IMANGALI MAIRA-Pulmonary TB. Lung Abscess.pptx
- Количество слайдов: 22

SSW Pulmonary tuberculosis-Clinical picture. Lung abscess. Past Perfect Continuous Tense Prepared by: Imangali Maira The faculty of General medicine Group: __14 -24 -2___ Checked by : Tilembaeva A. A.

Plan: • INTRODUCTION • Pulmonary tuberculosis Causes: • • • • Risk of catching TB Clinical features Exams and Tests Treatment Lung Abscess Etiology Clinical presentation Signs Pathology Treatment Past Perfect Continuous USE 1 Duration Before Something in the Past USE 2 Cause of Something in the Past Continuous vs. Past Perfect Continuous Conclusion References

INTRODUCTION • Pulmonary tuberculosis (TB) is a common infectious disease and a major cause of illness and death throughout the world, particularly in developing countries.

Pulmonary tuberculosis Causes: • Pulmonary tuberculosis (TB) is caused by the bacteria Mycobacterium tuberculosis (M. tuberculosis). You can get TB by breathing in air droplets from a cough or sneeze of an infected person. • The resulting lung infection is called primary TB. • Most people recover from primary TB infection without further evidence of the disease. The infection may stay inactive (dormant) for years. However, in some people it can reactivate. • Most people who develop symptoms of a TB infection first became infected in the past. In some cases, the disease becomes active within weeks after the primary infection.

Risk of catching TB • The following persons are at high risk of active TB: • Elderly • Infants • People with weakened immune systems, for example due to AIDS, chemotherapy, diabetes, or medicines that weaken the immune system • Your risk of catching TB increases if you: • Are around people who have TB • Live in crowded or unclean living conditions • Have poor nutrition • The following factors may increase the rate of TB infection in a population: • Increase in HIV infections • Increase in number of homeless people (poor environment and nutrition) • The appearance of drug-resistant strains of TB

Clinical features • Cough is the commonest presentation. • Initially it may be nonproductive, but as inflammation and tissue necrosis ensue, sputum is produced. • Haemoptysis is occasionally a presenting symptom but usually results from previous disease and may not indicate active tuberculosis. • It may arise from tuberculous bronchiectasis, rupture of a dilated vessel in the wall of a cavity (Rasmussen's aneurysm), bacterial or fungal infection (especially Aspergillus mycetoma) in a cavity or erosion into an airway (broncholithiasis). • Inflammation of the lung parenchyma adjacent to a pleural surface may cause pleuritic pain. • Dyspnoea is unusual unless there is extensive disease and may result in respiratory failure • Rales or crackles may be heard in the area of involvement and bronchial breathing indicating consolidation.

Exams and Tests The doctor or nurse will perform a physical exam. This may show: • Clubbing of the fingers or toes (in people with advanced disease) • Swollen or tender lymph nodes in the neck or other areas • Fluid around a lung (pleural effusion) • Unusual breath sounds (crackles) Tests may include: • Biopsy of the affected tissue (rare) • Bronchoscopy • Chest CT scan • Chest x-ray • Interferon-gamma release blood test such as the QFT-Gold test to test for TB infection • Sputum examination and cultures • Thoracentesis • Tuberculin skin test (also called a PPD test)

Treatment Commonly used drugs include: • Isoniazid • Rifampin • Pyrazinamide • Ethambutol

Lung Abscess • Lung abscess is a circumscribed collection of pus within the lung, is are potentially life threatening. They are often complicated to manage and difficult to treat.

Etiology • Most lung abscesses develop after aspiration of oral secretions by patients with gingivitis or poor oral hygiene. • Typically, patients have altered consciousness as a result of alcohol intoxication, illicit drugs, anesthesia, sedatives, or opioids. • Older patients and those unable to handle their oral secretions, often because of neurologic disease, are also at risk. Lung abscesses can also develop secondary to endobronchial obstruction (eg, due to bronchial carcinoma) or to immunosuppression (eg, due to HIV/AIDS or after transplantation and use of immunosuppressive drugs). •
Clinical presentation • Lung abscesses are divided according to their duration into acute (< 6 weeks) and chronic (> 6 weeks). • Presentation is usually non-specific and generally similar to a non-cavitating chest infection. Symptoms include fever, cough and shortness of breath. • Peripheral abscesses may also cause pleuritic chest pain. • If chronic, symptoms are more indolent and include weight loss and constitutional symptoms. In some cases erosion into a bronchial vessel may result in sudden and potentially life threatening massive haemoptysis.
Signs • Tachypnoea • Tachycardia • Finger clubbing in chronic cases • Dehydration • High temperature • Localised dullness to percussion (if consolidation is also present or effusion) • Bronchial breathing and/or crepitations (if consolidation is present) • Also look for signs of severe periodontal disease and infective endocarditis

Pathology • A primary abscess is one which develops as a result of primary infection of the lung. They most commonly arise from aspiration, necrotising pneumonia or chronic pneumonia, e. g. pulmonary tuberculosis In patients who develop abscesses as a result of aspiration, mixed infections are most common, including anaerobes. Some organisms are particularly prone to causes significant necrotising pneumonia resulting in cavitation and abscess formation. These include 1: • Staphylococcus aureus • Klebsiella sp: Klebsiella pneumonia • Pseudomonas sp • Proteus sp
• A secondary abscess is one which develops as a result of another condition. Examples include: • bronchial obstruction: bronchogenic carcinoma, inhaled foreign body • haematogeneous spread: bacterial endocarditis, IVDU • direct extension from adjacent infection: mediastinum, subphrenic, chest wall • Also sometimes grouped with secondary abscesses are colonisation of pre-existing cavities with organisms
Treatment • Antibiotics • Most lung abscesses (80 -90%) are now successfully treated with antibiotics. • Begin with intravenous treatment, usually for about 2 -3 weeks, and follow with oral antibiotics for a further 4 -8 weeks. • Recommended first-line therapy includes beta-lactam/betalactamase inhibitor or cephalosporin (second- or thirdgeneration) plus clindamycin
![Past Perfect Continuous FORM • [had been + present participle] Examples: • You had Past Perfect Continuous FORM • [had been + present participle] Examples: • You had](https://present5.com/presentation/80211857_437109338/image-16.jpg)
Past Perfect Continuous FORM • [had been + present participle] Examples: • You had been waiting there for more than two hours when she finally arrived. • Had you been waiting there for more than two hours when she finally arrived? • You had not been waiting there for more than two hours when she finally arrived.
USE 1 Duration Before Something in the Past We use the Past Perfect Continuous to show that something started in the past and continued up until another time in the past. "For five minutes" and "for two weeks" are both durations which can be used with the Past Perfect Continuous. Notice that this is related to the Present Perfect Continuous; however, the duration does not continue until now, it stops before something else in the past. Examples: • They had been talking for over an hour before Tony arrived. • She had been working at that company for three years when it went out of business. • How long had you been waiting to get on the bus? • Mike wanted to sit down because he had been standing all day at work.
USE 2 Cause of Something in the Past • Using the Past Perfect Continuous before another action in the past is a good way to show cause and effect. Examples: • Jason was tired because he had been jogging. • Sam gained weight because he had been overeating. • Betty failed the final test because she had not been attending class.
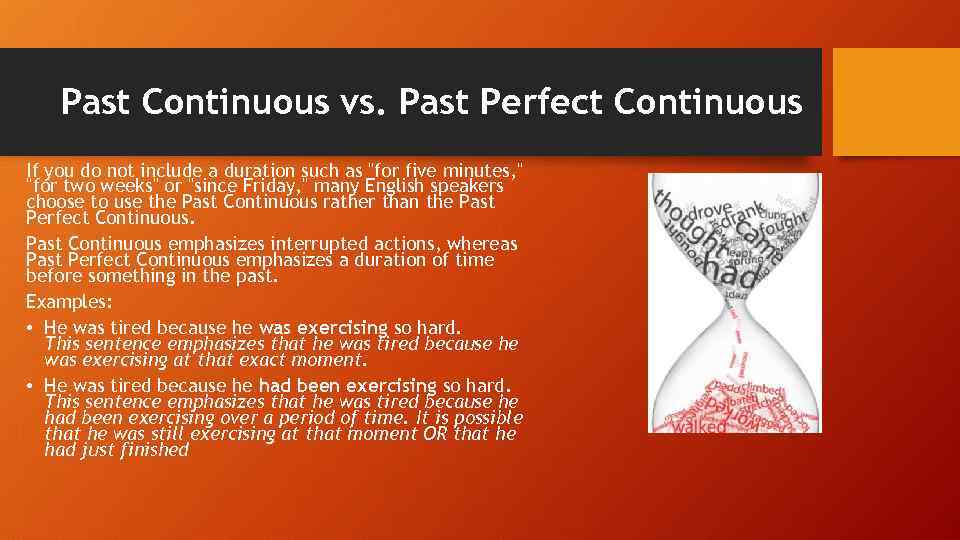
Past Continuous vs. Past Perfect Continuous If you do not include a duration such as "for five minutes, " "for two weeks" or "since Friday, " many English speakers choose to use the Past Continuous rather than the Past Perfect Continuous. Past Continuous emphasizes interrupted actions, whereas Past Perfect Continuous emphasizes a duration of time before something in the past. Examples: • He was tired because he was exercising so hard. This sentence emphasizes that he was tired because he was exercising at that exact moment. • He was tired because he had been exercising so hard. This sentence emphasizes that he was tired because he had been exercising over a period of time. It is possible that he was still exercising at that moment OR that he had just finished
Conclusion • The lungs are made up of approximately 350 million tiny sacs called alveoli, where carbon dioxide from the body is exchanged for oxygen from the air. Various diseases that affect the lungs

References • Chan PC, Huang LM, Wu PS, et al; Clinical management and outcome of childhood lung abscess: a 16 -year experience. J Microbiol Immunol Infect. 2005 Jun; 38(3): 183 -8. • Yu H, Higa F, Koide M, et al; Lung abscess caused by Legionella species: implication of the immune status of hosts. Intern Med. 2009; 48(23): 1997 -2002. Epub 2009 Dec 1. • Schiza S, Siafakas NM; Clinical presentation and management of empyema, lung abscess and pleural effusion. Curr Opin Pulm Med. 2006 May; 12(3): 205 -11. • Umemori Y, Hiraki A, Murakami T, et al; Chronic lung abscess with Pasteurella multocida infection. Intern Med. 2005 Jul; 44(7): 754 -6. • Ellner JJ. Tuberculosis. In: Goldman L, Schafer AI, eds. Goldman's Cecil Medicine. 24 th ed. Philadelphia, PA: Elsevier Saunders; 2011: chap 332. • Fitzgerald DW, Sterling TR, Haas DW. Mycobacterium tuberculosis. In: Mandell GL, Bennett JE, Dolan R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7 th ed. Philadelphia, PA: Elsevier Churchill-Livingstone; 2009: chap 250. • http: //englishpage. com/verbpage/pastperfectcontinuous. html
Thank you for your attention!
IMANGALI MAIRA-Pulmonary TB. Lung Abscess.pptx