7f99b5d83b9cb870d43c6dd2165e842c.ppt
- Количество слайдов: 38
 Stroke Matthew Simmons, MD Sept. 2013 Matthew. simmons@usd. edu
Stroke Matthew Simmons, MD Sept. 2013 Matthew. simmons@usd. edu
 TIA: Definition • “A transient episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia without acute infarction. ” • Note: Duration usually less than 60 minutes.
TIA: Definition • “A transient episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia without acute infarction. ” • Note: Duration usually less than 60 minutes.
 Stroke: New Definitions • CNS infarction: Brain, spinal cord, or retinal cell death due to ischemia. Based on: – Pathological, imaging, or other objective evidence – Clinical evidence • Symptoms greater than 24 hours (or until death) • Other etiologies excluded • Ischemic stroke: Clinical neurologic dysfunction with evidence as above • Silent CNS infarction: Evidence limited to imaging or neuropathological findings.
Stroke: New Definitions • CNS infarction: Brain, spinal cord, or retinal cell death due to ischemia. Based on: – Pathological, imaging, or other objective evidence – Clinical evidence • Symptoms greater than 24 hours (or until death) • Other etiologies excluded • Ischemic stroke: Clinical neurologic dysfunction with evidence as above • Silent CNS infarction: Evidence limited to imaging or neuropathological findings.
 Stroke Definitions (cont. ) Intracerebral hemorrhage Stroke caused by intracerebral hemorrhage Silent cerebral hemorrhage Subarachnoid hemorrhage Stroke caused by subarachnoid hemorrhage Stroke caused by cerebral sinus thrombosis: can be ischemic or hemorrhagic • Stroke not otherwise specified • • •
Stroke Definitions (cont. ) Intracerebral hemorrhage Stroke caused by intracerebral hemorrhage Silent cerebral hemorrhage Subarachnoid hemorrhage Stroke caused by subarachnoid hemorrhage Stroke caused by cerebral sinus thrombosis: can be ischemic or hemorrhagic • Stroke not otherwise specified • • •
 Stroke: Outline • • 1. 2. 3. 4. Prehospital care Emergency management Diagnostic approach Subacute care – Prevent complications – Rehabilitation – Secondary prevention
Stroke: Outline • • 1. 2. 3. 4. Prehospital care Emergency management Diagnostic approach Subacute care – Prevent complications – Rehabilitation – Secondary prevention
 Stroke: Prehospital care • • Primary prevention Public awareness/use 911 Emergency medical services (EMS) Hospital stroke care: – Acute Stoke-Ready Hospital – Primary Stroke Center – Comprehensive Stroke Center – Telemedicine
Stroke: Prehospital care • • Primary prevention Public awareness/use 911 Emergency medical services (EMS) Hospital stroke care: – Acute Stoke-Ready Hospital – Primary Stroke Center – Comprehensive Stroke Center – Telemedicine
 Stroke: EMS Checklist • • • ABC’s/ Establish time of symptom onset Oxygen/ NPO/ Check Glucometer Cardiac monitoring IV access (if no delay in transport) Rapid transport; alert receiving ED Avoid dextrose solutions; use Normal Saline
Stroke: EMS Checklist • • • ABC’s/ Establish time of symptom onset Oxygen/ NPO/ Check Glucometer Cardiac monitoring IV access (if no delay in transport) Rapid transport; alert receiving ED Avoid dextrose solutions; use Normal Saline
 Stroke: Emergency Management • ABC’s and recheck H & P • Labs: CMP, CBC, PT/PTT, TROPONIN (toxicology, Beta HCG, and HIV if indicated) • Imaging: CT (“gold standard”) or MRI • Cardiac Monitoring/EKG • Normothermia; avoid hyper/hypoglycemia • Cerebral ischemia pathway • Cerebral hemorrhage pathway • R/O Stroke Mimics.
Stroke: Emergency Management • ABC’s and recheck H & P • Labs: CMP, CBC, PT/PTT, TROPONIN (toxicology, Beta HCG, and HIV if indicated) • Imaging: CT (“gold standard”) or MRI • Cardiac Monitoring/EKG • Normothermia; avoid hyper/hypoglycemia • Cerebral ischemia pathway • Cerebral hemorrhage pathway • R/O Stroke Mimics.
 Common Acute Stroke Mimics • • Postictal deficits (Todd paralysis) Hypoglycemia Complicated migraine Mass lesions (i. e. tumor, subdural) Conversion reaction (psychogenic) Hypertensive encephalopathy Others: Subarachnoid hemorrhage, peripheral vestibulopathy, Bell’s Palsy, reactivation of old stroke.
Common Acute Stroke Mimics • • Postictal deficits (Todd paralysis) Hypoglycemia Complicated migraine Mass lesions (i. e. tumor, subdural) Conversion reaction (psychogenic) Hypertensive encephalopathy Others: Subarachnoid hemorrhage, peripheral vestibulopathy, Bell’s Palsy, reactivation of old stroke.
 Stroke mimic goals • Identify stroke mimics with 97% accuracy. • Means that less than 3% of patients who are diagnosed with acute stroke will have a stroke mimic that might be treated with thrombolytics.
Stroke mimic goals • Identify stroke mimics with 97% accuracy. • Means that less than 3% of patients who are diagnosed with acute stroke will have a stroke mimic that might be treated with thrombolytics.
 Stroke Imaging: CT/MRI • CT • MRI – Hemorrhage and Gradient Echo (GRE) – Diffusion-weighted images (DWI) and apparent diffusion coefficient (ADC) Map – Note non ischemic causes of diffusion restriction: • Inflammation, infection, tumors, post seizure, etc. • Vascular territories • Time related changes
Stroke Imaging: CT/MRI • CT • MRI – Hemorrhage and Gradient Echo (GRE) – Diffusion-weighted images (DWI) and apparent diffusion coefficient (ADC) Map – Note non ischemic causes of diffusion restriction: • Inflammation, infection, tumors, post seizure, etc. • Vascular territories • Time related changes
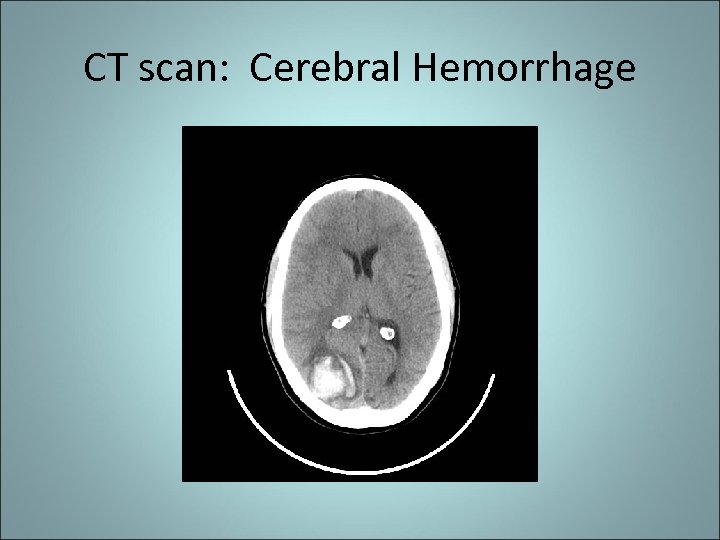 CT scan: Cerebral Hemorrhage
CT scan: Cerebral Hemorrhage
 Stroke: Cerebral Hemorrhage Pathway • Additional diagnostics: toxicology? , angiography, LP (if needed for R/O SAH) • Treatment – Supportive care (similar to ischemic stroke/TBI) – Anticoagulant reversal – BP Management per guidelines – Neurosurgery consultation
Stroke: Cerebral Hemorrhage Pathway • Additional diagnostics: toxicology? , angiography, LP (if needed for R/O SAH) • Treatment – Supportive care (similar to ischemic stroke/TBI) – Anticoagulant reversal – BP Management per guidelines – Neurosurgery consultation
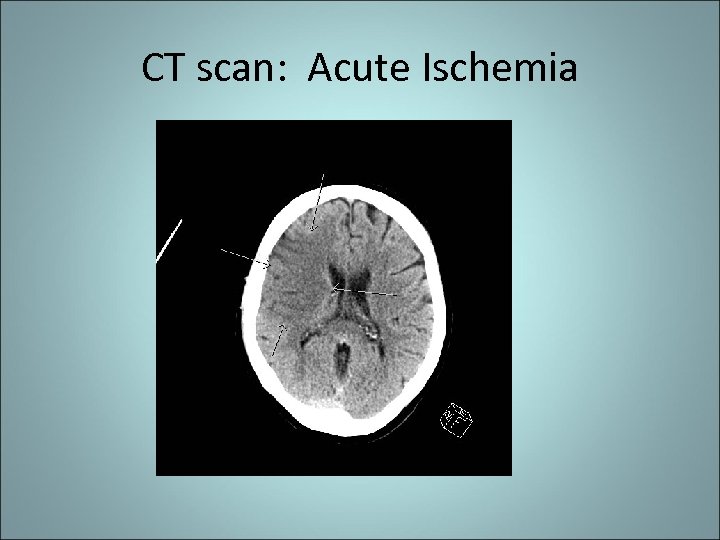 CT scan: Acute Ischemia
CT scan: Acute Ischemia
 Stroke: Acute Cerebral ischemia pathway • Systemic rt. PA per protocol (save penumbra) – If no rt. PA, then antiplatelet agent; NOT heparin • Acute BP management per protocol – If rt. PA: <185/110; post rt. PA <180/105 – If no rt. PA: <220/130 • Endovascular thrombolytic or clot retrieval • Admit to appropriate stroke unit • Initiate diagnostic workup
Stroke: Acute Cerebral ischemia pathway • Systemic rt. PA per protocol (save penumbra) – If no rt. PA, then antiplatelet agent; NOT heparin • Acute BP management per protocol – If rt. PA: <185/110; post rt. PA <180/105 – If no rt. PA: <220/130 • Endovascular thrombolytic or clot retrieval • Admit to appropriate stroke unit • Initiate diagnostic workup
 Stroke: Cerebral ischemia diagnostics • Major etiologies: – Atherothromboembolic disease • Artery to artery embolus (most common) • Stenosis/occlusion with distal hypoperfusion – Small vessel disease • Arteriosclerosis (fibrinoid necrosis) • Microatheromatous – Cardioembolic (including “paradoxical embolus? ”) – Hypotension (with or without stenosis) – Idiopathic/Cryptogenic (20 -30%) – Misc.
Stroke: Cerebral ischemia diagnostics • Major etiologies: – Atherothromboembolic disease • Artery to artery embolus (most common) • Stenosis/occlusion with distal hypoperfusion – Small vessel disease • Arteriosclerosis (fibrinoid necrosis) • Microatheromatous – Cardioembolic (including “paradoxical embolus? ”) – Hypotension (with or without stenosis) – Idiopathic/Cryptogenic (20 -30%) – Misc.
 Cryoptogenic Stroke: Current Issues • Patent Foramen Ovale – Closure vs. medical treatment – Studies on going • Atrial Fibrillation – Prolonged monitoring 20 -50 days • 12 -25% intermittent AFib – “Wake up stroke” • 3 X risk of new AFib
Cryoptogenic Stroke: Current Issues • Patent Foramen Ovale – Closure vs. medical treatment – Studies on going • Atrial Fibrillation – Prolonged monitoring 20 -50 days • 12 -25% intermittent AFib – “Wake up stroke” • 3 X risk of new AFib
 Stroke: Cerebral ischemia diagnostic tests • MRI with diffusion • Extra labs: Lipids; others (i. e. “thrombo”) • Echocardiogram with agitated saline – Sometimes TEE • Vascular imaging – Ultrasound (extracranial) – MRA (intracranial/extracranial) – CTA (intracranial/extracranial)
Stroke: Cerebral ischemia diagnostic tests • MRI with diffusion • Extra labs: Lipids; others (i. e. “thrombo”) • Echocardiogram with agitated saline – Sometimes TEE • Vascular imaging – Ultrasound (extracranial) – MRA (intracranial/extracranial) – CTA (intracranial/extracranial)
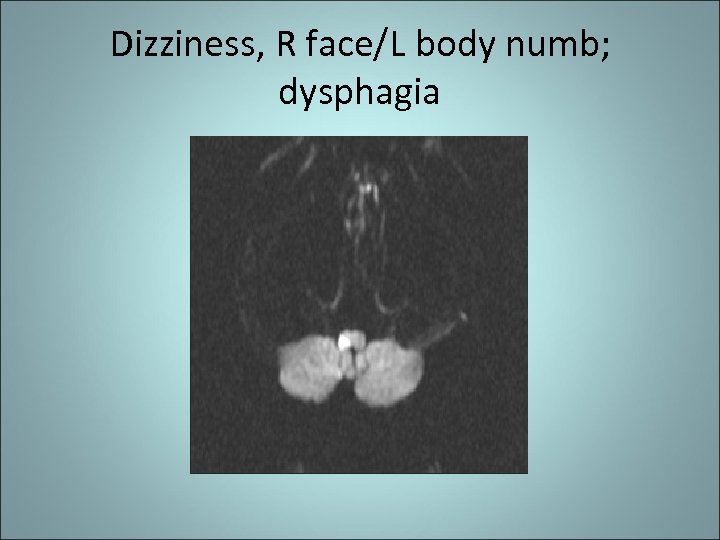 Dizziness, R face/L body numb; dysphagia
Dizziness, R face/L body numb; dysphagia
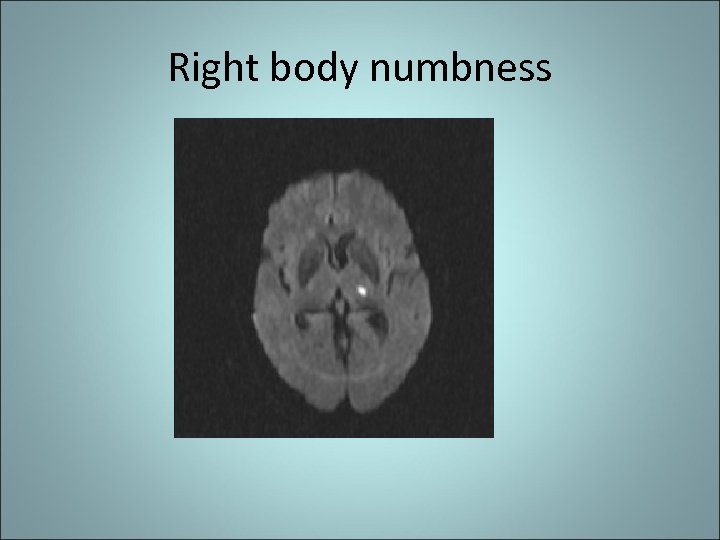 Right body numbness
Right body numbness
 Aphasia
Aphasia
 Left hemiplegia and neglect
Left hemiplegia and neglect
 MRI with ADC Map: Acute Ischemia
MRI with ADC Map: Acute Ischemia
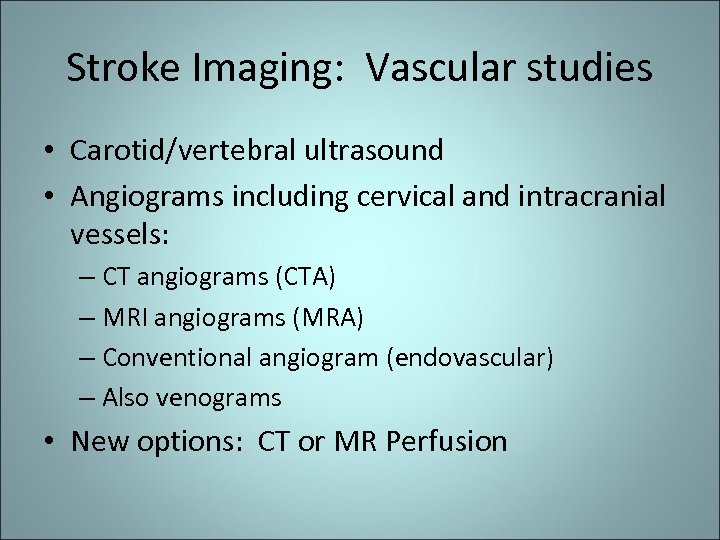 Stroke Imaging: Vascular studies • Carotid/vertebral ultrasound • Angiograms including cervical and intracranial vessels: – CT angiograms (CTA) – MRI angiograms (MRA) – Conventional angiogram (endovascular) – Also venograms • New options: CT or MR Perfusion
Stroke Imaging: Vascular studies • Carotid/vertebral ultrasound • Angiograms including cervical and intracranial vessels: – CT angiograms (CTA) – MRI angiograms (MRA) – Conventional angiogram (endovascular) – Also venograms • New options: CT or MR Perfusion
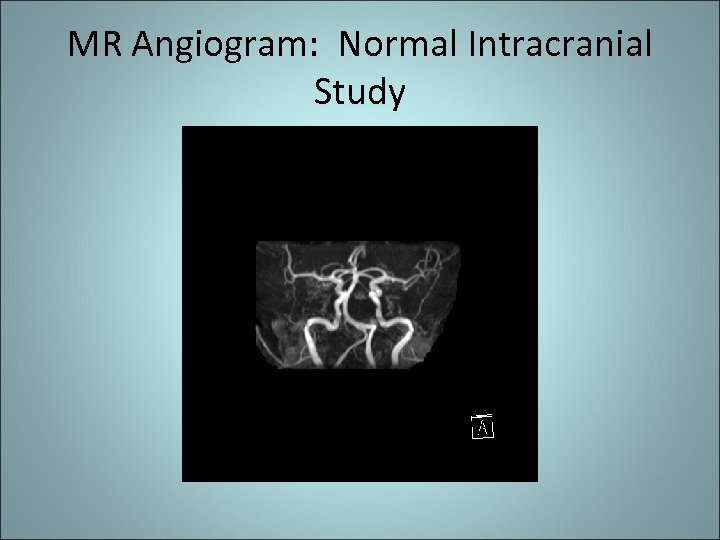 MR Angiogram: Normal Intracranial Study
MR Angiogram: Normal Intracranial Study
 MR Angiogram: Normal Cervical Study
MR Angiogram: Normal Cervical Study
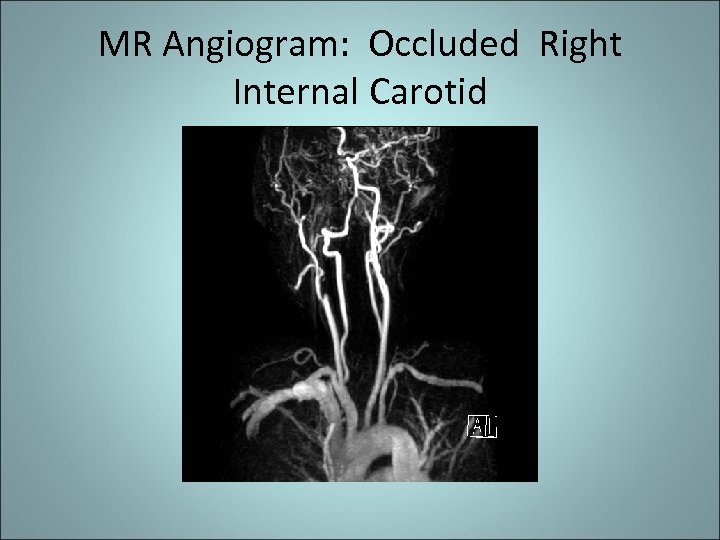 MR Angiogram: Occluded Right Internal Carotid
MR Angiogram: Occluded Right Internal Carotid
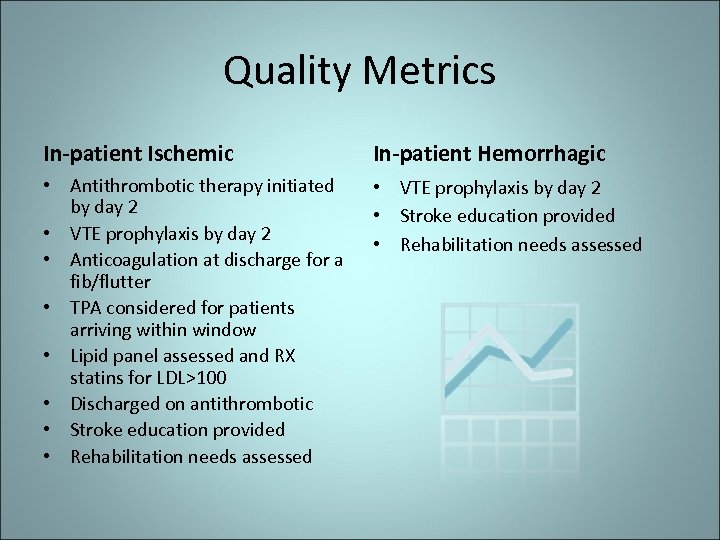 Quality Metrics In-patient Ischemic In-patient Hemorrhagic • Antithrombotic therapy initiated by day 2 • VTE prophylaxis by day 2 • Anticoagulation at discharge for a fib/flutter • TPA considered for patients arriving within window • Lipid panel assessed and RX statins for LDL>100 • Discharged on antithrombotic • Stroke education provided • Rehabilitation needs assessed • VTE prophylaxis by day 2 • Stroke education provided • Rehabilitation needs assessed
Quality Metrics In-patient Ischemic In-patient Hemorrhagic • Antithrombotic therapy initiated by day 2 • VTE prophylaxis by day 2 • Anticoagulation at discharge for a fib/flutter • TPA considered for patients arriving within window • Lipid panel assessed and RX statins for LDL>100 • Discharged on antithrombotic • Stroke education provided • Rehabilitation needs assessed • VTE prophylaxis by day 2 • Stroke education provided • Rehabilitation needs assessed
 Stroke: Subacute care • Major goals: – Reduce complications – Manage co morbidities – Maximize recovery/rehabilitation – Secondary prevention
Stroke: Subacute care • Major goals: – Reduce complications – Manage co morbidities – Maximize recovery/rehabilitation – Secondary prevention
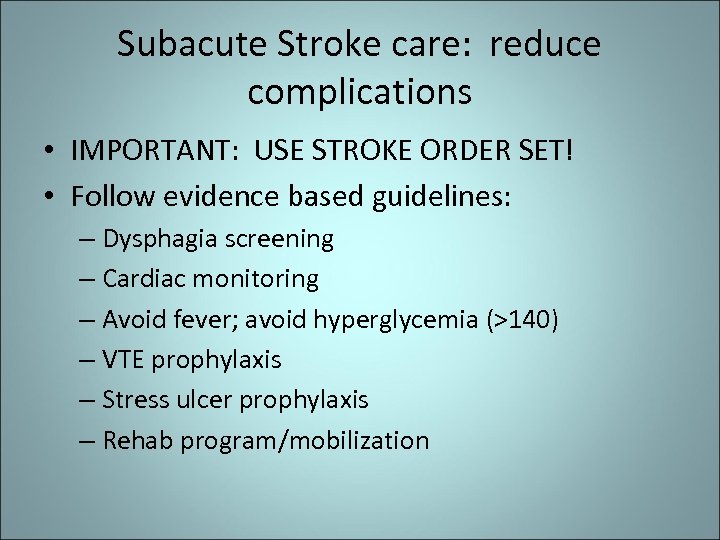 Subacute Stroke care: reduce complications • IMPORTANT: USE STROKE ORDER SET! • Follow evidence based guidelines: – Dysphagia screening – Cardiac monitoring – Avoid fever; avoid hyperglycemia (>140) – VTE prophylaxis – Stress ulcer prophylaxis – Rehab program/mobilization
Subacute Stroke care: reduce complications • IMPORTANT: USE STROKE ORDER SET! • Follow evidence based guidelines: – Dysphagia screening – Cardiac monitoring – Avoid fever; avoid hyperglycemia (>140) – VTE prophylaxis – Stress ulcer prophylaxis – Rehab program/mobilization
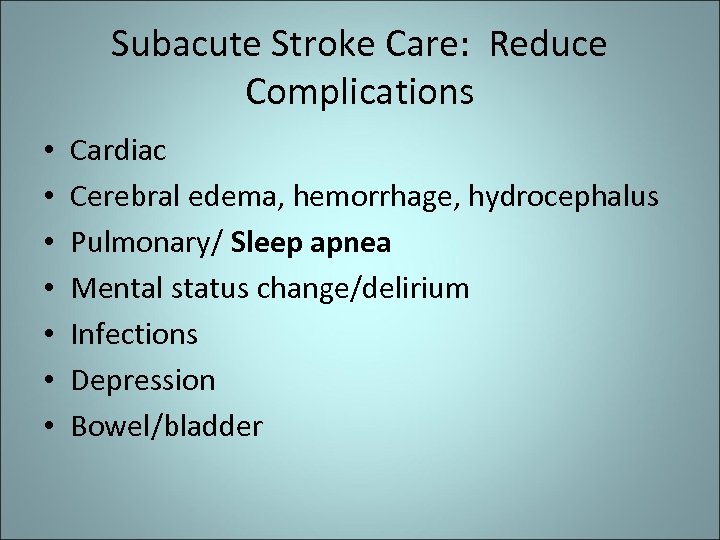 Subacute Stroke Care: Reduce Complications • • Cardiac Cerebral edema, hemorrhage, hydrocephalus Pulmonary/ Sleep apnea Mental status change/delirium Infections Depression Bowel/bladder
Subacute Stroke Care: Reduce Complications • • Cardiac Cerebral edema, hemorrhage, hydrocephalus Pulmonary/ Sleep apnea Mental status change/delirium Infections Depression Bowel/bladder
 Secondary Stroke Prevention • • Risk factor management Anticoagulants Antiplatelet agents Surgery
Secondary Stroke Prevention • • Risk factor management Anticoagulants Antiplatelet agents Surgery
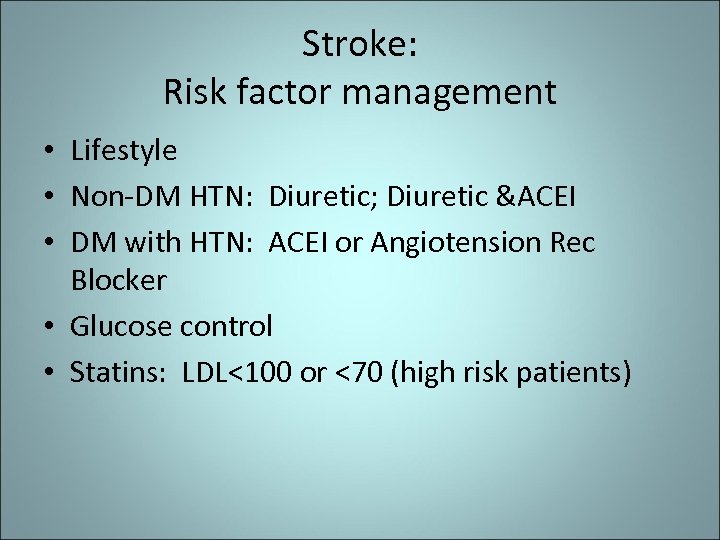 Stroke: Risk factor management • Lifestyle • Non-DM HTN: Diuretic; Diuretic &ACEI • DM with HTN: ACEI or Angiotension Rec Blocker • Glucose control • Statins: LDL<100 or <70 (high risk patients)
Stroke: Risk factor management • Lifestyle • Non-DM HTN: Diuretic; Diuretic &ACEI • DM with HTN: ACEI or Angiotension Rec Blocker • Glucose control • Statins: LDL<100 or <70 (high risk patients)
 Stroke: Anticoagulants • • • Cardiac source of embolus Some hyper thrombotic states? Venous sinus thrombosis Major arterial dissection Few others?
Stroke: Anticoagulants • • • Cardiac source of embolus Some hyper thrombotic states? Venous sinus thrombosis Major arterial dissection Few others?
 Stroke: Antiplatelet agents • For atherothomboembolic and small vessel disease • Aspirin • Clopidogrel – Note nonresponders/drug-drug interactions (PPI) – Platelet function tests? • Dipyridamole/aspirin • New agents?
Stroke: Antiplatelet agents • For atherothomboembolic and small vessel disease • Aspirin • Clopidogrel – Note nonresponders/drug-drug interactions (PPI) – Platelet function tests? • Dipyridamole/aspirin • New agents?
 Periprocedural management of antithrombotic medications • For Dental procedures: Can continue ASA or Warfarin. • ASA probably OK for invasive ocular anethesia, cataract surgery, derm procedures, US guided prostate biopsy, spinal/epidural procedures, and carpal tunnel surgery. • Warfarin probably ok for most derm procedures.
Periprocedural management of antithrombotic medications • For Dental procedures: Can continue ASA or Warfarin. • ASA probably OK for invasive ocular anethesia, cataract surgery, derm procedures, US guided prostate biopsy, spinal/epidural procedures, and carpal tunnel surgery. • Warfarin probably ok for most derm procedures.
 Secondary Stroke Prevention: Surgery • Carotid endarterectomy • Angioplasty/stenting • Cardiac surgery
Secondary Stroke Prevention: Surgery • Carotid endarterectomy • Angioplasty/stenting • Cardiac surgery
 Questions? Dr. Matthew Simmons matthew. simmons@usd. edu Kathy Hill, RN, MSN Rapid City Regional Hospital Stroke Coordinator khill@regionalhealth. com 605 -719 -4374
Questions? Dr. Matthew Simmons matthew. simmons@usd. edu Kathy Hill, RN, MSN Rapid City Regional Hospital Stroke Coordinator khill@regionalhealth. com 605 -719 -4374


