4b3a4af9ade9255aafd87c366b04cb2e.ppt
- Количество слайдов: 27

Stadiazione intraoperatoria dei tumori delle vie biliari Marco Filauro Dipartimento di chirurgia e malattie dell’apparato digerente SC di Chirurgia ( Dir. : M. Filauro) E. O. Ospedali Galliera Genova
Ann Surg. 1979 August; 190(2): 151– 157
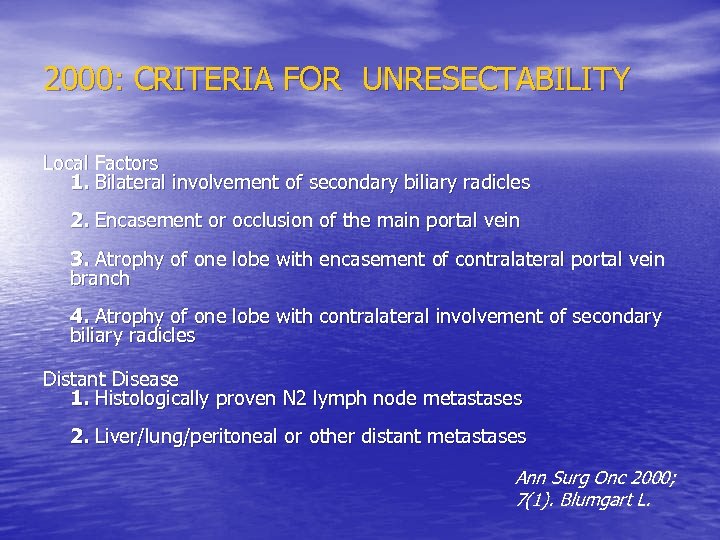
2000: CRITERIA FOR UNRESECTABILITY Local Factors 1. Bilateral involvement of secondary biliary radicles 2. Encasement or occlusion of the main portal vein 3. Atrophy of one lobe with encasement of contralateral portal vein branch 4. Atrophy of one lobe with contralateral involvement of secondary biliary radicles Distant Disease 1. Histologically proven N 2 lymph node metastases 2. Liver/lung/peritoneal or other distant metastases Ann Surg Onc 2000; 7(1). Blumgart L.
Perché stadiare ? • Indicazione ad intervento • Tipo di intervento
LA STADIAZIONE PREOPERATORIA • La stadiazione preoperatoria DEVE definire l’estensione endobiliare , extrabiliare e linfonodale della malattia • COME ? TC , RMN , Endo US , ERCP, ecc. . Però…. UNRESECTABLE AT PRESENTATION = UNRESECTABLE AT LAPAROTOMY ?

All’atto dell’intervento …
Perché i tumori delle vie biliari • possono essere multifocali (5%) • Possono dare metastasi linfonodali (50%) • Possono dare metastasi a distanza e/o peritoneali ( 10 -20 %)
La ristadiazione : la stadiazione intraoperatoria …. • Laparoscopia + LUS • Ecografia intraoperatoria • . . colangioscopia? • . . ma anche: dissezione delle strutture esame istologico intraop.
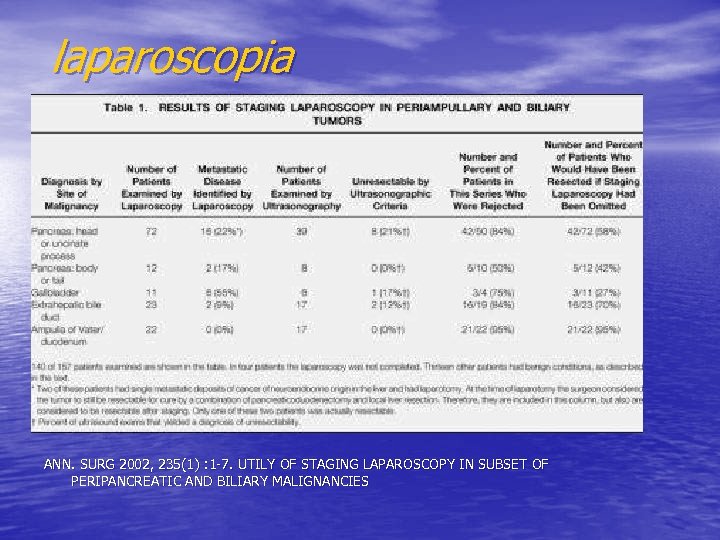
laparoscopia ANN. SURG 2002, 235(1) : 1 -7. UTILY OF STAGING LAPAROSCOPY IN SUBSET OF PERIPANCREATIC AND BILIARY MALIGNANCIES
LAPAROSCOPIA : conclusioni • SI: per ADK TESTA PANCREAS • NO: per tumori ampolla , vb distale • SI : per tumori della colecisti • I tumori dell’ilo e i tumori periferici ?
![Pero’… • Laparoscopy detected the majority (83% [33/40]) of patients with peritoneal or liver Pero’… • Laparoscopy detected the majority (83% [33/40]) of patients with peritoneal or liver](https://present5.com/presentation/4b3a4af9ade9255aafd87c366b04cb2e/image-12.jpg)
Pero’… • Laparoscopy detected the majority (83% [33/40]) of patients with peritoneal or liver metastases but failed to detect all locally advanced tumors (0/19) and most nodal metastases (2/10, P <. 0001). Ann Surg. 2002 March; 235(3): 392– 399. . Staging Laparoscopy in Patients With Extrahepatic Biliary Carcinoma Analysis of 100 Patients Sharon M. Weber, MD, Ronald P. De. Matteo, MD, Yuman Fong, MD, FACS, Leslie H. Blumgart, MD, FRCS, FACS, and William R. Jarnagin, MD, FACS From the Department of Surgery, Hepatobiliary Service, Memorial Sloan-Kettering Cancer Center, New York
Ecografia intraoperatoria • The technique provides important additional, sometimes unexpected, information to the surgeon at the time of operation, and contributes to operative decision making and surgical planning. Neoplasms can be staged, metastases identified, and unexpected lesions discovered and characterized. Intraoperative Sonography of the Biliary System Jonathan B. Kruskal 1 and Robert A. Kane 1 Both authors: Ultrasound Division, Department of Radiology, Beth Israel Deaconess Medical Center, West Campus 302 B, One Deaconess Rd. , Boston MA 02215.
Ecografia intraoperatoria • La conoscenza della anatomia biliare e delle sue varianti è un prerequisito per un corretto uso della metodica , ed è un fattore “ critico” per la resezione chirurgica
Ecografia intraoperatoria • La scelta della frequenza di lavoro e le scansioni sono un altro fattore “critico” per evidenziare lesioni superficiali
Ecografia intraoperatoria • Le flogosi croniche possono simulare neoplasie ; bisogna pertanto conoscere l’ecografia del fegato e delle vie biliari compiutamente : 3° fattore critico : lo skill ecografico
Ecografia intraoperatoria • E’ necessario controllare che non vi siano altre patologie associate e che queste non modifichino il planning chirurgico
Ecografia intraoperatoria • . . e nei casi dubbi il doppler ci può aiutare a distinguere i dotti dai vasi e a valutare la vascolarizzazione di pseudolesioni
I fattori prognostici post-resezione • • Journal of Clinical Oncology, Vol 15, 947 -954, Copyright © 1997 by American Society of Clinical Oncology Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors J Klempnauer, GJ Ridder, R von Wasielewski, M Werner, A Weimann and R Pichlmayr Department of Pathology, Hanover Medical School, Germany. PURPOSE: To define the prognostic factors after surgical resection of bile duct carcinomas at the hepatic bifurcation. PATIENTS AND METHODS: The retrospective single-center experience details 151 patients after surgical resection of central bile duct carcinoma performed between 1971 and 1995. Tumor removal was accomplished by resection of the bile duct bifurcation either alone (group I, n = 33), in combination with hepatic resection (group II, n = 77), or combined with hepatic and vascular resection (group III, n = 41). Survival analysis was performed by the Kaplan -Meier method and the relationship between each of the clinicopathologic variables and survival was assessed by the log-rank test. Multivariate results were confirmed using Cox regression. RESULTS: The overall hospital mortality rate was 9. 9% and depended on the extent of resection (group 1, 6. 1%; group II, 7. 8%; group III, 17. 1%). After exclusion of hospital deaths, the overall patient survival rate was 28. 4% at 5 and 15. 5% at 10 years, with a median survival duration of 2. 05 +/- 0. 23 years. Univariate survival analysis identified tumor size, lymph node metastases, residual tumor stage, and tumor grading as factors with a statistically significant prognostic impact. Survival prognosis was not influenced by the site of the tumor according to the classification of Bismuth and Corlette, extent of resection, International Union Against Cancer (UICC) stage, perineural and vascular invasion, age, or sex. In a multivariate Cox analysis, only lymph node metastases and residual tumor stage proved to be of independent prognostic significance. CONCLUSION: Resection of central bile duct carcinoma is feasible in many patients and a favorable outcome after resection is mainly determined by curative resection and the absence of lymph node metastases.
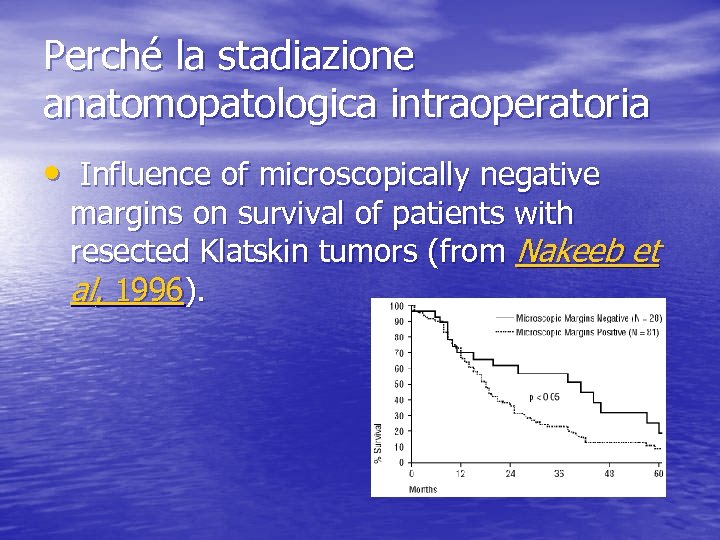
Perché la stadiazione anatomopatologica intraoperatoria • Influence of microscopically negative margins on survival of patients with resected Klatskin tumors (from Nakeeb et al, 1996).
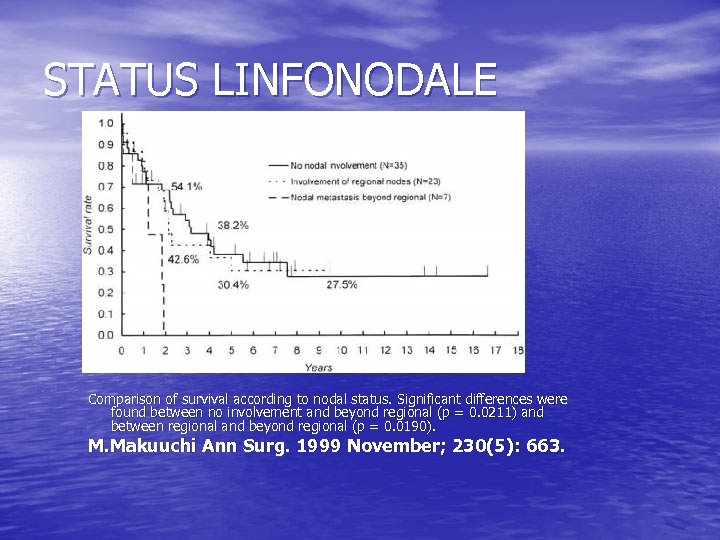
STATUS LINFONODALE Comparison of survival according to nodal status. Significant differences were found between no involvement and beyond regional (p = 0. 0211) and between regional and beyond regional (p = 0. 0190). M. Makuuchi Ann Surg. 1999 November; 230(5): 663.

L’importanza di un protocollo • It is important to evaluate all surgical margins carefully, including an assessment of vascular and perineural invasion. Local recurrence is often related to residual tumor located in the proximal or distal surgical margins of the bile duct or to tumor located along the dissected soft tissue margin in the portal area. Local recurrence (usually at the surgical margins) is most common with carcinomas arising in the hepatic duct(s). • In addition, malignant tumors of the extrahepatic bile ducts are often multifocal. Therefore, microscopic foci of carcinoma or dysplasia may be found at the margin(s) even though the main tumor mass has been resected. In some cases, it may be difficult to evaluate margins on frozen section preparations because of inflammation and reactive atypia of the surface epithelium or within the intramural mucous glands. If surgical margins are free of carcinoma, the distance between the closest margin and the tumor edge should be measured.
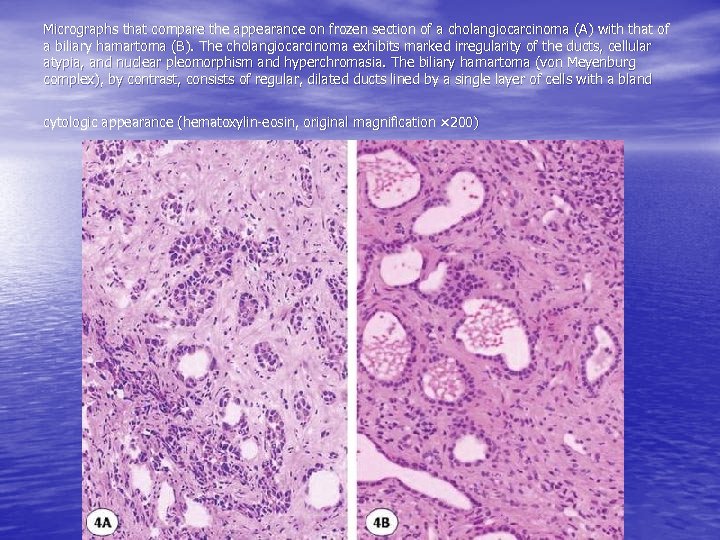
Micrographs that compare the appearance on frozen section of a cholangiocarcinoma (A) with that of a biliary hamartoma (B). The cholangiocarcinoma exhibits marked irregularity of the ducts, cellular atypia, and nuclear pleomorphism and hyperchromasia. The biliary hamartoma (von Meyenburg complex), by contrast, consists of regular, dilated ducts lined by a single layer of cells with a bland cytologic appearance (hematoxylin-eosin, original magnification × 200)
Artifacts and pittfalls cautery Figure 13: specimen showing marked artifact. This creates difficulties in the recognition of malignant structure, located at the center and on the right side (arrows) (hematoxylin-eosin, original magnification × 120). Figure 14. Photomicrograph of a margin with crush artifact, depicting the presence of a duct that exhibits significant dysplasia (hematoxylin-eosin, original magnification × 200)
. . Inoltre 2001 Digestive Disease Week • # 2451 Peritoneal Washings are not Predictive of Advanced Stage in Hilar Cholangiocarcinoma Robert C. G. Martin II, Yuman Fong, Ronald P. Dematteo, Leslie H. Blumgart, William R. Jarnagin, New York, NY
Per concludere: • LA STADIAZIONE INTRAOPERATORIA DEVE ESCLUDERE METASTASI A DISTANZA , MALATTIA MULTIFOCALE E METASTASI LINFONODALI (N 2) • LA STADIAZIONE INTRAOPERATORIA DEVE OTTIMIZZARE LA RESEZIONE • LA STADIAZIONE INTRAOPERATORIA RICHIEDE QUINDI UN TEAM “ASSOLUTAMENTE” AFFIATATO CON COMPETENZE RADIOLOGICHE , ANATOMOPATOLOGICHE E … OVVIAMENTE. . CHIRURGICHE
4b3a4af9ade9255aafd87c366b04cb2e.ppt