466545c1138ea3f8d3120ca6e384a399.ppt
- Количество слайдов: 73
Sustainability and Building Quality into Systems Donald M. Berwick, MD, MPP Institute for Healthcare Improvement 1000 Lives Campaign Plenary Session 30 September 2009 Swansea, Wales
My Topics • • • Looking Backward – to 2007 The Current Environment A Global View Quality and Cost in the New Economy Where Next for Wales?

My 2007 Advice 1. Declare patient injuries an enemy, and establish patient safety as a shared goal. 2. Cease blame. Substitute science. 3. Assess where you are starting. 4. Collaborate with other nations to pursue “Shared Aims. ” 4
My 2007 Advice 5. Establish knowledge exchange, and increase peer-to-peer learning 6. Foster a community of expertise – Faculty for Quality Improvement and “Health Care Improvement Fellows” 7. Reconvene annually to review, reflect, learn and celebrate. 5
Today’s Environment • • Global Financial Crisis Dominant Concern about Health Care Costs Governments under Intense Scrutiny Restructuring 6

An International Movement of Movements?

The Entire UK Is Engaged 8
England • Cause – To make the safety of patients everyone’s highest priority • Aim – No avoidable death and no avoidable harm • Interventions – Leadership for safety – Reducing harm from deterioration – Reducing harm in critical care – Reducing harm in perioperative care – Reducing harm from high risk medicines
Scotland • 5. 5 million people • Scottish Patient Safety Programme – 37 acute hospitals Ø Critical care Ø Peri-op Ø Medicines Ø General ward Ø Leadership • Aims – 15% reduction in mortality – 30% reduction in adverse events
Denmark • • • 5. 5 million inhabitants Health care is a public task 5 regions that are responsible for health care Operation Life: • 38 hospital units – – – • Rapid Response Systems AMI Bundle Medication Reconciliation Ventilator Bundle Central Line Bundle Surviving Sepsis Campaign Aims – Save 3000 lives during campaign period ü All regions present at campaign start ü Cover 75% of discharges www. operationlife. dk 11

Canada • 33 million people • 10 interventions + 2 pilots • 1035 teams enrolled • 80% of acute care hospitals enrolled • All regional health organizations outside of Quebec enrolled Aim • Reduce adverse events by 40 -100% dependent upon intervention www. saferhealthcarenow. ca

Japan “PARTNERS for Patient Safety” National Campaign for Patient Safety in Japan http: //kyodokodo. jp/

Wales • 3 million people • 1000 Lives Campaign – All Hospitals, Primary Care and Ambulance services Ø Leadership Ø Critical Care/Rapid response Ø Medicines Ø Healthcare associated infection Ø Surgical care Ø General medical and surgical care • Aims – To save 1000 lives, and – Avoid 50, 000 cases of harm in 2 years from April 2008 www. 1000 livescampaign. wales. nhs. uk

Scottish Patient Safety Program
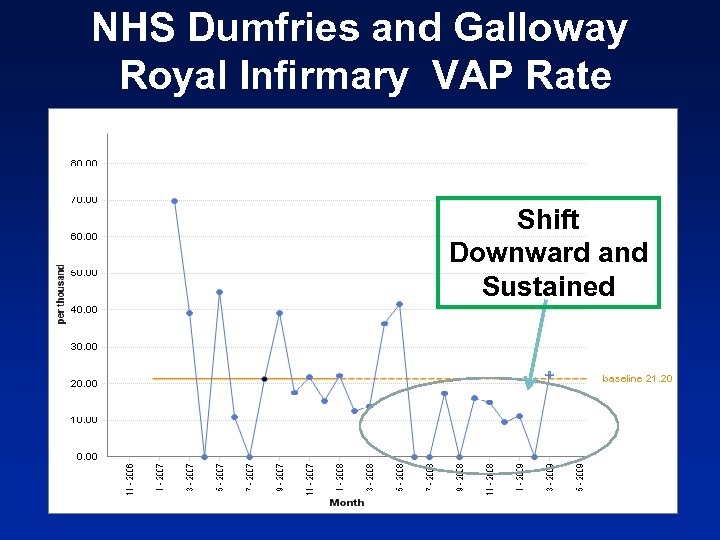
NHS Dumfries and Galloway Royal Infirmary VAP Rate Shift Downward and Sustained
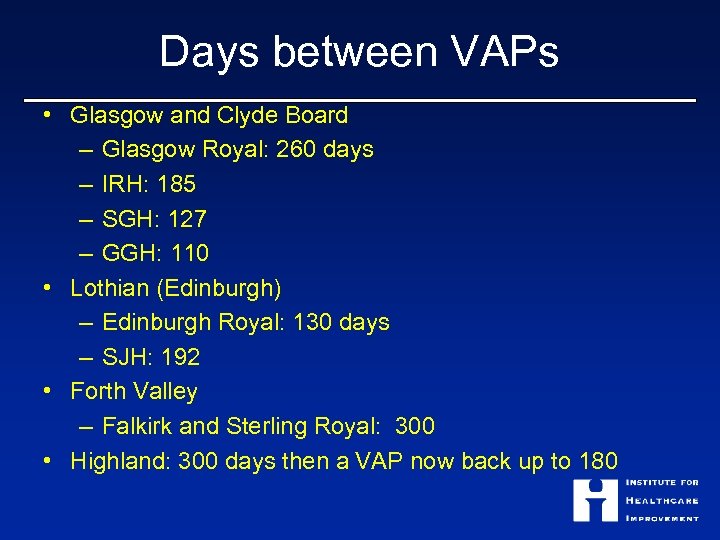
Days between VAPs • Glasgow and Clyde Board – Glasgow Royal: 260 days – IRH: 185 – SGH: 127 – GGH: 110 • Lothian (Edinburgh) – Edinburgh Royal: 130 days – SJH: 192 • Forth Valley – Falkirk and Sterling Royal: 300 • Highland: 300 days then a VAP now back up to 180
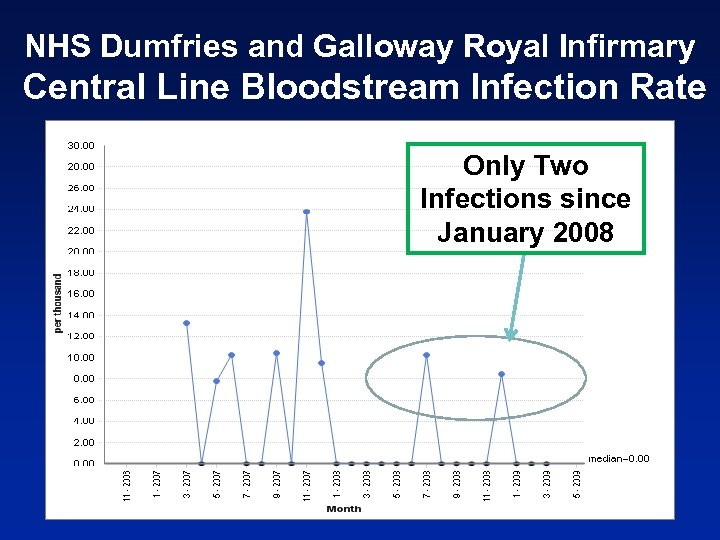
NHS Dumfries and Galloway Royal Infirmary Central Line Bloodstream Infection Rate Only Two Infections since January 2008
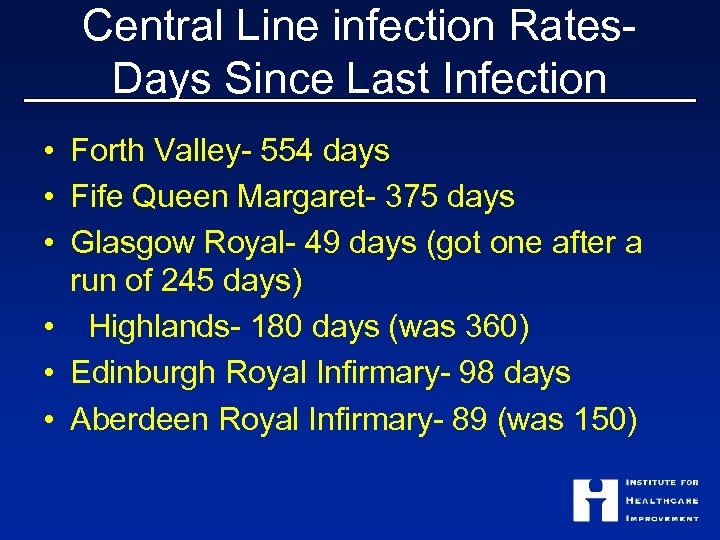
Central Line infection Rates- Days Since Last Infection • Forth Valley- 554 days • Fife Queen Margaret- 375 days • Glasgow Royal- 49 days (got one after a run of 245 days) • Highlands- 180 days (was 360) • Edinburgh Royal Infirmary- 98 days • Aberdeen Royal Infirmary- 89 (was 150)
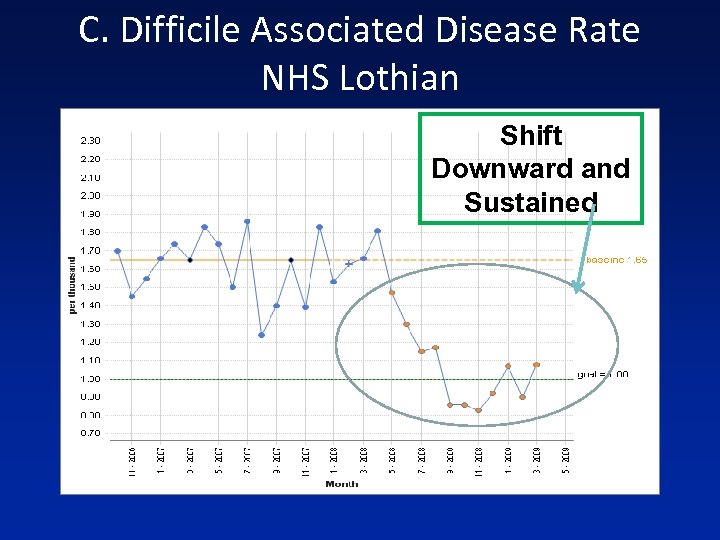
C. Difficile Associated Disease Rate NHS Lothian Shift Downward and Sustained

Quality and Cost Does Improvement Help?
IHI’s Work on Cost & Quality • Kano’s Three Levers • Triple Aim • “How Do They Do That? ” Project
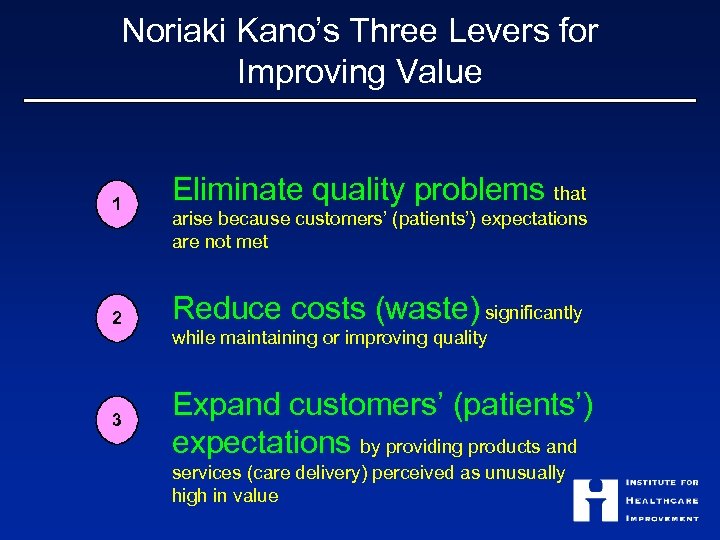
Noriaki Kano’s Three Levers for Improving Value 1 Eliminate quality problems that 2 Reduce costs (waste) significantly 3 arise because customers’ (patients’) expectations are not met while maintaining or improving quality Expand customers’ (patients’) expectations by providing products and services (care delivery) perceived as unusually high in value
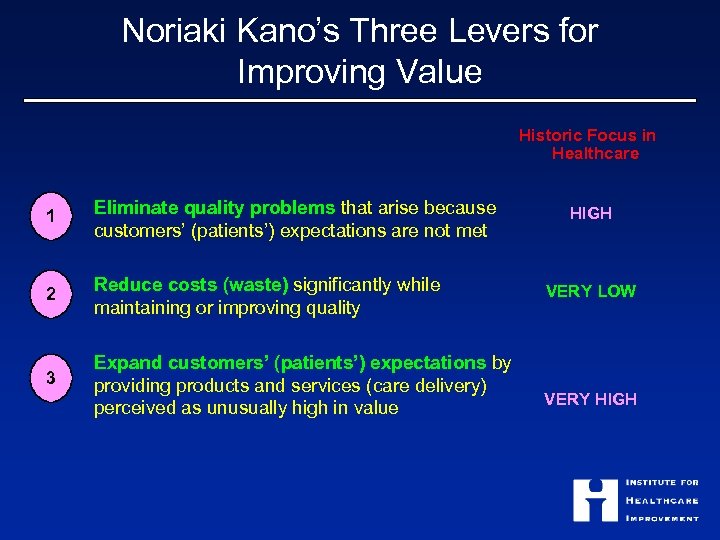
Noriaki Kano’s Three Levers for Improving Value Historic Focus in Healthcare 1 Eliminate quality problems that arise because customers’ (patients’) expectations are not met 2 Reduce costs (waste) significantly while maintaining or improving quality 3 Expand customers’ (patients’) expectations by providing products and services (care delivery) perceived as unusually high in value HIGH VERY LOW VERY HIGH
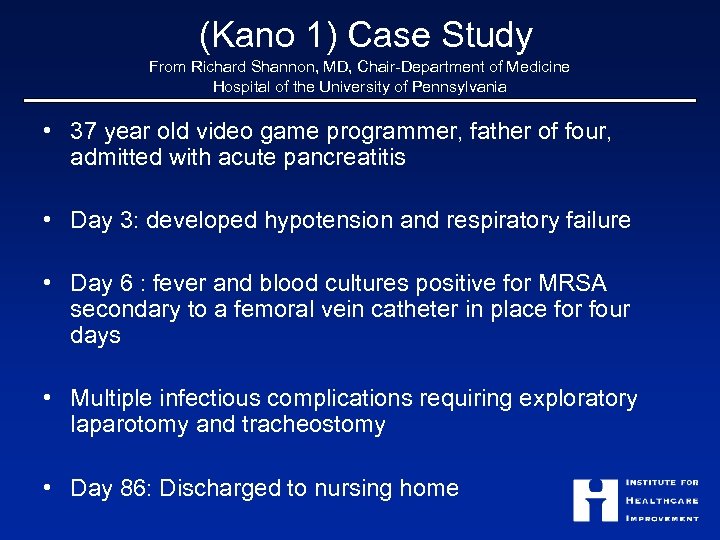
(Kano 1) Case Study From Richard Shannon, MD, Chair-Department of Medicine Hospital of the University of Pennsylvania • 37 year old video game programmer, father of four, admitted with acute pancreatitis • Day 3: developed hypotension and respiratory failure • Day 6 : fever and blood cultures positive for MRSA secondary to a femoral vein catheter in place for four days • Multiple infectious complications requiring exploratory laparotomy and tracheostomy • Day 86: Discharged to nursing home
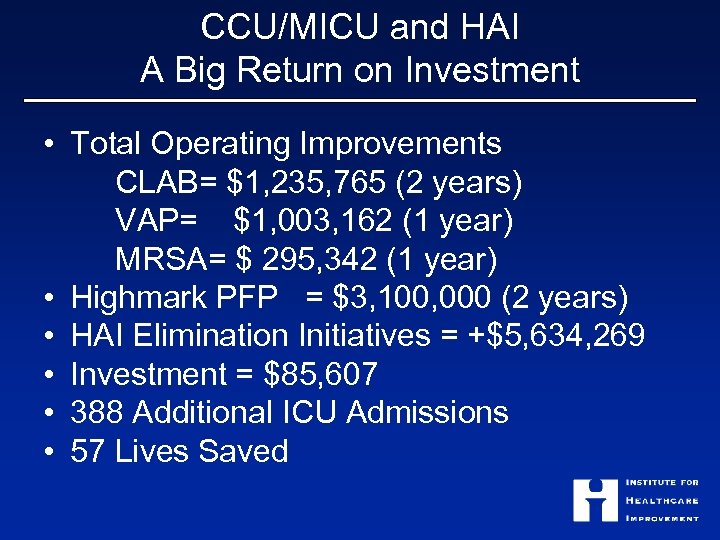
CCU/MICU and HAI A Big Return on Investment • Total Operating Improvements CLAB= $1, 235, 765 (2 years) VAP= $1, 003, 162 (1 year) MRSA= $ 295, 342 (1 year) • Highmark PFP = $3, 100, 000 (2 years) • HAI Elimination Initiatives = +$5, 634, 269 • Investment = $85, 607 • 388 Additional ICU Admissions • 57 Lives Saved
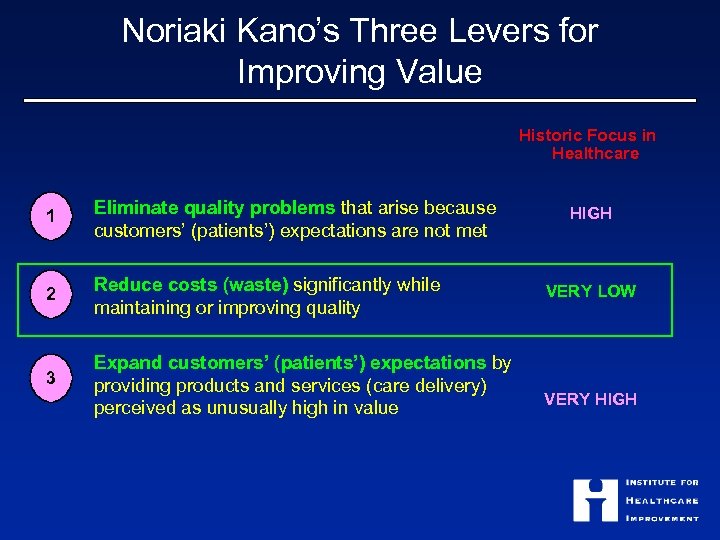
Noriaki Kano’s Three Levers for Improving Value Historic Focus in Healthcare 1 Eliminate quality problems that arise because customers’ (patients’) expectations are not met 2 Reduce costs (waste) significantly while maintaining or improving quality 3 Expand customers’ (patients’) expectations by providing products and services (care delivery) perceived as unusually high in value HIGH VERY LOW VERY HIGH
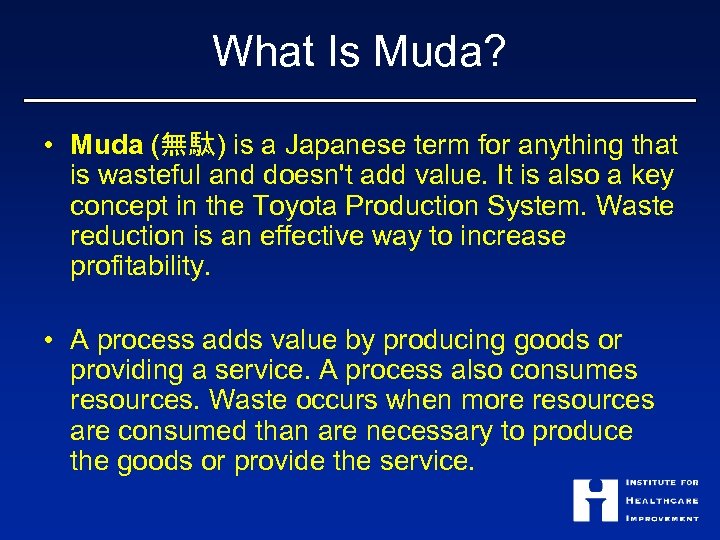
What Is Muda? • Muda (無駄) is a Japanese term for anything that is wasteful and doesn't add value. It is also a key concept in the Toyota Production System. Waste reduction is an effective way to increase profitability. • A process adds value by producing goods or providing a service. A process also consumes resources. Waste occurs when more resources are consumed than are necessary to produce the goods or provide the service.
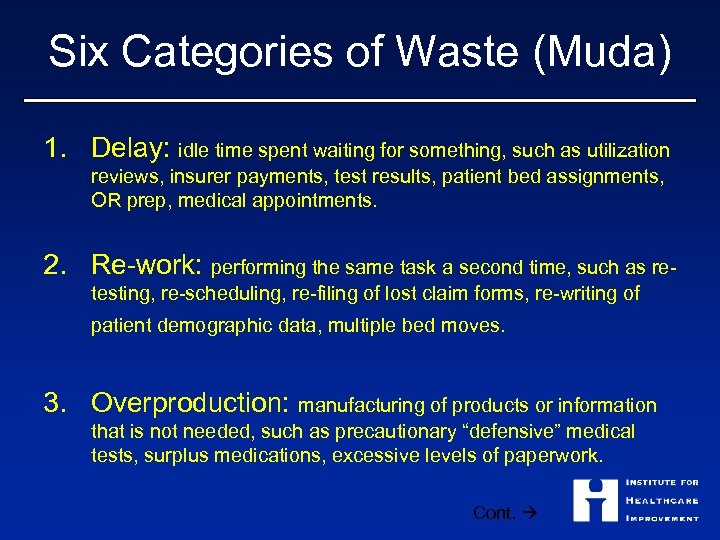
Six Categories of Waste (Muda) 1. Delay: idle time spent waiting for something, such as utilization reviews, insurer payments, test results, patient bed assignments, OR prep, medical appointments. 2. Re-work: performing the same task a second time, such as retesting, re-scheduling, re-filing of lost claim forms, re-writing of patient demographic data, multiple bed moves. 3. Overproduction: manufacturing of products or information that is not needed, such as precautionary “defensive” medical tests, surplus medications, excessive levels of paperwork. Cont.
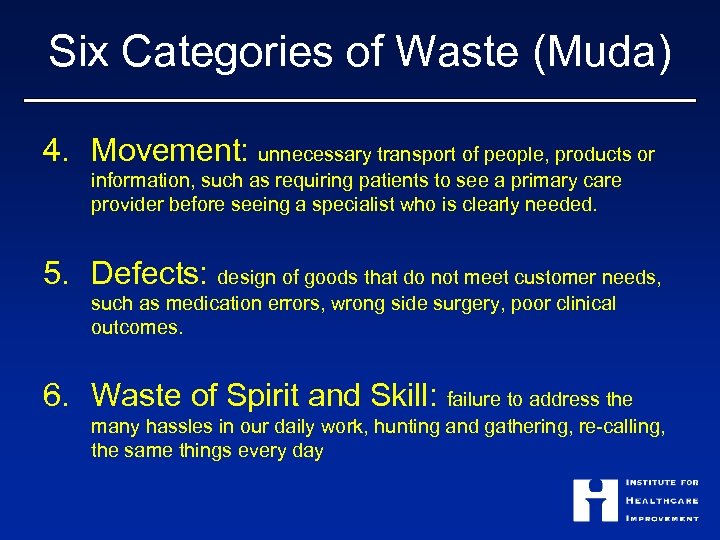
Six Categories of Waste (Muda) 4. Movement: unnecessary transport of people, products or information, such as requiring patients to see a primary care provider before seeing a specialist who is clearly needed. 5. Defects: design of goods that do not meet customer needs, such as medication errors, wrong side surgery, poor clinical outcomes. 6. Waste of Spirit and Skill: failure to address the many hassles in our daily work, hunting and gathering, re-calling, the same things every day
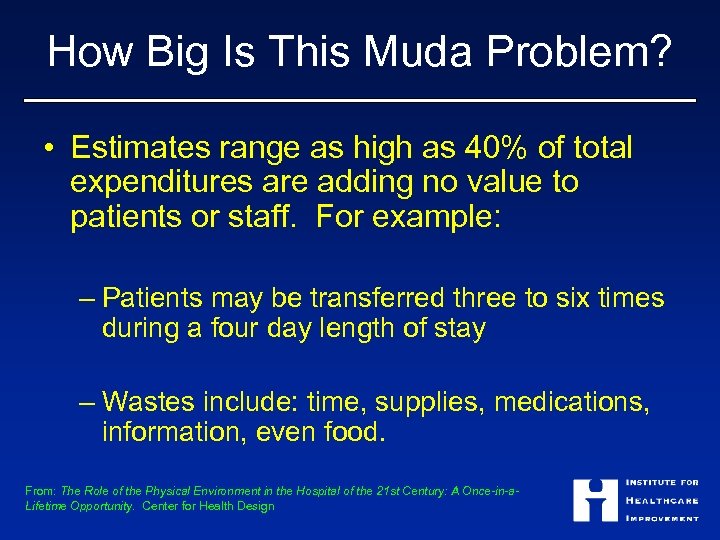
How Big Is This Muda Problem? • Estimates range as high as 40% of total expenditures are adding no value to patients or staff. For example: – Patients may be transferred three to six times during a four day length of stay – Wastes include: time, supplies, medications, information, even food. From: The Role of the Physical Environment in the Hospital of the 21 st Century: A Once-in-a. Lifetime Opportunity. Center for Health Design
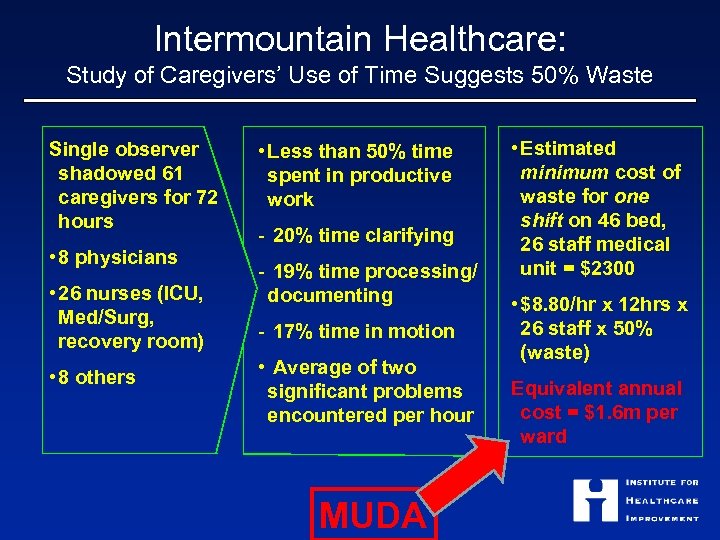
Intermountain Healthcare: Study of Caregivers’ Use of Time Suggests 50% Waste Single observer shadowed 61 caregivers for 72 hours • 8 physicians • 26 nurses (ICU, Med/Surg, recovery room) • 8 others • Less than 50% time spent in productive work - 20% time clarifying - 19% time processing/ documenting - 17% time in motion • Average of two significant problems encountered per hour MUDA • Estimated minimum cost of waste for one shift on 46 bed, 26 staff medical unit = $2300 • $8. 80/hr x 12 hrs x 26 staff x 50% (waste) Equivalent annual cost = $1. 6 m per ward
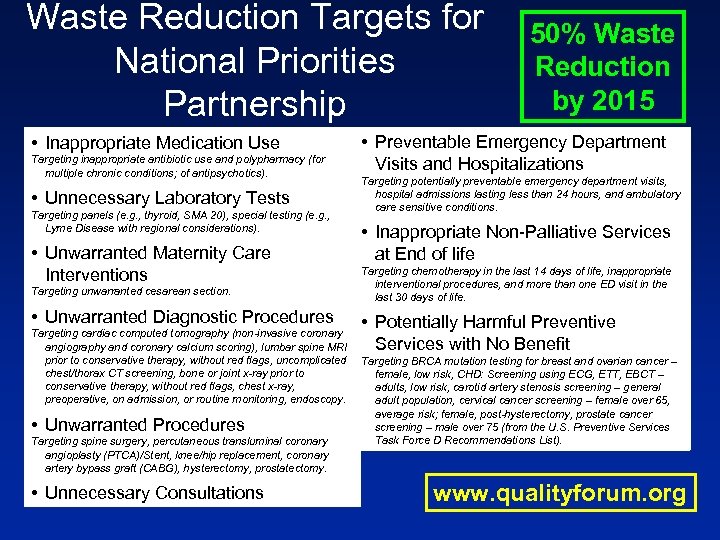
Waste Reduction Targets for National Priorities Partnership 50% Waste Reduction by 2015 *A partnership between the National Quality Forum and 28 other organizations • Preventable Emergency Department • Inappropriate Medication Use Targeting inappropriate antibiotic use and polypharmacy (for Visits and Hospitalizations multiple chronic conditions; of antipsychotics). • Unnecessary Laboratory Tests Targeting panels (e. g. , thyroid, SMA 20), special testing (e. g. , Lyme Disease with regional considerations). • Unwarranted Maternity Care Interventions Targeting unwarranted cesarean section. • Unwarranted Diagnostic Procedures Targeting cardiac computed tomography (non-invasive coronary angiography and coronary calcium scoring), lumbar spine MRI prior to conservative therapy, without red flags, uncomplicated chest/thorax CT screening, bone or joint x-ray prior to conservative therapy, without red flags, chest x-ray, preoperative, on admission, or routine monitoring, endoscopy. • Unwarranted Procedures Targeting spine surgery, percutaneous transluminal coronary angioplasty (PTCA)/Stent, knee/hip replacement, coronary artery bypass graft (CABG), hysterectomy, prostatectomy. • Unnecessary Consultations Targeting potentially preventable emergency department visits, hospital admissions lasting less than 24 hours, and ambulatory care sensitive conditions. • Inappropriate Non-Palliative Services at End of life Targeting chemotherapy in the last 14 days of life, inappropriate interventional procedures, and more than one ED visit in the last 30 days of life. • Potentially Harmful Preventive Services with No Benefit Targeting BRCA mutation testing for breast and ovarian cancer – female, low risk, CHD: Screening using ECG, ETT, EBCT – adults, low risk, carotid artery stenosis screening – general adult population, cervical cancer screening – female over 65, average risk; female, post-hysterectomy, prostate cancer screening – male over 75 (from the U. S. Preventive Services Task Force D Recommendations List). www. qualityforum. org
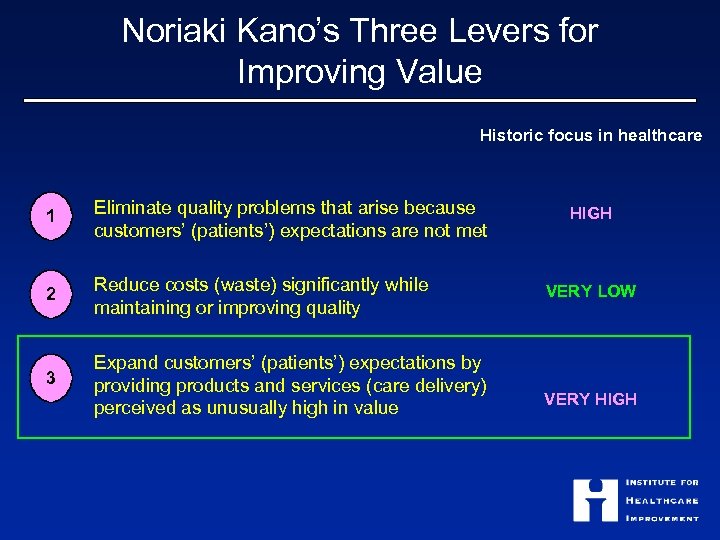
Noriaki Kano’s Three Levers for Improving Value Historic focus in healthcare 1 Eliminate quality problems that arise because customers’ (patients’) expectations are not met 2 Reduce costs (waste) significantly while maintaining or improving quality 3 Expand customers’ (patients’) expectations by providing products and services (care delivery) perceived as unusually high in value HIGH VERY LOW VERY HIGH
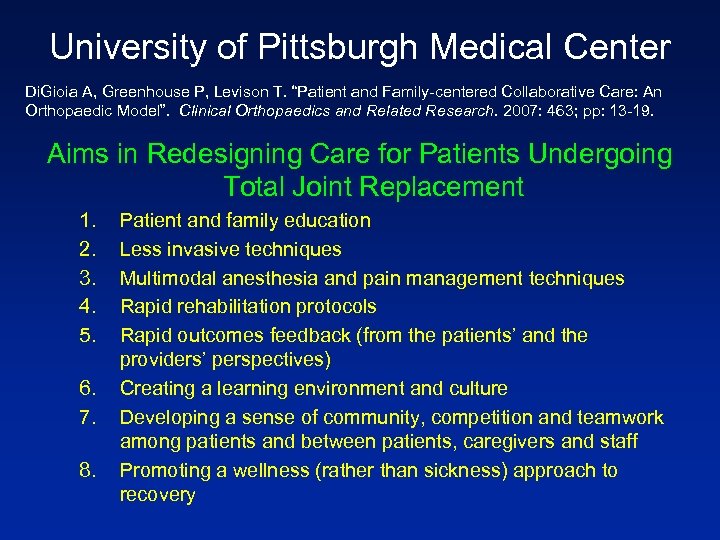
University of Pittsburgh Medical Center Di. Gioia A, Greenhouse P, Levison T. “Patient and Family-centered Collaborative Care: An Orthopaedic Model”. Clinical Orthopaedics and Related Research. 2007: 463; pp: 13 -19. Aims in Redesigning Care for Patients Undergoing Total Joint Replacement 1. 2. 3. 4. 5. 6. 7. 8. Patient and family education Less invasive techniques Multimodal anesthesia and pain management techniques Rapid rehabilitation protocols Rapid outcomes feedback (from the patients’ and the providers’ perspectives) Creating a learning environment and culture Developing a sense of community, competition and teamwork among patients and between patients, caregivers and staff Promoting a wellness (rather than sickness) approach to recovery
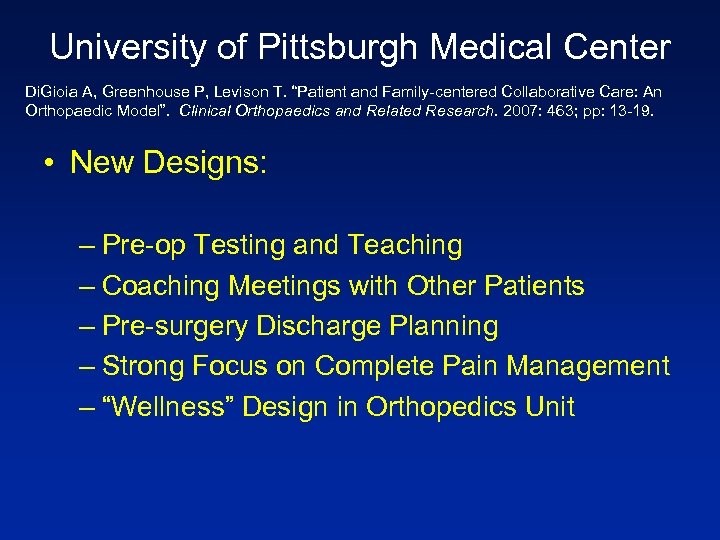
University of Pittsburgh Medical Center Di. Gioia A, Greenhouse P, Levison T. “Patient and Family-centered Collaborative Care: An Orthopaedic Model”. Clinical Orthopaedics and Related Research. 2007: 463; pp: 13 -19. • New Designs: – Pre-op Testing and Teaching – Coaching Meetings with Other Patients – Pre-surgery Discharge Planning – Strong Focus on Complete Pain Management – “Wellness” Design in Orthopedics Unit

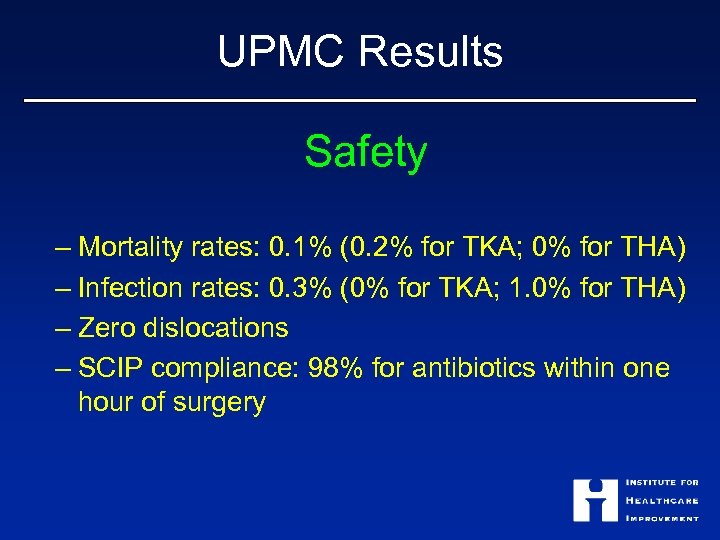
UPMC Results Safety – Mortality rates: 0. 1% (0. 2% for TKA; 0% for THA) – Infection rates: 0. 3% (0% for TKA; 1. 0% for THA) – Zero dislocations – SCIP compliance: 98% for antibiotics within one hour of surgery
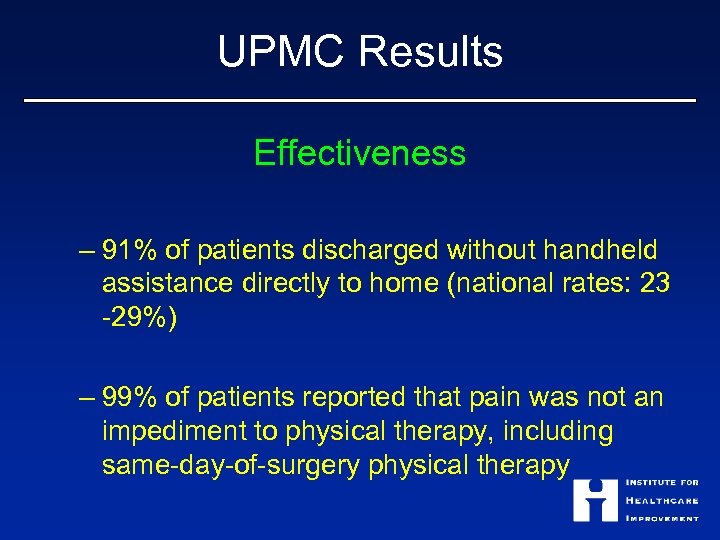
UPMC Results Effectiveness – 91% of patients discharged without handheld assistance directly to home (national rates: 23 -29%) – 99% of patients reported that pain was not an impediment to physical therapy, including same-day-of-surgery physical therapy
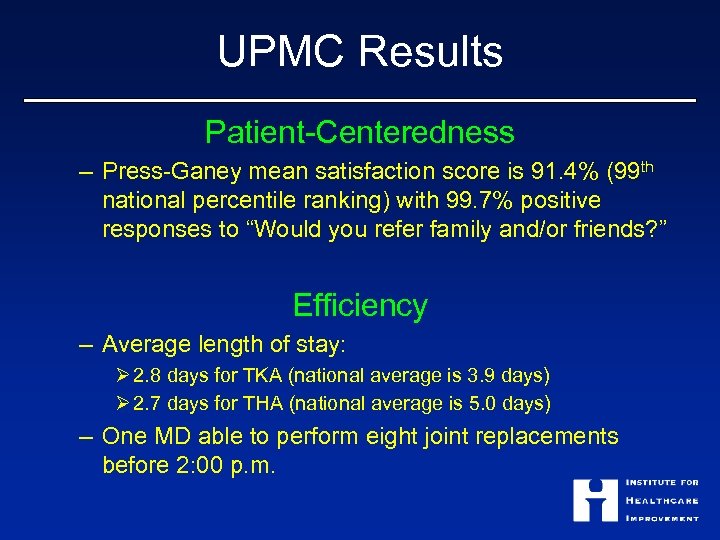
UPMC Results Patient-Centeredness – Press-Ganey mean satisfaction score is 91. 4% (99 th national percentile ranking) with 99. 7% positive responses to “Would you refer family and/or friends? ” Efficiency – Average length of stay: Ø 2. 8 days for TKA (national average is 3. 9 days) Ø 2. 7 days for THA (national average is 5. 0 days) – One MD able to perform eight joint replacements before 2: 00 p. m.

High Quality, Low Cost Care… IHI’s New Project… “How Do They Do That? ” – Identify High-Performing “Hospital Referral Regions” – Study the Dynamics of Their Health Economies
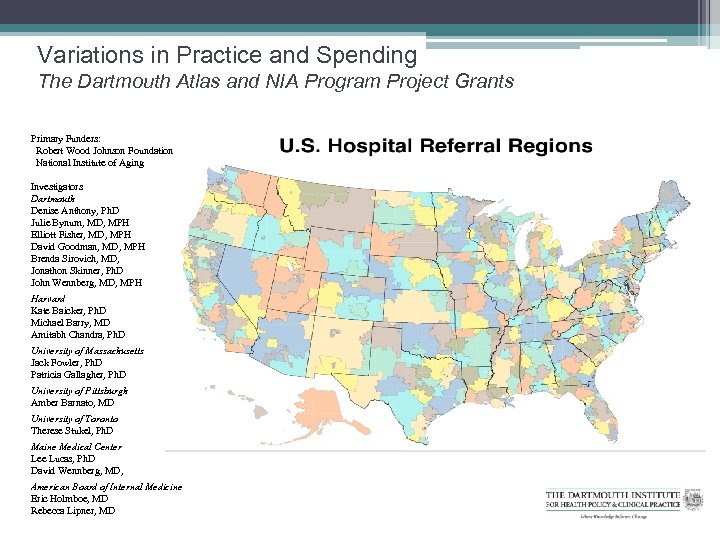
Variations in Practice and Spending The Dartmouth Atlas and NIA Program Project Grants Primary Funders: Robert Wood Johnson Foundation National Institute of Aging Investigators Dartmouth Denise Anthony, Ph. D Julie Bynum, MD, MPH Elliott Fisher, MD, MPH David Goodman, MD, MPH Brenda Sirovich, MD, Jonathon Skinner, Ph. D John Wennberg, MD, MPH Harvard Kate Baicker, Ph. D Michael Barry, MD Amitabh Chandra, Ph. D University of Massachusetts Jack Fowler, Ph. D Patricia Gallagher, Ph. D University of Pittsburgh Amber Barnato, MD University of Toronto Therese Stukel, Ph. D Maine Medical Center Lee Lucas, Ph. D David Wennberg, MD, American Board of Internal Medicine Eric Holmboe, MD Rebecca Lipner, MD
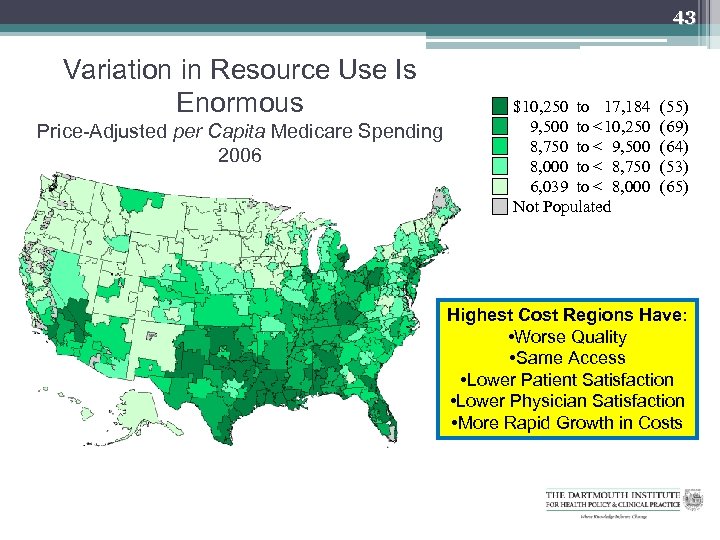
43 Variation in Resource Use Is Enormous Price-Adjusted per Capita Medicare Spending 2006 $10, 250 to 17, 184 9, 500 to < 10, 250 8, 750 to < 9, 500 8, 000 to < 8, 750 6, 039 to < 8, 000 Not Populated (55) (69) (64) (53) (65) Highest Cost Regions Have: • Worse Quality • Same Access • Lower Patient Satisfaction • Lower Physician Satisfaction • More Rapid Growth in Costs
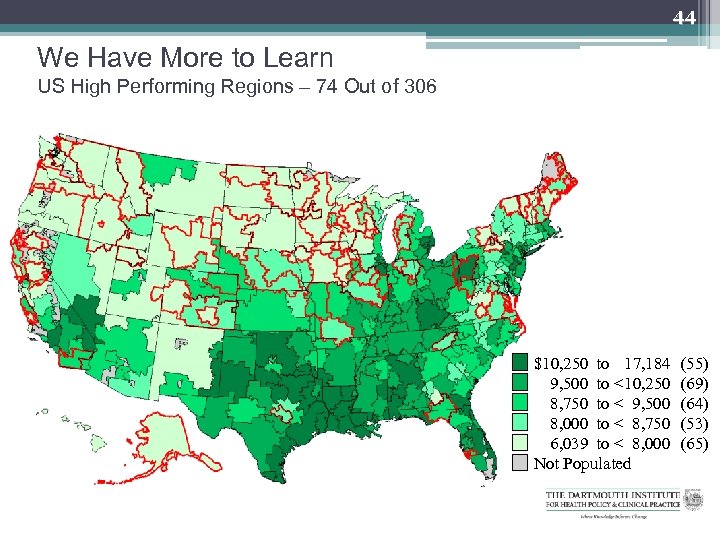
44 We Have More to Learn US High Performing Regions – 74 Out of 306 $10, 250 to 17, 184 9, 500 to < 10, 250 8, 750 to < 9, 500 8, 000 to < 8, 750 6, 039 to < 8, 000 Not Populated (55) (69) (64) (53) (65)
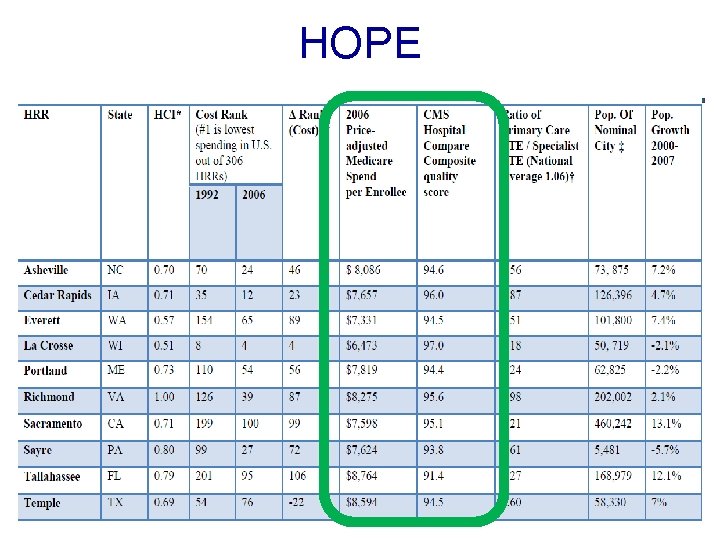
HOPE
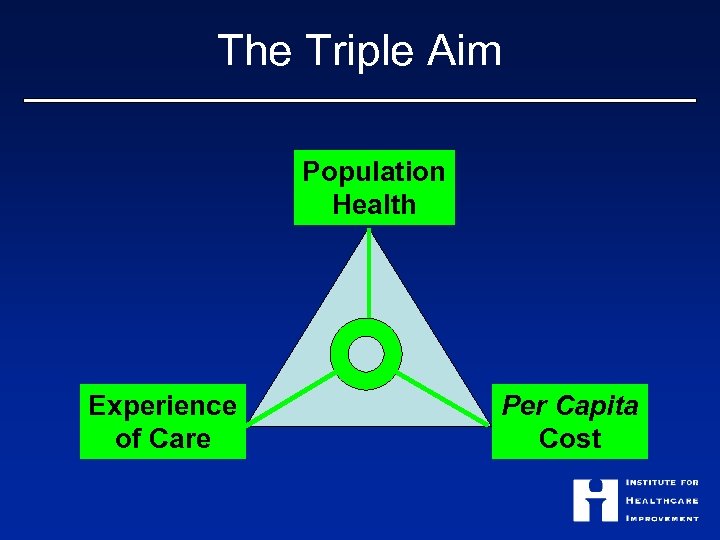
The Triple Aim Population Health Experience of Care Per Capita Cost
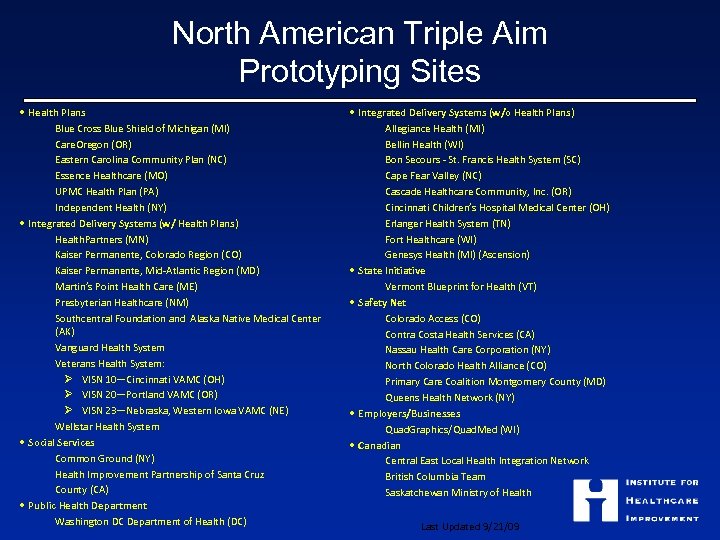
North American Triple Aim Prototyping Sites • Health Plans Blue Cross Blue Shield of Michigan (MI) Care. Oregon (OR) Eastern Carolina Community Plan (NC) Essence Healthcare (MO) UPMC Health Plan (PA) Independent Health (NY) • Integrated Delivery Systems (w/ Health Plans) Health. Partners (MN) Kaiser Permanente, Colorado Region (CO) Kaiser Permanente, Mid-Atlantic Region (MD) Martin’s Point Health Care (ME) Presbyterian Healthcare (NM) Southcentral Foundation and Alaska Native Medical Center (AK) Vanguard Health System Veterans Health System: Ø VISN 10—Cincinnati VAMC (OH) Ø VISN 20—Portland VAMC (OR) Ø VISN 23—Nebraska, Western Iowa VAMC (NE) Wellstar Health System • Social Services Common Ground (NY) Health Improvement Partnership of Santa Cruz County (CA) • Public Health Department Washington DC Department of Health (DC) • Integrated Delivery Systems (w/o Health Plans) Allegiance Health (MI) Bellin Health (WI) Bon Secours - St. Francis Health System (SC) Cape Fear Valley (NC) Cascade Healthcare Community, Inc. (OR) Cincinnati Children’s Hospital Medical Center (OH) Erlanger Health System (TN) Fort Healthcare (WI) Genesys Health (MI) (Ascension) • State Initiative Vermont Blueprint for Health (VT) • Safety Net Colorado Access (CO) Contra Costa Health Services (CA) Nassau Health Care Corporation (NY) North Colorado Health Alliance (CO) Primary Care Coalition Montgomery County (MD) Queens Health Network (NY) • Employers/Businesses Quad. Graphics/Quad. Med (WI) • Canadian Central East Local Health Integration Network British Columbia Team Saskatchewan Ministry of Health Last Updated 9/21/09
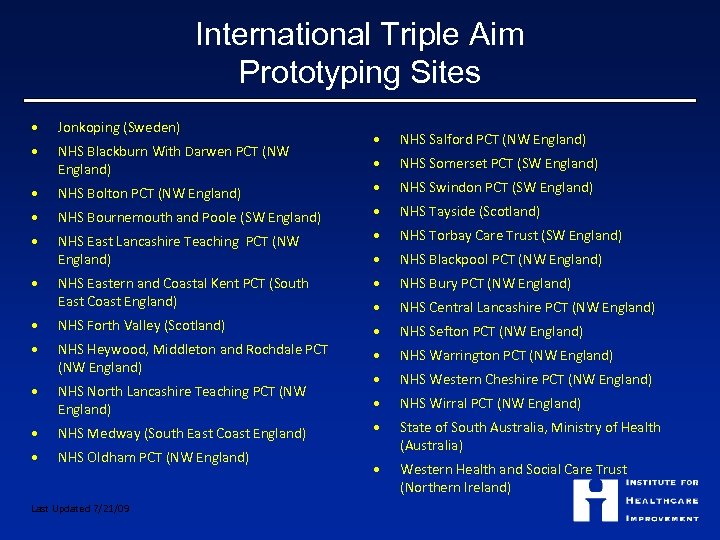
International Triple Aim Prototyping Sites • Jonkoping (Sweden) • NHS Blackburn With Darwen PCT (NW England) • NHS Bolton PCT (NW England) • • NHS Salford PCT (NW England) • NHS Somerset PCT (SW England) • NHS Swindon PCT (SW England) NHS Bournemouth and Poole (SW England) • NHS Tayside (Scotland) • NHS East Lancashire Teaching PCT (NW England) • NHS Torbay Care Trust (SW England) • NHS Blackpool PCT (NW England) • NHS Eastern and Coastal Kent PCT (South East Coast England) • NHS Bury PCT (NW England) • NHS Forth Valley (Scotland) • NHS Central Lancashire PCT (NW England) • NHS Heywood, Middleton and Rochdale PCT (NW England) • NHS Sefton PCT (NW England) • NHS Warrington PCT (NW England) • NHS North Lancashire Teaching PCT (NW England) • NHS Western Cheshire PCT (NW England) • NHS Wirral PCT (NW England) • NHS Medway (South East Coast England) • • NHS Oldham PCT (NW England) State of South Australia, Ministry of Health (Australia) • Western Health and Social Care Trust (Northern Ireland) Last Updated 7/21/09
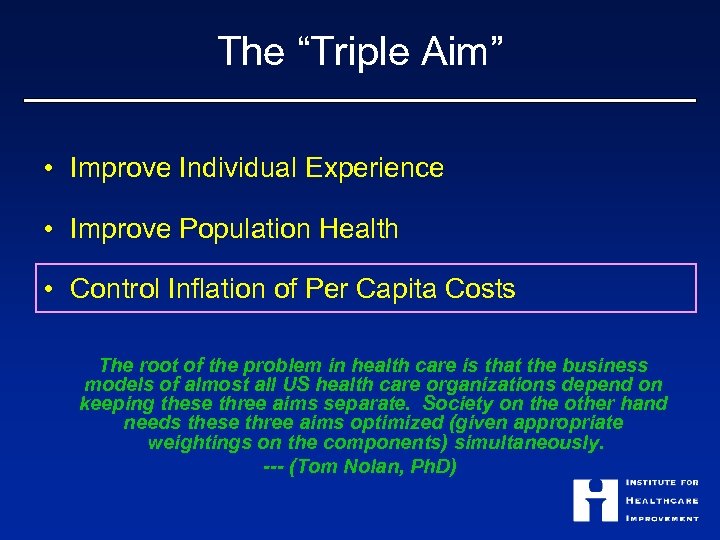
The “Triple Aim” • Improve Individual Experience • Improve Population Health • Control Inflation of Per Capita Costs The root of the problem in health care is that the business models of almost all US health care organizations depend on keeping these three aims separate. Society on the other hand needs these three aims optimized (given appropriate weightings on the components) simultaneously. --- (Tom Nolan, Ph. D)
So… Where Next for Wales? • “Constancy of Purpose for Improvement”
So… Where Next for Wales? • “Constancy of Purpose for Improvement” • Linkage of Improvement of Care to Sustainable Cost – A Focus on “Muda”
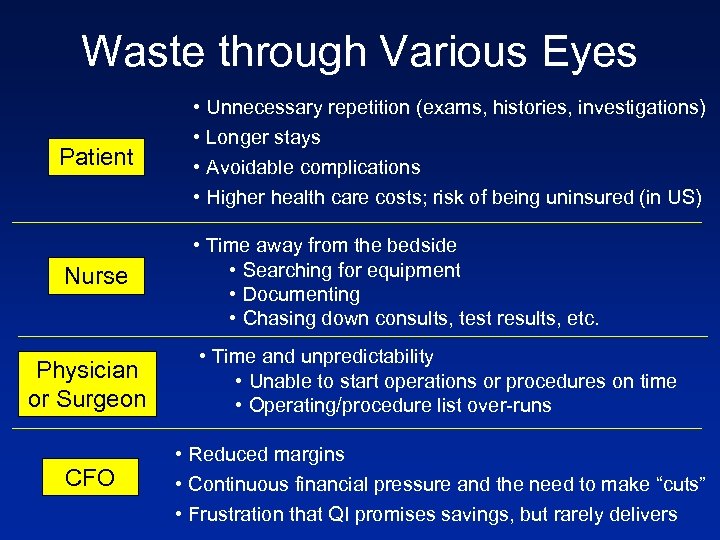
Waste through Various Eyes Patient • Unnecessary repetition (exams, histories, investigations) • Longer stays • Avoidable complications • Higher health care costs; risk of being uninsured (in US) Nurse • Time away from the bedside • Searching for equipment • Documenting • Chasing down consults, test results, etc. Physician or Surgeon • Time and unpredictability • Unable to start operations or procedures on time • Operating/procedure list over-runs CFO • Reduced margins • Continuous financial pressure and the need to make “cuts” • Frustration that QI promises savings, but rarely delivers
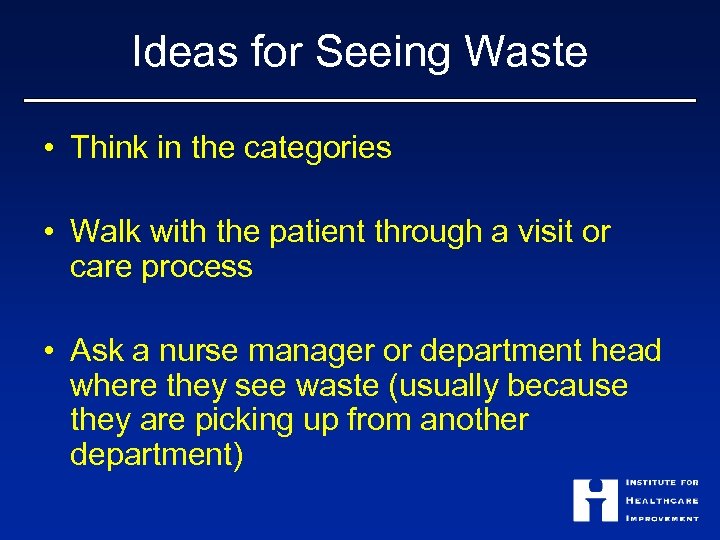
Ideas for Seeing Waste • Think in the categories • Walk with the patient through a visit or care process • Ask a nurse manager or department head where they see waste (usually because they are picking up from another department)
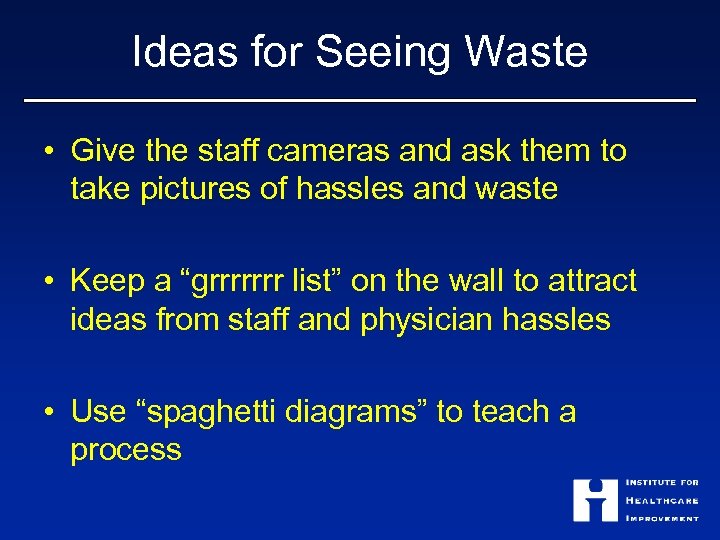
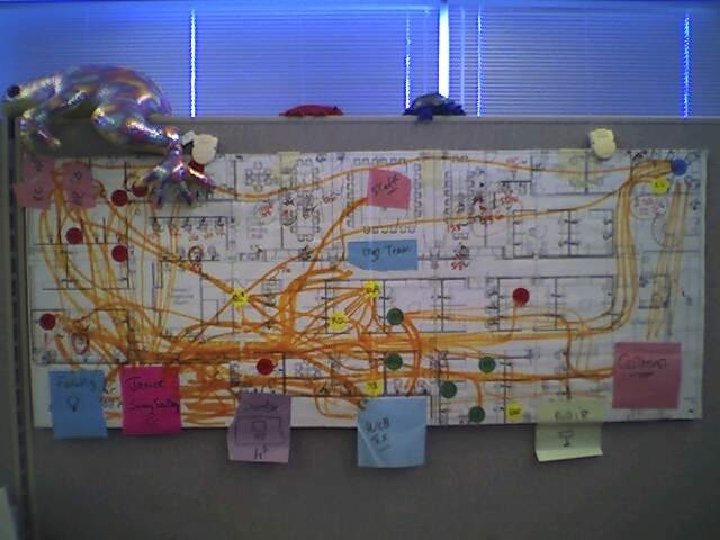
Ideas for Seeing Waste • Give the staff cameras and ask them to take pictures of hassles and waste • Keep a “grrrrrrr list” on the wall to attract ideas from staff and physician hassles • Use “spaghetti diagrams” to teach a process
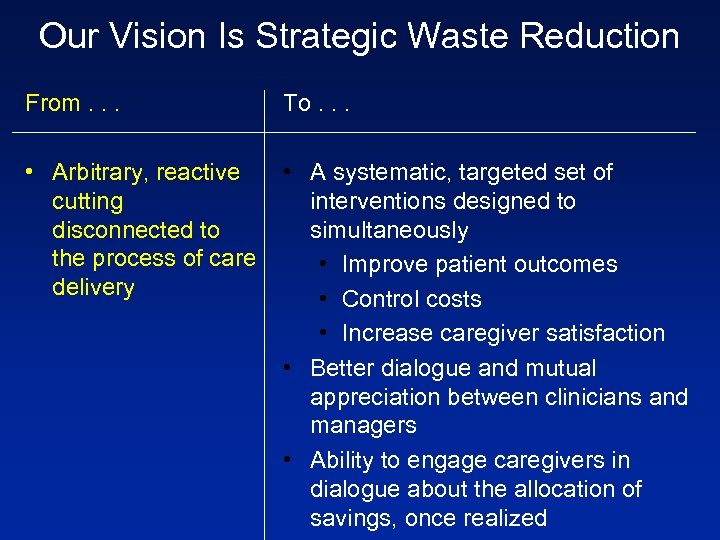
Our Vision Is Strategic Waste Reduction From. . . To. . . • Arbitrary, reactive • A systematic, targeted set of interventions designed to cutting simultaneously disconnected to the process of care • Improve patient outcomes delivery • Control costs • Increase caregiver satisfaction • Better dialogue and mutual appreciation between clinicians and managers • Ability to engage caregivers in dialogue about the allocation of savings, once realized

The NHS Institute…. . Is 4 years old …. . supports the NHS to transform healthcare for patients and the public by rapidly developing and spreading new ways of working, new technology and world class leadership. …. . Believes that success in improvement and innovation requires attention to Leadership, Measurement, Tools and Techniques and Relationships
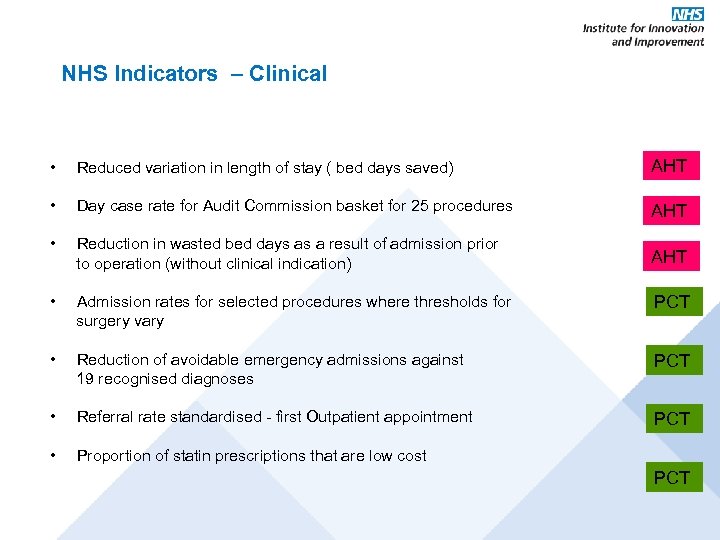
NHS Indicators – Clinical • Reduced variation in length of stay ( bed days saved) AHT • Day case rate for Audit Commission basket for 25 procedures AHT • Reduction in wasted bed days as a result of admission prior to operation (without clinical indication) AHT • Admission rates for selected procedures where thresholds for surgery vary PCT • Reduction of avoidable emergency admissions against 19 recognised diagnoses PCT • Referral rate standardised - first Outpatient appointment PCT • Proportion of statin prescriptions that are low cost PCT
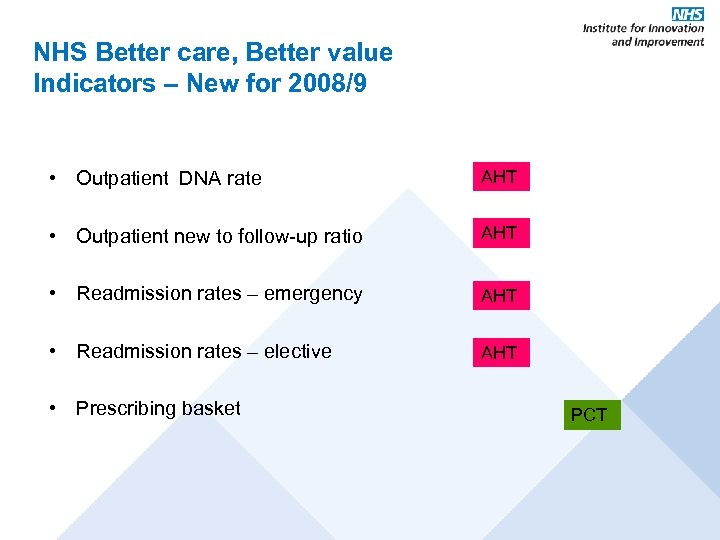
NHS Better care, Better value Indicators – New for 2008/9 • Outpatient DNA rate AHT • Outpatient new to follow-up ratio AHT • Readmission rates – emergency AHT • Readmission rates – elective AHT • Prescribing basket PCT
Typical Results Time on direct patient care from 25 -30% to 45 -50% Impact on Patient experience; Lo. S; Hospital acquired infection; Pressure area care; Meal wastage; Inventory use…… Impact on morale; on sickness absence…… Impact on “self efficacy”…. “No going back” “Not a project; a way of life” “Everyday feels like a Sunday”
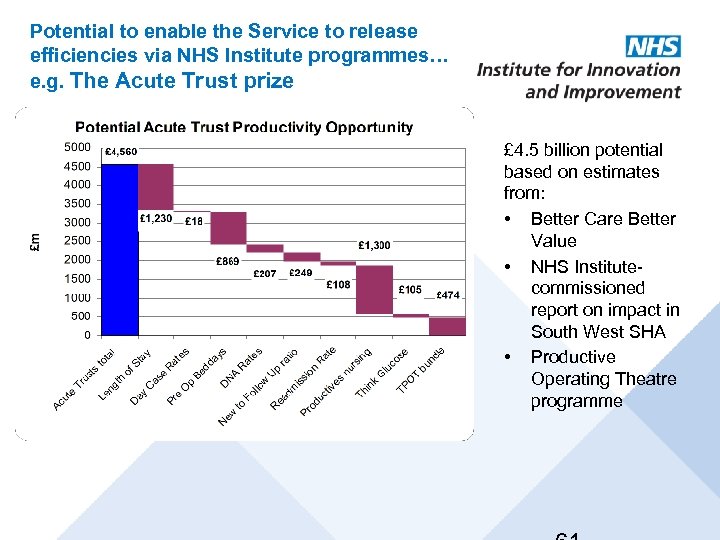
Potential to enable the Service to release efficiencies via NHS Institute programmes… e. g. The Acute Trust prize £ 4. 5 billion potential based on estimates from: • Better Care Better Value • NHS Institutecommissioned report on impact in South West SHA • Productive Operating Theatre programme
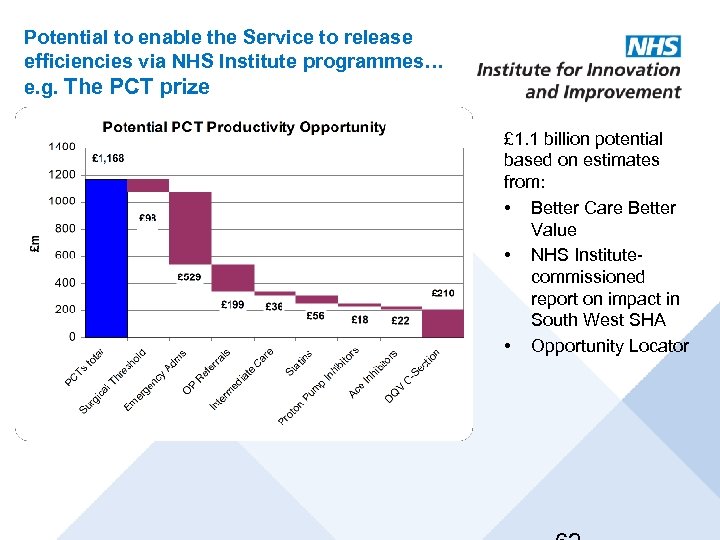
Potential to enable the Service to release efficiencies via NHS Institute programmes… e. g. The PCT prize £ 1. 1 billion potential based on estimates from: • Better Care Better Value • NHS Institute- commissioned report on impact in South West SHA • Opportunity Locator
So… Where Next for Wales? • “Constancy of Purpose for Improvement” • Linkage of Improvement of Care to Sustainable Cost – A Focus on “Muda” • Broadening the Agenda – beyond Safety to Embrace All Dimensions of “Goodness”
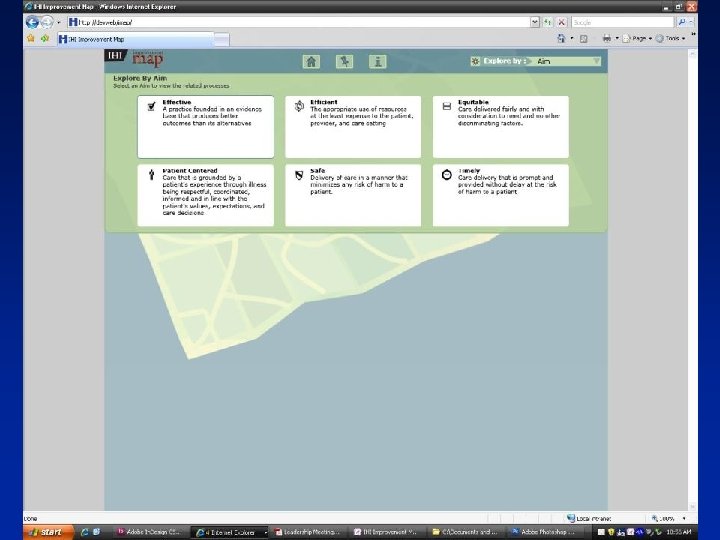
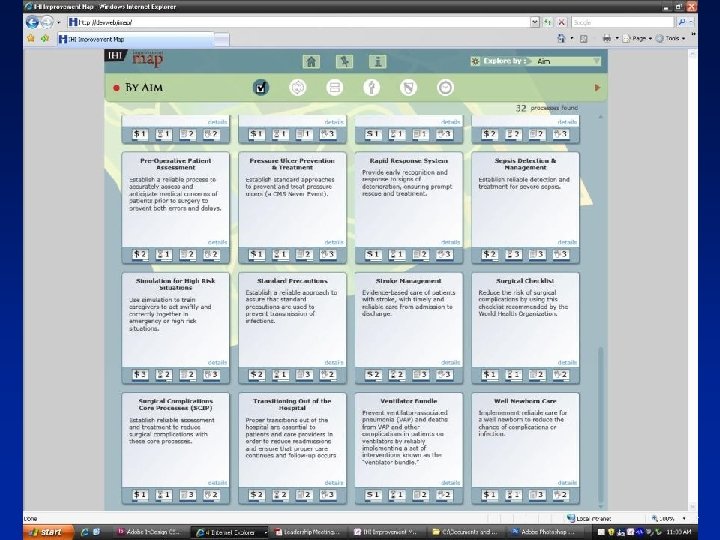
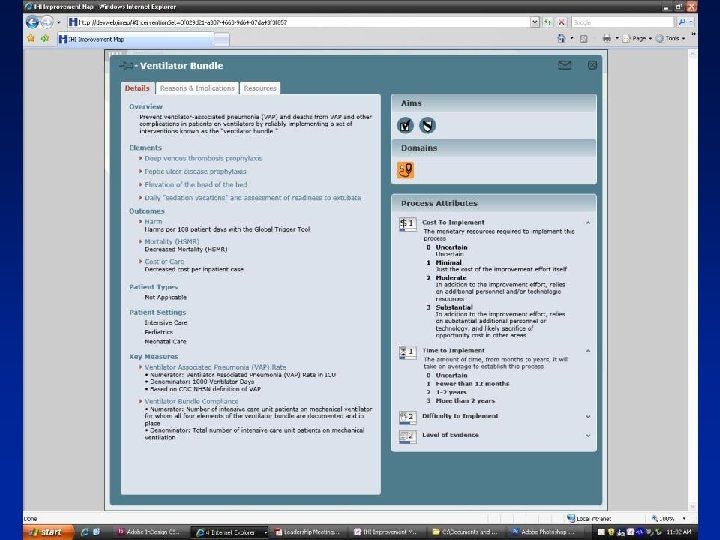
The IHI Improvement Map
• Builds on the great work of participants in the 100, 000 Lives Campaign and the 5 Million Lives Campaign. • “Help us make sense of the many complex and competing demands we face. ” • Brings together the best knowledge available on the key process improvements that will lead to exceptional hospital care. • Helps hospital leaders set change agendas, establish priorities, organize work, and optimize resources. • An open resource, available free of charge to anyone, anywhere. • Launched on 15 September 2009.

So… Where Next for Wales? • “Constancy of Purpose for Improvement” • Linkage of Improvement of Care to Sustainable Cost – A Focus on “Muda” • Broadening the Agenda – beyond Safety to Embrace All Dimensions of “Goodness” • Lead the World in Community-Wide Design and Improvement
So… Where Next for Wales? • “Constancy of Purpose for Improvement” • Linkage of Improvement of Care to Sustainable Cost – A Focus on “Muda” • Broadening the Agenda – beyond Safety to Embrace All Dimensions of “Goodness” • Lead the World in Community-Wide Design and Improvement • Push the Boundaries of “Patient and Family Centered Care” (PFCC)
IHI Measure of Patient-Centeredness “They give me exactly the help I need and want exactly when I need and want it. ” (John Wasson Modification…) “They give me exactly the help I need and want exactly when and how I need and want it. ”
My Proposed Working Definition Patient-Centeredness: “The experience (to the extent the informed, individual patient desires it) of transparency, individualization, recognition, respect, dignity, and choice in all matters, without exception, related to one’s person, circumstances, and relationships in health care. ”

THANK YOU!! What you are doing is important… • For Wales • For the World
466545c1138ea3f8d3120ca6e384a399.ppt