4bbb2a18430322a92cb73358992d368b.ppt
- Количество слайдов: 17
 Steady-State Optimal Insulin Infusion for Hyperglycemic ICU Patients J G Chase, G C Wake, Z-H Lam, J-Y Lee, K-S Hwang and G. Shaw University of Canterbury Dept of Mechanical Engineering Christchurch New Zealand ICARCV 2002, Singapore
Steady-State Optimal Insulin Infusion for Hyperglycemic ICU Patients J G Chase, G C Wake, Z-H Lam, J-Y Lee, K-S Hwang and G. Shaw University of Canterbury Dept of Mechanical Engineering Christchurch New Zealand ICARCV 2002, Singapore
 Diabetes – A Brief Overview • Diabetes – A disorder of the metabolism – Type I: Body produces little or no insulin. – Type II: Insulin resistance or impaired glucose tolerance. • Complications – kidney failure, blindness, nerve damage, amputation, heart attack, stroke. • High annual costs growing exponentially with number of cases • Estimated cost to NZ is $1 B per year in 2020 – A growing epidemic! – Similar numbers hold true throughout most of the world, including Singapore.
Diabetes – A Brief Overview • Diabetes – A disorder of the metabolism – Type I: Body produces little or no insulin. – Type II: Insulin resistance or impaired glucose tolerance. • Complications – kidney failure, blindness, nerve damage, amputation, heart attack, stroke. • High annual costs growing exponentially with number of cases • Estimated cost to NZ is $1 B per year in 2020 – A growing epidemic! – Similar numbers hold true throughout most of the world, including Singapore.
 Diabetes in the ICU • Elevated blood glucose levels or Hyperglycaemia is very common among the critically ill in the ICU – Stress of the disease – Many older patients are Type II diabetic individuals – Direct result of disease • Current Treatment – – Sliding scale protocols based on magnitude with very coarse resolution Feeding 1 -2 x daily in slow infusion Generally poor control (<8 mmol/L is considered “very good”) Often overlooked because of severity of other issues and disease • Why bother? 45 reasons for every 100! – Vandenberghe et al (2001) showed that tight glucose regulation in the ICU (levels < 6 mmol/L) resulted in up to a 45% decrease in mortality
Diabetes in the ICU • Elevated blood glucose levels or Hyperglycaemia is very common among the critically ill in the ICU – Stress of the disease – Many older patients are Type II diabetic individuals – Direct result of disease • Current Treatment – – Sliding scale protocols based on magnitude with very coarse resolution Feeding 1 -2 x daily in slow infusion Generally poor control (<8 mmol/L is considered “very good”) Often overlooked because of severity of other issues and disease • Why bother? 45 reasons for every 100! – Vandenberghe et al (2001) showed that tight glucose regulation in the ICU (levels < 6 mmol/L) resulted in up to a 45% decrease in mortality
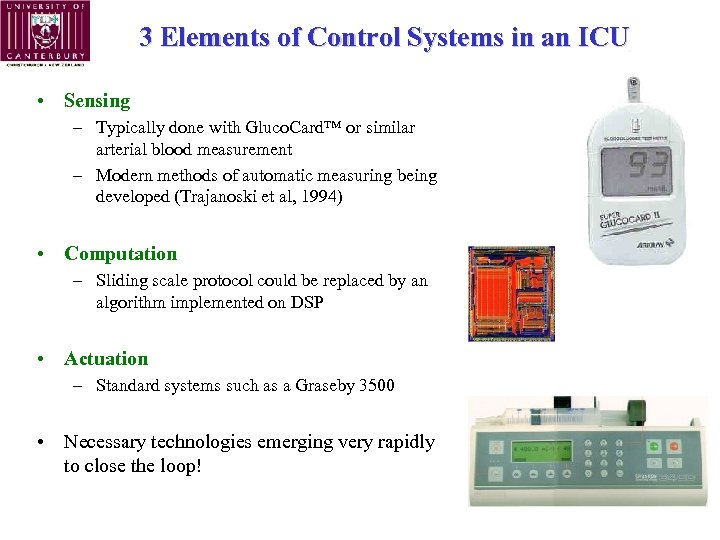 3 Elements of Control Systems in an ICU • Sensing – Typically done with Gluco. Card™ or similar arterial blood measurement – Modern methods of automatic measuring being developed (Trajanoski et al, 1994) • Computation – Sliding scale protocol could be replaced by an algorithm implemented on DSP • Actuation – Standard systems such as a Graseby 3500 • Necessary technologies emerging very rapidly to close the loop!
3 Elements of Control Systems in an ICU • Sensing – Typically done with Gluco. Card™ or similar arterial blood measurement – Modern methods of automatic measuring being developed (Trajanoski et al, 1994) • Computation – Sliding scale protocol could be replaced by an algorithm implemented on DSP • Actuation – Standard systems such as a Graseby 3500 • Necessary technologies emerging very rapidly to close the loop!
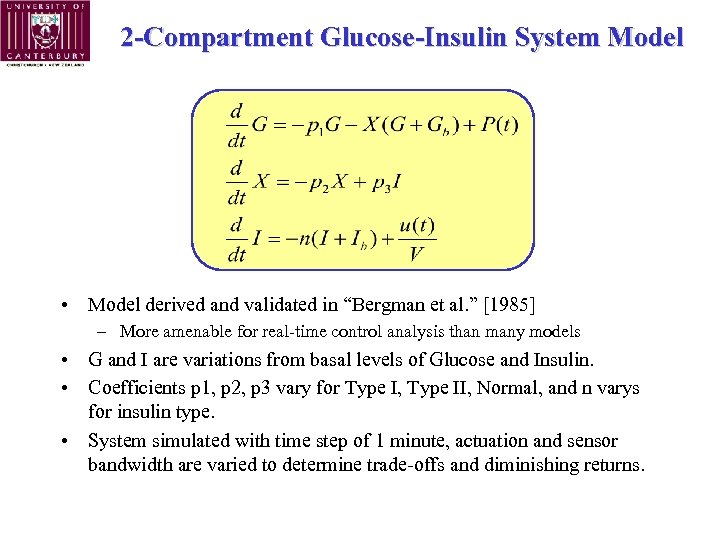 2 -Compartment Glucose-Insulin System Model • Model derived and validated in “Bergman et al. ” [1985] – More amenable for real-time control analysis than many models • G and I are variations from basal levels of Glucose and Insulin. • Coefficients p 1, p 2, p 3 vary for Type I, Type II, Normal, and n varys for insulin type. • System simulated with time step of 1 minute, actuation and sensor bandwidth are varied to determine trade-offs and diminishing returns.
2 -Compartment Glucose-Insulin System Model • Model derived and validated in “Bergman et al. ” [1985] – More amenable for real-time control analysis than many models • G and I are variations from basal levels of Glucose and Insulin. • Coefficients p 1, p 2, p 3 vary for Type I, Type II, Normal, and n varys for insulin type. • System simulated with time step of 1 minute, actuation and sensor bandwidth are varied to determine trade-offs and diminishing returns.
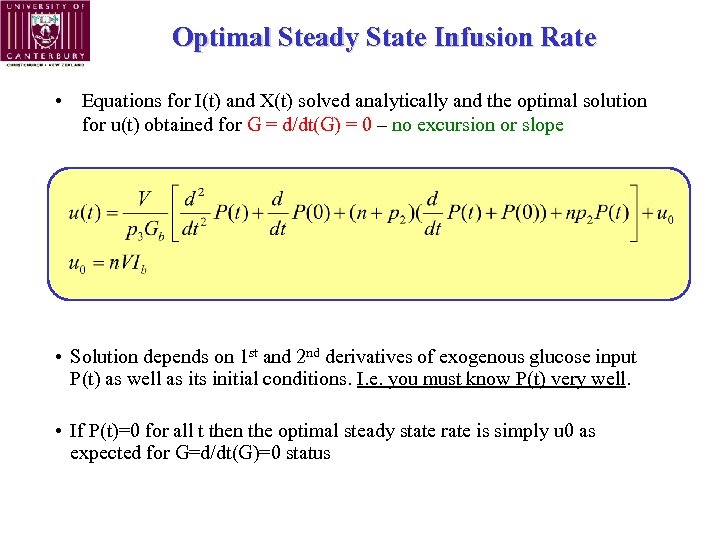 Optimal Steady State Infusion Rate • Equations for I(t) and X(t) solved analytically and the optimal solution for u(t) obtained for G = d/dt(G) = 0 – no excursion or slope • Solution depends on 1 st and 2 nd derivatives of exogenous glucose input P(t) as well as its initial conditions. I. e. you must know P(t) very well. • If P(t)=0 for all t then the optimal steady state rate is simply u 0 as expected for G=d/dt(G)=0 status
Optimal Steady State Infusion Rate • Equations for I(t) and X(t) solved analytically and the optimal solution for u(t) obtained for G = d/dt(G) = 0 – no excursion or slope • Solution depends on 1 st and 2 nd derivatives of exogenous glucose input P(t) as well as its initial conditions. I. e. you must know P(t) very well. • If P(t)=0 for all t then the optimal steady state rate is simply u 0 as expected for G=d/dt(G)=0 status
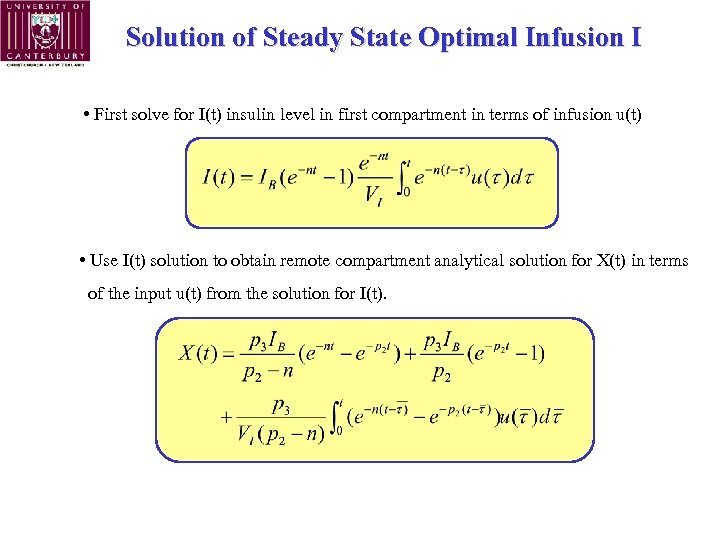 Solution of Steady State Optimal Infusion I • First solve for I(t) insulin level in first compartment in terms of infusion u(t) • Use I(t) solution to obtain remote compartment analytical solution for X(t) in terms of the input u(t) from the solution for I(t).
Solution of Steady State Optimal Infusion I • First solve for I(t) insulin level in first compartment in terms of infusion u(t) • Use I(t) solution to obtain remote compartment analytical solution for X(t) in terms of the input u(t) from the solution for I(t).
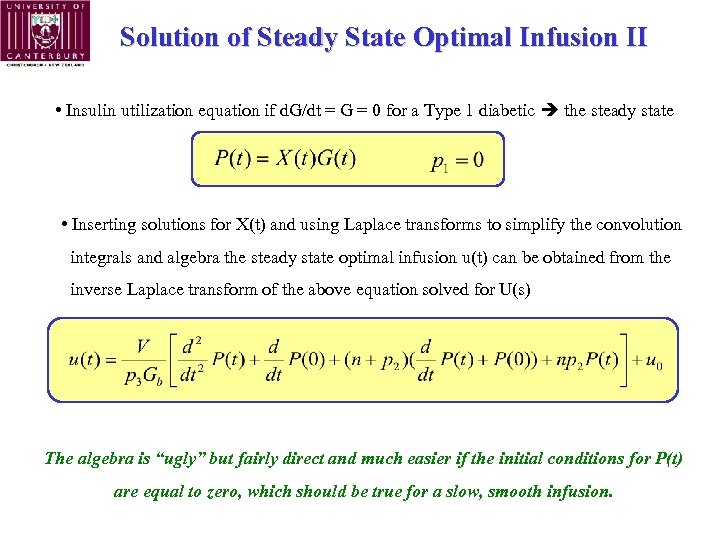 Solution of Steady State Optimal Infusion II • Insulin utilization equation if d. G/dt = G = 0 for a Type 1 diabetic the steady state • Inserting solutions for X(t) and using Laplace transforms to simplify the convolution integrals and algebra the steady state optimal infusion u(t) can be obtained from the inverse Laplace transform of the above equation solved for U(s) The algebra is “ugly” but fairly direct and much easier if the initial conditions for P(t) are equal to zero, which should be true for a slow, smooth infusion.
Solution of Steady State Optimal Infusion II • Insulin utilization equation if d. G/dt = G = 0 for a Type 1 diabetic the steady state • Inserting solutions for X(t) and using Laplace transforms to simplify the convolution integrals and algebra the steady state optimal infusion u(t) can be obtained from the inverse Laplace transform of the above equation solved for U(s) The algebra is “ugly” but fairly direct and much easier if the initial conditions for P(t) are equal to zero, which should be true for a slow, smooth infusion.
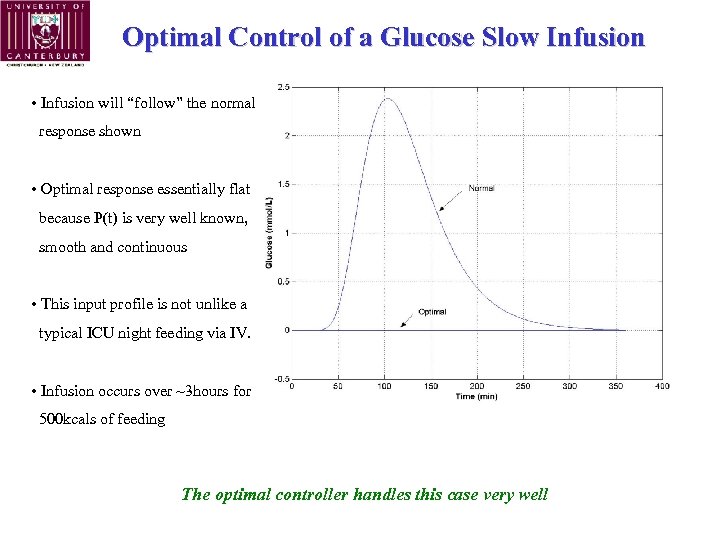 Optimal Control of a Glucose Slow Infusion • Infusion will “follow” the normal response shown • Optimal response essentially flat because P(t) is very well known, smooth and continuous • This input profile is not unlike a typical ICU night feeding via IV. • Infusion occurs over ~3 hours for 500 kcals of feeding The optimal controller handles this case very well
Optimal Control of a Glucose Slow Infusion • Infusion will “follow” the normal response shown • Optimal response essentially flat because P(t) is very well known, smooth and continuous • This input profile is not unlike a typical ICU night feeding via IV. • Infusion occurs over ~3 hours for 500 kcals of feeding The optimal controller handles this case very well
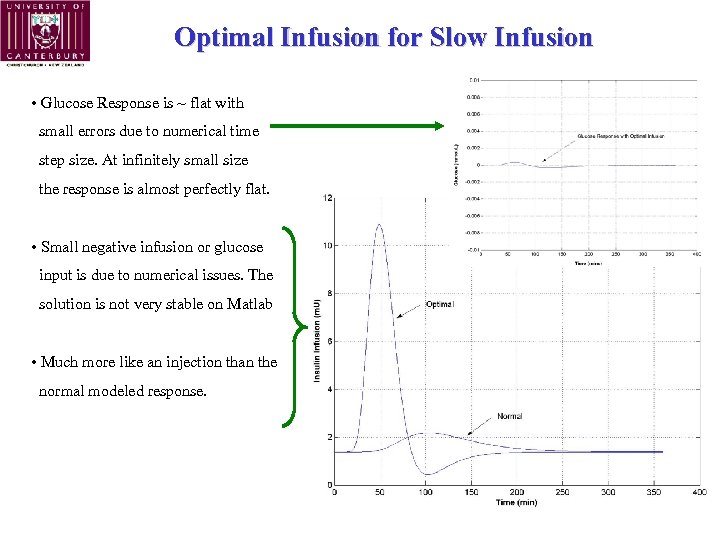 Optimal Infusion for Slow Infusion • Glucose Response is ~ flat with small errors due to numerical time step size. At infinitely small size the response is almost perfectly flat. • Small negative infusion or glucose input is due to numerical issues. The solution is not very stable on Matlab • Much more like an injection than the normal modeled response.
Optimal Infusion for Slow Infusion • Glucose Response is ~ flat with small errors due to numerical time step size. At infinitely small size the response is almost perfectly flat. • Small negative infusion or glucose input is due to numerical issues. The solution is not very stable on Matlab • Much more like an injection than the normal modeled response.
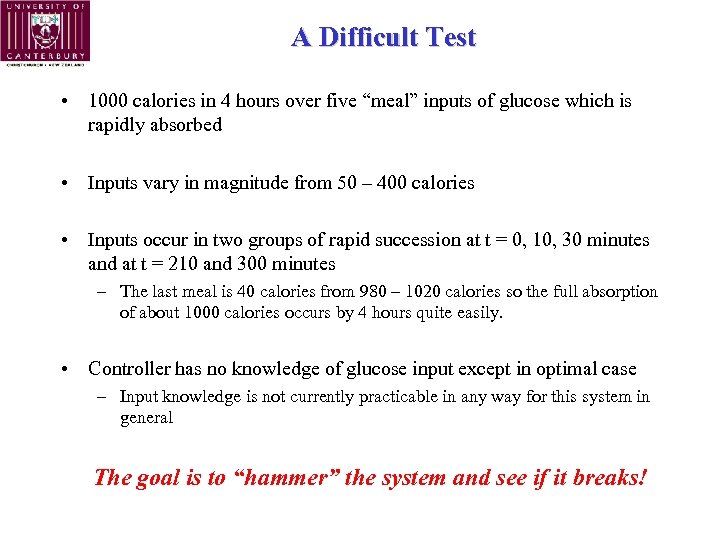 A Difficult Test • 1000 calories in 4 hours over five “meal” inputs of glucose which is rapidly absorbed • Inputs vary in magnitude from 50 – 400 calories • Inputs occur in two groups of rapid succession at t = 0, 10, 30 minutes and at t = 210 and 300 minutes – The last meal is 40 calories from 980 – 1020 calories so the full absorption of about 1000 calories occurs by 4 hours quite easily. • Controller has no knowledge of glucose input except in optimal case – Input knowledge is not currently practicable in any way for this system in general The goal is to “hammer” the system and see if it breaks!
A Difficult Test • 1000 calories in 4 hours over five “meal” inputs of glucose which is rapidly absorbed • Inputs vary in magnitude from 50 – 400 calories • Inputs occur in two groups of rapid succession at t = 0, 10, 30 minutes and at t = 210 and 300 minutes – The last meal is 40 calories from 980 – 1020 calories so the full absorption of about 1000 calories occurs by 4 hours quite easily. • Controller has no knowledge of glucose input except in optimal case – Input knowledge is not currently practicable in any way for this system in general The goal is to “hammer” the system and see if it breaks!
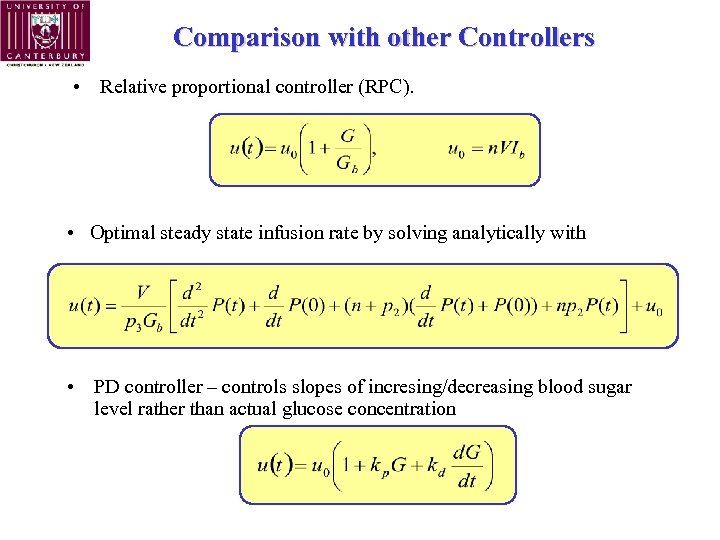 Comparison with other Controllers • Relative proportional controller (RPC). • Optimal steady state infusion rate by solving analytically with • PD controller – controls slopes of incresing/decreasing blood sugar level rather than actual glucose concentration
Comparison with other Controllers • Relative proportional controller (RPC). • Optimal steady state infusion rate by solving analytically with • PD controller – controls slopes of incresing/decreasing blood sugar level rather than actual glucose concentration
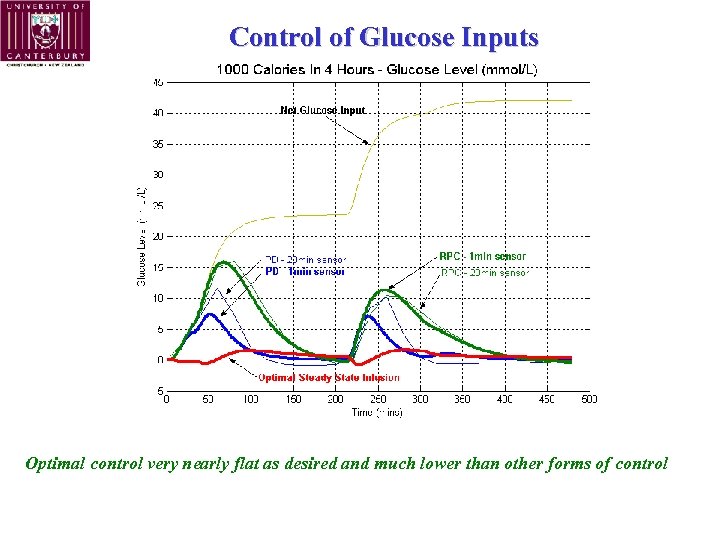 Control of Glucose Inputs Optimal control very nearly flat as desired and much lower than other forms of control
Control of Glucose Inputs Optimal control very nearly flat as desired and much lower than other forms of control
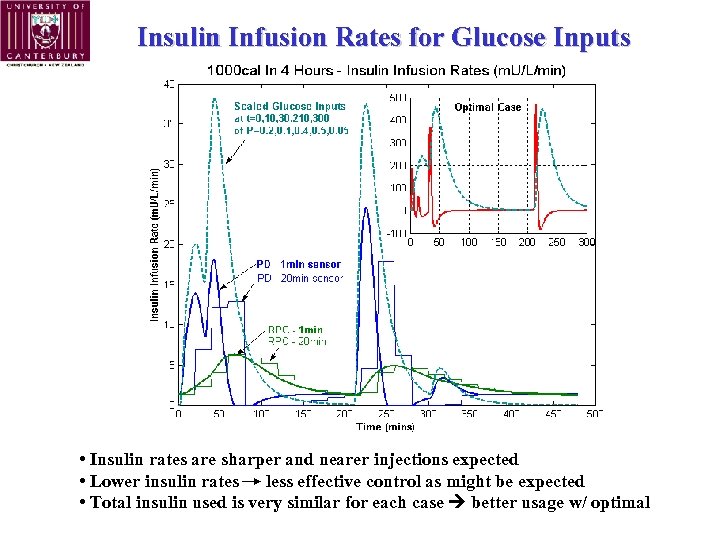 Insulin Infusion Rates for Glucose Inputs • Insulin rates are sharper and nearer injections expected • Lower insulin rates less effective control as might be expected • Total insulin used is very similar for each case better usage w/ optimal
Insulin Infusion Rates for Glucose Inputs • Insulin rates are sharper and nearer injections expected • Lower insulin rates less effective control as might be expected • Total insulin used is very similar for each case better usage w/ optimal
 Summary & Conclusions • A steady state optimal infusion solution is developed for a physiologically verified 3 compartment model of the glucose regulatory system • Solution is shown to provide the desired ~flat glucose response to steady, slow inputs as well as more significant challenges • Optimal solution does require knowledge of the glucose absorption function P(t) which is unlikely to be known outside of a controlled setting such as the ICU. Hence, it’s limited application clinically. • Optimal insulin infusions mimic the injection solutions which have been hand optimized for care over the prior 50+ years
Summary & Conclusions • A steady state optimal infusion solution is developed for a physiologically verified 3 compartment model of the glucose regulatory system • Solution is shown to provide the desired ~flat glucose response to steady, slow inputs as well as more significant challenges • Optimal solution does require knowledge of the glucose absorption function P(t) which is unlikely to be known outside of a controlled setting such as the ICU. Hence, it’s limited application clinically. • Optimal insulin infusions mimic the injection solutions which have been hand optimized for care over the prior 50+ years
 Acknowledgements… Lipids and Diabetes Research Group
Acknowledgements… Lipids and Diabetes Research Group
 Questions, Comments, “Complements”, …. “Failure is not an option (but it is much more interesting). ” -- G. Shaw, MD “No, no… (explicit adjective(s))” -- G. Chase, Ph. D
Questions, Comments, “Complements”, …. “Failure is not an option (but it is much more interesting). ” -- G. Shaw, MD “No, no… (explicit adjective(s))” -- G. Chase, Ph. D


