cb8db1c9564743b463d7311df000062b.ppt
- Количество слайдов: 84

“Stereotactic body radiotherapy (SBRT) for early stage lung cancer” 3 rd Annual Atlantic Canada Thoracic Oncology Conference October 20 -21, 2011 Pier 21, Halifax, NS Gregory M. M. Videtic, MD, CM, FRCPC Associate Professor, Cleveland Clinic Lerner College of Medicine; Section Head for Thoracic Malignancies, Dept. of Radiation Oncology, Taussig Cancer Institute The Cleveland Clinic

CONFLICTS OF INTEREST ¡ NONE

OBJECTIVES ¡ ¡ To review the nature and the problem of early stage lung cancer To review the standard of care with respect to managing early stage lung cancer To review the principles and practice of stereotactic body radiotherapy (SBRT) as they apply to early stage lung cancer To review SBRT experience at the Cleveland Clinic
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡Program initiated in 6/04 ¡~500 medically inoperable early stage NSCLC pts treated to date Some oligometastatic cases (~50) l 7 stage I SCLC cases (!) l

A little background first…

Epidemiology of Lung Cancer ¡ ¡ Leading cause of cancer-related deaths worldwide Most common malignancy worldwide l over 1 million cases now being diagnosed yearly l USA Cancer Statistics 2009 ¡ Estimated new cases: 219, 440 l ¡ 15% of all new cancer diagnoses Estimated Deaths: 159, 390 l 29% of all cancer deaths l (#1 Cancer Killer of Men and Women) Jemal A et al. CA Cancer J Clin. 2009; 59: 225
INTRODUCTION ¡ Definition of Early Stage Non-Small Cell Lung Cancer (NSCLC) l l l ¡ Confined to lung, about 15 -20% of total cases [30 -40, 000 cases annually] By TNM staging: IA or IB Thus, No LOCOREGIONAL lymph nodes Standard of care l Surgery: 5 -year survival 50 -70%

EARLY STAGE Node Negative Lung Cancer Gold Standard Rx = Surgery ¡ ¡ ¡ Time honored position Patient selection - proper staging (pathologic node negative ) - adequate pulmonary reserve - absent or controlled medical problems Effective treatment - impressive local control (65 -90%) - overall survival 60 -80% at 5 years

EARLY STAGE LUNG CANCER ¡ “Surgical resection remains the gold standard for treatment of patients with stage I and II NSCLC…” l ¡ Ginsberg RJ & Pot JL. Surgical therapy of stage I and non-T 3 N 0 stage II non-small cell lung cancer. In: “Lung Cancer-Principles and Practice”. Eds. Pass HI et al. Lippincott, Williams and Wilkins, Philadelphia, PA; 2000. p. 691. Mountain CF. Semin. Surg. Oncol. 18: 106– 115, 2000. l 5 -year Overall Survival for stage I NSCLC ¡ ¡ clinical stage IA-61% vs. pathologic stage IA-67% clinical stage IB-38% vs. pathologic stage IB-57%
Randomized Trial of Lobectomy Versus Limited Resection for T 1 N 0 Non-Small Cell Lung Cancer. Ginsberg and Rubinstein ¡ Conclusions l Compared with lobectomy, limited pulmonary resection does not confer improved perioperative morbidity, mortality, or late postoperative pulmonary function. Because of the higher death rate and locoregional recurrence rate associated with limited resection, lobectomy still must be considered the surgical procedure of choice for patients with peripheral T 1 N 0 non-small cell lung cancer.

Lung Cancer Study Group Ginsberg, et al. Ann Thorac Surg. 1995 Sep; 60(3): 615 -22

How Good is “Gold”? ¡ ¡ Surgery is a very good but non-perfect treatment NB: path stage I 5 -yr OS is “ONLY” 6070% l Local failures, death from cancer (even controlling for pathological staging) ¡ Toxicity, pain and suffering ¡ Expense - hospitalization, recovery, lost work/income, etc. ¡ Surgery not appropriate for many!
![INTRODUCTION ¡ Many early stage pts [30 -50%] potentially resectable but MAY have reasons INTRODUCTION ¡ Many early stage pts [30 -50%] potentially resectable but MAY have reasons](https://present5.com/presentation/cb8db1c9564743b463d7311df000062b/image-13.jpg)
INTRODUCTION ¡ Many early stage pts [30 -50%] potentially resectable but MAY have reasons for being medically inoperable l Co-morbidities preventing surgical resection include l l l ¡ COPD Cardio-vascular Disease Poor performance status Doing “nothing” is not good in med inop pts ¡ Mc. Garry et al. (Chest 2002): Lung cancer cause of death in 53% of 75 stage I medically inoperable pts treated with observation alone


EARLY STAGE LUNG CANCER ¡ Management of the medically inoperable early lung cancer pt l l O. S. with primary conventional daily fractionated RT historically poor BUT O. S. with RT confounded by Patient co-morbidities (competing death causes) ¡ RT interacting with co-morbidities l e. g. COPD exacerbation ¡
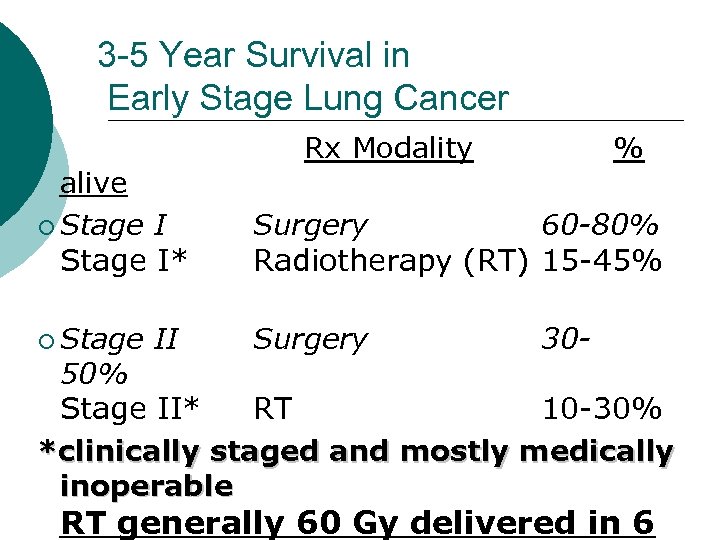
3 -5 Year Survival in Early Stage Lung Cancer Rx Modality % alive ¡ Stage I* Surgery 60 -80% Radiotherapy (RT) 15 -45% ¡ Stage Surgery II 30 - 50% Stage II* RT 10 -30% *clinically staged and mostly medically inoperable RT generally 60 Gy delivered in 6

“OLD-SCHOOL” RADIOTHERAPY ALONE CAN CURE LUNG CANCER! ¡ ¡ ¡ SELECTION LUCK? “The real reason we use conventionally fractionated RT is in fact because of the normal tissues, not the tumor. ” Bob Timmerman, 2007

Local Progression-Free Survival Is a Function of Dose ~ 84 Gy would be needed for ~ 50% local progression - free survival in 30 months Mehta M, Manon R. Sem Oncol. 2005; (Suppl 3): s 25–s 34.
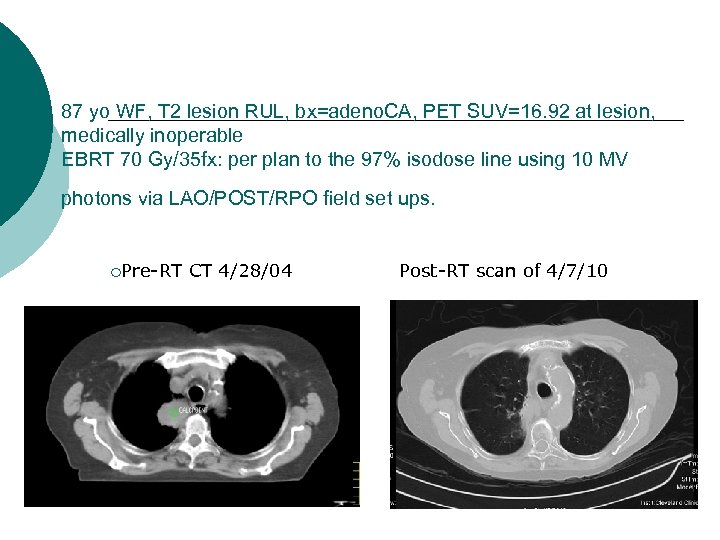
87 yo WF, T 2 lesion RUL, bx=adeno. CA, PET SUV=16. 92 at lesion, medically inoperable EBRT 70 Gy/35 fx: per plan to the 97% isodose line using 10 MV photons via LAO/POST/RPO field set ups. ¡Pre-RT CT 4/28/04 Post-RT scan of 4/7/10
RT and lung cancer ¡ The efficacy and safety of RT reflect the interplay between total dose delivered to the malignant tumor l the rate of dose delivery (daily fractionation) l the volume (and type) of tumorbearing organ irradiated. l The intrinsic tolerance of the tissue irradiated l
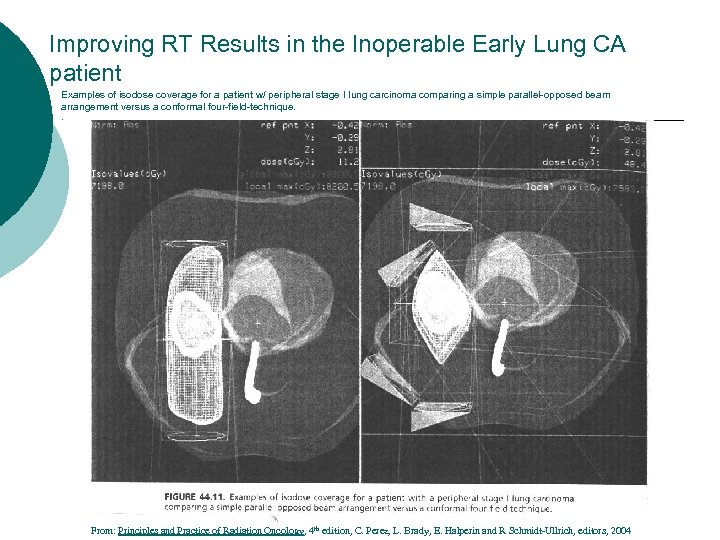
Improving RT Results in the Inoperable Early Lung CA patient Examples of isodose coverage for a patient w/ peripheral stage I lung carcinoma comparing a simple parallel-opposed beam arrangement versus a conformal four-field-technique. . From: Principles and Practice of Radiation Oncology, 4 th edition, C. Perez, L. Brady, E. Halperin and R Schmidt-Ullrich, editors, 2004



Spread out the Entrance Dose/focus on the target

The origins of lung stereotactic body radiotherapy (SBRT) ¡ Modeled after brain radiosurgery principles l l l Multiple convergent beams Rigid patient immobilization Precise localization via stereotactic coordinate system Single fraction treatment Size-restriction for target

INTRODUCTION ¡ What is SBRT? Technical l l Multiple convergent beams of RT aimed at target Requires rigid patient immobilization MUST account OR compensate for organ motion Precise localization of target via stereotactic coordinate system Size-restriction for target
INTRODUCTION ¡ What is SBRT? Technical l Typically few-fraction (1 to 5) RT using large individual fraction doses l High dose conformality, i. e. , “tight around target” l Rapid dose fall-off from target to surrounding normal tissue.

Many ways to skin a cat…

INTRODUCTION Use of “Image Guidance”Technology for frequent 2 D and 3 D imaging, during RT, to verify/direct radiation therapy checked against the “standard” : Imaging coordinates set by images set at simulation and used for planning
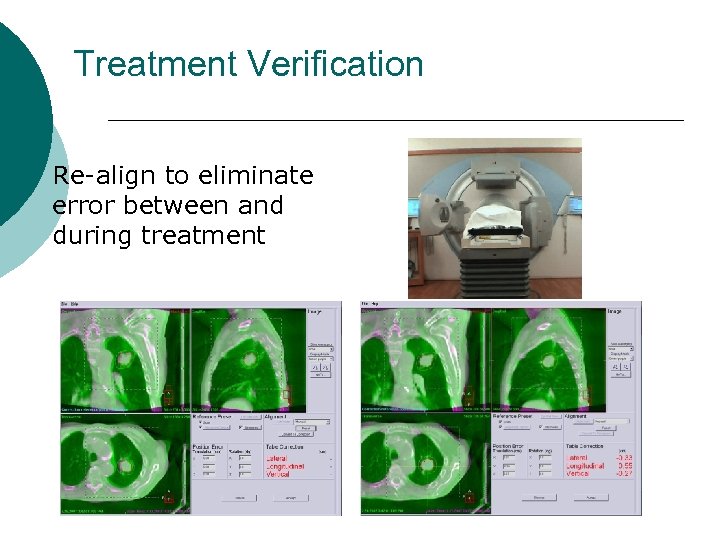
Treatment Verification ¡ Re-align to eliminate error between and during treatment
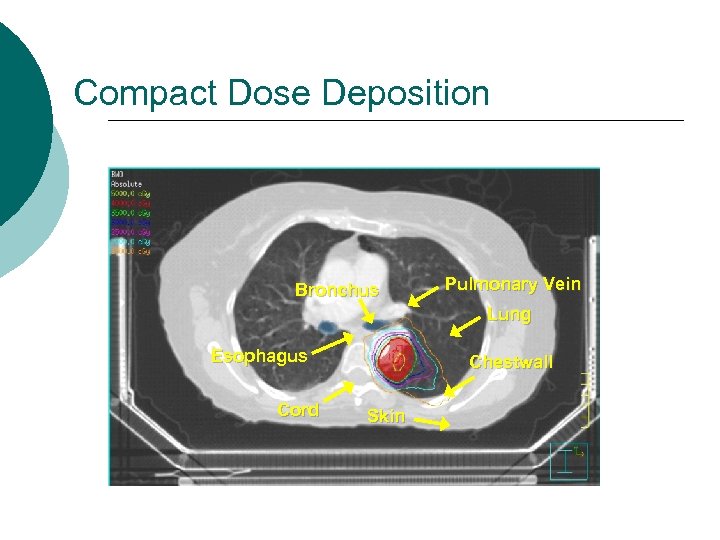
Compact Dose Deposition Bronchus Pulmonary Vein Lung Esophagus Cord Chestwall Skin

Lung tumors move with time
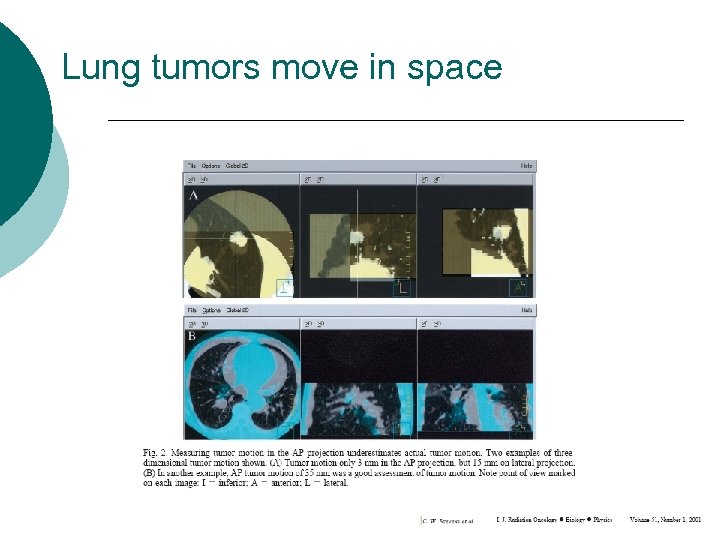
Lung tumors move in space
How do we deal with tumor motion? ¡ Solutions (is there just one? ? ) l Tumor factors Stop the tumor from moving. . somehow ¡ Follow the tumor as it is moving and treat as it moves ¡ l Patient factors Stop the patient from breathing (!) ¡ Control the patient’s breathing ¡ l Machine factors ¡ Turn on machine only when it “sees” tumor

SBRT and Early Lung Cancer CLINICAL EXPERIENCE Numerous series document efficacy and safety of SBRT in early lung cancer Recent review of rationale, techniques, applications and optimization of SBRT for various extracranial sites (Song et al. Oncology, 2004) -Includes lung cancer (primary/metastatic)
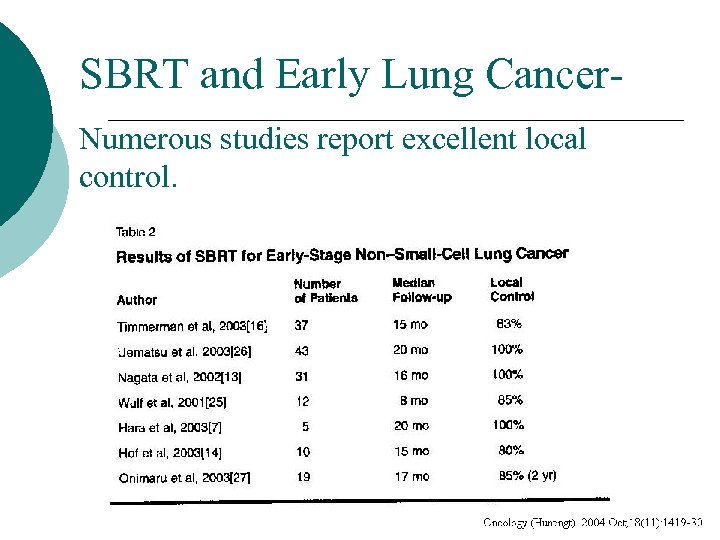
SBRT and Early Lung Cancer. Numerous studies report excellent local control.

SBRT and Early Lung Cancer. The radiobiological dose matters, I. e. , >100 Gy equivalent

SBRT and Early Lung Cancer ¡ Treatment Toxicities l Reported rates generally low ¡ l > grade 3 pneumonitis, hypoxia: < 5% Related to tumor location ¡ RTOG SBRT eligibility l l l Tumors must be at “ 2 cm or beyond the zone of the proximal bronchial tree” Restriction due to high bronchial injury rates Based on work of Timmerman et al at U Indiana
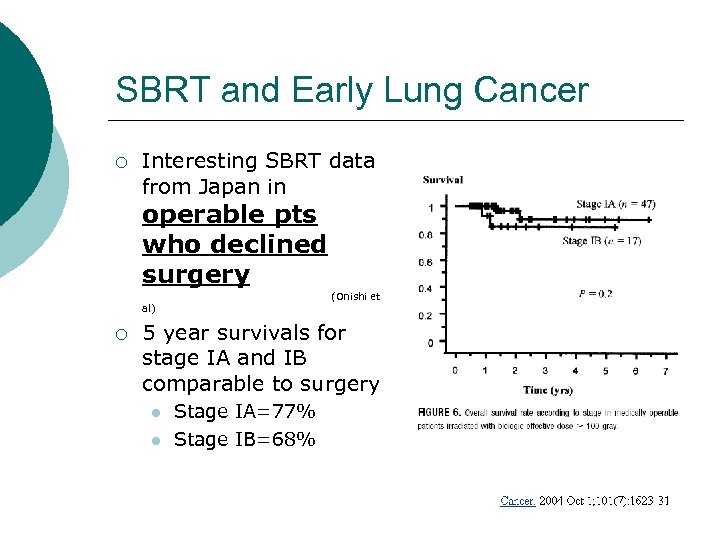
SBRT and Early Lung Cancer ¡ Interesting SBRT data from Japan in operable pts who declined surgery (Onishi et al) ¡ 5 year survivals for stage IA and IB comparable to surgery l l Stage IA=77% Stage IB=68%

SBRT for Early Lung Cancer: The Cleveland Clinic program
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡Program initiated in 6/04 ¡~500 medically inoperable early stage NSCLC pts treated to date Some oligometastatic cases (~50) l 7 stage I SCLC cases (!) l

SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ PATIENT SELECTION Defined as early stage AND medically inoperable following l l Review by the Thoracic Multidisciplinary Lung Team ¡ Surgeon ¡ Pulmonologist ¡ Radiation Oncologist ¡ Medical Oncologist ¡ (Cardiothoracic service/Cardiology) Staging (complete) to include ¡ PET ¡ +(/-) Mediastinoscopy ¡ +(/-) Biopsy- morbidity of procedure of

SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Treatment Regimen Model l Uematsu et al. IJROBP 2001; 51: 666 -670 5 yr. reported experience with Stage I NSCLC ¡ 50 patients (medically inoperable / refused surgery) ¡ Dose 50 -60 Gy / 5 -10# /1 -2 wks ¡ T size 0. 8 -5. 0 cm ¡ Staged by CXR, CT chest, no PET, no mediastinoscopy ¡ Results: ¡ l l l 3 yr o. s. 66% for 50 patients 3 yr o. s. 86% for the 29 medically inoperable patients 3 yr c. s. s. 80% for 50 patients
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Treatment Unit Novalis Brain. Lab System 6 MV Linac ¡ Special characteristics “Automated image-guided radiation therapy system, utilizes highresolution X-rays to pinpoint internal tumor sites seconds before treatment, robotically corrects patient set-up errors and tracks any patient movement throughout the treatment, all within a standard treatment time slot” ¡
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ SBRT l l l on NOVALIS By restriction (immobilization) By tumor motion studies By creating reference frame to provide real-time verification of patient positioning and set-up
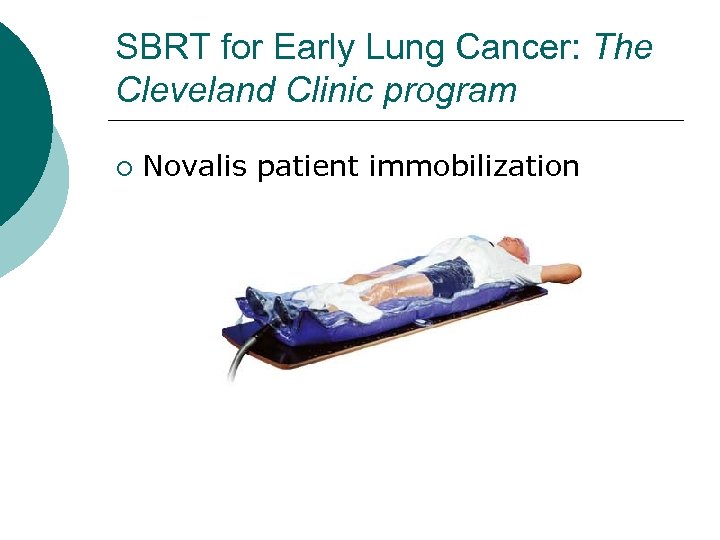
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Novalis patient immobilization Body. Fix Stereotactic Immobilizer

SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Abdominal compression/breathing restriction
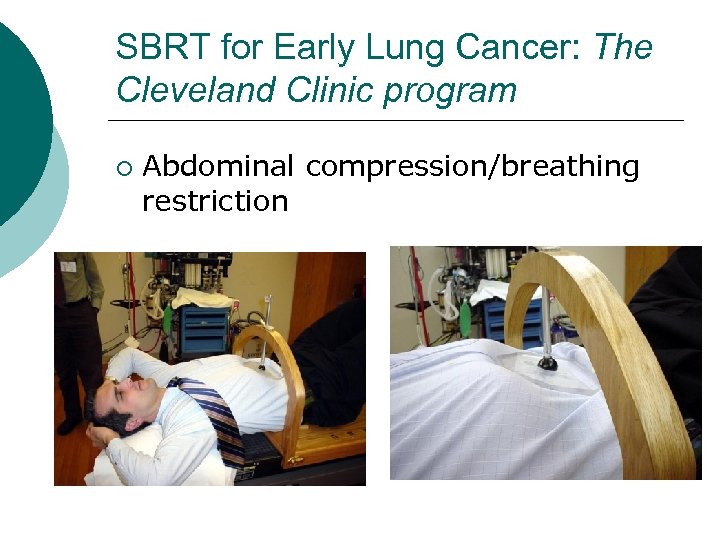
SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Abdominal compression/breathing restriction


MATERIALS & METHODS ¡ CT simulation images acquired at rest, at full inhalation, and at full exhalation were fused to generate an internal gross tumor volume (ITV) that reflected residual motion after external compression ¡ CT Sim: Assessment of target motion l free breathing, full inhale, and full exhale

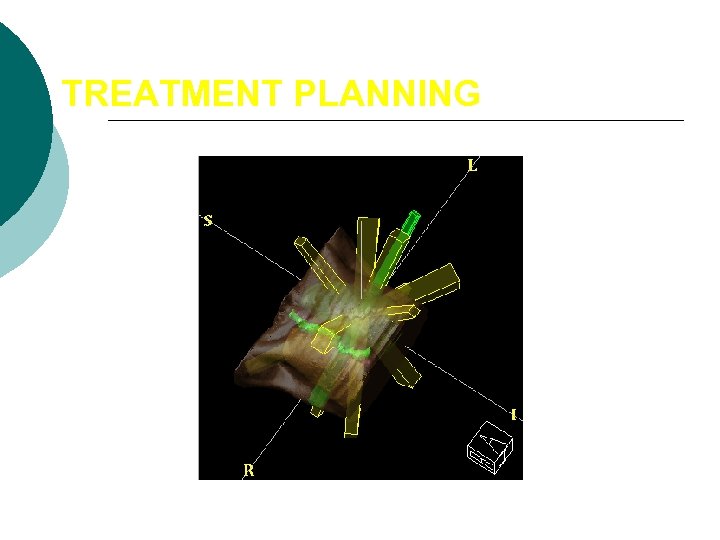
TREATMENT PLANNING




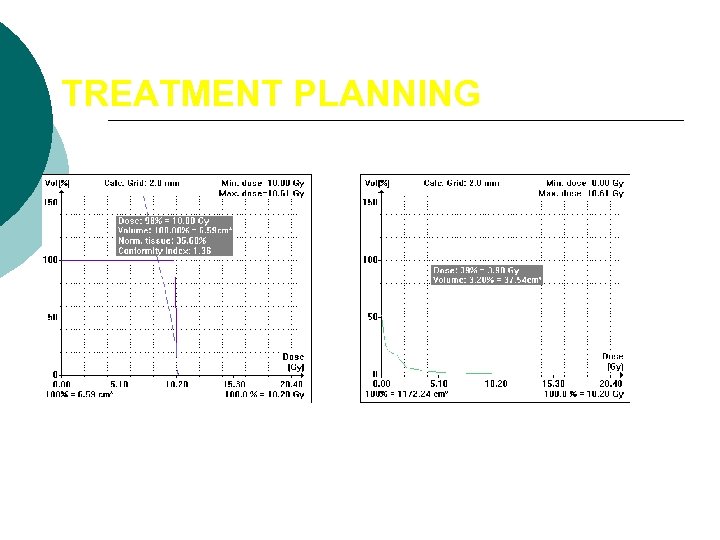
TREATMENT PLANNING
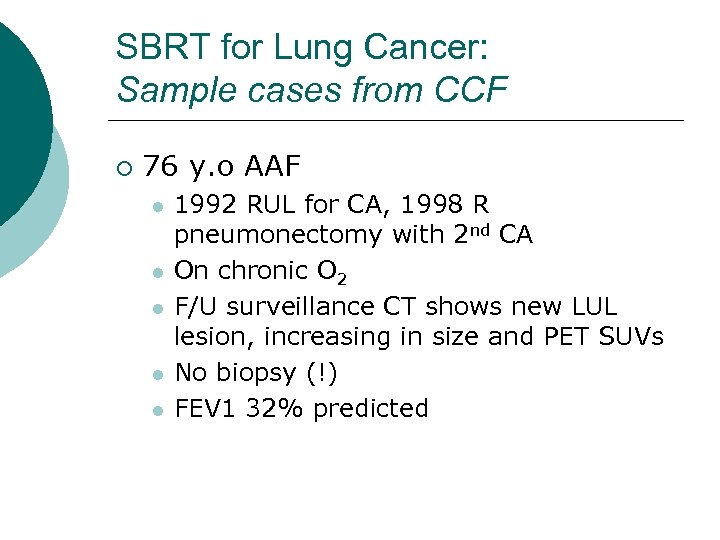
SBRT for Lung Cancer: Sample cases from CCF ¡ 76 y. o AAF l l l 1992 RUL for CA, 1998 R pneumonectomy with 2 nd CA On chronic O 2 F/U surveillance CT shows new LUL lesion, increasing in size and PET SUVs No biopsy (!) FEV 1 32% predicted
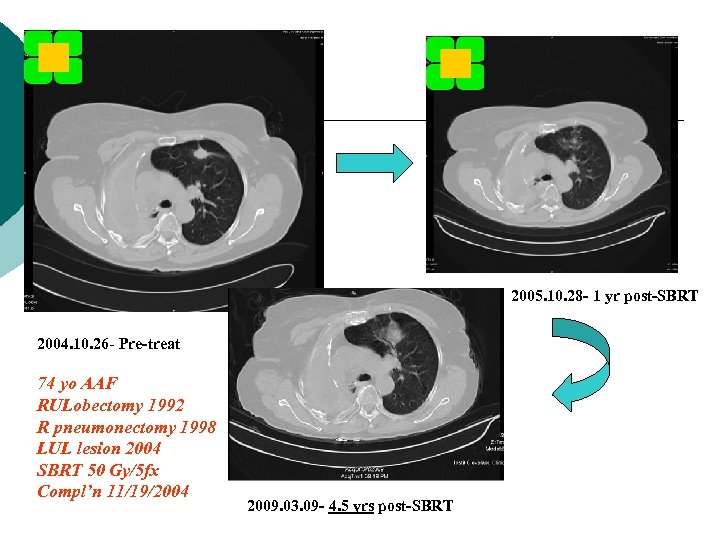
2005. 10. 28 - 1 yr post-SBRT 2004. 10. 26 - Pre-treat 74 yo AAF RULobectomy 1992 R pneumonectomy 1998 LUL lesion 2004 SBRT 50 Gy/5 fx Compl’n 11/19/2004 2009. 03. 09 - 4. 5 yrs post-SBRT

SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ SBRT administration l “In-House” standard Central tumors: 50 Gy in 5 sequential fractions of 10 Gy [Monday through Friday] ¡ Peripheral tumors: 60 Gy in 3 fractions [over 8 -14 days, min 40 hrs/max 7 days between fractions ¡ l Selected cases ¡ 48 Gy in 4 fractions ¡ 60 Gy in 8 fractions ¡ 50 Gy in 10 fractions ¡ 30 Gy in one fraction


SBRT for Early Lung Cancer: The Cleveland Clinic program ¡ Follow-up schedule for control and assessment of toxicity l 6 weeks, then Q 3 m for 2 yrs ¡ ¡ CT chest + contrast Q 3 months PFTs/DLCO Q 6 months


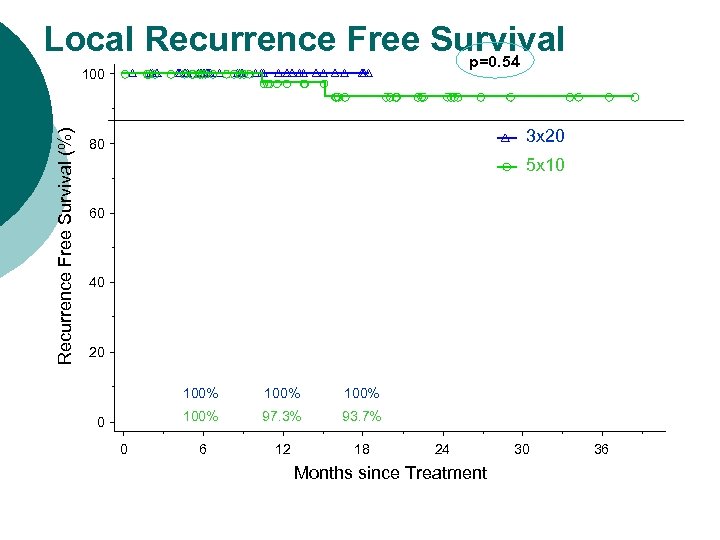
Local Recurrence Free Survival p=0. 54 Recurrence Free Survival (%) 100 3 x 20 80 5 x 10 60 40 20 100% 0 100% 97. 3% 93. 7% 6 12 18 24 Months since Treatment 30 36

Overall Survival 100 80 Overall Survival (%) p=0. 68 3 x 20 5 x 10 60 40 20 90. 5% 0 76. 9% 93. 9% 0 76. 9% 83. 1% 75. 9% 55. 5% 6 12 18 24 30 Months since Treatment 36 42 48
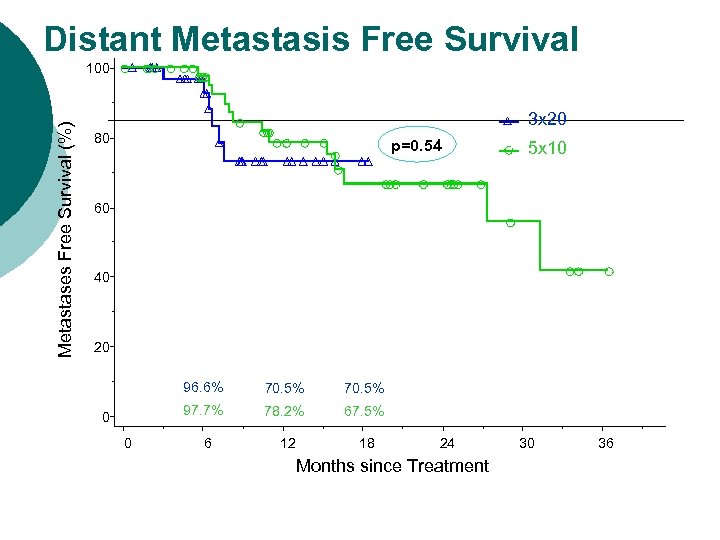
Distant Metastasis Free Survival Metastases Free Survival (%) 100 3 x 20 80 p=0. 54 5 x 10 60 40 20 96. 6% 0 70. 5% 97. 7% 0 70. 5% 78. 2% 67. 5% 12 18 6 24 Months since Treatment 30 36



Developing Lung SBRT: An approach to Research ¡ Collaborative Group Support l RTOG 0236 -phase I/II of 60 Gy/3 fx l l RTOG 0813 -phase I/II- set MTD of SBRT for early-stage, centrally located NSCLC l l Ongoing, CCF accrual YTD 6 pts RTOG 0915 -randomized phase II, peripheral tumors, 34 Gy/1 fraction vs. . 48 Gy/4 fractions, primary end point of toxicity l l CCF 3 rd highest accruer Roswell Park phase III study of 30 Gy/1 fx vs. 60 Gy/ 3 fx l 15 pts accrued YTD


Developing Lung SBRT: An approach to Research Establish IRB approved prospective data registry of all SBRT patients ¡ 1. ¡ 2. Demonstrate efficacy l l l Videtic GMM, Stephans K, Reddy CA, Gajdos S, Kolar M, Clouser E, Djemil T. IMRT-based Stereotactic Body Radiotherapy for Medically Inoperable Early Stage Lung Cancer: Excellent Local Control. Int J Radiat Oncol Biol Phys. 2010; 77: 344 -349. Stephans KL, Djemil T, Reddy CA, Gajdos SM, Kolar M, Mason D, Murthy S, Rice TW, Mazzone P, Machuzak M, Mekhail T, Videtic GM. A comparison of two stereotactic body radiation fractionation schedules for medically inoperable stage I non-small cell lung cancer: the Cleveland Clinic experience. J Thorac Oncol. 2009; 4: 976 -982

Developing Lung SBRT: An approach to Research ¡ 3. Establish acute safety l ¡ 4. Stephans KL, Djemil T, Reddy CA, Gajdos SA, Kolar M, Mazzone P, Videtic GMM. Comprehensive assessment of Pulmonary Function Test (PFT) Changes after Stereotactic Body Radiotherapy (SBRT) for Stage I Lung Cancer in Medically Inoperable Patients. J Thorac Oncol. 2009; 4: 838 -844. What about long-term safety? l Woody NM, Djemil T, Adelstein DJ, Mason DP, Rice TW, Videtic GMM. Severe Local Toxicity after Lung Stereotactic Body Radiation Therapy (SBRT): Lesional abscess leading to bronchocutaneous fistula requiring surgical marsupialization. J Thorac Oncol. 2010; 5: 1874 -1875. l Stephans KL, Djemil T, Tendulkar RD, Robinson CG, Reddy CA, Videtic GM. Prediction of Chest Wall Toxicity From Lung Stereotactic Body Radiotherapy (SBRT). Int J Radiat Oncol Biol Phys. 2011 Feb 5. [Epub ahead of print]

Developing Lung SBRT: An approach to Research ¡ 5. Advancing the discipline l l l Burdick MJ, Stephans KL, Reddy CA, Djemil T, Srinivas SM, Videtic GMM. SUVmax from Staging FDG- PET/CT Does Not Predict Treatment Outcome for Early Stage NSCLC Treated with SBRT. Int J Radiat Oncol Biol Phys. 2010 Nov 15; 78(4): 1033 -9. Videtic GM, Stephans K, Woody N, Pennell N, Shapiro M, Reddy C, Djemil T. A Stereotactic body radiotherapybased treatment model for stage I medically inoperable small cell lung cancer. IASLC- 14 th World Conference on Lung Cancer, July 3 -7, 2011; Amsteram, The Netherlands. Videtic GM, Reddy C, Sorenson L. Prospective Study of Fatigue and Quality of Life after Stereotactic Body Radiotherapy for Medically Inoperable Early-Stage Lung Cancer. 52 nd Annual meeting of ASTRO, October 31 November 4, 2010; San Diego, CA.
Developing Lung SBRT: An approach to Research ¡ 5. Advancing the discipline l l C. Robinson, K. Stephans, C. Reddy, T. Djemil, G. Videtic. Stereotactic Body Radiotherapy (SBRT) for Radiographically Diagnosed Primary Lung Cancer without Histologic Confirmation. 51 st Annual Meeting of the American Society for Therapeutic Radiology and Oncology, November 3, 2009; Chicago, IL. Woody NM, Stephans KL, Videtic GMM, Djemil T, Xia P. Defining Target Volume for Lung Stereotactic Body Radiotherapy (SBRT): Fixed or Motion-derived Margins? IJROB. Provisionally accepted.
Developing Lung SBRT: An approach to Research ¡ 6. Setting standards l Videtic GMM, Stephans KL. The role of stereotactic body radiotherapy in the management of non-small cell lung cancer: An emerging standard for the medically inoperable patient? Curr Oncol Rep. 2010; 12: 235 -241.
Developing Lung SBRT: An approach to Research ASTRO 2011 - Videtic: early experience with single fraction lung radiosurgery - Stephans: bronchial toxicity with SBRT: moving beyond RTOG 0813 parameters -Woody: SBRT outcomes for tumors >4 cm - Haque: outcomes for SBRT pts with PET borderline abnormalities in the mediastinum
Horizons ¡ ¡ ¡ ¡ Single fraction dosing for peripheral tumors? Ideal dose for central tumors Enhanced staging (EBUS? ) Slightly more operable patients Treatment of larger tumors Adjuvant chemo? Boost for stage III disease, or recurrence Very limited use for select oligometastatic patients.

Conclusions SBRT powerful tool for treating early lung cancer safely and effectively in medically inoperable pts ¡ Cancer control rates impressive, likely comparable to surgery ¡ Distant control: an area for innovation and investigation, given the nature of the patient population ¡

Conclusions Morbidity of treatment strikingly minimal in the acute phase ¡ LATE TO VERY LATE TOXICITY: ¡ l l Clearly highlights necessity of long term follow-up (years) Will be critical to define for operable patients
Conclusions Current technique for treating pts at CCF with tumor motion control and coverage by SBRT of potential tumor volume safe, tolerable, feasible, rapid ¡ Further enhancements in delivery technique being explored ¡ Studies in medically operable pts warranted! ¡
cb8db1c9564743b463d7311df000062b.ppt