1fdd2785833d3a8a6f39a1baa4bbde4d.ppt
- Количество слайдов: 39
 STAGING MCR Staff Show Me Healthy Women March 27, 2008 Supported by a Cooperative Agreement between DHSS and the Centers for Disease Control and Prevention (CDC) and a Surveillance Contract between DHSS and MU
STAGING MCR Staff Show Me Healthy Women March 27, 2008 Supported by a Cooperative Agreement between DHSS and the Centers for Disease Control and Prevention (CDC) and a Surveillance Contract between DHSS and MU
 Staging Grouping of cancer cases according to similar degrees of spread or extent of disease. Extent of disease is a detailed description of how far the tumor has spread from organ or site of origin (the primary site).
Staging Grouping of cancer cases according to similar degrees of spread or extent of disease. Extent of disease is a detailed description of how far the tumor has spread from organ or site of origin (the primary site).
 Staging n PURPOSES n Determine appropriate treatment n Predict prognosis n Evaluate results of treatment n Facilitate exchange of information n Contribute to research of human cancer
Staging n PURPOSES n Determine appropriate treatment n Predict prognosis n Evaluate results of treatment n Facilitate exchange of information n Contribute to research of human cancer
 Staging Elements n Elements to be considered in any staging system are the n primary tumor site, n tumor size, n multiplicity (number of tumors), n depth of invasion and extension to regional or distant tissues, n involvement of regional lymph nodes, and n distant metastases.
Staging Elements n Elements to be considered in any staging system are the n primary tumor site, n tumor size, n multiplicity (number of tumors), n depth of invasion and extension to regional or distant tissues, n involvement of regional lymph nodes, and n distant metastases.
 Types of Staging Systems n Summary Staging n American Joint Committee on Cancer (AJCC) Staging System n Collaborative Staging n Others n FIGO (GYN) n Dukes (colorectal) n Ann Arbor ( Lymphoma)
Types of Staging Systems n Summary Staging n American Joint Committee on Cancer (AJCC) Staging System n Collaborative Staging n Others n FIGO (GYN) n Dukes (colorectal) n Ann Arbor ( Lymphoma)
 FIGO n Acronym for the French term that means International Federation for Gynecology and Obstetrics. The American Joint Committee on Cancer has developed the tumor (T) component of the TNM staging system to correspond to FIGO staging.
FIGO n Acronym for the French term that means International Federation for Gynecology and Obstetrics. The American Joint Committee on Cancer has developed the tumor (T) component of the TNM staging system to correspond to FIGO staging.
 How to? n Where did the cancer start? n Where did the cancer go? n How did the cancer get there? n What is the stage?
How to? n Where did the cancer start? n Where did the cancer go? n How did the cancer get there? n What is the stage?
 Staging Sources n Physical Exam n Radiologic Procedures n X-rays n Scans n Endoscopies n Tumor markers n Pathologic exams n Surgical reports n Progress Notes and Discharge Summaries
Staging Sources n Physical Exam n Radiologic Procedures n X-rays n Scans n Endoscopies n Tumor markers n Pathologic exams n Surgical reports n Progress Notes and Discharge Summaries
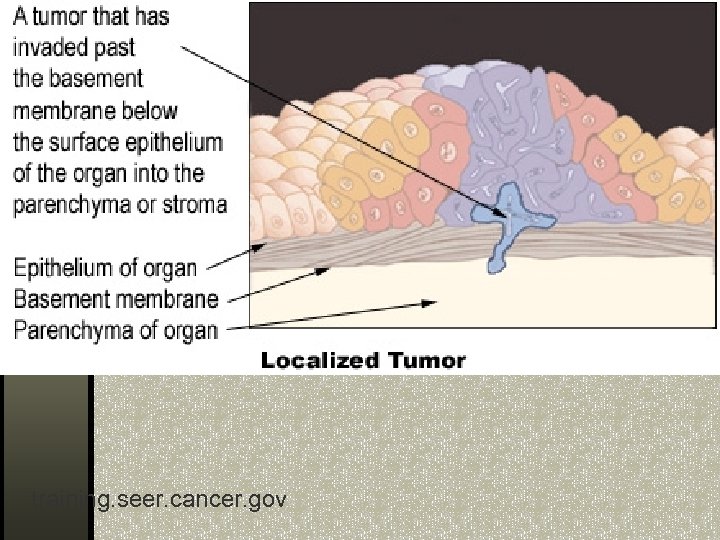
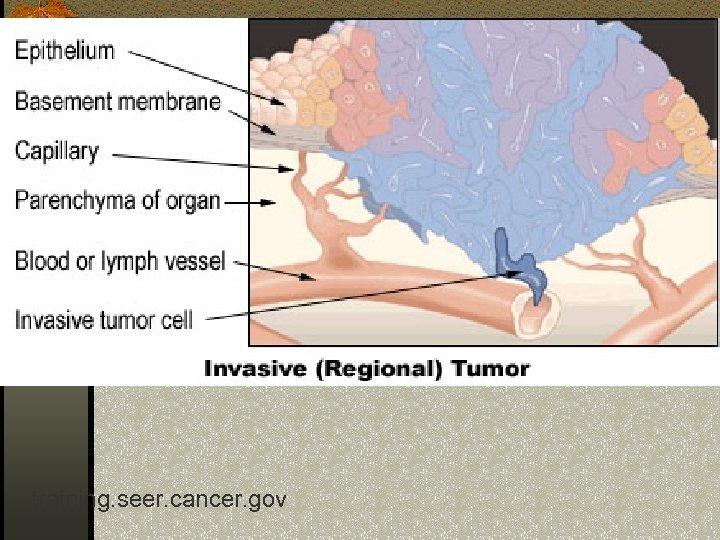
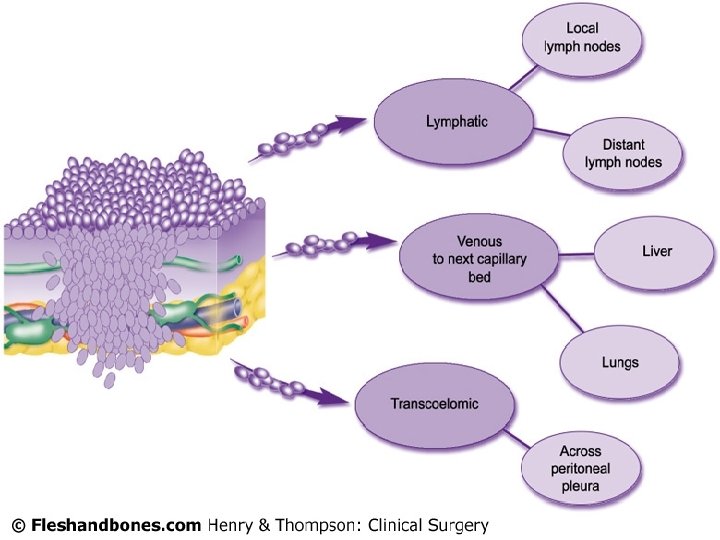
 How Cancer Spreads n Local invasion n Direct extension n Lymphatic metastases n Blood-borne metastases n Intra-cavitary
How Cancer Spreads n Local invasion n Direct extension n Lymphatic metastases n Blood-borne metastases n Intra-cavitary
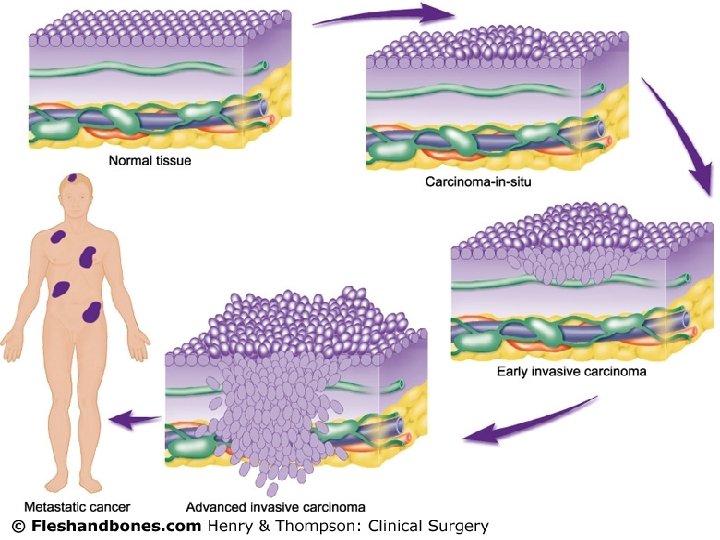
 Summary Staging 0 – in situ 1 – localized 2 – regional by direct extension only 3 – regional lymph nodes involved only 4 – regional by both direct extension and lymph node involvement n 5 – regional, NOS (not otherwise specified) n 7 - distant site(s)/node(s) involved n 9 – unknown (unstaged, unknown or unspecified) n n n
Summary Staging 0 – in situ 1 – localized 2 – regional by direct extension only 3 – regional lymph nodes involved only 4 – regional by both direct extension and lymph node involvement n 5 – regional, NOS (not otherwise specified) n 7 - distant site(s)/node(s) involved n 9 – unknown (unstaged, unknown or unspecified) n n n
 training. seer. cancer. gov
training. seer. cancer. gov
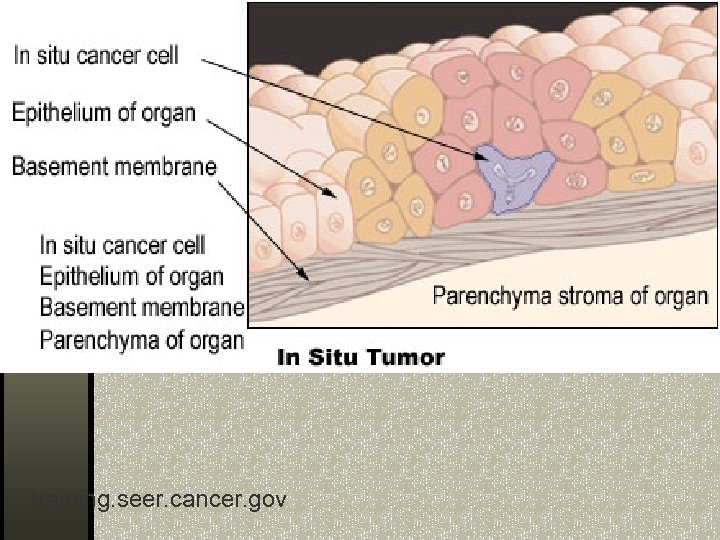
 In Situ Terms n CIN III n Confined to epithelium n Intracystic, non-infiltrating n Intraductal n Intraepidermal n Intra-epithelial n Intrasquamous n Stage 0
In Situ Terms n CIN III n Confined to epithelium n Intracystic, non-infiltrating n Intraductal n Intraepidermal n Intra-epithelial n Intrasquamous n Stage 0
 In Situ Terms n Involvement up to but not including the basement membrane n Lobular neoplasia n Non-infiltrating n Non-invasive n No stromal invasion n Preinvasive
In Situ Terms n Involvement up to but not including the basement membrane n Lobular neoplasia n Non-infiltrating n Non-invasive n No stromal invasion n Preinvasive
 CIN III n CIN III (cervical intraepithelial neoplasia grade iii) must be carefully reviewed, because this diagnosis includes both carcinoma in situ and severe dysplasia.
CIN III n CIN III (cervical intraepithelial neoplasia grade iii) must be carefully reviewed, because this diagnosis includes both carcinoma in situ and severe dysplasia.
 Microinvasion n Microinvasion implies invasion through the basement membrane. The stage would be INVASIVE not insitu. n Any foci of invasion makes the stage invasive rather than insitu.
Microinvasion n Microinvasion implies invasion through the basement membrane. The stage would be INVASIVE not insitu. n Any foci of invasion makes the stage invasive rather than insitu.
 training. seer. cancer. gov
training. seer. cancer. gov
 training. seer. cancer. gov
training. seer. cancer. gov
 Distant n Distant mets can be by: ndirect contiguous extension nimplantation (discontinuous) mets nlymph node involvement
Distant n Distant mets can be by: ndirect contiguous extension nimplantation (discontinuous) mets nlymph node involvement
 Unstageable n Unknown primaries n Not enough information to stage n Death certificate only
Unstageable n Unknown primaries n Not enough information to stage n Death certificate only
 AJCC (TNM) Staging Louanne Currence, RHIT, CTR
AJCC (TNM) Staging Louanne Currence, RHIT, CTR
 What is TNM Staging? n Developed by physicians (AJCC) n Uniform staging system to determine treatment, prognosis & end results n T = Tumor n N = Nodes n M = Metastasis n Group Stage = summary of TNM
What is TNM Staging? n Developed by physicians (AJCC) n Uniform staging system to determine treatment, prognosis & end results n T = Tumor n N = Nodes n M = Metastasis n Group Stage = summary of TNM
 Clinical Staging n Used to select primary treatment n Each site has specific guidelines of what is acceptable under c. TNM Physical exam Radiology Endoscopy Biopsy
Clinical Staging n Used to select primary treatment n Each site has specific guidelines of what is acceptable under c. TNM Physical exam Radiology Endoscopy Biopsy
 Pathologic Staging n Based on pre-treatment evidence and/or subsequent surgery/path n Used to n Determine adjuvant therapy n Estimate prognosis n Report end results
Pathologic Staging n Based on pre-treatment evidence and/or subsequent surgery/path n Used to n Determine adjuvant therapy n Estimate prognosis n Report end results
 T n Primary "Tumor" and its contiguous extension n. Based on size (invasive only) n. Based on penetration n. Extension of primary
T n Primary "Tumor" and its contiguous extension n. Based on size (invasive only) n. Based on penetration n. Extension of primary
 T n T-value increases with worsening scenario n. Tx - cannot assess n. T 0 - no evidence of primary n. Tis - In situ (never sarcomas) n. T 1 -4
T n T-value increases with worsening scenario n. Tx - cannot assess n. T 0 - no evidence of primary n. Tis - In situ (never sarcomas) n. T 1 -4
 Sample "T"s n < 1. 0 cm breast lesion = T 1 n 3. 0 cm LOQ breast lesion = T 2 n Carcinoma confined to uterus = T 1 n Cervical carcinoma extends to pelvic wall = T 3
Sample "T"s n < 1. 0 cm breast lesion = T 1 n 3. 0 cm LOQ breast lesion = T 2 n Carcinoma confined to uterus = T 1 n Cervical carcinoma extends to pelvic wall = T 3
 N n Regional lymph nodes n. Absence or presence of + LN n# of + LNs/size of metastasis n. Laterality of + LNs/size of mets n Named LN chains
N n Regional lymph nodes n. Absence or presence of + LN n# of + LNs/size of metastasis n. Laterality of + LNs/size of mets n Named LN chains
 N n Increases in severity n. Nx - cannot assess n. N 0 - no regional LN mets n. N 1 -3
N n Increases in severity n. Nx - cannot assess n. N 0 - no regional LN mets n. N 1 -3
 Sample "N"s n Breast n Metastasis in axillary LNs fixed or matted = N 2 n 1 of 15 axillary LNs + (breast) = N 1 n Cervix n 1 + pelvic node = N 1
Sample "N"s n Breast n Metastasis in axillary LNs fixed or matted = N 2 n 1 of 15 axillary LNs + (breast) = N 1 n Cervix n 1 + pelvic node = N 1
 M n Some sites have listing n Mx - cannot assess n M 0 - no distant mets n M 1 - distant mets found
M n Some sites have listing n Mx - cannot assess n M 0 - no distant mets n M 1 - distant mets found
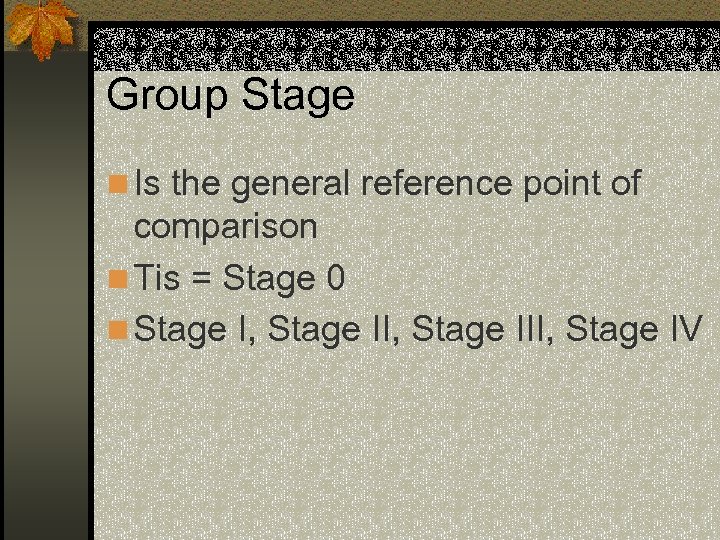 Group Stage n Is the general reference point of comparison n Tis = Stage 0 n Stage I, Stage III, Stage IV
Group Stage n Is the general reference point of comparison n Tis = Stage 0 n Stage I, Stage III, Stage IV
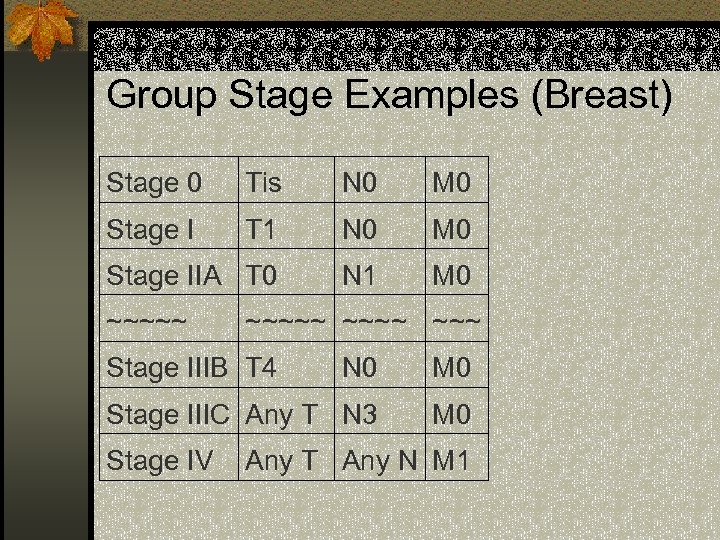 Group Stage Examples (Breast) Stage 0 Tis N 0 M 0 Stage I T 1 N 0 M 0 Stage IIA T 0 N 1 M 0 ~~~~~ Stage IIIB T 4 N 0 M 0 Stage IIIC Any T N 3 M 0 Stage IV Any T Any N M 1
Group Stage Examples (Breast) Stage 0 Tis N 0 M 0 Stage I T 1 N 0 M 0 Stage IIA T 0 N 1 M 0 ~~~~~ Stage IIIB T 4 N 0 M 0 Stage IIIC Any T N 3 M 0 Stage IV Any T Any N M 1
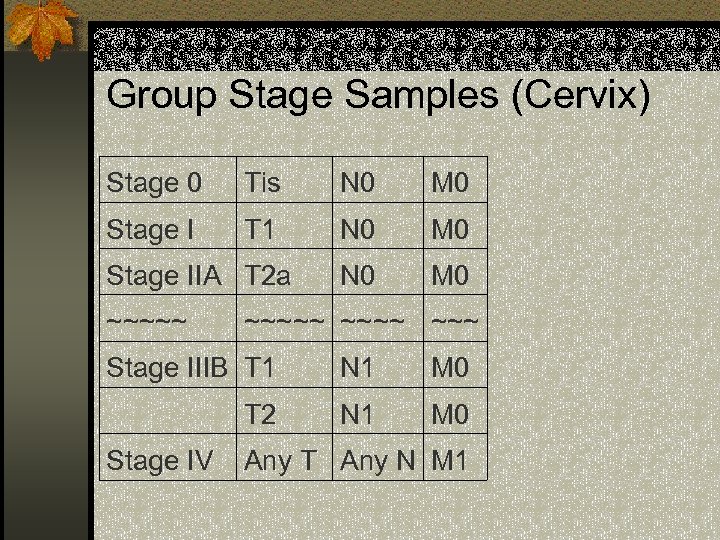 Group Stage Samples (Cervix) Stage 0 Tis N 0 M 0 Stage I T 1 N 0 M 0 Stage IIA T 2 a ~~~~~ Stage IIIB T 1 N 1 M 0 T 2 N 1 M 0 Stage IV Any T Any N M 1
Group Stage Samples (Cervix) Stage 0 Tis N 0 M 0 Stage I T 1 N 0 M 0 Stage IIA T 2 a ~~~~~ Stage IIIB T 1 N 1 M 0 T 2 N 1 M 0 Stage IV Any T Any N M 1
 Collaborative Stage n Collaborative Staging (CS) data items n CS Extension n CS Lymph Nodes n CS Mets at Dx
Collaborative Stage n Collaborative Staging (CS) data items n CS Extension n CS Lymph Nodes n CS Mets at Dx
 Steps for Staging 1) Determine primary site & histology 3) Is histology included? 4) Review list of regional LNs 5) Review rules of classification 6) Find staging information in chart 7) Determine T, N, M and group stage
Steps for Staging 1) Determine primary site & histology 3) Is histology included? 4) Review list of regional LNs 5) Review rules of classification 6) Find staging information in chart 7) Determine T, N, M and group stage
 Exercises
Exercises
 Missouri Cancer Registry Help Line: 800 -392 -2829 n Help interpreting path report for staging http: //mcr. umh. edu n For further information, please contact: Sue Vest, Project Manager, vests@health. missouri. edu Nancy Cole, Assistant Project Manager colen@health. missouri. edu
Missouri Cancer Registry Help Line: 800 -392 -2829 n Help interpreting path report for staging http: //mcr. umh. edu n For further information, please contact: Sue Vest, Project Manager, vests@health. missouri. edu Nancy Cole, Assistant Project Manager colen@health. missouri. edu


