2991a1d2b8590bb80c4e4721b6f3fad8.ppt
- Количество слайдов: 32
Stroke and VTE: A Deadly Combination Amjad Al. Mahameed, MD, MPH, FACP Division of Cardiology Beth Israel Deaconess Medical Center Boston, MA
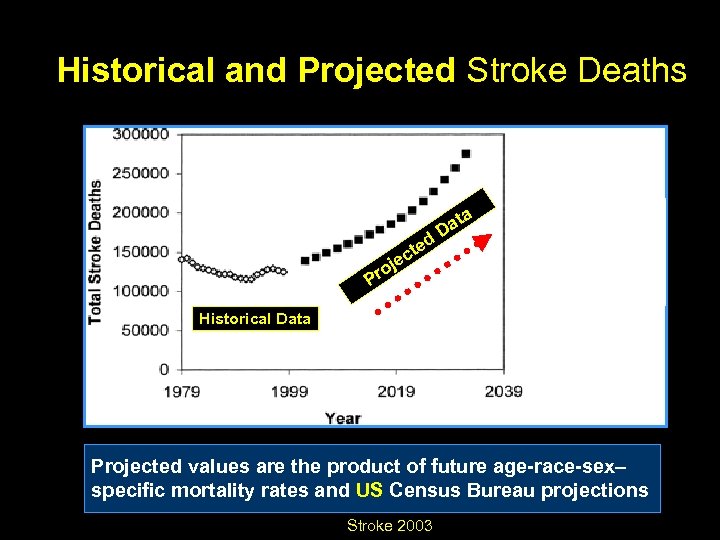
Historical and Projected Stroke Deaths ted jec ata D o Pr Historical Data Projected values are the product of future age-race-sex– specific mortality rates and US Census Bureau projections Stroke 2003
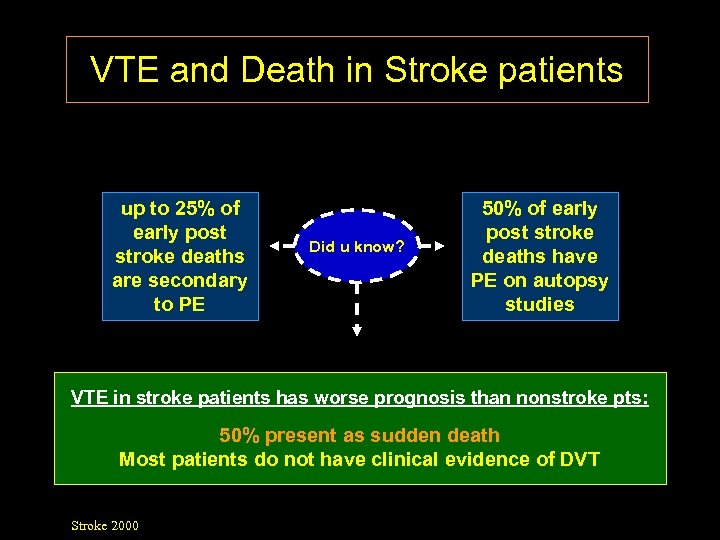
VTE and Death in Stroke patients up to 25% of early post stroke deaths are secondary to PE Did u know? 50% of early post stroke deaths have PE on autopsy studies VTE in stroke patients has worse prognosis than nonstroke pts: 50% present as sudden death Most patients do not have clinical evidence of DVT Stroke 2000
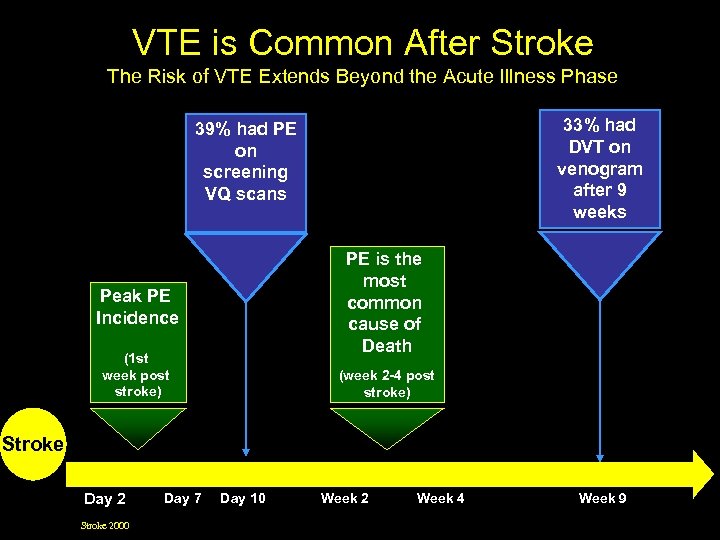
VTE is Common After Stroke The Risk of VTE Extends Beyond the Acute Illness Phase 33% had DVT on venogram after 9 weeks 39% had PE on screening VQ scans PE is the most common cause of Death Peak PE Incidence (1 st week post stroke) (week 2 -4 post stroke) Stroke Day 2 Stroke 2000 Day 7 Day 10 Week 2 Week 4 Week 9
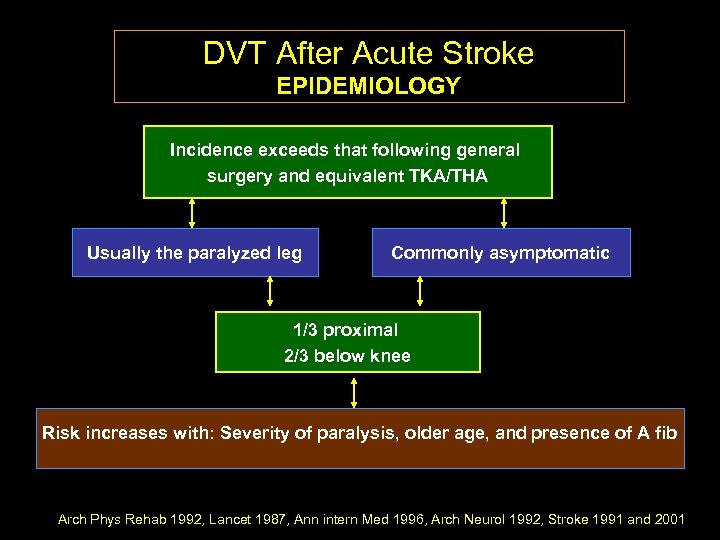
DVT After Acute Stroke EPIDEMIOLOGY Incidence exceeds that following general surgery and equivalent TKA/THA Usually the paralyzed leg Commonly asymptomatic 1/3 proximal 2/3 below knee Risk increases with: Severity of paralysis, older age, and presence of A fib Arch Phys Rehab 1992, Lancet 1987, Ann intern Med 1996, Arch Neurol 1992, Stroke 1991 and 2001
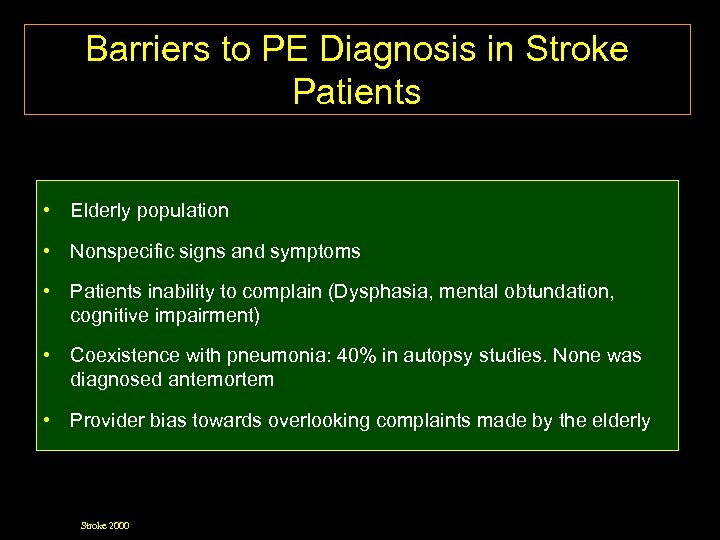
Barriers to PE Diagnosis in Stroke Patients • Elderly population • Nonspecific signs and symptoms • Patients inability to complain (Dysphasia, mental obtundation, cognitive impairment) • Coexistence with pneumonia: 40% in autopsy studies. None was diagnosed antemortem • Provider bias towards overlooking complaints made by the elderly Stroke 2000
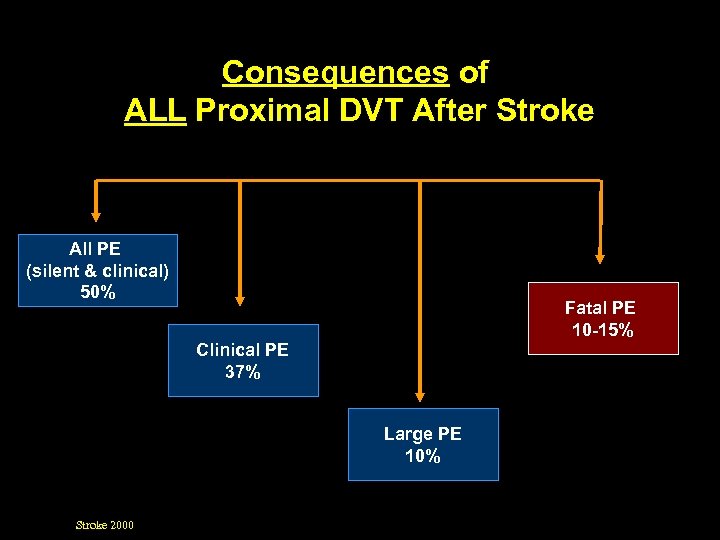
Consequences of ALL Proximal DVT After Stroke All PE (silent & clinical) 50% Fatal PE 10 -15% Clinical PE 37% Large PE 10% Stroke 2000
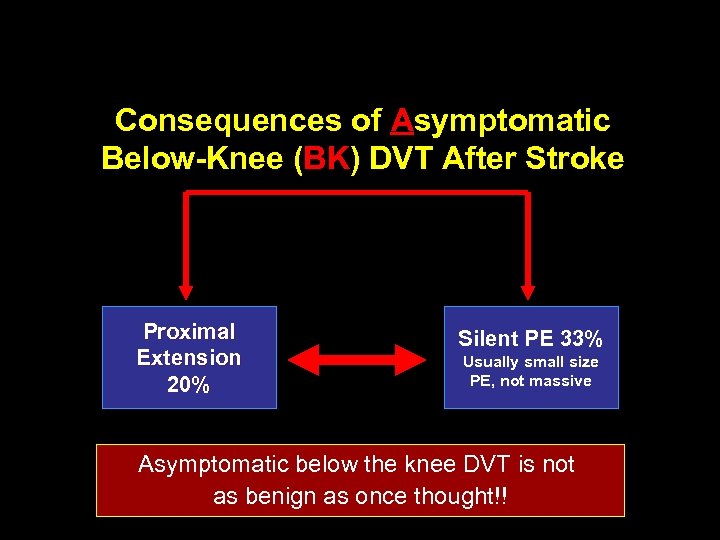
Consequences of Asymptomatic Below-Knee (BK) DVT After Stroke Proximal Extension 20% Silent PE 33% Usually small size PE, not massive Asymptomatic below the knee DVT is not as benign as once thought!!
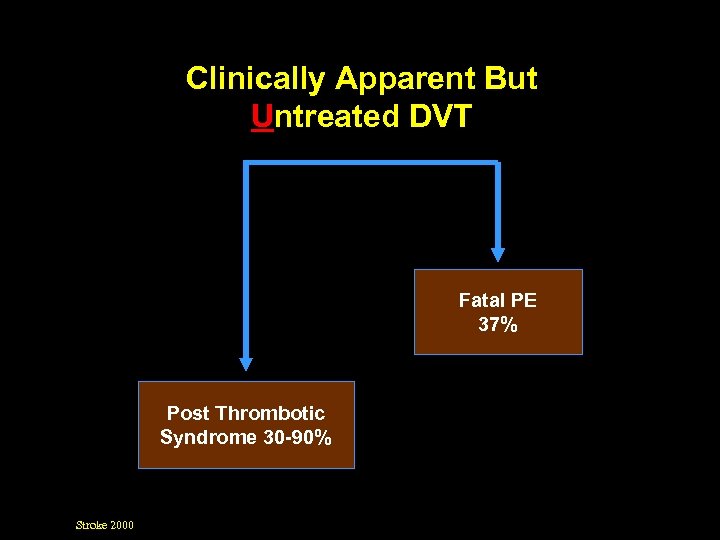
Clinically Apparent But Untreated DVT Fatal PE 37% Post Thrombotic Syndrome 30 -90% Stroke 2000
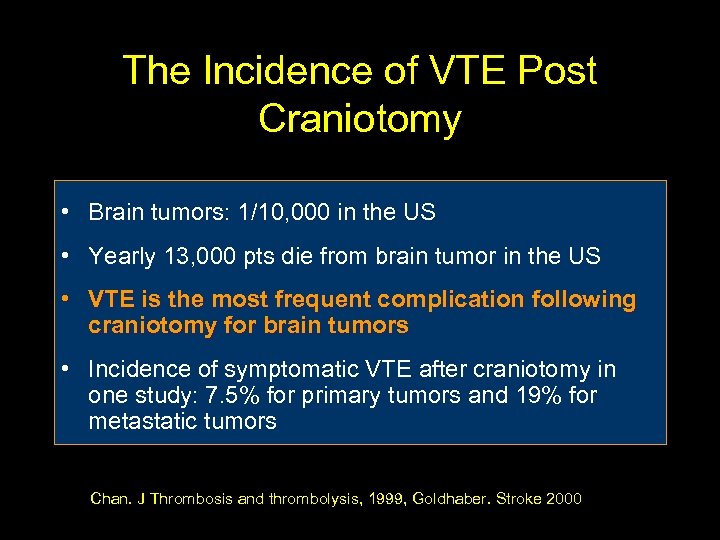
The Incidence of VTE Post Craniotomy • Brain tumors: 1/10, 000 in the US • Yearly 13, 000 pts die from brain tumor in the US • VTE is the most frequent complication following craniotomy for brain tumors • Incidence of symptomatic VTE after craniotomy in one study: 7. 5% for primary tumors and 19% for metastatic tumors Chan. J Thrombosis and thrombolysis, 1999, Goldhaber. Stroke 2000
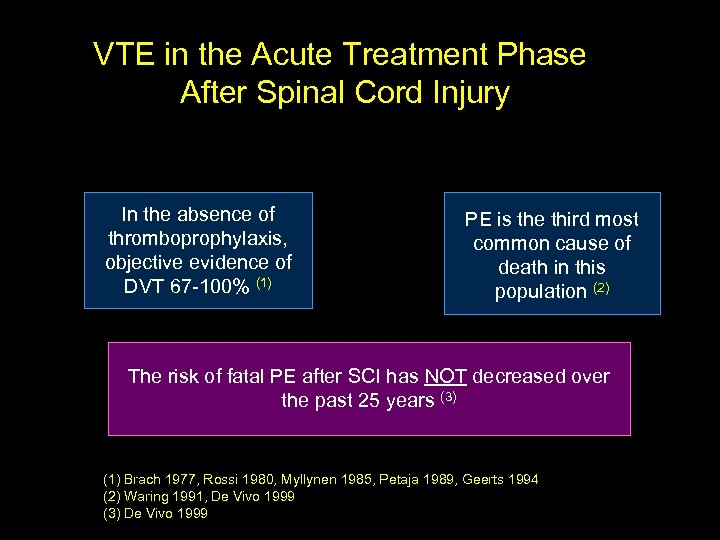
VTE in the Acute Treatment Phase After Spinal Cord Injury In the absence of thromboprophylaxis, objective evidence of DVT 67 -100% (1) PE is the third most common cause of death in this population (2) The risk of fatal PE after SCI has NOT decreased over the past 25 years (3) (1) Brach 1977, Rossi 1980, Myllynen 1985, Petaja 1989, Geerts 1994 (2) Waring 1991, De Vivo 1999 (3) De Vivo 1999
The risk of VTE post neurological events (stroke, spinal cord injury/surgery, and craniotomy) is even higher in the presence of other risk factors for VTE
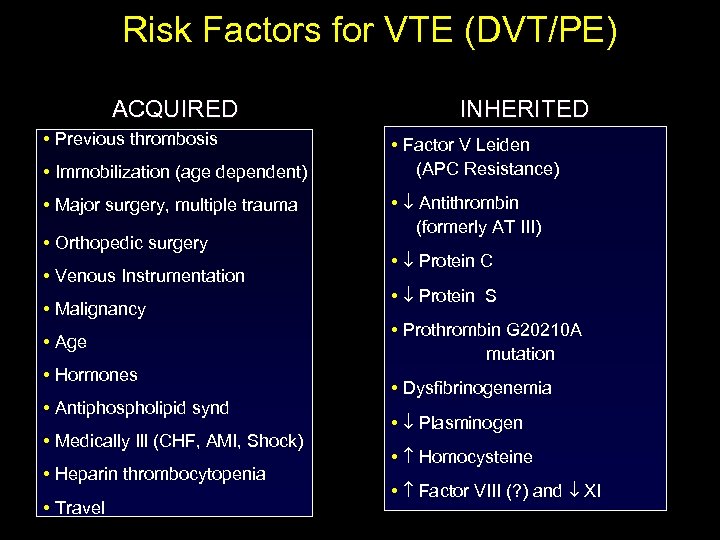
Risk Factors for VTE (DVT/PE) ACQUIRED • Previous thrombosis • Immobilization (age dependent) • Major surgery, multiple trauma • Orthopedic surgery • Venous Instrumentation • Malignancy • Age • Hormones • Antiphospholipid synd • Medically Ill (CHF, AMI, Shock) • Heparin thrombocytopenia • Travel INHERITED • Factor V Leiden (APC Resistance) • Antithrombin (formerly AT III) • Protein C • Protein S • Prothrombin G 20210 A mutation • Dysfibrinogenemia • Plasminogen • Homocysteine • Factor VIII (? ) and XI
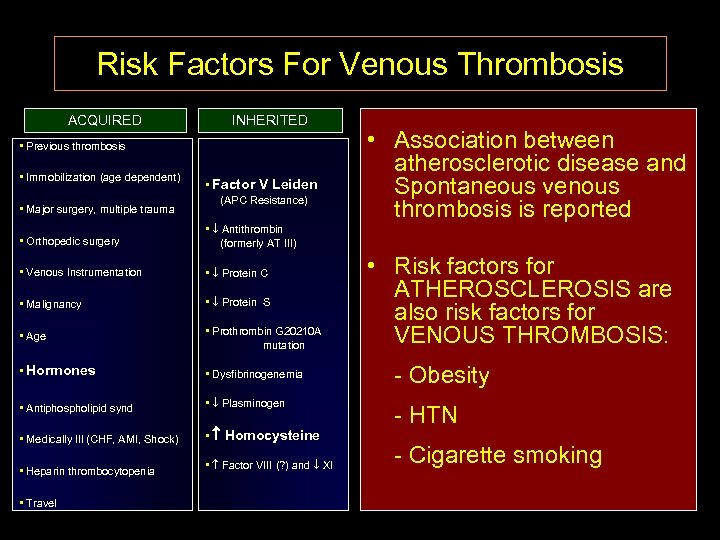
Risk Factors For Venous Thrombosis ACQUIRED INHERITED • Previous thrombosis • Immobilization (age dependent) • Major surgery, multiple trauma • Factor V Leiden (APC Resistance) • Orthopedic surgery • Antithrombin (formerly AT III) • Venous Instrumentation • Protein C • Malignancy • Protein S • Age • Prothrombin G 20210 A mutation • Hormones • Dysfibrinogenemia • Antiphospholipid synd • Plasminogen • Medically Ill (CHF, AMI, Shock) • • Heparin thrombocytopenia • Factor VIII (? ) and XI • Association between atherosclerotic disease and Spontaneous venous thrombosis is reported • Travel Homocysteine • Risk factors for ATHEROSCLEROSIS are also risk factors for VENOUS THROMBOSIS: - Obesity - HTN - Cigarette smoking
Primary Prevention Strategies
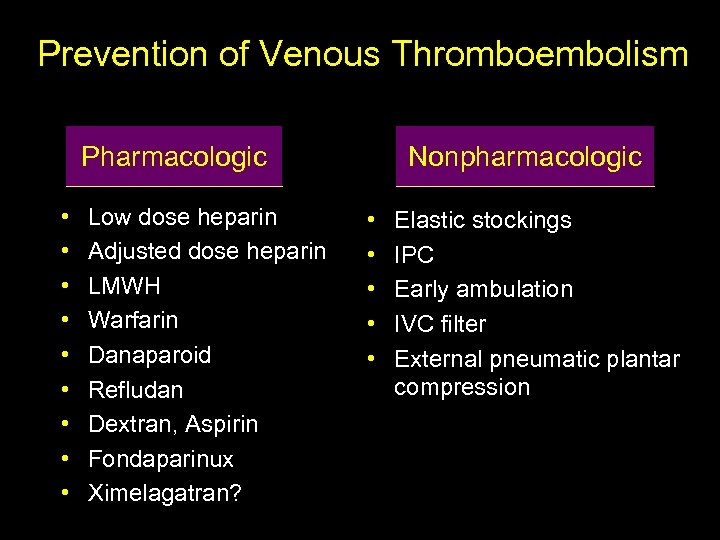
Prevention of Venous Thromboembolism Pharmacologic • • • Low dose heparin Adjusted dose heparin LMWH Warfarin Danaparoid Refludan Dextran, Aspirin Fondaparinux Ximelagatran? Nonpharmacologic • • • Elastic stockings IPC Early ambulation IVC filter External pneumatic plantar compression
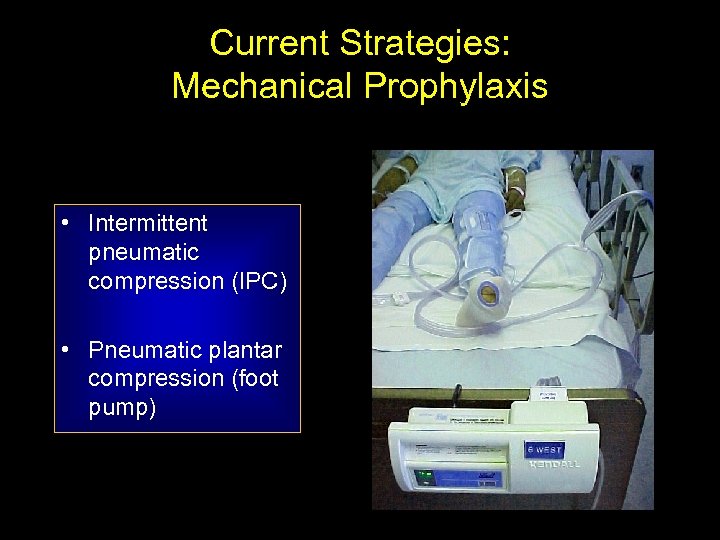
Current Strategies: Mechanical Prophylaxis • Intermittent pneumatic compression (IPC) • Pneumatic plantar compression (foot pump)
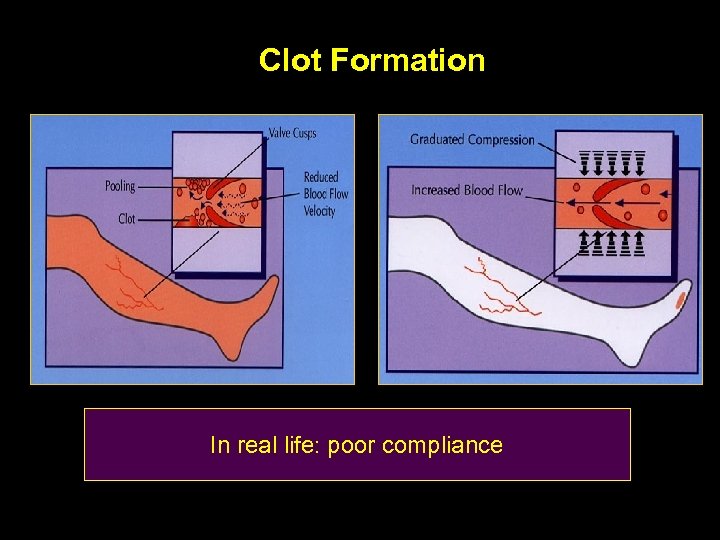
Clot Formation In real life: poor compliance
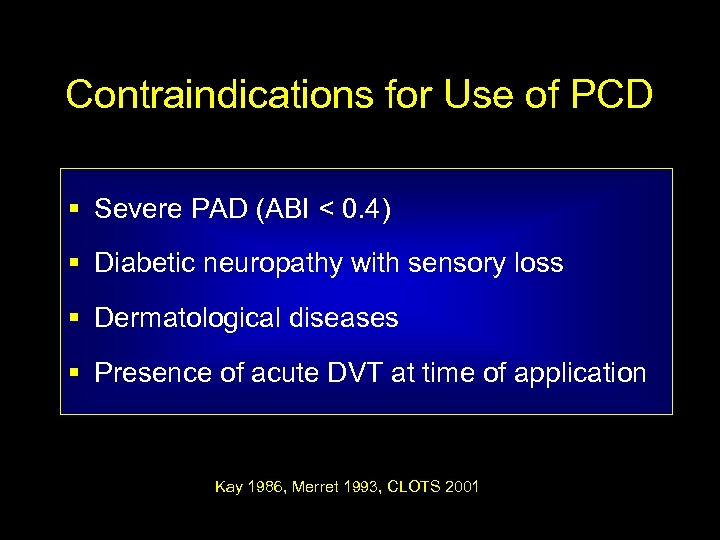
Contraindications for Use of PCD § Severe PAD (ABI < 0. 4) § Diabetic neuropathy with sensory loss § Dermatological diseases § Presence of acute DVT at time of application Kay 1986, Merret 1993, CLOTS 2001
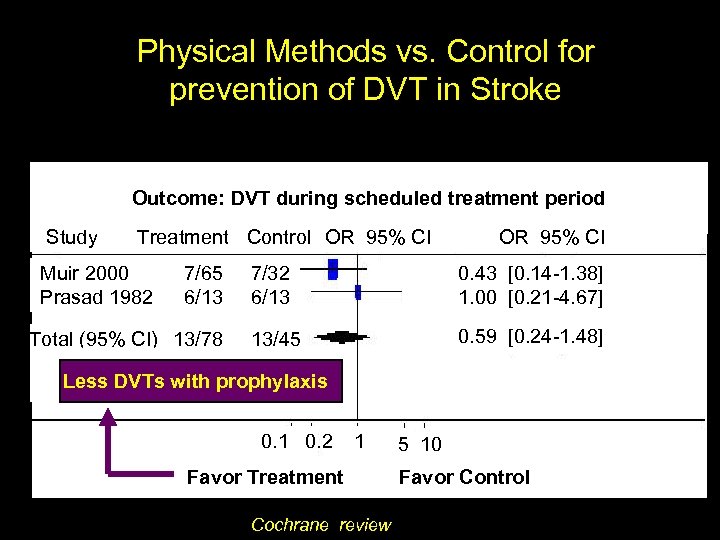
Physical Methods vs. Control for prevention of DVT in Stroke Outcome: DVT during scheduled treatment period Study Treatment Control OR 95% CI Muir 2000 Prasad 1982 7/65 6/13 Total (95% CI) 13/78 OR 95% CI 7/32 6/13 0. 43 [0. 14 -1. 38] 1. 00 [0. 21 -4. 67] 13/45 0. 59 [0. 24 -1. 48] Less DVTs with prophylaxis 0. 1 0. 2 1 Favor Treatment Cochrane review 5 10 Favor Control
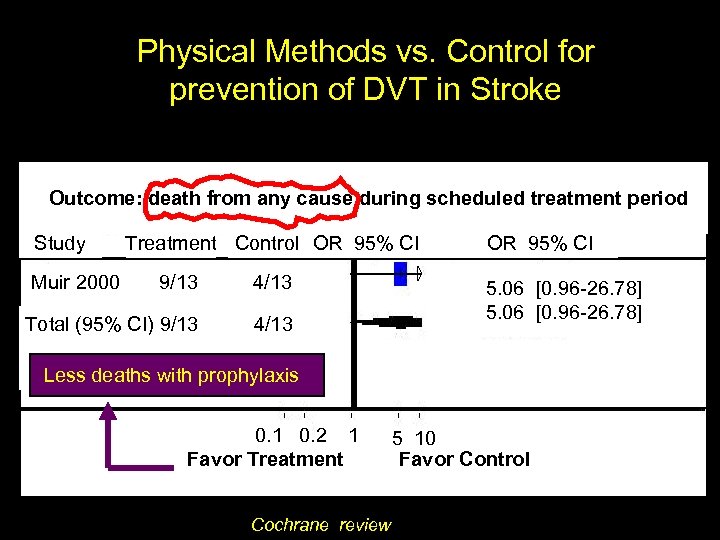
Physical Methods vs. Control for prevention of DVT in Stroke Outcome: death from any cause during scheduled treatment period Study Muir 2000 Treatment Control OR 95% CI 9/13 4/13 Total (95% CI) 9/13 4/13 OR 95% CI 5. 06 [0. 96 -26. 78] Less deaths with prophylaxis 0. 1 0. 2 1 Favor Treatment Cochrane review 5 10 Favor Control
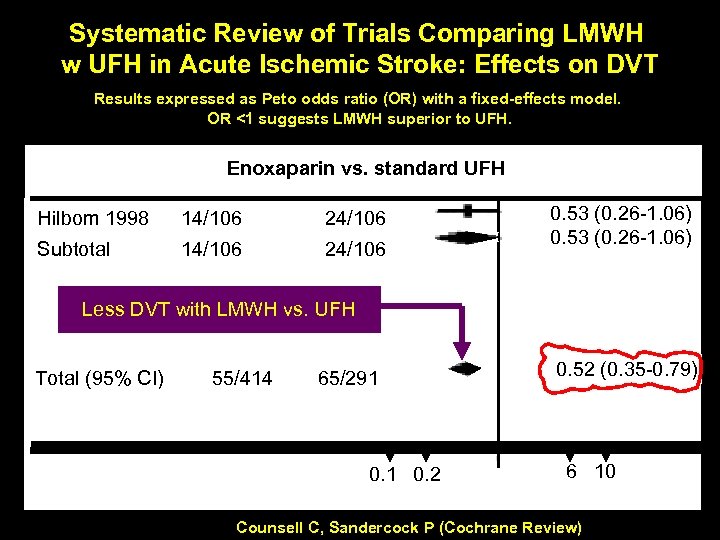
Systematic Review of Trials Comparing LMWH w UFH in Acute Ischemic Stroke: Effects on DVT Results expressed as Peto odds ratio (OR) with a fixed-effects model. OR <1 suggests LMWH superior to UFH. Enoxaparin vs. standard UFH Hilbom 1998 14/106 24/106 Subtotal 14/106 24/106 0. 53 (0. 26 -1. 06) Less DVT with LMWH vs. UFH Total (95% CI) 55/414 65/291 0. 2 0. 52 (0. 35 -0. 79) 6 10 Counsell C, Sandercock P (Cochrane Review)
VTE Prophylaxis Post Trauma, SCIs and Craniotomy
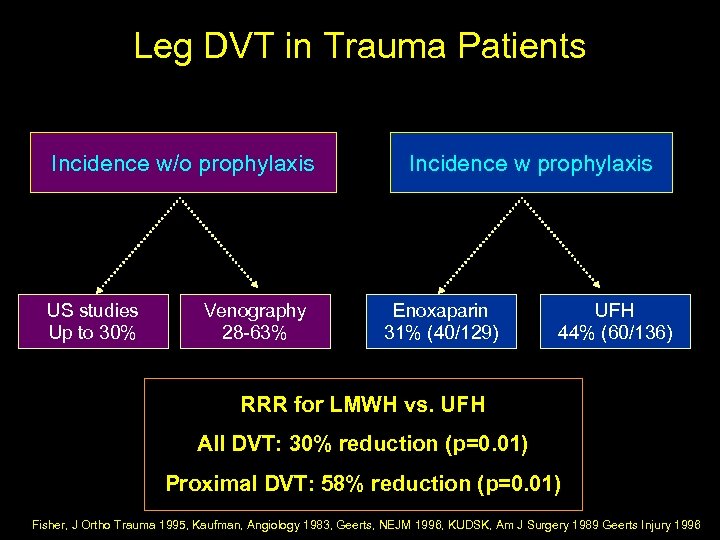
Leg DVT in Trauma Patients Incidence w/o prophylaxis US studies Up to 30% Venography 28 -63% Incidence w prophylaxis Enoxaparin 31% (40/129) UFH 44% (60/136) RRR for LMWH vs. UFH All DVT: 30% reduction (p=0. 01) Proximal DVT: 58% reduction (p=0. 01) Fisher, J Ortho Trauma 1995, Kaufman, Angiology 1983, Geerts, NEJM 1996, KUDSK, Am J Surgery 1989 Geerts Injury 1996
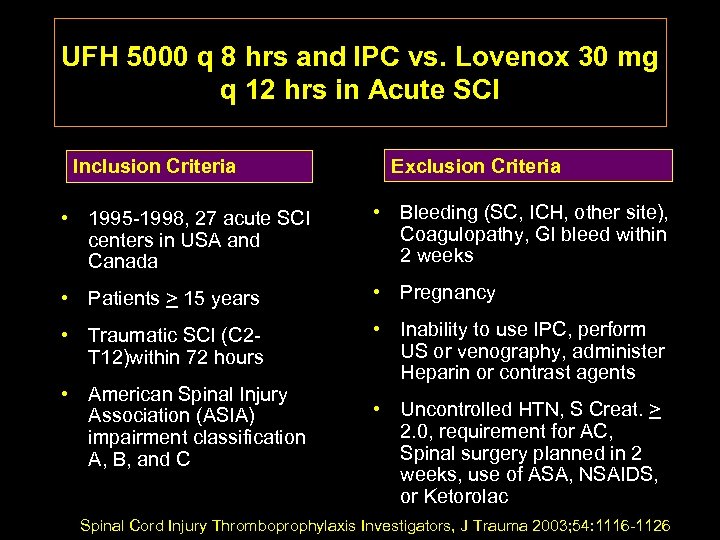
UFH 5000 q 8 hrs and IPC vs. Lovenox 30 mg q 12 hrs in Acute SCI Inclusion Criteria Exclusion Criteria • 1995 -1998, 27 acute SCI centers in USA and Canada • Bleeding (SC, ICH, other site), Coagulopathy, GI bleed within 2 weeks • Patients > 15 years • Pregnancy • Traumatic SCI (C 2 T 12)within 72 hours • Inability to use IPC, perform US or venography, administer Heparin or contrast agents • American Spinal Injury Association (ASIA) impairment classification A, B, and C • Uncontrolled HTN, S Creat. > 2. 0, requirement for AC, Spinal surgery planned in 2 weeks, use of ASA, NSAIDS, or Ketorolac Spinal Cord Injury Thromboprophylaxis Investigators, J Trauma 2003; 54: 1116 -1126
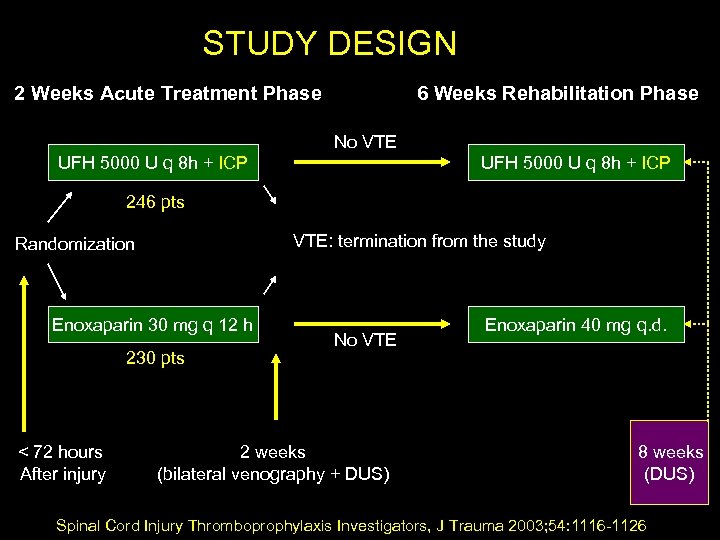
STUDY DESIGN 2 Weeks Acute Treatment Phase 6 Weeks Rehabilitation Phase No VTE UFH 5000 U q 8 h + ICP 246 pts VTE: termination from the study Randomization Enoxaparin 30 mg q 12 h 230 pts < 72 hours After injury No VTE 2 weeks (bilateral venography + DUS) Enoxaparin 40 mg q. d. 8 weeks (DUS) Spinal Cord Injury Thromboprophylaxis Investigators, J Trauma 2003; 54: 1116 -1126
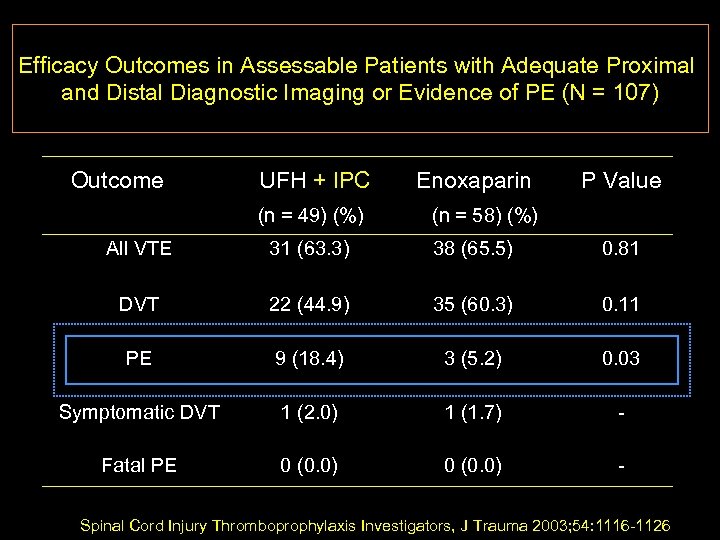
Efficacy Outcomes in Assessable Patients with Adequate Proximal and Distal Diagnostic Imaging or Evidence of PE (N = 107) Outcome UFH + IPC (n = 49) (%) Enoxaparin P Value (n = 58) (%) All VTE 31 (63. 3) 38 (65. 5) 0. 81 DVT 22 (44. 9) 35 (60. 3) 0. 11 PE 9 (18. 4) 3 (5. 2) 0. 03 Symptomatic DVT 1 (2. 0) 1 (1. 7) - Fatal PE 0 (0. 0) - Spinal Cord Injury Thromboprophylaxis Investigators, J Trauma 2003; 54: 1116 -1126
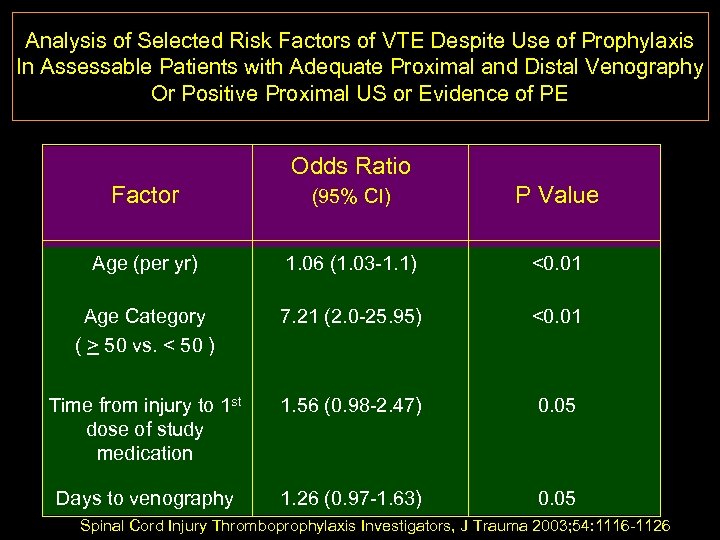
Analysis of Selected Risk Factors of VTE Despite Use of Prophylaxis In Assessable Patients with Adequate Proximal and Distal Venography Or Positive Proximal US or Evidence of PE Odds Ratio Factor (95% CI) P Value Age (per yr) 1. 06 (1. 03 -1. 1) <0. 01 Age Category ( > 50 vs. < 50 ) 7. 21 (2. 0 -25. 95) <0. 01 Time from injury to 1 st dose of study medication 1. 56 (0. 98 -2. 47) 0. 05 Days to venography 1. 26 (0. 97 -1. 63) 0. 05 Spinal Cord Injury Thromboprophylaxis Investigators, J Trauma 2003; 54: 1116 -1126
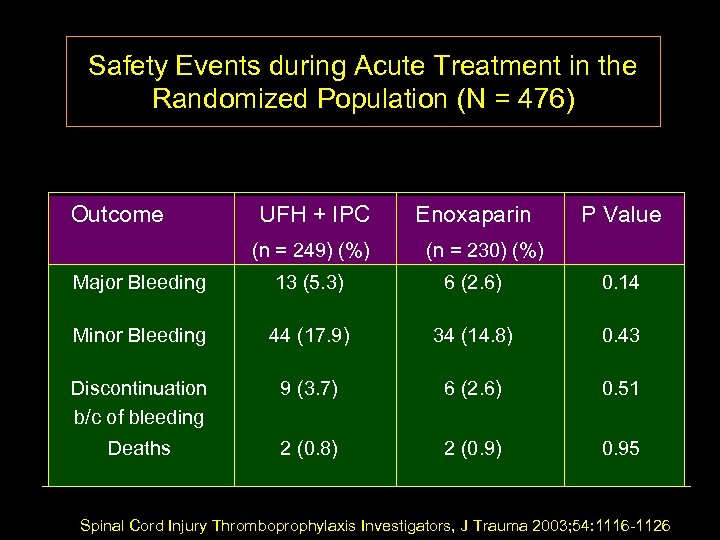
Safety Events during Acute Treatment in the Randomized Population (N = 476) Outcome UFH + IPC (n = 249) (%) Enoxaparin P Value (n = 230) (%) Major Bleeding 13 (5. 3) 6 (2. 6) 0. 14 Minor Bleeding 44 (17. 9) 34 (14. 8) 0. 43 Discontinuation b/c of bleeding 9 (3. 7) 6 (2. 6) 0. 51 Deaths 2 (0. 8) 2 (0. 9) 0. 95 Spinal Cord Injury Thromboprophylaxis Investigators, J Trauma 2003; 54: 1116 -1126
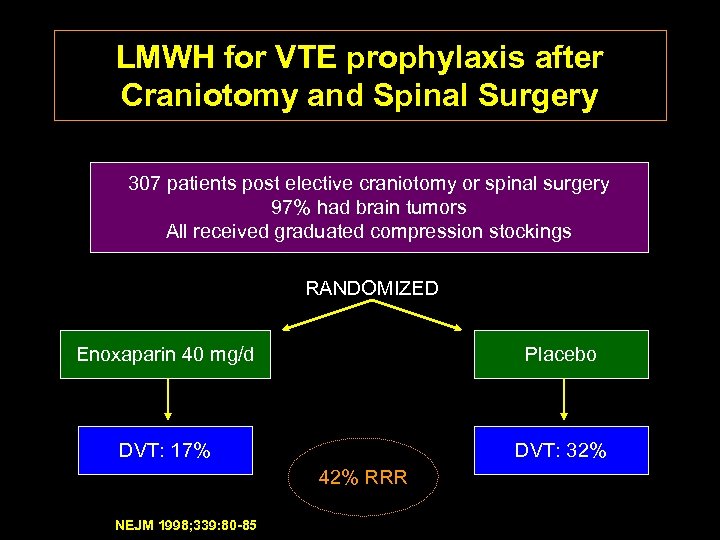
LMWH for VTE prophylaxis after Craniotomy and Spinal Surgery 307 patients post elective craniotomy or spinal surgery 97% had brain tumors All received graduated compression stockings RANDOMIZED Enoxaparin 40 mg/d Placebo DVT: 17% DVT: 32% 42% RRR NEJM 1998; 339: 80 -85
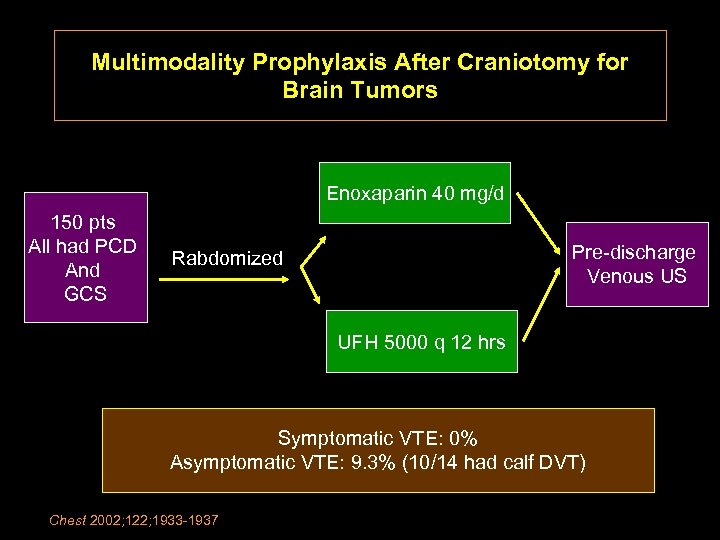
Multimodality Prophylaxis After Craniotomy for Brain Tumors Enoxaparin 40 mg/d 150 pts All had PCD And GCS Pre-discharge Venous US Rabdomized UFH 5000 q 12 hrs Symptomatic VTE: 0% Asymptomatic VTE: 9. 3% (10/14 had calf DVT) Chest 2002; 122; 1933 -1937
Strategies for decreasing the Incidence of VTE after Acute Ischemic Stroke, SCI, and Post craniotomy • Effective and optimal in-patient prophylaxis • ? Extended out of hospital prophylaxis • ? Early diagnosis of subclinical VTE (screening serial US, D-Dimer, MRV) • ? Multi-modality approach • Prompt diagnosis and treatment of clinically apparent VTE (saves life and prevents recurrence)
2991a1d2b8590bb80c4e4721b6f3fad8.ppt