fc978855ceed3081a6e57e079c2693da.ppt
- Количество слайдов: 39
Suicide Risk Assessment and Management & CBT Primary Care Mental Health Link Working Service Mental Health Workers Jaikumar Shanmugasundaram Mike Jackson
TRUE or FALSE Suicide is a rare occurrence FALSE: The World Health Organization says suicide is a leading cause of death worldwide, and one of the three leading causes of death for young people under 25 Those who talk about suicide do not commit suicide FALSE When a person shows signs of improvement, or survives a suicide attempt, they are out of danger FALSE: One of the most dangerous times is immediately following the crisis or when the person is in hospital following an attempt. The week following discharge is of particular risk
TRUE or FALSE Children do not commit suicide. They do not understand the finality of death and are cognitively incapable of engaging in a suicidal act FALSE: Although rare, children do commit suicide and ANY gesture at ANY age must be taken seriously The number of visits to GPs usually increases significantly before committing suicide TRUE Suicides are inevitable FALSE: Avoiding marginalisation and supporting at personal crisis times will help prevent (Do. H)
TRUE or FALSE Suicide is always an impulsive act and happens without warning FALSE: Many individuals give verbal or behavioural warnings about their intentions Suicidal individuals really want to die or are determined to kill themselves FALSE: Most people who are feeling suicidal will share their thoughts with at least one other person Suicide Risk assessment is a clinical judgement based on available clinical details Vs Suicide prediction is foretelling based on statistical probability TRUE: Suicide prediction - foretelling based on the presence or absence of a specific number of defined factors, within definable limits of statistical probability Suicide (risk) Assessment - clinical judgment of risk based on the weighing of a very large mass of available clinical detail. Risk assessment carried out in a systematic, disciplined way is more than a guess or intuition.
TRUE or FALSE Once a person attempts suicide, they will never do it again FALSE: Previous suicide attempts are a critical predictor of suicide. 1 in 5 will make a further attempt within 1 year Asking about suicide does increase the risk of suicide FALSE: In fact, people feel relieved they are being asked Suicide is an act that cannot be reversed TRUE: effective prevention is the only way to minimize the risk
Luton Statistics on Suicide Male > female in Luton In 2005 – 2009, there were 79 deaths among Luton residents from suicide and undetermined injury • 75% males • 33% under 35 years • 77% under 55 years • 72% born in the UK • 13% were born in Eastern Europe
What Research and Statistics say 1 % of population have suicidal thoughts per week Between a quarter and a half of those committing suicide have previously carried out a non-fatal act About 70 to 80 psychiatric inpatients die annually by suicide Highest risk : 14 days post-discharge (7 day follow up) Primary care plays an important role in the prevention of suicide – HOW?
Risk Factors for Suicide Ø Suicidal thoughts Ø h/o any mental health/ Chronic physical health problems Ø Factors that reduce self control Ø Social isolation and lack of support Ø h/o suicidal/ self-harm attempts Ø Presence of ongoing ‘real life’ difficulties Ø Preparation
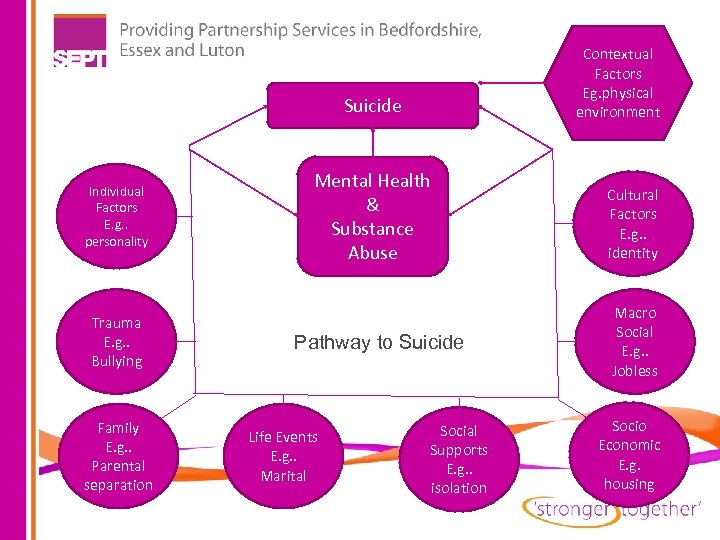
Contextual Factors Eg. physical environment Suicide Individual Factors E. g. . personality Trauma E. g. . Bullying Family E. g. . Parental separation Mental Health & Substance Abuse Pathway to Suicide Life Events E. g. . Marital Social Supports E. g. . isolation Cultural Factors E. g. . identity Macro Social E. g. . Jobless Socio Economic E. g. housing
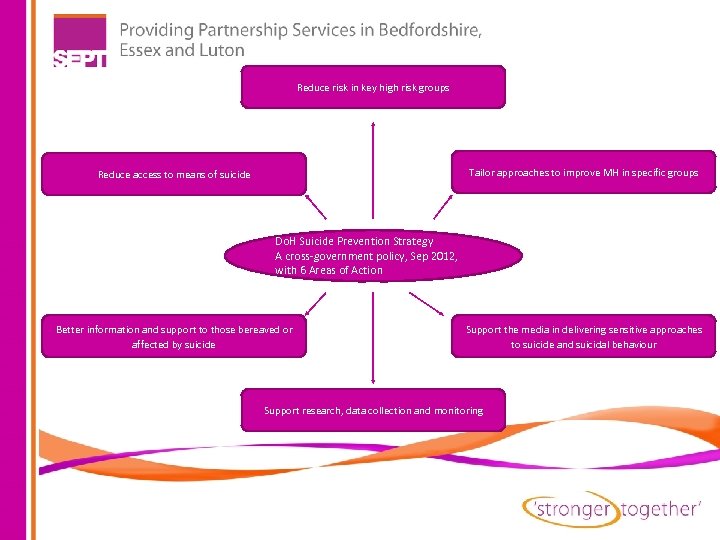
Reduce risk in key high risk groups Tailor approaches to improve MH in specific groups Reduce access to means of suicide Do. H Suicide Prevention Strategy A cross-government policy, Sep 2012, with 6 Areas of Action Better information and support to those bereaved or affected by suicide Support the media in delivering sensitive approaches to suicide and suicidal behaviour Support research, data collection and monitoring
High Risk Groups Young and middle aged men People in the care of mental health services, including inpatients People with a history of self-harm People in contact with Criminal Justice System Specific occupational groups (Doctors, nurses, farmers, etc. )
Primary Care Contribution Effective liaison, networking and communication with specialist mental health professionals Timely referral to appropriate services Good rapport, communication and follow-up Early identification and prompt, effective treatment of depression Skilful assessment and identification of suicidal/ self harming intent, thought, behaviour
THE ART OF SUICIDE ASSESSMENT AND INTERVENTION “Currently, the major bottleneck in suicide prevention is not remediation, for there are fairly well-known and effective treatment procedures for many types of suicidal states; rather it is in diagnosis and identification. ” – Edwin Shneidman, father of modern suicidolgy.
ASSESSMENT Unstructured Clinical Approach No systematic gathering of info, anecdotal and inconsistent Actuarial Approach risk factors based statistics, on large sample of people, used with caution, can be a part of risk assessment, Rating scales Structured Clinical (or Professional) Judgement Approach Professional judgement based on a thorough and systematic overall clinical assessment
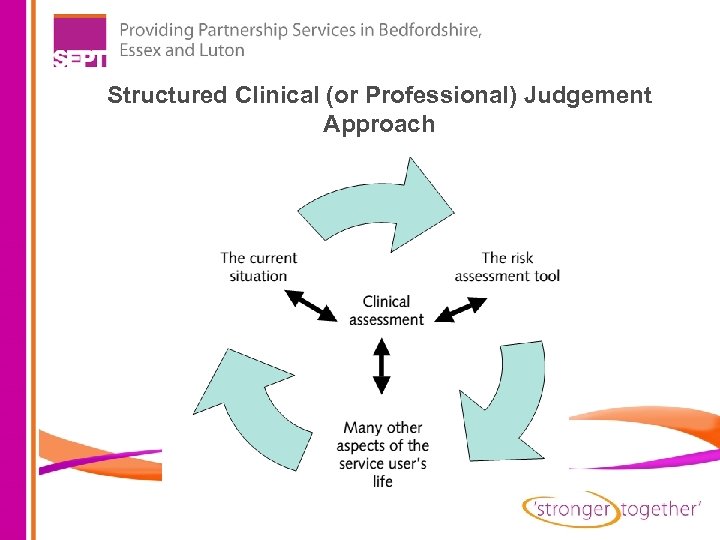
Structured Clinical (or Professional) Judgement Approach
RATING SCALES Examples of reliable, quick measures commonly used: BHS (Becks Hopelessness Scale) 20 item, self-report, less than 10 minutes Sad Persons 10 risk factors, limited contribution SIS (Suicidal Intent Scale) 15 item, interview-based or self-assessment SSI (Scale for Suicide Ideation) 21 item, self administered
RATING SCALES A few others Beck Scale for Suicide Ideation (Beck & Steer, 1991) Behavioural Health Monitor (Kopta & Lowry, 2002) Brief Symptom Inventory (Derogotis & Savitz, 1999) Columbia-Suicide Severity Rating Scale (C-SSRS) (Posner, K. , et al. 2008) Outcome-Questionnare-45. 2 (OQ-45. 2) (Lambert, Burlingame, et al. , 1996) PHQ 9 and GAD 7 http: //www. phqscreeners. com/

INTERVIEWING THE PATIENT Motivational Interviewing avoiding argumentation and direct “heavy” confrontation expressing empathy through reflective listening supporting self-efficacy and optimism identifying discrepancies between the client’s goals or values and their current behaviour
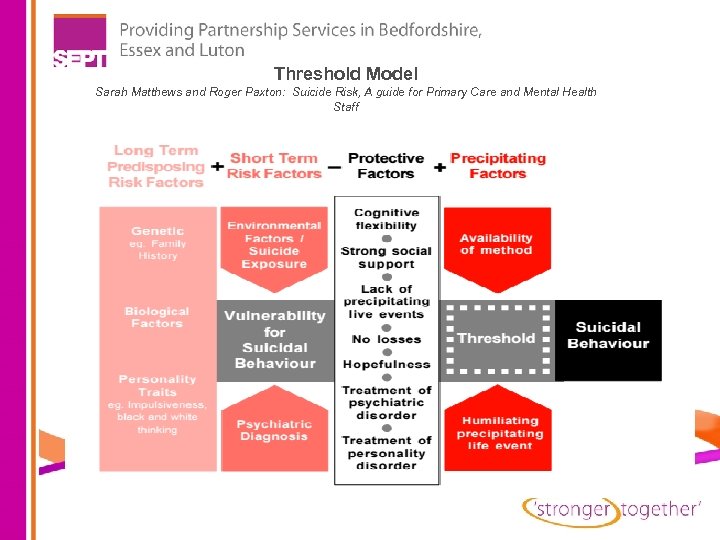
Threshold Model Sarah Matthews and Roger Paxton: Suicide Risk, A guide for Primary Care and Mental Health Staff
Stages in Applying Threshold Model o Establishing Rapport o Current distressing symptoms (physical/mental), alcohol/ substance abuse (Short term risk factors) o History of problems and coping strategies (long term risk factors) o Assessing support (Protective factors) o Asking about current circumstances (Precipitating factors) o Asking about Suicidal intent
Some question formats You may have good or even better questions than those mentioned below –just a guide Intention How do you see the future? Do you think things will get better for you? Are there times when you feel you have had enough of life itself? Are there times when you wish you were dead, or when you feel it would be better if you had died? I know this may be a difficult question, but have you even considered ending your own life?
Some question formats You may have good or even better questions than those mentioned below –just a guide Preparation What triggered this action? How long did it take you to attempt it from the time you actually thought about it? Did you worry that people might find out? Did you say goodbye to your loved ones?
Some question formats You may have good or even better questions than those mentioned below –just a guide Following Failed Suicidal Attempt Are you relieved that you did not die? If the person tells you that they are disappointed that they survived, this indicates a continuing high risk
Management Plan v • Exploring support availability (family, friends) v • Assess protective factors (faith, family) v • If patient aware of support available (how to and when to call services) v • Advising or educating patient about deterioration and asking for help (No-Suicide Contract, Hope-Kit) v • arrange help appropriate to the level of risk v • Frequent follow ups and encourage involvement of other professionals
Management of Suicide Risk (Level of Risk) If Risk Low: § § § FRAMES approach maintain usual contact arrangements seek advice from colleagues or people in other nearby services Encourage persons current or past coping methods persons existing support system Arrange earlier contact by telephone or an appointment If Risk High: § alert other involved professionals § refer the person for more urgent or more specialist care

Positive Risk Management as part of a carefully constructed plan is a required competence for all mental health practitioner (Best Practice in Managing Risk, Do. H, June 2007) Ø Is not negligent ignorance of potential risk Ø Is about real empowering of people through collaborative working Ø Is about supporting people to access opportunities Ø Is based on establishment of trusting working relationship Ø Is person-centred, working positively and constructively with risk and full appreciation of patients strengths Ø Is knowing support is available if things being to go wrong Ø Is about explicit setting boundaries to contain situation
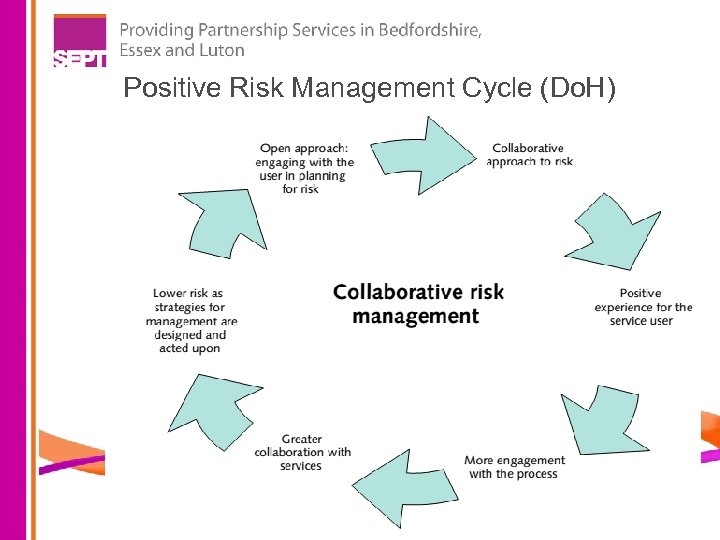
Positive Risk Management Cycle (Do. H)
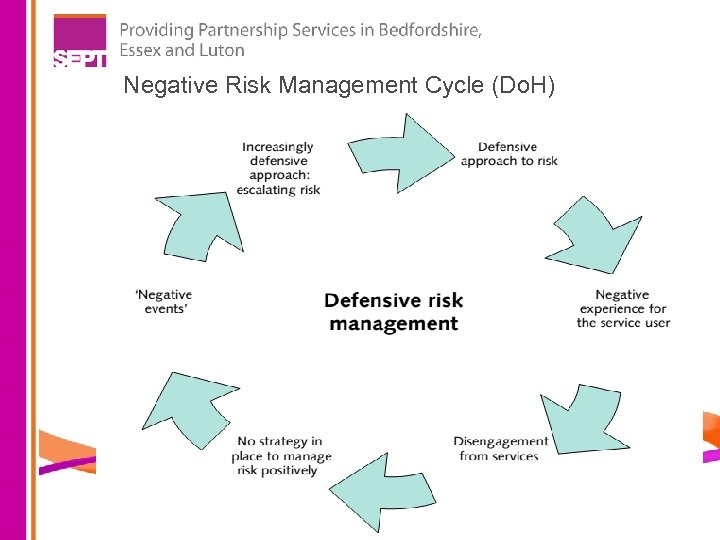
Negative Risk Management Cycle (Do. H)
Facts about Medication/ Hospitalisation Only Lithium and Clozapine have good evidence for reducing suicide Medication/ hospitalisation have good face validity for being helpful, but limited evidence of ‘anti-suicidal’ effect Sometimes treatment with medication give access to means (1/3 rd self poison with medications) Side effects of medications such as Akathisia increases suicide risk High risk of suicide among post-discharge
CASE SCENARIO 1 Sandra 55 year old; working in probation service (17 years now). Feeling very low in mood (4 months) since her brother killed himself (another brother committed suicide some years ago). This was sudden and unexpected and was overseas in South Africa. She has had difficulty going to work, sleeping excessively, feeling tired with poor appetite. She has had thoughts of self-harm and suicide but no current plans or intent. She feels she is not able to put her family through another suicide. Able to attend to her daily living needs. She lives alone with most of her family members in South Africa (two adult children and grandchildren live locally with regular contacts). She declined antidepressant therapy and referral to mental health services. p/h of work-related depression 3 years ago that required no specific treatment. High Risk – Admission Crisis Support Specialist care referral Primary care/ GP follow-up No follow-up
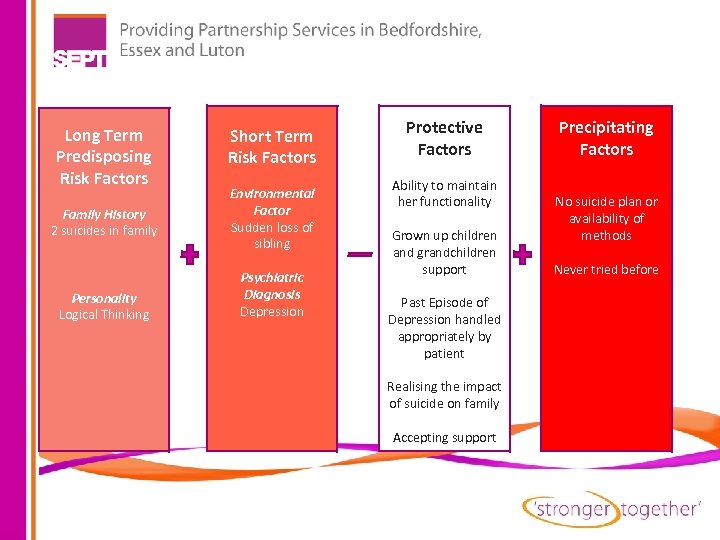
Long Term Predisposing Risk Factors Family History 2 suicides in family Personality Logical Thinking Short Term Risk Factors Environmental Factor Sudden loss of sibling Psychiatric Diagnosis Depression Protective Factors Ability to maintain her functionality Grown up children and grandchildren support Past Episode of Depression handled appropriately by patient Realising the impact of suicide on family Accepting support Precipitating Factors No suicide plan or availability of methods Never tried before
CASE SCENARIO 2 Ruth is a 44 year old divorced, unemployed mother of 2. She has been depressed for 6 years following the death of her mum who committed suicide. She was recently discharged from psychiatric hospital. She was found by a neighbour in a newly bought car in the garage, with the motor running and brought to A & E. She had send her children away for the weekend and had parked her own car in front of the garage hoping no one would discover her. She is bitterly disappointed to have failed to end her life. She always had thoughts to kill self and tried overdosing herself twice in the past. High Risk – Admit Discharge Home – with Crisis Support Discharge Home – with specialist care referral Discharge Home – with primary care/ GP follow-up Discharge Home – with no follow-up
CASE SCENARIO 3 Lisy is a 21 year old who presents to A&E having taken 20 paracetamol and ½ a bottle of Vodka. She had a fight with her boyfriend earlier in the evening. She used whatever she could find in the house and called an ambulance when she felt sick. She had wanted to end things at the time, but now regrets her actions. Works as a teaching assistant and lives with supportive parents. First time she tried killing herself and no past involvement with mental health services. High Risk – Admit Discharge Home – with Crisis Support Discharge Home – with specialist care referral Discharge Home – with primary care/ GP follow-up Discharge Home – with no follow-up
FRAMES APPROACH (Miller and Sanchez, 1993) Feedback to the patient Responsibility for change lies with the patient Advice to change Menu of strategies for bringing about change Empathy as a counselling style Self-efficacy or optimism
SUICIDES ACTION PLANS Symptoms of depression Underlying psychiatric problems Indication of maladaptive personality features Check life events Intent to commit suicide Depression/suicide in family history Environmental factors Suicide attempt in the past Avoid repeat prescribing Counselling approach Team discussion and supervision Identify risk on notes Offer follow up or earlier appointment Need to refer on? Plan the next few days Liaise with other professionals Awareness of non-statutory services Note informal supports Specialist care
PIPIAS P Past attempt (including self harm) I Ideation P Plan (to commit suicide) I Intention/impulsivity A Access to methods S Strengths (to avoid suicide)
Resources Available Nationally/ Locally Samaritans (08457 90 90 90) Childline (0800 1111) PAPYRUS (0800 068 41 41) SOBS (0300 111 5065) (Survivors of Bereavement by Suicide) 999/ A & E Emergency Duty Team (0300 8123) Crisis Team (18 to 65 yrs. ) L & D Psychiatric Liaison Team (65+ yrs. ; Dr H Pantula, Consultant) AMHP (07860 955 795, 07775 002 906)
Useful websites www. livingworks. net http: //suicide-parasuicide. rumos. com www. metanoia. org/suicide www. stampoutsuicide. org. uk - Points of contact for those feeling down, depressed and/or suicidal www. save. org www. theblackdog. net - Supportive site for men who suffer from depression and/or suicidal thoughts

POINTS TO TAKE HOME • • Risk dynamic and needs regular reassessment Early identification and treatment Ask direct questions Good communication between primary and secondary care
fc978855ceed3081a6e57e079c2693da.ppt