in syncope • Decreased cerebral perfusion may occur as a result of decreased cardiac output or decreased systemic vascular resistance.
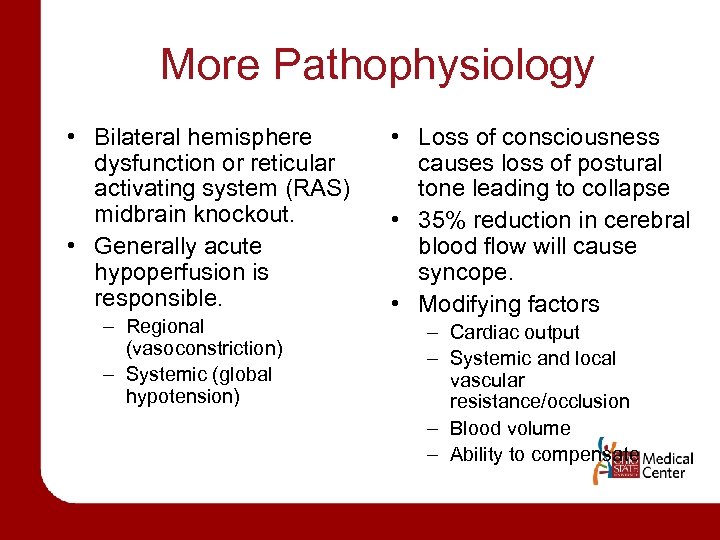
More Pathophysiology • Bilateral hemisphere dysfunction or reticular activating system (RAS) midbrain knockout. • Generally acute hypoperfusion is responsible. – Regional (vasoconstriction) – Systemic (global hypotension) • Loss of consciousness causes loss of postural tone leading to collapse • 35% reduction in cerebral blood flow will cause syncope. • Modifying factors – Cardiac output – Systemic and local vascular resistance/occlusion – Blood volume – Ability to compensate
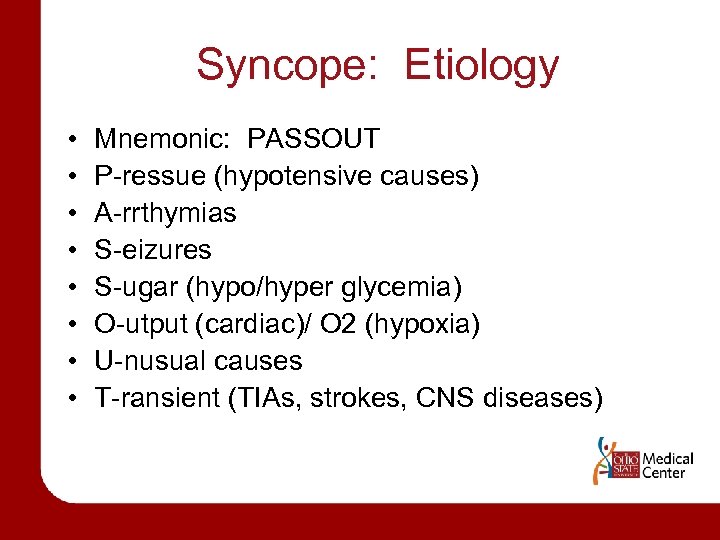
Syncope: Etiology • • Mnemonic: PASSOUT P-ressue (hypotensive causes) A-rrthymias S-eizures S-ugar (hypo/hyper glycemia) O-utput (cardiac)/ O 2 (hypoxia) U-nusual causes T-ransient (TIAs, strokes, CNS diseases)
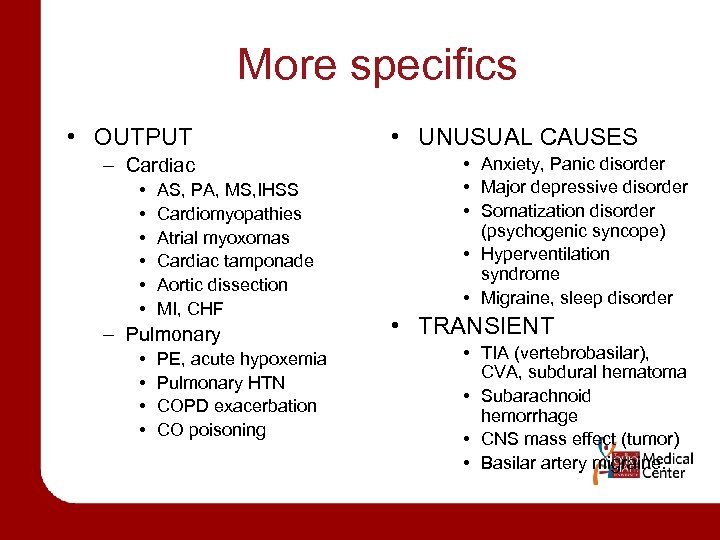
More specifics • OUTPUT – Cardiac • • • AS, PA, MS, IHSS Cardiomyopathies Atrial myoxomas Cardiac tamponade Aortic dissection MI, CHF – Pulmonary • • PE, acute hypoxemia Pulmonary HTN COPD exacerbation CO poisoning • UNUSUAL CAUSES • Anxiety, Panic disorder • Major depressive disorder • Somatization disorder (psychogenic syncope) • Hyperventilation syndrome • Migraine, sleep disorder • TRANSIENT • TIA (vertebrobasilar), CVA, subdural hematoma • Subarachnoid hemorrhage • CNS mass effect (tumor) • Basilar artery migraine.
Syncope • CAUSES (Head---Heart---Vessels) – Reflex mediated • Vasovagal, carotid sinus, situational – Cardiac • Mechanical , arrhythmias – Orthostatic • Drugs, autonomic failure – Cerebrovascular – Unknown – Nonsyncopal causes
Neurally mediated reflex syncope (36 -62%); average (24%) • Vasovagal, carotid sinus, situational • No increased risk for cardiovascular morbidity or mortality associated with reflex mediated syncope.
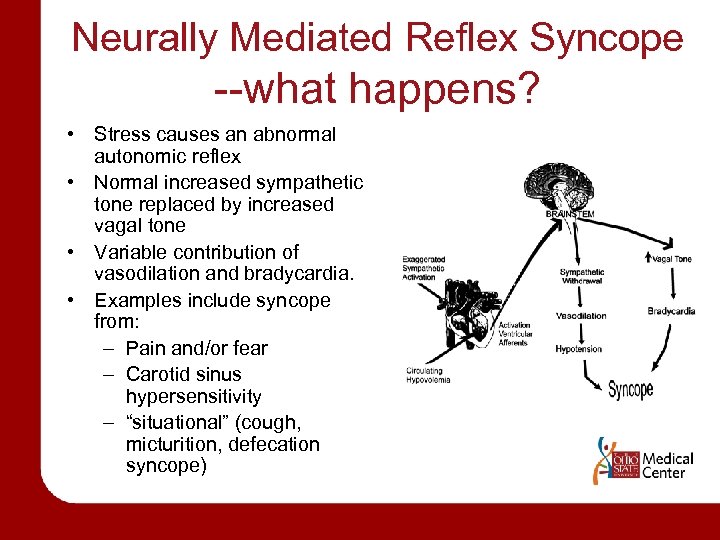
Neurally Mediated Reflex Syncope --what happens? • Stress causes an abnormal autonomic reflex • Normal increased sympathetic tone replaced by increased vagal tone • Variable contribution of vasodilation and bradycardia. • Examples include syncope from: – Pain and/or fear – Carotid sinus hypersensitivity – “situational” (cough, micturition, defecation syncope)
Vasovagal syncope • Most common cause of syncope in young adults • Precipitating event is often identifiable – Stress, trauma, pain, sight of blood, prolonged standing, heat exposure
Vasovagal Syncope • 3 PHASES • --Prodrome • Diaphoresis, epigastric discomfort, weakness, nausea, dizziness • Lasts about 2 minutes • --Loss of consciousness • Usually lasts 5 -20 seconds • --Postsyncopal phase • Nausea, dizziness, general sense of poor health • If present, confusion which lasts no more than 30 seconds
Prevalence of Vaso. Vagal Syncope • Prevalence poorly known (8 -37% with mean of 18%) • Important points – Patients with VVS younger than Carotid sinus syndrome patients – Age range teens to elderly with mean 43 years – Pallor, nausea, sweating, palpitations are common – Amnesia for warning symptoms in older patients
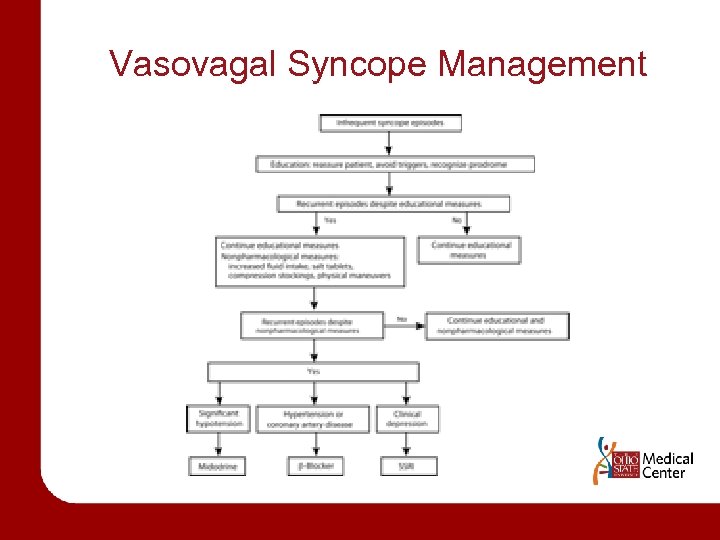
Vasovagal Syncope Management
Management for Vasovagal syncope • Optimal management is source of debate – – Patient education, reassurance, instruction Fluids (sports drinks), salt, diet Tilt training Support hose (waist high) • Drug therapies • Pacing (DDD pacing) – Class II indication if positive tilt test and cardioinhibitory or mixed reflex
Drug therapies for Vasovagal syncope • Salt/volume – Salt, sports drinks, fludrocortisone • Beta-adrenergic blockers – 1 positive control study using atenolol – Use if hx of htn • Disopyramide • SSRIs – 1 controlled study – Use if hx of depression • Vasoconstrictors (eg, midodrine) – 1 negative controlled study (etilephrine) – ? Efficacy of neosynephrine – Use midodrine if significant hypotension
Postural Orthostatic Tachycardia Syndrome • Upright symptoms without hypotension. • Upright tachycardia—excessive HR response to maintain a low normal BP. • 500, 000 Americans, usually young women • Partial dysautonomia • Antecedent infection, surgery, pregnancy • Treatment—low dose propanolol 10 mg tid
Carotid Sinus Syncope • Syncope related to head turning, shaving, wearing a tight collar • Pathophysiology – Carotid sinus pressure causes a reflex decrease in heart rate and blood pressure
Carotid sinus massage • Site – Carotid arterial pulse just below thyroid cartilage • Method – Massage, not occlusion. – Right followed by left, pause between – Duration: 5 -10 seconds – Posture: supine and erect • Risks – 1/5000 massages complicated by TIA • Outcome – 3 sec asystole and/or 50 mm. Hg fall in systolic blood pressure with reproduction of symptoms ==CAROTID SINUS SYNDROME • Contraindications – Carotid bruit, known but significant carotid arterial disease, previous CVA, MI last 3 months.
Situational Syncope • Related to micturition, defecation, swallowing or coughing • Induced by baroreceptor and mechanoreceptors causing vagal stimulation • Circumstances of the event are typically diagnostic
Orthostatic syncope • • When vertical, blood follows gravity and pools. Increased sympathetic tone counteracts this. If the response is inadequate, syncope occurs. Drop in BP: 20 systolic or 10 diastolic within 3 minutes of standing • Present in 40% of patients over 70 years old • May be due to – Drugs – Volume loss – Neurologic damage
More on Orthostatic Hypotension • Volume loss – Assoc. with tachycardia • Medications – Seen in elderly 45% of time • Situational – Micturition, cough, postprandial, carotid sinus sensitivity, defecation, laughing • Adrenal insufficiency • Primary autonomic disease – Idiopathic, parkinsons disease, multisystem atrophy (Shy-Dragger) • Secondary autonomic disease – Neuropathic (dm, amyloid, alcoholism, autoimmune, vitamin deficiency, etc) – CNS (cva, MS, tumors, spinal cord)
Cardiac Syncope • Two basic types – Dysrhythmia mediated – Structural cardiopulmonary lesions • Both cause the heart to be unable to sufficiently increase cardiac output to meet demand • Double the risk of mortality compared with other syncopal patients. Up to 50% mortality. • Patients with underlying cardiac disease are at greatest risk for cardiac syncope. Only 3% have no previous heart disease. • Cardiac arrythymias especially in the elderly have high mortality.
Neurologic Syncope • Rarely the primary cause of syncope • Ischemia to the RAS in the brainstem may cause “drop attacks” • Results from Vertebrobasilar insufficiency due to TIA (sometimes basilar migraine) • Usually accompanied by vertigo, ataxia, dysarthia, diplopia • Other examples • Subclavian steal—occurs with arm activity. Systolic BP in arms (difference of 10 mm. Hg) • Subarachnoid hemorrhage
Psychiatric causes • Most commonly associated with • Anxiety • Panic • Major depressive disorders • Variety of mechanisms may be involved • Hyperventilation • Increased vagal tone
Syncope-like States • • Migraine Acute hypoxia Hyperventilation Somatization disorder (psychogenic syncope) Acute intoxication (ie alcohol) Seizures Hypoglycemia Sleep disorders
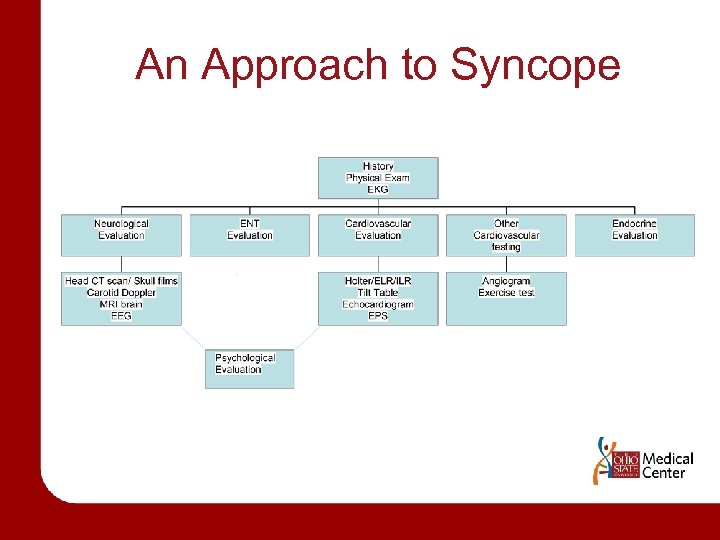
An Approach to Syncope
HISTORY • RAPID ASSESSMENT – Identify Life-Threatening causes – – – – Dysrhythmias cardiac ischemia Critical aortic stenosis Aortic dissection Pulmonary embolus CVA SAH Toxic-metabolic derangement
HISTORY • HISTORY alone identifies the cause up to 85% of the time • POINTS – Previous episodes – Character of the events, witnesses – Events preceding the syncope – Events during and after the episode
HISTORY • Events preceding the syncope – Prolonged standing (vasovagal) – Immediately upon standing (orthostatic) – With exertion (cardiac) – Sudden without warning or palpitations (cardiac) – Aggressive dieting – Heat exposure – Emotional stress • Events during and after the episode – Trauma (implication important) – Chest pain (CAD, PE) – Seizure (incontinence, confusion, tongue laceration, postictal behavior) – Cerebrovascular syndrome (diplopia, dysarthia, hemiparesis) – Associated with n/v/sweating (vasovagal)
HISTORY • Associated symptoms – Chest pain, SOB, lightheadedness, incontinence • Past medical history – Identifying risk factors – Morbidity and mortality increases with organic causes • Parkinsons (orthostatic) • Epilepsy (seizure) • DM (cardiac, autonomic dysfunction, glucose) • Cardiac disease • Medications – Antihypertensives, diuretics (orthostatic) – Antiarrthymics (cardiac syncope) – TCA, Amiodarone (cardiac/prolonged QT) • Family history – Sudden death (cardiac syncope/prolonged QT or Brugada)
PHYSICAL EXAM • Vital signs – Orthostatics—most important • Drop in BP and fixed HR >dysautonomia • Drop in BP and increase HR -> volume depletion/ vasodilatation • Insignificant drop in BP and marked increase in HR -> POTS – Temperature • Hypo/hyperthermia (sepsis, toxic-metabolic, exposure) – Heart rate • Tachy/brady, dysrhythmia – Respiratory rate • Tachypnea (pe, hypoxia, anxiety) • Bradypnea (cns, toxicmetabolic) – Blood pressure • High (cns, toxic/metabolic) • Low (hypovolemia, cardiogenic shock, sepsis)
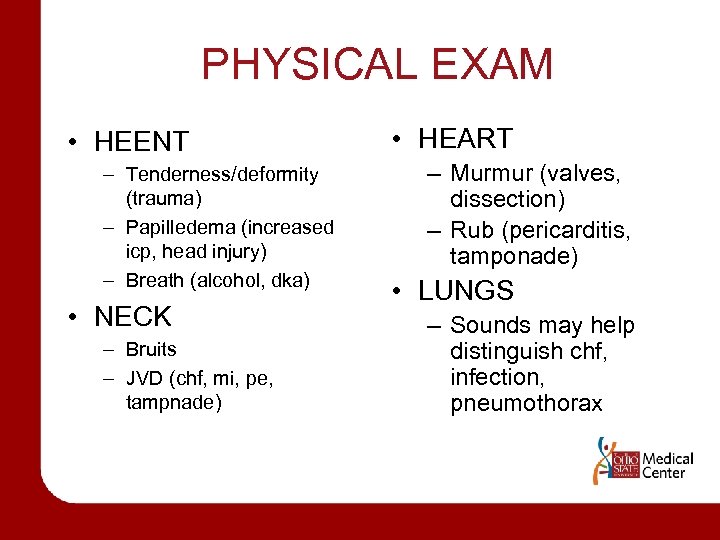
PHYSICAL EXAM • HEENT – Tenderness/deformity (trauma) – Papilledema (increased icp, head injury) – Breath (alcohol, dka) • NECK – Bruits – JVD (chf, mi, pe, tampnade) • HEART – Murmur (valves, dissection) – Rub (pericarditis, tamponade) • LUNGS – Sounds may help distinguish chf, infection, pneumothorax
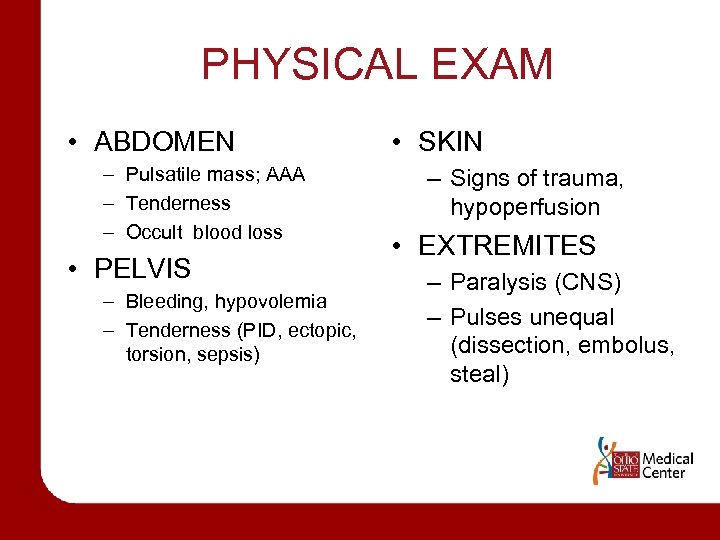
PHYSICAL EXAM • ABDOMEN – Pulsatile mass; AAA – Tenderness – Occult blood loss • PELVIS – Bleeding, hypovolemia – Tenderness (PID, ectopic, torsion, sepsis) • SKIN – Signs of trauma, hypoperfusion • EXTREMITES – Paralysis (CNS) – Pulses unequal (dissection, embolus, steal)
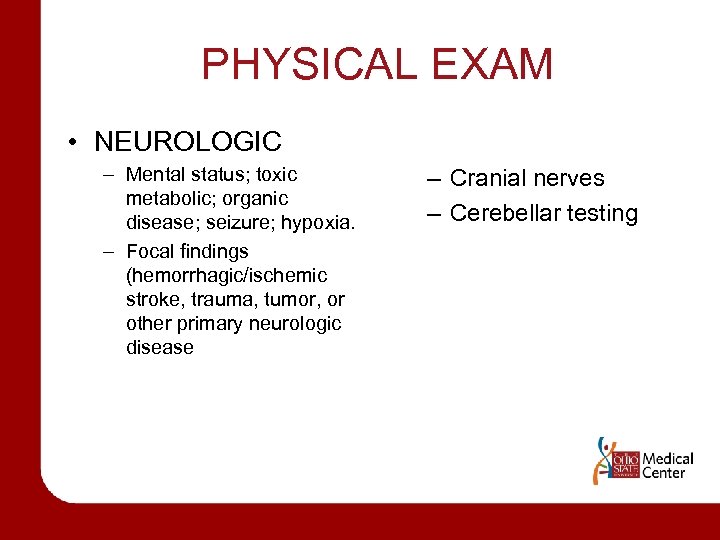
PHYSICAL EXAM • NEUROLOGIC – Mental status; toxic metabolic; organic disease; seizure; hypoxia. – Focal findings (hemorrhagic/ischemic stroke, trauma, tumor, or other primary neurologic disease – Cranial nerves – Cerebellar testing
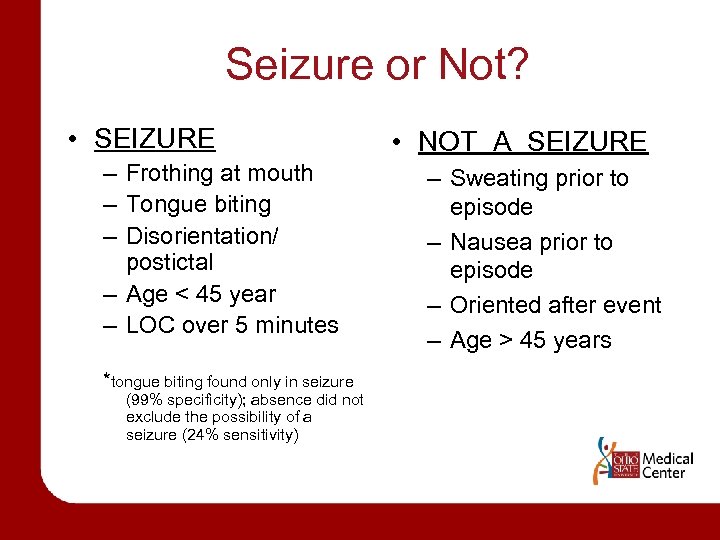
Seizure or Not? • SEIZURE – Frothing at mouth – Tongue biting – Disorientation/ postictal – Age < 45 year – LOC over 5 minutes *tongue biting found only in seizure (99% specificity); absence did not exclude the possibility of a seizure (24% sensitivity) • NOT A SEIZURE – Sweating prior to episode – Nausea prior to episode – Oriented after event – Age > 45 years
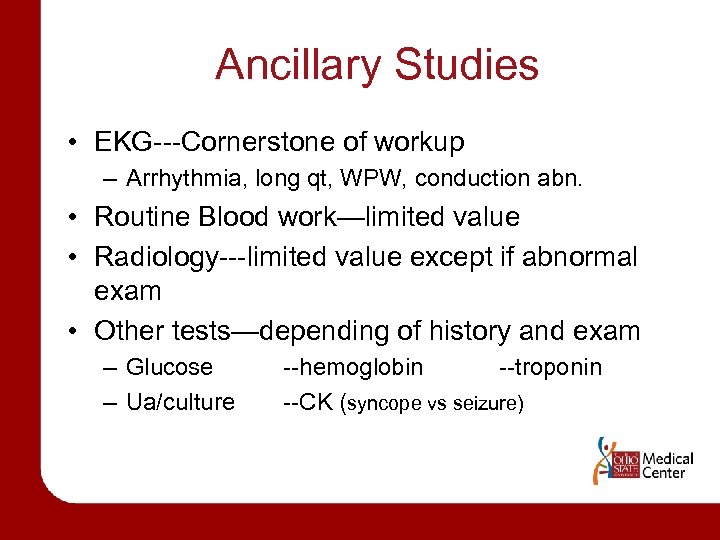
Ancillary Studies • EKG---Cornerstone of workup – Arrhythmia, long qt, WPW, conduction abn. • Routine Blood work—limited value • Radiology---limited value except if abnormal exam • Other tests—depending of history and exam – Glucose – Ua/culture --hemoglobin --troponin --CK (syncope vs seizure)
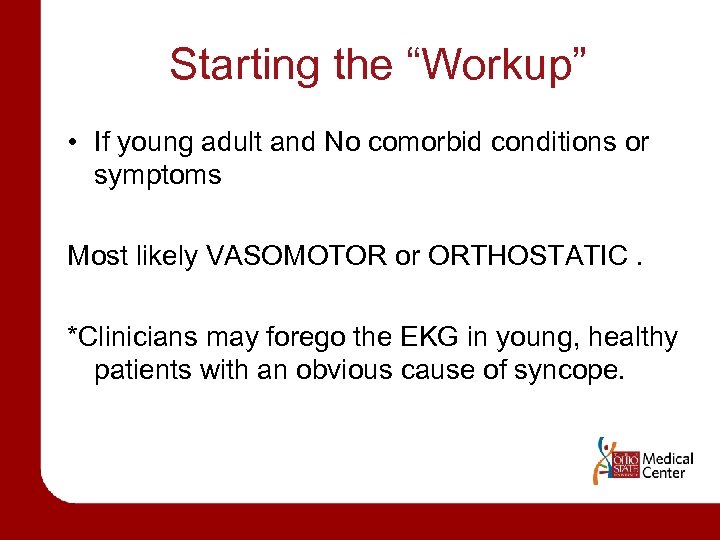
Starting the “Workup” • If young adult and No comorbid conditions or symptoms Most likely VASOMOTOR or ORTHOSTATIC. *Clinicians may forego the EKG in young, healthy patients with an obvious cause of syncope.
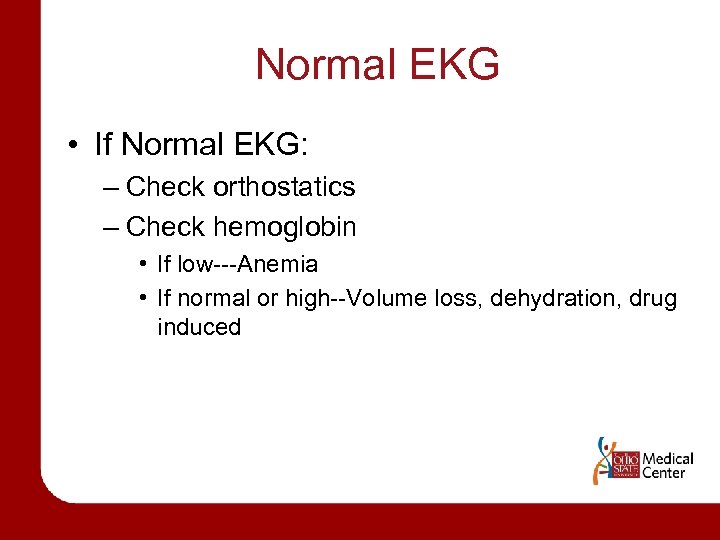
Normal EKG • If Normal EKG: – Check orthostatics – Check hemoglobin • If low---Anemia • If normal or high--Volume loss, dehydration, drug induced
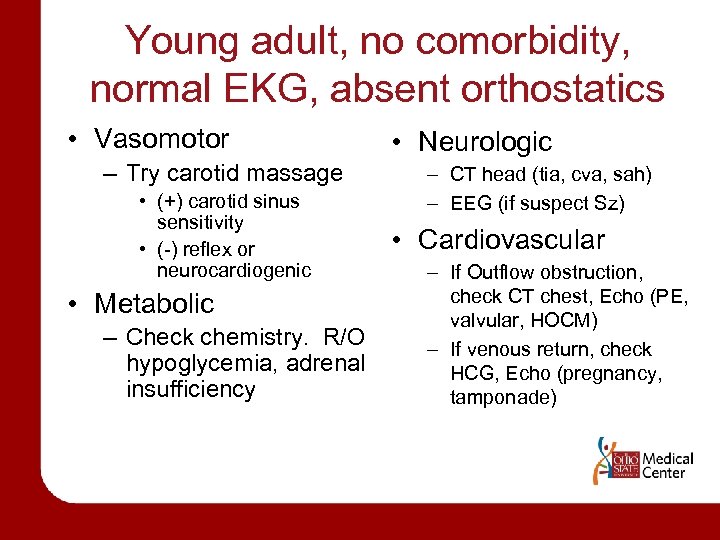
Young adult, no comorbidity, normal EKG, absent orthostatics • Vasomotor – Try carotid massage • (+) carotid sinus sensitivity • (-) reflex or neurocardiogenic • Metabolic – Check chemistry. R/O hypoglycemia, adrenal insufficiency • Neurologic – CT head (tia, cva, sah) – EEG (if suspect Sz) • Cardiovascular – If Outflow obstruction, check CT chest, Echo (PE, valvular, HOCM) – If venous return, check HCG, Echo (pregnancy, tamponade)
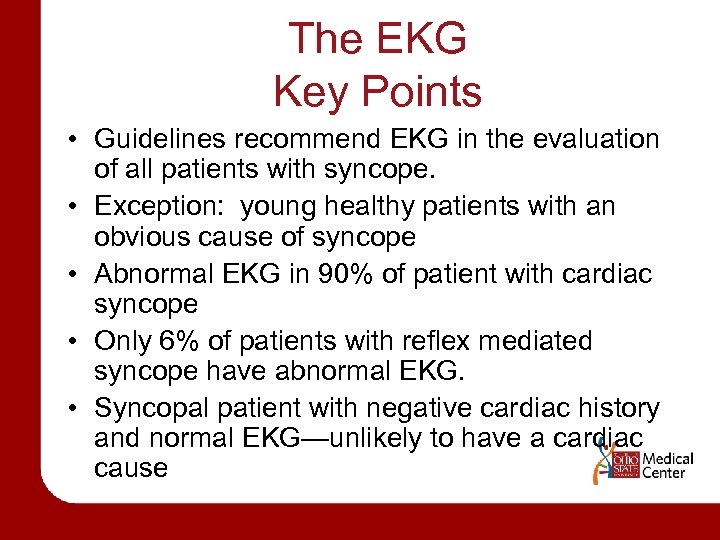
The EKG Key Points • Guidelines recommend EKG in the evaluation of all patients with syncope. • Exception: young healthy patients with an obvious cause of syncope • Abnormal EKG in 90% of patient with cardiac syncope • Only 6% of patients with reflex mediated syncope have abnormal EKG. • Syncopal patient with negative cardiac history and normal EKG—unlikely to have a cardiac cause
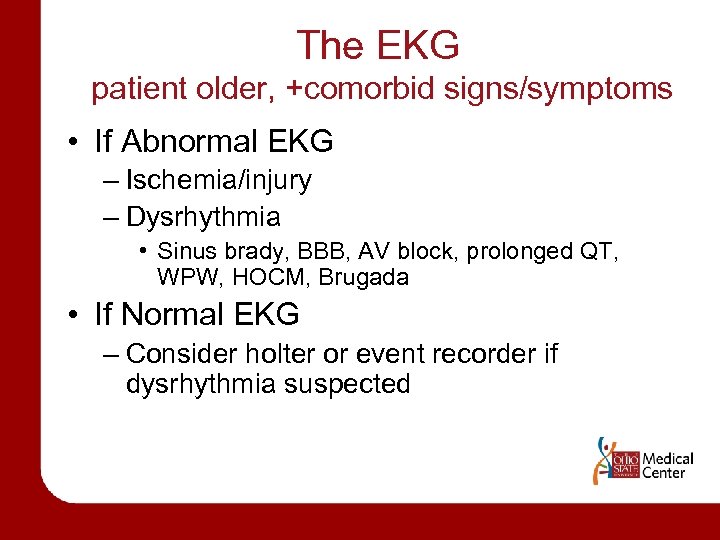
The EKG patient older, +comorbid signs/symptoms • If Abnormal EKG – Ischemia/injury – Dysrhythmia • Sinus brady, BBB, AV block, prolonged QT, WPW, HOCM, Brugada • If Normal EKG – Consider holter or event recorder if dysrhythmia suspected
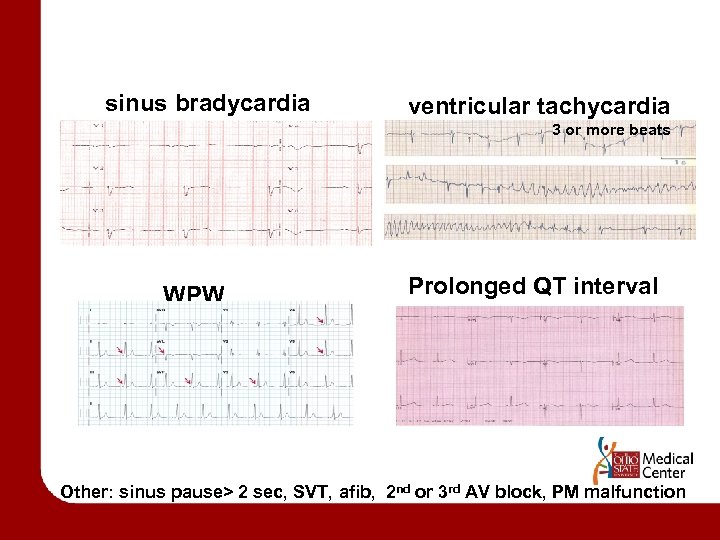
sinus bradycardia ventricular tachycardia 3 or more beats WPW Prolonged QT interval Other: sinus pause> 2 sec, SVT, afib, 2 nd or 3 rd AV block, PM malfunction
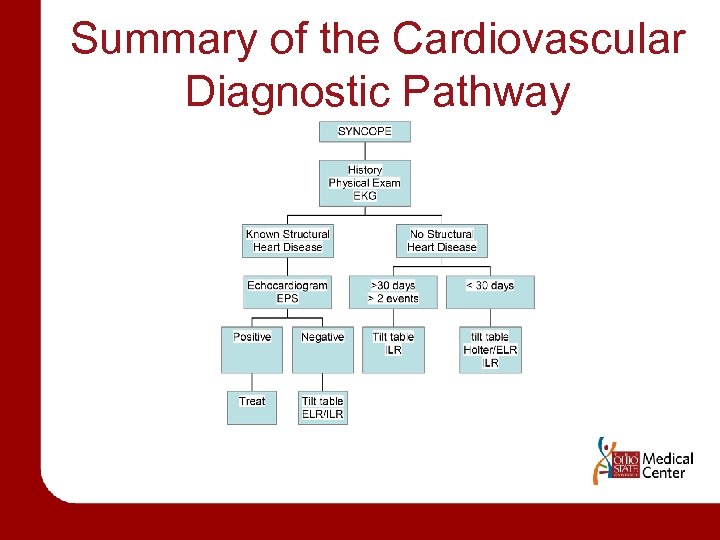
Summary of the Cardiovascular Diagnostic Pathway
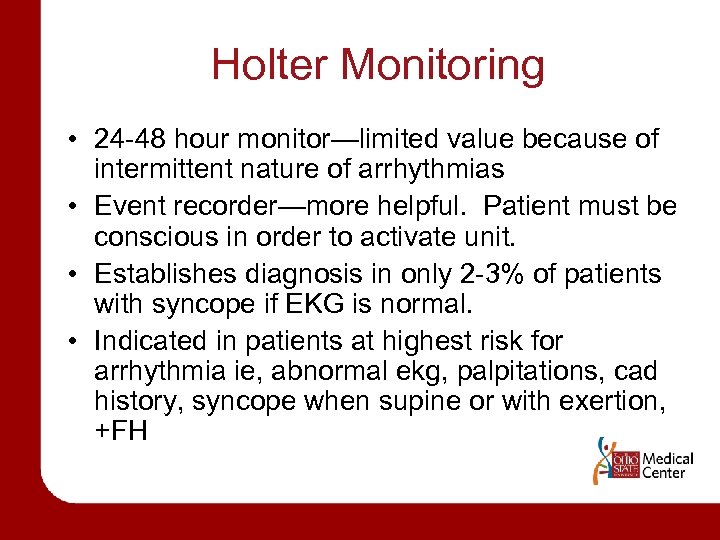
Holter Monitoring • 24 -48 hour monitor—limited value because of intermittent nature of arrhythmias • Event recorder—more helpful. Patient must be conscious in order to activate unit. • Establishes diagnosis in only 2 -3% of patients with syncope if EKG is normal. • Indicated in patients at highest risk for arrhythmia ie, abnormal ekg, palpitations, cad history, syncope when supine or with exertion, +FH
Holter results--summary • PACs and PVCs – Usually not significant – Exception: ie 3 consecutive 3 PVCs at 100 bpm • Bigeminy—may be significant • AV block---is important • Bradycardia---if signs and symptoms correlate
Loop Event Recorders • Provides longer monitoring—weeks to months • Can activate the monitor after symptoms occur, thereby freezing in its memory the readings from the previous 2 -5 minutes and the subsequent 1 minute • In patients with recurrent syncope, arrhythmias were found during symptoms in 8 -20%. • Limitations: compliance, use of device, transmission
ECHOCARDIOGRAM • Access structural causes of cardiac syncope – AS, MS, HOCM, atrial myoxoma • Unlikely to be helpful in the absence of known cardiac disease or an abnormal ekg. • INDICATIONS – Abnormal EKG – Murmur ---history of heart disease ---exercise assoc. syncope
Structural Heart Disease • Aortic Stenosis – Most common structural lesion associated with syncope in the elderly • Hypertrophic Obstructive Cardiomyopathy – Vasodilatation (drugs/hot bath) can induce syncope • Obstruction to Right Ventricular Outflow – PE, pulmonary stenosis, pulmonary htn
EXERCISE STRESS TEST • Syncope during exercise is more likely to be related to an arrhythmia • Post-exertional syncope is usually neurally mediated. • Echocardiogram should be done prior to EST to r/o structural abnormality. • INDICATION – Syncope during or shortly after exercise (exertional syncope)
EPS—Intracardiac EPS • Rarely indicated in • Difficult to correlate patients with structurally spontaneous events and normal hearts and laboratory findings normal ekg. • Ineffective for assessing • Diagnostic yield greatest bradyarrhythmias in patients with known • Often must settle for an heart disease but nonattributable cause diagnostic ekg monitoring. • Abnormal finding on EPS • Heart disease-------5080% • No heart disease---1850% does not guarantee that this was what caused the patient’s syncope. • EPS is abnormal in 1868% of patients with syncope of unknown cause.
EP testing—Useful Diagnostic findings • Inducible monomorphic VT • Sinus node response time > 3000 ms or carotid sinus response time >600 ms • Inducible SVT with hypotension • HV interval > 100 ms (especially in absence of inducible VT) • Pacing induced infra-nodal block
TILT TABLE TEST • Changes in position to reproduce symptoms of the syncopal event. • Positive tilt table test – Induction of bradycardia and hypotension – Considered diagnostic for vasovagal syncope
Indications for Tilt table test • Unexplained recurrent syncope or syncope associated with injury in absence of structural heart ds. • Unexplained recurrent syncope or syncope associated with injury in setting of organic heart disease after exclusion of potential cardiac cause of syncope • Identification of neurally mediated syncope could alter treatment • Evaluation of recurrent unexplained falls. • Evaluation of near syncope or dizziness
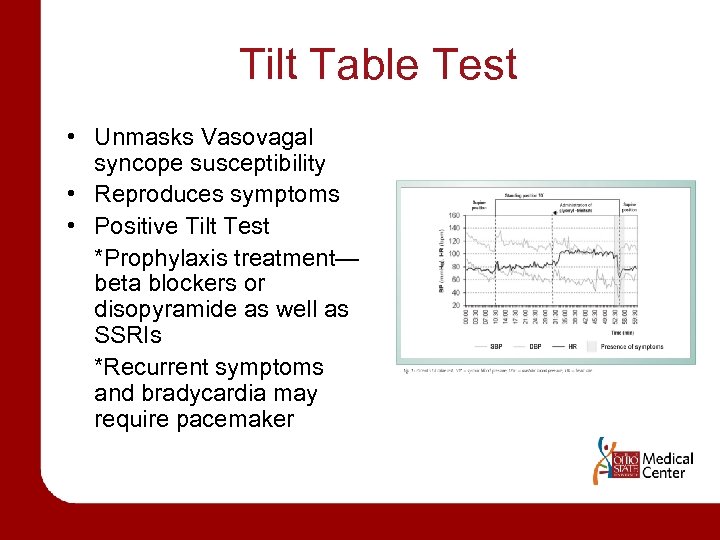
Tilt Table Test • Unmasks Vasovagal syncope susceptibility • Reproduces symptoms • Positive Tilt Test *Prophylaxis treatment— beta blockers or disopyramide as well as SSRIs *Recurrent symptoms and bradycardia may require pacemaker
NEUROLOGIC TESTING • Tend to be overused • Includes EEG, CT head, MRI head, Carotid dopplers • In contrast, Cardiovascular tests are underused. • INDICATION – Only if history and physical exam suggests a neurologic cause or testing for other causes is complete.
EEG • Not a first line of testing • To differentiate syncope from seizure • Abnormal EEG in the interval between two attacks -> Epilepsy • Normal EEG -> does not tell us anything
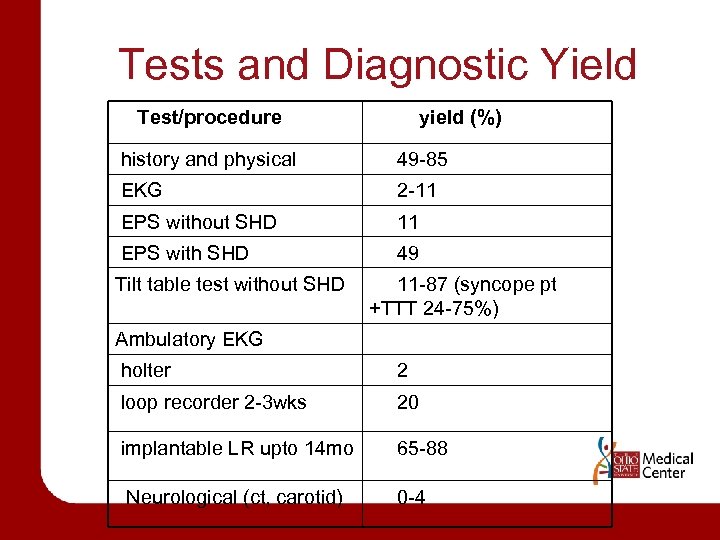
Tests and Diagnostic Yield Test/procedure yield (%) history and physical 49 -85 EKG 2 -11 EPS without SHD 11 EPS with SHD 49 Tilt table test without SHD 11 -87 (syncope pt +TTT 24 -75%) Ambulatory EKG holter 2 loop recorder 2 -3 wks 20 implantable LR upto 14 mo 65 -88 Neurological (ct, carotid) 0 -4
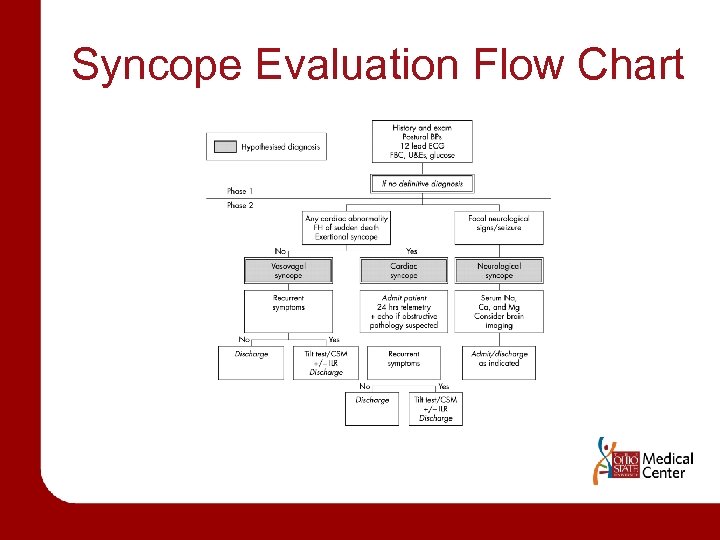
Syncope Evaluation Flow Chart
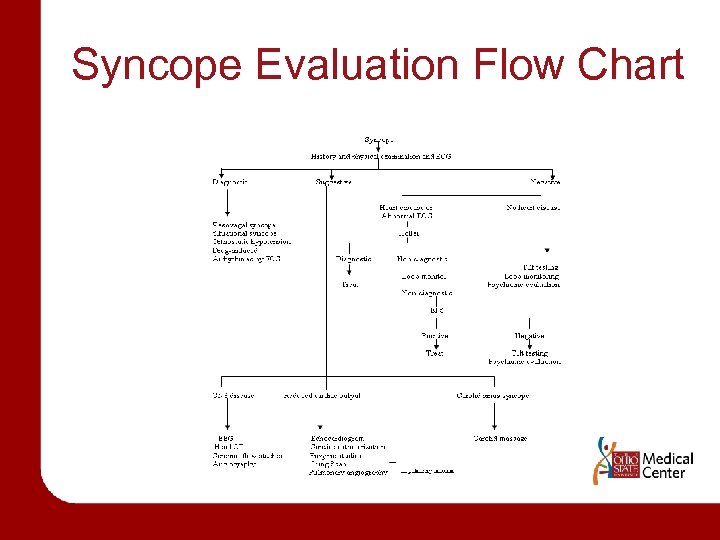
Syncope Evaluation Flow Chart
When to Admit • Consider admitting if age greater than 40 years • Discharge if benign etiology – Vasovagal, micturition, psychogenic syncope • Admit if – Suspected or known significant heart disease ie cardiac ischemia, CHF, structural heart ds or +family hx of SCD – EKG suggestive of arrhythmia or syncope during exercise – Stroke – Syncope causing severe injury – Severe orthostatic hypotension ACEP guidelines
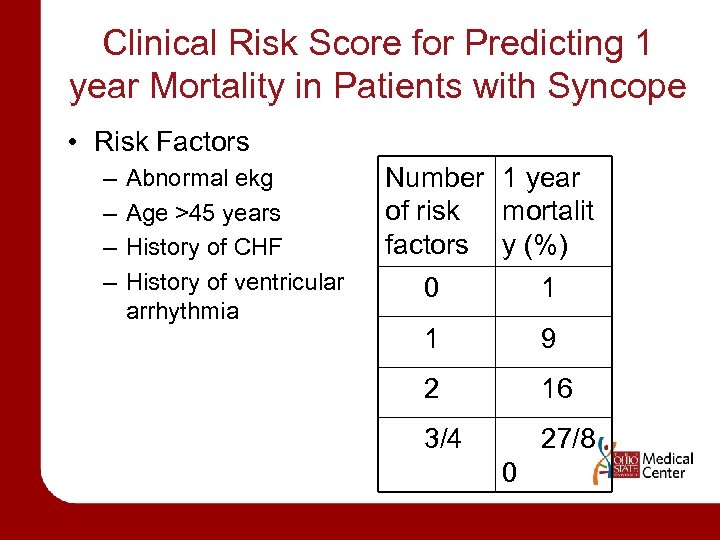
Clinical Risk Score for Predicting 1 year Mortality in Patients with Syncope • Risk Factors – – Abnormal ekg Age >45 years History of CHF History of ventricular arrhythmia Number 1 year of risk mortalit factors y (%) 0 1 1 9 2 16 3/4 27/8 0
Congestive Heart Failure • CHF = poor outcome – N=491; 12% with syncope – Cardiac syncope; 49% dead 1 year – Noncardiac syncope; 39% dead 1 year – No syncope; 12% dead 1 year *CHF is a risk factor for poor outcome in multiple studies
San Francisco Syncope Rule • Risk Factors – – – C H E S S History of CHF Hematocrit less than 30 Non-sinus rhythm or new changes in EKG Systolic BP less than 90 Shortness of breath • Predicting Serious Outcome (at 7 days) – Low risk (no risk factor)---0. 3% serious outcome – High risk (1+risk factor)---15. 2% serious outcome
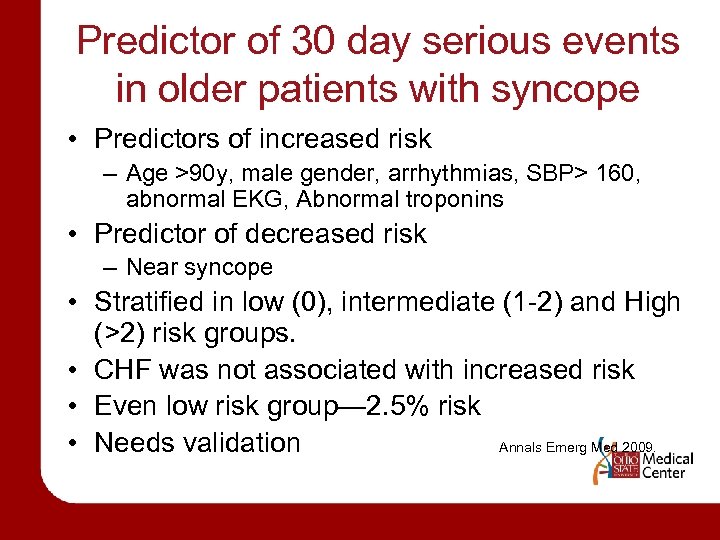
Predictor of 30 day serious events in older patients with syncope • Predictors of increased risk – Age >90 y, male gender, arrhythmias, SBP> 160, abnormal EKG, Abnormal troponins • Predictor of decreased risk – Near syncope • Stratified in low (0), intermediate (1 -2) and High (>2) risk groups. • CHF was not associated with increased risk • Even low risk group— 2. 5% risk • Needs validation Annals Emerg Med 2009.
Driving and Return to Work • Vasovagal syncope---can return to work • VT---no driving for 3 -6 months • In Ohio, can not be a Commercial Driver if diagnosed with syncope
Case #1 Continues • • • Physical exam: Normal Orthostatics: Normal EKG: Normal Labs: no anemia. Glucose normal. ECHO: Normal Tilt Table Test: after 7 minutes of 70 degrees upright, HR 36, BP 51/41, LOC. Regained consciousness with supine position.
Case #1 Conclusion • DIAGNOSIS----Vasovagal Syncope • TREATMENT---Florinef, Ted hose, Fluids • OUTCOME---No reoccurence of symptoms when followed up at 3 months, 6 months, and 1 year later.
Case #2 Continues • Emergency Room workup—negative. Electrolytes, CBC normal. EKG showed NSR with occasional PVCs. • Decision made to ADMIT. • 2 hours later---Nonsustained Vtach. • EP study—Inducible Vtach. Automated internal defibrillator placed. • Cardiac cath---diffuse coronary artery disease.
SUMMARY • Syncope is a transient loss of consciousness due to decreased cerebral blood flow. • Most common causes: vasovagal, cardiac (cardiac arrhythmia), and orthostatic hypotension. Seizures are rare. • Patients with cardiac syncope are at increased risk of death. • History and Physical exam are the MOST important to identify the cause • Orthostatic BPs should be done on all pts.
SUMMARY • • Shotgun approach is Not helpful. EKG should be considered in all patients. Tilt table test can diagnosis vasovagal syncope. Neurologic testing is low yield and often overused. • Holter monitoring, Echo, EST, EP considered in patients at high risk for cardiac syncope. • Patients remain undiagnosed in 34% of cases.
Clues to the Etiology of Syncope • Cough, micturition, defecation, swallowing--situational syncope • Syncope with arm exercise---subclavian steal • Syncope with shaving---carotid sinus syncope • Syncope with change of position---orthostatic • Prodromal symptoms (nausea, diaphoresis)--neurally mediated reflex (vasovagal)
Clues to the Etiology of Syncope • Syncope with exertion---AS, IHSS, arrhythmias • Abrupt onset---cardiac syncope • Blood pressure/pulse differential---Aortic dissection, subclavian steal syndrome • Post-syncopal disorientation; incontinence--seizure
REFERENCES • Engel. Ann Internal Med. 1978. 89; 403412 • Kapor, W. Medicine. 1990. 69; 160 -175. • Krahn. Cardiology Clinic. 1997 • ACEP Clinical Policy on Syncope. • Ann Emerg Med. 2009. • Mayo Clinic Proceedings. Nov 2008.
c85985fa904e75b8ab5713cca17eb8ec.ppt