ab078ac44fc4e11b9c8dad16041b340e.ppt
- Количество слайдов: 51
 Surgical treatment of shoulder sports injuries Mr Lee Van Rensburg United Kingdom
Surgical treatment of shoulder sports injuries Mr Lee Van Rensburg United Kingdom
 Objectives • Surgical options for shoulder instability – Glenohumeral • Acute traumatic • Recurrent traumatic
Objectives • Surgical options for shoulder instability – Glenohumeral • Acute traumatic • Recurrent traumatic
 30 YO male, Professional Rugby payer,
30 YO male, Professional Rugby payer,
 Surgical options
Surgical options
 Shoulder Instability Hippocrates 400 BC • method of reduction • cauterisation of inferior capsule
Shoulder Instability Hippocrates 400 BC • method of reduction • cauterisation of inferior capsule
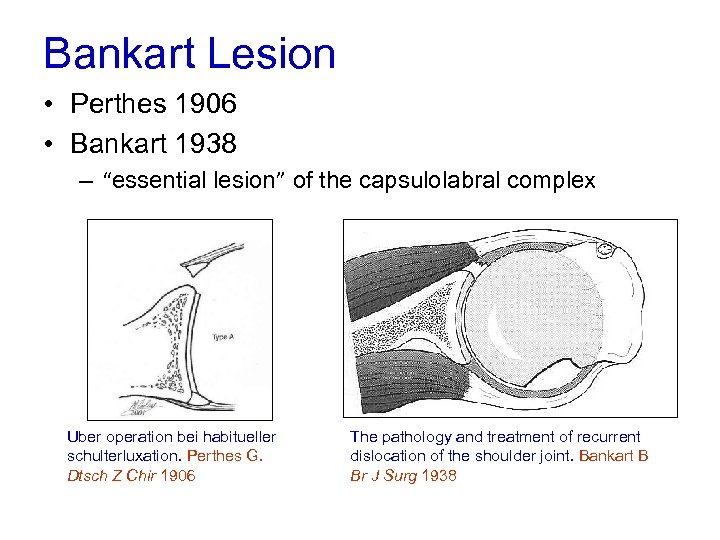 Bankart Lesion • Perthes 1906 • Bankart 1938 – “essential lesion” of the capsulolabral complex Uber operation bei habitueller schulterluxation. Perthes G. Dtsch Z Chir 1906 The pathology and treatment of recurrent dislocation of the shoulder joint. Bankart B Br J Surg 1938
Bankart Lesion • Perthes 1906 • Bankart 1938 – “essential lesion” of the capsulolabral complex Uber operation bei habitueller schulterluxation. Perthes G. Dtsch Z Chir 1906 The pathology and treatment of recurrent dislocation of the shoulder joint. Bankart B Br J Surg 1938
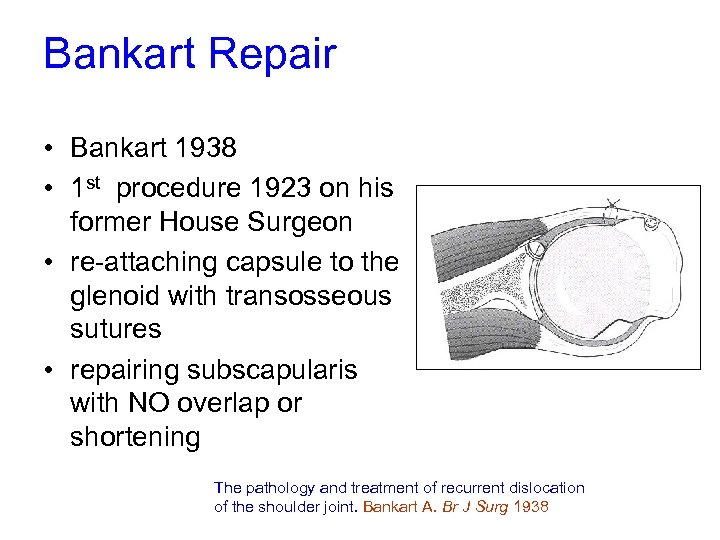 Bankart Repair • Bankart 1938 • 1 st procedure 1923 on his former House Surgeon • re-attaching capsule to the glenoid with transosseous sutures • repairing subscapularis with NO overlap or shortening The pathology and treatment of recurrent dislocation of the shoulder joint. Bankart A. Br J Surg 1938
Bankart Repair • Bankart 1938 • 1 st procedure 1923 on his former House Surgeon • re-attaching capsule to the glenoid with transosseous sutures • repairing subscapularis with NO overlap or shortening The pathology and treatment of recurrent dislocation of the shoulder joint. Bankart A. Br J Surg 1938
 Modified Open Bankart Repair • Numerous modifications - capsular imbrication - suture anchors • Multiple series published • Accepted recurrence rate Open Bankart Repair 8 – 12% • Loss of ER
Modified Open Bankart Repair • Numerous modifications - capsular imbrication - suture anchors • Multiple series published • Accepted recurrence rate Open Bankart Repair 8 – 12% • Loss of ER
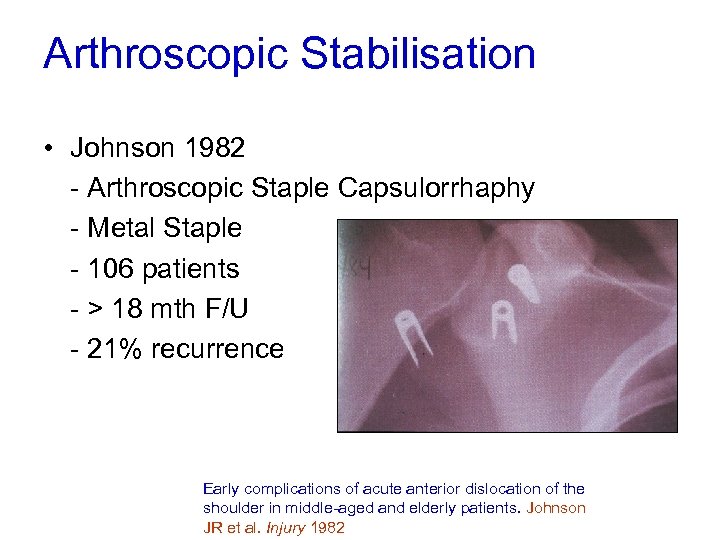 Arthroscopic Stabilisation • Johnson 1982 - Arthroscopic Staple Capsulorrhaphy - Metal Staple - 106 patients - > 18 mth F/U - 21% recurrence Early complications of acute anterior dislocation of the shoulder in middle-aged and elderly patients. Johnson JR et al. Injury 1982
Arthroscopic Stabilisation • Johnson 1982 - Arthroscopic Staple Capsulorrhaphy - Metal Staple - 106 patients - > 18 mth F/U - 21% recurrence Early complications of acute anterior dislocation of the shoulder in middle-aged and elderly patients. Johnson JR et al. Injury 1982
 Staple Capsulorrhaphy Lane et al 1993 - 54 patients Staple Capsulorrhaphy - >39 month F/U - 18 (33%) re-dislocated - 36 stable – 15 % loose staple + articular injury - < 50 loss of ER - Caution in considering Staple Capsulorrhaphy - ROM & functional level well maintained Arthroscopic staple capsulorrhaphy: A long term followup. Lane JG et al. Arthroscopy 1993
Staple Capsulorrhaphy Lane et al 1993 - 54 patients Staple Capsulorrhaphy - >39 month F/U - 18 (33%) re-dislocated - 36 stable – 15 % loose staple + articular injury - < 50 loss of ER - Caution in considering Staple Capsulorrhaphy - ROM & functional level well maintained Arthroscopic staple capsulorrhaphy: A long term followup. Lane JG et al. Arthroscopy 1993
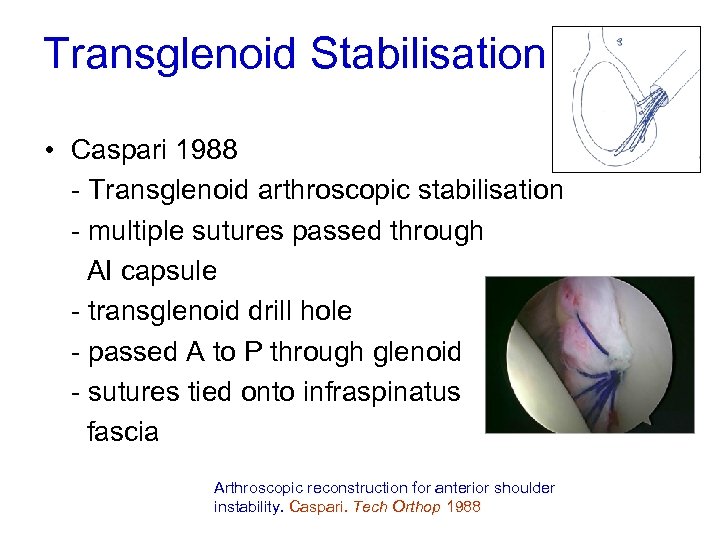 Transglenoid Stabilisation • Caspari 1988 - Transglenoid arthroscopic stabilisation - multiple sutures passed through AI capsule - transglenoid drill hole - passed A to P through glenoid - sutures tied onto infraspinatus fascia Arthroscopic reconstruction for anterior shoulder instability. Caspari. Tech Orthop 1988
Transglenoid Stabilisation • Caspari 1988 - Transglenoid arthroscopic stabilisation - multiple sutures passed through AI capsule - transglenoid drill hole - passed A to P through glenoid - sutures tied onto infraspinatus fascia Arthroscopic reconstruction for anterior shoulder instability. Caspari. Tech Orthop 1988
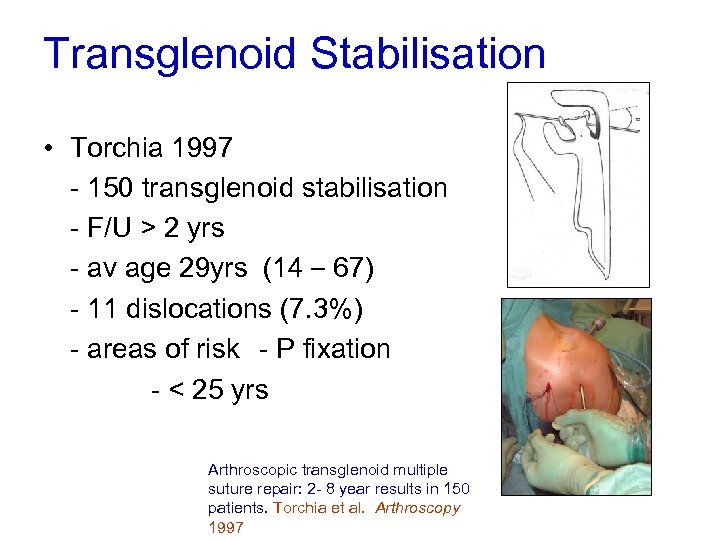 Transglenoid Stabilisation • Torchia 1997 - 150 transglenoid stabilisation - F/U > 2 yrs - av age 29 yrs (14 – 67) - 11 dislocations (7. 3%) - areas of risk - P fixation - < 25 yrs Arthroscopic transglenoid multiple suture repair: 2 - 8 year results in 150 patients. Torchia et al. Arthroscopy 1997
Transglenoid Stabilisation • Torchia 1997 - 150 transglenoid stabilisation - F/U > 2 yrs - av age 29 yrs (14 – 67) - 11 dislocations (7. 3%) - areas of risk - P fixation - < 25 yrs Arthroscopic transglenoid multiple suture repair: 2 - 8 year results in 150 patients. Torchia et al. Arthroscopy 1997
 Transglenoid Stabilisation • Soderlund 2008 - 455 army recruits (1992 – 2000) Questionaire - 312 (68. 5%) responded av 20 yr (18 -28) - Av time from surg 6. 4 yrs (1 -14) - 177 (56%) re-dislocations Long-term outcome of a transglenoid suture technique for anterior shoulder instability in young adults. Soderlund et al JBJS Br 2008
Transglenoid Stabilisation • Soderlund 2008 - 455 army recruits (1992 – 2000) Questionaire - 312 (68. 5%) responded av 20 yr (18 -28) - Av time from surg 6. 4 yrs (1 -14) - 177 (56%) re-dislocations Long-term outcome of a transglenoid suture technique for anterior shoulder instability in young adults. Soderlund et al JBJS Br 2008
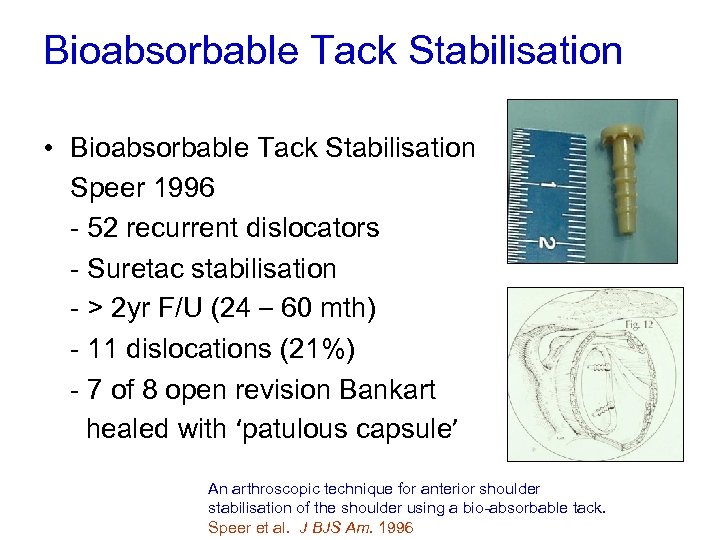 Bioabsorbable Tack Stabilisation • Bioabsorbable Tack Stabilisation Speer 1996 - 52 recurrent dislocators - Suretac stabilisation - > 2 yr F/U (24 – 60 mth) - 11 dislocations (21%) - 7 of 8 open revision Bankart healed with ‘patulous capsule’ An arthroscopic technique for anterior shoulder stabilisation of the shoulder using a bio-absorbable tack. Speer et al. J BJS Am. 1996
Bioabsorbable Tack Stabilisation • Bioabsorbable Tack Stabilisation Speer 1996 - 52 recurrent dislocators - Suretac stabilisation - > 2 yr F/U (24 – 60 mth) - 11 dislocations (21%) - 7 of 8 open revision Bankart healed with ‘patulous capsule’ An arthroscopic technique for anterior shoulder stabilisation of the shoulder using a bio-absorbable tack. Speer et al. J BJS Am. 1996
 Arthroscopic Stabilisation • Suture Anchor Stabilisation - problems staple & transglenoid fixation - difficulty in capsule plication with tacks - improvements in suture anchor design - improvements in instrumentation
Arthroscopic Stabilisation • Suture Anchor Stabilisation - problems staple & transglenoid fixation - difficulty in capsule plication with tacks - improvements in suture anchor design - improvements in instrumentation
 Arthroscopic washout Arthroscopic Stabilisation v Arthroscopic Lavage • 2 yr f/u (1 lavage & 3 stabilisation – lost) - Re-dislocation - stab - lavage 3/42 ( 7%) 16/42 (38%) - Reduction in risk - 76% re-disc & 82% instab Primary arthroscopic stabilisation for a first-time anterior dislocation of the shoulder. Robinson JBJS Am 2008
Arthroscopic washout Arthroscopic Stabilisation v Arthroscopic Lavage • 2 yr f/u (1 lavage & 3 stabilisation – lost) - Re-dislocation - stab - lavage 3/42 ( 7%) 16/42 (38%) - Reduction in risk - 76% re-disc & 82% instab Primary arthroscopic stabilisation for a first-time anterior dislocation of the shoulder. Robinson JBJS Am 2008
 Suture Anchor Stabilisation • Metanalysis Hobby 2007 - 20 suture anchor stabilisation studies - 1030 patients - recurrence as end point - failure rates ranged from 0 – 30% - most < 10% Is arthroscopic surgery for chronic shoulder instability as effective as open surgery? A systematic review and metaanalysis of 62 studies including 3044 arthroscopic operations. Hobby et al. JBJS Br. 2007
Suture Anchor Stabilisation • Metanalysis Hobby 2007 - 20 suture anchor stabilisation studies - 1030 patients - recurrence as end point - failure rates ranged from 0 – 30% - most < 10% Is arthroscopic surgery for chronic shoulder instability as effective as open surgery? A systematic review and metaanalysis of 62 studies including 3044 arthroscopic operations. Hobby et al. JBJS Br. 2007
 Surgical options summary • Hot Poker in axilla • Open Bankart • Arthroscopic – Staple – Transglenoid suture – Suture tacks – Arthroscopic washout – Suture anchors
Surgical options summary • Hot Poker in axilla • Open Bankart • Arthroscopic – Staple – Transglenoid suture – Suture tacks – Arthroscopic washout – Suture anchors
 Again? • Age 30 continues to play what are chances it will happen again
Again? • Age 30 continues to play what are chances it will happen again
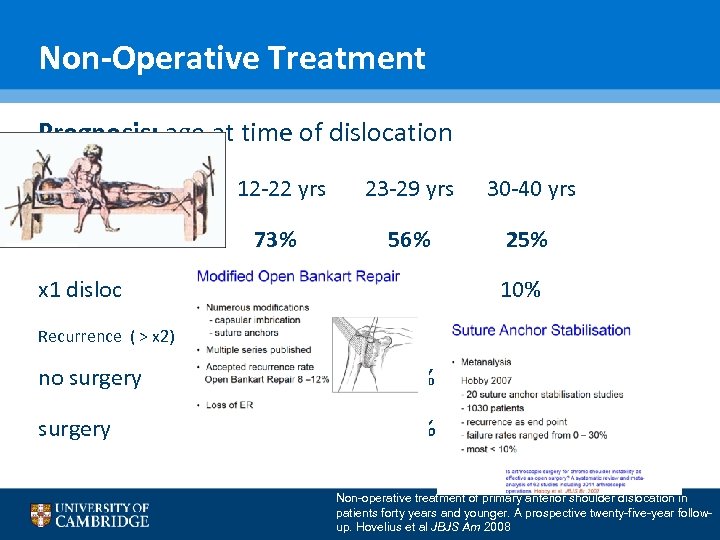 Non-Operative Treatment Prognosis: age at time of dislocation 12 -22 yrs 23 -29 yrs 30 -40 yrs Re dislocated 73% 56% 25% x 1 disloc 20% 18% 10% no surgery 12% 10% 5% surgery 40% 28% 10% Recurrence ( > x 2) Non-operative treatment of primary anterior shoulder dislocation in patients forty years and younger. A prospective twenty-five-year followup. Hovelius et al JBJS Am 2008
Non-Operative Treatment Prognosis: age at time of dislocation 12 -22 yrs 23 -29 yrs 30 -40 yrs Re dislocated 73% 56% 25% x 1 disloc 20% 18% 10% no surgery 12% 10% 5% surgery 40% 28% 10% Recurrence ( > x 2) Non-operative treatment of primary anterior shoulder dislocation in patients forty years and younger. A prospective twenty-five-year followup. Hovelius et al JBJS Am 2008
 Open Access Journal of Sports Medicine 2011: 2 19– 24
Open Access Journal of Sports Medicine 2011: 2 19– 24
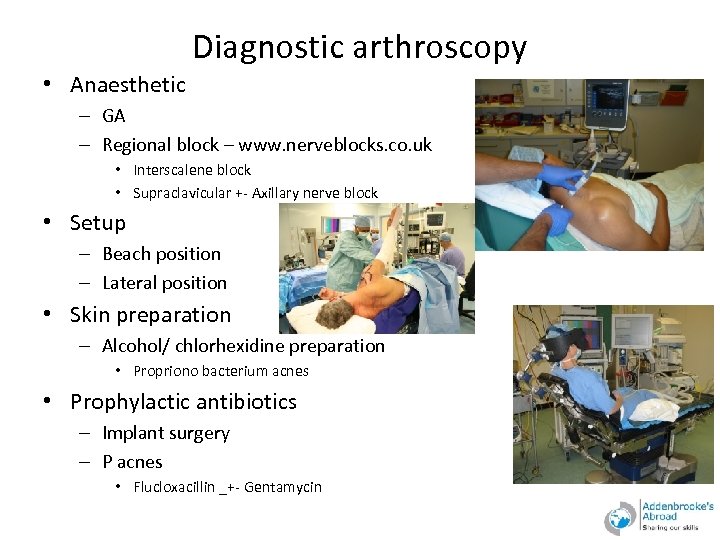 Diagnostic arthroscopy • Anaesthetic – GA – Regional block – www. nerveblocks. co. uk • Interscalene block • Supraclavicular +- Axillary nerve block • Setup – Beach position – Lateral position • Skin preparation – Alcohol/ chlorhexidine preparation • Propriono bacterium acnes • Prophylactic antibiotics – Implant surgery – P acnes • Flucloxacillin _+- Gentamycin
Diagnostic arthroscopy • Anaesthetic – GA – Regional block – www. nerveblocks. co. uk • Interscalene block • Supraclavicular +- Axillary nerve block • Setup – Beach position – Lateral position • Skin preparation – Alcohol/ chlorhexidine preparation • Propriono bacterium acnes • Prophylactic antibiotics – Implant surgery – P acnes • Flucloxacillin _+- Gentamycin
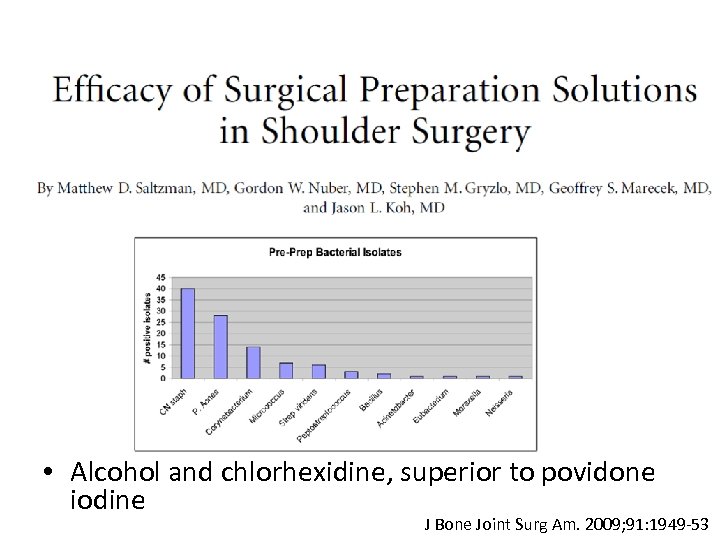 • Alcohol and chlorhexidine, superior to povidone iodine J Bone Joint Surg Am. 2009; 91: 1949 -53
• Alcohol and chlorhexidine, superior to povidone iodine J Bone Joint Surg Am. 2009; 91: 1949 -53
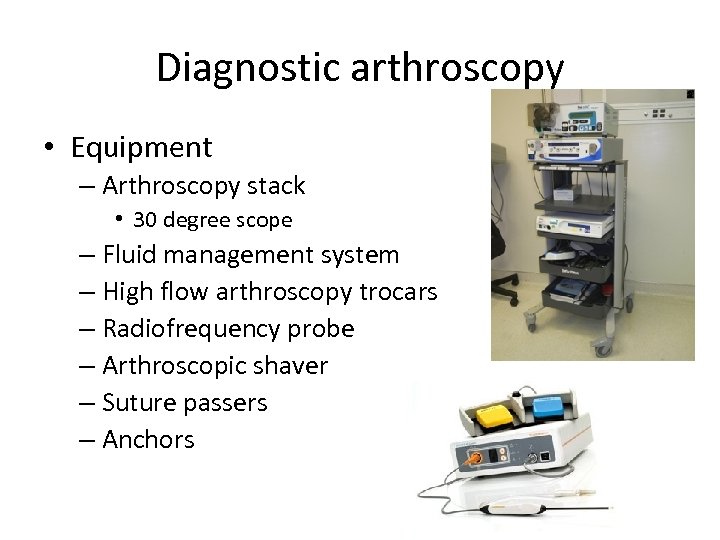 Diagnostic arthroscopy • Equipment – Arthroscopy stack • 30 degree scope – Fluid management system – High flow arthroscopy trocars – Radiofrequency probe – Arthroscopic shaver – Suture passers – Anchors
Diagnostic arthroscopy • Equipment – Arthroscopy stack • 30 degree scope – Fluid management system – High flow arthroscopy trocars – Radiofrequency probe – Arthroscopic shaver – Suture passers – Anchors
 Diagnostic arthroscopy • Portals – Posterior – viewing portal – Anterior- working portal (inside out, spinal needle) • Procedure – – – – – Biceps anchor Anterior labrum MGHL Subscapularis SGHL (Pulley) Biceps (tunnel) Supraspinatus Inferior recess Articular surfaces • • • Glenoid Humeral head Closure – Subcuticular prolene
Diagnostic arthroscopy • Portals – Posterior – viewing portal – Anterior- working portal (inside out, spinal needle) • Procedure – – – – – Biceps anchor Anterior labrum MGHL Subscapularis SGHL (Pulley) Biceps (tunnel) Supraspinatus Inferior recess Articular surfaces • • • Glenoid Humeral head Closure – Subcuticular prolene
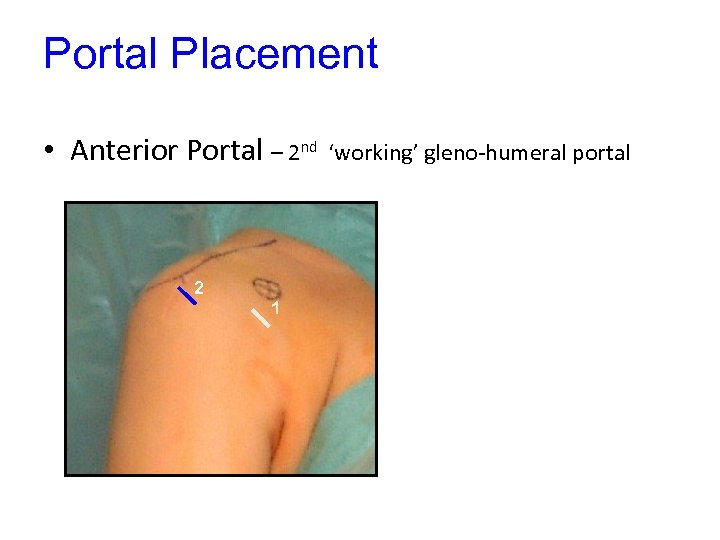 Portal Placement • Anterior Portal – 2 nd 2 1 ‘working’ gleno-humeral portal
Portal Placement • Anterior Portal – 2 nd 2 1 ‘working’ gleno-humeral portal
 Arthroscopic Bankart
Arthroscopic Bankart
 Diagnostic Arthroscopy
Diagnostic Arthroscopy
 Suture Anchor Insertion
Suture Anchor Insertion
 Knott Tying
Knott Tying
 Second Anchor
Second Anchor
 Arthroscopic stabilisation
Arthroscopic stabilisation
 Arthroscopic stabilisation
Arthroscopic stabilisation
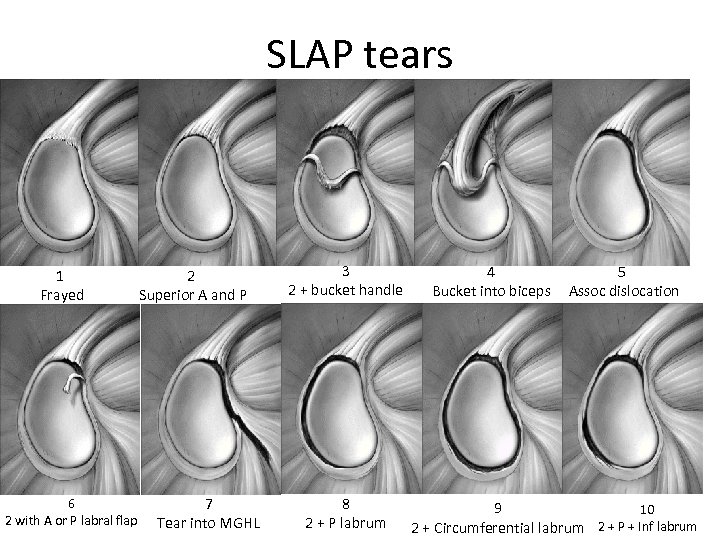 SLAP tears 1 Frayed 6 2 with A or P labral flap 2 Superior A and P 7 Tear into MGHL 3 2 + bucket handle 8 2 + P labrum 4 Bucket into biceps 5 Assoc dislocation 9 10 2 + Circumferential labrum 2 + P + Inf labrum
SLAP tears 1 Frayed 6 2 with A or P labral flap 2 Superior A and P 7 Tear into MGHL 3 2 + bucket handle 8 2 + P labrum 4 Bucket into biceps 5 Assoc dislocation 9 10 2 + Circumferential labrum 2 + P + Inf labrum
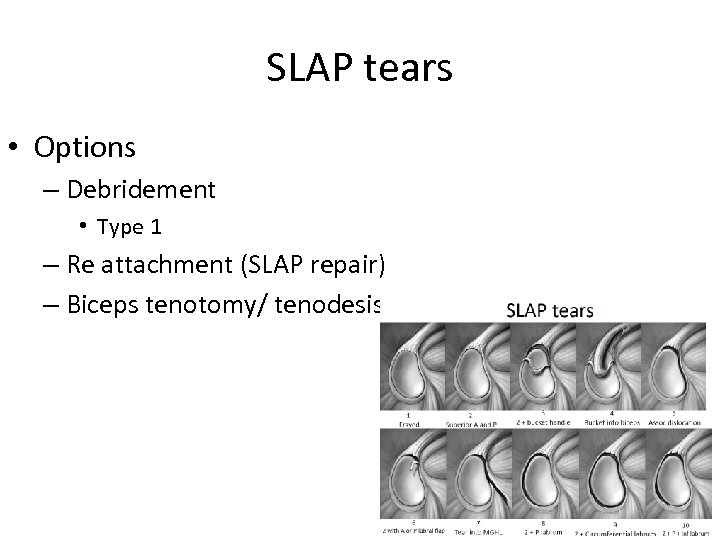 SLAP tears • Options – Debridement • Type 1 – Re attachment (SLAP repair) – Biceps tenotomy/ tenodesis
SLAP tears • Options – Debridement • Type 1 – Re attachment (SLAP repair) – Biceps tenotomy/ tenodesis
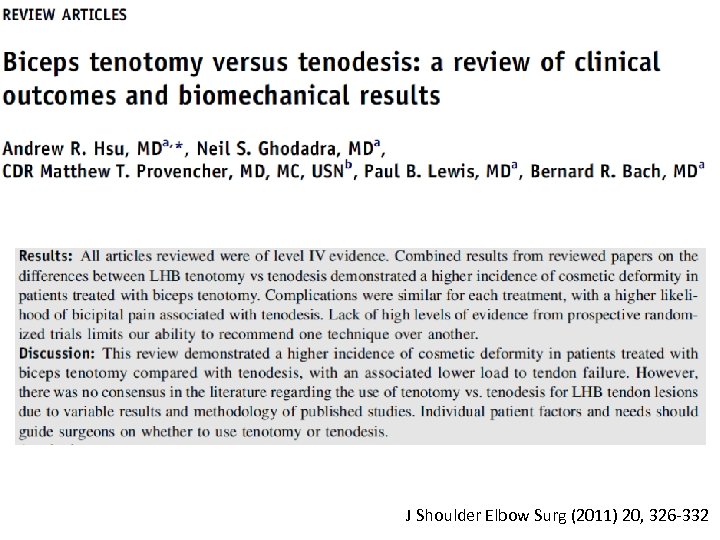 J Shoulder Elbow Surg (2011) 20, 326 -332
J Shoulder Elbow Surg (2011) 20, 326 -332
 Again?
Again?
 • Recurrence rates – Arthroscopic (suture anchor) 8 -11% – Open (Bankart) 0 -11% • Arthroscopic slightly better ROM Sports Health. 2011 Jul; 3(4): 396 -404.
• Recurrence rates – Arthroscopic (suture anchor) 8 -11% – Open (Bankart) 0 -11% • Arthroscopic slightly better ROM Sports Health. 2011 Jul; 3(4): 396 -404.
 Glenoid Bone Loss • Re-Dislocation - 194 arthroscopic stabilisations - 21 significant bone loss - no bone loss - inverted pear 4% recurrence 61% recurrence - “Inverted Pear” 25% of glenoid surface area Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the glenoid’s “inverted pear” and the humeral “engaging Hills-Sachs lesion”. Burkhart & De Beer Arthroscopy 2000
Glenoid Bone Loss • Re-Dislocation - 194 arthroscopic stabilisations - 21 significant bone loss - no bone loss - inverted pear 4% recurrence 61% recurrence - “Inverted Pear” 25% of glenoid surface area Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the glenoid’s “inverted pear” and the humeral “engaging Hills-Sachs lesion”. Burkhart & De Beer Arthroscopy 2000
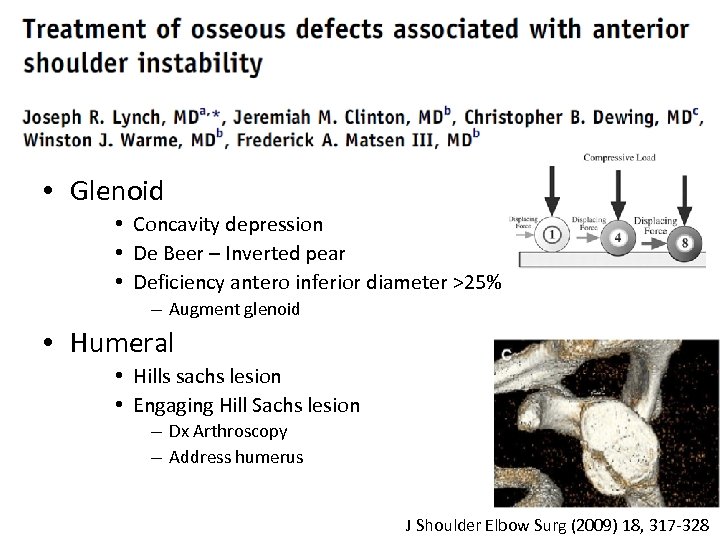 • Glenoid • Concavity depression • De Beer – Inverted pear • Deficiency antero inferior diameter >25% – Augment glenoid • Humeral • Hills sachs lesion • Engaging Hill Sachs lesion – Dx Arthroscopy – Address humerus J Shoulder Elbow Surg (2009) 18, 317 -328
• Glenoid • Concavity depression • De Beer – Inverted pear • Deficiency antero inferior diameter >25% – Augment glenoid • Humeral • Hills sachs lesion • Engaging Hill Sachs lesion – Dx Arthroscopy – Address humerus J Shoulder Elbow Surg (2009) 18, 317 -328
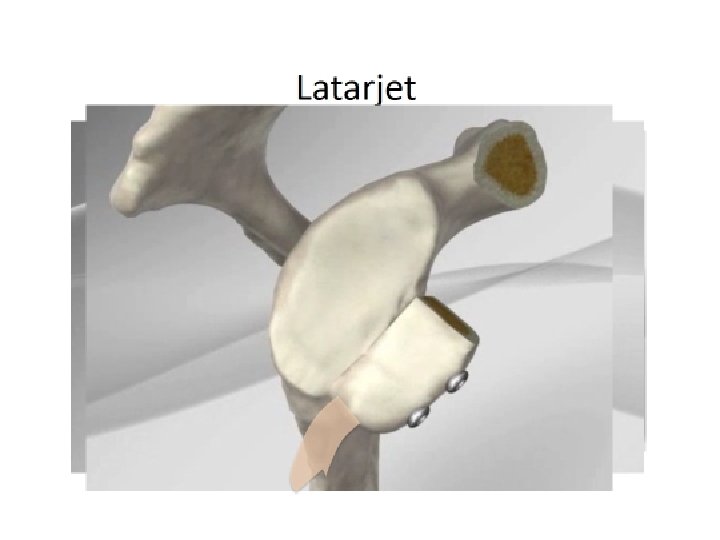
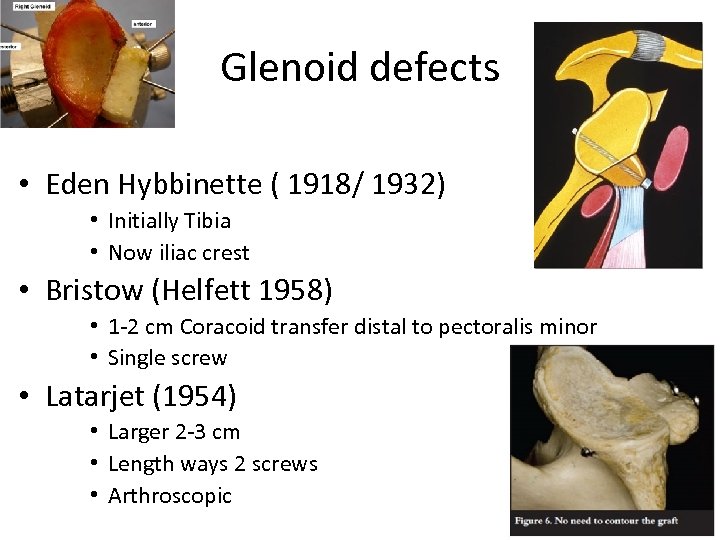 Glenoid defects • Eden Hybbinette ( 1918/ 1932) • Initially Tibia • Now iliac crest • Bristow (Helfett 1958) • 1 -2 cm Coracoid transfer distal to pectoralis minor • Single screw • Latarjet (1954) • Larger 2 -3 cm • Length ways 2 screws • Arthroscopic
Glenoid defects • Eden Hybbinette ( 1918/ 1932) • Initially Tibia • Now iliac crest • Bristow (Helfett 1958) • 1 -2 cm Coracoid transfer distal to pectoralis minor • Single screw • Latarjet (1954) • Larger 2 -3 cm • Length ways 2 screws • Arthroscopic
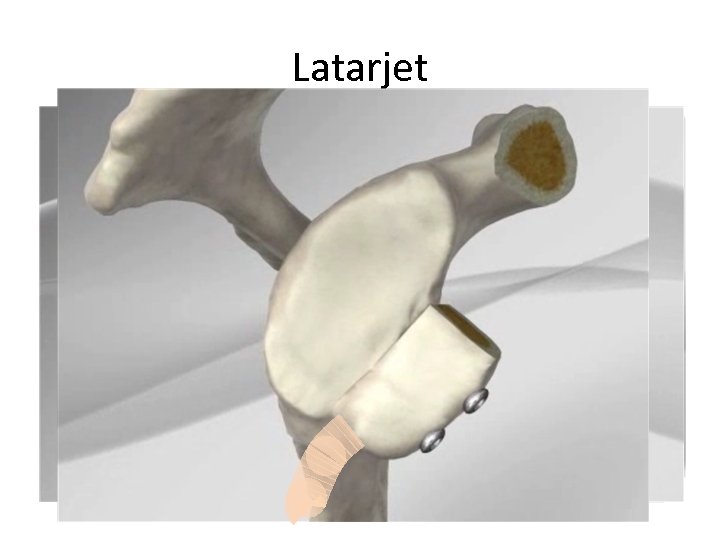 Latarjet
Latarjet
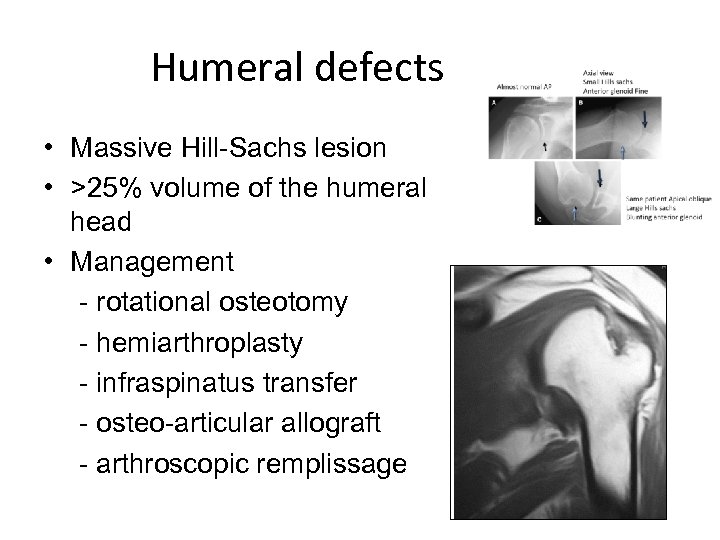 Humeral defects • Massive Hill-Sachs lesion • >25% volume of the humeral head • Management - rotational osteotomy - hemiarthroplasty - infraspinatus transfer - osteo-articular allograft - arthroscopic remplissage
Humeral defects • Massive Hill-Sachs lesion • >25% volume of the humeral head • Management - rotational osteotomy - hemiarthroplasty - infraspinatus transfer - osteo-articular allograft - arthroscopic remplissage
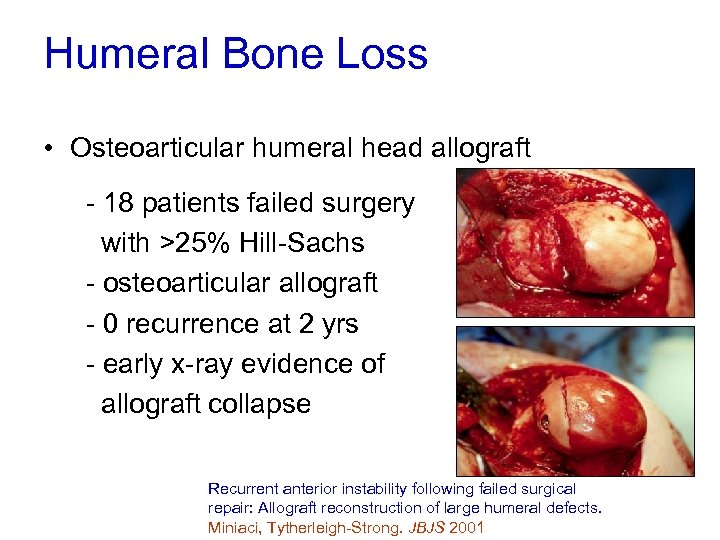 Humeral Bone Loss • Osteoarticular humeral head allograft - 18 patients failed surgery with >25% Hill-Sachs - osteoarticular allograft - 0 recurrence at 2 yrs - early x-ray evidence of allograft collapse Recurrent anterior instability following failed surgical repair: Allograft reconstruction of large humeral defects. Miniaci, Tytherleigh-Strong. JBJS 2001
Humeral Bone Loss • Osteoarticular humeral head allograft - 18 patients failed surgery with >25% Hill-Sachs - osteoarticular allograft - 0 recurrence at 2 yrs - early x-ray evidence of allograft collapse Recurrent anterior instability following failed surgical repair: Allograft reconstruction of large humeral defects. Miniaci, Tytherleigh-Strong. JBJS 2001
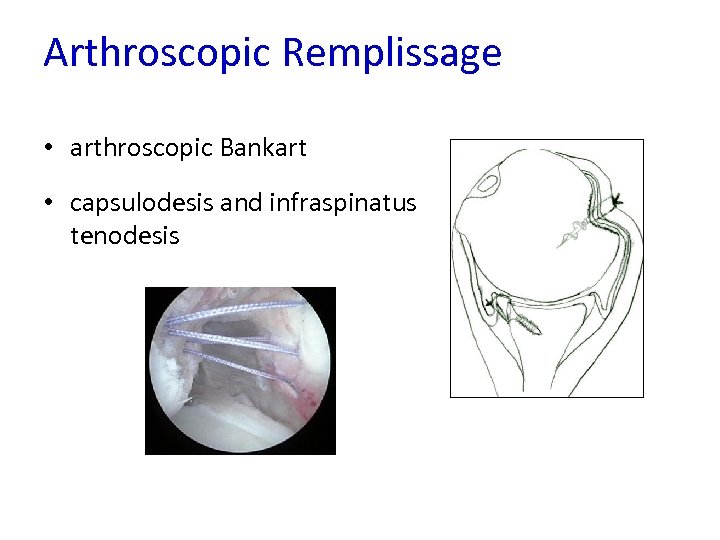 Arthroscopic Remplissage • arthroscopic Bankart • capsulodesis and infraspinatus tenodesis
Arthroscopic Remplissage • arthroscopic Bankart • capsulodesis and infraspinatus tenodesis
 Summary Young sports dislocation 1 week
Summary Young sports dislocation 1 week
 Bone loss - Plain x-ray - CT recon
Bone loss - Plain x-ray - CT recon
 Practically • Arthroscopic Bankart with anchors – 1 st time dislocator – Recurrent with no bony defect • Open Latarjet – Failed arthroscopic Bankart – Bony defects (glenoid) – Chronic dislocation
Practically • Arthroscopic Bankart with anchors – 1 st time dislocator – Recurrent with no bony defect • Open Latarjet – Failed arthroscopic Bankart – Bony defects (glenoid) – Chronic dislocation
 J Bone Joint Surg Am. 2009; 91: 966 -78
J Bone Joint Surg Am. 2009; 91: 966 -78
 The End
The End
