d441f4f330afae00775a89fd2da39508.ppt
- Количество слайдов: 13
 Standardized Pediatric Vancomycin Dosing and Influence on Target Concentrations Jenny L Boucher, Tibisay Villalobos-Fry, Lauren Maurer and Kristin Held. Children’s Hospital at Lehigh Valley Health Network Allentown, Pennsylvania.
Standardized Pediatric Vancomycin Dosing and Influence on Target Concentrations Jenny L Boucher, Tibisay Villalobos-Fry, Lauren Maurer and Kristin Held. Children’s Hospital at Lehigh Valley Health Network Allentown, Pennsylvania.
 Background n n Vancomycin is the antibiotic of choice for invasive MRSA infections. Higher target vancomycin trough concentrations are recommended for adults and this recommendations has been extrapolated to pediatrics though limited data is available for the pediatric population. A few published articles suggest that larger than traditional doses will be required to achieve higher concentrations. IDSA recommends an initial dose of 15 mg/Kg/dose every 6 h in order to reach trough concentration of 15 -20 mg/dl in pediatric patients but recent pediatric literature suggest higher doses are needed achieve that target.
Background n n Vancomycin is the antibiotic of choice for invasive MRSA infections. Higher target vancomycin trough concentrations are recommended for adults and this recommendations has been extrapolated to pediatrics though limited data is available for the pediatric population. A few published articles suggest that larger than traditional doses will be required to achieve higher concentrations. IDSA recommends an initial dose of 15 mg/Kg/dose every 6 h in order to reach trough concentration of 15 -20 mg/dl in pediatric patients but recent pediatric literature suggest higher doses are needed achieve that target.
 Background n In a retrospective evaluation performed at Lehigh Valley Hospital in 2011, a database was collected to look at baseline dosing and trough targets success rates. Data was collected and separated based on patient age and dose of Vancomycin: n Age groups: Infant (2 -23 months) Young child (2 -23 months) Child (6 -12 years) Adolescent (13 -17 years) n Dosing groups: < 45 mg/Kg/day 45 -54 mg/Kg/day 55 -64 mg/Kg/day 65 -74 mg/Kg/day >75 mg/Kg/day n The primary objective was to determine the number of patients to achieve a target trough concentration of 10 to 20 mg/L, with a secondary objective of the number of patients to achieve a target trough of 15 to 20 mg/L.
Background n In a retrospective evaluation performed at Lehigh Valley Hospital in 2011, a database was collected to look at baseline dosing and trough targets success rates. Data was collected and separated based on patient age and dose of Vancomycin: n Age groups: Infant (2 -23 months) Young child (2 -23 months) Child (6 -12 years) Adolescent (13 -17 years) n Dosing groups: < 45 mg/Kg/day 45 -54 mg/Kg/day 55 -64 mg/Kg/day 65 -74 mg/Kg/day >75 mg/Kg/day n The primary objective was to determine the number of patients to achieve a target trough concentration of 10 to 20 mg/L, with a secondary objective of the number of patients to achieve a target trough of 15 to 20 mg/L.
 Background n One hundred and two patients charts (102) were included in the analysis with a mean age of 6. 2 years (range 6 months-17 years). n There were 159 appropriately drawn troughs included in the evaluation: 46 (28. 9 %) were within 10 -20 mg/L and 11 (6. 9%) were within the 15 -20 mg/L.
Background n One hundred and two patients charts (102) were included in the analysis with a mean age of 6. 2 years (range 6 months-17 years). n There were 159 appropriately drawn troughs included in the evaluation: 46 (28. 9 %) were within 10 -20 mg/L and 11 (6. 9%) were within the 15 -20 mg/L.
 Vancomycin levels by age n Trough 10 -20 mg/L 2 -23 months 2 -5 years 6 -12 years 13 -17 years 24. 1% 21. 7% 33. 3% 45. 5% n Trough 15 -20 mg/L 0 3. 3 % 8. 3 % 22. 7 %
Vancomycin levels by age n Trough 10 -20 mg/L 2 -23 months 2 -5 years 6 -12 years 13 -17 years 24. 1% 21. 7% 33. 3% 45. 5% n Trough 15 -20 mg/L 0 3. 3 % 8. 3 % 22. 7 %
 Vancomycin dosing groups and levels 10 -20 mg/L (%) <45 mg/kg/day 45 -54 mg/kg/day 55 -64 mg/kg/day 65 -74 mg/kg/day >75 mg/kg/day 20 10. 5 31. 7 38. 1 63. 6 15 -20 mg/L (%) 11. 1 0 4. 8 18. 2
Vancomycin dosing groups and levels 10 -20 mg/L (%) <45 mg/kg/day 45 -54 mg/kg/day 55 -64 mg/kg/day 65 -74 mg/kg/day >75 mg/kg/day 20 10. 5 31. 7 38. 1 63. 6 15 -20 mg/L (%) 11. 1 0 4. 8 18. 2
 Methods: n Standard dosing of vancomycin for all pediatric patients between 2 months and 17 years with normal renal function. Dosing options are built into CPOE and can be accessed by house staff and providers with prescribing privileges n Patients must have at least one appropriately drawn trough concentration to be included in the study. Orders for levels are automatically place by pharmacy at initiation of therapy and scheduled within one hour of the next scheduled dose at steady state.
Methods: n Standard dosing of vancomycin for all pediatric patients between 2 months and 17 years with normal renal function. Dosing options are built into CPOE and can be accessed by house staff and providers with prescribing privileges n Patients must have at least one appropriately drawn trough concentration to be included in the study. Orders for levels are automatically place by pharmacy at initiation of therapy and scheduled within one hour of the next scheduled dose at steady state.
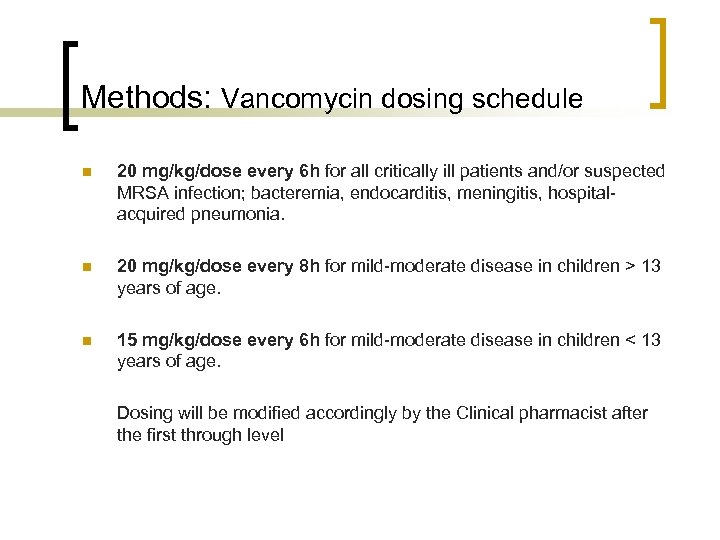 Methods: Vancomycin dosing schedule n 20 mg/kg/dose every 6 h for all critically ill patients and/or suspected MRSA infection; bacteremia, endocarditis, meningitis, hospitalacquired pneumonia. n 20 mg/kg/dose every 8 h for mild-moderate disease in children > 13 years of age. n 15 mg/kg/dose every 6 h for mild-moderate disease in children < 13 years of age. Dosing will be modified accordingly by the Clinical pharmacist after the first through level
Methods: Vancomycin dosing schedule n 20 mg/kg/dose every 6 h for all critically ill patients and/or suspected MRSA infection; bacteremia, endocarditis, meningitis, hospitalacquired pneumonia. n 20 mg/kg/dose every 8 h for mild-moderate disease in children > 13 years of age. n 15 mg/kg/dose every 6 h for mild-moderate disease in children < 13 years of age. Dosing will be modified accordingly by the Clinical pharmacist after the first through level
 Methods: n The database will include: patient demographics, underlying medical condition; vancomycin dose, interval, number of doses administered before trough draw, date and time; concomitant nephrotoxic drugs, baseline and maximum serum creatinine. n Data will be separated based on patient age and daily dose of vancomycin. n Dosing groups will be tracked as follow: 60 -69 mg/kg/day; 70 -79 mg/kg/day; 80 -89 mg/kg/day; 90 -99 mg/kg/day and > 100 mg/kg/day. n Dosing interval will be tracked every 8 h; every 6 h; every 4 h and continuous infusion. n A logistic regression model will be used to evaluate the overall effect of age, dose and interval on the ability to achieve a trough in the target range of 10 -20 mg/L and 15 -20 mg/L
Methods: n The database will include: patient demographics, underlying medical condition; vancomycin dose, interval, number of doses administered before trough draw, date and time; concomitant nephrotoxic drugs, baseline and maximum serum creatinine. n Data will be separated based on patient age and daily dose of vancomycin. n Dosing groups will be tracked as follow: 60 -69 mg/kg/day; 70 -79 mg/kg/day; 80 -89 mg/kg/day; 90 -99 mg/kg/day and > 100 mg/kg/day. n Dosing interval will be tracked every 8 h; every 6 h; every 4 h and continuous infusion. n A logistic regression model will be used to evaluate the overall effect of age, dose and interval on the ability to achieve a trough in the target range of 10 -20 mg/L and 15 -20 mg/L
 Results n n n With the standardization of initial vancomycin dosing at 60 mg/kg/day we predict an increase in the vancomycin trough levels that successfully reach the 10 -20 mg/L range. We expect to replicate the pattern seen in our prior observation and also what have been published in similar pediatric patients. We expect to be able to use this data to help us make evidence-based recommendations on the adequate dose of vancomycin in our children hospital.
Results n n n With the standardization of initial vancomycin dosing at 60 mg/kg/day we predict an increase in the vancomycin trough levels that successfully reach the 10 -20 mg/L range. We expect to replicate the pattern seen in our prior observation and also what have been published in similar pediatric patients. We expect to be able to use this data to help us make evidence-based recommendations on the adequate dose of vancomycin in our children hospital.
 References n n n n Frymoyer A; Guglielmo BJ; Wilson SD; Scarpace SB; Benet LZ; Hersh AL. Impact of a hospitalwide increase in empiric pediatric vancomycin dosing on initial trough concentrations. Pharmacotherapy. 2011; 31(9): 871 -6. Frymoyer A; Hersh AL; Benet LZ; Guglielmo BJ. Current recommended dosing of vancomycin for children with invasive methicillin-resistant Staphylococcus aureus infections is inadequate. Pediatr Infect Dis J. 2009; 28(5): 398 -402. Eiland LS; English TM; Eiland EH. Assessment of vancomycin dosing and subsequent serum concentrations in pediatric patients. Ann Pharmacother. 2011; 45(5): 582 -9. Broome L; So TY. An evaluation of initial vancomycin dosing in infants, children, and adolescents. Int J Pediatr. 2011; 2011: 470364. Miller M; Miller JL; Hagemann TM; Harrison D; Chavez-Bueno S; Johnson PN. Vancomycin dosage in overweight and obese children. Am J Health Syst Pharm. 2011; 68(21): 2062 -8. Moffett BS; Kim S; Edwards MS. . Vancomycin dosing in obese pediatric patients. Clin Pediatr (Phila). 2011; 50(5): 442 -6. Gordon CL; Thompson C; Carapetis JR; Turnidge J; Kilburn C; Currie BJ. Trough concentrations of vancomycin: adult therapeutic targets are not appropriate for children. Pediatr Infect Dis J. 2012; 31(12): 1269 -71
References n n n n Frymoyer A; Guglielmo BJ; Wilson SD; Scarpace SB; Benet LZ; Hersh AL. Impact of a hospitalwide increase in empiric pediatric vancomycin dosing on initial trough concentrations. Pharmacotherapy. 2011; 31(9): 871 -6. Frymoyer A; Hersh AL; Benet LZ; Guglielmo BJ. Current recommended dosing of vancomycin for children with invasive methicillin-resistant Staphylococcus aureus infections is inadequate. Pediatr Infect Dis J. 2009; 28(5): 398 -402. Eiland LS; English TM; Eiland EH. Assessment of vancomycin dosing and subsequent serum concentrations in pediatric patients. Ann Pharmacother. 2011; 45(5): 582 -9. Broome L; So TY. An evaluation of initial vancomycin dosing in infants, children, and adolescents. Int J Pediatr. 2011; 2011: 470364. Miller M; Miller JL; Hagemann TM; Harrison D; Chavez-Bueno S; Johnson PN. Vancomycin dosage in overweight and obese children. Am J Health Syst Pharm. 2011; 68(21): 2062 -8. Moffett BS; Kim S; Edwards MS. . Vancomycin dosing in obese pediatric patients. Clin Pediatr (Phila). 2011; 50(5): 442 -6. Gordon CL; Thompson C; Carapetis JR; Turnidge J; Kilburn C; Currie BJ. Trough concentrations of vancomycin: adult therapeutic targets are not appropriate for children. Pediatr Infect Dis J. 2012; 31(12): 1269 -71
 References n n n n Liu C; Bayer A; Cosgrove SE; Daum RS; Fridkin SK; Gorwitz RJ; Kaplan SL; Karchmer AW; Levine DP; Murray BE; J Rybak M; Talan DA; Chambers HF; Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011; 52(3): e 18 -55 Mc. Kamy S; Chen T; Lee M; Ambrose PJ. Evaluation of a pediatric continuousinfusion vancomycin therapy guideline. Am J Health Syst Pharm. 2012; 69(23): 2066 -71 Fung L. Continuous infusion vancomycin for treatment of methicillin-resistant Staphylococcus aureus in cystic fibrosis patients. Ann Pharmacother. 2012; 46(10): e 26 Piro CC; Crossno CL; Collier A; Ho R; Koyama T; Frangoul H. Initial vancomycin dosing in pediatric oncology and stem cell transplant patients. J Pediatr Hematol Oncol. 2009; 31(1): 3 -7 Mc. Kamy S; Hernandez E; Jahng M; Moriwaki T; Deveikis A; Le J. Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr. 2011; 158(3): 422 -6 Cies JJ; Shankar V. Nephrotoxicity in patients with vancomycin trough concentrations of 15 -20 μg/ml in a pediatric intensive care unit. Pharmacotherapy. 2013; 33(4): 392 -400 (ISSN: 1875 -9114) Ito H; Shime N; Kosaka T. Pharmacokinetics of glycopeptide antibiotics in children. J Infect Chemother. 2013; 19(2): 352 -5 (ISSN: 1437 -7780)
References n n n n Liu C; Bayer A; Cosgrove SE; Daum RS; Fridkin SK; Gorwitz RJ; Kaplan SL; Karchmer AW; Levine DP; Murray BE; J Rybak M; Talan DA; Chambers HF; Clinical practice guidelines by the infectious diseases society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. 2011; 52(3): e 18 -55 Mc. Kamy S; Chen T; Lee M; Ambrose PJ. Evaluation of a pediatric continuousinfusion vancomycin therapy guideline. Am J Health Syst Pharm. 2012; 69(23): 2066 -71 Fung L. Continuous infusion vancomycin for treatment of methicillin-resistant Staphylococcus aureus in cystic fibrosis patients. Ann Pharmacother. 2012; 46(10): e 26 Piro CC; Crossno CL; Collier A; Ho R; Koyama T; Frangoul H. Initial vancomycin dosing in pediatric oncology and stem cell transplant patients. J Pediatr Hematol Oncol. 2009; 31(1): 3 -7 Mc. Kamy S; Hernandez E; Jahng M; Moriwaki T; Deveikis A; Le J. Incidence and risk factors influencing the development of vancomycin nephrotoxicity in children. J Pediatr. 2011; 158(3): 422 -6 Cies JJ; Shankar V. Nephrotoxicity in patients with vancomycin trough concentrations of 15 -20 μg/ml in a pediatric intensive care unit. Pharmacotherapy. 2013; 33(4): 392 -400 (ISSN: 1875 -9114) Ito H; Shime N; Kosaka T. Pharmacokinetics of glycopeptide antibiotics in children. J Infect Chemother. 2013; 19(2): 352 -5 (ISSN: 1437 -7780)
 Thanks
Thanks


