72936c96c28001d8a2d867297f4574cc.ppt
- Количество слайдов: 47

Supporting HIV Patient Self-Management The Evidence Base, Practice Implications, and Provider Support Joseph Rukeyser, Ph. D National Quality Center Jenny Knight, FNP Harlem Hospital Center, NY Funded by HRSA HIV/AIDS Bureau
The Problem • Patients often have difficulty in taking care of the longterm, day-to-day management of their own health. They may: § Miss appointments or follow-up referrals § Not follow diet or activity recommendations § Take medications or supplements that interfere with prescribed therapies § Ignore or not recognize signs of adverse events or disease progression § Behave in ways that put themselves at risk including not adhering with prescribed medical therapies • Clinicians have limited time to address these issues 2 National Quality Center (NQC)
Patients who are effective self-managers: • • • 3 Learn about their HIV disease Practice effective communication skills Actively partner with providers in decision-making Practice action-planning and problem solving Self-monitor symptoms and follow treatment directions Seek and follow expert medical care and advice Use family, peer, and community support resources Maintain emotional and psychological balance Practice health-promoting behaviors National Quality Center (NQC)

Helping patients be better self-managers can… • Improve § Patient health outcomes § Patient health-promoting behaviors § Patient self-efficacy § Communication with providers § Utilization of community resources § Containment of health care costs § The quality and efficacy of HIV care 4 National Quality Center (NQC)
Providers Can Make A Difference • Providers have key roles in supporting patient self-management by § Ensuring effective communication and education § Collaborative goal-setting § Shared decision-making § Anticipating and planning for symptom and side effects management § Designing systems and support teams that aid patients in developing and utilizing self-care skills and resources 5 National Quality Center (NQC)
Learning Objectives • Define “patient self-management” and provider “selfmanagement support” • Describe evidence supporting self-management by patients with chronic illnesses (e. g. , asthma, diabetes, arthritis) • Discuss the value of self-management in the chronic care of patients with HIV/AIDS • Review the HIV provider training curriculum: “Making Sure HIV Patient Self-management Works” • Discuss provider practice-based self-management support interventions for patients with HIV/AIDS 6 National Quality Center (NQC)
Patient self-management is… “The capability of patients with chronic illnesses, in a complementary partnership with and the support of their health care providers, to manage the symptoms, treatment, lifestyle behavior changes, and the many physical and psycho-social challenges that they face each day. ” A composite of definitions in the literature 7 National Quality Center (NQC)

Growing Support for Patient Self-Management “Increasing evidence shows that self-management support reduces hospitalizations, emergency department use, and overall managed care costs. ” “Physician support of patient self-management is one of the key elements of a system’s-oriented chronic care model. ” Coleman and Newton. Supporting self-management in patients with chronic illness. Am Fam Physician 2005; 72(8): 1503 -10 8 National Quality Center (NQC)

HIV/AIDS is similar in some ways to chronic illnesses • Potent antiretroviral therapy has improved the health and extended the lives of many people with HIV infection • HIV shares similarities with other chronic diseases: the need to take medications daily; regular office visits and monitoring; risks of treatmentrelated side effects; • But also important differences: constant threat of acute illness; stigma, drug resistance; infectious nature; marginalization • HIV therapy is constant, life-long, and treatment strategies must be sustainable and flexible to meet changing situations • HIV patients have day-to day responsibilities for their care • Providers must provide support, motivation, tools, and education Aberg J. The Changing Face of HIV Care: Common Things Really Are Common. Ann Intern Med. 2006; 145(6): 463 -65 9 National Quality Center (NQC)

Patient self-management is used effectively in many chronic illnesses and is an essential component of the Chronic Care Model (CCM) Funded by HRSA HIV/AIDS Bureau
Asthma Studies of asthma patient self management programs show that they can… § reduce morbidity § improve lung function § enhance feelings of self control § reduce absenteeism from school and number of days with restricted activity § reduce nocturnal episodes § reduce visits to an emergency department Guevarra P et al. Effects of educational interventions for self management of asthma in children and adolescents: a systematic review and meta-analysis. BMJ 2003; 326: 1308 -13 11 National Quality Center (NQC)
Arthritis • In multiple randomized trials, the Arthritis Patient Self-management Program has been found to improve § health behaviors § self-efficacy § health status § cost savings 1, 2 • Patient self-management of arthritis reduced anxiety and depression and improved participants’ perceived self-efficacy to manage symptoms. 3 1. Lorig K and Holman H. Arthritis Self-Management Studies: A Twelve-Year Review. Health Education Quarterly. 1993; 20(1): 17 -28 2. Lorig K, et al. Arthritis Self; Management Program Variations: Three Studies. Arthritis Care and Research. 1998; 11(6): 448 -454 3. Buszewicz M et al. Self management of arthritis in primary care: randomised controlled trial. BMJ 2006; Online First bmj. com 12 National Quality Center (NQC)
Diabetes § Most well-studied disease category § Group visits and individualized problem- solving are effective self-management tools resulting in • Improved recommended prevention behaviors • Improved health status (SF-36) • Fewer specialty and ED visits • Enhanced patient satisfaction and self-efficacy • Improved Hb. A 1 c levels Wagner E et al. Chronic care clinics for diabetes in primary care. Diabetes Care 2001; 25: 695 -700; Anderson R et al. Patient empowerment: results of randomized controlled trial. Diabetes Care 1995; 18(7): 943 -949 13 National Quality Center (NQC)

Systematic Review of 39 Diabetes Studies Using at least one component of the CCM • 17 of 20 studies that included a patient selfmanagement component found positive outcomes § ↓ health care costs § ↓ length of hospital stay § ↑ health outcomes (e. g. , improved Hb. A 1 c) Bodenheimer T, et al. Improving Primary care for Patients with Chronic Illness: The Chronic care Model, Part 2. JAMA. 2002; 288(15): 1909 -1914 14 National Quality Center (NQC)

The body of evidence shows that supporting patient self-management… § reduces hospitalizations § reduces ER visits § reduces overall managed care costs § increases patient satisfaction with care § improves health outcomes (e. g. , ) • Glycemic control • Nocturnal asthma symptoms • Blood pressure control Coleman and Newton, Am Fam Physician, 2005 15 National Quality Center (NQC)
Self-management support includes… • Collaborative goal setting and shared decision making • Regular follow-up, monitoring and assessing progress towards achievable goals • Revising goals and supportive interventions as necessary • Education and tools tailored to patient’s unique needs and social and cultural environment • Integrating support to the individual’s regular source of medical care and monitoring their effects on a patient’s health 16 National Quality Center (NQC)

Clinicians can provide increased support of patient self-management by… • structuring patient-physician interactions to include collaborative goal-setting, problem-solving, and decision-making strategies • using self-management support evidence base to guide daily practice and decision-making • making office system changes optimizing the care team, use planned interactions • providing self-management education and referrals, linking patients to community self-management programs and other resources. Coleman M. and Newton K. Supporting Self-management in Patients with Chronic Illness. Am Fam Physician. 2005; 72; 8: 1503 -10. 17 National Quality Center (NQC)
Sample Patient Self-Management Supports Clinicians Can Use • Patient education classes, resource referrals and reading • Tools for goal-setting, action-planning, information organization, problem solving, and decision-making • Collaborative communication, information sharing, and resource development • Organizational or system supports (group visits; reminder calls; pre-MD visit, medication guides, provider team coordination) • Guides for self-monitoring symptoms, medication adherence, side-effects, and appropriate use of medical resources • Ongoing assessment and adjustment to changing circumstances and behavior-change needs • Use of the 5 A’s: Ask, Advise, Agree, Assist, and Arrange 18 National Quality Center (NQC)
Few Self-Management Studies with HIV Patients • No strong evidence yet of efficacy • Only pilot studies have been done • Results show: § Increase in self efficacy correlated with increase in CD 4 count and decrease in viral load* • More studies needed of in-office interventions and system supports *Ironson G, Weiss S et al(2005) The impact of improved self-efficacy on HIV viral load and distress in culturally diverse women living with AIDS: the SMART/EST Women’s Project. AIDS Care 17: 222 -36 19 National Quality Center (NQC)
Stanford HIV Self-Management Education Pilot Study • Pilot test of a group self-management course for HIV/AIDS patients § ↓ symptom severity index in the education session group and ↑ in the control group. § ↑ self-efficacy in the educational group and ↓ in the control group. § secondary outcomes (pain fatigue, psychosocial symptoms, changes in stress/relaxation exercises, and HIV/AIDS knowledge were not significantly different in the two groups. • No follow-up of this pilot study reported to date. Gifford A, Pilot Randomized Trial of Education to Improve Self-Management Skills of Men with Symptomatic HIV/AIDS. JAIDSHR. 1998; 18136 -144. 20 National Quality Center (NQC)
Limitations of Patient Self-Management Education In a meta-analysis of 71 trials of self-management education across several chronic disease states the authors concluded that… • While self-management education programs are conceptually appealing, the findings of this review suggest that not all selfmanagement education programs for all diseases or for all patients are effective. • Patient self-management programs which tailor educational content and methodology to individual patients and which are integrated into medical care may prove to be more effective than structured selfmanagement education courses, for which only specific patient subgroups may be ready. Warsi A, et al. Self-management Education Programs in Chronic Disease. Arch Inter Med. 2004; 164: 1641 -1649. 21 National Quality Center (NQC)
Potential Barriers to Initiating Patient Self-Management Support Programs • • 22 Comfort with traditional model of care Reluctance to lose “control” Time constraints Unpreparedness for dealing with “non-medical” issues Reimbursement concerns Lack of skills training Insufficient support from management Unfamiliarity with the evidence basis National Quality Center (NQC)

Getting Past the Barriers • Join efforts with other self-management supporters • Use in-services and study groups to get “buyin” from clinicians and administration • Create multi-disciplinary teams to plan and implement programs • Share the responsibilities of patient support among members of the health care team • Use community resources 23 National Quality Center (NQC)
www. nationalqualitycenter. org 24 National Quality Center (NQC)

Provider Training Curriculum • “Making Sure HIV Patient Self-Management Works: A Training Workshop for HIV Care Providers” § Curriculum guide for workshop facilitators § NQC/ NYSDOH AIDS Institute/ HRSA HIV/AIDS Bureau § Pilot tested with a range of care providers § An activity-based guide to preparing providers to support patients in § § 25 their own HIV self-management Interactive and experiential learning activities Targets knowledge, attitudes and behavior change Hands-on practice in the use of patient action-oriented selfmanagement supports Guide to 8 facilitator-led activities National Quality Center (NQC)
Curriculum Goals • Training curriculum goals: - To meet the needs of providers in developing individual understandings and expertise in patient selfmanagement - To create a core group of interested and informed providers - To assist providers in initiating or further developing practice-based patient self-management support programs - To improve the quality of HIV/AIDS health care by fostering collaborative interaction between patients and their providers in support of increased patient selfefficacy and self-management 26 National Quality Center (NQC)
Curriculum Activities (I) • Develop an operational definition of selfmanagement § Health care self-management continuum § Share personal experiences with managing health and health care • Patient Case Study § Small group brainstorming activity § Andy and Zeke* • Brothers with similar health challenges and different degrees of success with self-management *Case study based on Bodenheimer et al, JAMA 2002 27 National Quality Center (NQC)
Curriculum Activities (II): • The To-Do List § Small group activity to plan an approach to collaborative care with Zeke (HIV+) § Guide to assessing Zeke’s concerns, needs, strengths and priorities § What are the key management tasks? § Whose responsibility? (Zeke, providers, both? ) • Brainstorming patient self-management supports § Patient-centered § Provider-centered § System-centered 28 National Quality Center (NQC)
Curriculum Activities (III) • Action Planning Role Play § Practice effective listening and communication skills § Focus on developing collaborative goal-setting and action-planning skills § Use of a sample action-planning worksheet 29 National Quality Center (NQC)

Action Planning Worksheet Patient Name: _______ Physician Name: _______ Assess patient’s primary concern or problem: (e. g. , “What is your greatest concern now? ”; “What one thing would you most like to change? ”) _________________________ Explore patient’s feelings about the problem: (“What do you think makes this so hard for you? ”; “How will you feel if things don’t change? ”) ________________________ Identify patient’s goals: (“How would you like the situation to change? ” “What one thing do you want to change? ”) ________________________ Brainstorm solution ideas: (“What do you think might work or help you to reach that goal? ”; How do you think you might solve this problem? ”; ”What have you tried in the past? ”; “How might I or someone else help you to do this? ”) ________________________ Choose a solution and Action Steps to try: (“What do you think you could do? ”; “When would you do it? ”; How often do you think you could do that? ”; What will you do to get started? ”) ________________________ Estimate self-efficacy [Use the “Getting to 7” Scale]: (“Does this sound like something you can do? ” ”Are you sure this is something you want to do? ” “On a scale of 1 to 10 how likely is it that you will actually be able to do that? ” ) 30 National Quality Center (NQC)
Curriculum Summary • • 31 Targeted toward a range of care providers Modular Interactive Experiential Learner-centered Brief (~4 hours) Model for collaborative approach National Quality Center (NQC)
Patient Self-Management: Conclusions • Actual time clinicians and patients spend together is very limited; in between visits patients “self-manage” their own care • Patient self-management of chronic disease can improve health outcomes and reduce costs • Some patients are better self-managers than others; all patients can become better managers • Clinicians play an important role in supporting patient self-management (education, skills, tools, encouragement, and resources) • Resources are available to assist clinicians in supporting patient self-management 32 National Quality Center (NQC)

Selected Resources • Living Well with HIV and AIDS. Gifford A. et al. Bull Publishing Company. 2000 • Living a Healthy life with Chronic Conditions. Lorig K. et al. Bull Publishing Company. 2000 • The Art of Empowerment. Anderson B and Funnell M. American Diabetes Association. 2000 • A Guide to Consumer Involvement. NYS DOH AIDS Institute and HRSA HIV/AIDS Bureau. 2006 • Making Sure Your HIV Care is the Best it Can Be: A consumer training curriculum. NYS DOH AIDS Institute. 2005 • Making Sure that Patient Self-management Works: A provider training curriculum. NYS DOH AIDS Institute. 2007 • www. hivguidelines. org • www. ihi. org 33 National Quality Center (NQC)

Selected References Aberg J. The Changing Face of HIV Care: Common Things Really Are Common. Ann Intern Med. 2006; 145(6): 463 -65 Anderson R et al. Patient empowerment: results of randomized controlled trial. Diabetes Care 1995; 18(7): 943949 Anderson R. Patient Empowerment and the Traditional Medical Model. Diabetes Care. 1995; 18(3): 412 -5. Bodenheimer T, et al. Improving Primary care for Patients with Chronic Illness: The Chronic care Model, Part 2. JAMA. 2002; 288(15): 1909 -1914 Bodenheimer T, Lorig K, Holman H, et al. Patient Self-management of Chronic Disease in Primary Care. JAMA. 2002; 288(19): 2463 -2475. Buszewicz M et al. Self management of arthritis in primary care: randomised controlled trial. BMJ 2006; Online First bmj. com Coleman M and Newton K. Supporting Self-management in Patients with Chronic Illness. Am Fam Physician 2005; 72: 1503 -10. Glasgow R, Davis C, Funnell M, et al. Implementing practical interventions to support chronic illness selfmanagement. Jt Comm J Qual Saf. 2003; 29(11): 563 -74. Gifford A, Laurent D, Gonzales V, et al. Pilot Randomized Trial of Education to Improve Self-Management Skills of Men with Symptomatic HIV/AIDS. JAIDSHR. 1998; 18: 136 -144. Guevarra P et al. Effects of educational interventions for self management of asthma in children and adolescents: a systematic review and meta-analysis. BMJ 2003; 326: 1308 -13 HRSA HIV AIDS Bureau. Self-Management and the Chronic Care Model. HRSA CARE Action. January 2006. Ironson G, Weiss S et al(2005) The impact of improved self-efficacy on HIV viral load and distress in culturally diverse women living with AIDS: the SMART/EST Women’s Project. AIDS Care 17: 222 -36 Lorig K and Holman H. Arthritis Self-Management Studies: A Twelve-Year Review. Health Education Quarterly. 1993; 20(1): 17 -28 Lorig K, et al. Arthritis Self; Management Program Variations: Three Studies. Arthritis Care and Research. 1998; 11(6): 448 -454 Wagner E et al. Chronic care clinics for diabetes in primary care. Diabetes Care 2001; 25: 695 -700; Warsi A, Wang P, La. Valley M, et al. Self-management Education Programs in Chronic Disease. Arch Intern Med. 2004; 164: 1641 -1649. 34 National Quality Center (NQC)
Integrating Patient Self Management into Clinical Practice Harlem Hospital New York City 35 National Quality Center (NQC)
Harlem Hospital • Our team was part of a one-year national learning community sponsored by the Institute for Healthcare Improvement on patient selfmanagement (included 20 sites, 2 other HIV) • The Family-Centered Care Program (FCP) was our target population • Participated in extended follow-up project to measure sustainability of change 36 National Quality Center (NQC)
Population of Focus • 25% of FCP patients are recent immigrants from West Africa • The remaining 75% of FCP patients are predominantly African-American or Hispanic • Many face legal, linguistic and cultural barriers to care • The self-management model is well-suited to assist these patients in overcoming barriers and achieving better health outcomes 37 National Quality Center (NQC)

Introducing Self-Management • Developed a goal setting tool to set a patientdriven healthcare goal and develop an action plan during the clinic visit • Developed a model to accomplish this within the time constraints of the clinic setting 38 National Quality Center (NQC)
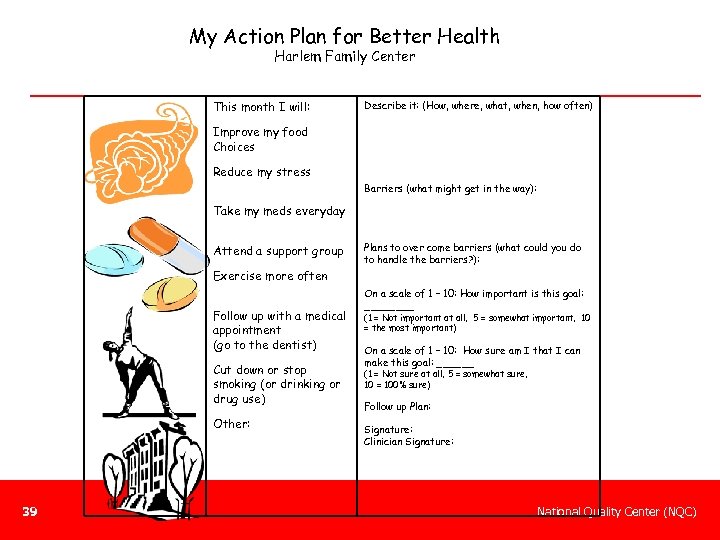
My Action Plan for Better Health Harlem Family Center This month I will: Describe it: (How, where, what, when, how often) Improve my food Choices Reduce my stress Barriers (what might get in the way): Take my meds everyday Attend a support group Plans to over come barriers (what could you do to handle the barriers? ): Exercise more often Follow up with a medical appointment (go to the dentist) Cut down or stop smoking (or drinking or drug use) Other: 39 On a scale of 1 – 10: How important is this goal: ____ (1 = Not important at all, 5 = somewhat important, 10 = the most important) On a scale of 1 – 10: How sure am I that I can make this goal: ______ (1 = Not sure at all, 5 = somewhat sure, 10 = 100% sure) Follow up Plan: Signature: Clinician Signature: National Quality Center (NQC)

Refine Goal Setting Delivery Implement – Goal Setting Delivery Design Optimize Goalsetting in Mom/Baby Clinic ata D S A P S D A D D S P A P S D D S P A Cycle 4: Expand approach to two RN/Provider teams in Adult HIV clinic Cycle 3: Team approach implemented in Mom/Baby Clinic. Case manager plays role in supporting plan Cycle 2: RN uses goal-setting tool with patients prior to provider Visit at one clinic session. Provider reinforces goals/plan Cycle 1: Providers use goal-setting tools with patients 40 National Quality Center (NQC)
Team Approach • Piloted in Mom-Baby Clinic § Later expanded to several providers in ID Clinic • • 41 Nurse sets goal with pt during triage Provider reviewed goals with pt during visit Case manager available to reinforce goals Goal and action plan filed in patients’ chart National Quality Center (NQC)
Goal-setting was Patient-Driven • Easier than expected to generate goals from patients • Encouraged the patient to identify the goal themselves, come with action plan, identify barriers, come up with solution that worked for them • Skills included: asking opening ended questions, reflective listening, summarizing 42 National Quality Center (NQC)
Impact of Goal-Setting • Can solve impasse around behavior change • Gives providers deeper understanding of the patient • Improves relationship between patient-nurse and patient-provider • Empowers pt to make needed behavior changes, or at least think about them if they are not ready 43 National Quality Center (NQC)
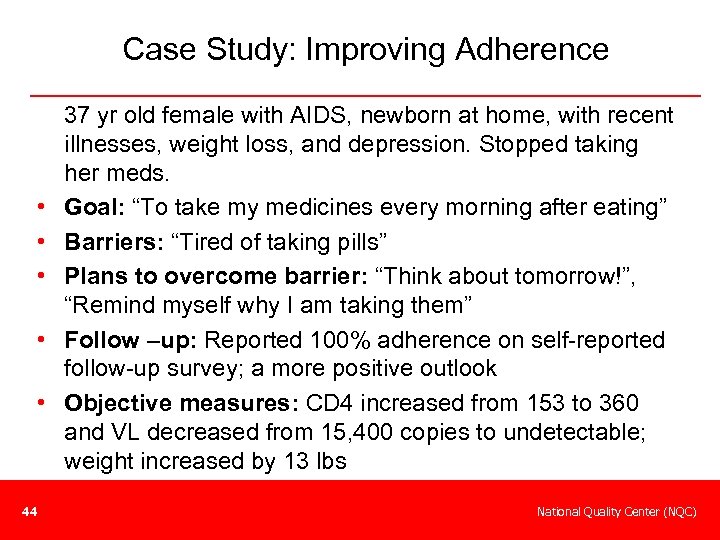
Case Study: Improving Adherence • • • 44 37 yr old female with AIDS, newborn at home, with recent illnesses, weight loss, and depression. Stopped taking her meds. Goal: “To take my medicines every morning after eating” Barriers: “Tired of taking pills” Plans to overcome barrier: “Think about tomorrow!”, “Remind myself why I am taking them” Follow –up: Reported 100% adherence on self-reported follow-up survey; a more positive outlook Objective measures: CD 4 increased from 153 to 360 and VL decreased from 15, 400 copies to undetectable; weight increased by 13 lbs National Quality Center (NQC)

Case Study: Coordination of Care 46 yr old male with AIDS with hx of substance use and poor adherence. • Returned to NYC 8/06 after several months of incarceration in Virginia with CD 4 277 and VL <50 and reengaged in care • By 11/06 CD 4 180, VL > 100, 000. Pt was at the hospital daily attending support programs (HATS, COBRA, HABARI, Harm Reduction, Nutrition, Hep C) 45 National Quality Center (NQC)

Presenter Contacts Joseph Rukeyser, Ph. D jar 08@aol. com Jenny Knight, FNP Harlem Hospital Center, NY jk 2106@columbia. edu 46 National Quality Center (NQC)
National Quality Center (NQC) NYSDOH AIDS Institute 90 Church Street— 13 th Floor New York, NY 10007 -2919 888 -NQC-QI-TA Info@National. Quality. Center. org Funded by HRSA HIV/AIDS Bureau
72936c96c28001d8a2d867297f4574cc.ppt