081d6f5038c340554994bd327540936e.ppt
- Количество слайдов: 51
 Stroke Mimics Monica Witte, PA-C Department of Neurology North. Shore University Health System
Stroke Mimics Monica Witte, PA-C Department of Neurology North. Shore University Health System
 Objectives: • Define stroke mimics and understand the importance of recognizing a mimic in the inpatient setting • Discuss common mimics, including their pathophysiology and manifestations • Distinguish between an ischemic stroke and a mimic • Cases
Objectives: • Define stroke mimics and understand the importance of recognizing a mimic in the inpatient setting • Discuss common mimics, including their pathophysiology and manifestations • Distinguish between an ischemic stroke and a mimic • Cases
 What is a stroke mimic? • A condition that causes signs and symptoms similar to that of an acute stroke (ie focal neurologic deficit) • 19% of >400 pts presenting with suspected stroke were mimics in a 1995 study 1 and 31% of >300 pts were mimics in a 2006 study by Hand 2
What is a stroke mimic? • A condition that causes signs and symptoms similar to that of an acute stroke (ie focal neurologic deficit) • 19% of >400 pts presenting with suspected stroke were mimics in a 1995 study 1 and 31% of >300 pts were mimics in a 2006 study by Hand 2
 Characteristics of a mimic • Younger, female, fewer stroke risk factors 3 • Global aphasia with minimal to no paresis 4 • • Milder baseline stroke severity (median admission NIHSS of 4 in mimics compared to 8 in ischemic stroke)5 Other studies have found no distinction in gender/age/risk factors
Characteristics of a mimic • Younger, female, fewer stroke risk factors 3 • Global aphasia with minimal to no paresis 4 • • Milder baseline stroke severity (median admission NIHSS of 4 in mimics compared to 8 in ischemic stroke)5 Other studies have found no distinction in gender/age/risk factors
 Common acute stroke mimics • Postictal deficits (Todd paralysis) (21%)1 • Sepsis (13%)1 • Metabolic (hypoglycemia, ETOH intox, hyponatremia, hepatic encephalopathy, etc) (11%)1 • Migraine with aura • Mass lesions • Peripheral vestibulopathy • Conversion reaction
Common acute stroke mimics • Postictal deficits (Todd paralysis) (21%)1 • Sepsis (13%)1 • Metabolic (hypoglycemia, ETOH intox, hyponatremia, hepatic encephalopathy, etc) (11%)1 • Migraine with aura • Mass lesions • Peripheral vestibulopathy • Conversion reaction
 Migraine with aura/hemiplegic migraine
Migraine with aura/hemiplegic migraine
 Migraine facts • Typically characterized by unilateral, pulsating pain a/w n/v and/or photo/phonophobia • Aura occurs in 20% • Lifetime prevalence: women 43%, men 18%6 • Only 37% of Americans with chronic migraine (≥ 15 HA/m, ≥ 4 hrs/d) are employed full time 6 • Common triggers: diet, sleep disturbance, head trauma, meds, hormones, dehydration
Migraine facts • Typically characterized by unilateral, pulsating pain a/w n/v and/or photo/phonophobia • Aura occurs in 20% • Lifetime prevalence: women 43%, men 18%6 • Only 37% of Americans with chronic migraine (≥ 15 HA/m, ≥ 4 hrs/d) are employed full time 6 • Common triggers: diet, sleep disturbance, head trauma, meds, hormones, dehydration
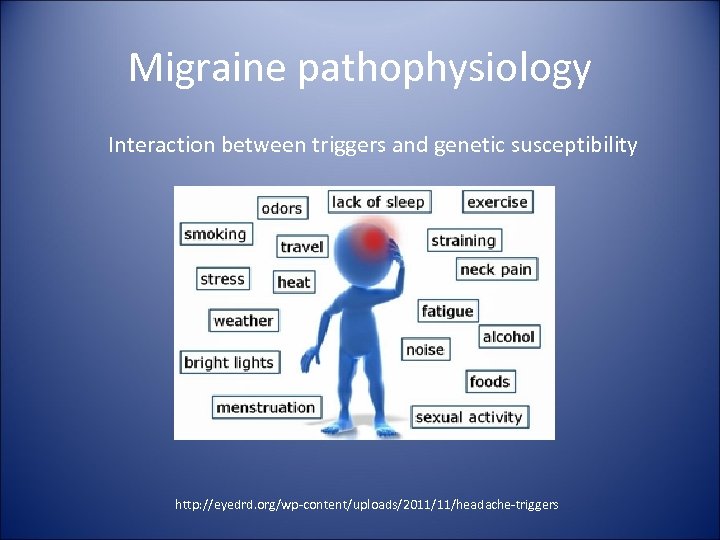 Migraine pathophysiology Interaction between triggers and genetic susceptibility http: //eyedrd. org/wp-content/uploads/2011/11/headache-triggers
Migraine pathophysiology Interaction between triggers and genetic susceptibility http: //eyedrd. org/wp-content/uploads/2011/11/headache-triggers
 Migraine pathophysiology • Once thought to be primarily vascular • A complex sequence of changes occur – Cortical spreading depression – Trigeminovascular system • Converge in trigeminal nucleus caudalis • Fibers ascend to cortical/subcortical sites, incl thalamus • Trigeminal ganglion stimulation-> vasoactive neuropeptides (substance P, CGRP)->inflammation (vasodilation, protein extravasation) – Sensitization
Migraine pathophysiology • Once thought to be primarily vascular • A complex sequence of changes occur – Cortical spreading depression – Trigeminovascular system • Converge in trigeminal nucleus caudalis • Fibers ascend to cortical/subcortical sites, incl thalamus • Trigeminal ganglion stimulation-> vasoactive neuropeptides (substance P, CGRP)->inflammation (vasodilation, protein extravasation) – Sensitization
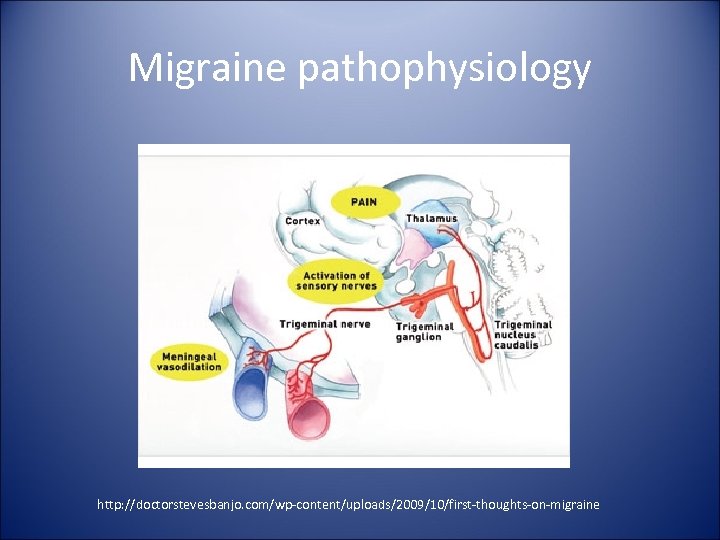 Migraine pathophysiology http: //doctorstevesbanjo. com/wp-content/uploads/2009/10/first-thoughts-on-migraine
Migraine pathophysiology http: //doctorstevesbanjo. com/wp-content/uploads/2009/10/first-thoughts-on-migraine
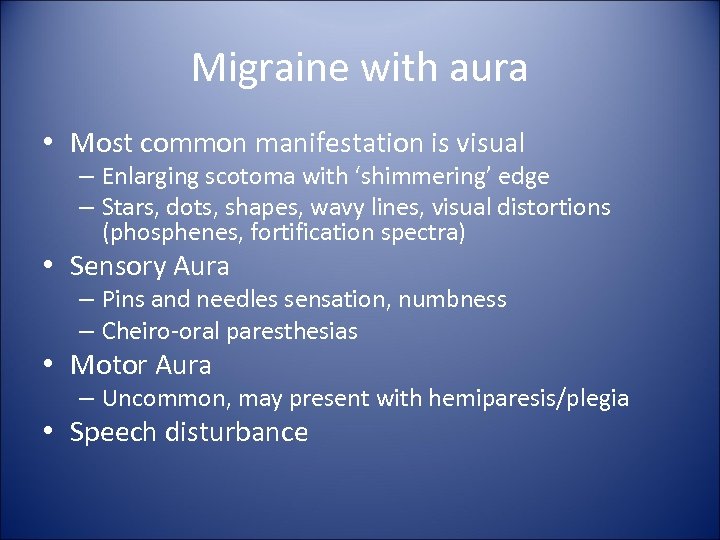 Migraine with aura • Most common manifestation is visual – Enlarging scotoma with ‘shimmering’ edge – Stars, dots, shapes, wavy lines, visual distortions (phosphenes, fortification spectra) • Sensory Aura – Pins and needles sensation, numbness – Cheiro-oral paresthesias • Motor Aura – Uncommon, may present with hemiparesis/plegia • Speech disturbance
Migraine with aura • Most common manifestation is visual – Enlarging scotoma with ‘shimmering’ edge – Stars, dots, shapes, wavy lines, visual distortions (phosphenes, fortification spectra) • Sensory Aura – Pins and needles sensation, numbness – Cheiro-oral paresthesias • Motor Aura – Uncommon, may present with hemiparesis/plegia • Speech disturbance
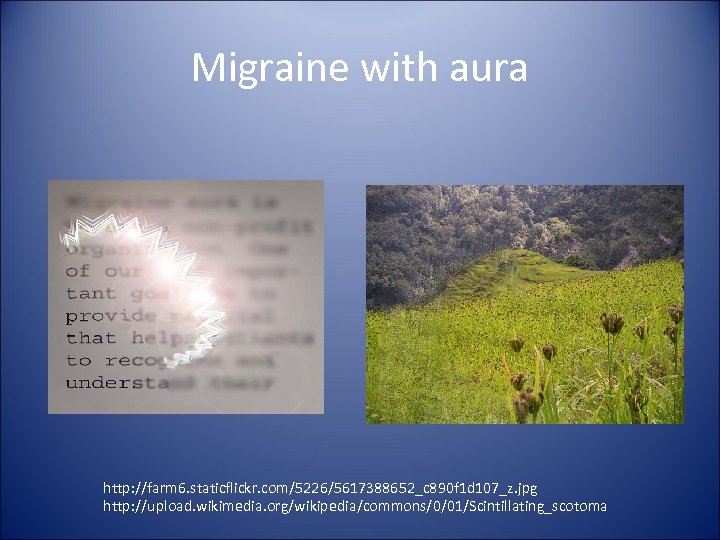 Migraine with aura http: //farm 6. staticflickr. com/5226/5617388652_c 890 f 1 d 107_z. jpg http: //upload. wikimedia. org/wikipedia/commons/0/01/Scintillating_scotoma
Migraine with aura http: //farm 6. staticflickr. com/5226/5617388652_c 890 f 1 d 107_z. jpg http: //upload. wikimedia. org/wikipedia/commons/0/01/Scintillating_scotoma
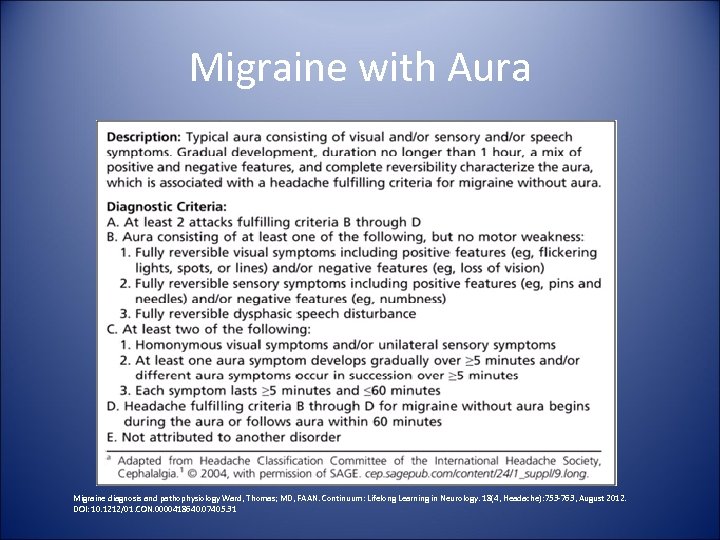 Migraine with Aura Migraine diagnosis and pathophysiology Ward, Thomas; MD, FAAN. Continuum: Lifelong Learning in Neurology. 18(4, Headache): 753 -763, August 2012. DOI: 10. 1212/01. CON. 0000418640. 07405. 31
Migraine with Aura Migraine diagnosis and pathophysiology Ward, Thomas; MD, FAAN. Continuum: Lifelong Learning in Neurology. 18(4, Headache): 753 -763, August 2012. DOI: 10. 1212/01. CON. 0000418640. 07405. 31
 Migraine with aura Dysphasic speech disturbance Reporter Serene Branson on-air
Migraine with aura Dysphasic speech disturbance Reporter Serene Branson on-air
 Hemiplegic migraine • Aura of weakness 5 min – 24 hrs but can last days; never the only type of aura during an attack • Visual->sensory-> motor->aphasic-> brainstem • Weakness typically moves from hand->arm->face • Can switch sides b/t, during attacks; may be b/l in FHM • Rare - est prevalence is 0. 01 % 7 • Avg age of onset 12 to 17 years
Hemiplegic migraine • Aura of weakness 5 min – 24 hrs but can last days; never the only type of aura during an attack • Visual->sensory-> motor->aphasic-> brainstem • Weakness typically moves from hand->arm->face • Can switch sides b/t, during attacks; may be b/l in FHM • Rare - est prevalence is 0. 01 % 7 • Avg age of onset 12 to 17 years
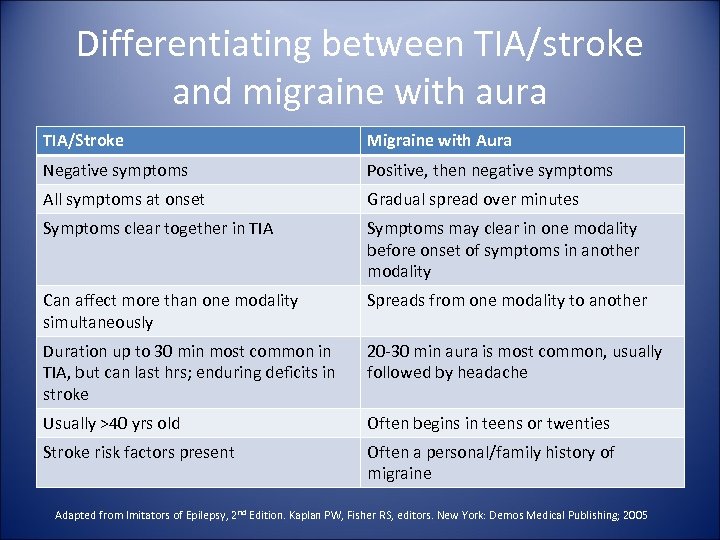 Differentiating between TIA/stroke and migraine with aura TIA/Stroke Migraine with Aura Negative symptoms Positive, then negative symptoms All symptoms at onset Gradual spread over minutes Symptoms clear together in TIA Symptoms may clear in one modality before onset of symptoms in another modality Can affect more than one modality simultaneously Spreads from one modality to another Duration up to 30 min most common in TIA, but can last hrs; enduring deficits in stroke 20 -30 min aura is most common, usually followed by headache Usually >40 yrs old Often begins in teens or twenties Stroke risk factors present Often a personal/family history of migraine Adapted from Imitators of Epilepsy, 2 nd Edition. Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005
Differentiating between TIA/stroke and migraine with aura TIA/Stroke Migraine with Aura Negative symptoms Positive, then negative symptoms All symptoms at onset Gradual spread over minutes Symptoms clear together in TIA Symptoms may clear in one modality before onset of symptoms in another modality Can affect more than one modality simultaneously Spreads from one modality to another Duration up to 30 min most common in TIA, but can last hrs; enduring deficits in stroke 20 -30 min aura is most common, usually followed by headache Usually >40 yrs old Often begins in teens or twenties Stroke risk factors present Often a personal/family history of migraine Adapted from Imitators of Epilepsy, 2 nd Edition. Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005
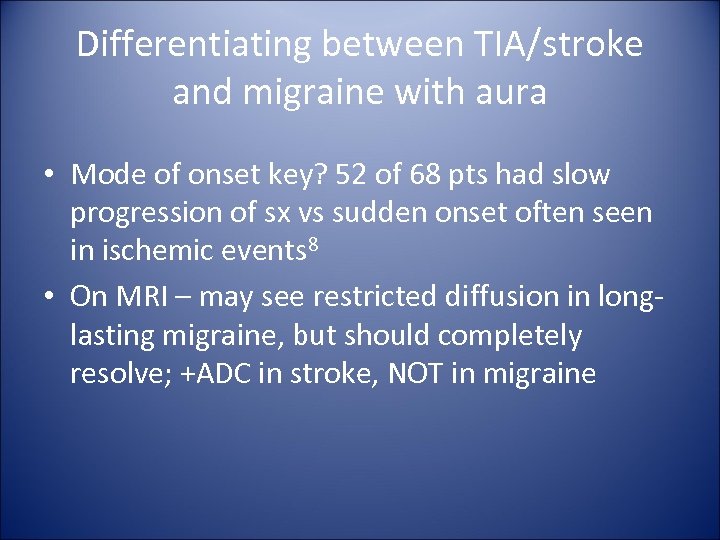 Differentiating between TIA/stroke and migraine with aura • Mode of onset key? 52 of 68 pts had slow progression of sx vs sudden onset often seen in ischemic events 8 • On MRI – may see restricted diffusion in longlasting migraine, but should completely resolve; +ADC in stroke, NOT in migraine
Differentiating between TIA/stroke and migraine with aura • Mode of onset key? 52 of 68 pts had slow progression of sx vs sudden onset often seen in ischemic events 8 • On MRI – may see restricted diffusion in longlasting migraine, but should completely resolve; +ADC in stroke, NOT in migraine
 An interesting study… • 2012 study looked at 1850 consecutive suspected strokes 9 • 1% (20) ultimately dx w/migraine with aura • Hypoperfusion found in 70% – >1 vascular territory affected in ALL – PCA area affected in visual aura; MCA area with motor or speech disturbance – Complete resolution at follow-up
An interesting study… • 2012 study looked at 1850 consecutive suspected strokes 9 • 1% (20) ultimately dx w/migraine with aura • Hypoperfusion found in 70% – >1 vascular territory affected in ALL – PCA area affected in visual aura; MCA area with motor or speech disturbance – Complete resolution at follow-up
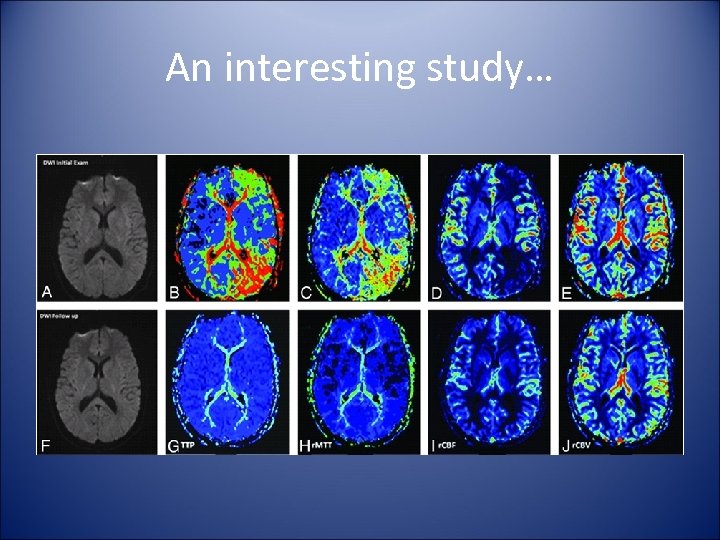 An interesting study…
An interesting study…
 Postictal paresis (Todd paralysis)
Postictal paresis (Todd paralysis)
 What is a seizure? Episode of neurologic dysfunction with abnormal neuronal firing presenting with changes in: – – motor control sensory perception behavior autonomic function 10 Epilepsy - name given to recurrent, spontaneous seizures that are suggestive of ongoing altered electrical activity
What is a seizure? Episode of neurologic dysfunction with abnormal neuronal firing presenting with changes in: – – motor control sensory perception behavior autonomic function 10 Epilepsy - name given to recurrent, spontaneous seizures that are suggestive of ongoing altered electrical activity
 Seizure Pathophysiology Disruption in the normal balance b/t excitatory and inhibitory currents in the brain Mediated via 2 types of ion channels – – Voltage gated – activated by changes in membrane potential. Na/Ca are excitatory; K/Cl are inhibitory Ligand gated – activated by NTs. Glutamate is excitatory; GABA is inhibitory Glial cells help regulate ion/NT concentrations
Seizure Pathophysiology Disruption in the normal balance b/t excitatory and inhibitory currents in the brain Mediated via 2 types of ion channels – – Voltage gated – activated by changes in membrane potential. Na/Ca are excitatory; K/Cl are inhibitory Ligand gated – activated by NTs. Glutamate is excitatory; GABA is inhibitory Glial cells help regulate ion/NT concentrations
 Seizure Pathophysiology Anything that alters the balance b/t excitation and inhibition: trauma, infection, drugs, etc. . . Recurrent seizures -> decreased threshold for additional seizures http: //www. socialsecurityinsider. com/wp-content/uploads/2008/11/istock_000004646701 xsmall. jpg
Seizure Pathophysiology Anything that alters the balance b/t excitation and inhibition: trauma, infection, drugs, etc. . . Recurrent seizures -> decreased threshold for additional seizures http: //www. socialsecurityinsider. com/wp-content/uploads/2008/11/istock_000004646701 xsmall. jpg
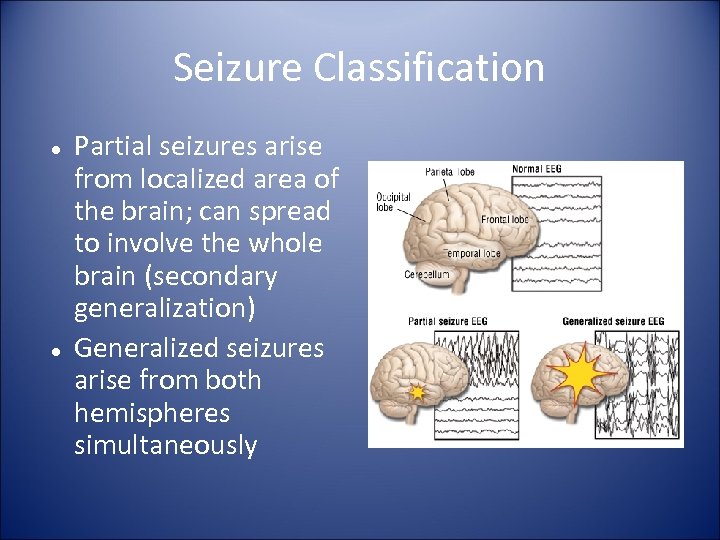 Seizure Classification Partial seizures arise from localized area of the brain; can spread to involve the whole brain (secondary generalization) Generalized seizures arise from both hemispheres simultaneously
Seizure Classification Partial seizures arise from localized area of the brain; can spread to involve the whole brain (secondary generalization) Generalized seizures arise from both hemispheres simultaneously
 What is Todd paralysis? Postictal phenomenon->hemiparesis/plegia contralateral to seizure focus May include visual disturbance, rarely hemineglect Results from complex partial or generalized seizures Occurs in 13% of seizure cases 11 Can last b/t 0. 5 and 36 hrs
What is Todd paralysis? Postictal phenomenon->hemiparesis/plegia contralateral to seizure focus May include visual disturbance, rarely hemineglect Results from complex partial or generalized seizures Occurs in 13% of seizure cases 11 Can last b/t 0. 5 and 36 hrs
 So. . . who is Todd? Robert Bentley Todd (18091860) – Clinician, anatomist, pathologist, physiologist – Introduced the terms afferent and efferent – Founded King's College Hospital – London – First to formulate an electrical theory of epilepsy
So. . . who is Todd? Robert Bentley Todd (18091860) – Clinician, anatomist, pathologist, physiologist – Introduced the terms afferent and efferent – Founded King's College Hospital – London – First to formulate an electrical theory of epilepsy
 Todd's hypothesis “Epileptic hemiplegia” - he stated that: 'A paralytic state remains sometimes after the epileptic convulsion. . particularly the case when the convulsion has affected only one side or one limb. . . will remain paralytic for some hours or even days. . . but it will ultimately perfectly recover. ' Attributed this to 'depression or exhaustion' induced by the excessive discharge of cells 12
Todd's hypothesis “Epileptic hemiplegia” - he stated that: 'A paralytic state remains sometimes after the epileptic convulsion. . particularly the case when the convulsion has affected only one side or one limb. . . will remain paralytic for some hours or even days. . . but it will ultimately perfectly recover. ' Attributed this to 'depression or exhaustion' induced by the excessive discharge of cells 12
 Other explanations Gowers (1845 -1915) a British neurologist, felt that inhibition of motor centers, not exhaustion, led to postictal paralysis Yarnell (1975) and Kimura (1998) demonstrated hyperperfusion in pts w/postictal paralysis; ? vasomotor, metabolic changes Multifactorial – NT depletion, desensitization, altered local cerebral blood flow, inhibition?
Other explanations Gowers (1845 -1915) a British neurologist, felt that inhibition of motor centers, not exhaustion, led to postictal paralysis Yarnell (1975) and Kimura (1998) demonstrated hyperperfusion in pts w/postictal paralysis; ? vasomotor, metabolic changes Multifactorial – NT depletion, desensitization, altered local cerebral blood flow, inhibition?
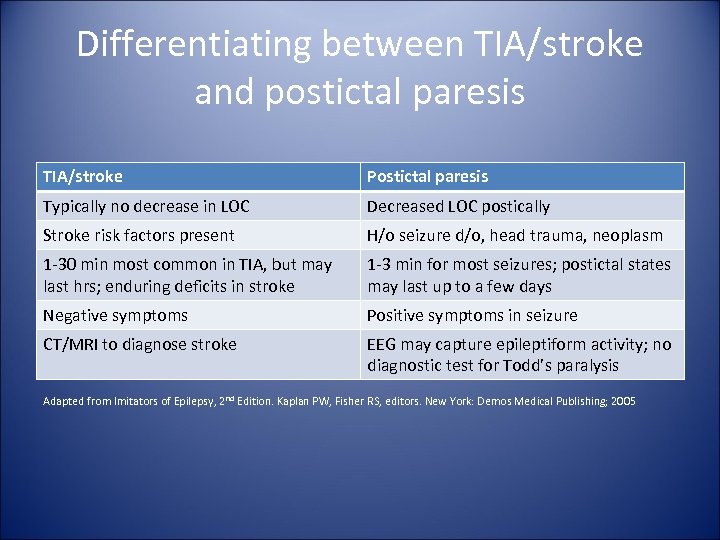 Differentiating between TIA/stroke and postictal paresis TIA/stroke Postictal paresis Typically no decrease in LOC Decreased LOC postically Stroke risk factors present H/o seizure d/o, head trauma, neoplasm 1 -30 min most common in TIA, but may last hrs; enduring deficits in stroke 1 -3 min for most seizures; postictal states may last up to a few days Negative symptoms Positive symptoms in seizure CT/MRI to diagnose stroke EEG may capture epileptiform activity; no diagnostic test for Todd’s paralysis Adapted from Imitators of Epilepsy, 2 nd Edition. Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005
Differentiating between TIA/stroke and postictal paresis TIA/stroke Postictal paresis Typically no decrease in LOC Decreased LOC postically Stroke risk factors present H/o seizure d/o, head trauma, neoplasm 1 -30 min most common in TIA, but may last hrs; enduring deficits in stroke 1 -3 min for most seizures; postictal states may last up to a few days Negative symptoms Positive symptoms in seizure CT/MRI to diagnose stroke EEG may capture epileptiform activity; no diagnostic test for Todd’s paralysis Adapted from Imitators of Epilepsy, 2 nd Edition. Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005
 Other Stroke Mimics
Other Stroke Mimics
 Toxic-metabolic insults Well known phenomenon of hemiplegia and aphasia in hypoglycemia (<45 mg/dl in studies)14 – – – Pathophysiology unclear Diminished LOC may or may not be present Can resolve immediately w/IV glucose, or take hrs Hyponatremia, uremia, hepatic encephalopathy, etc. . . may also mimic stroke PMH important, as are appropriate lab studies; may see asterixis on exam
Toxic-metabolic insults Well known phenomenon of hemiplegia and aphasia in hypoglycemia (<45 mg/dl in studies)14 – – – Pathophysiology unclear Diminished LOC may or may not be present Can resolve immediately w/IV glucose, or take hrs Hyponatremia, uremia, hepatic encephalopathy, etc. . . may also mimic stroke PMH important, as are appropriate lab studies; may see asterixis on exam
 CNS tumors Includes primary tumors, abscesses, metastatic lesions Symptoms are typically progressive but onset may be abrupt, possibly due to intralesional hemorrhage, hydrocephalus or seizure from edema/mass effect 15 History and imaging help make diagnosis
CNS tumors Includes primary tumors, abscesses, metastatic lesions Symptoms are typically progressive but onset may be abrupt, possibly due to intralesional hemorrhage, hydrocephalus or seizure from edema/mass effect 15 History and imaging help make diagnosis
 Why is it important to differentiate mimic from stroke? • Risk of symptomatic ICH about 6% in t. PA treated pts 16 but…. – – No inc risk in mimics and no need for hesitation if c/w acute stroke and a t. PA candidate 2010 retrospective study of >500 consecutive ischemic stroke admits given t. PA; 10. 4% mimics - no s. ICH 5 • May delay appropriate treatments (ie delay in migraine specific therapy or initiation of AED in seizure)
Why is it important to differentiate mimic from stroke? • Risk of symptomatic ICH about 6% in t. PA treated pts 16 but…. – – No inc risk in mimics and no need for hesitation if c/w acute stroke and a t. PA candidate 2010 retrospective study of >500 consecutive ischemic stroke admits given t. PA; 10. 4% mimics - no s. ICH 5 • May delay appropriate treatments (ie delay in migraine specific therapy or initiation of AED in seizure)
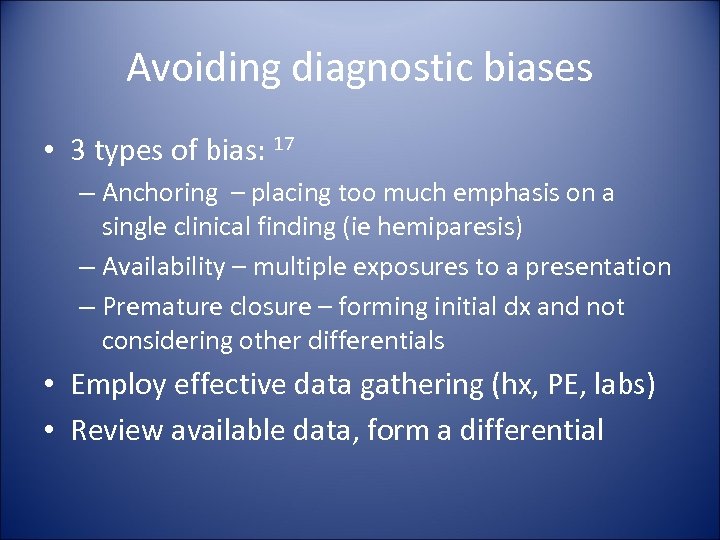 Avoiding diagnostic biases • 3 types of bias: 17 – Anchoring – placing too much emphasis on a single clinical finding (ie hemiparesis) – Availability – multiple exposures to a presentation – Premature closure – forming initial dx and not considering other differentials • Employ effective data gathering (hx, PE, labs) • Review available data, form a differential
Avoiding diagnostic biases • 3 types of bias: 17 – Anchoring – placing too much emphasis on a single clinical finding (ie hemiparesis) – Availability – multiple exposures to a presentation – Premature closure – forming initial dx and not considering other differentials • Employ effective data gathering (hx, PE, labs) • Review available data, form a differential
 Cases
Cases
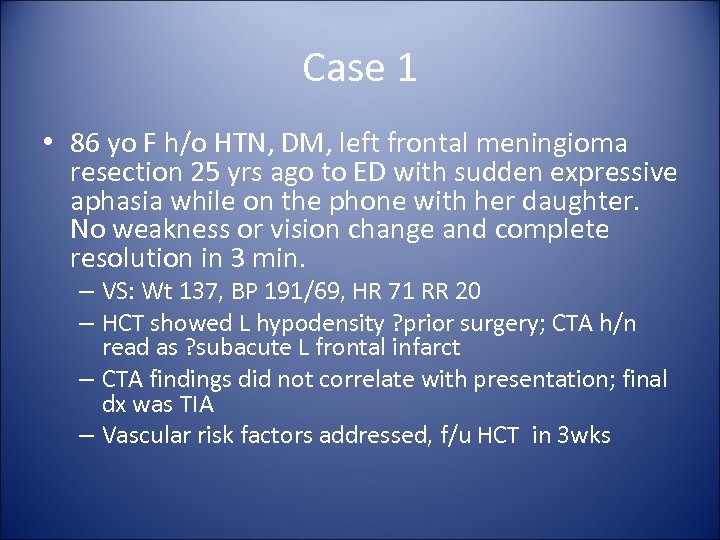 Case 1 • 86 yo F h/o HTN, DM, left frontal meningioma resection 25 yrs ago to ED with sudden expressive aphasia while on the phone with her daughter. No weakness or vision change and complete resolution in 3 min. – VS: Wt 137, BP 191/69, HR 71 RR 20 – HCT showed L hypodensity ? prior surgery; CTA h/n read as ? subacute L frontal infarct – CTA findings did not correlate with presentation; final dx was TIA – Vascular risk factors addressed, f/u HCT in 3 wks
Case 1 • 86 yo F h/o HTN, DM, left frontal meningioma resection 25 yrs ago to ED with sudden expressive aphasia while on the phone with her daughter. No weakness or vision change and complete resolution in 3 min. – VS: Wt 137, BP 191/69, HR 71 RR 20 – HCT showed L hypodensity ? prior surgery; CTA h/n read as ? subacute L frontal infarct – CTA findings did not correlate with presentation; final dx was TIA – Vascular risk factors addressed, f/u HCT in 3 wks
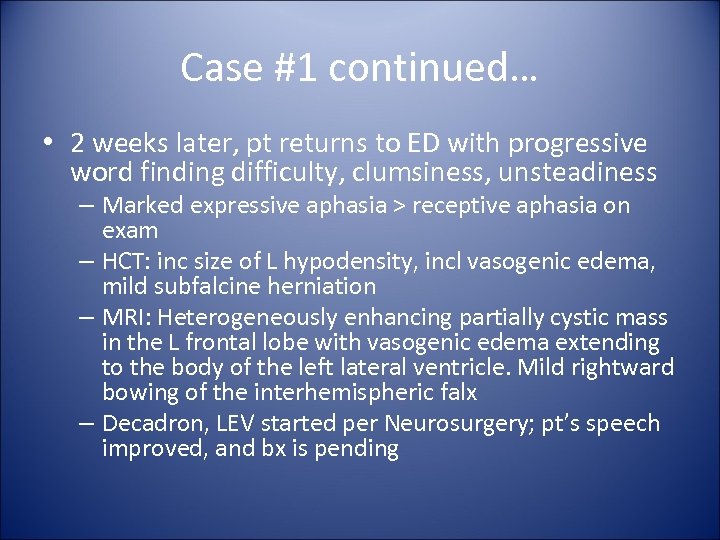 Case #1 continued… • 2 weeks later, pt returns to ED with progressive word finding difficulty, clumsiness, unsteadiness – Marked expressive aphasia > receptive aphasia on exam – HCT: inc size of L hypodensity, incl vasogenic edema, mild subfalcine herniation – MRI: Heterogeneously enhancing partially cystic mass in the L frontal lobe with vasogenic edema extending to the body of the left lateral ventricle. Mild rightward bowing of the interhemispheric falx – Decadron, LEV started per Neurosurgery; pt’s speech improved, and bx is pending
Case #1 continued… • 2 weeks later, pt returns to ED with progressive word finding difficulty, clumsiness, unsteadiness – Marked expressive aphasia > receptive aphasia on exam – HCT: inc size of L hypodensity, incl vasogenic edema, mild subfalcine herniation – MRI: Heterogeneously enhancing partially cystic mass in the L frontal lobe with vasogenic edema extending to the body of the left lateral ventricle. Mild rightward bowing of the interhemispheric falx – Decadron, LEV started per Neurosurgery; pt’s speech improved, and bx is pending
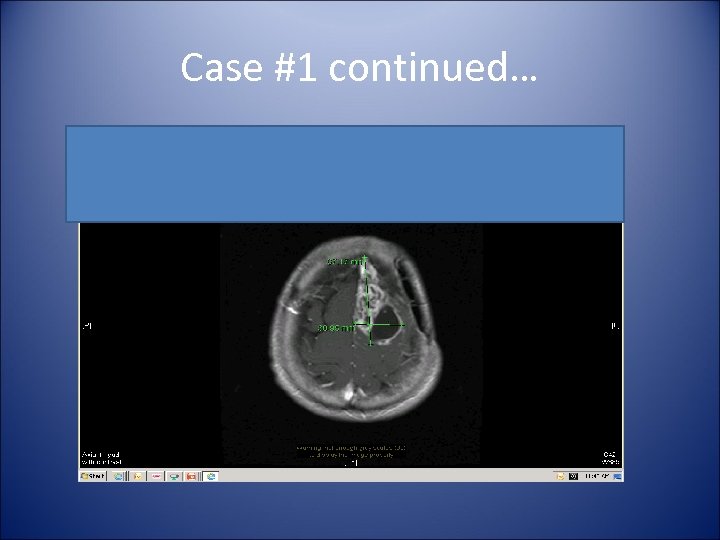 Case #1 continued…
Case #1 continued…
 Case 2 • Mrs. Jackson calls EMS because she woke up in the morning to find her 35 -year-old husband lying in bed confused, exhibiting a left-side facial droop and not moving his left arm and leg. EMS arrived and see the patient lying in bed confused with slurred speech, left-side facial droop and left side-paralysis. They administer oxygen (O 2) via non-rebreather mask at 12 L/min and start an IV of normal saline TKO and transported to the stroke center on the ECG monitor. En route, the crew checks his blood glucose serum level; it’s 35 mg/d. L. They administer an amp (50 cc's) of dextrose 50% D 50 in water, and the symptoms cleared. At the hospital, the emergency department (ED) physician consults with the neurology department, and an MRI is performed and found to be negative for stroke. http: //www. jems. com/article/patient-care/identifying-diseasesmimic-str
Case 2 • Mrs. Jackson calls EMS because she woke up in the morning to find her 35 -year-old husband lying in bed confused, exhibiting a left-side facial droop and not moving his left arm and leg. EMS arrived and see the patient lying in bed confused with slurred speech, left-side facial droop and left side-paralysis. They administer oxygen (O 2) via non-rebreather mask at 12 L/min and start an IV of normal saline TKO and transported to the stroke center on the ECG monitor. En route, the crew checks his blood glucose serum level; it’s 35 mg/d. L. They administer an amp (50 cc's) of dextrose 50% D 50 in water, and the symptoms cleared. At the hospital, the emergency department (ED) physician consults with the neurology department, and an MRI is performed and found to be negative for stroke. http: //www. jems. com/article/patient-care/identifying-diseasesmimic-str
 Case 3 • 74 yo M h/o CAD s/p CABG, HLD, DM 2, R PCA territory stroke to ED with R hemiparesis, slurred speech after syncopal episode at Ophtho office. NIHSS 6 in ED (2 pts from old stroke) – – – VS: Wt BP 189/90 (dec to 160 systolic with 5 mg labetalol), HR 92 RR 18 No early infarct signs on HCT t. PA given - shortly after, RUE/RLE weakness resolved; slight R facial droop/dysarthia from prior stroke
Case 3 • 74 yo M h/o CAD s/p CABG, HLD, DM 2, R PCA territory stroke to ED with R hemiparesis, slurred speech after syncopal episode at Ophtho office. NIHSS 6 in ED (2 pts from old stroke) – – – VS: Wt BP 189/90 (dec to 160 systolic with 5 mg labetalol), HR 92 RR 18 No early infarct signs on HCT t. PA given - shortly after, RUE/RLE weakness resolved; slight R facial droop/dysarthia from prior stroke
 Case 3 continued… • Additional hx: – • During VF test, pt suddenly stared into space, unresponsive for 1. 5 min; confused, pale MRI/A - no evidence of acute stroke; chronic strokes, severe intracranial atherosclerotic disease • Normal EEG • Trileptal 150 mg BID for CPS
Case 3 continued… • Additional hx: – • During VF test, pt suddenly stared into space, unresponsive for 1. 5 min; confused, pale MRI/A - no evidence of acute stroke; chronic strokes, severe intracranial atherosclerotic disease • Normal EEG • Trileptal 150 mg BID for CPS
 Case 4 46 yo F h/o HTN, migraine with/without aura (scotoma) since birth of her child 10 yrs ago to ED with slow progression over min of L hand->arm->face->numbness while shoveling snow. Gradual resolution over 10 min ->mild apical HA x few hrs • Other hx: – Few mos ago: • episode of nausea, lightheadedness, unknowingly speaking native language x 10 s at work ->dull apical HA • ‘Lost time’ briefly at work. Outpatient 24 hr EEG was normal VS: Wt 149 lbs, BP 120/80, HR 94, RR 18 – Neurologic exam non-focal
Case 4 46 yo F h/o HTN, migraine with/without aura (scotoma) since birth of her child 10 yrs ago to ED with slow progression over min of L hand->arm->face->numbness while shoveling snow. Gradual resolution over 10 min ->mild apical HA x few hrs • Other hx: – Few mos ago: • episode of nausea, lightheadedness, unknowingly speaking native language x 10 s at work ->dull apical HA • ‘Lost time’ briefly at work. Outpatient 24 hr EEG was normal VS: Wt 149 lbs, BP 120/80, HR 94, RR 18 – Neurologic exam non-focal
 Differential diagnosis?
Differential diagnosis?
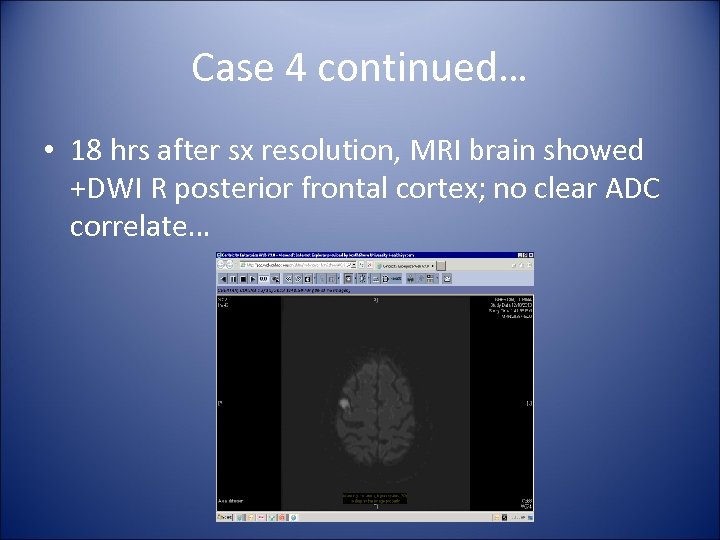 Case 4 continued… • 18 hrs after sx resolution, MRI brain showed +DWI R posterior frontal cortex; no clear ADC correlate…
Case 4 continued… • 18 hrs after sx resolution, MRI brain showed +DWI R posterior frontal cortex; no clear ADC correlate…
 Does this change your differential?
Does this change your differential?
 Case 4 continued… • Ordered MRA along with limited cut repeat MRI: persistent +DWI, now with +ADC = migraine assoc infarct • D/c on nortriptyline for prevention • Few mos later: At work, wave of nausea, speaking native language, witnessed lip smacking, lost time x 1 min – c/w CPS; earlier events also likely seizure – Switched to TPX->Depakote – Currently no further events
Case 4 continued… • Ordered MRA along with limited cut repeat MRI: persistent +DWI, now with +ADC = migraine assoc infarct • D/c on nortriptyline for prevention • Few mos later: At work, wave of nausea, speaking native language, witnessed lip smacking, lost time x 1 min – c/w CPS; earlier events also likely seizure – Switched to TPX->Depakote – Currently no further events
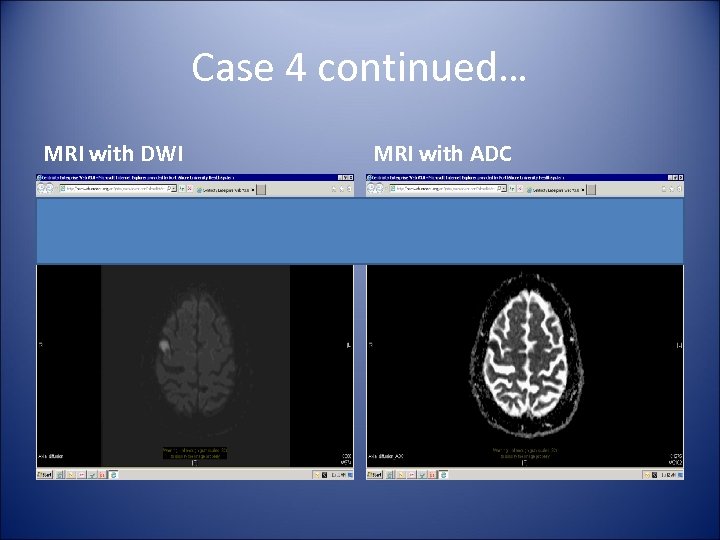 Case 4 continued… MRI with DWI MRI with ADC
Case 4 continued… MRI with DWI MRI with ADC
 Conclusion • Many conditions share clinical features with TIA/stroke • Thorough hx, PE, labs, judicious use of imaging can help differentiate • Use of t. PA shown to be safe in mimics
Conclusion • Many conditions share clinical features with TIA/stroke • Thorough hx, PE, labs, judicious use of imaging can help differentiate • Use of t. PA shown to be safe in mimics
 Questions?
Questions?
 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Libman R, Wirkowski E, Alvir J, Rao T. Conditions that mimic stroke in the emergency department: Implications for acute stroke trials. Archives of Neurology. 1993; 52: 1119 -1122. Hand P, Kwan J, Lindley R, Dennis M, Wardlaw J. Distinguishing between stroke and mimic at the bedside: The brain attack study. Stroke. 2006; 37: 769 -775. Zinkstok S, Engelter S, Gensicke H, et al. Safety of thrombolysis in stroke mimcs. Stroke. 2013; 44: 1080 -1084 Winkler D, Fluri F, Fuhr P, et al. Thrombolysis in stroke mimics: Frequency, clinical characteristics and outcome. Stroke. 2009; 40: 1522 -1525 Tsivgoulis G, Alexandrov A, Chang J, et al. Safety and outcomes of intravenous thrombolysis in stroke mimics. Stroke. 2011; 42: 17711774 Ward, T. Migraine diagnosis and pathophysiology. Continuum Lifelong Learning Neurol. 2012; 18: 753 -763. Black D, Robertson C. Hemiplegic migraine. In: Up. To. Date, Swanson J, (Ed), Up. To. Date, Waltham, MA, 2014. Bousser M, Welch K. Relation between migraine and stroke. Lancet Neurol. 2005; 4: 533 -542 Floery D, Vosko M, Fellner F, et al. Acute-onset migrainous aura mimicking acute stroke: MR perfusion imaging features. Am J Neuroradiol. 2012; 33: 1546 -1552 Stafstrom C, Rho J. Pathophysiology of seizures and epilepsy. In: Up. To. Date, Pedley T, (Ed), Up. To. Date, Waltham, MA, 2014. Gallmetzer P, Leutmezer F, Serles W, et al. Postictal paresis in focal epilepsies – incidence, duration, and causes. Neurology. 2004; 62: 2160 -2164. Binder D. A history of Todd and his paralysis. Neurosurgery. 2004; 54: 480 -487. Silverstein A, Alexander J. Acute postictal cerebral imaging. Am J Neuroradiol. 1998; 19: 1485 -1488. Montgomery BM, Pinner CA, Newberry SC. Transient hypoglycemic hemiplegia. Arch Int Med. 1964; 114: 680 -684. Snyder H, Robinson K, Shah D, Brennan R, Handrigan M. Signs and symptoms of patients with brain tumors presenting to the emergency department. Jour Emerg Med. 1993; 11: 253 -258. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA stroke study group. Stroke. 1997; 28: 2109 -2118 Brosinski C. Implementing diagnostic reasoning to differentiate Todd’s paralysis from acute ischemic stroke. Advanced Emergency Nursing Journal. 2014; 36: 78 -86. Scott P, Silbergleit R. Misdiagnosis of stroke in tissue plasminogen activator treated patients: Characteristics and outcomes. Annals of Emergency Medicine. 2003; 42: 611 -618. Barrett K, Levine J, Johnston K. Diagnosis of stroke and stroke mimics in the emergency setting. Continuum Lifelong Learning Neurol. 2008; 14: 13 -27. Nau K, Crocco T, Biola J, Larrabee H. Is it stroke, or something else? The Journal of Family Practice. 2010; 59: 26 -31.
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Libman R, Wirkowski E, Alvir J, Rao T. Conditions that mimic stroke in the emergency department: Implications for acute stroke trials. Archives of Neurology. 1993; 52: 1119 -1122. Hand P, Kwan J, Lindley R, Dennis M, Wardlaw J. Distinguishing between stroke and mimic at the bedside: The brain attack study. Stroke. 2006; 37: 769 -775. Zinkstok S, Engelter S, Gensicke H, et al. Safety of thrombolysis in stroke mimcs. Stroke. 2013; 44: 1080 -1084 Winkler D, Fluri F, Fuhr P, et al. Thrombolysis in stroke mimics: Frequency, clinical characteristics and outcome. Stroke. 2009; 40: 1522 -1525 Tsivgoulis G, Alexandrov A, Chang J, et al. Safety and outcomes of intravenous thrombolysis in stroke mimics. Stroke. 2011; 42: 17711774 Ward, T. Migraine diagnosis and pathophysiology. Continuum Lifelong Learning Neurol. 2012; 18: 753 -763. Black D, Robertson C. Hemiplegic migraine. In: Up. To. Date, Swanson J, (Ed), Up. To. Date, Waltham, MA, 2014. Bousser M, Welch K. Relation between migraine and stroke. Lancet Neurol. 2005; 4: 533 -542 Floery D, Vosko M, Fellner F, et al. Acute-onset migrainous aura mimicking acute stroke: MR perfusion imaging features. Am J Neuroradiol. 2012; 33: 1546 -1552 Stafstrom C, Rho J. Pathophysiology of seizures and epilepsy. In: Up. To. Date, Pedley T, (Ed), Up. To. Date, Waltham, MA, 2014. Gallmetzer P, Leutmezer F, Serles W, et al. Postictal paresis in focal epilepsies – incidence, duration, and causes. Neurology. 2004; 62: 2160 -2164. Binder D. A history of Todd and his paralysis. Neurosurgery. 2004; 54: 480 -487. Silverstein A, Alexander J. Acute postictal cerebral imaging. Am J Neuroradiol. 1998; 19: 1485 -1488. Montgomery BM, Pinner CA, Newberry SC. Transient hypoglycemic hemiplegia. Arch Int Med. 1964; 114: 680 -684. Snyder H, Robinson K, Shah D, Brennan R, Handrigan M. Signs and symptoms of patients with brain tumors presenting to the emergency department. Jour Emerg Med. 1993; 11: 253 -258. Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. The NINDS t-PA stroke study group. Stroke. 1997; 28: 2109 -2118 Brosinski C. Implementing diagnostic reasoning to differentiate Todd’s paralysis from acute ischemic stroke. Advanced Emergency Nursing Journal. 2014; 36: 78 -86. Scott P, Silbergleit R. Misdiagnosis of stroke in tissue plasminogen activator treated patients: Characteristics and outcomes. Annals of Emergency Medicine. 2003; 42: 611 -618. Barrett K, Levine J, Johnston K. Diagnosis of stroke and stroke mimics in the emergency setting. Continuum Lifelong Learning Neurol. 2008; 14: 13 -27. Nau K, Crocco T, Biola J, Larrabee H. Is it stroke, or something else? The Journal of Family Practice. 2010; 59: 26 -31.


