fd9566dcd6b207192cf16c47016d3fa1.ppt
- Количество слайдов: 74
 Surgical Positioning Jeffrey Groom Ph. D, CRNA Nurse Anesthetist Program Florida International University
Surgical Positioning Jeffrey Groom Ph. D, CRNA Nurse Anesthetist Program Florida International University
 SURGICAL POSITIONING OBJECTIVES • Identify the role and responsibility of the anesthesia provider in patient positioning. • Describe the complications associated with improper patient positioning. • Describe the physiological changes that occur with the various positions. • Identify scenarios involving medicolegal liability associated with improper patient positioning.
SURGICAL POSITIONING OBJECTIVES • Identify the role and responsibility of the anesthesia provider in patient positioning. • Describe the complications associated with improper patient positioning. • Describe the physiological changes that occur with the various positions. • Identify scenarios involving medicolegal liability associated with improper patient positioning.
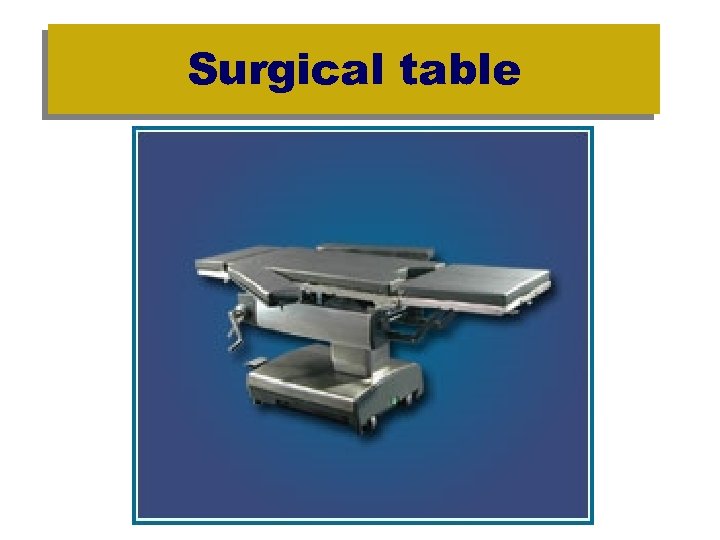 Surgical table
Surgical table
 Surgical Positioning SUPINE
Surgical Positioning SUPINE
 Surgical Positioning Trendelenberg – Reverse Trendelenberg
Surgical Positioning Trendelenberg – Reverse Trendelenberg
 Surgical Positioning Lateral Tilt
Surgical Positioning Lateral Tilt
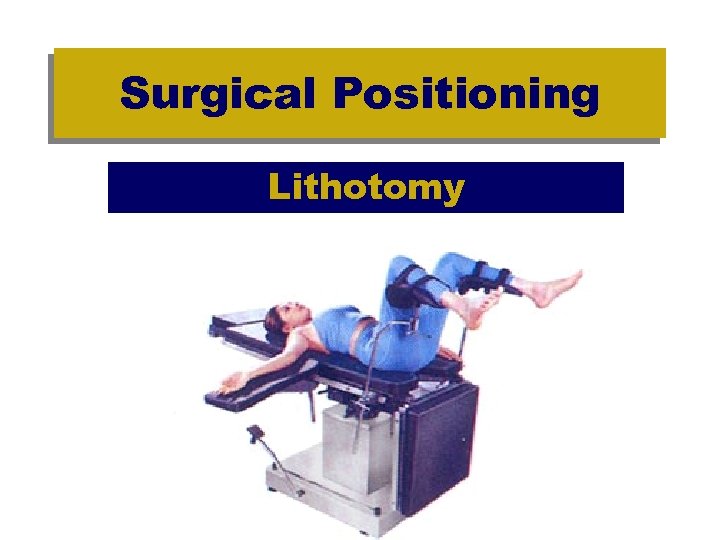 Surgical Positioning Lithotomy
Surgical Positioning Lithotomy
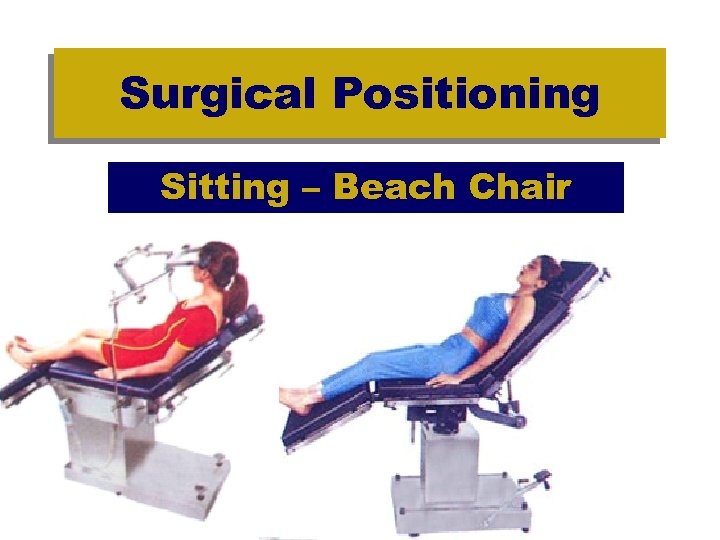 Surgical Positioning Sitting – Beach Chair
Surgical Positioning Sitting – Beach Chair
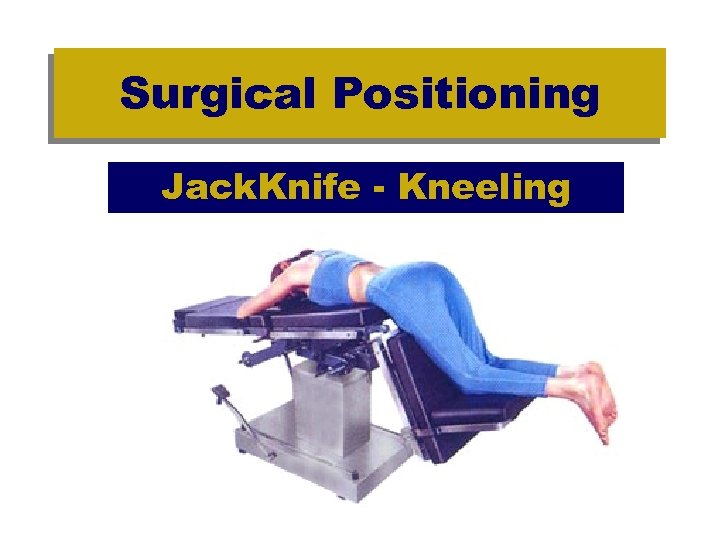 Surgical Positioning Jack. Knife - Kneeling
Surgical Positioning Jack. Knife - Kneeling
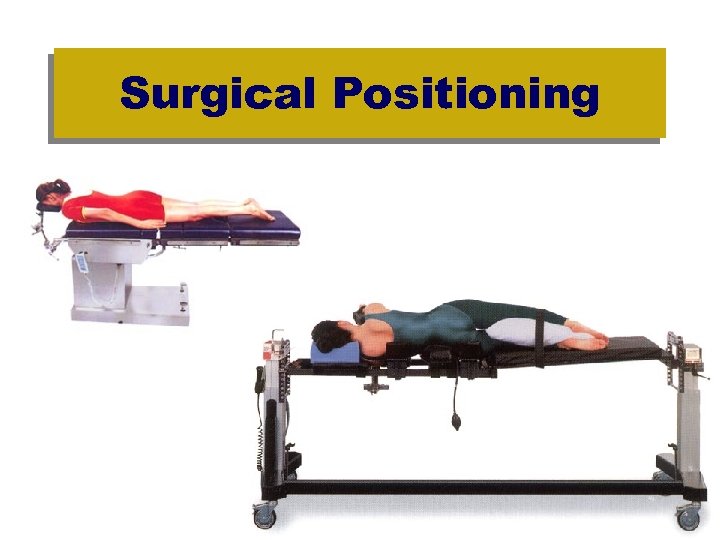 Surgical Positioning
Surgical Positioning
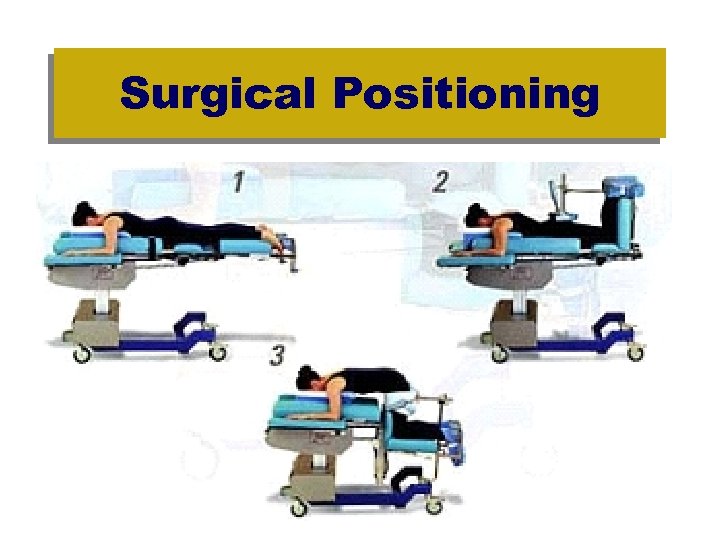 Surgical Positioning
Surgical Positioning
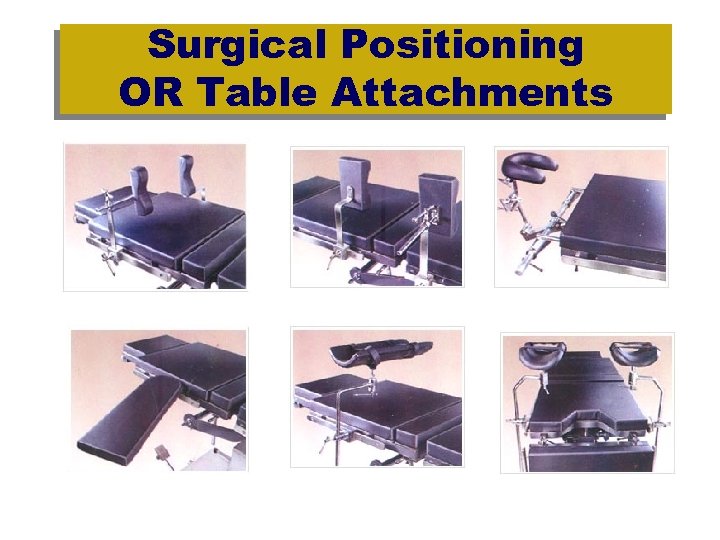 Surgical Positioning OR Table Attachments
Surgical Positioning OR Table Attachments
 Surgical Positioning • All positioning schemes have 3 goals: – 1. Maximum exposure to the surgical area while maintaining homeostasis and preventing injury – 2. Position must provide the Anesthetist with adequate access to the patient for airway management, ventilation, medications, and monitoring – 3. Promote the enhancement of a satisfactory surgical result
Surgical Positioning • All positioning schemes have 3 goals: – 1. Maximum exposure to the surgical area while maintaining homeostasis and preventing injury – 2. Position must provide the Anesthetist with adequate access to the patient for airway management, ventilation, medications, and monitoring – 3. Promote the enhancement of a satisfactory surgical result
 Surgical Positioning What happens when the anesthetized patient can’t care for themselves?
Surgical Positioning What happens when the anesthetized patient can’t care for themselves?
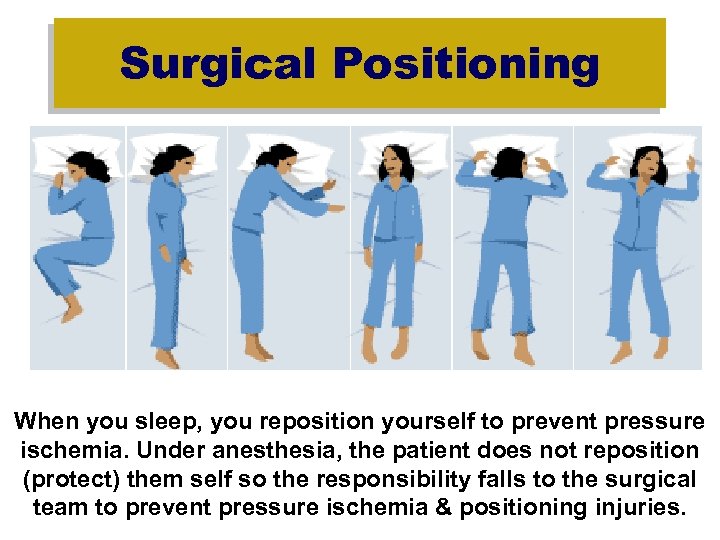 Surgical Positioning When you sleep, you reposition yourself to prevent pressure ischemia. Under anesthesia, the patient does not reposition (protect) them self so the responsibility falls to the surgical team to prevent pressure ischemia & positioning injuries.
Surgical Positioning When you sleep, you reposition yourself to prevent pressure ischemia. Under anesthesia, the patient does not reposition (protect) them self so the responsibility falls to the surgical team to prevent pressure ischemia & positioning injuries.
 Surgical Positioning Why is there a risk for injury ? • Positioning and Anesthesia – Blunted or obtunded reflexes prevent patients from repositioning themselves for relief of discomfort – Anesthesia may blunt compensatory sympathetic nervous system reflexes that would minimize systemic BP changes with abrupt position changes – Rendering patients unconscious and relaxed may permit placement in position they may not have normally tolerated in an awake state
Surgical Positioning Why is there a risk for injury ? • Positioning and Anesthesia – Blunted or obtunded reflexes prevent patients from repositioning themselves for relief of discomfort – Anesthesia may blunt compensatory sympathetic nervous system reflexes that would minimize systemic BP changes with abrupt position changes – Rendering patients unconscious and relaxed may permit placement in position they may not have normally tolerated in an awake state
 Patient Injury and Surgical Positioning • Most are nerve injuries due to overstretching and/or compression. • 90% undergo complete recovery. • 10% are left with residual weakness or sensory loss. • Many injuries can produce lasting disability. • Many injuries lead to litigation. • General anesthesia removes many of the bodies natural protective mechanisms. • Recognition of risks and prevention is essential.
Patient Injury and Surgical Positioning • Most are nerve injuries due to overstretching and/or compression. • 90% undergo complete recovery. • 10% are left with residual weakness or sensory loss. • Many injuries can produce lasting disability. • Many injuries lead to litigation. • General anesthesia removes many of the bodies natural protective mechanisms. • Recognition of risks and prevention is essential.
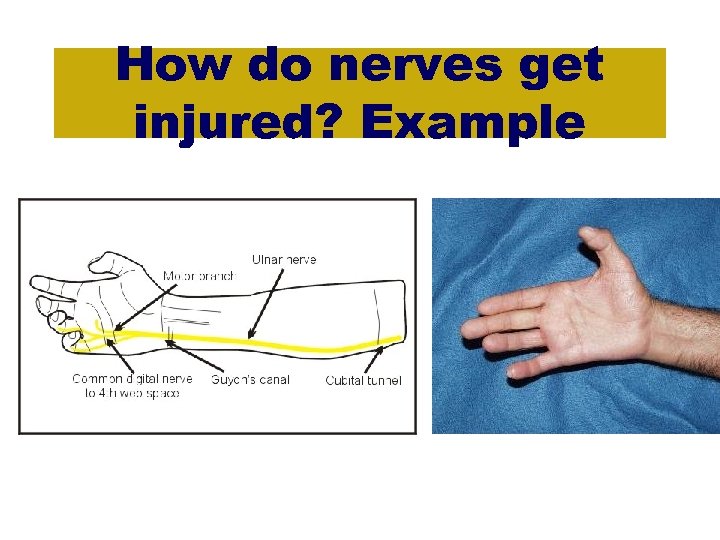 How do nerves get injured? Example
How do nerves get injured? Example
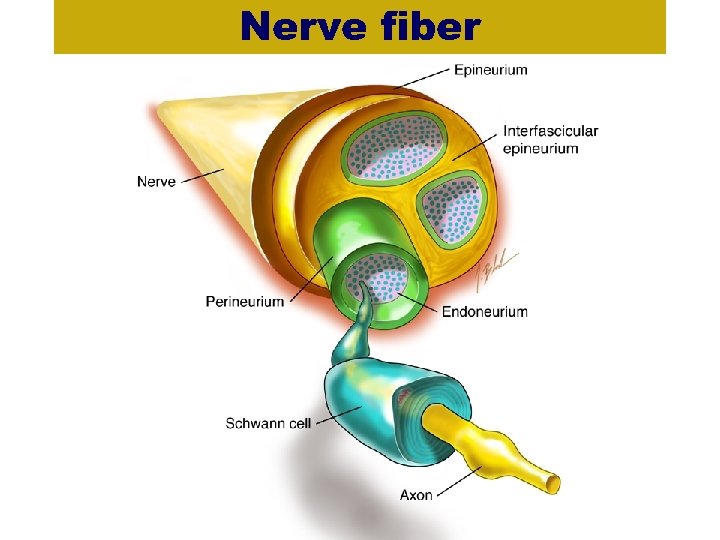 Nerve fiber
Nerve fiber
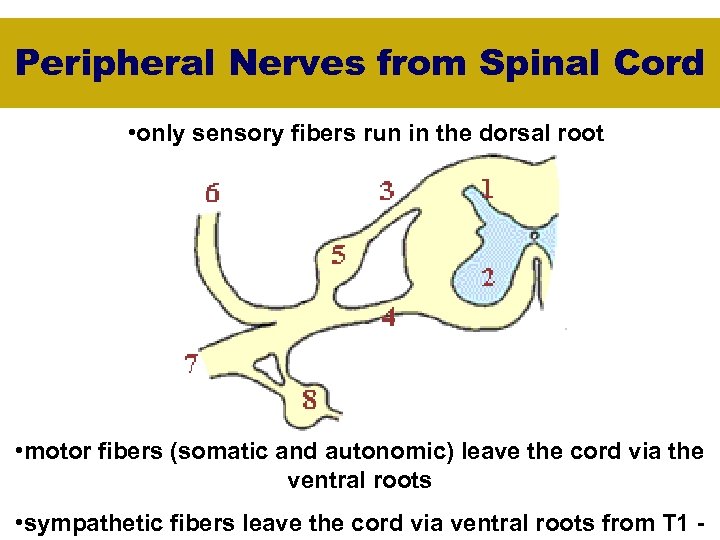 Peripheral Nerves from Spinal Cord • only sensory fibers run in the dorsal root • motor fibers (somatic and autonomic) leave the cord via the ventral roots • sympathetic fibers leave the cord via ventral roots from T 1 -
Peripheral Nerves from Spinal Cord • only sensory fibers run in the dorsal root • motor fibers (somatic and autonomic) leave the cord via the ventral roots • sympathetic fibers leave the cord via ventral roots from T 1 -
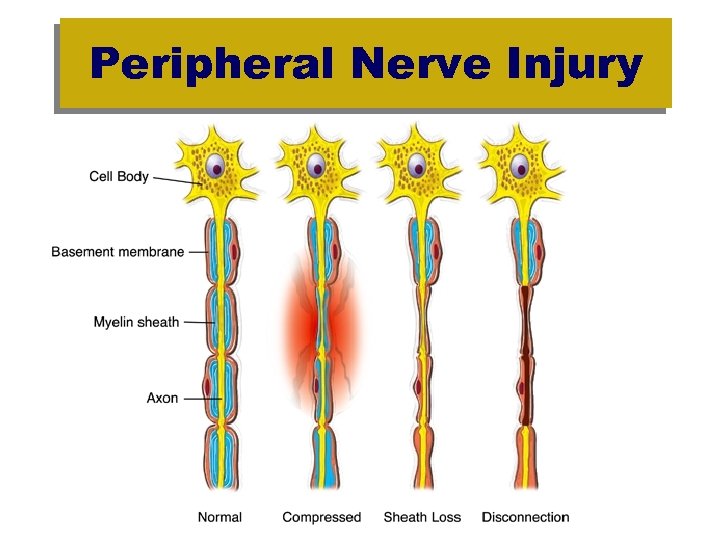 Peripheral Nerve Injury
Peripheral Nerve Injury
 Preoperative History and Physical Assessment Preexisting patient attributes associated with increased incidence of perioperative neuropathies: – extremes of age or body weight, – preexisting neurologic symptoms, – diabetes mellitus, – peripheral vascular disease, – alcohol dependency, – smoking, – and arthritis.
Preoperative History and Physical Assessment Preexisting patient attributes associated with increased incidence of perioperative neuropathies: – extremes of age or body weight, – preexisting neurologic symptoms, – diabetes mellitus, – peripheral vascular disease, – alcohol dependency, – smoking, – and arthritis.
 Surgical Positioning ASA Closed Claims • 1999 - 670 claims for anesthesiarelated nerve injuries • #1 - Ulnar nerve (28%) • #2 - Brachial plexus (20%) • #3 - Common peroneal (13%)
Surgical Positioning ASA Closed Claims • 1999 - 670 claims for anesthesiarelated nerve injuries • #1 - Ulnar nerve (28%) • #2 - Brachial plexus (20%) • #3 - Common peroneal (13%)
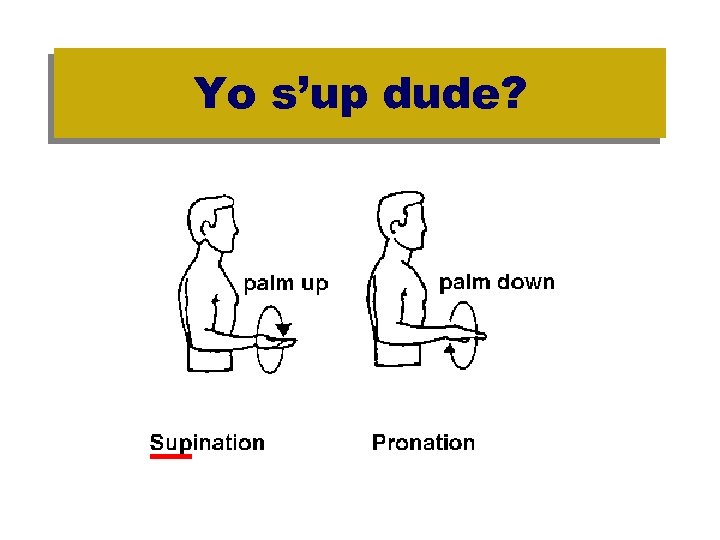
 Surgical Positioning • • Ulnar nerve injury Caused by arms along side patient in pronation Ulnar nerve compressed at elbow between table and medial epicondyle. Prevented by positioning arms in supination. Hypotension and hypoperfuison increase risk.
Surgical Positioning • • Ulnar nerve injury Caused by arms along side patient in pronation Ulnar nerve compressed at elbow between table and medial epicondyle. Prevented by positioning arms in supination. Hypotension and hypoperfuison increase risk.
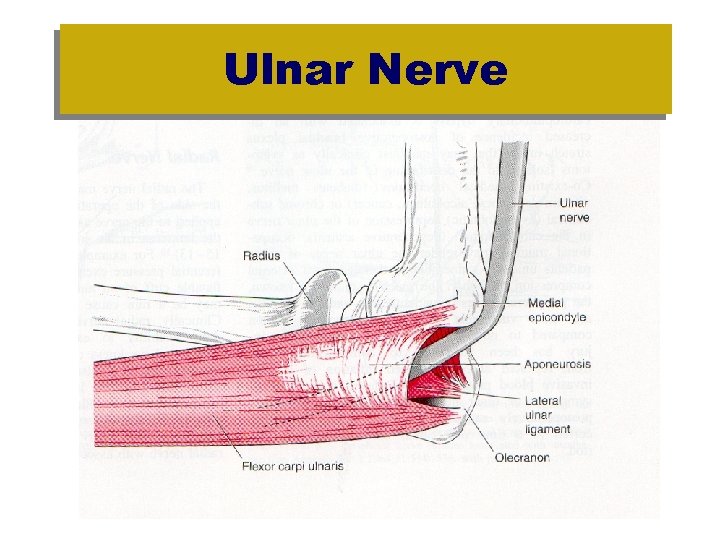 Ulnar Nerve
Ulnar Nerve
 Yo s’up dude?
Yo s’up dude?
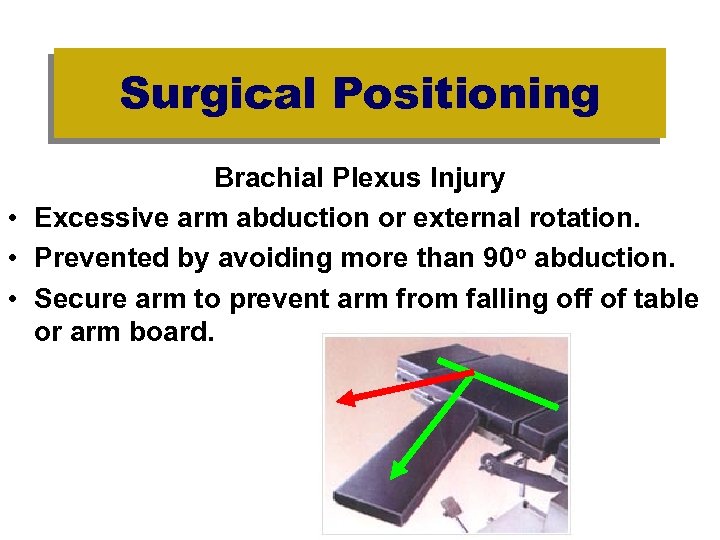 Surgical Positioning Brachial Plexus Injury • Excessive arm abduction or external rotation. • Prevented by avoiding more than 90 o abduction. • Secure arm to prevent arm from falling off of table or arm board.
Surgical Positioning Brachial Plexus Injury • Excessive arm abduction or external rotation. • Prevented by avoiding more than 90 o abduction. • Secure arm to prevent arm from falling off of table or arm board.
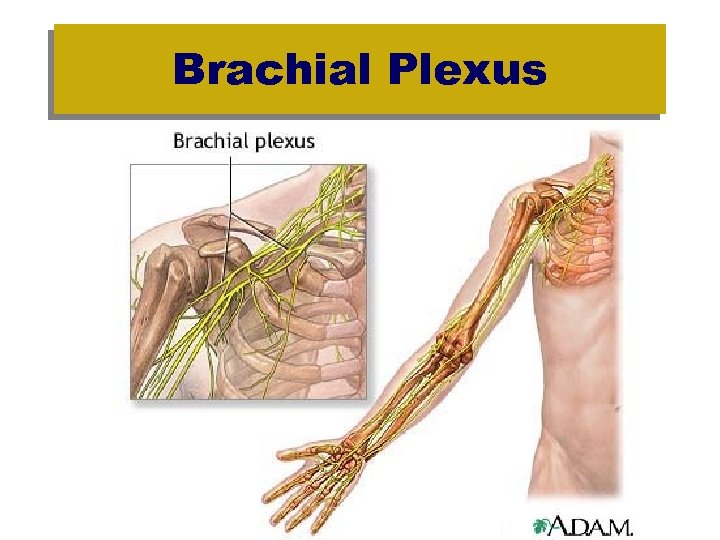 Brachial Plexus
Brachial Plexus
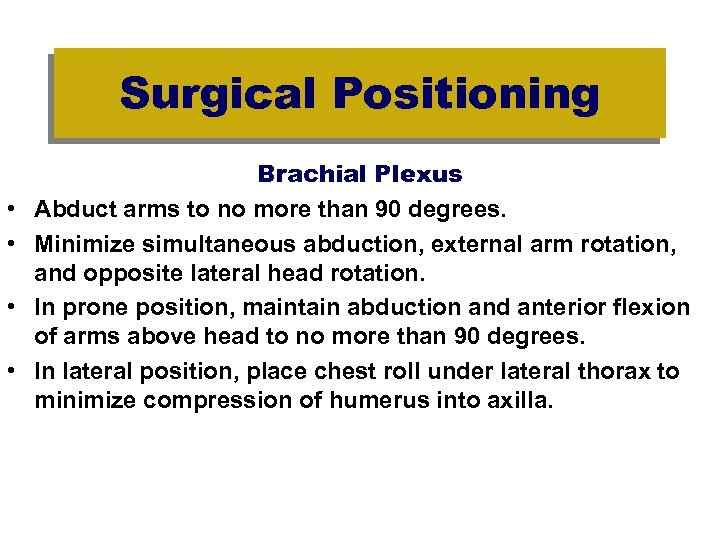 Surgical Positioning • • Brachial Plexus Abduct arms to no more than 90 degrees. Minimize simultaneous abduction, external arm rotation, and opposite lateral head rotation. In prone position, maintain abduction and anterior flexion of arms above head to no more than 90 degrees. In lateral position, place chest roll under lateral thorax to minimize compression of humerus into axilla.
Surgical Positioning • • Brachial Plexus Abduct arms to no more than 90 degrees. Minimize simultaneous abduction, external arm rotation, and opposite lateral head rotation. In prone position, maintain abduction and anterior flexion of arms above head to no more than 90 degrees. In lateral position, place chest roll under lateral thorax to minimize compression of humerus into axilla.
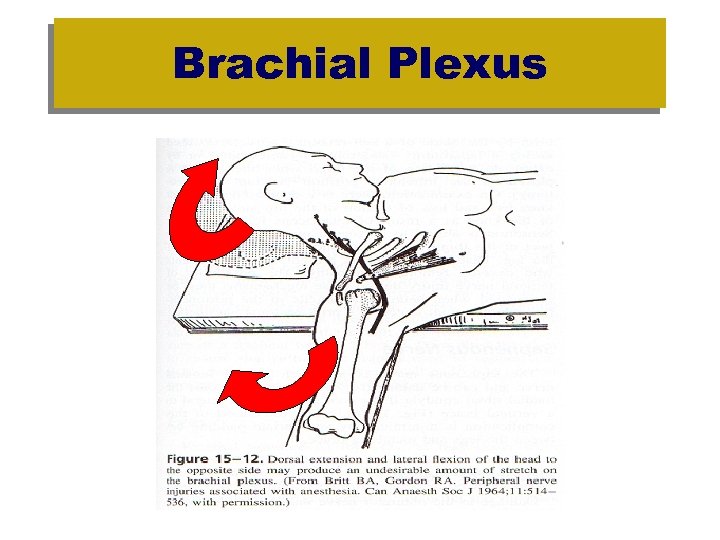 Brachial Plexus
Brachial Plexus
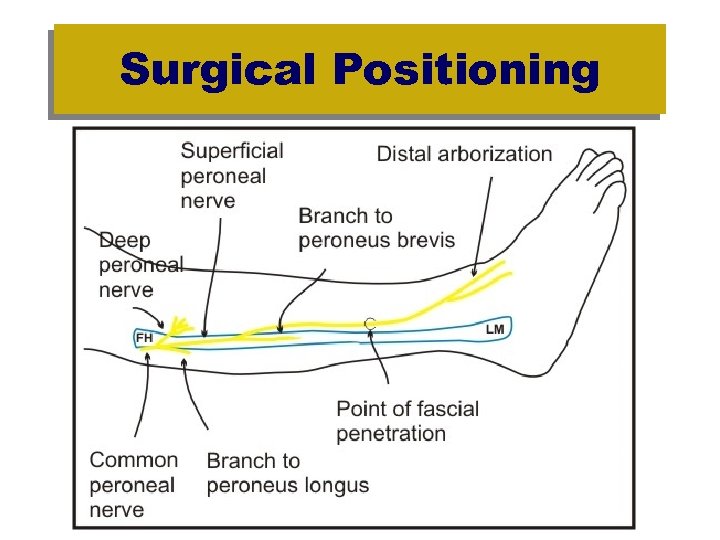
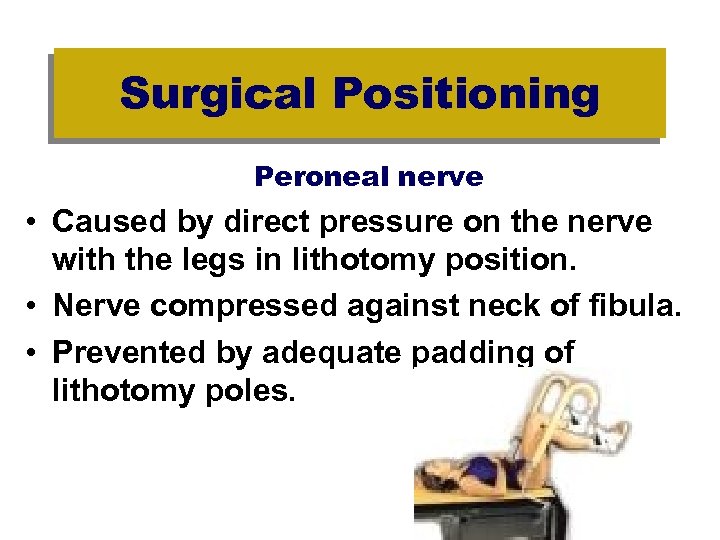 Surgical Positioning Peroneal nerve • Caused by direct pressure on the nerve with the legs in lithotomy position. • Nerve compressed against neck of fibula. • Prevented by adequate padding of lithotomy poles.
Surgical Positioning Peroneal nerve • Caused by direct pressure on the nerve with the legs in lithotomy position. • Nerve compressed against neck of fibula. • Prevented by adequate padding of lithotomy poles.
 Surgical Positioning
Surgical Positioning
 Surgical Positioning
Surgical Positioning
 Surgical Positions and Anesthesia Implications
Surgical Positions and Anesthesia Implications
 Surgical Positioning SUPINE
Surgical Positioning SUPINE
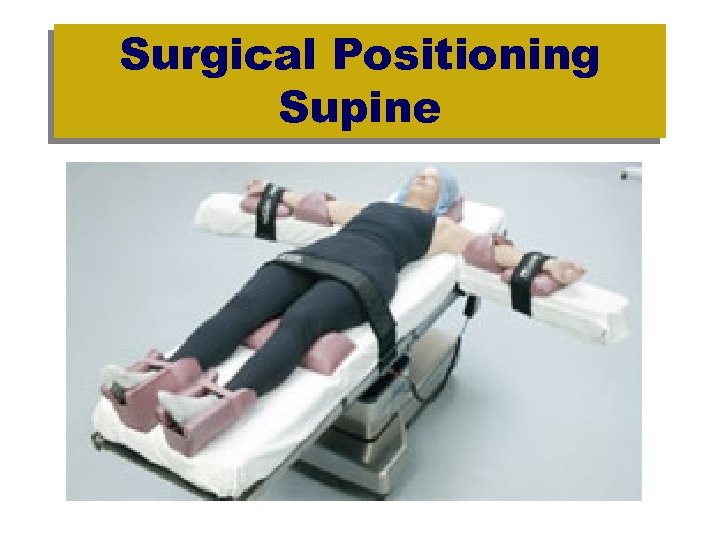
 Surgical Positioning Supine • Most frequently used position. • Cervical, thoracic, lumbar vertebrae should be in a straight, horizontal line. • Minimal effects on circulation. • FRC decreases 25 -30% from upright. • Arm boards and arm must be less than 90 o abduction angle to the torso.
Surgical Positioning Supine • Most frequently used position. • Cervical, thoracic, lumbar vertebrae should be in a straight, horizontal line. • Minimal effects on circulation. • FRC decreases 25 -30% from upright. • Arm boards and arm must be less than 90 o abduction angle to the torso.
 Surgical Positioning Supine (con't) • Arms at greater than 90 o angle results in stretch of the subclavian and axillary vessels resulting in radial pulse obliteration and arterial thrombosis. • Injuries have been reported with as little as 60 o abduction. • Palms up- relieves pressure on the ulnar nerve as it passes through the humeral notch at the elbow.
Surgical Positioning Supine (con't) • Arms at greater than 90 o angle results in stretch of the subclavian and axillary vessels resulting in radial pulse obliteration and arterial thrombosis. • Injuries have been reported with as little as 60 o abduction. • Palms up- relieves pressure on the ulnar nerve as it passes through the humeral notch at the elbow.
 Surgical Positioning Supine • Ulnar nerve injury – Hypotension and hypoperfusion increase risk – Inability to abduct or oppose the 5 th finger – Atrophy of the intrinsic muscles of the hand (claw hand).
Surgical Positioning Supine • Ulnar nerve injury – Hypotension and hypoperfusion increase risk – Inability to abduct or oppose the 5 th finger – Atrophy of the intrinsic muscles of the hand (claw hand).
 Surgical Positioning Supine • Extreme rotation of the head can cause occlusion and thrombosis of the vertebral artery. • Pressure from a mask or head strap can cause injuries of the supraorbital and facial nerves. • Relaxation of the paraspinous muscles and flattening of the normal lumbar convexity results in tension on the interlumbar and lumbosacral ligaments causing a backache.
Surgical Positioning Supine • Extreme rotation of the head can cause occlusion and thrombosis of the vertebral artery. • Pressure from a mask or head strap can cause injuries of the supraorbital and facial nerves. • Relaxation of the paraspinous muscles and flattening of the normal lumbar convexity results in tension on the interlumbar and lumbosacral ligaments causing a backache.
 Surgical Positioning Supine
Surgical Positioning Supine
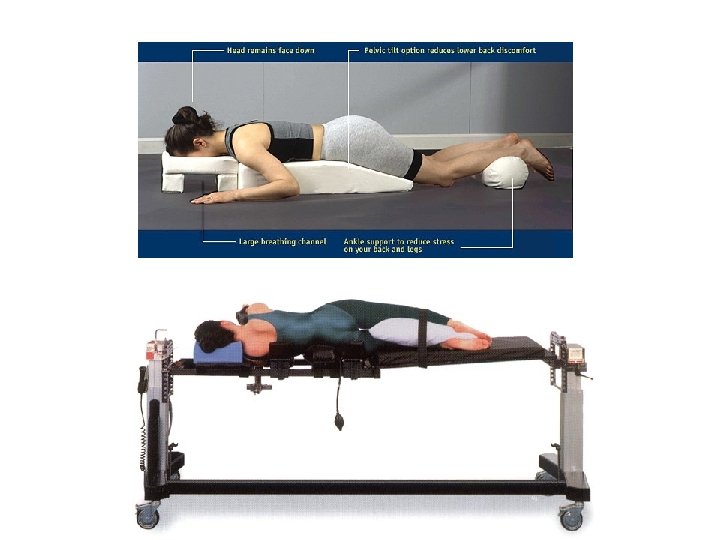
 Surgical Positioning Prone
Surgical Positioning Prone
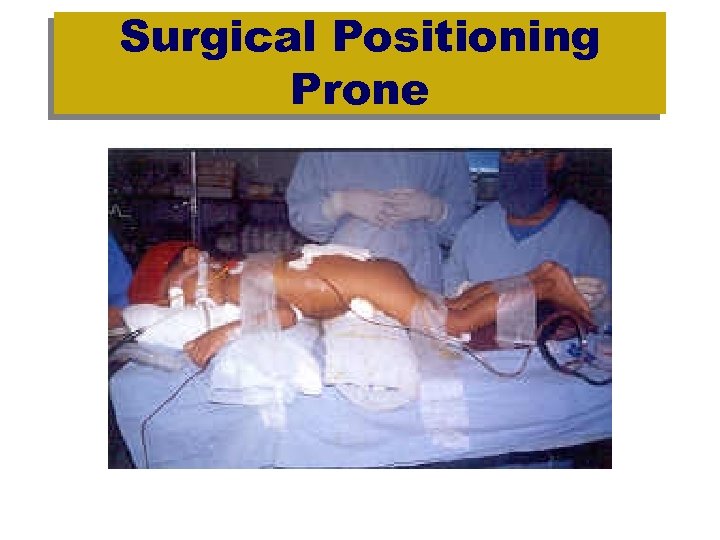
 Surgical Positioning Prone • Induction completed on stretcher, then patient logrolled to OR table under command of CRNA • Body ‘logrolled’ as a unit in a smooth, slow, and gentle manner. • Neck in alignment with spinal column. • Eyes and ears protected and not depressed. • Chest rolls, or bolsters are placed lengthwise on both sides of the thorax, extending from the acromioclavicular joints to iliac crest- adequate lung expansion and diaphragm excursion.
Surgical Positioning Prone • Induction completed on stretcher, then patient logrolled to OR table under command of CRNA • Body ‘logrolled’ as a unit in a smooth, slow, and gentle manner. • Neck in alignment with spinal column. • Eyes and ears protected and not depressed. • Chest rolls, or bolsters are placed lengthwise on both sides of the thorax, extending from the acromioclavicular joints to iliac crest- adequate lung expansion and diaphragm excursion.
 Surgical Positioning Prone • Protect female breasts & male genitalia. • Pillow under legs & ankles to flex knees and prevent pressure on toes and plantar flexion of feet. • Arms at side or extended alongside the head on arm boards • Documentation: pressure points padded, free abdominal and chest expansion, position of the arms, eye care
Surgical Positioning Prone • Protect female breasts & male genitalia. • Pillow under legs & ankles to flex knees and prevent pressure on toes and plantar flexion of feet. • Arms at side or extended alongside the head on arm boards • Documentation: pressure points padded, free abdominal and chest expansion, position of the arms, eye care
 Surgical Positioning Prone • Cardiac – - Pooling of blood in extremities Compression of abdominal muscles Decrease preload, c. o. , and blood pressure Increased SVR and PVR Decreased stroke volume and cardiac index TEDS or pneumatic sequential compression stockings to minimize pooling of blood
Surgical Positioning Prone • Cardiac – - Pooling of blood in extremities Compression of abdominal muscles Decrease preload, c. o. , and blood pressure Increased SVR and PVR Decreased stroke volume and cardiac index TEDS or pneumatic sequential compression stockings to minimize pooling of blood
 Surgical Positioning Prone • Respiratory – Decreased lung compliance – Increased work of breathing – Thoracic Outlet Syndrome-secondary to thoracic nerve compression (agonizing, debilitating, and unremitting pain postoperatively following overhead arm placement – ETT dislodgement - Extubation
Surgical Positioning Prone • Respiratory – Decreased lung compliance – Increased work of breathing – Thoracic Outlet Syndrome-secondary to thoracic nerve compression (agonizing, debilitating, and unremitting pain postoperatively following overhead arm placement – ETT dislodgement - Extubation
 Surgical Positioning Trendelenberg – Reverse Trendelenberg
Surgical Positioning Trendelenberg – Reverse Trendelenberg
 Surgical Positioning Trendelenburg • Cardiac – Activation of baroreceptors – Decrease in C. O. , PVR, HR, and BP – Does not improve C. O. in hypotension & hypovolemia • Respiratory – Decreased FRC, total lung capacity and pulmonary compliance secondary to shift of abdominal viscera – Increased V/Q mismatching – Atlectasis – Increased likelihood of regurgitation • Use of shoulder braces to prevent cephalad mvmt
Surgical Positioning Trendelenburg • Cardiac – Activation of baroreceptors – Decrease in C. O. , PVR, HR, and BP – Does not improve C. O. in hypotension & hypovolemia • Respiratory – Decreased FRC, total lung capacity and pulmonary compliance secondary to shift of abdominal viscera – Increased V/Q mismatching – Atlectasis – Increased likelihood of regurgitation • Use of shoulder braces to prevent cephalad mvmt
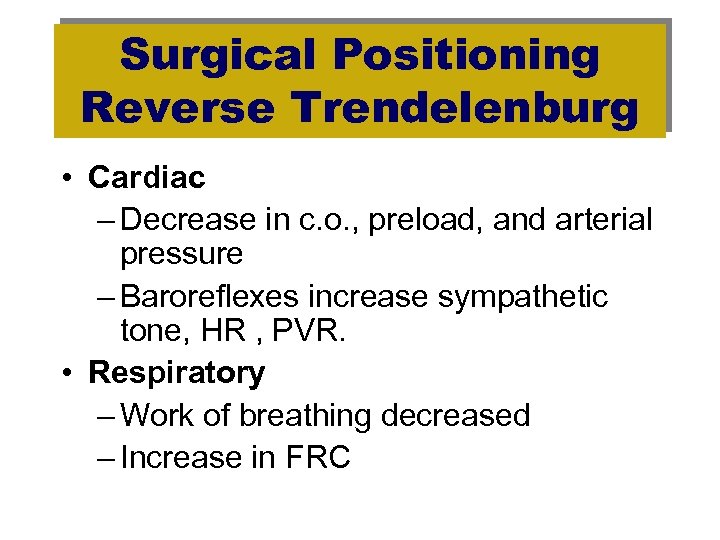 Surgical Positioning Reverse Trendelenburg • Cardiac – Decrease in c. o. , preload, and arterial pressure – Baroreflexes increase sympathetic tone, HR , PVR. • Respiratory – Work of breathing decreased – Increase in FRC
Surgical Positioning Reverse Trendelenburg • Cardiac – Decrease in c. o. , preload, and arterial pressure – Baroreflexes increase sympathetic tone, HR , PVR. • Respiratory – Work of breathing decreased – Increase in FRC
 Surgical Positioning Lateral Decubitus
Surgical Positioning Lateral Decubitus
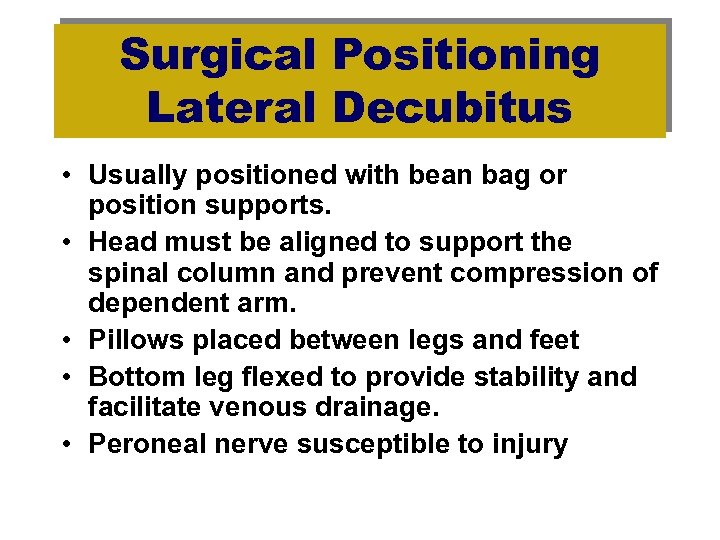 Surgical Positioning Lateral Decubitus • Usually positioned with bean bag or position supports. • Head must be aligned to support the spinal column and prevent compression of dependent arm. • Pillows placed between legs and feet • Bottom leg flexed to provide stability and facilitate venous drainage. • Peroneal nerve susceptible to injury
Surgical Positioning Lateral Decubitus • Usually positioned with bean bag or position supports. • Head must be aligned to support the spinal column and prevent compression of dependent arm. • Pillows placed between legs and feet • Bottom leg flexed to provide stability and facilitate venous drainage. • Peroneal nerve susceptible to injury
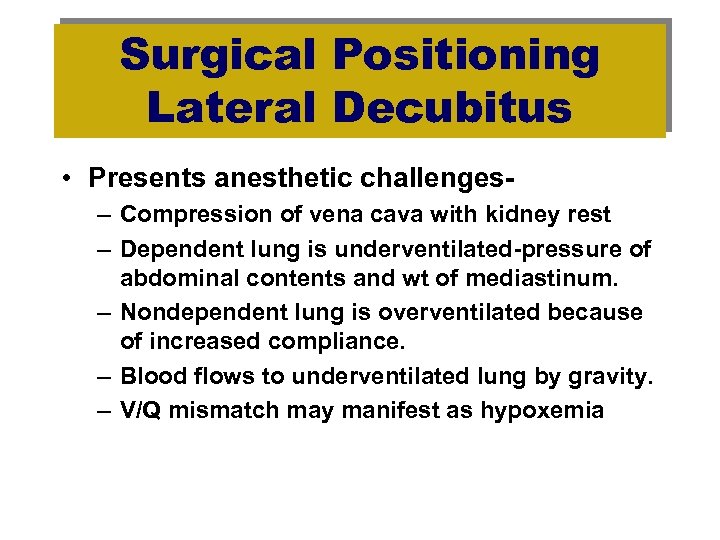 Surgical Positioning Lateral Decubitus • Presents anesthetic challenges– Compression of vena cava with kidney rest – Dependent lung is underventilated-pressure of abdominal contents and wt of mediastinum. – Nondependent lung is overventilated because of increased compliance. – Blood flows to underventilated lung by gravity. – V/Q mismatch may manifest as hypoxemia
Surgical Positioning Lateral Decubitus • Presents anesthetic challenges– Compression of vena cava with kidney rest – Dependent lung is underventilated-pressure of abdominal contents and wt of mediastinum. – Nondependent lung is overventilated because of increased compliance. – Blood flows to underventilated lung by gravity. – V/Q mismatch may manifest as hypoxemia
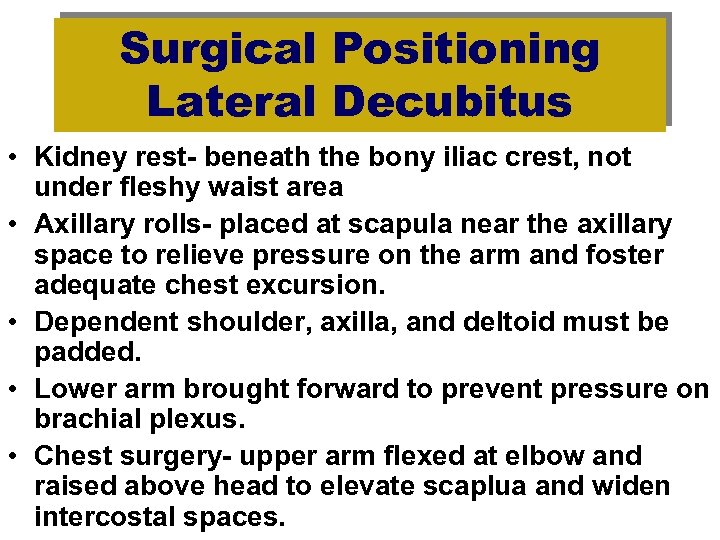 Surgical Positioning Lateral Decubitus • Kidney rest- beneath the bony iliac crest, not under fleshy waist area • Axillary rolls- placed at scapula near the axillary space to relieve pressure on the arm and foster adequate chest excursion. • Dependent shoulder, axilla, and deltoid must be padded. • Lower arm brought forward to prevent pressure on brachial plexus. • Chest surgery- upper arm flexed at elbow and raised above head to elevate scaplua and widen intercostal spaces.
Surgical Positioning Lateral Decubitus • Kidney rest- beneath the bony iliac crest, not under fleshy waist area • Axillary rolls- placed at scapula near the axillary space to relieve pressure on the arm and foster adequate chest excursion. • Dependent shoulder, axilla, and deltoid must be padded. • Lower arm brought forward to prevent pressure on brachial plexus. • Chest surgery- upper arm flexed at elbow and raised above head to elevate scaplua and widen intercostal spaces.
 Surgical Positioning Lateral Decubitus • Cardiac – Output unchanged unless venous return obstructed (kidney rest). – May see decrease in arterial blood pressure as a result of decreased vascular resistance (R > L). • Respiratory – Decreased volume and increased perfusion of dependant lung, V/Q mismatch potential
Surgical Positioning Lateral Decubitus • Cardiac – Output unchanged unless venous return obstructed (kidney rest). – May see decrease in arterial blood pressure as a result of decreased vascular resistance (R > L). • Respiratory – Decreased volume and increased perfusion of dependant lung, V/Q mismatch potential
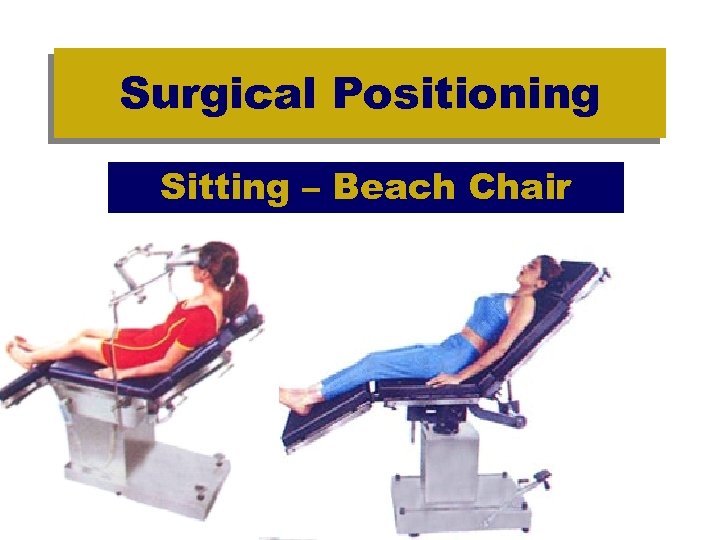 Surgical Positioning Sitting – Beach Chair
Surgical Positioning Sitting – Beach Chair
 Surgical Positioning Sitting • Cardiac – Pooling blood in lower body decreases central blood volume. – ABP fall despite increase in HR & SVR. (30%) – C. O. decreases 20 -40% – Increase in sympathetic /parasympathetic tone – Intrathoracic blood volume decreases as much as 500 ml • Respiratory – Lung volumes are increased. – FRC is increased. – Work of breathing is decreased.
Surgical Positioning Sitting • Cardiac – Pooling blood in lower body decreases central blood volume. – ABP fall despite increase in HR & SVR. (30%) – C. O. decreases 20 -40% – Increase in sympathetic /parasympathetic tone – Intrathoracic blood volume decreases as much as 500 ml • Respiratory – Lung volumes are increased. – FRC is increased. – Work of breathing is decreased.
 Surgical Positioning Sitting • Posterior Foss Craniotomy & shoulder procedures. • Full sitting position is uncommon. • Lounge chair, beach chair. • Facilitates venous drainage. • Venous air embolism risk is potential hazard
Surgical Positioning Sitting • Posterior Foss Craniotomy & shoulder procedures. • Full sitting position is uncommon. • Lounge chair, beach chair. • Facilitates venous drainage. • Venous air embolism risk is potential hazard
 Surgical Positioning Sitting • Complications – Postural hypotension – Air emboli • Potentially lethal • Chances increase with degree of elevation of op site. • Dx: change in heart rate, murmur, decreased in exp CO 2, cardiac dysrythmias, change in heart sounds generated by a parasternal Dopppler. • TEE most sensitive for detection (0. 015 ml/kg/air) • Gasp breath may be first indicator • Decreased Pa 02, et. CO 2, increased et. N
Surgical Positioning Sitting • Complications – Postural hypotension – Air emboli • Potentially lethal • Chances increase with degree of elevation of op site. • Dx: change in heart rate, murmur, decreased in exp CO 2, cardiac dysrythmias, change in heart sounds generated by a parasternal Dopppler. • TEE most sensitive for detection (0. 015 ml/kg/air) • Gasp breath may be first indicator • Decreased Pa 02, et. CO 2, increased et. N
 Surgical Positioning Sitting • Complications – Ocular compression – Pneumocephalus – Edema of face, head, and neck due to prolonged neck flexion resulting in venous and lymphatic obstruction. – Sciatic nerve injury • Bended knees without flexion of the hips • Foot drop is clinical manifestation
Surgical Positioning Sitting • Complications – Ocular compression – Pneumocephalus – Edema of face, head, and neck due to prolonged neck flexion resulting in venous and lymphatic obstruction. – Sciatic nerve injury • Bended knees without flexion of the hips • Foot drop is clinical manifestation
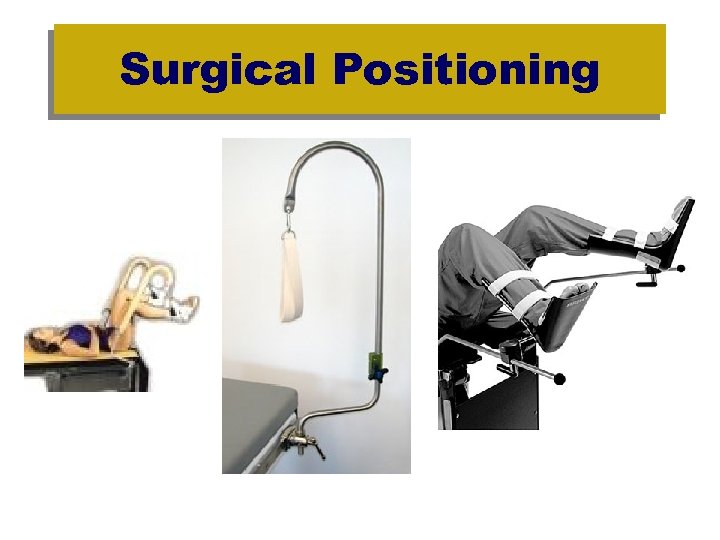
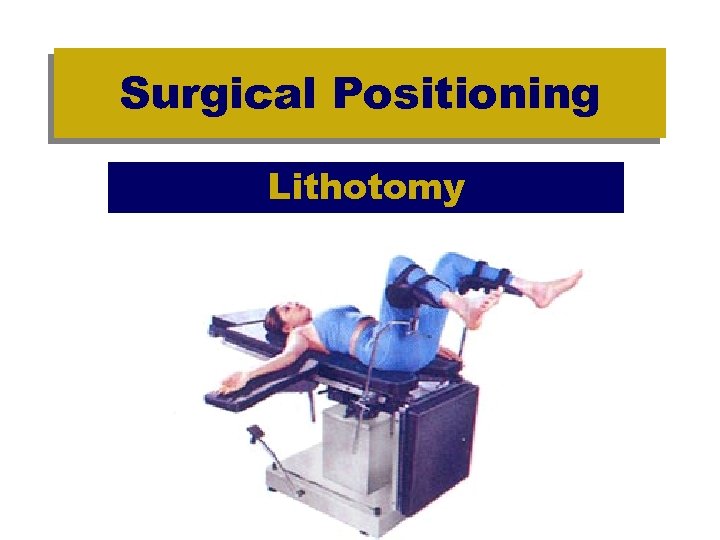 Surgical Positioning Lithotomy
Surgical Positioning Lithotomy
 Surgical Positioning Lithotomy • Cephalad displacement of the diaphragm. • Principle hazards: – Common peroneal- foot drop – Femoral- decreased or absent knee jerk – Saphenous– Obturator-inability to adduct leg & diminished sensation over medial side of the thigh – Sciatic nerve- weakness of all skeletal muscles below the knee • Both legs should be elevated & flexed at same time to avoid stretching of peripheral nerves • Thighs should be no more than 90 o
Surgical Positioning Lithotomy • Cephalad displacement of the diaphragm. • Principle hazards: – Common peroneal- foot drop – Femoral- decreased or absent knee jerk – Saphenous– Obturator-inability to adduct leg & diminished sensation over medial side of the thigh – Sciatic nerve- weakness of all skeletal muscles below the knee • Both legs should be elevated & flexed at same time to avoid stretching of peripheral nerves • Thighs should be no more than 90 o
 AANA Scope and Standards for Nurse Anesthesia Practice Standard V Nurse anesthetists should “monitor and assess patient positioning and protective measures at frequent intervals. ” Failure to follow professional standards and guidelines may result in positioning injuries and liability.
AANA Scope and Standards for Nurse Anesthesia Practice Standard V Nurse anesthetists should “monitor and assess patient positioning and protective measures at frequent intervals. ” Failure to follow professional standards and guidelines may result in positioning injuries and liability.
 LIABILITY EXAMPLES Pommier vs Savoy Memorial Hospital 55 y. o female w/fractured hip 2 hr 20 min surgery Developed peroneal palsy post-op Protective and monitoring measures were not taken nor documented. No prior injury present. Conclusion at trial – injury would not have occurred had there not been negligence – res ipsa loquitur.
LIABILITY EXAMPLES Pommier vs Savoy Memorial Hospital 55 y. o female w/fractured hip 2 hr 20 min surgery Developed peroneal palsy post-op Protective and monitoring measures were not taken nor documented. No prior injury present. Conclusion at trial – injury would not have occurred had there not been negligence – res ipsa loquitur.
 Shahine vs. Louisiana State University Medical Center, 680 So. 2 d 1352 (La. App. , 1996) • "#6 table with safety strap in place 2" above knees supine with bean bag underneath patient post induction & catheter insertion into the left side, with right side up, per __M. D. & __M. D, - auxiliary roll in place (1000 cc bag IV fluid wrapped in muslin cover) - held in place per surgeons until bean bag deflated with suction - pillow placed under right leg with left leg bent slightly - U drape in place per surgeons prep - left arm extended on padded arm board right arm placed on mayo tray that is padded. " Protective and monitoring measures were taken and documented. Brachial plexus injury reported postop. No prior injury present. Conclusion at trial – injury was a risk of the procedure however personnel
Shahine vs. Louisiana State University Medical Center, 680 So. 2 d 1352 (La. App. , 1996) • "#6 table with safety strap in place 2" above knees supine with bean bag underneath patient post induction & catheter insertion into the left side, with right side up, per __M. D. & __M. D, - auxiliary roll in place (1000 cc bag IV fluid wrapped in muslin cover) - held in place per surgeons until bean bag deflated with suction - pillow placed under right leg with left leg bent slightly - U drape in place per surgeons prep - left arm extended on padded arm board right arm placed on mayo tray that is padded. " Protective and monitoring measures were taken and documented. Brachial plexus injury reported postop. No prior injury present. Conclusion at trial – injury was a risk of the procedure however personnel
 ASA Practice Advisory – Sets a legal standard of care LINK to Advisory in the Course Outline Page
ASA Practice Advisory – Sets a legal standard of care LINK to Advisory in the Course Outline Page
 Upper extremity positioning • Arm abduction should be limited to 90° in supine patients; patients who are positioned prone may tolerate arm abduction greater than 90° • Arms should be positioned to decrease pressure on the postcondylar groove of the humerus (ulnar groove). • When arms are tucked at the side, a neutral forearm position is recommended. When arms are abducted on armboards, either supination or a neutral forearm position is acceptable • Prolonged pressure on the radial nerve in the spiral groove of the humerus should be avoided • Extension of the elbow beyond a comfortable range may stretch the median nerve
Upper extremity positioning • Arm abduction should be limited to 90° in supine patients; patients who are positioned prone may tolerate arm abduction greater than 90° • Arms should be positioned to decrease pressure on the postcondylar groove of the humerus (ulnar groove). • When arms are tucked at the side, a neutral forearm position is recommended. When arms are abducted on armboards, either supination or a neutral forearm position is acceptable • Prolonged pressure on the radial nerve in the spiral groove of the humerus should be avoided • Extension of the elbow beyond a comfortable range may stretch the median nerve
 Lower extremity positioning • Lithotomy positions that stretch the hamstring muscle group beyond a comfortable range may stretch the sciatic nerve • Prolonged pressure on the peroneal nerve at the fibular head should be avoided • Neither extension nor flexion of the hip within normal range of motion increases the risk of femoral neuropathy
Lower extremity positioning • Lithotomy positions that stretch the hamstring muscle group beyond a comfortable range may stretch the sciatic nerve • Prolonged pressure on the peroneal nerve at the fibular head should be avoided • Neither extension nor flexion of the hip within normal range of motion increases the risk of femoral neuropathy
 Protective padding • Padded armboards may decrease the risk of upper extremity neuropathy • The use of chest rolls in laterally positioned patients may decrease the risk of upper extremity neuropathies • Padding at the elbow and at the fibular head may decrease the risk of upper and lower extremity neuropathies, respectively Equipment • Properly functioning automated blood pressure cuffs on the upper arms do not affect the risk of upper extremity neuropathies • Shoulder braces in steep head-down positions may increase the risk of brachial plexus neuropathies
Protective padding • Padded armboards may decrease the risk of upper extremity neuropathy • The use of chest rolls in laterally positioned patients may decrease the risk of upper extremity neuropathies • Padding at the elbow and at the fibular head may decrease the risk of upper and lower extremity neuropathies, respectively Equipment • Properly functioning automated blood pressure cuffs on the upper arms do not affect the risk of upper extremity neuropathies • Shoulder braces in steep head-down positions may increase the risk of brachial plexus neuropathies
 Postoperative assessment • A simple postoperative assessment of extremity nerve function may lead to early recognition of peripheral neuropathies Documentation • Charting specific positioning actions during the care of patients may result in improvements of care by (1) helping practitioners focus attention on relevant aspects of patient positioning; (2) providing information that continuous improvement processes can use to lead to refinements in patient care; and (3) provide medicolegal defense
Postoperative assessment • A simple postoperative assessment of extremity nerve function may lead to early recognition of peripheral neuropathies Documentation • Charting specific positioning actions during the care of patients may result in improvements of care by (1) helping practitioners focus attention on relevant aspects of patient positioning; (2) providing information that continuous improvement processes can use to lead to refinements in patient care; and (3) provide medicolegal defense
 Surgical Positioning Checklist
Surgical Positioning Checklist
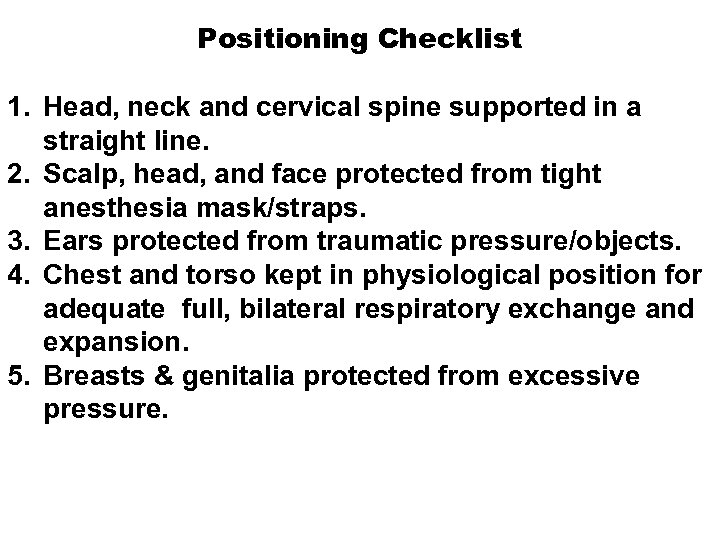 Positioning Checklist 1. Head, neck and cervical spine supported in a straight line. 2. Scalp, head, and face protected from tight anesthesia mask/straps. 3. Ears protected from traumatic pressure/objects. 4. Chest and torso kept in physiological position for adequate full, bilateral respiratory exchange and expansion. 5. Breasts & genitalia protected from excessive pressure.
Positioning Checklist 1. Head, neck and cervical spine supported in a straight line. 2. Scalp, head, and face protected from tight anesthesia mask/straps. 3. Ears protected from traumatic pressure/objects. 4. Chest and torso kept in physiological position for adequate full, bilateral respiratory exchange and expansion. 5. Breasts & genitalia protected from excessive pressure.
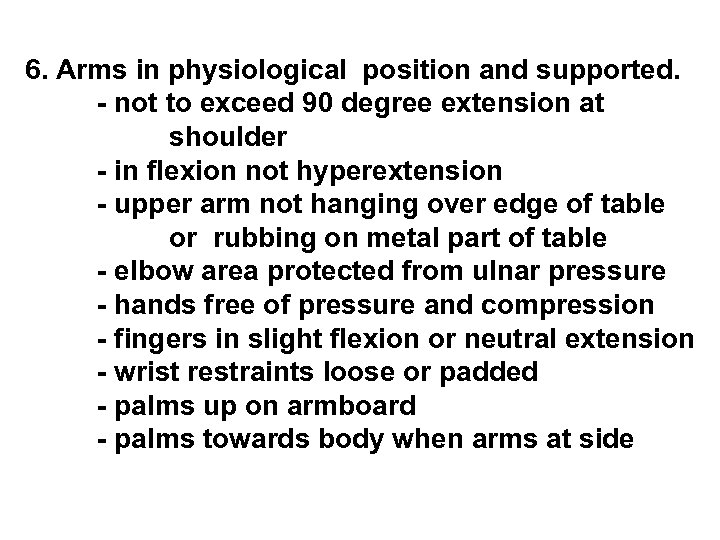 6. Arms in physiological position and supported. - not to exceed 90 degree extension at shoulder - in flexion not hyperextension - upper arm not hanging over edge of table or rubbing on metal part of table - elbow area protected from ulnar pressure - hands free of pressure and compression - fingers in slight flexion or neutral extension - wrist restraints loose or padded - palms up on armboard - palms towards body when arms at side
6. Arms in physiological position and supported. - not to exceed 90 degree extension at shoulder - in flexion not hyperextension - upper arm not hanging over edge of table or rubbing on metal part of table - elbow area protected from ulnar pressure - hands free of pressure and compression - fingers in slight flexion or neutral extension - wrist restraints loose or padded - palms up on armboard - palms towards body when arms at side
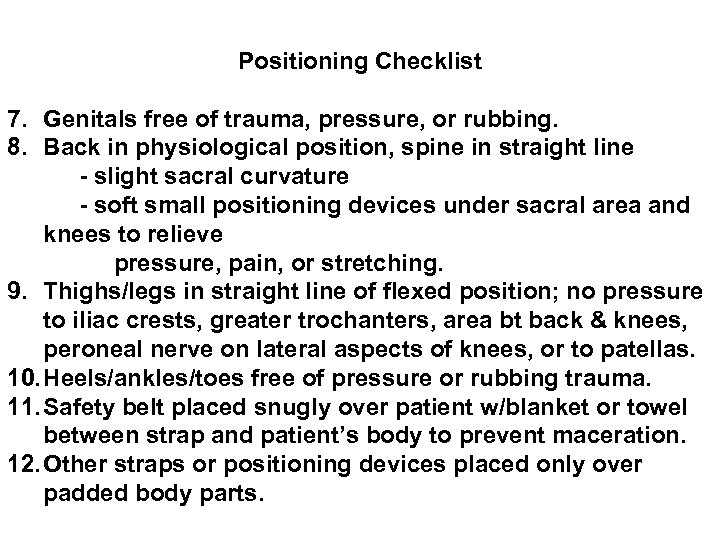 Positioning Checklist 7. Genitals free of trauma, pressure, or rubbing. 8. Back in physiological position, spine in straight line - slight sacral curvature - soft small positioning devices under sacral area and knees to relieve pressure, pain, or stretching. 9. Thighs/legs in straight line of flexed position; no pressure to iliac crests, greater trochanters, area bt back & knees, peroneal nerve on lateral aspects of knees, or to patellas. 10. Heels/ankles/toes free of pressure or rubbing trauma. 11. Safety belt placed snugly over patient w/blanket or towel between strap and patient’s body to prevent maceration. 12. Other straps or positioning devices placed only over padded body parts.
Positioning Checklist 7. Genitals free of trauma, pressure, or rubbing. 8. Back in physiological position, spine in straight line - slight sacral curvature - soft small positioning devices under sacral area and knees to relieve pressure, pain, or stretching. 9. Thighs/legs in straight line of flexed position; no pressure to iliac crests, greater trochanters, area bt back & knees, peroneal nerve on lateral aspects of knees, or to patellas. 10. Heels/ankles/toes free of pressure or rubbing trauma. 11. Safety belt placed snugly over patient w/blanket or towel between strap and patient’s body to prevent maceration. 12. Other straps or positioning devices placed only over padded body parts.
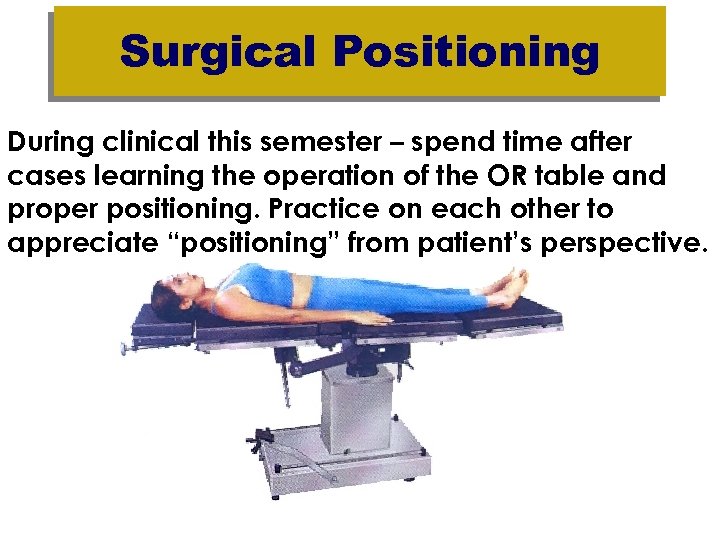 Surgical Positioning During clinical this semester – spend time after cases learning the operation of the OR table and proper positioning. Practice on each other to appreciate “positioning” from patient’s perspective.
Surgical Positioning During clinical this semester – spend time after cases learning the operation of the OR table and proper positioning. Practice on each other to appreciate “positioning” from patient’s perspective.


