5fb2259ff08da7b59a63274a7b5d0250.ppt
- Количество слайдов: 85
Surgical management of Pediatric Brain Tumors JIE MA Dept. of Pediatric Neurosurgery Xin Hua Hospital School of Medicine Shanghai Jiao. Tong University
Ped- Brain Tumor General Information Brain tumor is most common cause of cancer death in Child Second most common of cancer Many tumor are treated with surgery Either alone or combination with RT or Chem Recent advance in survival and decrease morbidity Full understanding of biology and primary treat modality Common feature Unique feature in each tumor Summarize some of these features and treatment modality
儿童脑肿瘤 发病率:小儿恶性肿瘤第二位 5~8岁是高发期 影响因素多 某些与基因突变、缺失有关 胶质瘤: 17 p基因缺失 高分化胶质瘤: 9 p基因缺失 脑膜瘤 10号染色体部分缺失 髓母细胞瘤 17 p缺失
病理类型 胶质细胞瘤(Glioma) 星形细胞瘤 室管膜瘤 多形性成胶质细胞瘤 原始神经外胚层细胞瘤(PNET) 胚胎残余组织形成的颅内肿瘤 其他
临床表现 颅高压症状 头痛、呕吐、视乳头水肿 、前囟饱满、颅缝裂开 局灶性症状和体征 肢体瘫痪 癫痫发作 共济失调 视力减退、视野缺损 下丘脑和垂体功能障碍
Goal of Surgery Interventation • Tissue diagnosis • Re-establishment CSF pathway • Tumor debulking • Complete tumor resection
Primitive neuroectodermal tumors Cerebellum-PNET– Medulloblastoma Supratentorial- PNETs Obstructive hydrocephalus symptoms and signs PNETs- Seisures rare Total resection for MB Adjuvant therapy(Chem + RT)>2 y Poor Prognosis < 2 y Supratentorial Metastatic presence 1 cm Residual tumor ramain
Ependymoma Slow growing Hydrocephalus sign and symptoms Malignant – anaplastic ependymoma Commonly locate posterior fossa as PNET-MB Five-year survival 50 -70%- Tatal removal 20%------residual disease Poor prognosis <3 y Subtotal removal Metastatic diseases Presence tumor in posterior fossa Anaplasia
Choroid Plexus tumors Bengin choroid plexus papillomas Total removal: 5 -year survival rate is 100% Gross total removal: 40% Choroid plexus carcinoma Poor prognosis: • Brain invasion • Necrosis • Mitoses • Reduced immunoreactivity of S 100 protein
Conclusion Many Ped brain tumor can be treated effictively Surgery can cure Pilocytic astrocytoma Craniopharyngioma Choroid plexus tumor Surgery+RT+Chem. T cure PNET Ependymoma Future treatment
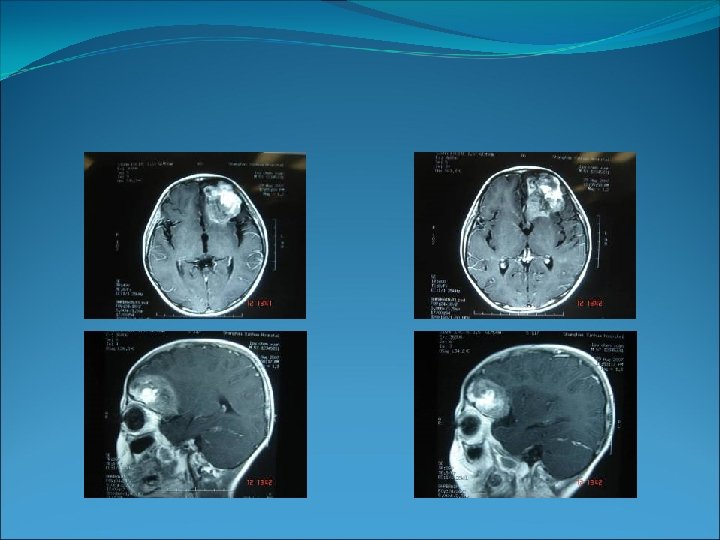
Meningioma 8 years old boy His right upper and lower extremities had lower strength for 1 month. Babinski sign negative. Further physical, neurologic, and ophthalmologic examination disclosed no abnormalities.
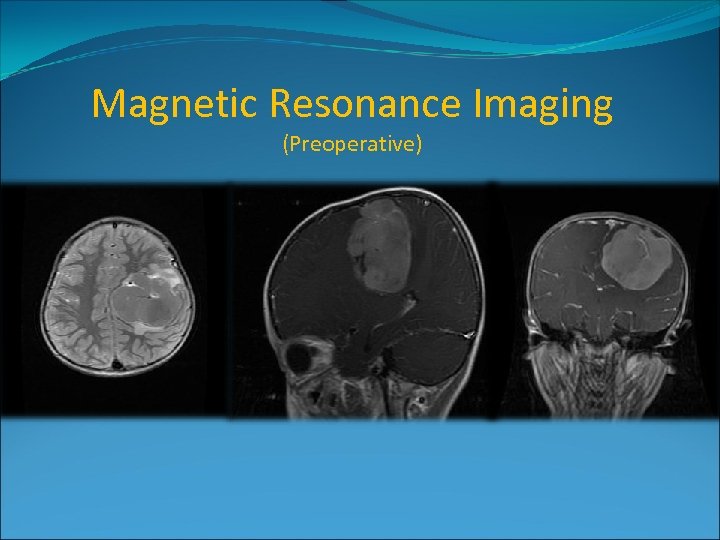
Magnetic Resonance Imaging (Preoperative)
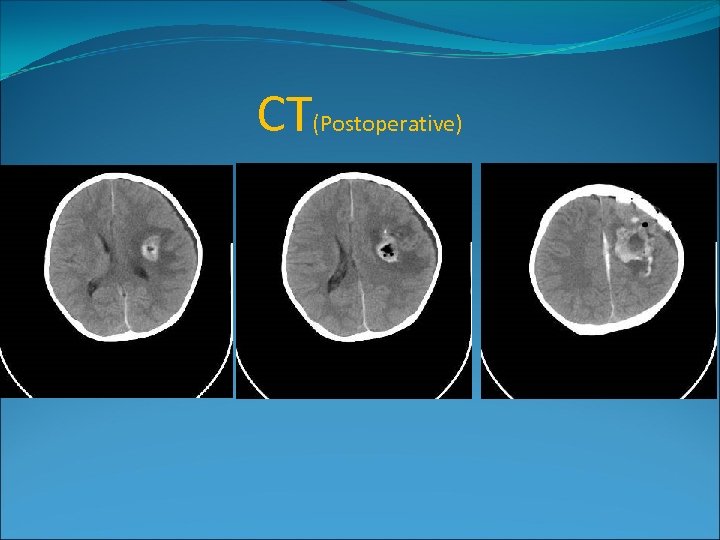
CT(Postoperative)
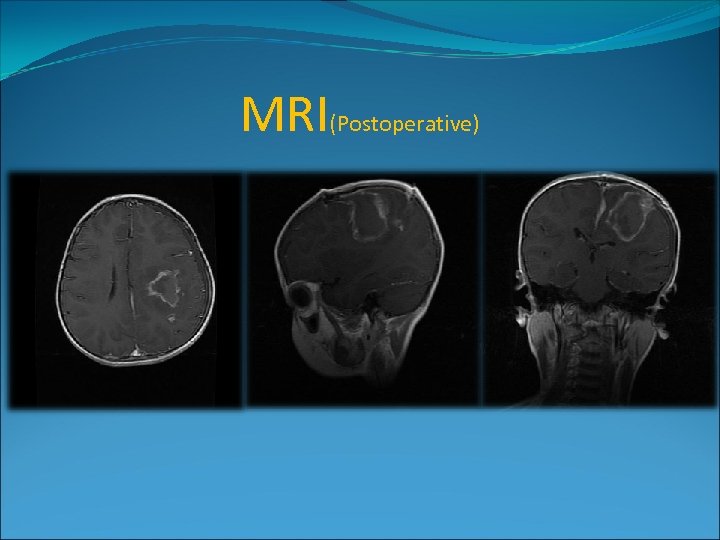
MRI(Postoperative)

肿瘤药物敏感试验
l 11 -year-old boy l. Epilepsy for 6 months l. Right extremities anaesthetic 20 days ago l. Strength of right extremities was IV-V l. Right babinski sign positive l. Poor ability of memory for 2 weeks l. Abnormal EEG l. No family history l. Depakine and Oxcarbazepine for half a year
The patient (preoperative)

MRI (07. 11. 30)
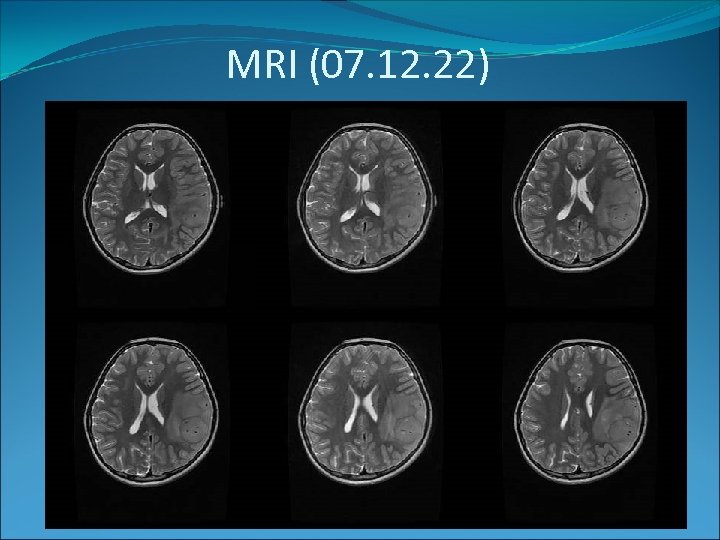
MRI (07. 12. 22)
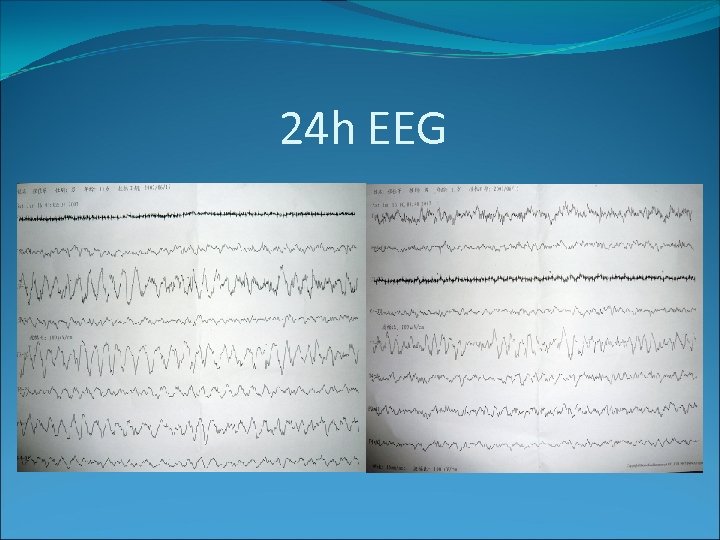
24 h EEG
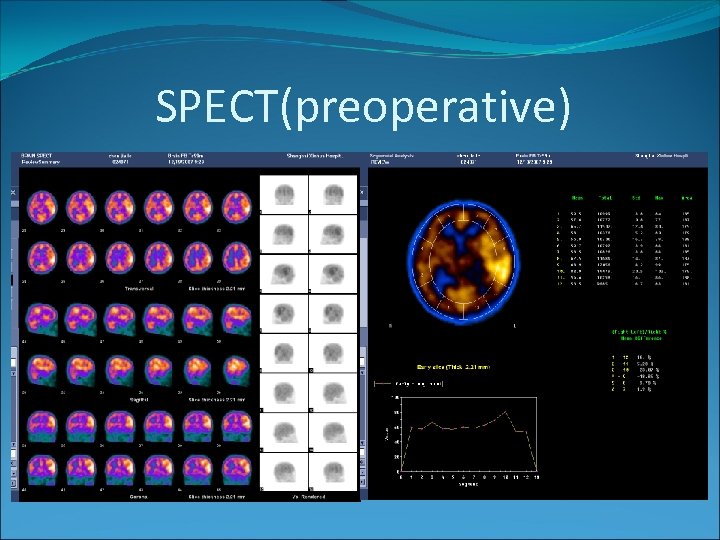
SPECT(preoperative)
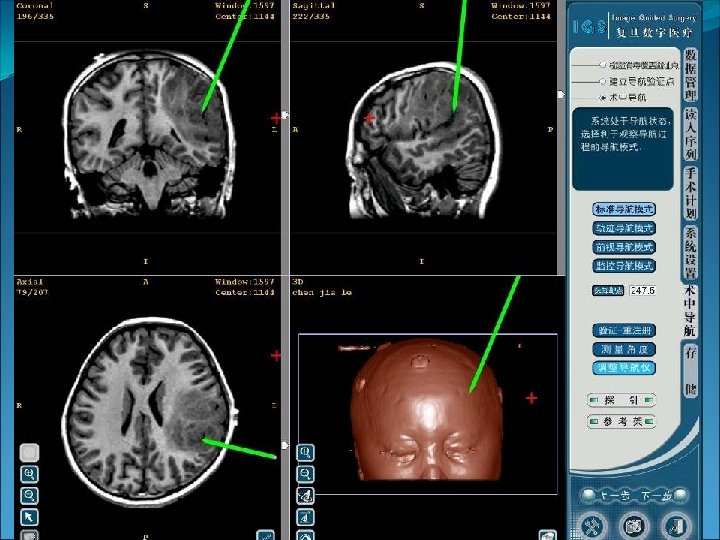
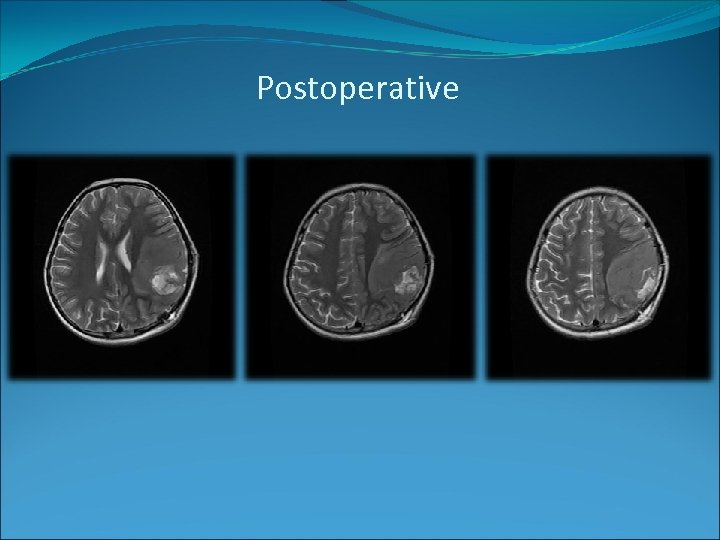
Postoperative
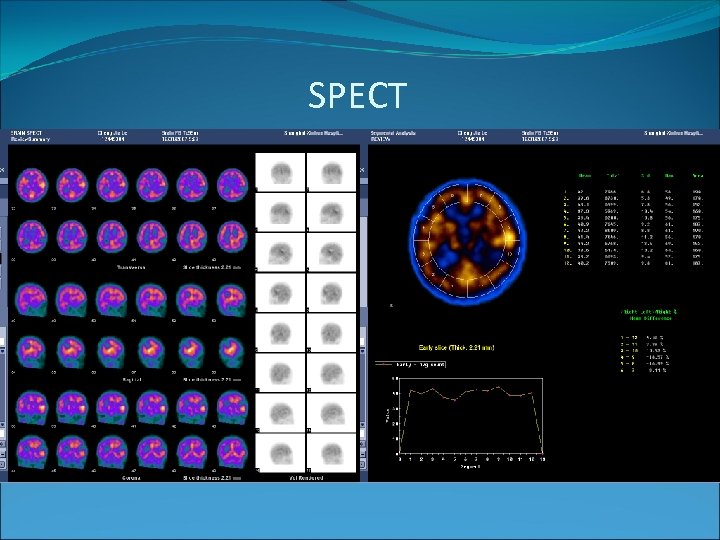
SPECT
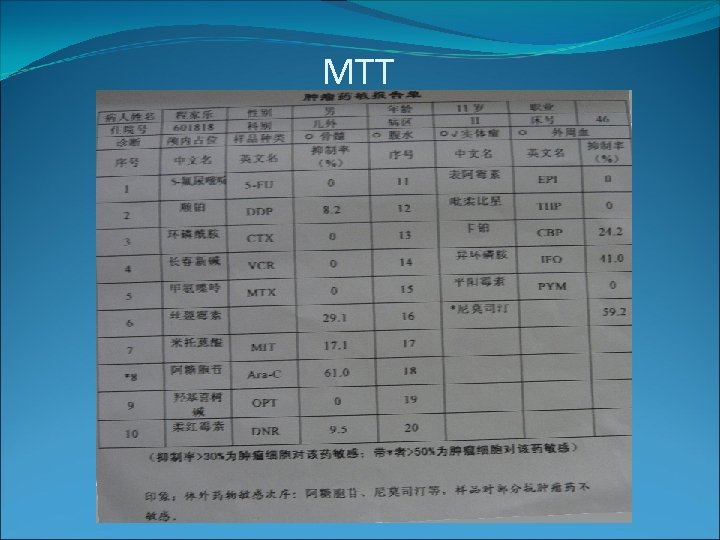
MTT

Dept. of Pediatric Neurosurgery Xin Hua Hospital Affiliated to Shanghai Jiao. Tong University School of Medicine
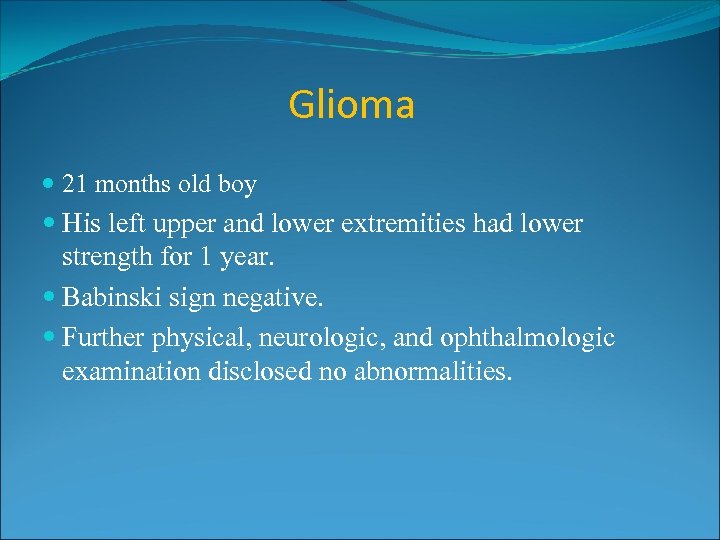
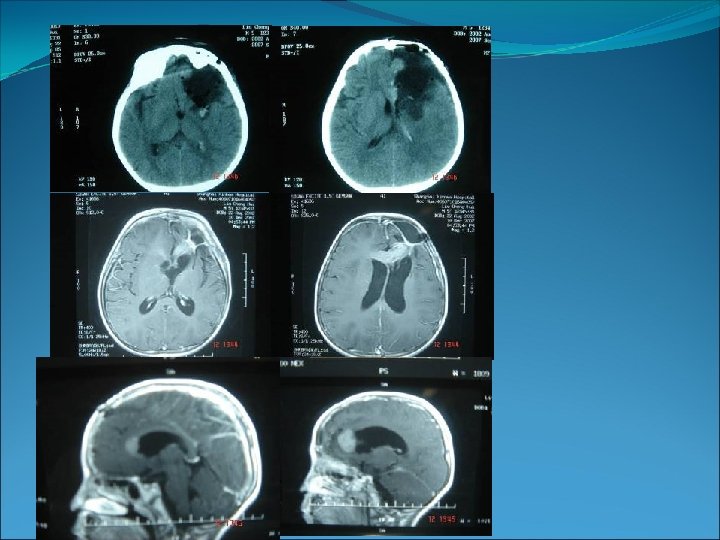
Glioma 21 months old boy His left upper and lower extremities had lower strength for 1 year. Babinski sign negative. Further physical, neurologic, and ophthalmologic examination disclosed no abnormalities.
Magnetic Resonance Imaging (Preoperative)
MRI(Postoperative)
肿瘤药物敏感试验
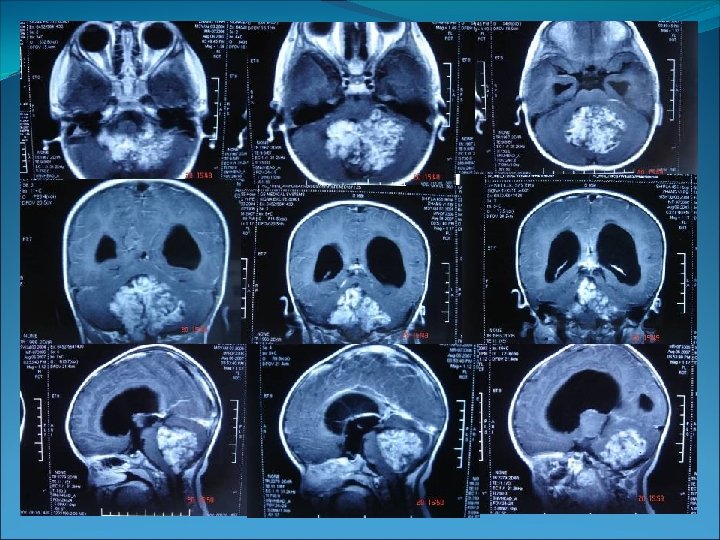
PNET (primitive neuroectodermal tumor) 8 year old boy Polyuria for two years Headache for two weeks Left eye squint to the left two days before admission No family history Others normal
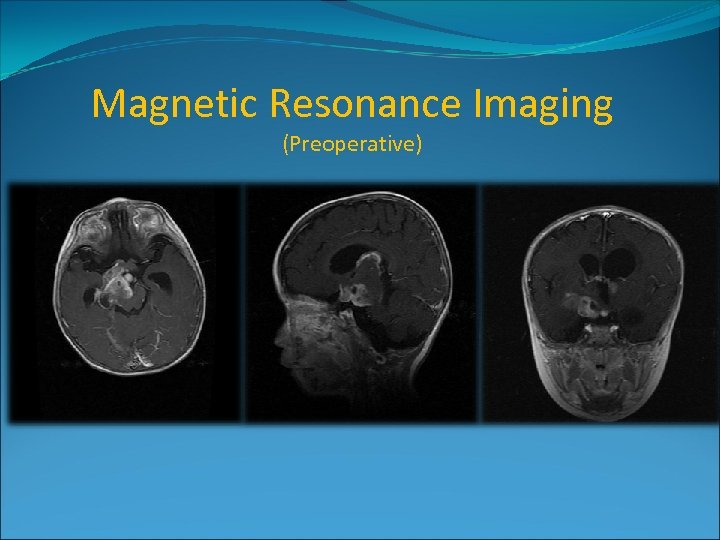
Magnetic Resonance Imaging (Preoperative)
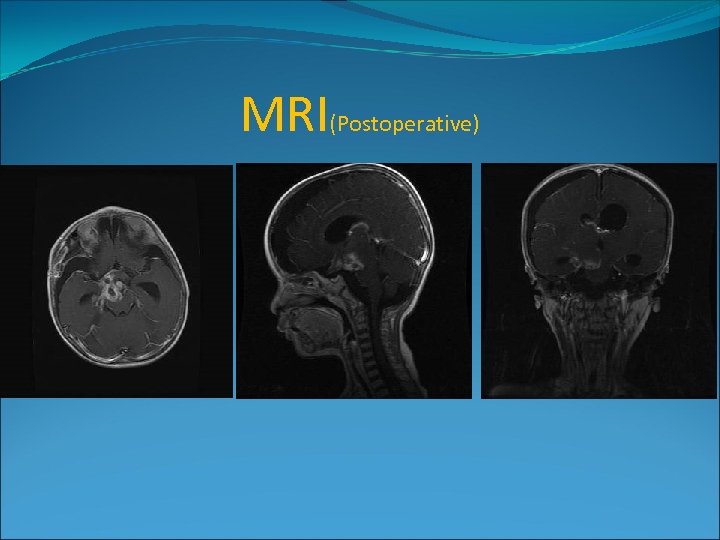
CT(Postoperative)

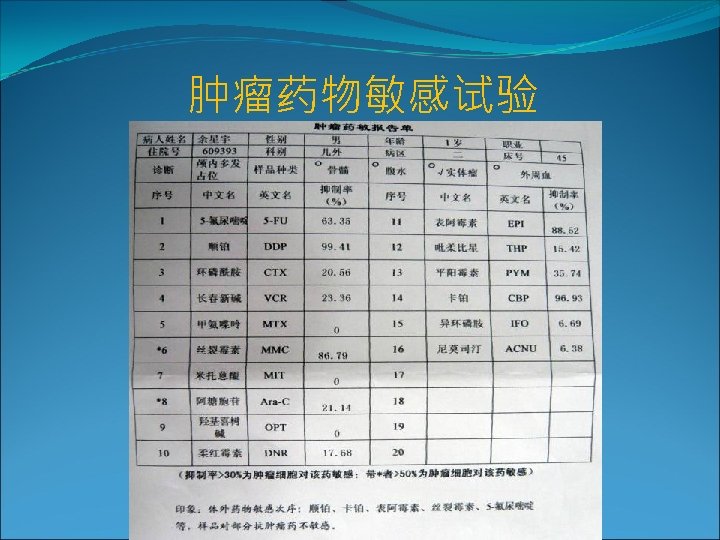
肿瘤药物敏感试验
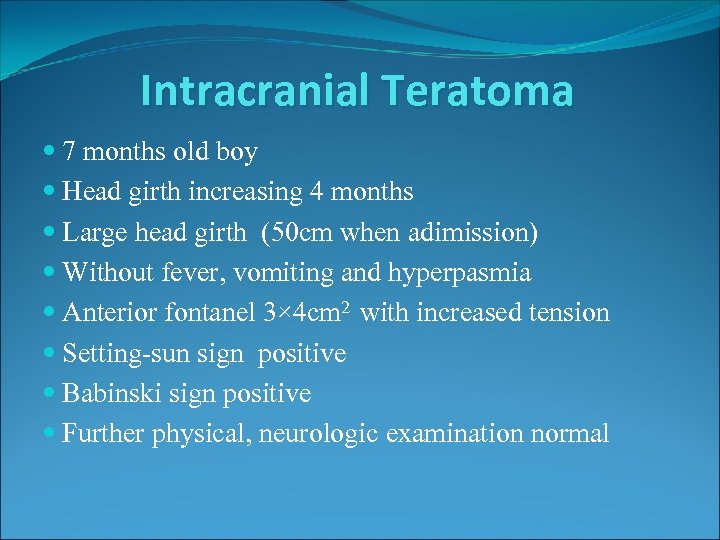
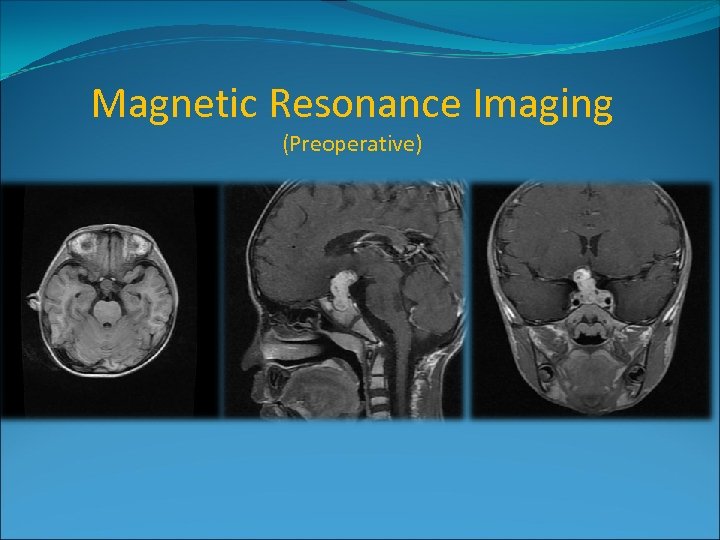
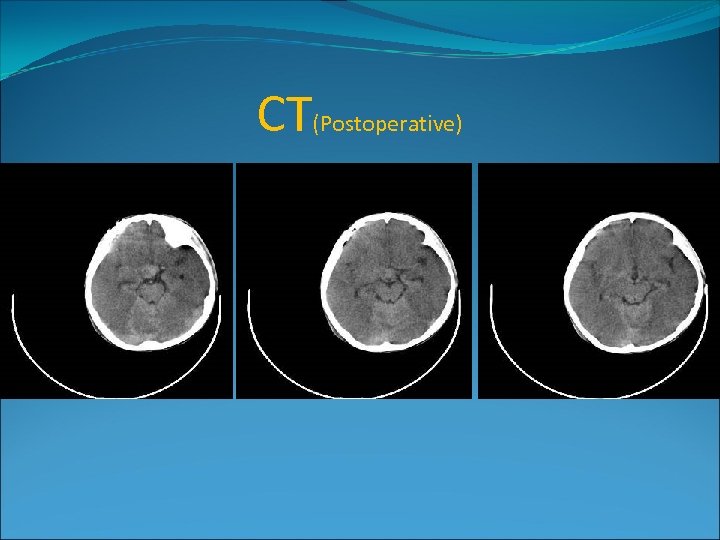
Intracranial Teratoma 7 months old boy Head girth increasing 4 months Large head girth (50 cm when adimission) Without fever, vomiting and hyperpasmia Anterior fontanel 3× 4 cm 2 with increased tension Setting-sun sign positive Babinski sign positive Further physical, neurologic examination normal
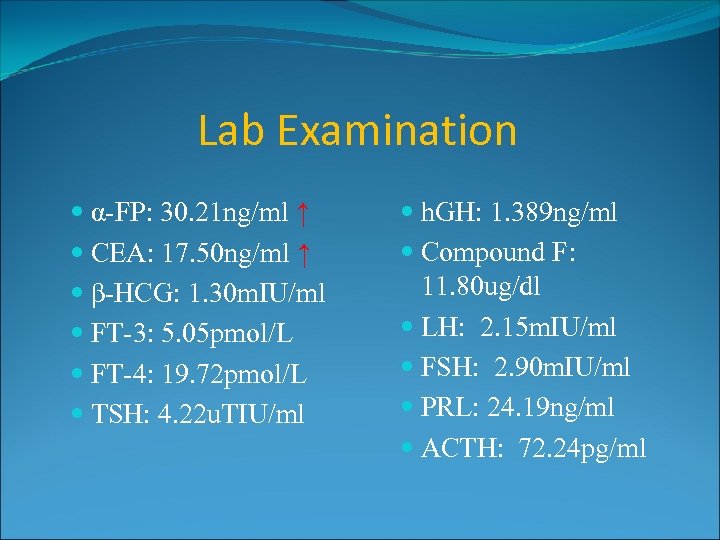
Lab Examination α-FP: 30. 21 ng/ml ↑ CEA: 17. 50 ng/ml ↑ β-HCG: 1. 30 m. IU/ml FT-3: 5. 05 pmol/L FT-4: 19. 72 pmol/L TSH: 4. 22 u. TIU/ml h. GH: 1. 389 ng/ml Compound F: 11. 80 ug/dl LH: 2. 15 m. IU/ml FSH: 2. 90 m. IU/ml PRL: 24. 19 ng/ml ACTH: 72. 24 pg/ml
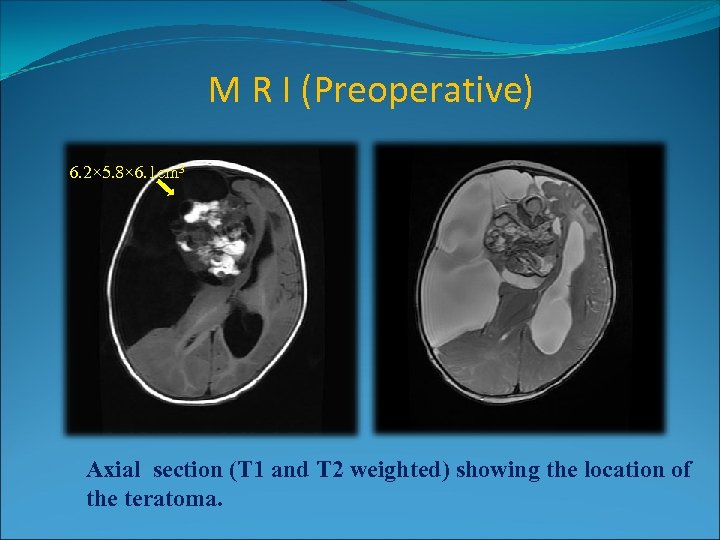
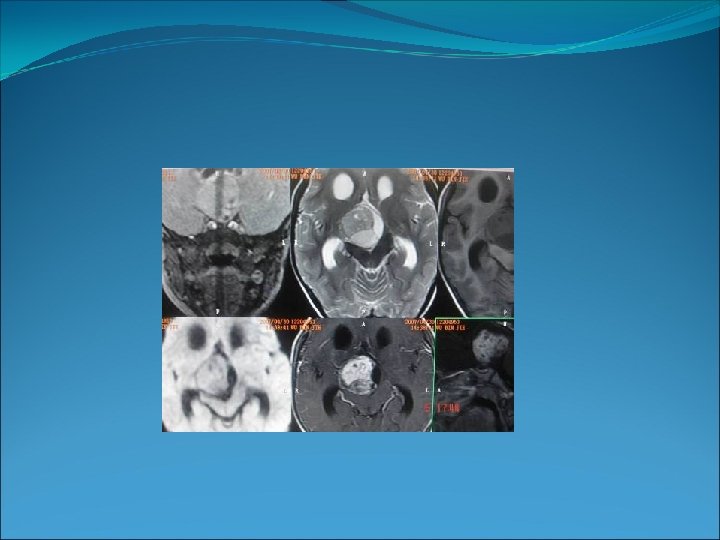
M R I (Preoperative) 6. 2× 5. 8× 6. 1 cm 3 Axial section (T 1 and T 2 weighted) showing the location of the teratoma.
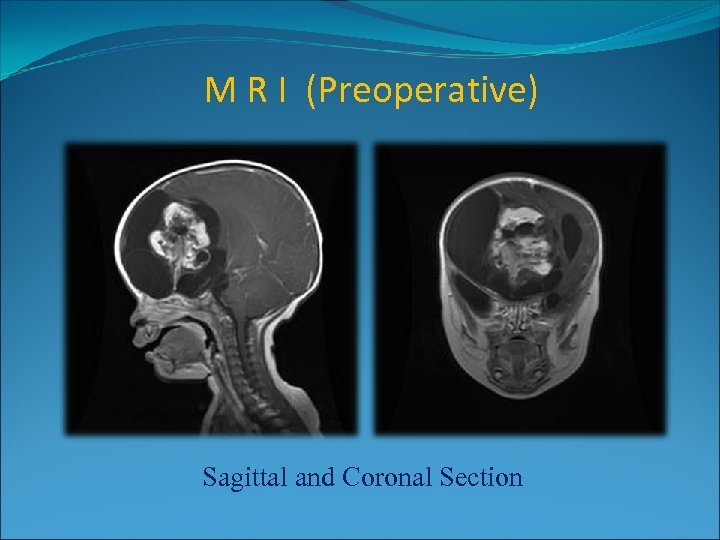
M R I (Preoperative) Sagittal and Coronal Section
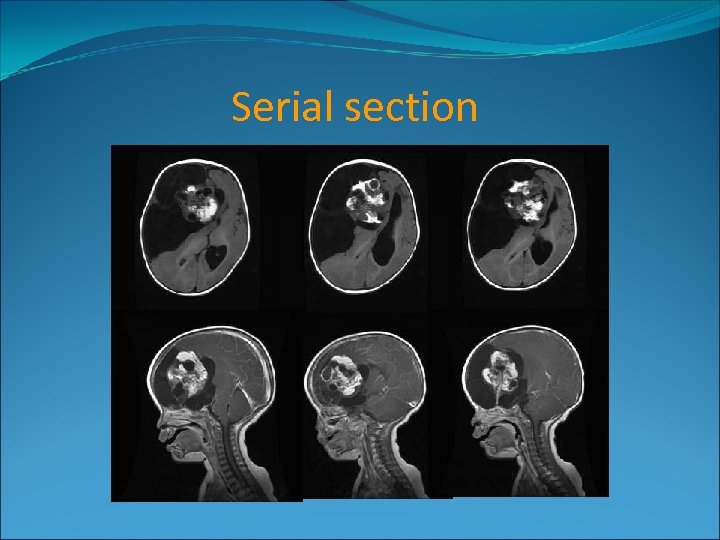
Serial section
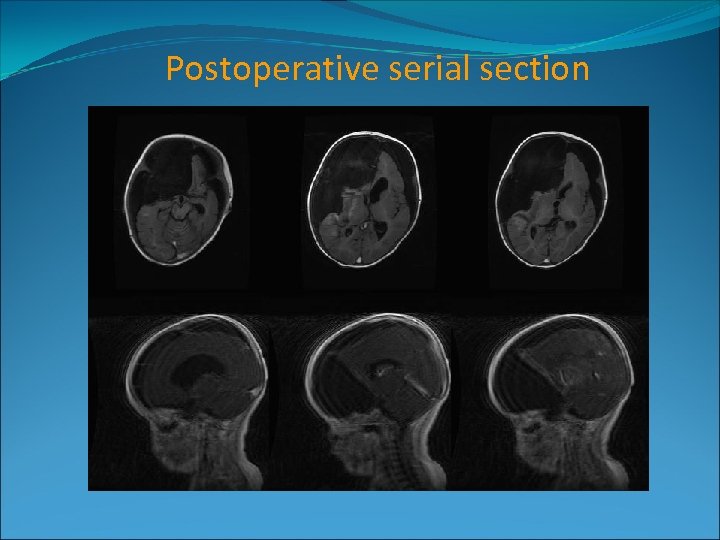
Postoperative serial section
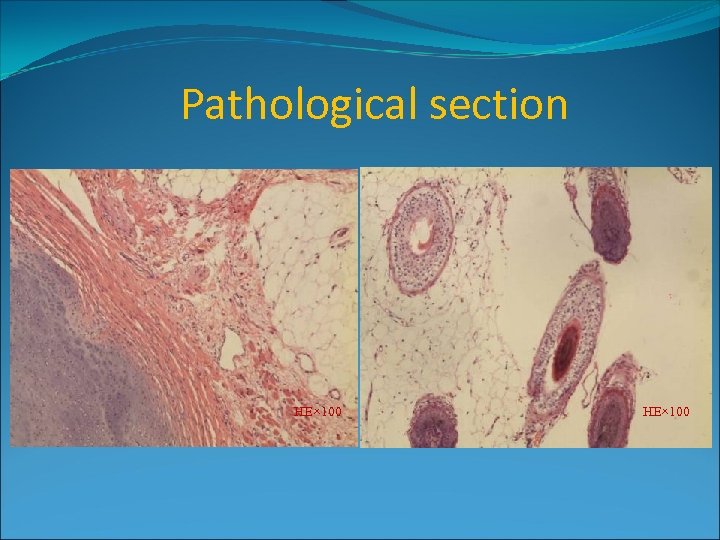
Pathological section HE× 100
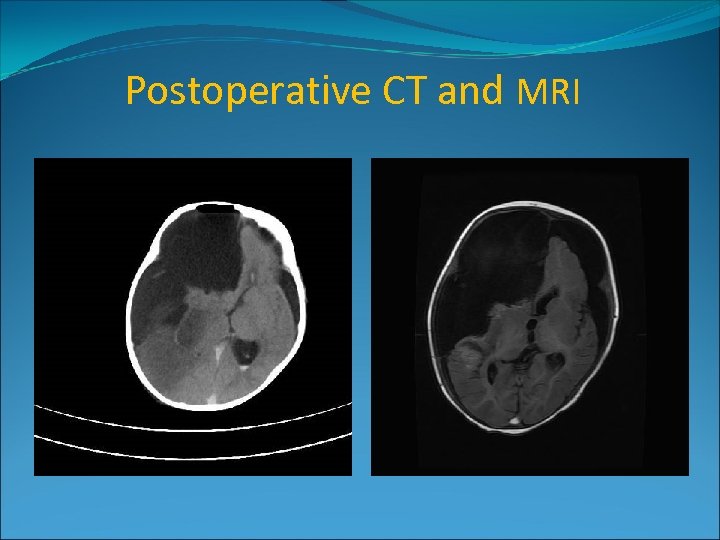
Postoperative CT and MRI
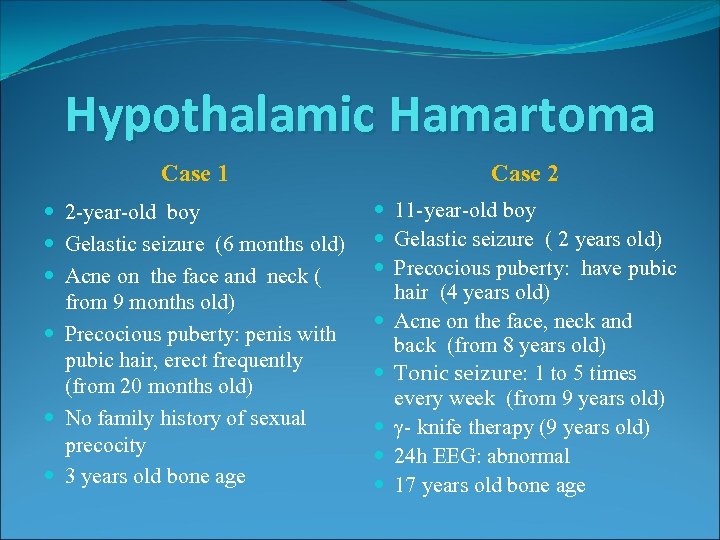
Hypothalamic Hamartoma Case 1 Case 2 2 -year-old boy Gelastic seizure (6 months old) Acne on the face and neck ( from 9 months old) Precocious puberty: penis with pubic hair, erect frequently (from 20 months old) No family history of sexual precocity 3 years old bone age 11 -year-old boy Gelastic seizure ( 2 years old) Precocious puberty: have pubic hair (4 years old) Acne on the face, neck and back (from 8 years old) Tonic seizure: 1 to 5 times every week (from 9 years old) γ- knife therapy (9 years old) 24 h EEG: abnormal 17 years old bone age
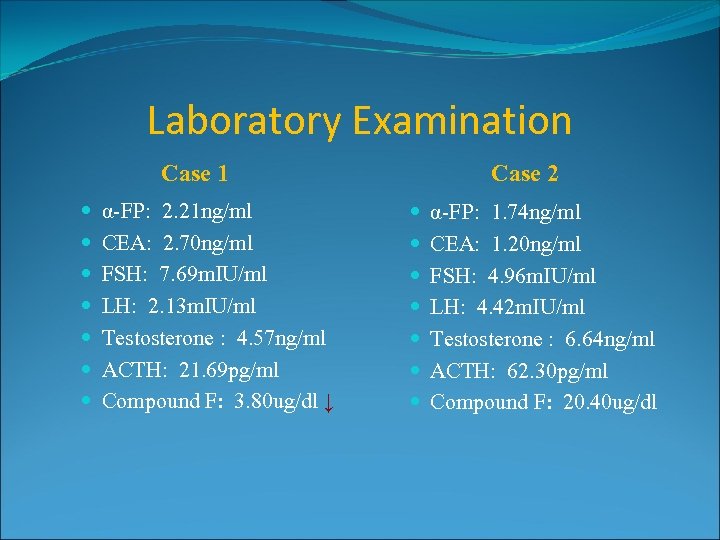
Laboratory Examination Case 1 α-FP: 2. 21 ng/ml CEA: 2. 70 ng/ml FSH: 7. 69 m. IU/ml LH: 2. 13 m. IU/ml Testosterone : 4. 57 ng/ml ACTH: 21. 69 pg/ml Compound F: 3. 80 ug/dl ↓ Case 2 α-FP: 1. 74 ng/ml CEA: 1. 20 ng/ml FSH: 4. 96 m. IU/ml LH: 4. 42 m. IU/ml Testosterone : 6. 64 ng/ml ACTH: 62. 30 pg/ml Compound F: 20. 40 ug/dl
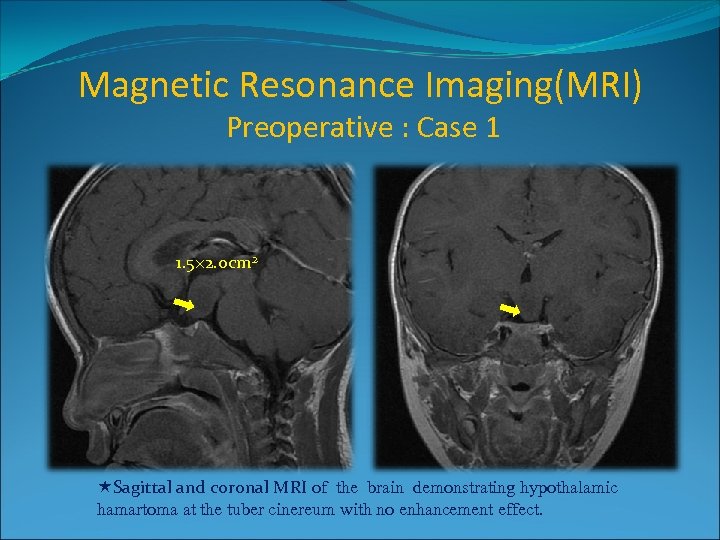
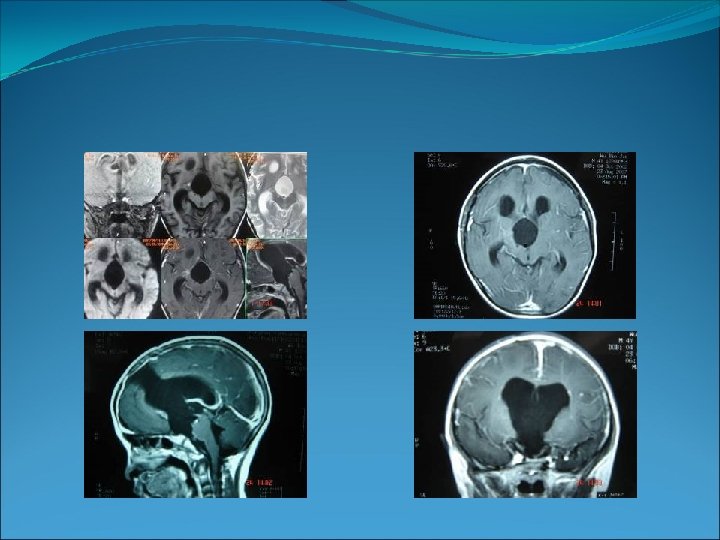
Magnetic Resonance Imaging(MRI) Preoperative : Case 1 1. 5× 2. 0 cm 2 Sagittal and coronal MRI of the brain demonstrating hypothalamic hamartoma at the tuber cinereum with no enhancement effect.
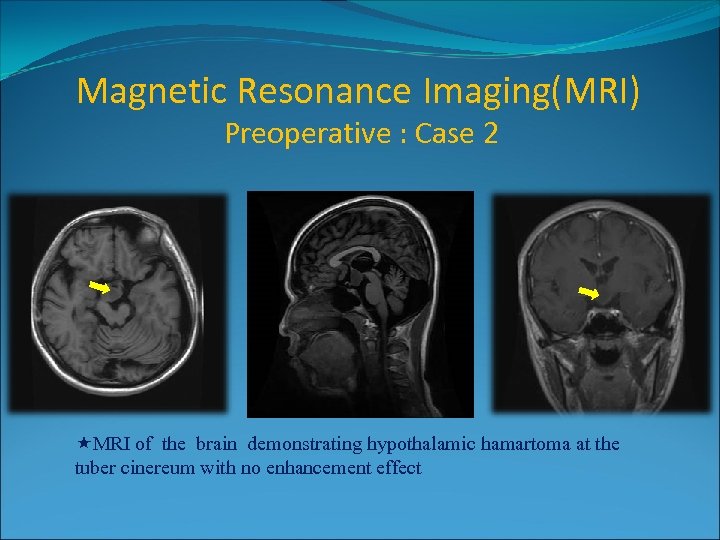
Magnetic Resonance Imaging(MRI) Preoperative : Case 2 2× 3 cm 2 MRI of the brain demonstrating hypothalamic hamartoma at the tuber cinereum with no enhancement effect
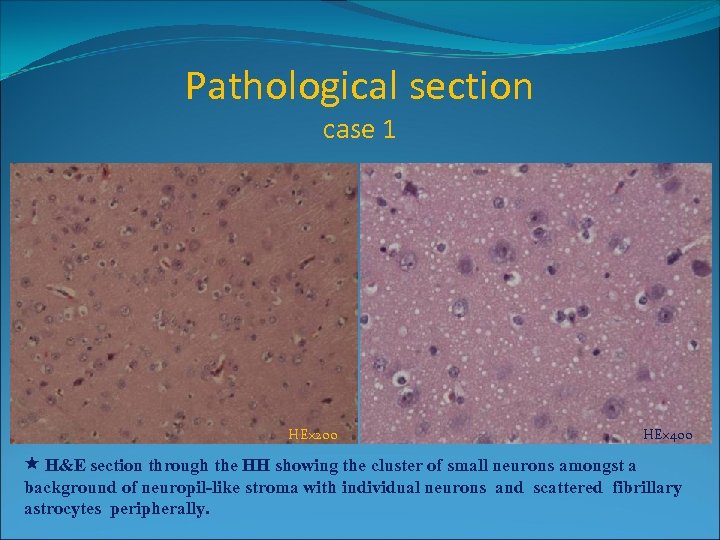
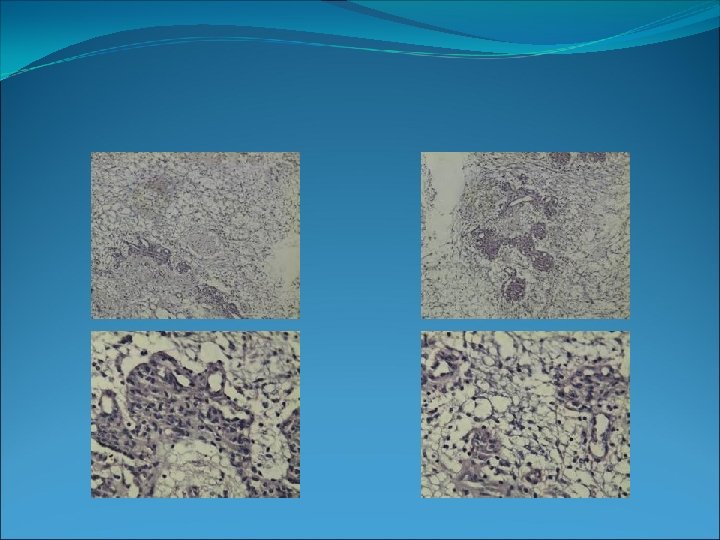
Pathological section case 1 HE× 200 HE× 400 H&E section through the HH showing the cluster of small neurons amongst a background of neuropil-like stroma with individual neurons and scattered fibrillary astrocytes peripherally.
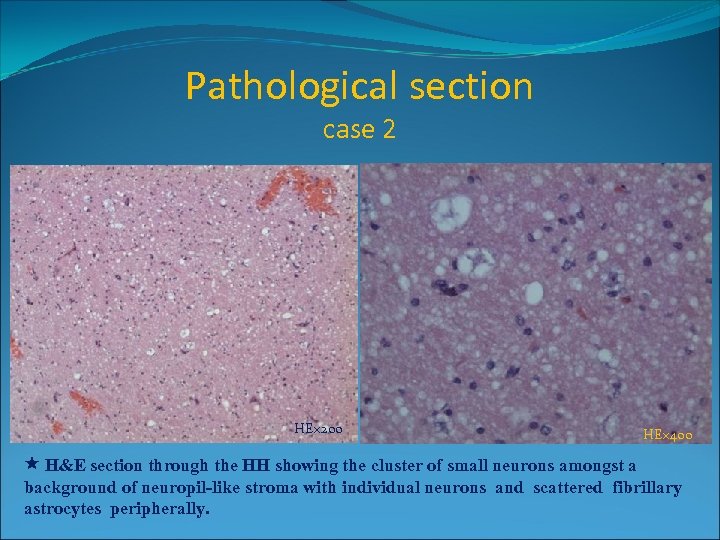
Pathological section case 2 HE× 200 HE× 400 H&E section through the HH showing the cluster of small neurons amongst a background of neuropil-like stroma with individual neurons and scattered fibrillary astrocytes peripherally.
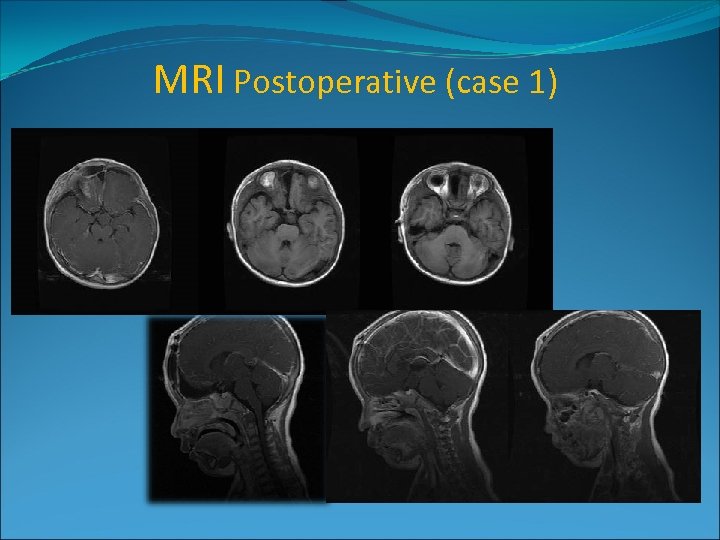
MRI Postoperative (case 1)
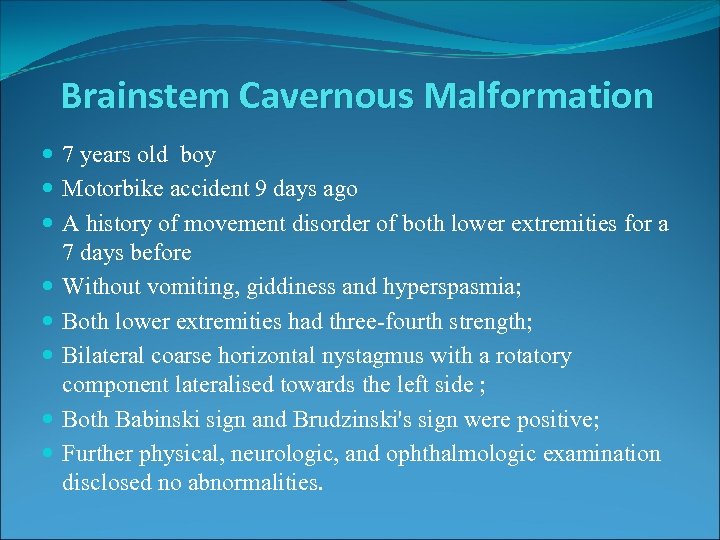
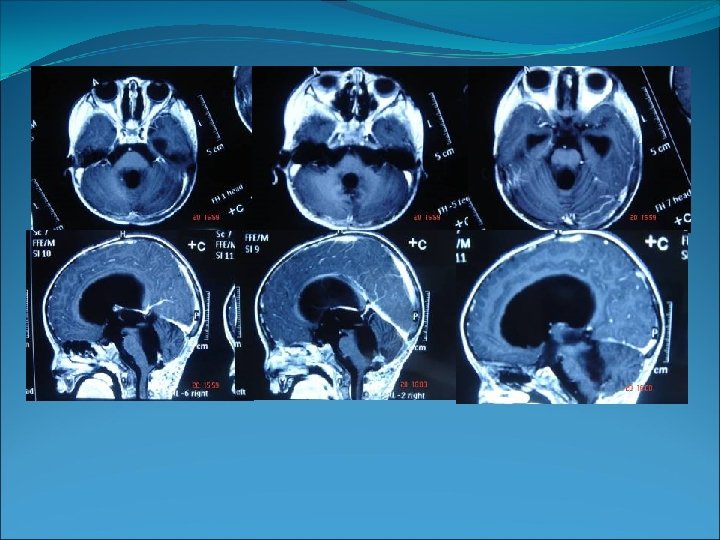
Brainstem Cavernous Malformation 7 years old boy Motorbike accident 9 days ago A history of movement disorder of both lower extremities for a 7 days before Without vomiting, giddiness and hyperspasmia; Both lower extremities had three-fourth strength; Bilateral coarse horizontal nystagmus with a rotatory component lateralised towards the left side ; Both Babinski sign and Brudzinski's sign were positive; Further physical, neurologic, and ophthalmologic examination disclosed no abnormalities.
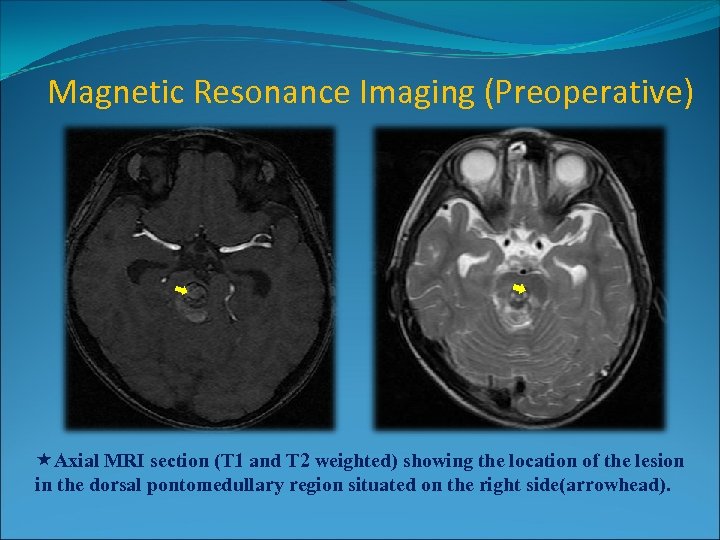
Magnetic Resonance Imaging (Preoperative) Axial MRI section (T 1 and T 2 weighted) showing the location of the lesion in the dorsal pontomedullary region situated on the right side(arrowhead).
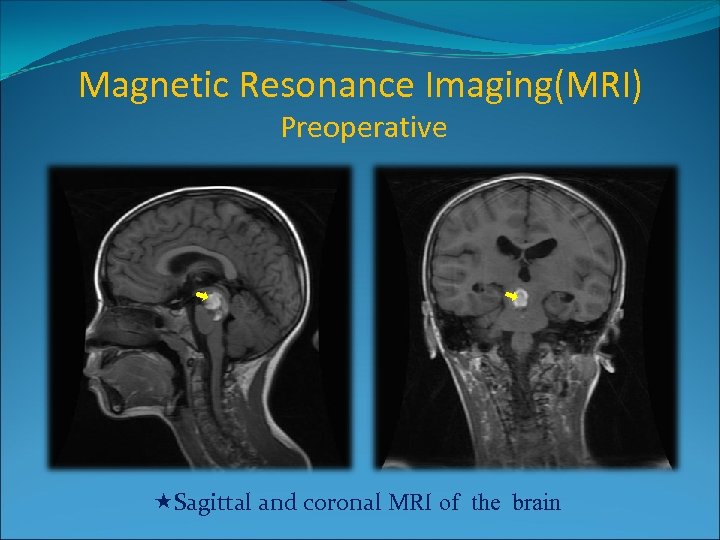
Magnetic Resonance Imaging(MRI) Preoperative Sagittal and coronal MRI of the brain
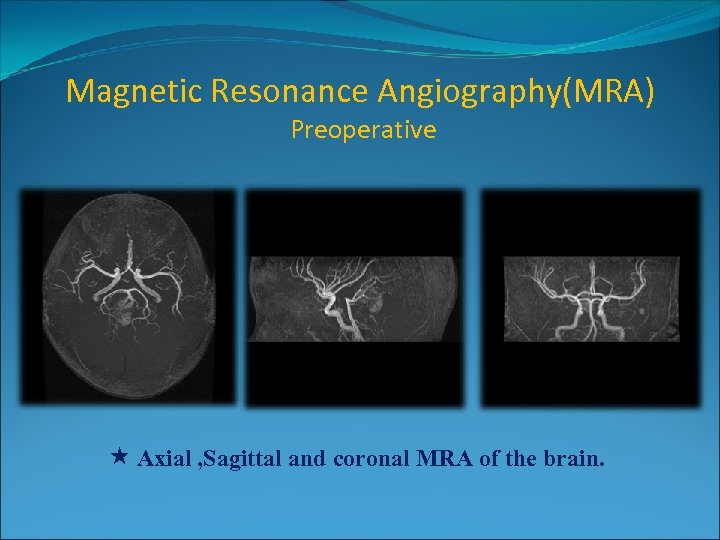
Magnetic Resonance Angiography(MRA) Preoperative Axial , Sagittal and coronal MRA of the brain.
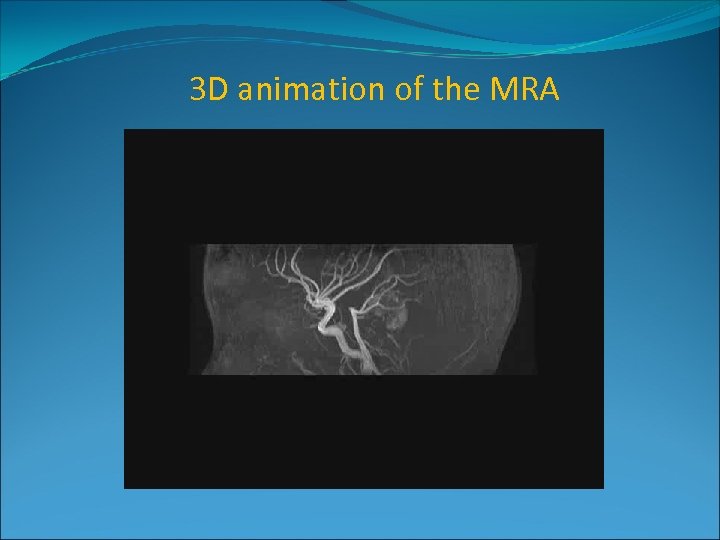
3 D animation of the MRA
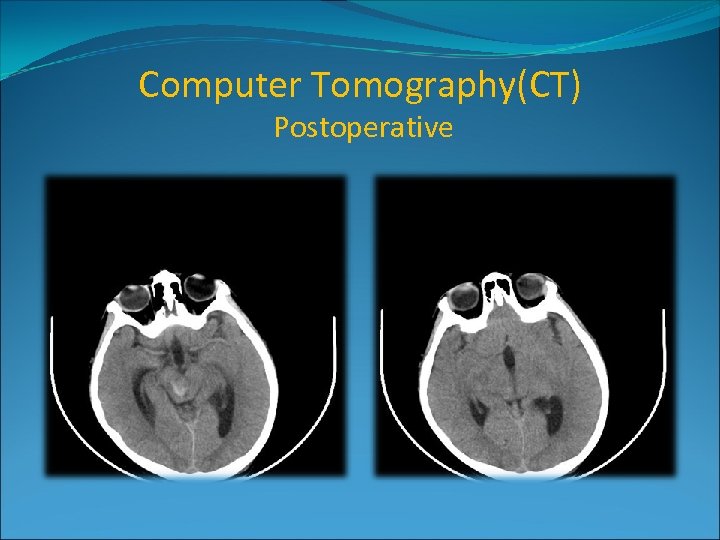
Computer Tomography(CT) Postoperative
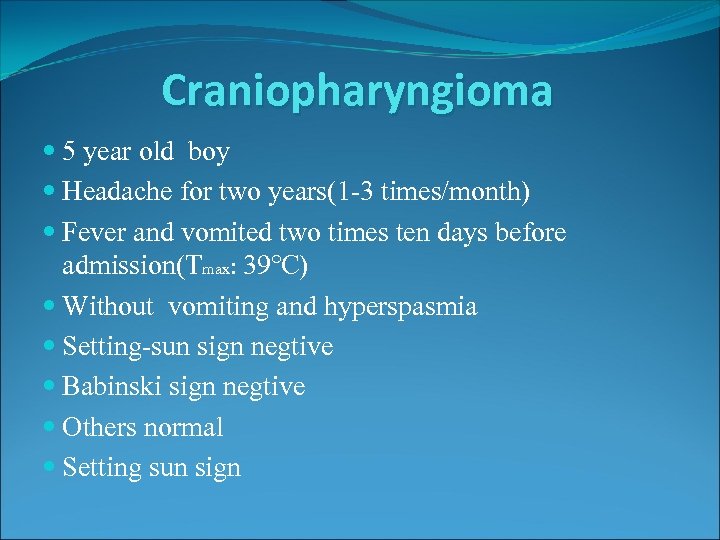
Craniopharyngioma 5 year old boy Headache for two years(1 -3 times/month) Fever and vomited two times ten days before admission(Tmax: 39℃) Without vomiting and hyperspasmia Setting-sun sign negtive Babinski sign negtive Others normal Setting sun sign
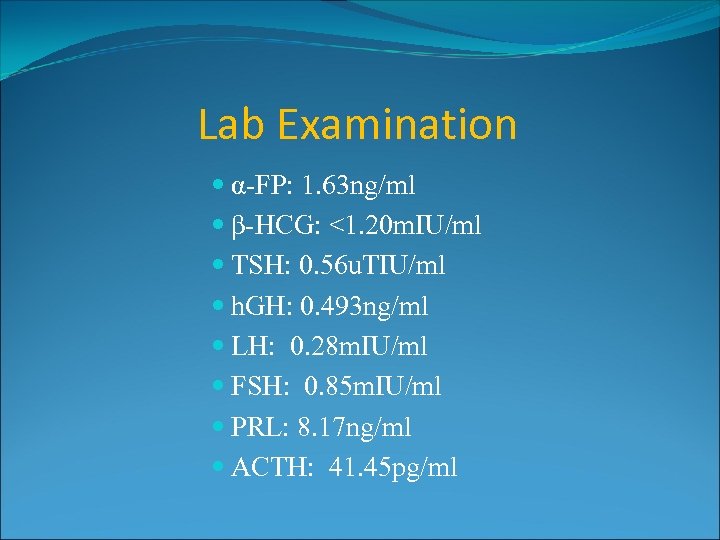
Lab Examination α-FP: 1. 63 ng/ml β-HCG: <1. 20 m. IU/ml TSH: 0. 56 u. TIU/ml h. GH: 0. 493 ng/ml LH: 0. 28 m. IU/ml FSH: 0. 85 m. IU/ml PRL: 8. 17 ng/ml ACTH: 41. 45 pg/ml
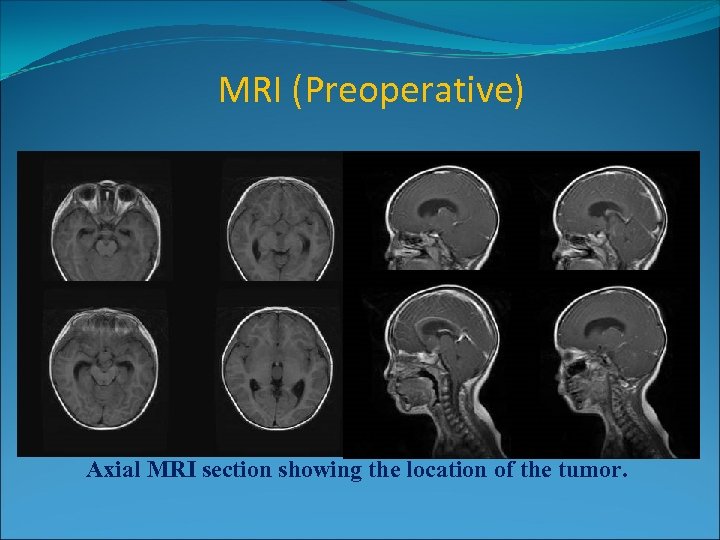
MRI (Preoperative) 3. 8× 1. 8× 2. 4 cm 3 Axial MRI section showing the location of the tumor.
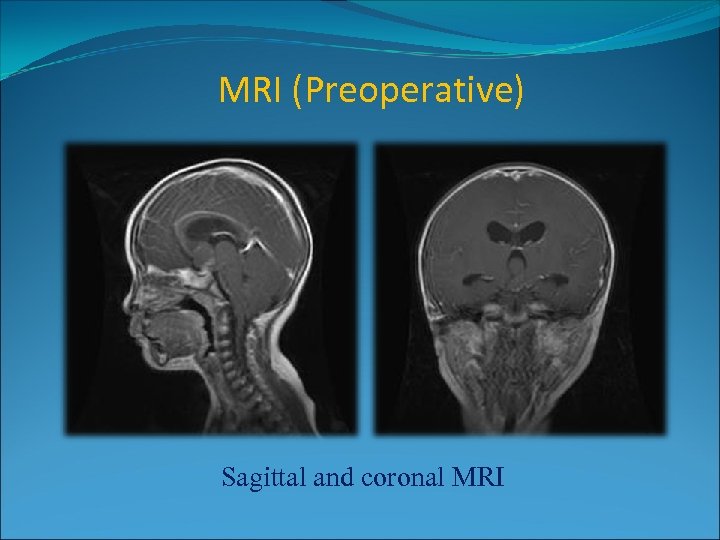
MRI (Preoperative) Sagittal and coronal MRI
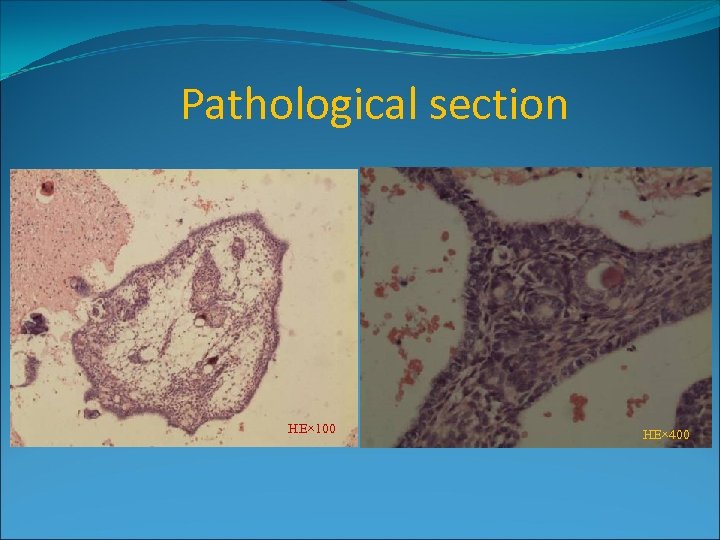
Pathological section HE× 100 HE× 400
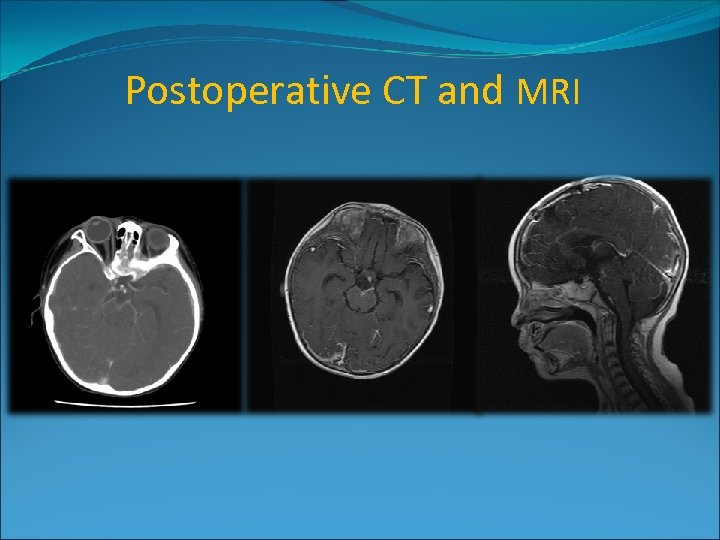
Postoperative CT and MRI
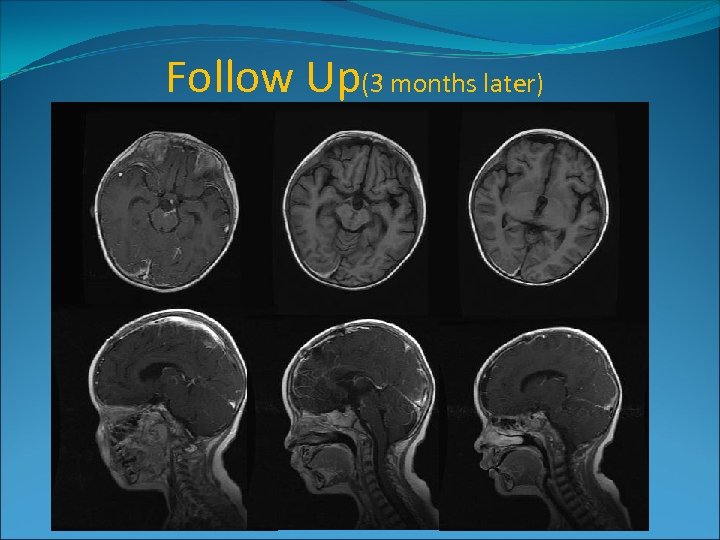
Follow Up(3 months later)
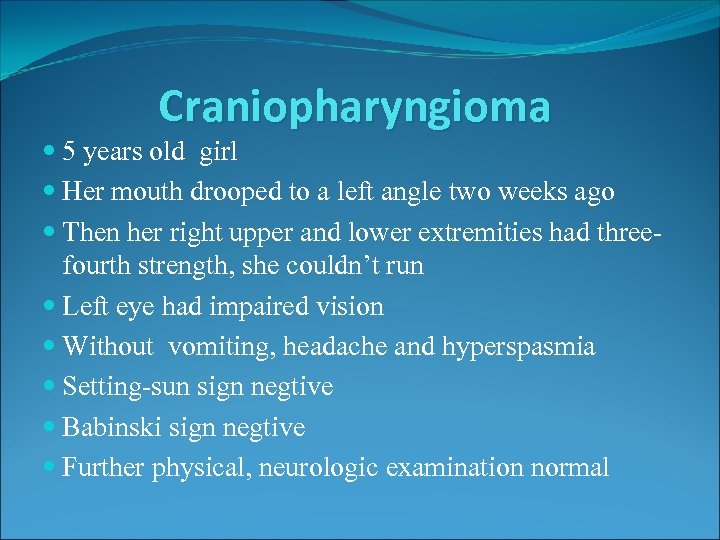
Craniopharyngioma 5 years old girl Her mouth drooped to a left angle two weeks ago Then her right upper and lower extremities had threefourth strength, she couldn’t run Left eye had impaired vision Without vomiting, headache and hyperspasmia Setting-sun sign negtive Babinski sign negtive Further physical, neurologic examination normal
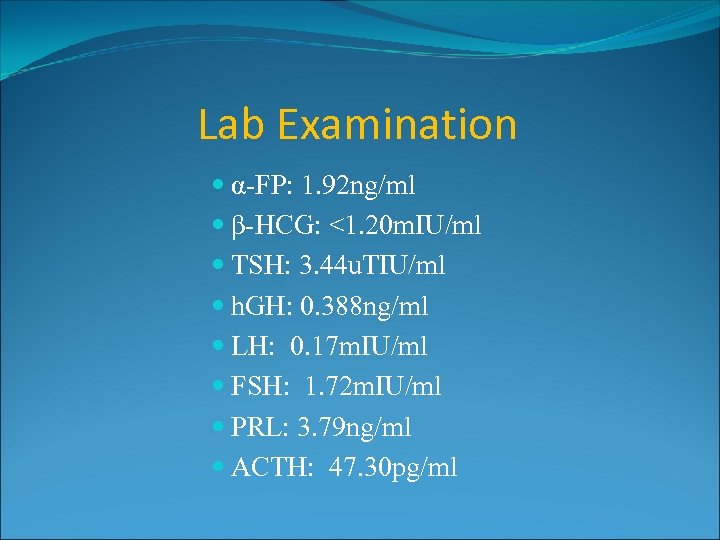
Lab Examination α-FP: 1. 92 ng/ml β-HCG: <1. 20 m. IU/ml TSH: 3. 44 u. TIU/ml h. GH: 0. 388 ng/ml LH: 0. 17 m. IU/ml FSH: 1. 72 m. IU/ml PRL: 3. 79 ng/ml ACTH: 47. 30 pg/ml
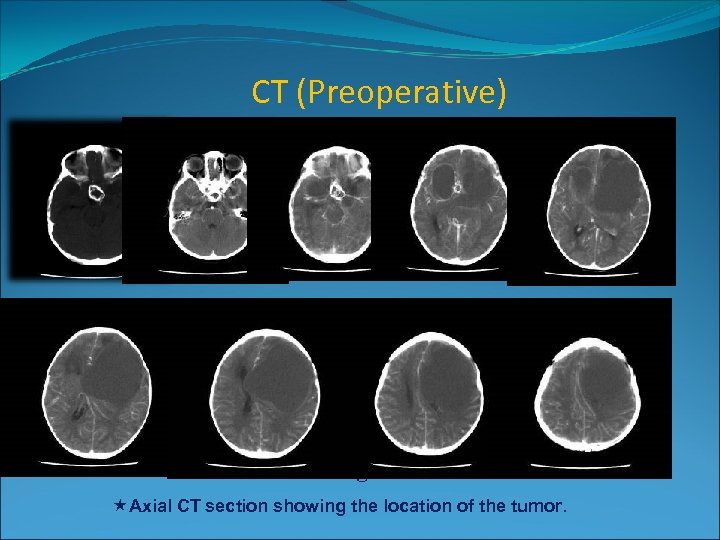
CT (Preoperative) 5× 4× 5 cm 3 Axial CT section showing the location of the tumor.
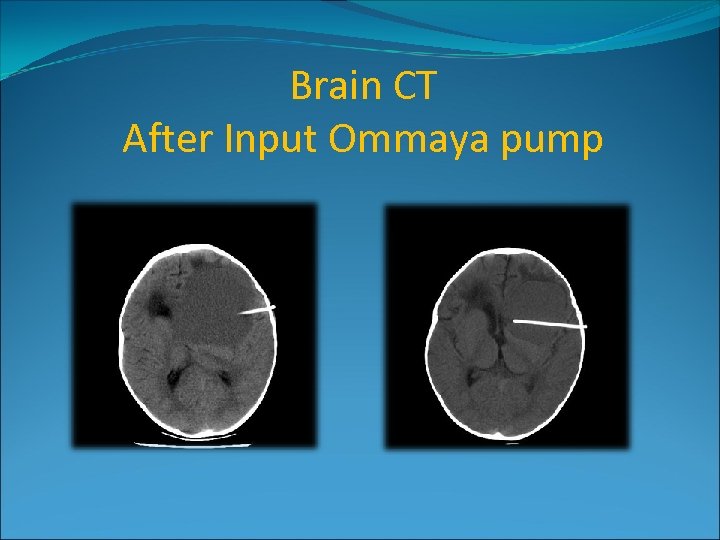
Brain CT After Input Ommaya pump

Pathological section HE× 100
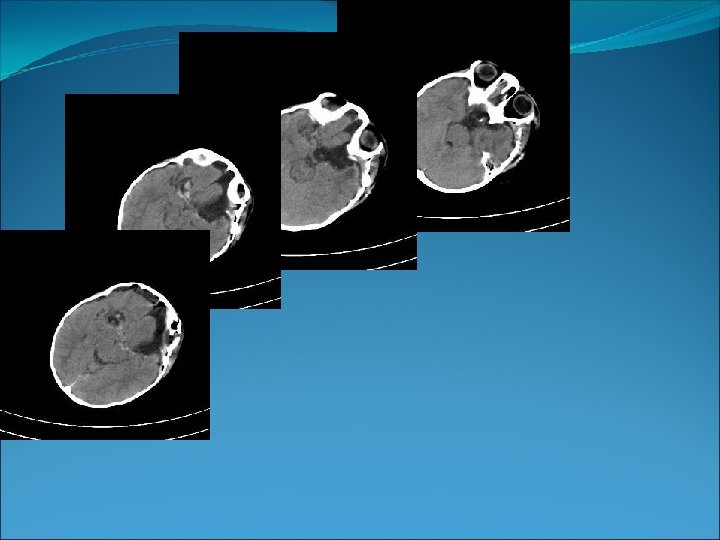
Postoperative CT
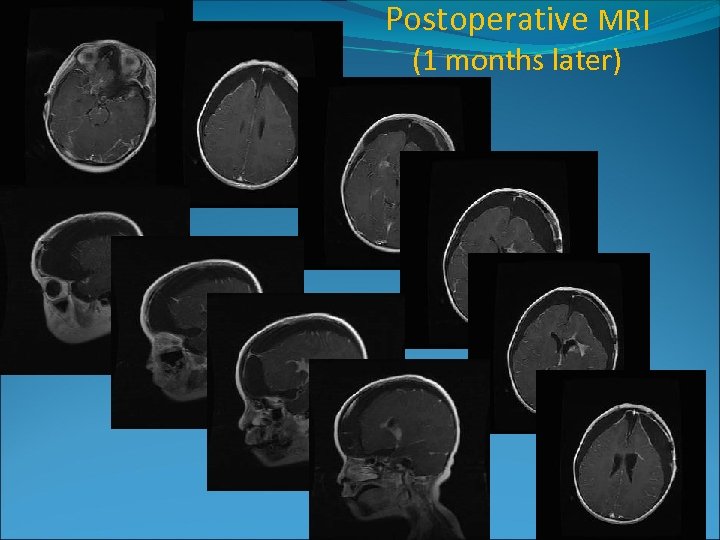
Postoperative MRI (1 months later)
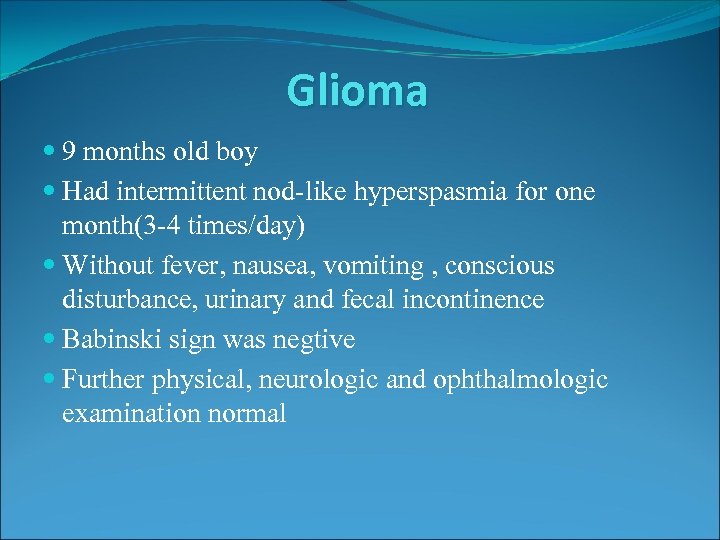
Glioma 9 months old boy Had intermittent nod-like hyperspasmia for one month(3 -4 times/day) Without fever, nausea, vomiting , conscious disturbance, urinary and fecal incontinence Babinski sign was negtive Further physical, neurologic and ophthalmologic examination normal
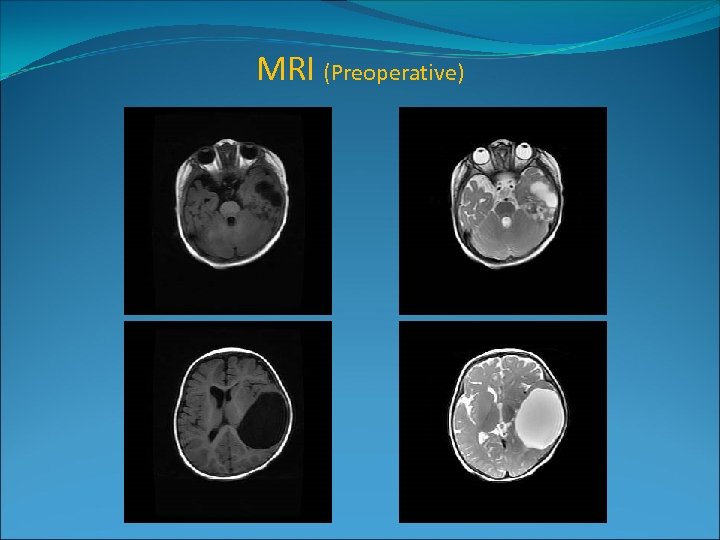
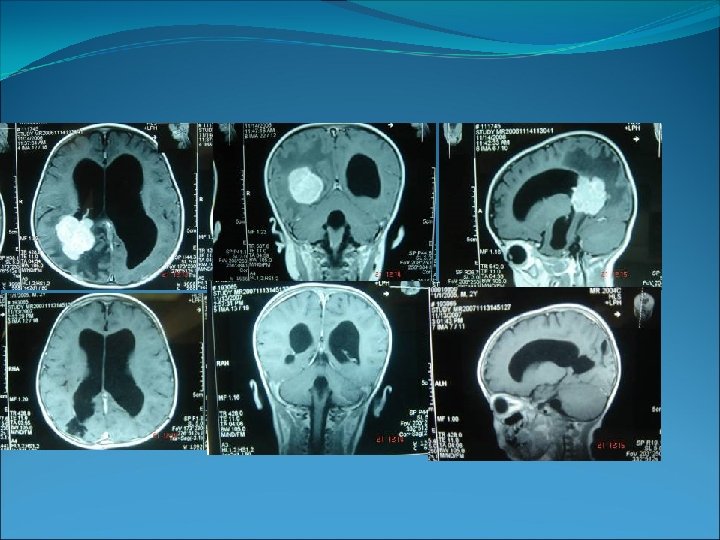
MRI (Preoperative)
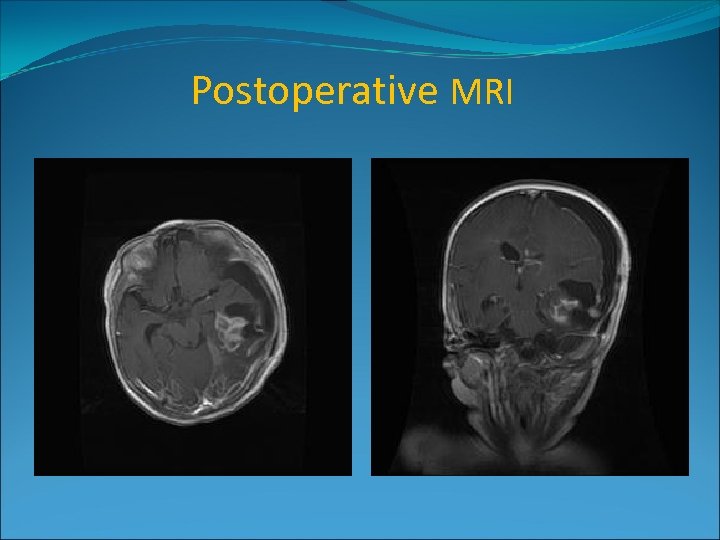
Postoperative MRI
Scoliosis and spinal cord thickening 23 -month-old boy Scoliosis (for 17 months) Without pain Normal in action Without urinary and fecal incontinence No family history of scoliosis could be found Further physical, neurologic examination normal
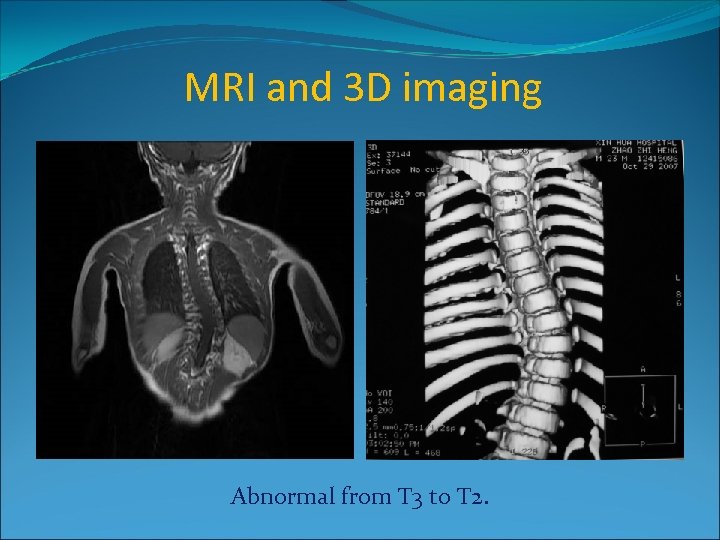
MRI and 3 D imaging Abnormal from T 3 to T 2.
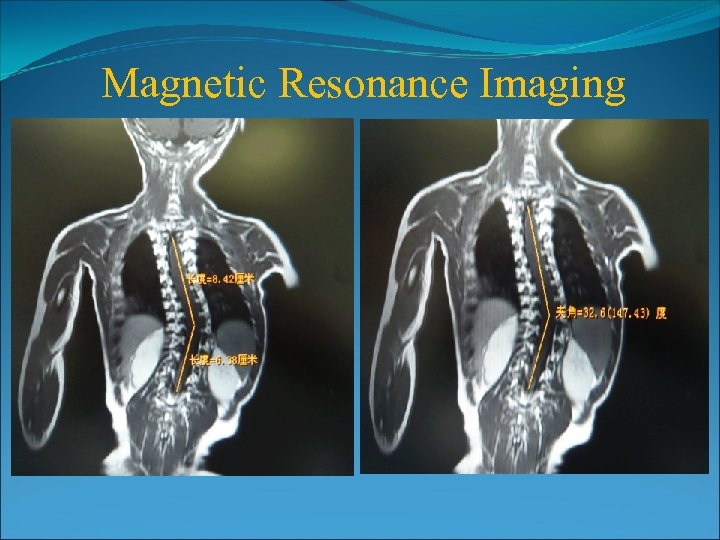
Magnetic Resonance Imaging
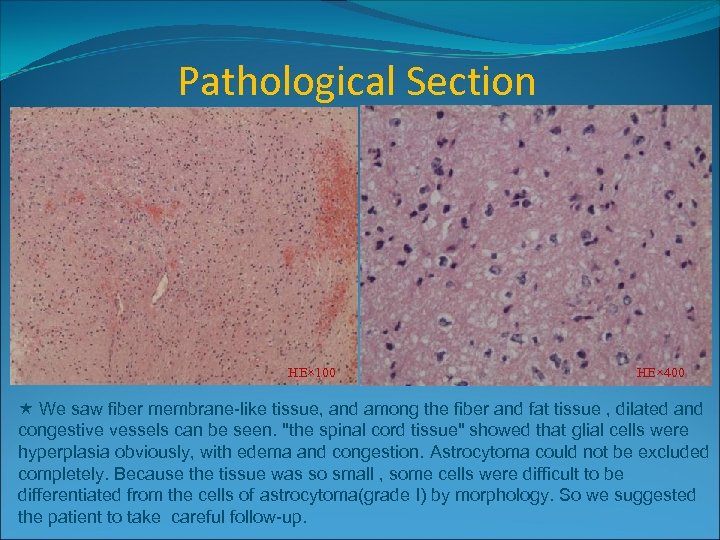
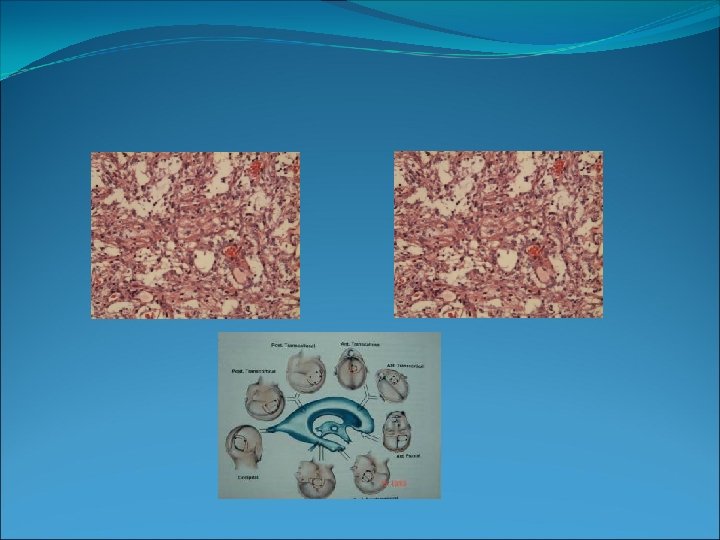
Pathological Section HE× 100 HE× 400 We saw fiber membrane-like tissue, and among the fiber and fat tissue , dilated and congestive vessels can be seen. "the spinal cord tissue" showed that glial cells were hyperplasia obviously, with edema and congestion. Astrocytoma could not be excluded completely. Because the tissue was so small , some cells were difficult to be differentiated from the cells of astrocytoma(grade I) by morphology. So we suggested the patient to take careful follow-up.
5fb2259ff08da7b59a63274a7b5d0250.ppt