0d512268cb11990a083e09834ebff37d.ppt
- Количество слайдов: 17
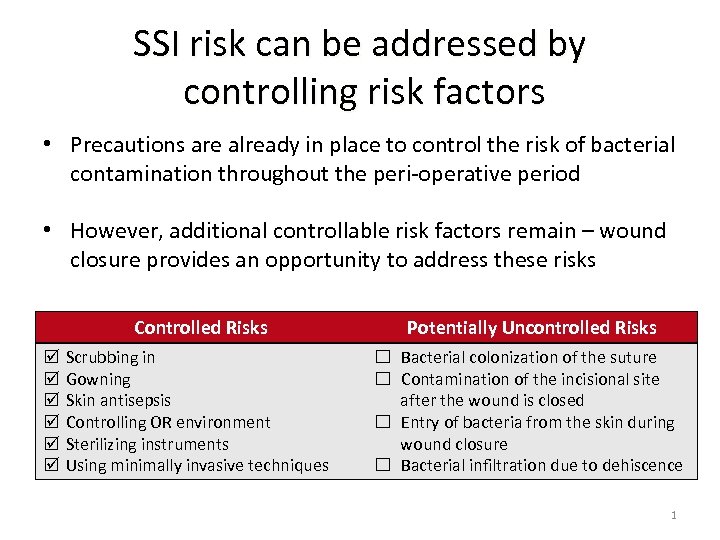
SSI risk can be addressed by controlling risk factors • Precautions are already in place to control the risk of bacterial contamination throughout the peri‐operative period • However, additional controllable risk factors remain – wound closure provides an opportunity to address these risks Controlled Risks þ þ þ Potentially Uncontrolled Risks Scrubbing in Gowning Skin antisepsis Controlling OR environment Sterilizing instruments Using minimally invasive techniques ☐ Bacterial colonization of the suture ☐ Contamination of the incisional site after the wound is closed ☐ Entry of bacteria from the skin during wound closure ☐ Bacterial infiltration due to dehiscence 1
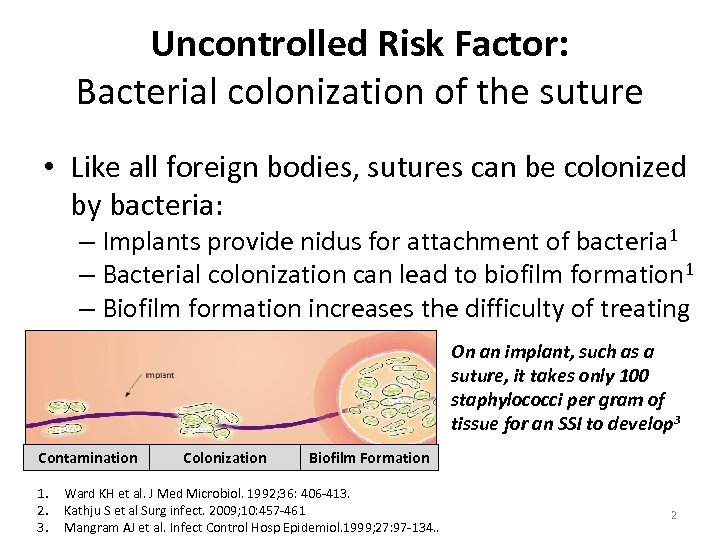
Uncontrolled Risk Factor: Bacterial colonization of the suture • Like all foreign bodies, sutures can be colonized by bacteria: – Implants provide nidus for attachment of bacteria 1 – Bacterial colonization can lead to biofilm formation 1 – Biofilm formation increases the difficulty of treating an infection 2 On an implant, such as a suture, it takes only 100 staphylococci per gram of tissue for an SSI to develop 3 Contamination 1. 2. 3. Colonization Biofilm Formation Ward KH et al. J Med Microbiol. 1992; 36: 406‐ 413. Kathju S et al Surg infect. 2009; 10: 457‐ 461 Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 27: 97‐ 134. . 2
Why Antimicrobial Suture? OR Air Current Contamination In teaching hospitals: Surgeon leaves room Resident, Physician Assistant or Nurse Practitioner work on incision Circulating Nurse counts sponges and starts room breakdown Scrub Technician starts breaking down tables and preparing instruments for Central Processing Anesthesia move in and out of room Instrument representative might leave room and Visitors may leave room
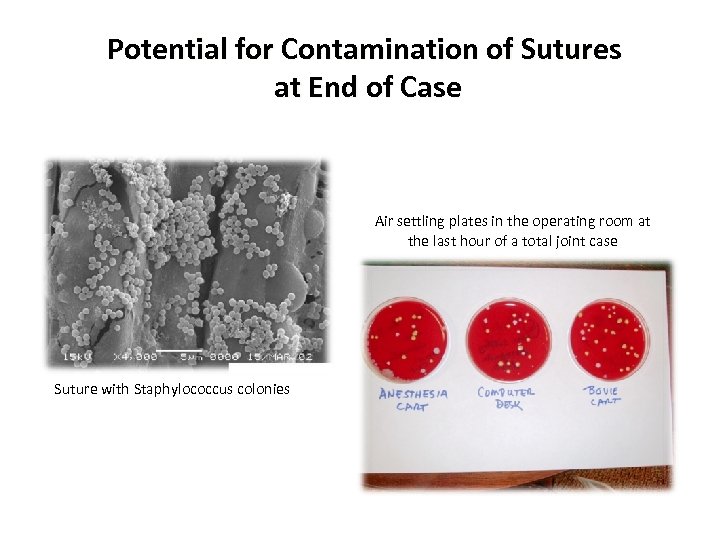
Potential for Contamination of Sutures at End of Case Air settling plates in the operating room at the last hour of a total joint case Suture with Staphylococcus colonies
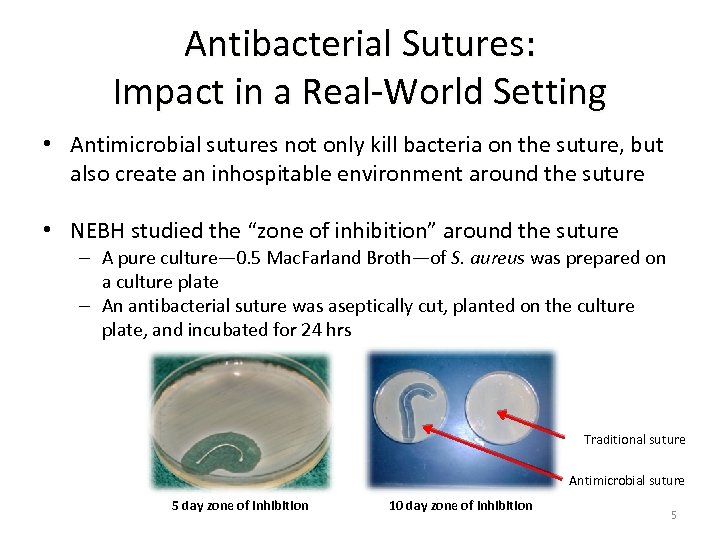
Antibacterial Sutures: Impact in a Real‐World Setting • Antimicrobial sutures not only kill bacteria on the suture, but also create an inhospitable environment around the suture • NEBH studied the “zone of inhibition” around the suture – A pure culture— 0. 5 Mac. Farland Broth—of S. aureus was prepared on a culture plate – An antibacterial suture was aseptically cut, planted on the culture plate, and incubated for 24 hrs Traditional suture Antimicrobial suture 5 day zone of inhibition 10 day zone of inhibition 5
Plus Antibacterial Sutures: Impact in a Real‐World Setting • NEBH One Year Prospective Study of 3800 Total Joints and Antimicrobial Sutures – In July 2005, implemented a full‐year evaluation of antibacterial sutures usage in an orthopedic setting – Changed product over July 4 th holiday and did not tell all surgeons (only those involved with study) • At the end of the year‐long trial period: – 45% reduction in SSIs caused by Staph aureus and MRSA – Reduction in total joint infections rate during trial period – Infection rate dropped from 0. 44% to 0. 33% with three less infections NAON Poster Presentation ‐ 2010 § Spencer M, et al: Reducing the Risk of Orthopedic Infections: The Role of Innovative Suture Technology 6
Triclosan‐coated sutures for the reduction of sternal wound infection Fleck et al. , Ann Thoracic Surg. 2007 • 479 patients – CABG, Valve, CABG‐Valve, Redo • 376 conventional closure; 103 impregnated technology • IV ABX Prophylaxis – 30 minutes prior to incision • 24 sternal wound infections in conventional closure group (10 superficial; 14 deep – MSSA, MRSA, MSSE, Enterococcus) • No infections observed in impregnated closure group • Economic consideration – “increase in suture cost was negligible if even one sternal wound infection can be prevented”
Antibiotic coating of abdominal closure sutures and wound infection Justinger et al 2009 • 2, 088 abdominal operations via midline incision. • Prospective cohort comparison PDS II loop suture vs Vicryl plus • No other changes in protocols of patient care. • Risk factors for SSI were comparable between the 2 groups. • Primary outcome was the number of wound infections. • PDS SSI 10. 8% vs. Vicryl plus SSI 4. 9% (p <. 001)
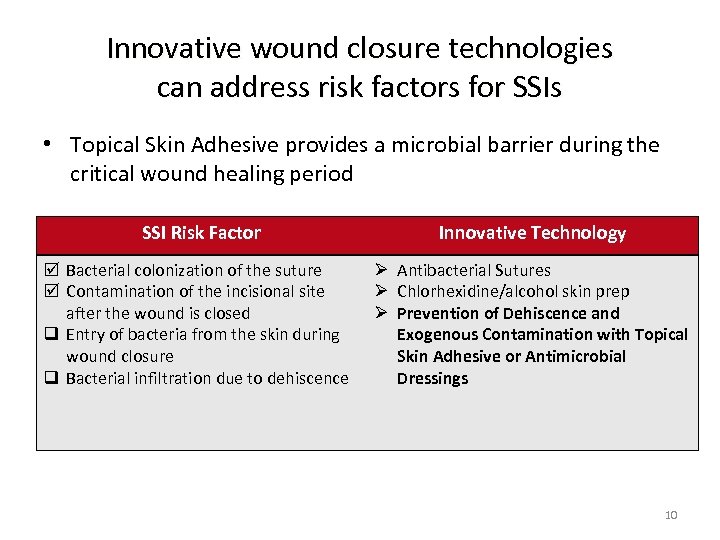
Innovative wound closure technologies can address risk factors for SSIs • Topical Skin Adhesive provides a microbial barrier during the critical wound healing period SSI Risk Factor þ Bacterial colonization of the suture þ Contamination of the incisional site after the wound is closed q Entry of bacteria from the skin during wound closure q Bacterial infiltration due to dehiscence Innovative Technology Ø Antibacterial Sutures Ø Chlorhexidine/alcohol skin prep Ø Prevention of Dehiscence and Exogenous Contamination with Topical Skin Adhesive or Antimicrobial Dressings 10

Post‐op Skin Issues in Orthopedics Anterior fusion with tape burns Posterior fusion with contaminated steri‐strips Contaminated steri‐strips Staples increase infection rate
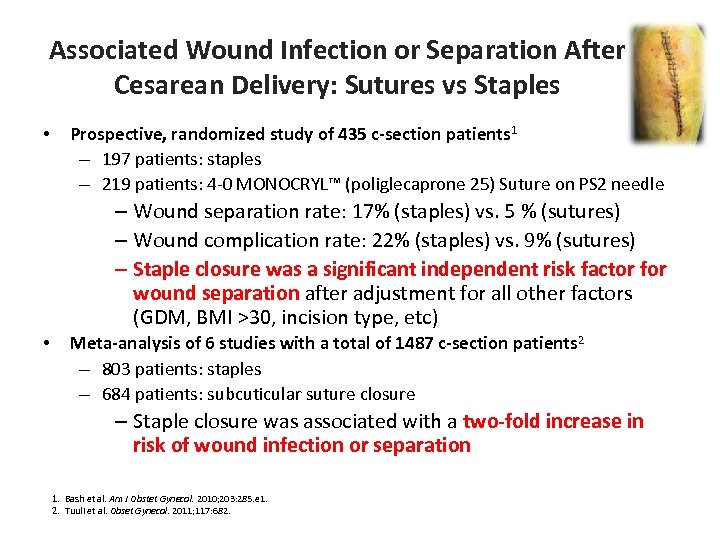
Associated Wound Infection or Separation After Cesarean Delivery: Sutures vs Staples • Prospective, randomized study of 435 c-section patients 1 – 197 patients: staples – 219 patients: 4‐ 0 MONOCRYL™ (poliglecaprone 25) Suture on PS 2 needle – Wound separation rate: 17% (staples) vs. 5 % (sutures) – Wound complication rate: 22% (staples) vs. 9% (sutures) – Staple closure was a significant independent risk factor for wound separation after adjustment for all other factors (GDM, BMI >30, incision type, etc) • Meta-analysis of 6 studies with a total of 1487 c-section patients 2 – 803 patients: staples – 684 patients: subcuticular suture closure – Staple closure was associated with a two-fold increase in risk of wound infection or separation 1. Bash et al. Am J Obstet Gynecol. 2010; 203: 285. e 1. 2. Tuuli et al. Obset Gynecol. 2011; 117: 682.
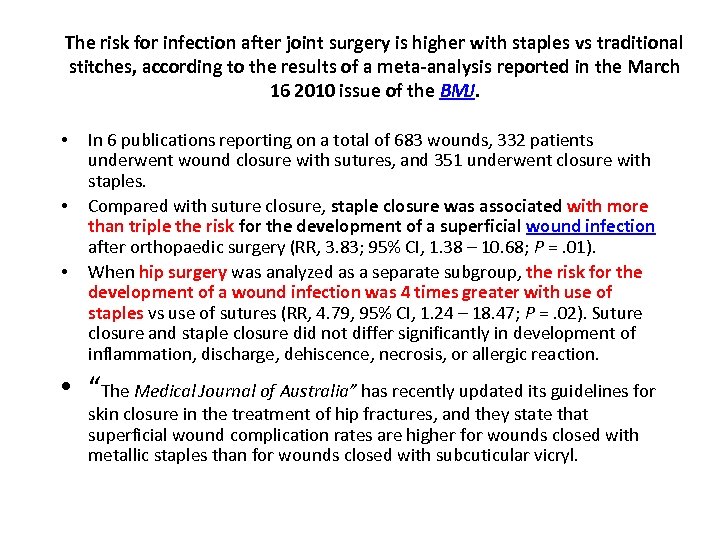
The risk for infection after joint surgery is higher with staples vs traditional stitches, according to the results of a meta-analysis reported in the March 16 2010 issue of the BMJ. • • • In 6 publications reporting on a total of 683 wounds, 332 patients underwent wound closure with sutures, and 351 underwent closure with staples. Compared with suture closure, staple closure was associated with more than triple the risk for the development of a superficial wound infection after orthopaedic surgery (RR, 3. 83; 95% CI, 1. 38 – 10. 68; P =. 01). When hip surgery was analyzed as a separate subgroup, the risk for the development of a wound infection was 4 times greater with use of staples vs use of sutures (RR, 4. 79, 95% CI, 1. 24 – 18. 47; P =. 02). Suture closure and staple closure did not differ significantly in development of inflammation, discharge, dehiscence, necrosis, or allergic reaction. • “The Medical Journal of Australia” has recently updated its guidelines for skin closure in the treatment of hip fractures, and they state that superficial wound complication rates are higher for wounds closed with metallic staples than for wounds closed with subcuticular vicryl.
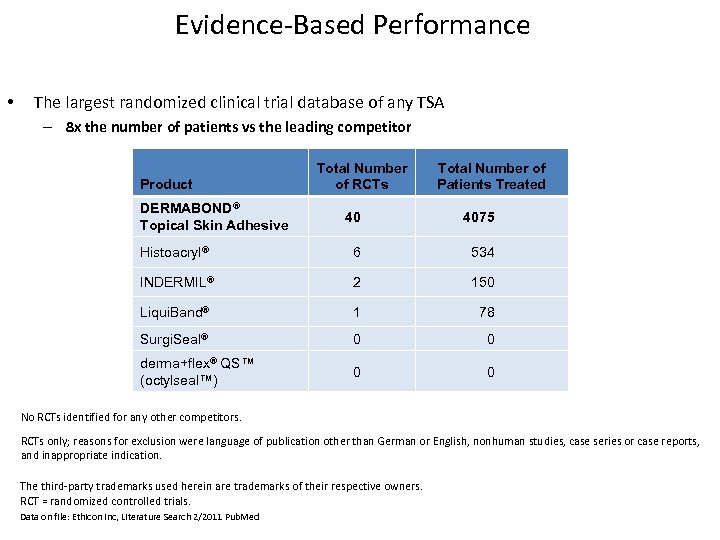
Evidence‐Based Performance • The largest randomized clinical trial database of any TSA – 8 x the number of patients vs the leading competitor Product DERMABOND® Topical Skin Adhesive Total Number of RCTs Total Number of Patients Treated 40 4075 Histoacryl® 6 534 INDERMIL® 2 150 Liqui. Band® 1 78 Surgi. Seal® 0 0 derma+flex® QS™ (octylseal™) 0 0 No RCTs identified for any other competitors. RCTs only; reasons for exclusion were language of publication other than German or English, nonhuman studies, case series or case reports, and inappropriate indication. The third‐party trademarks used herein are trademarks of their respective owners. RCT = randomized controlled trials. Data on file: Ethicon Inc, Literature Search 2/2011 Pub. Med
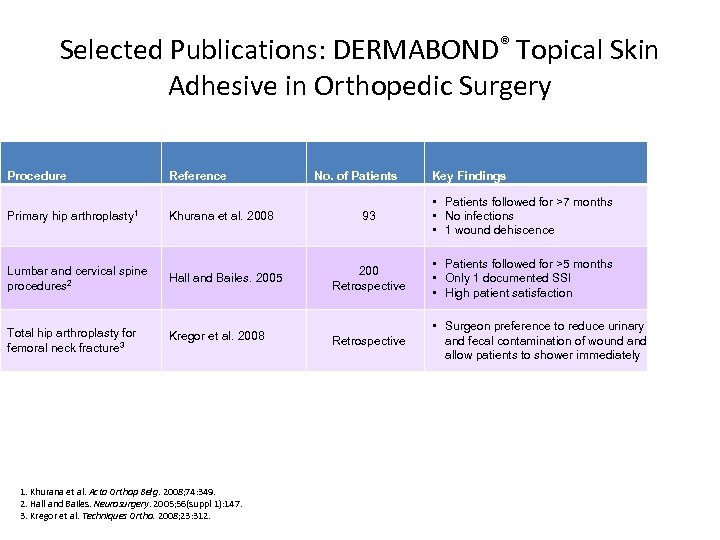
Selected Publications: DERMABOND® Topical Skin Adhesive in Orthopedic Surgery Procedure Primary hip Reference arthroplasty 1 Khurana et al. 2008 Lumbar and cervical spine procedures 2 Hall and Bailes. 2005 Total hip arthroplasty for femoral neck fracture 3 Kregor et al. 2008 1. Khurana et al. Acta Orthop Belg. 2008; 74: 349. 2. Hall and Bailes. Neurosurgery. 2005; 56(suppl 1): 147. 3. Kregor et al. Techniques Ortho. 2008; 23: 312. No. of Patients Key Findings 93 • Patients followed for >7 months • No infections • 1 wound dehiscence 200 Retrospective • Patients followed for >5 months • Only 1 documented SSI • High patient satisfaction Retrospective • Surgeon preference to reduce urinary and fecal contamination of wound allow patients to shower immediately
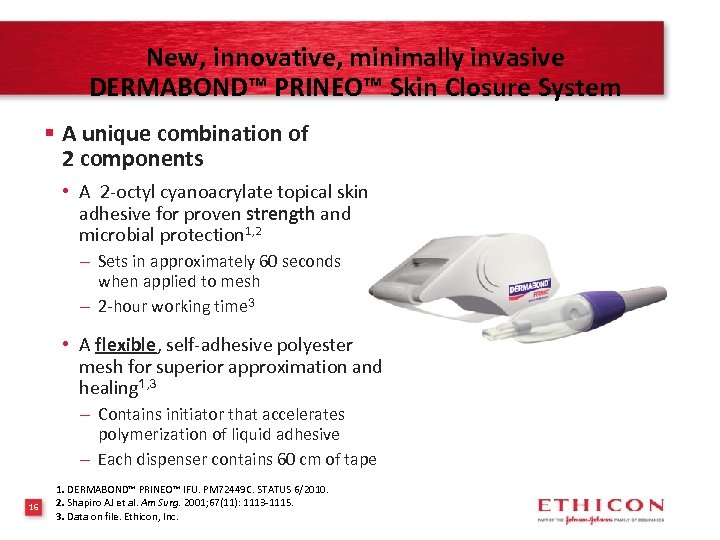
New, innovative, minimally invasive DERMABOND™ PRINEO™ Skin Closure System § A unique combination of 2 components • A 2‐octyl cyanoacrylate topical skin adhesive for proven strength and microbial protection 1, 2 – Sets in approximately 60 seconds when applied to mesh – 2‐hour working time 3 • A flexible, self‐adhesive polyester mesh for superior approximation and healing 1, 3 – Contains initiator that accelerates polymerization of liquid adhesive – Each dispenser contains 60 cm of tape 16 1. DERMABOND™ PRINEO™ IFU. PM 72449 C. STATUS 6/2010. 2. Shapiro AJ et al. Am Surg. 2001; 67(11): 1113‐ 1115. 3. Data on file. Ethicon, Inc.
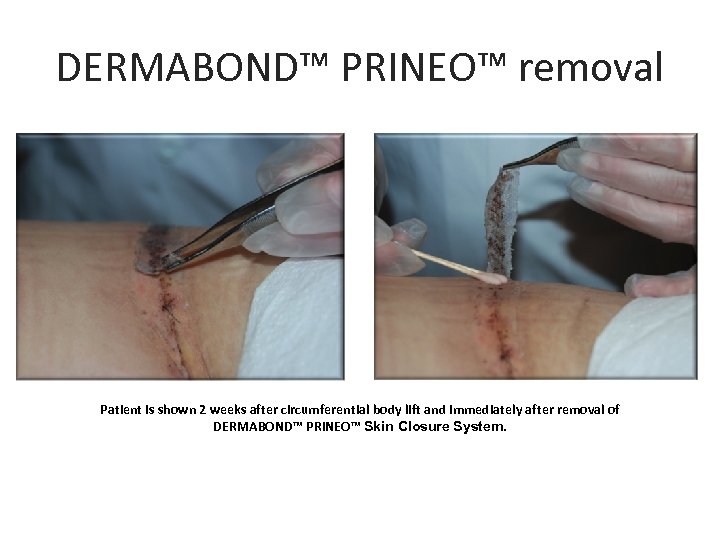
DERMABOND™ PRINEO™ removal Patient is shown 2 weeks after circumferential body lift and immediately after removal of DERMABOND™ PRINEO™ Skin Closure System.
0d512268cb11990a083e09834ebff37d.ppt