eccbb9bb320645206d39cf4962bc1594.ppt
- Количество слайдов: 20
Strengthening Urban Health for advancing Universal Health Coverage in India Universal Health Coverage Day 2017 12 Dec 2017; New Delhi; India Chandrakant Lahariya, MD, MBA, DNB, FIPHA National Professional Officer- Universal Health Coverage World Health Organization India Mobile: 09810160665; email: lahariyac@who. int ; c. lahariya@gmail. com
Urban challenges (& inequities) are increasingly being recognized • In London, people live 17 years longer in Westminster area than those just a few stations further along • People in some communities in Baltimore, USA, live 20 fewer years than others in the same city. • Inequities, in all spheres, within urban areas have been widely documented (Globally). • A study of >100 countries reported that body mass index (BMI) & blood cholesterol levels, both major risk factors for NCDs, rose rapidly with increases in national income & level of urbanization • Urbanization comes with its own and unique
Understandable International attention (1/2) • World Health Day 2010: 1000 Cities, 1000 Lives campaign • 2010, WHO and UN-Habitat report “Hidden Cities: unmasking and overcoming health inequities in urban settings”. • UNICEF’s State of the world’s children 2012: Children in an urban world • UNAIDS’ 2014: The cities report • Save the Children’s (2015): State of the world’s mothers: the urban disadvantage.
Understandable International attention (1/2) • ‘Global Forum on Urbanization and Health’ in Kobe, Japan, 2010, ‘call to action’ focused on three major areas – evidence-based action – multisectoral coordination & – community participation in decision-making. • UN conference on ‘housing and sustainable urban development, Quito; Oct 2016 • WHO ‘Urban Health Equity Assessment & Response Tool (Urban HEART): Tools to help local authorities & civil society to plan action on health inequities
. . urban issues, part of SDGs § SDG 3. 8: UHC that is key to advancing equity, § SDG 11. 3: Planning and management for inclusive and sustainable urbanization. § SDG 3. 9 for health and SDG 11. 6 for cities, both focus on the impacts of air pollution. § former emphasizes reducing deaths and disease, § the latter focuses on the environmental impacts. § Targets 3. 6 &11. 2, both relate to improving road safety.
Urban health challenges in India documented o Multiple agencies delivering services, limited coordination & multiple authorities to govern (MOH & Municipalities) o Mixed health system: public, private (for profit) and not for profit providers o Primary health care lacking in urban settings o Paucity of public sector facilities, Catered by formal & informal private sector: Often overcharging with high OOPE o Higher prevalence of NCD risk factors in urban o NUHM (2013) designed to address these Source: Mo. HFW, 2013 6
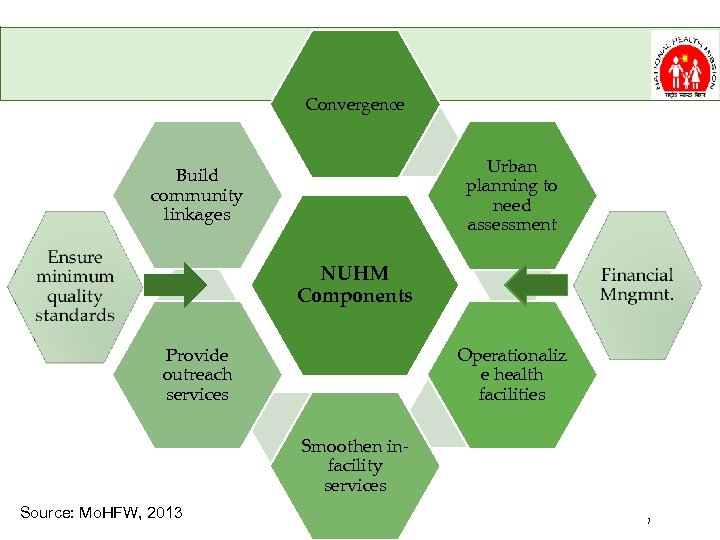
Convergence Urban planning to need assessment Build community linkages NUHM Components Operationaliz e health facilities Provide outreach services Smoothen infacility services Source: Mo. HFW, 2013 7
NUHM has made some difference; however, there areas for improvement WHO India studies & analyses: o Analysis of urban health scenario from health systems perspective o Training Need Assessment for urban health in tier 2 & 3 cities o Assessment of Health Care Delivery for NCDs in Urban Areas through the Public Health System 8
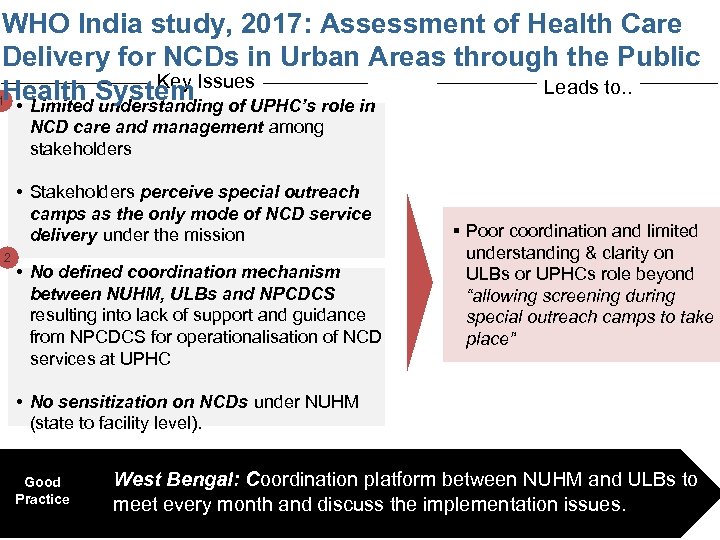
WHO India study, 2017: Assessment of Health Care Delivery for NCDs in Urban Areas through the Public Key Leads to. . Health System Issues. UPHC’s role in 1 • Limited understanding of NCD care and management among stakeholders • Stakeholders perceive special outreach camps as the only mode of NCD service delivery under the mission 2 • No defined coordination mechanism between NUHM, ULBs and NPCDCS resulting into lack of support and guidance from NPCDCS for operationalisation of NCD services at UPHC § Poor coordination and limited understanding & clarity on ULBs or UPHCs role beyond “allowing screening during special outreach camps to take place” • No sensitization on NCDs under NUHM (state to facility level). Good Practice § West Bengal: Coordination platform between NUHM and ULBs to meet every month and discuss the implementation issues.
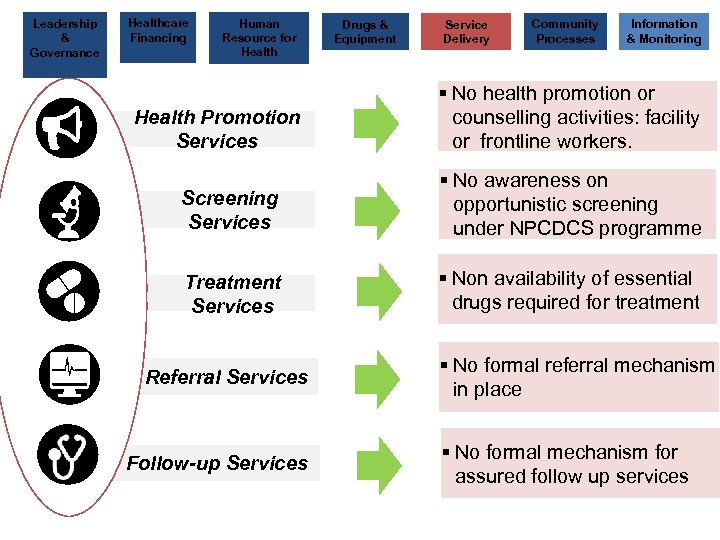
Leadership & Governance Healthcare Financing Human Resource for Health Promotion Services Drugs & Equipment Service Delivery Community Processes Information & Monitoring § No health promotion or counselling activities: facility or frontline workers. Screening Services § No awareness on opportunistic screening under NPCDCS programme Treatment Key Findings (7/11) Services § Non availability of essential drugs required for treatment Referral Services Follow-up Services § No formal referral mechanism in place § No formal mechanism for assured follow up services
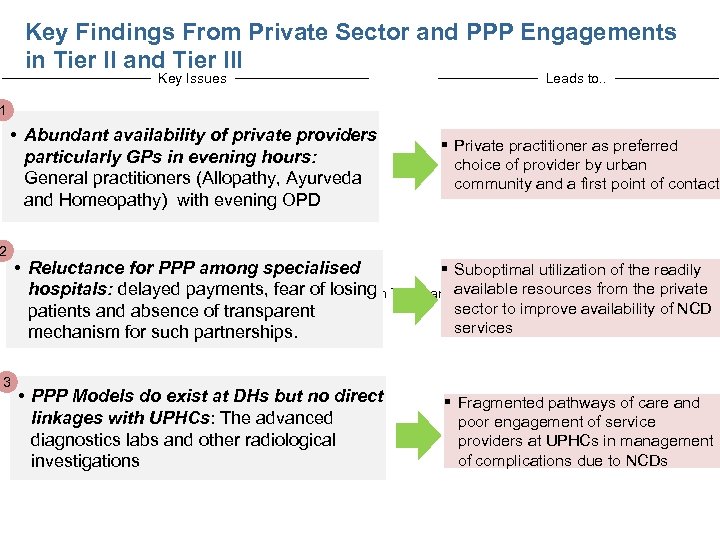
Key Findings From Private Sector and PPP Engagements in Tier II and Tier III Key Issues Leads to. . • Abundant availability of private providers particularly GPs in evening hours: General practitioners (Allopathy, Ayurveda and Homeopathy) with evening OPD § Private practitioner as preferred choice of provider by urban community and a first point of contact 1 2 3 • Reluctance for PPP among specialised § Suboptimal utilization of the readily hospitals: delayed payments, fear of losing Key Findings From Private Sector and PPP Engagements in Tier II andavailable resources from the private Tier III cities (10/11) sector to improve availability of NCD patients and absence of transparent services mechanism for such partnerships. • PPP Models do exist at DHs but no direct linkages with UPHCs: The advanced diagnostics labs and other radiological investigations § Fragmented pathways of care and poor engagement of service providers at UPHCs in management of complications due to NCDs
Are there success stories?
Cities often cited as case studies for urban initiatives (including for health) • Curitiba, Brazil: Continued political leadership and public commitment; Integrated urban services and an independent planning and implementing agency • New York City, USA: Strong and sustained leadership of Mayor of New York City and legislative support • Guangzhou, China: Leadership & sustainable healthcare financing • Bogota, Columbia: Focus on non- health issues and sustainable financing • Dar es Salaam, Tanzania: Capacity building, community participation & sustainable finding Source: Barbiero VK. Glob Health Sci Pract. 2014 Global report on urban health; WHO; 2016
Common success factors in these cities • High level of sustained political leadership • Multi-sectoral & inter-sectoral actions and in coordination with different urban agencies : • Improved planning, implementation, and management capacity of urban municipalities
The way forward
What has worked in other settings, should work for India as well • High level of sustained political leadership & champions for urban health • Multi-sectoral & inter-sectoral actions and in coordination with different urban agencies : • Improved planning, implementation, and management capacity of urban
Prioritize urban primary healthcare • An UPHC for every 50, 000 population: Is this right approach? – In catchment area, around 20% of DM & HT cases would be approx. 8, 000 cases in need of regular medications. – We need additional approaches than an UPHC for 50 K. • The idea of converting HSC into Health & Wellness centres should be fully used to expand urban PHC – Capital investment to build HWC – HRH reforms, task shifting; capacity building, community participation; Establishing continuity of care
Innovations and demonstrations • Design and implement a set of urban health demonstration projects. • Potential role of medical colleges: Urban health centres and integrated care • District hospitals to partner in integrated continuity of care: run a few HWC and UPHC
Indicative steps to improve urban health services 1. Develop & offer agreed package of quality health services 2. Enroll additional providers & facilities to address the quantity gap in health services 3. Implement agreed strategies to tackle NCDs 4. Develop robust mechanisms to identify target population through using information and communication technology 5. Strengthen population health services 6. Engage self-government institutions Source: Lahariya C, Bhagwat S, Saksena P , Samuel R (2016) J Health and local Management
Thank you Dr Chandrakant Lahariya National Professional Officer, WHO India
eccbb9bb320645206d39cf4962bc1594.ppt