0ea751475adb48937765fc924ea28892.ppt
- Количество слайдов: 51
State Research Center of Virology and Biotechnology “VECTOR” Institute of Molecular Biology Department of Molecular Virology INTERNATIONAL COLLABORATION IN STUDY OF THE FLAVIVIRUSES V. B. Loktev Lescar et al, Cell, 2001
Family: Flaviviridae Genus: Prototype virus Flavivirus Yellow fever virus Flavivirus genus contains approximately 72 viruses Pestivirus Bovine diarrhea virus Hepacivirus Hepatitis C virus
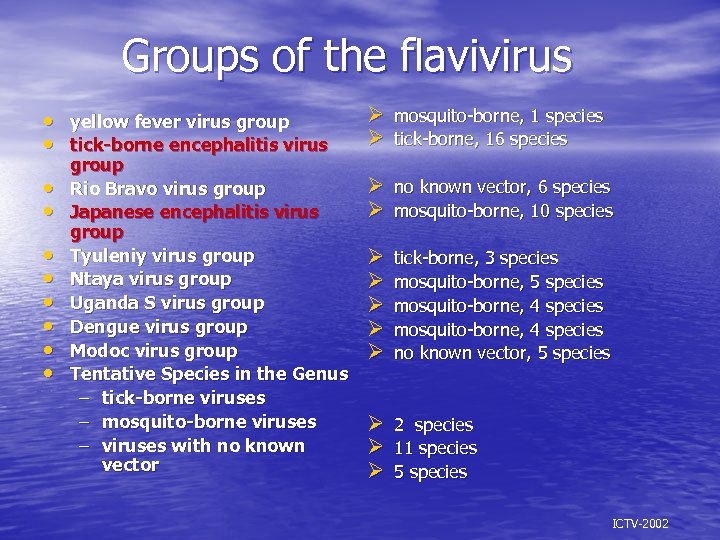
Groups of the flavivirus • • • yellow fever virus group tick-borne encephalitis virus group Rio Bravo virus group Japanese encephalitis virus group Tyuleniy virus group Ntaya virus group Uganda S virus group Dengue virus group Modoc virus group Tentative Species in the Genus – tick-borne viruses – mosquito-borne viruses – viruses with no known vector Ø mosquito-borne, 1 species Ø tick-borne, 16 species Ø no known vector, 6 species Ø mosquito-borne, 10 species Ø Ø Ø tick-borne, 3 species mosquito-borne, 5 species mosquito-borne, 4 species no known vector, 5 species Ø 2 species Ø 11 species Ø 5 species ICTV-2002
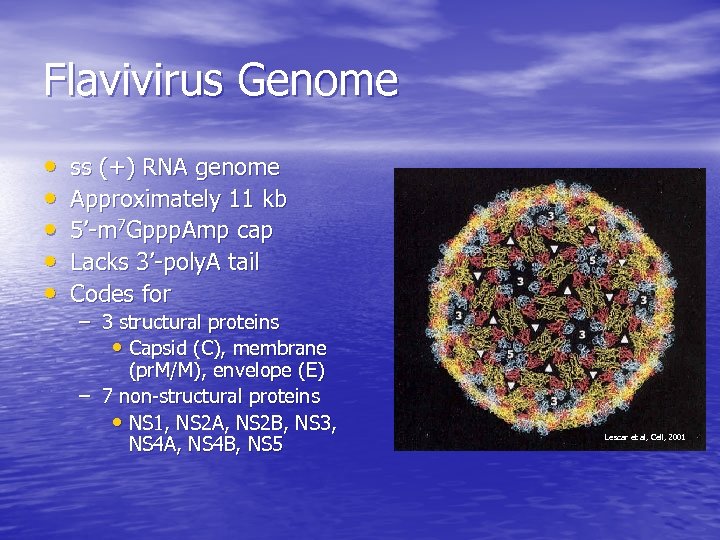
Flavivirus Genome • • • ss (+) RNA genome Approximately 11 kb 5’-m 7 Gppp. Amp cap Lacks 3’-poly. A tail Codes for – 3 structural proteins • Capsid (C), membrane (pr. M/M), envelope (E) – 7 non-structural proteins • NS 1, NS 2 A, NS 2 B, NS 3, NS 4 A, NS 4 B, NS 5 Lescar et al, Cell, 2001
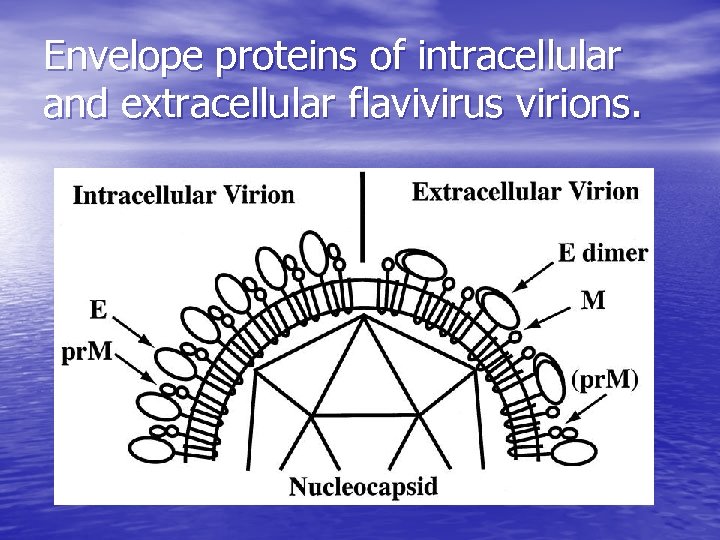
Envelope proteins of intracellular and extracellular flavivirus virions.
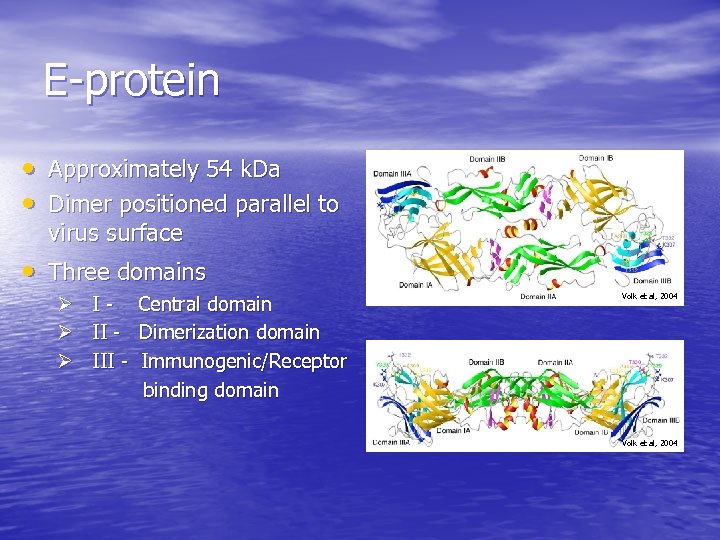
E-protein • Approximately 54 k. Da • Dimer positioned parallel to virus surface • Three domains Ø I - Central domain Ø II - Dimerization domain Ø III - Immunogenic/Receptor binding domain Volk et al, 2004
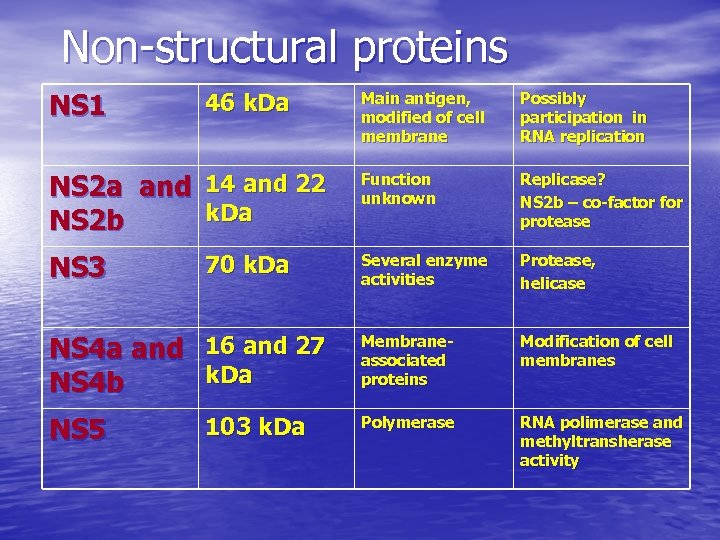
Non-structural proteins NS 1 46 k. Da Main antigen, modified of cell membrane Possibly participation in RNA replication NS 2 a and 14 and 22 k. Da NS 2 b Function unknown Replicase? NS 2 b – co-factor for protease NS 3 Several enzyme activities Protease, helicase NS 4 a and 16 and 27 k. Da NS 4 b Membraneassociated proteins Modification of cell membranes NS 5 Polymerase RNA polimerase and methyltransherase activity 70 k. Da 103 k. Da
Major Flavivirus Diseases • Dengue • Japanese encephalitis • Tick-borne encephalitis • West Nile • Yellow fever
Current Flavivirus Vaccines Live attenuated/weakened • Yellow fever • Japanese encephalitis Inactivated/killed • Japanese encephalitis • Tick-borne encephalitis No vaccines • Dengue • West Nile
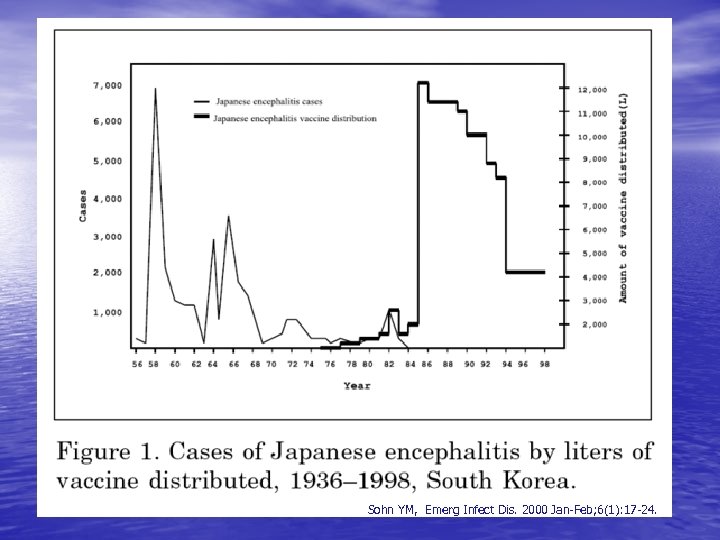
Sohn YM, Emerg Infect Dis. 2000 Jan-Feb; 6(1): 17 -24.
West Nile Virus • First isolated in 1937 in Uganda. • First recorded epidemic in Israel in 1950’s. • Found in Africa, Europe and Asia. • Introduced into Western hemisphere during 1999 in New York.
Family: Flaviviridae Genus: Flavivirus Japanese encephalitis virus group • Alfuy virus • Japanese encephalitis virus • Kokobera virus • Koutango virus • Kunjin virus • Murray Valley encephalitis virus • St. Louis encephalitis virus • Stratford virus • Usutu virus • West Nile virus ICTV-2002
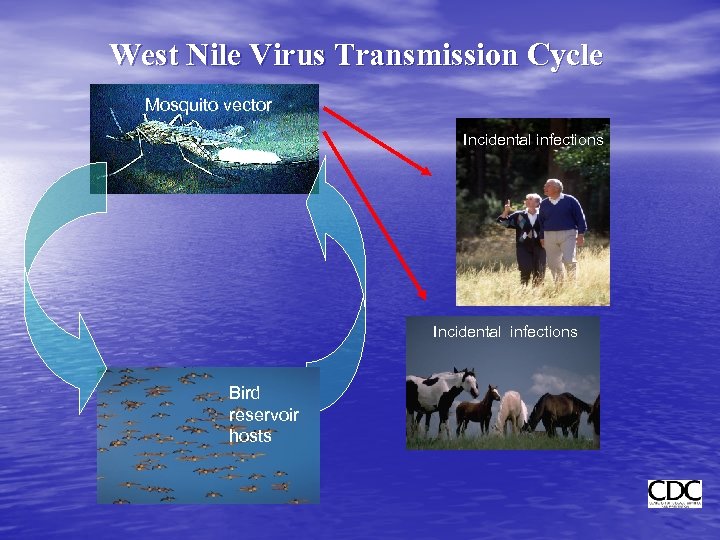
West Nile Virus Transmission Cycle Mosquito vector Incidental infections Bird reservoir hosts
Animal hosts: • Bird • Horse • Human • Hamster • Mouse ВЗН обнаружен в более чем в 115 различных видах организмов !!!
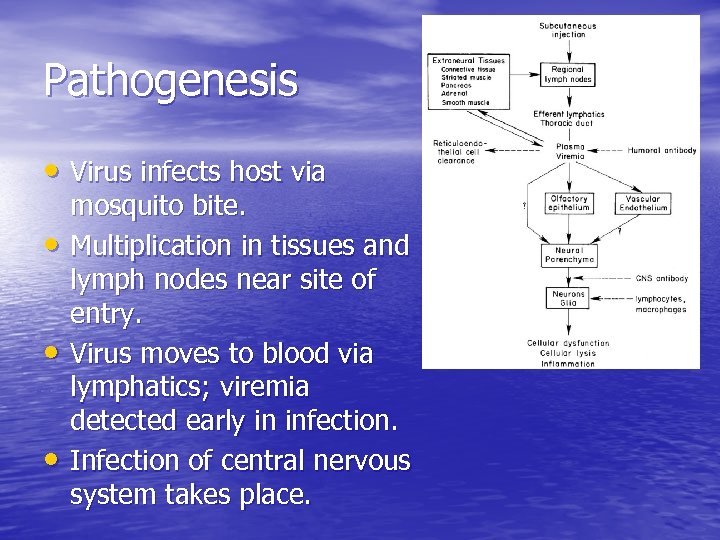
Pathogenesis • Virus infects host via • • • mosquito bite. Multiplication in tissues and lymph nodes near site of entry. Virus moves to blood via lymphatics; viremia detected early in infection. Infection of central nervous system takes place.
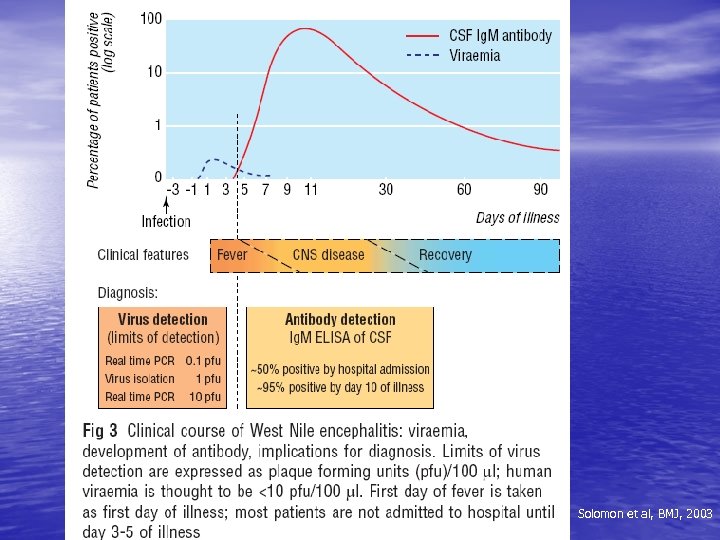
Solomon et al, BMJ, 2003
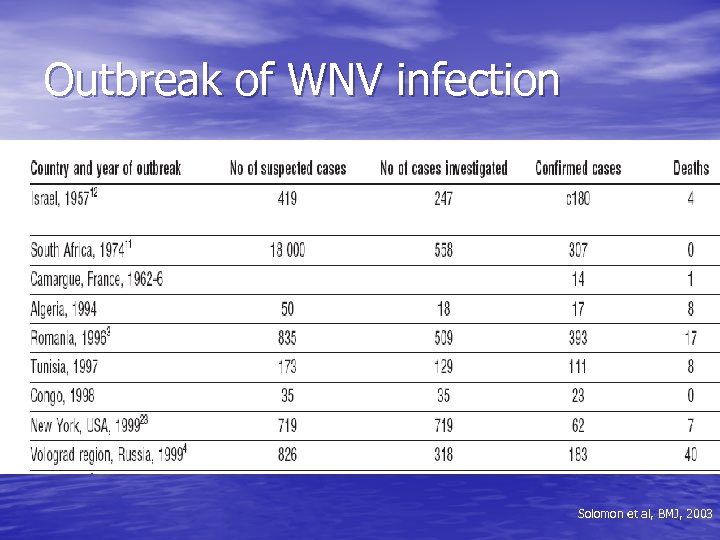
Outbreak of WNV infection Solomon et al, BMJ, 2003
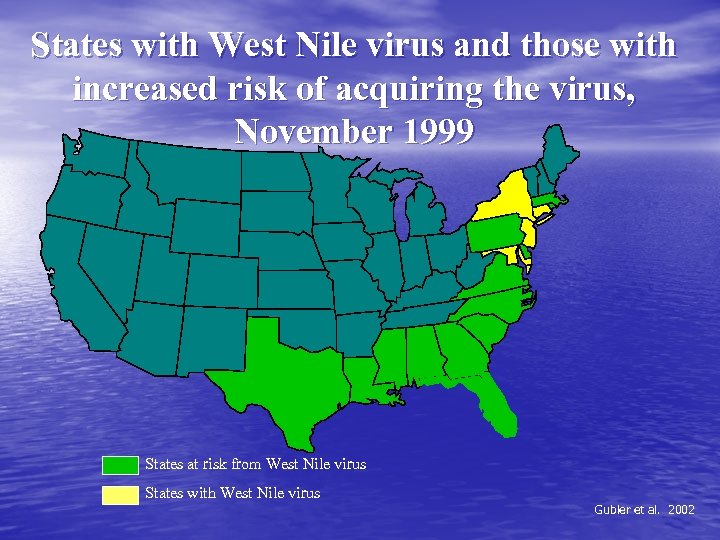
States with West Nile virus and those with increased risk of acquiring the virus, November 1999 States at risk from West Nile virus States with West Nile virus Gubler et al. 2002
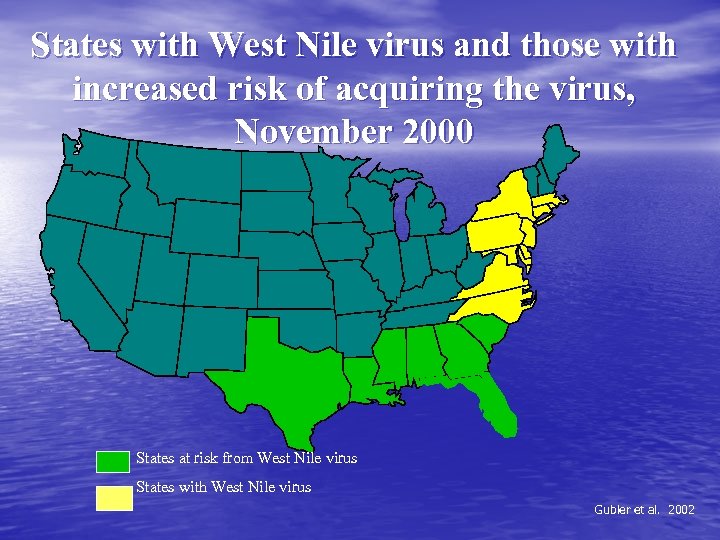
States with West Nile virus and those with increased risk of acquiring the virus, November 2000 States at risk from West Nile virus States with West Nile virus Gubler et al. 2002
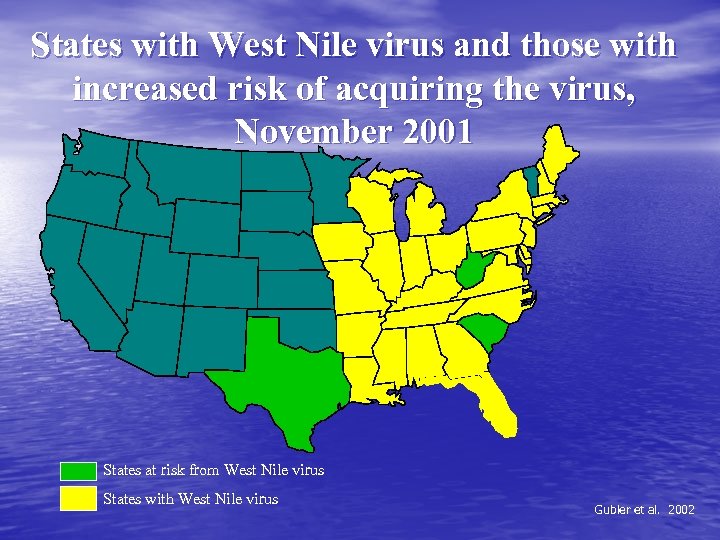
States with West Nile virus and those with increased risk of acquiring the virus, November 2001 States at risk from West Nile virus States with West Nile virus Gubler et al. 2002
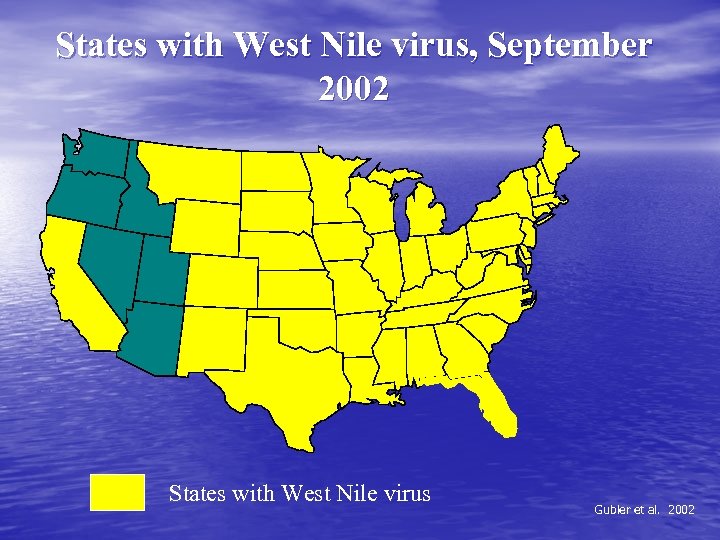
States with West Nile virus, September 2002 States with West Nile virus Gubler et al. 2002
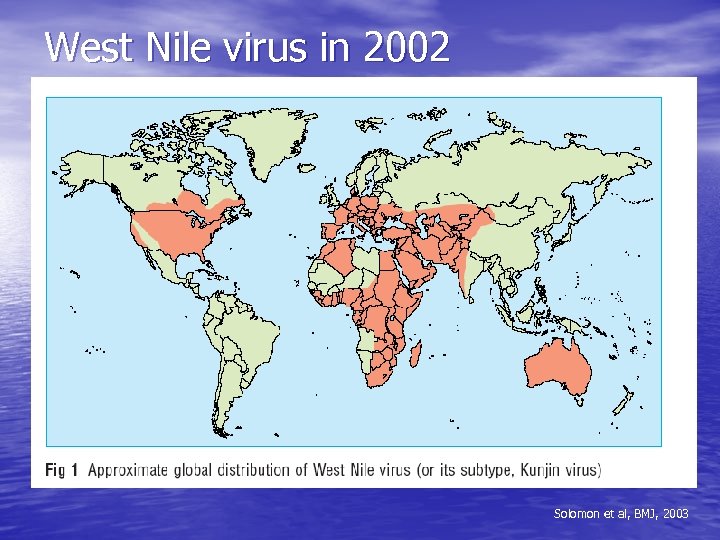
West Nile virus in 2002 Solomon et al, BMJ, 2003
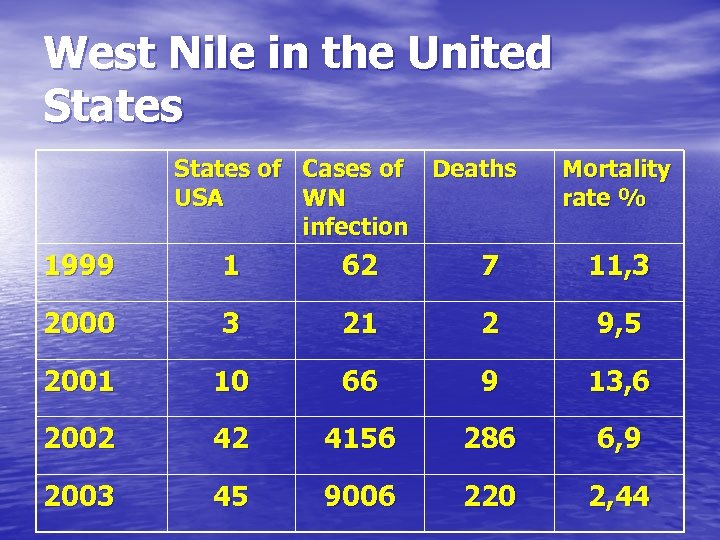
West Nile in the United States of Cases of Deaths USA WN infection Mortality rate % 1999 1 62 7 11, 3 2000 3 21 2 9, 5 2001 10 66 9 13, 6 2002 42 4156 286 6, 9 2003 45 9006 220 2, 44
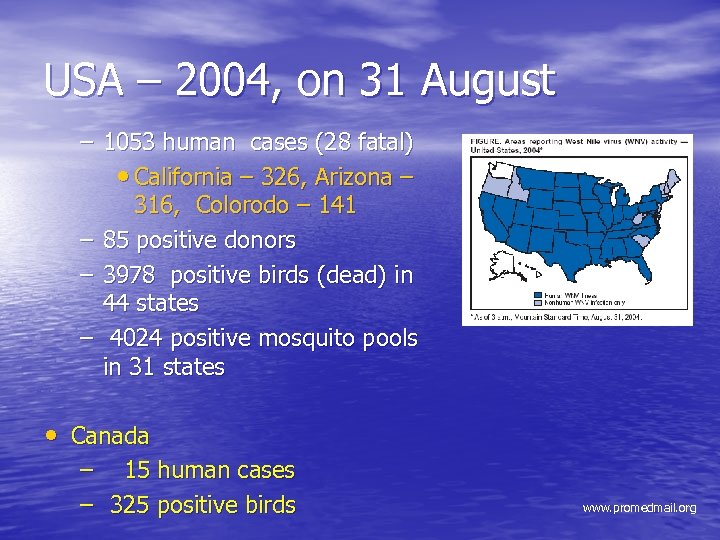
USA – 2004, on 31 August – 1053 human cases (28 fatal) • California – 326, Arizona – 316, Colorodo – 141 – 85 positive donors – 3978 positive birds (dead) in 44 states – 4024 positive mosquito pools in 31 states • Canada – 15 human cases – 325 positive birds www. promedmail. org
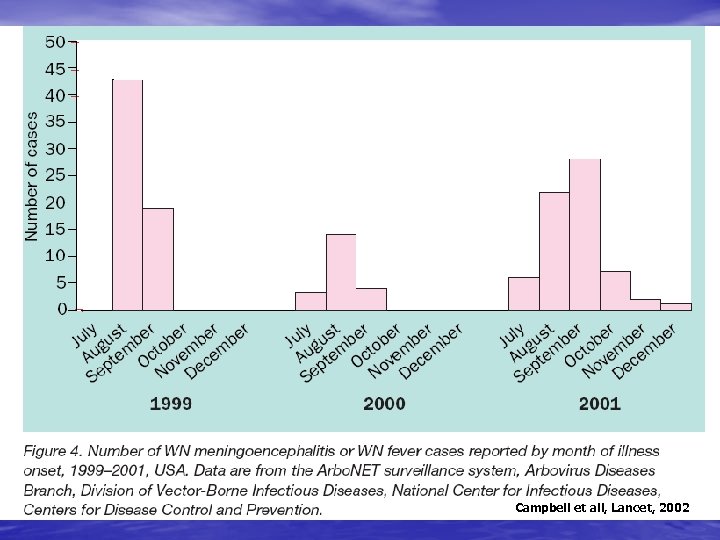
Campbell et all, Lancet, 2002
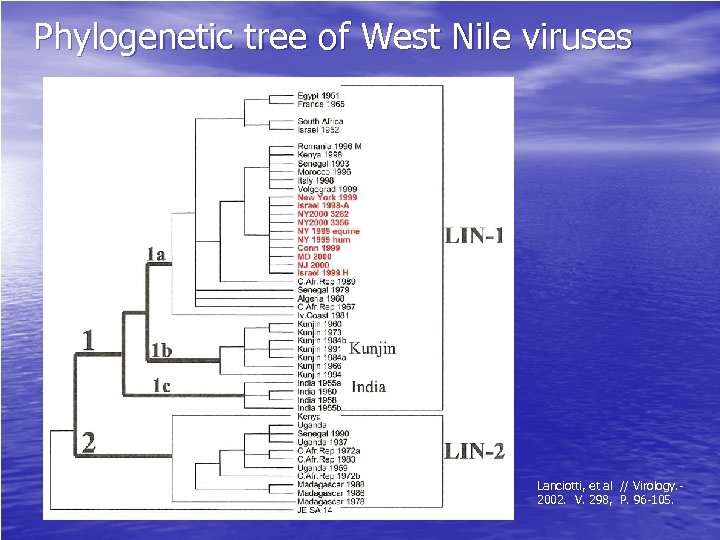
Phylogenetic tree of West Nile viruses Lanciotti, et al // Virology. - 2002. V. 298, P. 96 -105.
New moments in epidemiology of the WN infection • Blood transfusion (737 donors on 25. 11. 2003) • Organs transplantation • Breast-feeding • Stem cells transplantation • Laboratory incidents • Transplacental pathway
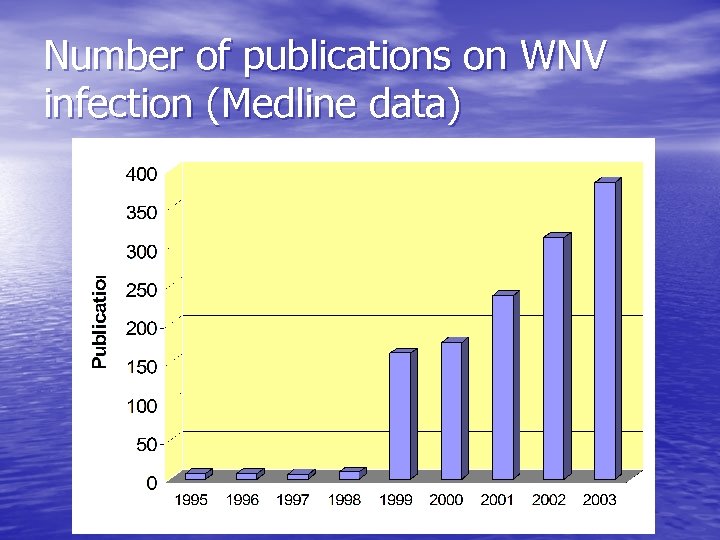
Number of publications on WNV infection (Medline data)
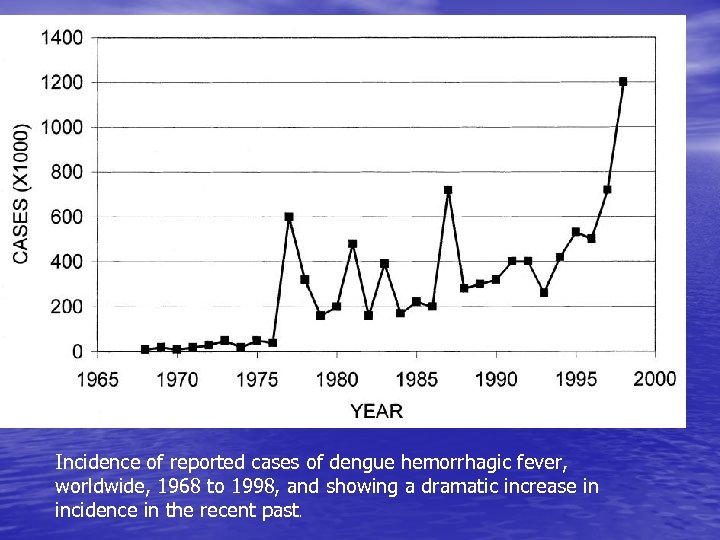
Incidence of reported cases of dengue hemorrhagic fever, worldwide, 1968 to 1998, and showing a dramatic increase in incidence in the recent past.
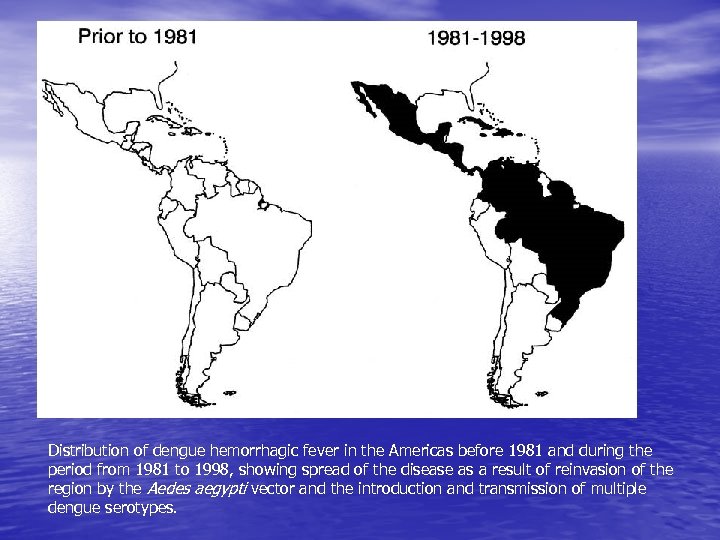
Distribution of dengue hemorrhagic fever in the Americas before 1981 and during the period from 1981 to 1998, showing spread of the disease as a result of reinvasion of the region by the Aedes aegypti vector and the introduction and transmission of multiple dengue serotypes.

West Nile in the Russia, outbreak of WN infection in 1999 380 confirmed cases including 38 fatalities Volgograd Astrakhan 95 confirmed cases including 5 fatalities
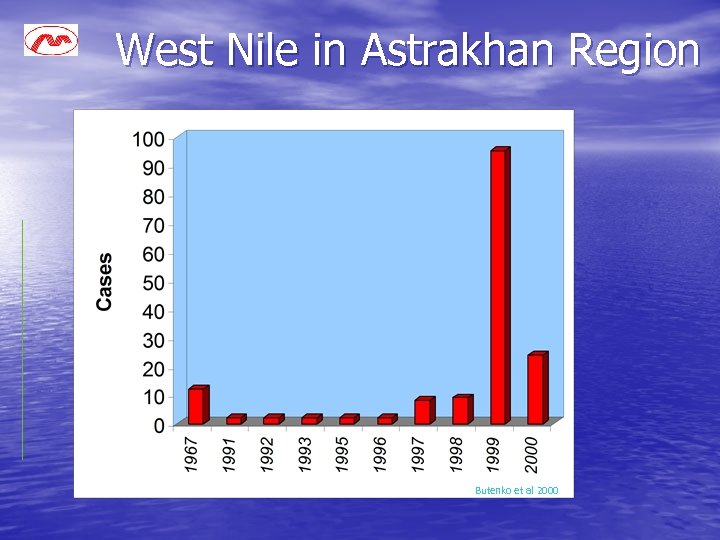
West Nile in Astrakhan Region Butenko et al 2000
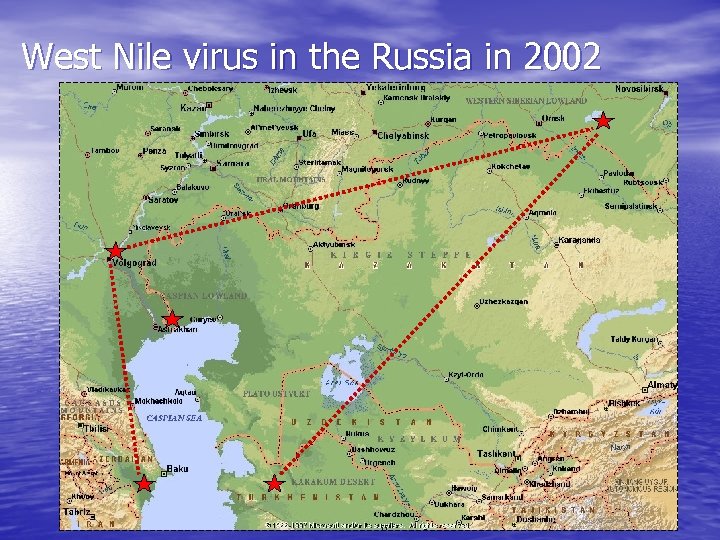
West Nile virus in the Russia in 2002

West Nile virus in 2003 2300 km 4000 km
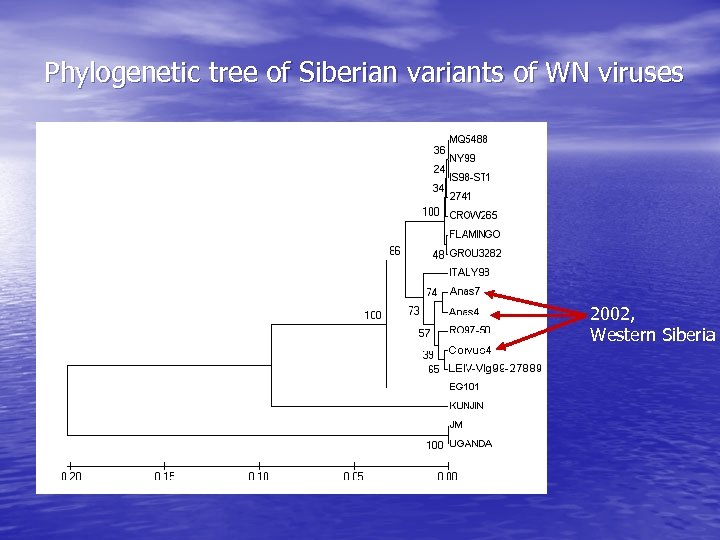
Phylogenetic tree of Siberian variants of WN viruses 2002, Western Siberia
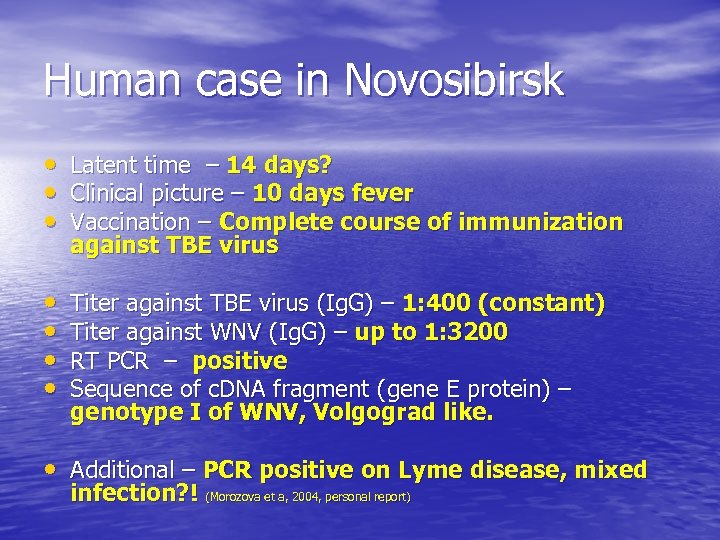
Human case in Novosibirsk • Latent time – 14 days? • Clinical picture – 10 days fever • Vaccination – Complete course of immunization against TBE virus • • Titer against TBE virus (Ig. G) – 1: 400 (constant) Titer against WNV (Ig. G) – up to 1: 3200 RT PCR – positive Sequence of c. DNA fragment (gene E protein) – genotype I of WNV, Volgograd like. • Additional – PCR positive on Lyme disease, mixed infection? ! (Morozova et a, 2004, personal report)
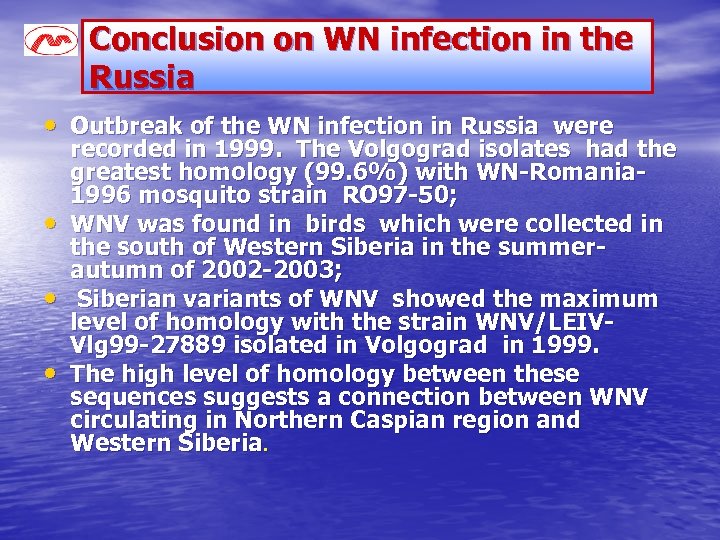
Conclusion on WN infection in the Russia • Outbreak of the WN infection in Russia were • • • recorded in 1999. The Volgograd isolates had the greatest homology (99. 6%) with WN-Romania 1996 mosquito strain RO 97 -50; WNV was found in birds which were collected in the south of Western Siberia in the summerautumn of 2002 -2003; Siberian variants of WNV showed the maximum level of homology with the strain WNV/LEIVVlg 99 -27889 isolated in Volgograd in 1999. The high level of homology between these sequences suggests a connection between WNV circulating in Northern Caspian region and Western Siberia.
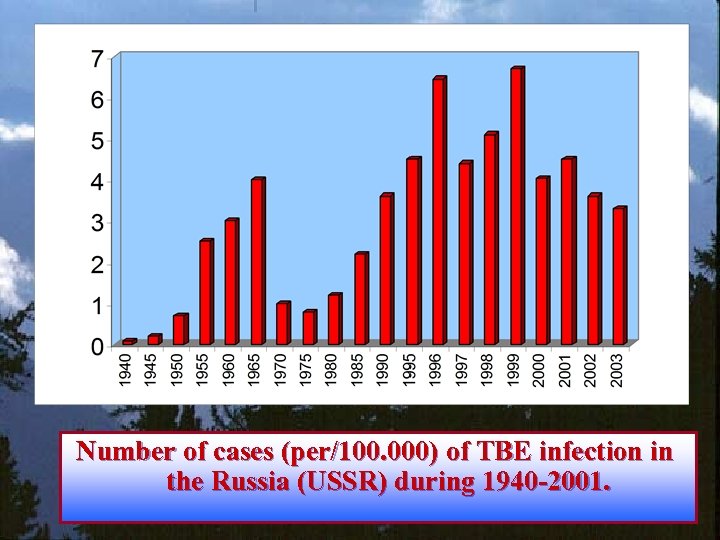
Number of cases (per/100. 000) of TBE infection in the Russia (USSR) during 1940 -2001.
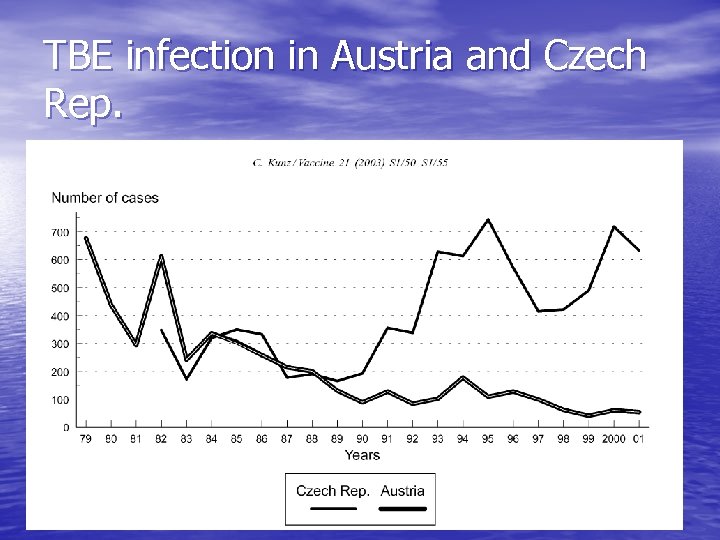
TBE infection in Austria and Czech Rep.
New Variants of Tick-Borne Encephalitis Virus Discovered by Retrospective Investigation of Fatal Cases of Tick-Borne Encephalitis with Hemorrhagic Syndrome Occurred in Novosibirsk Region (Russia) During Summer of 1999
Background: In 1999, 447 TBE cases confirmed by enzyme immunoassay were reported in Novosibirsk region. The mortality rate was 2. 0%. The fatal outcomes of eight patients were associated with development of a pronounced hemorrhagic syndrome. Archival samples of formalin-fixed brain tissue from the fatal cases were collected only in March 2000. Previously they were stored for 8 9 months in 10% formaldehyde solution at room temperature
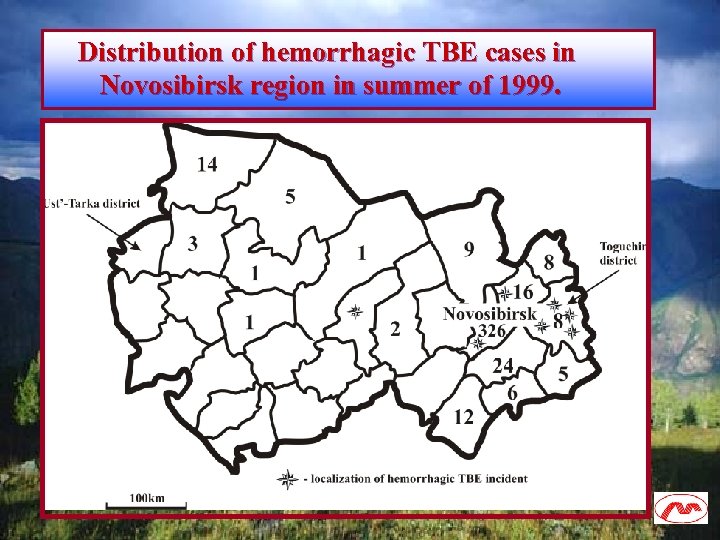
Distribution of hemorrhagic TBE cases in Novosibirsk region in summer of 1999.
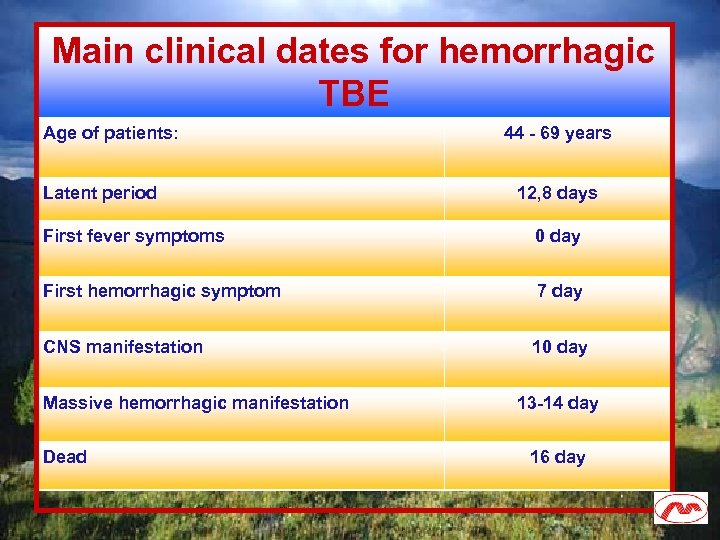
Main clinical dates for hemorrhagic TBE Age of patients: Latent period 44 - 69 years 12, 8 days First fever symptoms 0 day First hemorrhagic symptom 7 day CNS manifestation 10 day Massive hemorrhagic manifestation Dead 13 -14 day 16 day
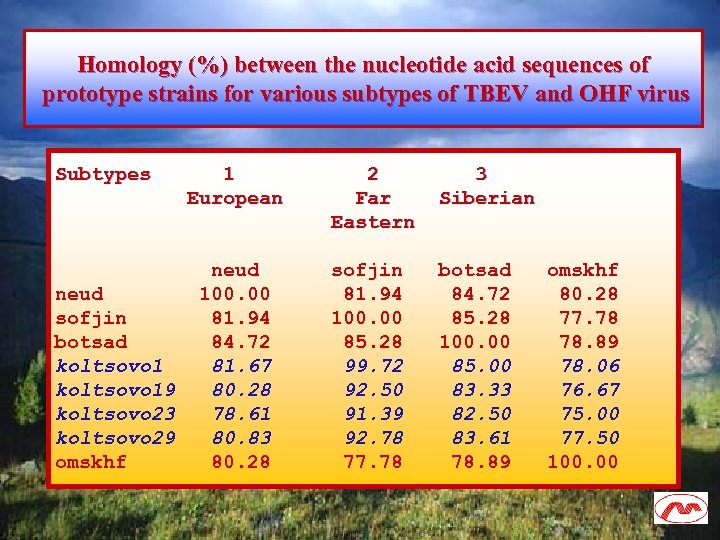
Homology (%) between the nucleotide acid sequences of prototype strains for various subtypes of TBEV and OHF virus Subtypes 1 2 3 European Far Siberian Eastern neud sofjin botsad omskhf neud 100. 00 81. 94 84. 72 80. 28 sofjin 81. 94 100. 00 85. 28 77. 78 botsad 84. 72 85. 28 100. 00 78. 89 koltsovo 1 81. 67 99. 72 85. 00 78. 06 koltsovo 19 80. 28 92. 50 83. 33 76. 67 koltsovo 23 78. 61 91. 39 82. 50 75. 00 koltsovo 29 80. 83 92. 78 83. 61 77. 50 omskhf 80. 28 77. 78 78. 89 100. 00
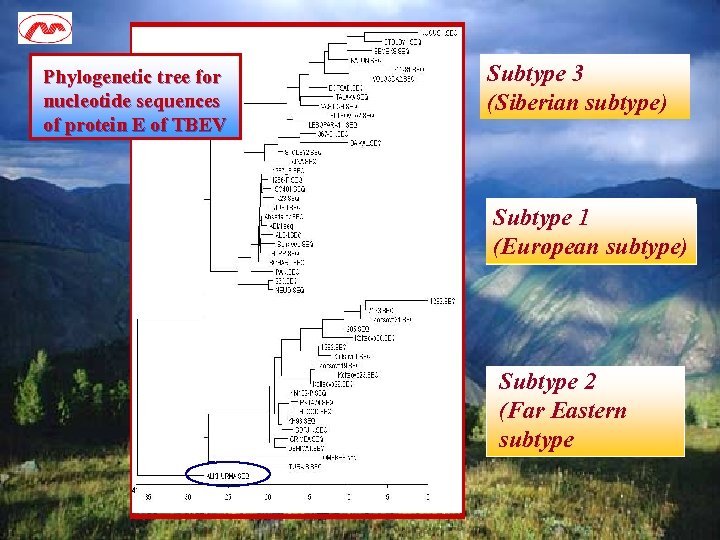
Phylogenetic tree for nucleotide sequences of protein E of TBEV Subtype 3 (Siberian subtype) Subtype 1 (European subtype) Subtype 2 (Far Eastern subtype
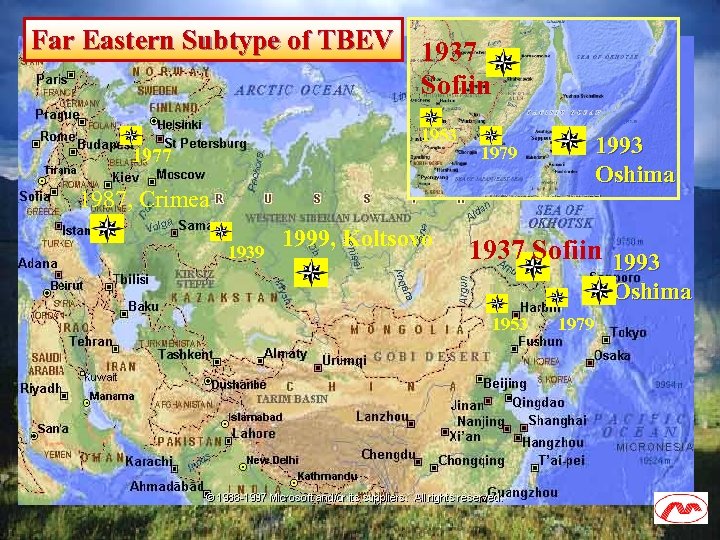
Far Eastern Subtype of TBEV 1937 Sofiin 1953 1977 1993 Oshima 1979 1987, Crimea 1939 1999, Koltsovo 1937 Sofiin 1993 Oshima 1953 1979
Conclusion on hemorrhagic TBEV: Analysis of nucleotide sequences of these fragments showed that homology with subtype 3 (Siberian subtype) of TBEV was approximately 82%. The new variants cluster together with subtype 2 (Far Eastern subtype) of TBEV (homology, 94. 7%) in phylogenetic analysis. Thirteen new amino acid mutations in domain II of protein E were mapped. We conclude that new and unusual variants of TBEV have recently emerged in Novosibirsk region. These variants appear to be capable of inducing a hemorrhagic syndrome in the infected humans.
Summary: • Emerging of new variants of flaviviruses is new threat for the human and public health. • Modern variants of flaviviruses are distributed in most countries of world. • The flaviviruses is hot problem of modern virology.
• SRC VB «Vector» – – – – V. A. Ternovoi A. M. Shestopalov E. V. Protopopova S. I. Zolotykh Yu. V. Kononova S. V. Netesov V. B. Loktev • Novosibirsk State Medical Academy – G. P. Kurzhukov • 1 st Municipal Clinical Infectious Hospital of Novosibirsk – G. Y. Ivanov – Y. V. Sokolov • D. I. Ivanovsky Institute of Virology, Russian Academy of Medical Sciences, Moscow – M. Yu. Shchelkanov – V. A. Aristova – V. L. Gromashevsky, – D. K. L’vov • University of North Carolina, USA – R. W. Ryder • Stanford University, USA – A. V. Loktev • Institute of Systematic and Ecology of Animal, SB RAS, Novosibirsk – A. V. Druzyaka
• Institute of Epidemiology and Microbiology, SB RAMS, Irkutsk – M. A. Khasnatinov • National Center for Infectious Diseases, Ulan-Bator, Mongolia – D. Abmid • National Center for Natural Foci Infectious Diseases, Ulan-Bator, Mongolia – D. Tserennorov – D. Batjav – D. Otgonbaatar • JSC “Vector-Best”, Novosibirsk – M. P. Grishaev • Research Institute of Epidemiology and Microbiology, SB RAMS, Vladivostok – G. N. Leonova • Khasan Natural Park, Primorye Region – E. V. Radiulov

Many thanks for your attention !
0ea751475adb48937765fc924ea28892.ppt