a679c5cbc2f15b50a064f61dd234aa01.ppt
- Количество слайдов: 37
Substance abuse in pregnancy Tom Archer, MD, MBA UCSD Anesthesia
Prevalence of substance abuse during pregnancy • Perhaps 5% of pregnant women in US use illicit drugs. • Perhaps 19% use alcohol. Abel EL Am J Obstet Gynecol 2002; 186: 768 -72.
Substances abused • • Alcohol Tobacco Cocaine Opioids Methamphetamine Ecstasy Benzodiazepines Solvents
Substance abuse is associated with: • +HIV (particularly with amphetamine use) • Suicide attempts • Lack of prenatal care
Ethical problem • Drug or alcohol- abusing mother may be subject to child abuse laws • This is a disincentive for her to self-report. • What is our role?
Mandatory testing of pregnant women for drugs and alcohol? • Would it protect children? • Would it discourage prenatal care? • Would it discourage women from seeking treatment? • 1997 criminal prosecution in South Carolina for exposing fetus to cocaine. • Health care personnel attitudes are relevant to enforcement of any laws to be enacted.
Should society punish / treat women who drink or use drugs during pregnancy? • Michigan study shows predominant opinion of MDs is in favor of defining drug and alcohol use during pregnancy as “child abuse” and requiring testing and / or compulsory treatment or punishment. • National organizations of peds, OBs and FPs are more “politically correct” (less punitive and intrusive). • What is the right mix of punishment vs. treatment? • How will this affect our dealing with these patients? Abel EL Am J Obstet Gynecol 2002; 186: 768 -72.
Reporting maternal drug use • Pediatricians more likely to report than OBs? • Pediatricians see less of a problem with “patient confidentiality. ”
Evidence of fetal withdrawal syndrome at birth or fetal alcohol syndrome • Grounds for removal of infant from maternal custody?
Dangers of drug use to fetus • • Brain damage Teratogenesis (e. g. fetal alcohol syndrome) Behavioral disorders Growth restriction d/t chronic placental insufficiency • Placental abruption • Infection (e. g. HIV).
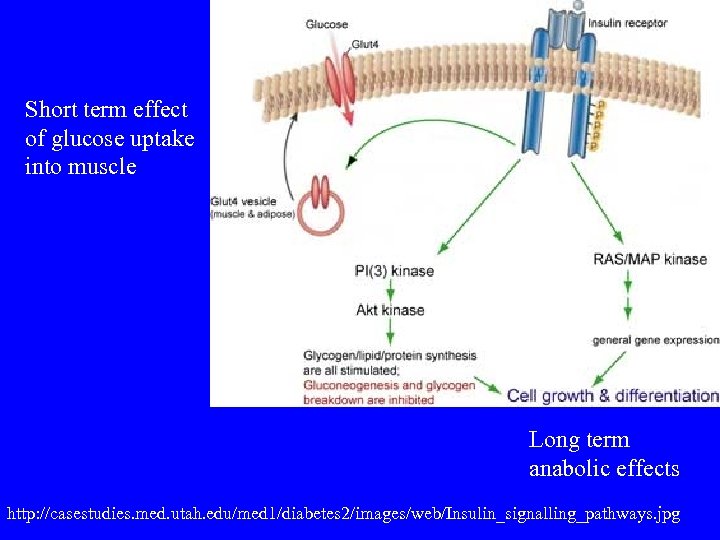
Short term effect of glucose uptake into muscle Long term anabolic effects http: //casestudies. med. utah. edu/med 1/diabetes 2/images/web/Insulin_signalling_pathways. jpg
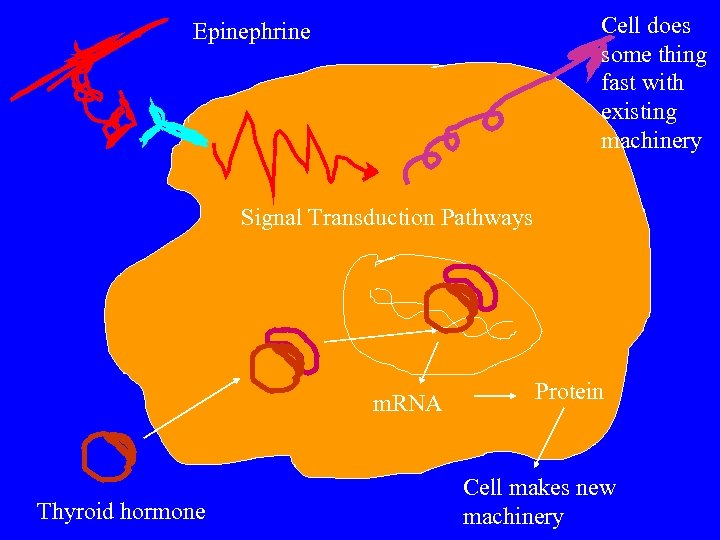
Cell does some thing fast with existing machinery Epinephrine Signal Transduction Pathways m. RNA Thyroid hormone Protein Cell makes new machinery
Perinatal testing • Maternal / fetal hair for cocaine / other drugs. • Meconium for fatty acid ethyl esters (FAEEs) from heavy ETOH use.
Alcohol • Fetal alcohol syndrome (high doses) • Alcohol related neurodevelopmental disorder (ARND) (lower doses)
Cocaine • Placental abruption, IUGR, prematurity, neurodevelopmental problems, IUFD. • Fetal exposure varies widely at same maternal dosage (placental metabolism? ) • Cocaine in fetal hair IDs mothers taking cocaine in last trimester (addicted? ), since hair forms only in last trimester.
Cocaine • Diagnosis is hard– patients are loathe to report. • Urine testing • Hair testing.
MAC and cocaine / methamphetamine • Chronic use may decrease MAC • Acute intoxication may increase MAC.
Cocaine • Local anesthetic – blocks sodium channels • Blocks reuptake of dopamine, norepinephrine and serotonin in CNS. • Euphoria, hypertension, tachycardia, vasconstriction, coronary vasospasm, thrombosis. • Associated vasculitis?
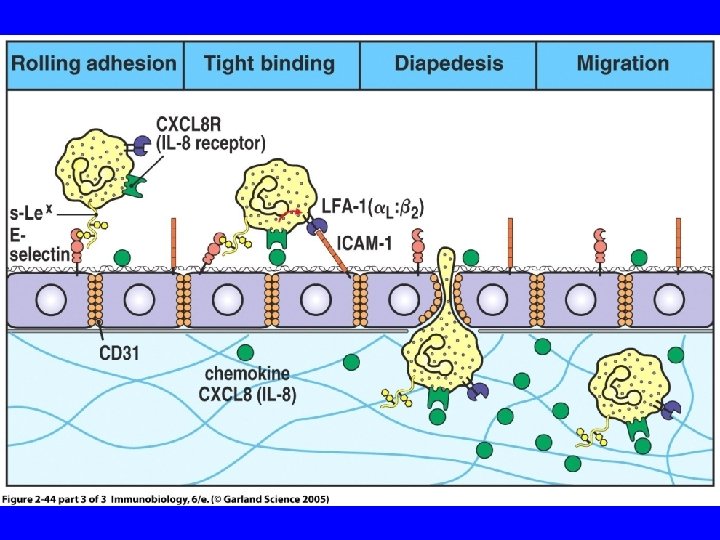
Cocaine • Increases vascular cell adhesion molecules (promoting white cell infiltration into tissues) • Promotes thrombosis • Cocaine is like obesity and hyperglycemia in this respect!
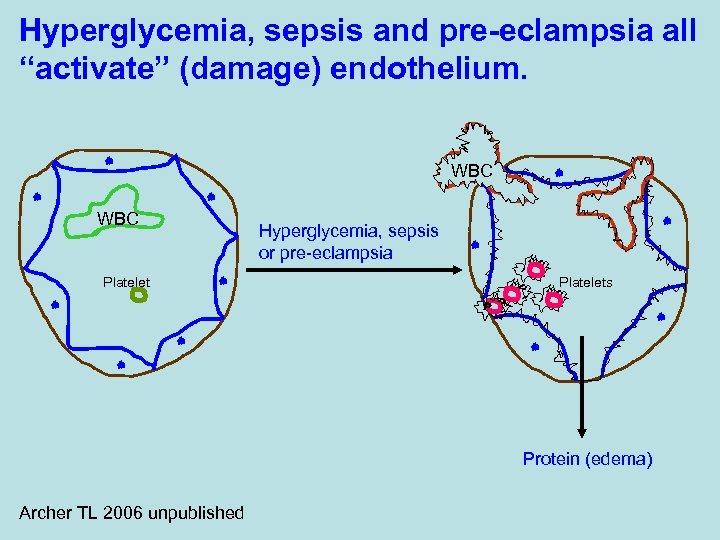
Hyperglycemia, sepsis and pre-eclampsia all “activate” (damage) endothelium. WBC Platelet Hyperglycemia, sepsis or pre-eclampsia Platelets Protein (edema) Archer TL 2006 unpublished
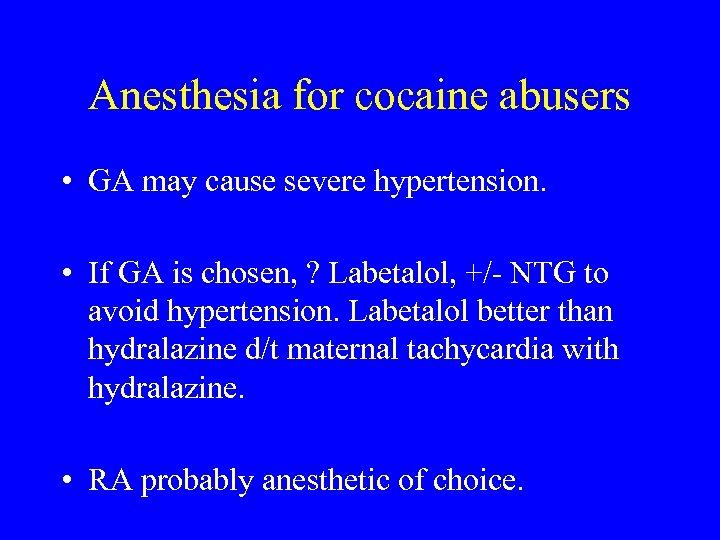
Anesthesia for cocaine abusers • GA may cause severe hypertension. • If GA is chosen, ? Labetalol, +/- NTG to avoid hypertension. Labetalol better than hydralazine d/t maternal tachycardia with hydralazine. • RA probably anesthetic of choice.
Risks of anesthesia for cocaine abusers • GA may cause severe hypertension. • RA probably anesthetic of choice. • RA dangers: platelet dysfunction, severe hypotension, lack of response to ephedrine. • Uncooperative, unhappy patient
Cocaine, endothelium and MI • Direct hemodynamic effects (inc HR, BP) • Coronary vasospasm • Endothelial effects (increased tissue factor and decreased tissue factor pathway inhibitor) – Increased thrombotic tendency
CART– cocaine and amphetamine regulated transcript (peptide) • Constricts arterioles by an Endothelin A mechanism
Hypertension in pregnancy • • Pre-eclampsia Cocaine use Methamphetamine use Alcohol, opioid withdrawal Pheochromocytoma Hyperthyroidism MH
Smoking • Carbon monoxide administration to fetus • Placental vascular constriction
Nicotine • Maternal use in pregnancy affects birth weight, infant cognition, behavior. • Perhaps 25% of women smoke during pregnancy. • Fetal brain has nicotine receptors. • Fetal exposure to nicotine may predispose to attention deficit disorder, conduct disorder and substance abuse.
Ecstasy • “MDMA” increases serotonin and (less) dopamine in brain. • Brain damage • Hyperthermia
The End
• 16036808 Authors. Fiala M. Eshleman AJ. Cashman J. Lin J. Lossinsky AS. Suarez V. Yang W. Zhang J. Popik W. Singer E. Chiappelli F. Carro E. Weinand M. Witte M. Arthos J. Authors Full Name. Fiala, Milan. Eshleman, Amy J. Cashman, John. Lin, Justin. Lossinsky, Albert S. Suarez, Vannina. Yang, Wendy. Zhang, Jun. Popik, Waldemar. Singer, Elyse. Chiappelli, Francesco. Carro, Eva. Weinand, Martin. Witte, Marlys. Arthos, James. Institution. Department of Medicine, West Los Angeles VA Medical Center and UCLA School of Medicine, Los Angeles, CA 90095, USA. Fiala@ucla. edu Title. Cocaine increases human immunodeficiency virus type 1 neuroinvasion through remodeling brain microvascular endothelial cells. Source. Journal of Neurovirology. 11(3): 281 -91, 2005 Jul. Local Messages*UTHSCSA LIBRARIES DO NOT OWN THIS TITLE* Abstract. Cocaine is a suspected cofactor in human immunodeficiency virus (HIV)-associated dementia but cocaine's effects are not clear. Herein the authors describe investigations of the mechanisms by which cocaine increases HIV-1 invasion through brain microvascular endothelial cells (BMVECs). Cocaine binds to a site on BMVECs, which is not a biogenic amine transporter, a binding site for estrogen, or a muscarinic receptor and for which benztropine and tamoxifen have the highest affinity. Cocaine treatment of BMVECs disrupts intercellular junctions and induces cell ruffling, which could account for their increased permeability and decreased electrical resistance. HIV-1 enters BMVECs by macropinocytosis and is transported to lysosomes and inactivated. In cocaine-treated BMVECs, the virus enters and persists in large cytoplasmic "lakes. " Cocaine exposure of BMVECs up-regulates transcription of genes important in cytoskeleton organization, signal transduction, cell swelling, vesicular trafficking, and cell adhesion. The toxicity of cocaine for the blood-brain barrier may lead to increased virus neuroinvasion and neurovascular complications of cocaine abuse. Publication Type. Journal Article. Research Support, N. I. H. , Extramural. Research Support, U. S. Gov't, P. H. S. .
• 15637118 Authors. Chen Y. Ke Q. Xiao YF. Wu G. Kaplan E. Hampton TG. Malek S. Min JY. Amende I. Morgan JP. Authors Full Name. Chen, Yu. Ke, Qingen. Xiao, Yong-Fu. Wu, Guifu. Kaplan, Emel. Hampton, Thomas G. Malek, Sohail. Min, Jiang-Yong. Amende, Ivo. Morgan, James P. Institution. Cardiovascular Division, Department of Medicine, The Charles A. Dana Research Institute and Harvard-Thorndike Laboratories, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts 02215, USA. Title. Cocaine and catecholamines enhance inflammatory cell retention in the coronary circulation of mice by upregulation of adhesion molecules. Source. American Journal of Physiology - Heart & Circulatory Physiology. 288(5): H 2323 -31, 2005 May. Local Messages*UTHSCSA LIBRARIES OWN JOURNAL. CLICK LIBRARY HOLDINGS FOR VOLS OWNED* Abstract. Cocaine treatment of mice with viral myocarditis significantly increases neutrophil infiltration into the myocardium and exacerbates the inflammatory response. The mechanisms of these effects are unknown; however, it may be that cocaine increases circulating catecholamines and consequently increases inflammatory cell adhesion to the coronary endothelium. Here, we examined the hypothesis that cocaine enhances inflammatory cell infiltration via catecholamine-induced upregulation of cell adhesion molecule (CAM) expression in adult BALB/c mouse hearts. Intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), endothelial leukocyte adhesion molecule-1 (E-selectin), and leukocyte adhesion molecule-1 (L-selectin) were detected by gene array analysis, RT-PCR, Western blotting, and immunohistochemical staining. CAMs were significantly upregulated in cocaine-treated mouse hearts. beta-Adrenergic stimulation with epinephrine also upregulated CAM expression, confirming the effects obtained with cocaine. Beta-adrenergic blockade with propranolol inhibited epinephrine-induced CAM expression. In hearts infused with polymorphonuclear neutrophils (PMN), an increased adhesion of PMN to the coronary endothelium was observed in cocaine-treated and epinephrine-treated mouse hearts compared with control hearts. Blocking antibodies against ICAM-1, E-selectin, and L-selectin significantly inhibited epinephrine-enhanced PMN adhesion, whereas anti-VCAM-1 had lesser effects. Our findings suggest that cocaine-induced neutrophil infiltration is mediated by beta-adrenergic stimulation through upregulation of CAM expression, which enhances PMN adhesion. Conversely, beta-adrenergic blockade with propranolol inhibits the effects of cocaine and epinephrine on CAM expression and decreases PMN adhesion to the coronary endothelium. These observations may be of significance for the development of preventative and therapeutic approaches to patients with cocaine- or catecholamine-induced myocarditis. Publication Type. Journal Article. Research Support, Non-U. S. Gov't. Research Support, U. S. Gov't, P. H. S. .
• 14738173 Authors. Mastrogiannis DS. O'Brien WF. Authors Full Name. Mastrogiannis, D S. O'Brien, W F. Institution. Department of Maternal Fetal Medicine, Good Samaritan Hospital, West Islip, New York, USA. Title. Cocaine affects prostaglandin production in human umbilical cord cell cultures. Source. Journal of Maternal-Fetal & Neonatal Medicine. 14(4): 261 -6, 2003 Oct. Local Messages*UTHSCSA LIBRARIES OWN JOURNAL. CLICK LIBRARY HOLDINGS FOR VOLS OWNED* Abstract. OBJECTIVE: To investigate the possible effects of cocaine on prostacyclin and prostaglandin (PG) E 2 production from endothelial cells derived from human umbilical cord. STUDY DESIGN: First-passaged endothelial cells derived from the umbilical vein were incubated with various doses of cocaine, procaine and lidocaine and 24 h later the supematants were assayed for prostacyclin metabolites 6 -keto-PGF 1 alpha and PGE 2. Cocaine concentrations tested were 0, 100, 500 and 1000 microg/ml. RESULTS: Cocaine produced a dose-dependent reduction in prostacyclin and PGE 2 production from endothelial cells (p) < 0. 05). Acetylcholinesterase (a possible detoxifier of cocaine) abolished the effect of cocaine on prostacyclin production. Procaine, an esteroltype anesthetic, produced a similar effect on prostacyclin production, an effect not observed with lidocaine. CONCLUSION: It is speculated that, when present in high concentrations, cocaine may affect vascular tone by inhibition of endothelial cell prostacyclin and PGE 2 release. Publication Type. Journal Article.
• 12757774 Authors. Togna GI. Togna AR. Graziani M. Franconi M. Authors Full Name. Togna, Giuseppina I. Togna, Anna Rita. Graziani, Manuela. Franconi, Matteo. Institution. Dipartimento di Fisiologia Umana e Farmacologia, Istituto di Farmacologia Medica, Universita di Roma La Sapienza, P. le A. Moro, 5 -00185 Rome, Italy. giuseppina. togna@uniroma 1. it Title. Testosterone and cocaine: vascular toxicity of their concomitant abuse. Source. Thrombosis Research. 109(4): 195 -201, 2003 Feb 15. Local Messages*UTHSCSA LIBRARIES OWN JOURNAL. CLICK LIBRARY HOLDINGS FOR VOLS OWNED* Abstract. Over the last few years, several studies have described an increase in the use of anabolicandrogenic steroids (AAS). More important, frequency of AAS use was significantly associated with frequency of psychotropic drug use, such as cocaine. Since information is not available on the effects of their concomitant abuse, and taking into account that cocaine and testosterone, when singly abused, are known to induce severe adverse effects on vascular system, our purpose was to evaluate in vitro the combined effect of these drugs on platelet and endothelial functions. Results show that testosterone, at concentrations not exerting any appreciably acute effects on their own, is capable of potentiating the cocaine effect on endothelial and platelet functions, indicating that concomitant use of testosterone and cocaine could result in enhancement of the thrombotic risk ascribed to these drugs. Publication Type. In Vitro. Journal Article.
• 16341998 Authors. Wu YW. Lynch JK. Nelson KB. Authors Full Name. Wu, Yvonne W. Lynch, John K. Nelson, Karin B. Institution. Department of Neurology, University of California San Francisco, California 94117, USA. Title. Perinatal arterial stroke: understanding mechanisms and outcomes. [Review] [103 refs] Source. Seminars in Neurology. 25(4): 424 -34, 2005 Dec. Local Messages*UTHSCSA LIBRARIES OWN JOURNAL. CLICK LIBRARY HOLDINGS FOR VOLS OWNED* Abstract. Arterial ischemic infarction occurring around the time of birth is an increasingly recognized cause of neurological disability in children. The rate of arterial infarction in neonates is as high as the annual incidence of large -vessel ischemic stroke in adults. Factors contributing to this increased risk of stroke among neonates include complications that occur before, during, and after delivery. Maternal conditions that have been associated with perinatal stroke in the fetus include prothrombotic disorders, cocaine abuse, and placental complications such as chorioamnionitis and placental vasculopathy. In many cases, the placenta is suspected to be the underlying embolic source for perinatal stroke, although data on placental pathology is often lacking. During the delivery process, an infant may develop a cervical arterial dissection that leads to stroke. Several conditions in the neonatal period predispose to perinatal stroke including prothrombotic disorders, congenital heart disease, meningitis, and systemic infection. Perinatal stroke may present with neonatal seizures during the first weeks of life or may be asymptomatic until months later when the infant is first noted to have pathological handedness. The outcome of perinatal stroke is variable and depends on severity, anatomic localization, and other factors not yet well characterized. As many as 50% of infants with documented stroke recognized in the newborn period do not develop a hemiparesis. The incidence, clinical presentation, pathogenesis, risk factors, and outcome of this increasingly recognized disorder are reviewed. [References: 103] Publication Type. Journal Article. Review.
• 15027587 Authors. Foidart JM. Seak-San S. Emonts P. Schaaps JP. Authors Full Name. Foidart, Jean-Michel. Seak-San, Sonteara. Emonts, Patrick. Schaaps, Jean-Pierre. Institution. Maternite Universitaire, CHR Citadelle, boulevard du 12 e-de-Ligne, 1, B-4000 Liege, Belgique. jmfoidart@ulg. ac. be Title[Vascular placental pathology in high-risk groups: definition and synopsis]. [Review] [89 refs] [French] Source. Annales de Medecine Interne. 154(5 -6): 332 -9, 2003 Sep-Oct. Local Messages*UTHSCSA LIBRARIES OWN JOURNAL. CLICK LIBRARY HOLDINGS FOR VOLS OWNED* Abstract. The vascular placental pathology (VPP) is associated with many etiologies. Some are the consequence of a maternal genetic or acquired predisposition. Others are associated with a chronic maternal disease (hypertension, lupus, obesity, diabetes, . . . ). Finally, some others are associated with placental implantation leading to fetal ischemia (multiple pregnancy, chorioangioma, primiparity, feto-placental hydrops) or to environmental (altitude) or nutritional factors (famine and specific alimentary depressions). We classify these factors into three categories according to the risk level (moderate, significant and elevated). While any of these factors can increase the risk of VPP, no one is sufficiently sensitive or specific in predict inevitable onset of VPP. In most cases VPP results from a combination of two (or more) risk factors. The risk factors of VPP classified as moderate include age (> or = 35 years), increased blood pressure during the second trimester of pregnancy, a new paternity, dietetic factors or environmental factors, smoking and controlled diabetes (class B, C), or inactive systemic diseases. Risk is significantly elevated among obese (BMI > or = 25), primiparous women, women with a past familial history (first degree) of preeclampsia or eclampsia, cocaine use or association of tobacco and caffeine use, increased placental mass (associated with twin pregnancy, fetal hydrops or molar pregnancy), uncontrolled diabetes, lupus, active scleroderma. Risk is considered to be high among patients with chronic hypertension, women with a past history of preeclampsia, diabetes (class D, F, R), patients with active systemic disease or with antiphospholipid antibodies or women with lupus or renal lesions and/or proteinuria as well as chronic kidney disease resulting in proteinuria, hypertension and renal insufficiency. Finally, the risk of VPP is considered to be increased in the presence of acquired thrombophilia. It remains moderate in the presence of isolated genetic thrombophilia, except in forms presenting with multiple genetic mutations or associated with an hyperhomocysteinemia. A "high-risk group" is defined among women with past history of deep venous thromboembolic events outside pregnancy, or with a past history of placental vascular pathology (intra-uterine death, placental abruptio, severe and precocious placental, intra-uterine growth retardation, early and repetitive fetal loss) and who, in addition, present with acquired thrombophilia (antiphospholipid antibodies, thrombocytemia), unique homozygous genetic thrombophilia, amultiple genetic thrombophilia or unique heterozygous genetic thrombophilia associated with hyperhomocysteinemia. Prophylactic treatment of acquired thrombophilia and of the multiple genetic forms or associated with hypercysteinemia is a logical rationale, particularly among women with a past history of placental vascular pathology, or with a past history of venous thromboembolic events. On the contrary, prophylaxis using low-molecular-weight heparin in the event of asymptomatic genetic thrombophilic mutations and for women without a past history of deep venous thromboembolism or vascular placental pathology remains controversial. [References: 89] Publication Type. English Abstract. Journal Article. Review.
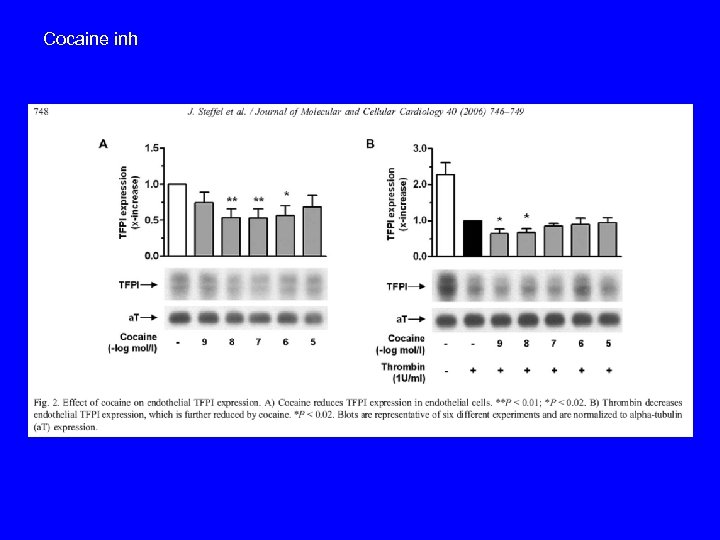
Cocaine inh
a679c5cbc2f15b50a064f61dd234aa01.ppt