Spine Anne Mitchener Consultant Neurosurgeon Back Pain-theory Disc

Spine Anne Mitchener Consultant Neurosurgeon
Back Pain-theory Disc degeneration Micro instability Joint hypertrophy Ligamentous hypertrophy
Back pain-syndromes Disc dehydration Disc prolapse Facet joint pain Canal stenosis Foraminal stenosis Spondylolisthesis Scoliosis
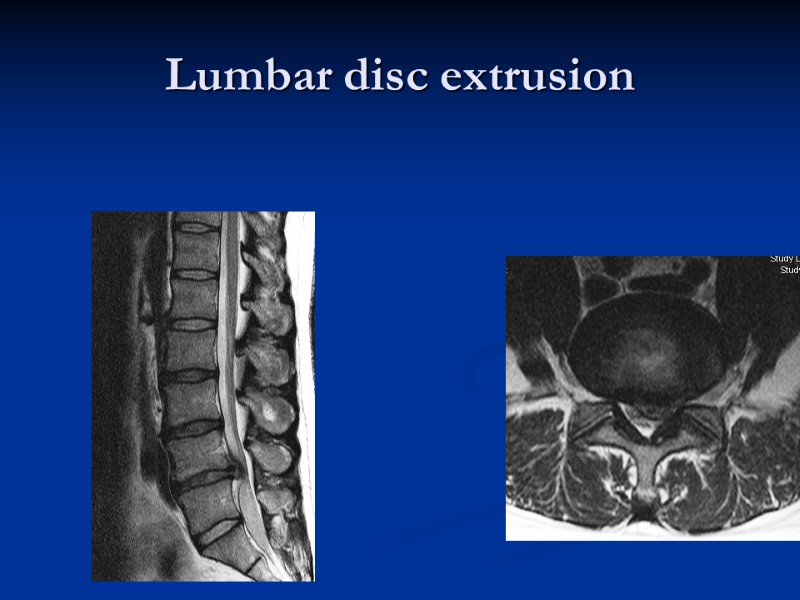
Lumbar disc extrusion
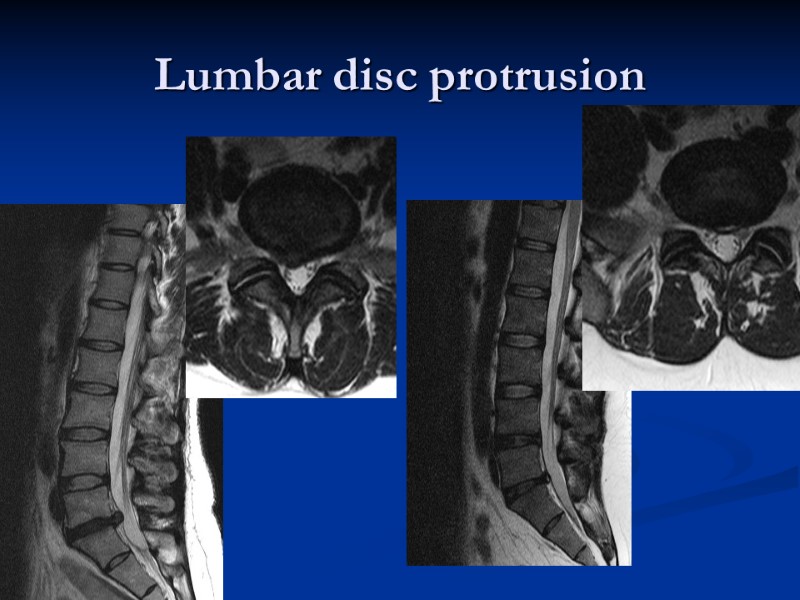
Lumbar disc protrusion
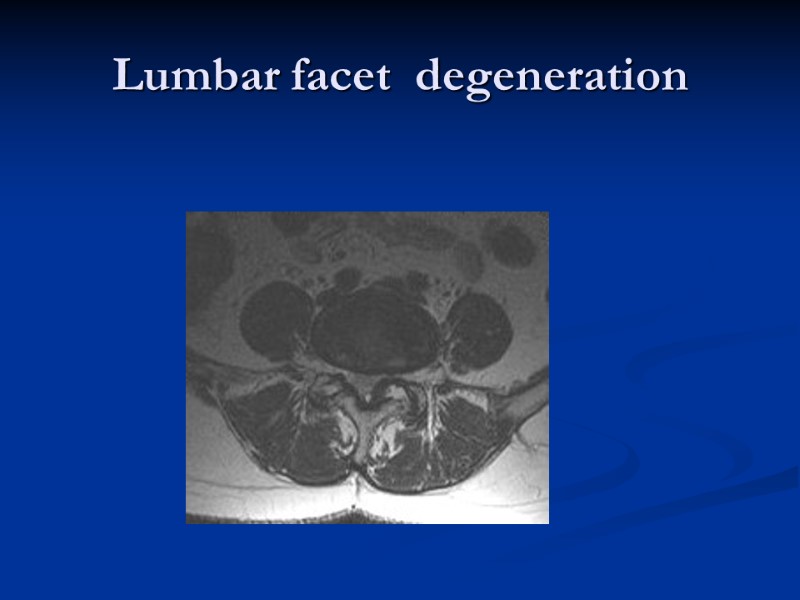
Lumbar facet degeneration
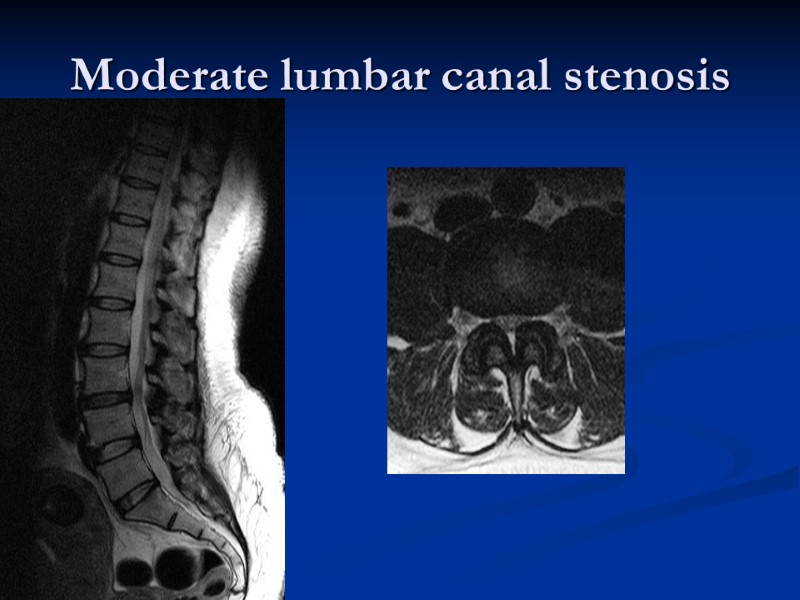
Moderate lumbar canal stenosis
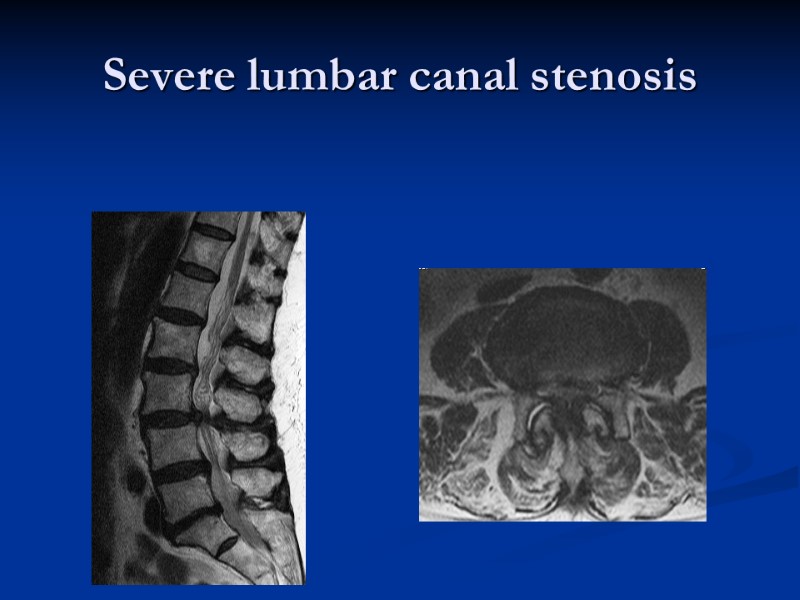
Severe lumbar canal stenosis
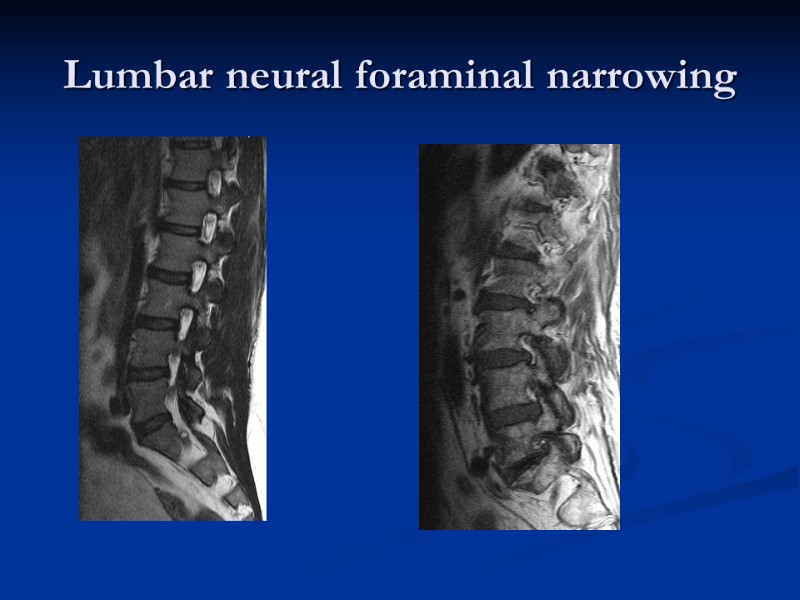
Lumbar neural foraminal narrowing
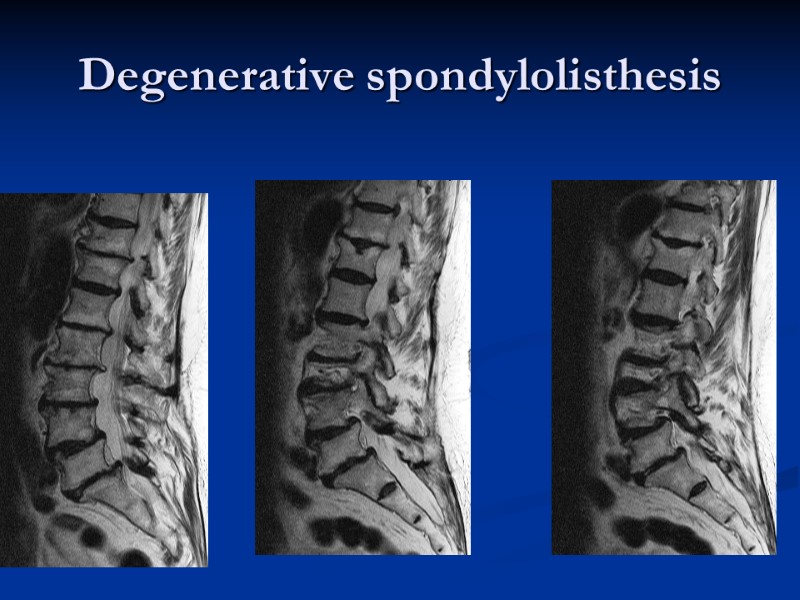
Degenerative spondylolisthesis
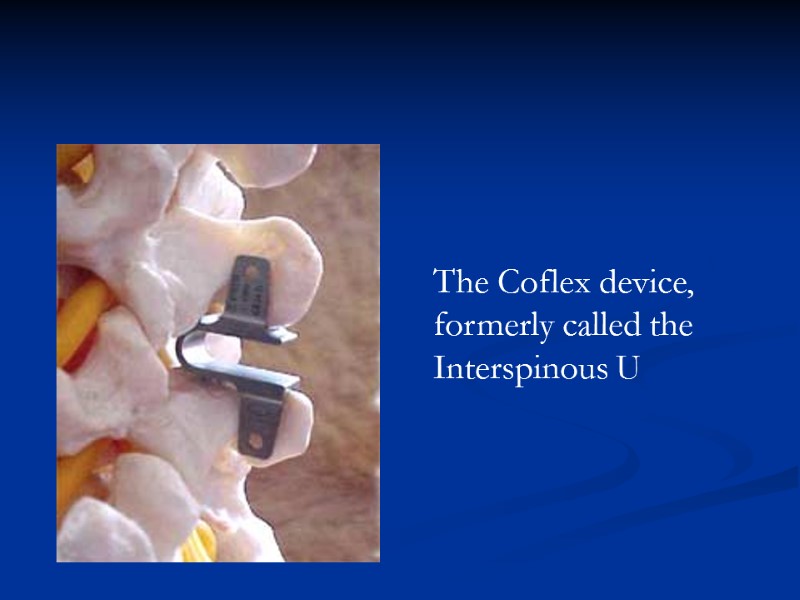
The Coflex device, formerly called the Interspinous U
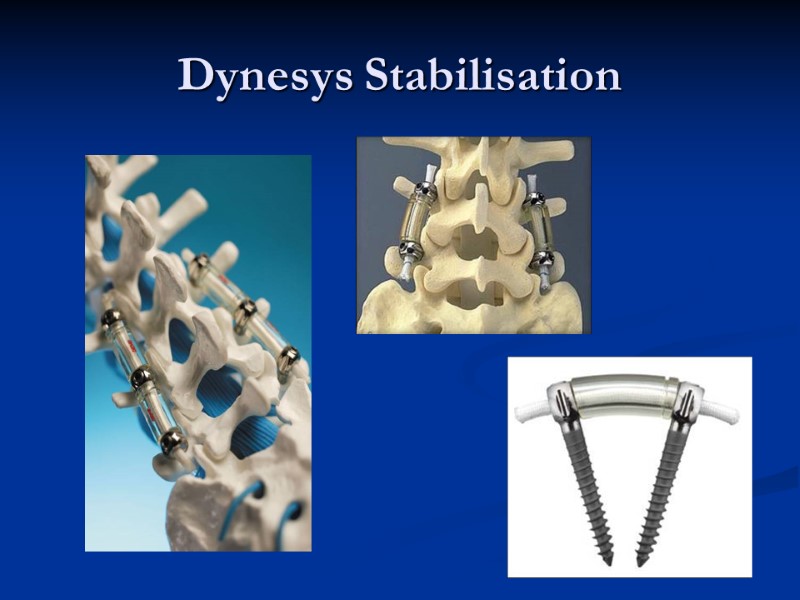
Dynesys Stabilisation

Fusion-titanium vs peek
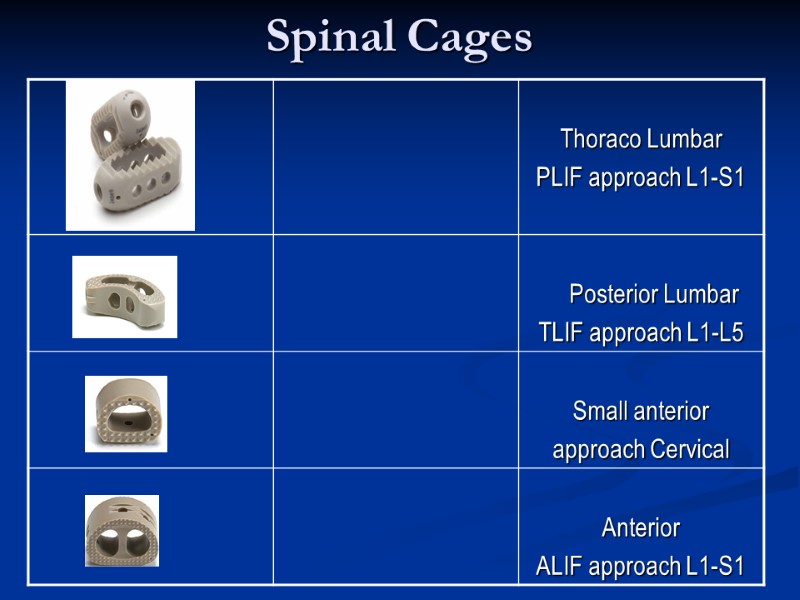
Spinal Cages
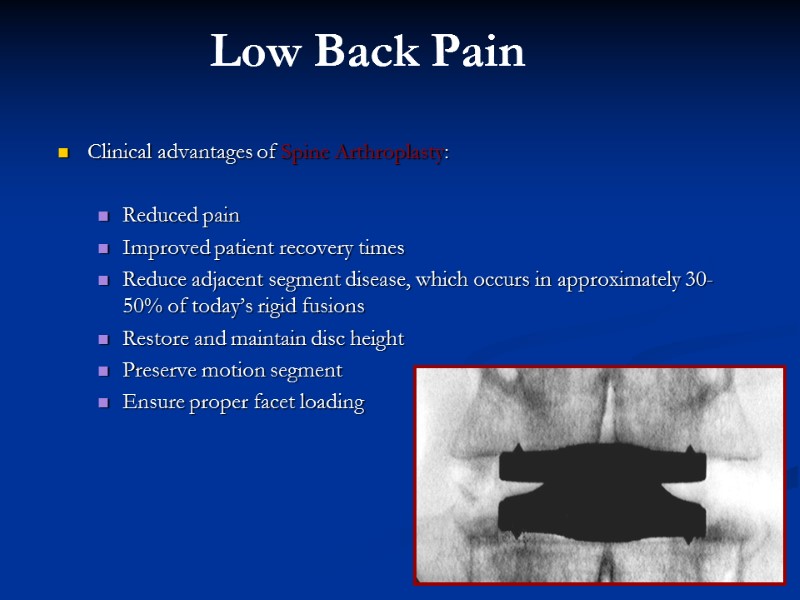
Clinical advantages of Spine Arthroplasty: Reduced pain Improved patient recovery times Reduce adjacent segment disease, which occurs in approximately 30-50% of today’s rigid fusions Restore and maintain disc height Preserve motion segment Ensure proper facet loading Low Back Pain
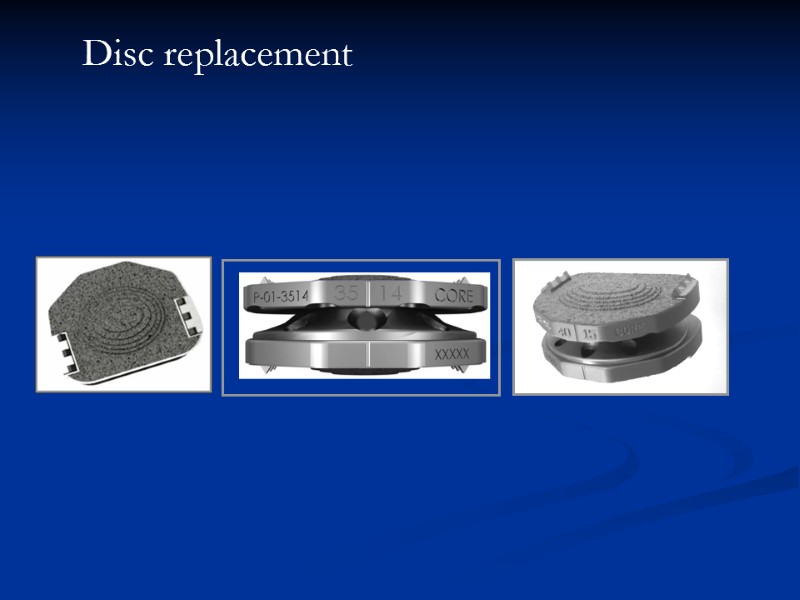
Disc replacement
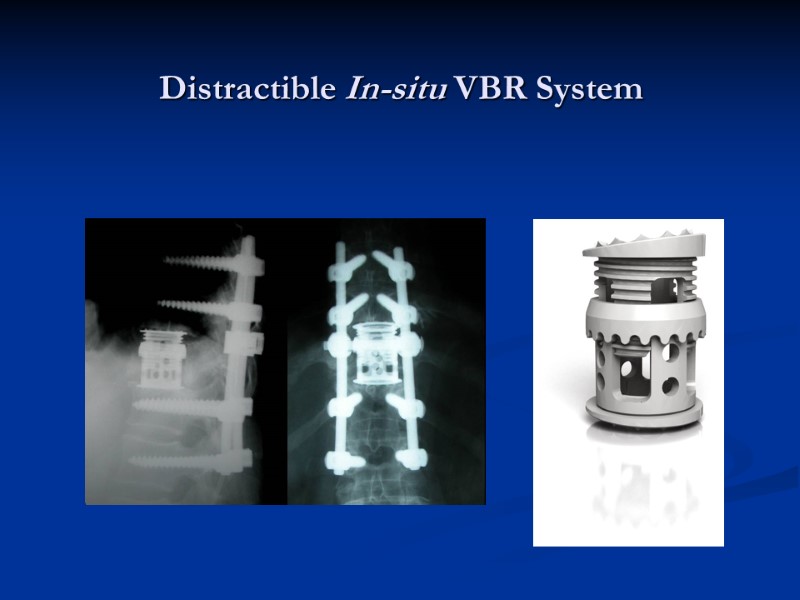
Distractible In-situ VBR System
Back pain If the patient appears to be a candidate for intervention consider referral... There are many and varied treatment options to be tailored to needs.
Cervical degenerative spine disorders Mrs Anne Mitchener Consultant Neurosurgeon
Cervical Degenerative Disease Cervical Disc Herniation-protrusion/extrusion of nucleus pulposus-”acute” Cervical Spondylosis-involves osteophyte formation-”chronic”
Cervical Degenerative Disease Occurs when flexion, extension ,rotation or lateral flexion exceeds the strength of the disc annulus and anterior and posterior ligaments Posterior ligament weak laterally herniations and radiculopathy more common than myelopathy. Pain,motor,sensory and reflex deficits occur. Commonest levels C5/6 and C6/7
Cervical degenerative Disease Myelopathy results from central cervical disc herniation Complete or commonly incomplete clinically Segmental damage at the cord level and long tract signs below.
Cervical Spondylosis Age related progressive changes on imaging 50% over 50 years and 75% over 65 years show spondylosis Few develop functional neurological deficits of radiculopathy/myelopathy
Myelopathic Symptoms Impaired coordination of hands Gait abnormality-weakness/ataxia Cervicobrachalgia Spasticity,para/tetraparesis Autonomic disturbance such as micturition L’Hermittes Sign
Cervical Spondylosis Discs degenerate, loss of water and disc height Micro movement postulated Clear instability rarely demonstrated Facet joints and ligaments hypertrophy bone grows over herniated disc-osteophyte Canal/foramen narrows-myelopathy/radiculopathy can result
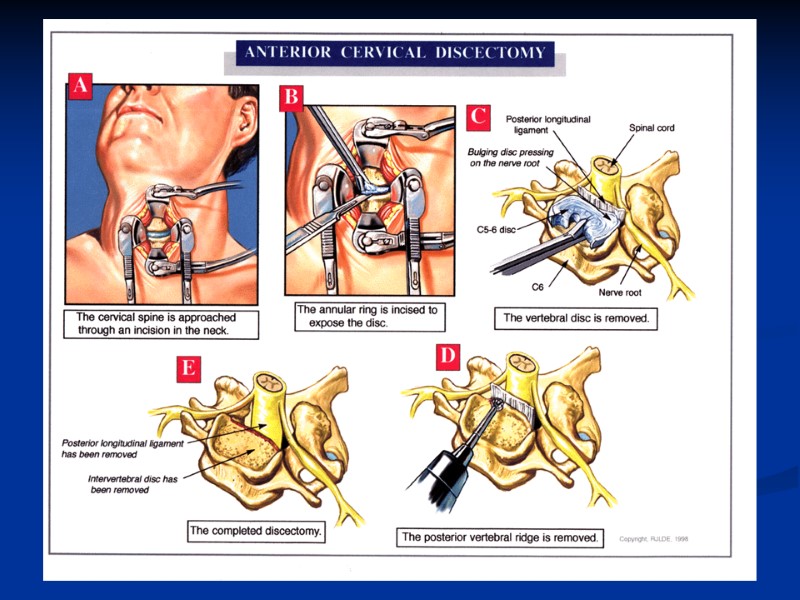
Surgical approaches Posterior surgical approach began with Sir victor Horsley in 1895-laminectomy /foraminotomy Anterior approach began in 1958 was developed by Cloward-discectomy and fusion
Results Posterior Approach Laminectomy can lead to instability and incomplete decompression-less reliable Foraminotomy can have excellent results for radiculopathy
Results Anterior Approaches Radiculopathy 75-90% excellent recovery Myelopathy 85% marked improvement-depends on severity, performed to prevent deterioration
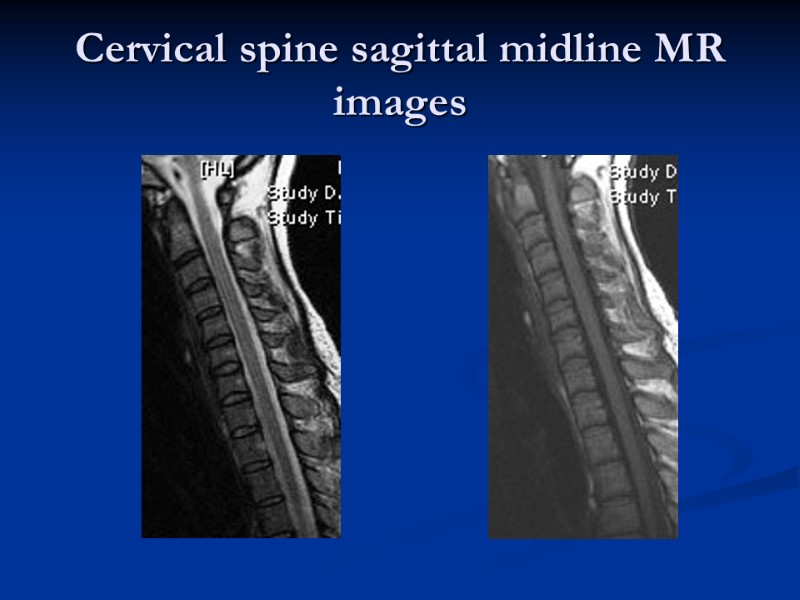
Cervical spine sagittal midline MR images
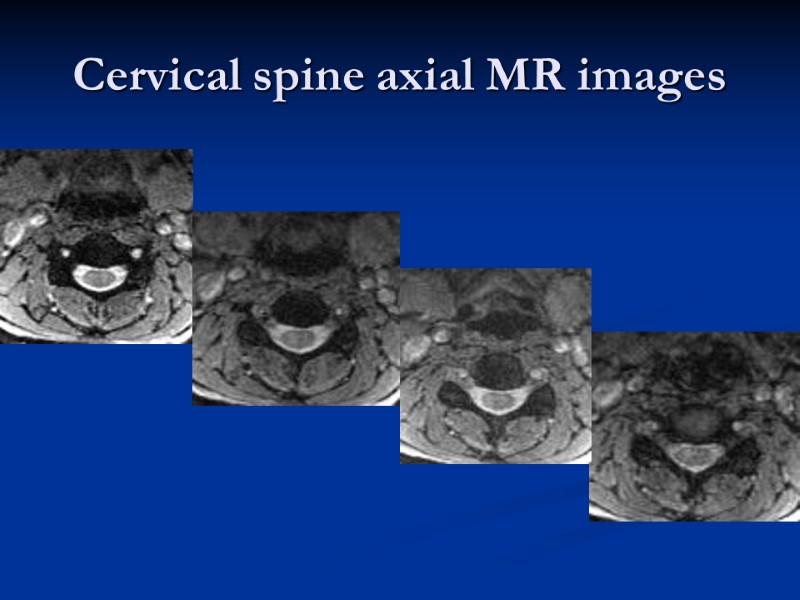
Cervical spine axial MR images
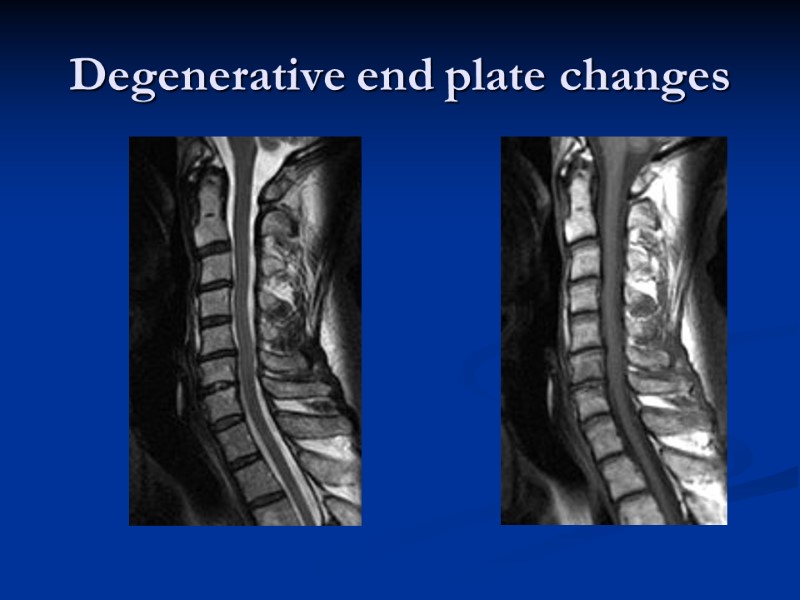
Degenerative end plate changes
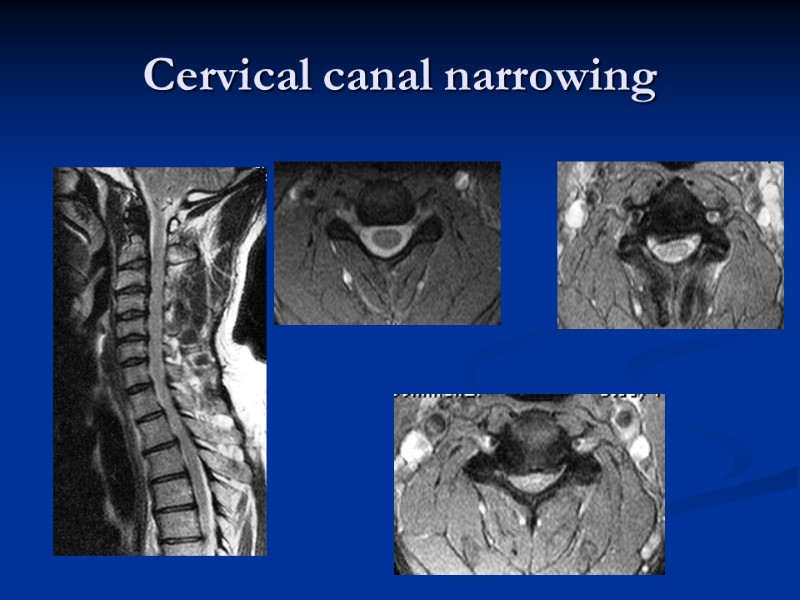
Cervical canal narrowing
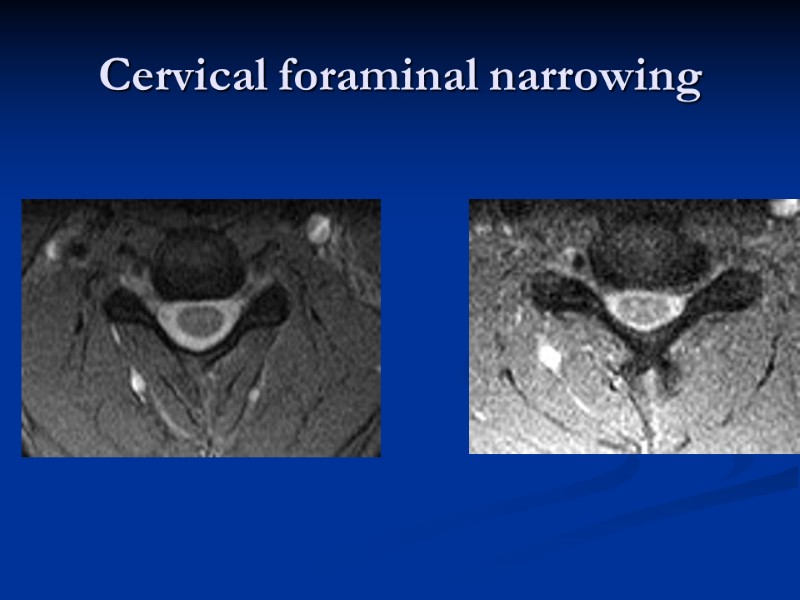
Cervical foraminal narrowing
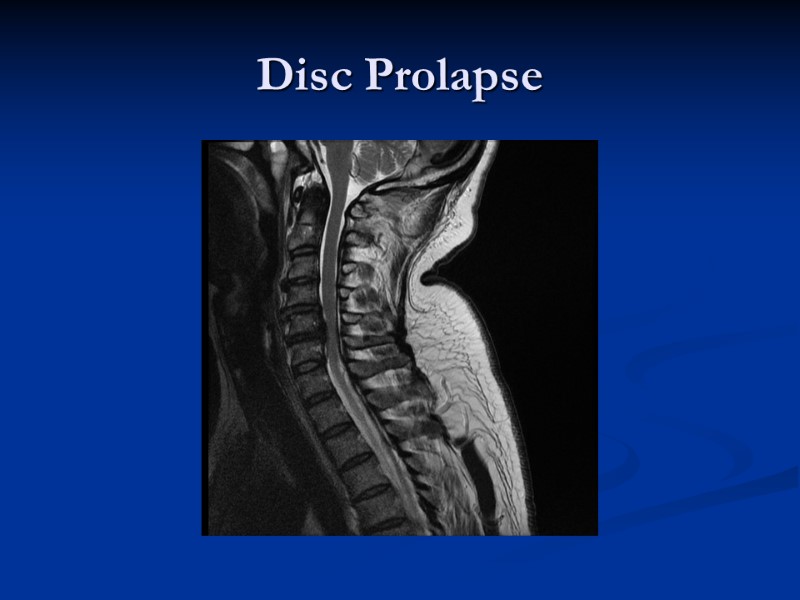
Disc Prolapse
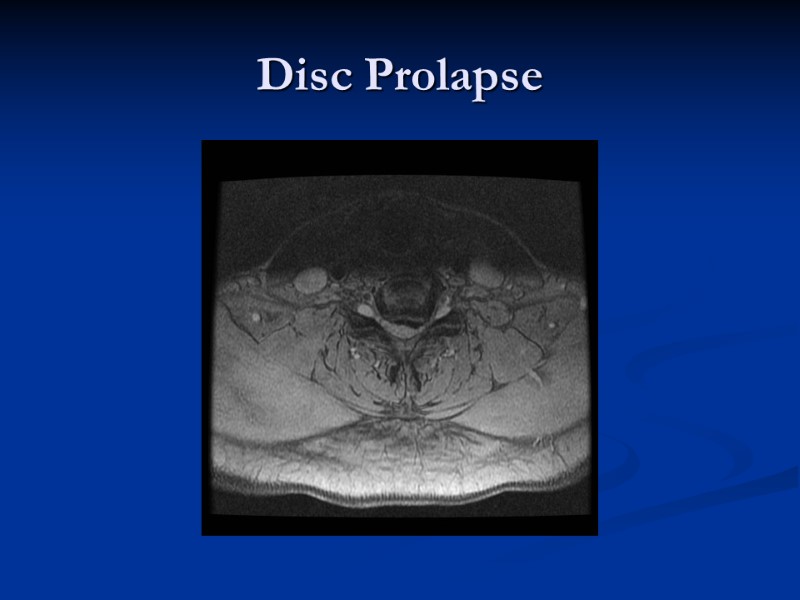
Disc Prolapse
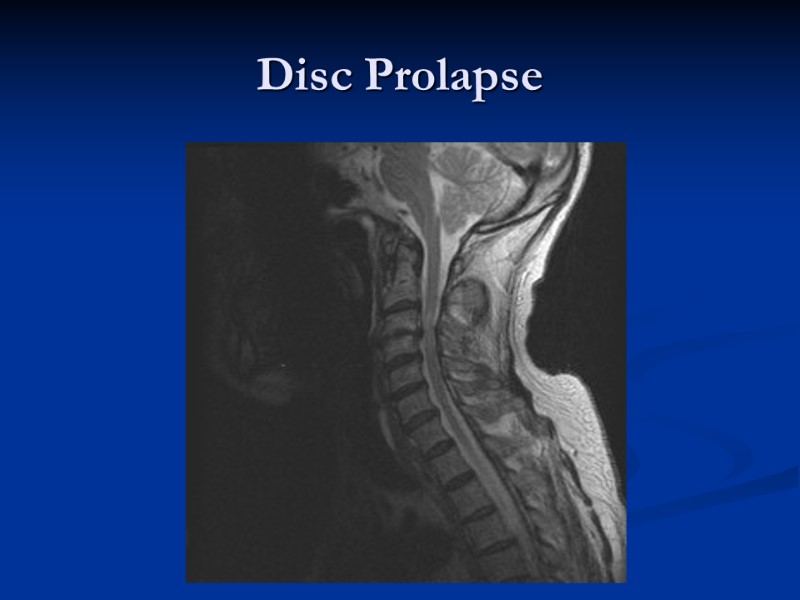
Disc Prolapse
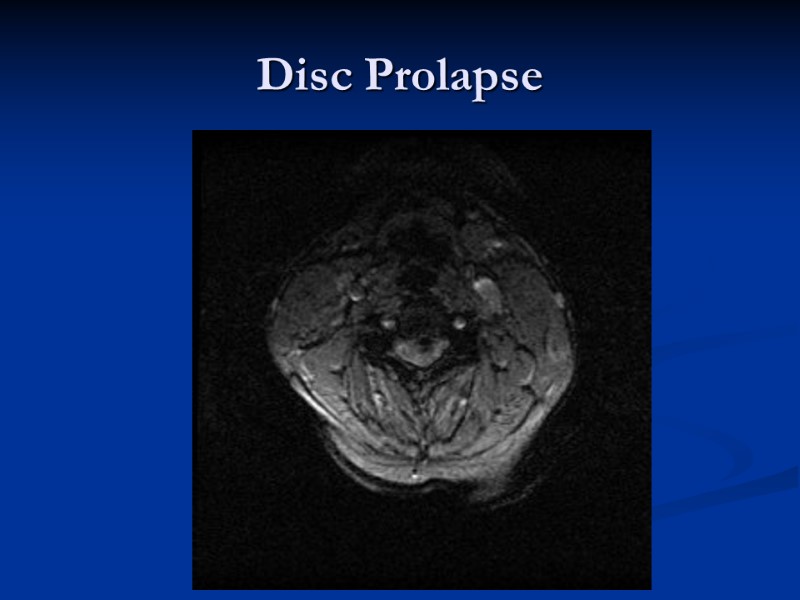
Disc Prolapse
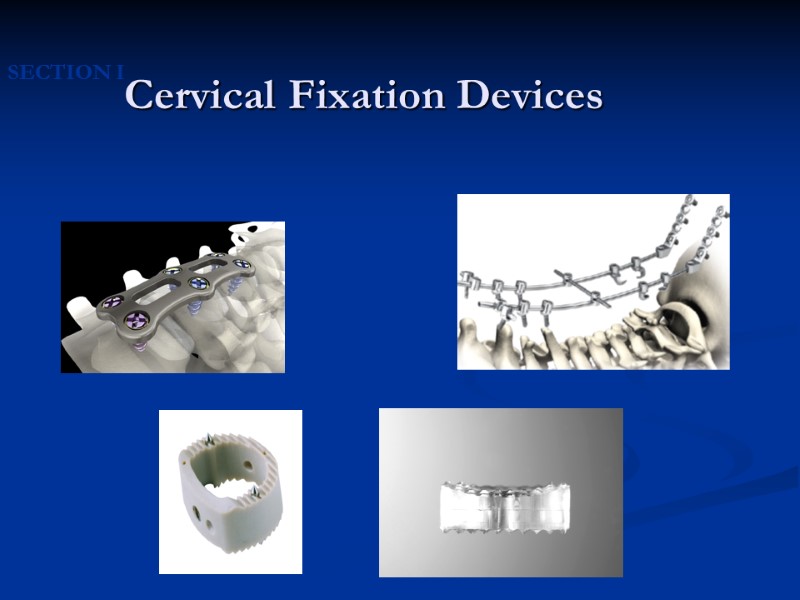
Cervical Fixation Devices SECTION I

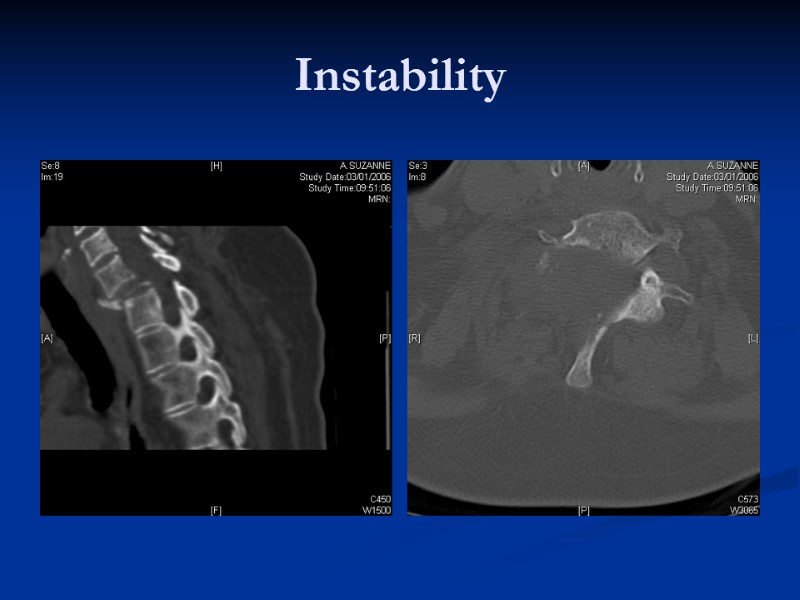
Instability

FlexiCore® Cervical disc replacement
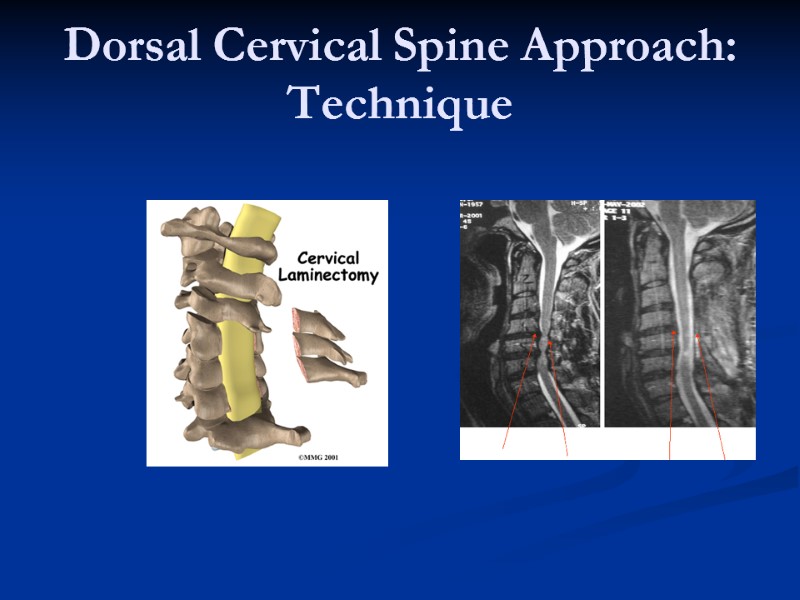
Dorsal Cervical Spine Approach: Technique
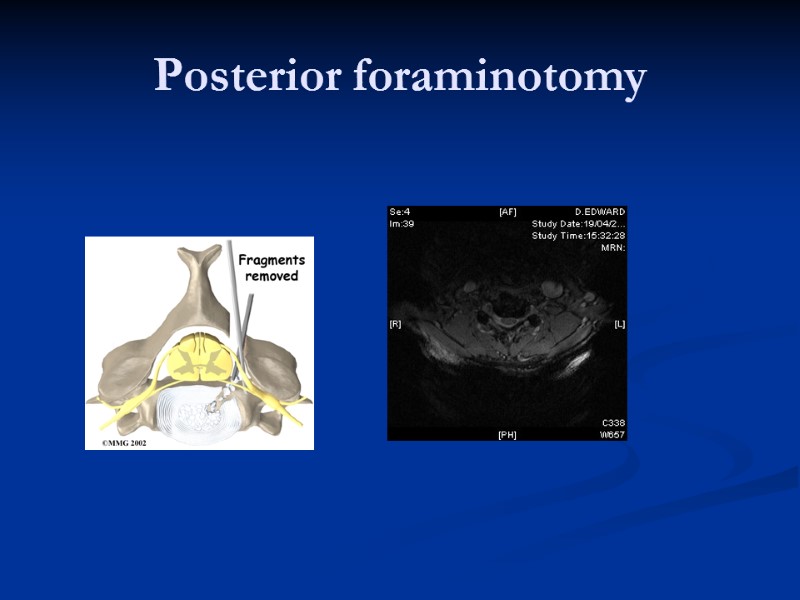
Posterior foraminotomy
KYPHOPLASTY
Minimally Invasive
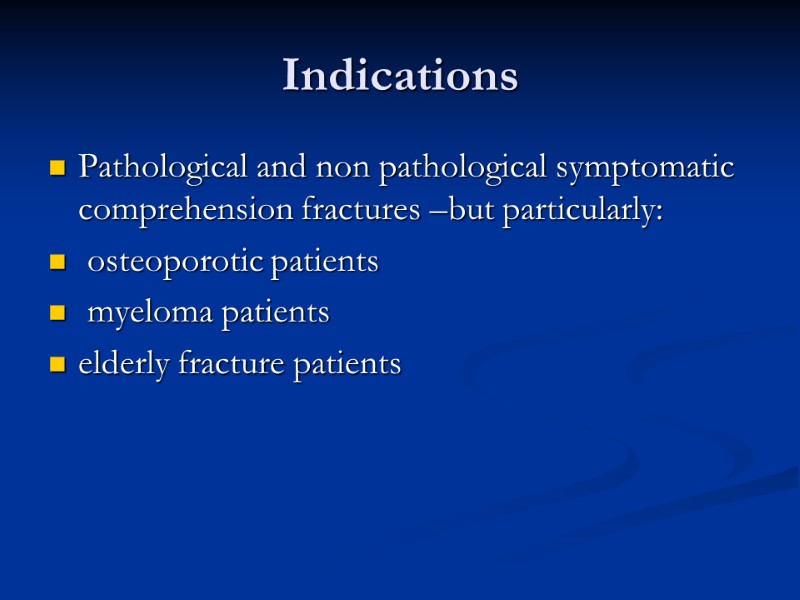
Indications Pathological and non pathological symptomatic comprehension fractures –but particularly: osteoporotic patients myeloma patients elderly fracture patients
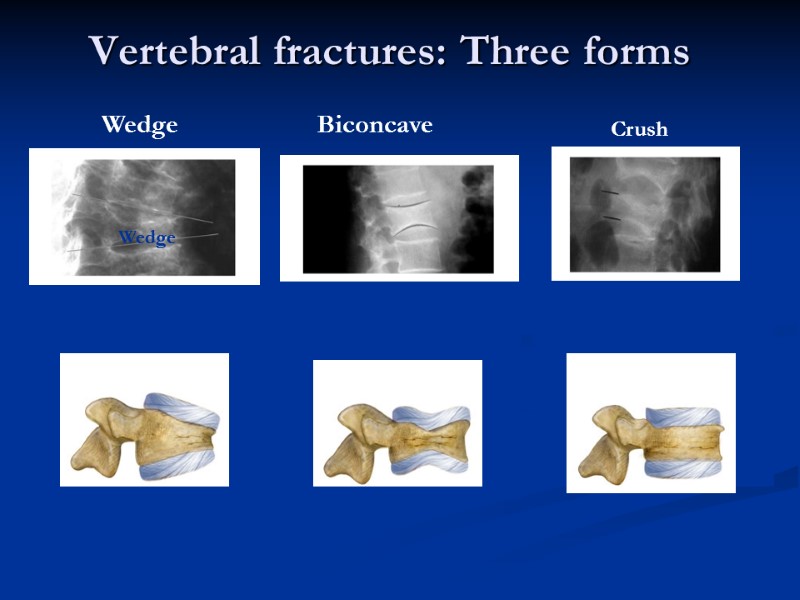
Vertebral fractures: Three forms Wedge Biconcave Crush Wedge
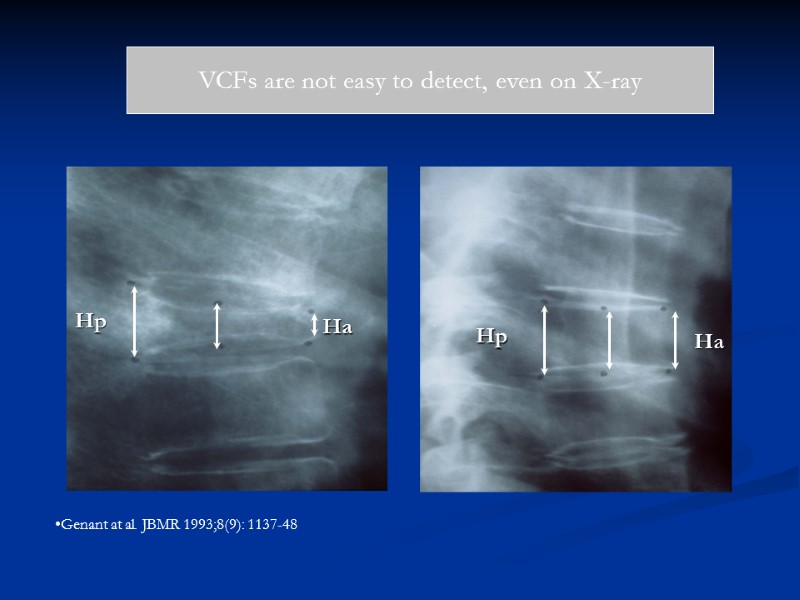
VCFs are not easy to detect, even on X-ray Genant at al. JBMR 1993;8(9): 1137-48
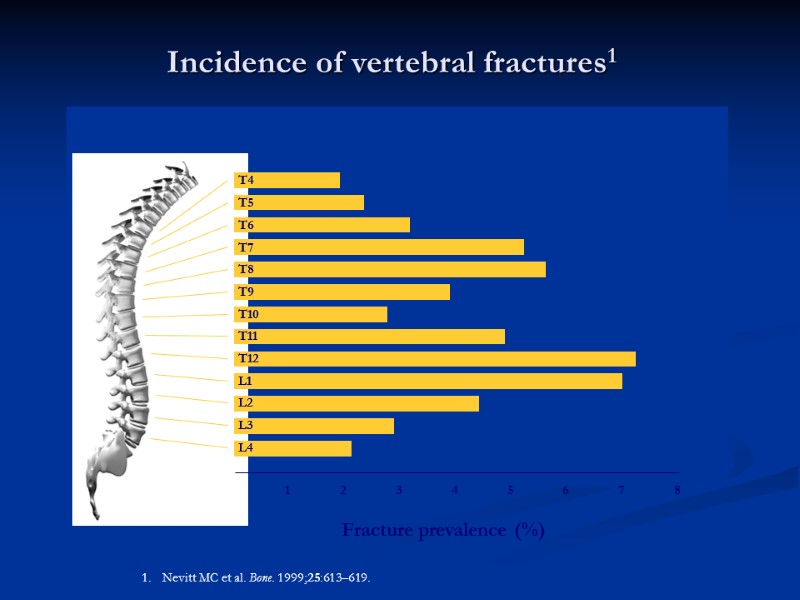
Incidence of vertebral fractures1 1 2 3 4 5 6 7 8 Fracture prevalence (%) Nevitt MC et al. Bone. 1999;25:613–619. T4 T5 T6 T7 T8 T9 T10 T11 T12 L1 L2 L3 L4
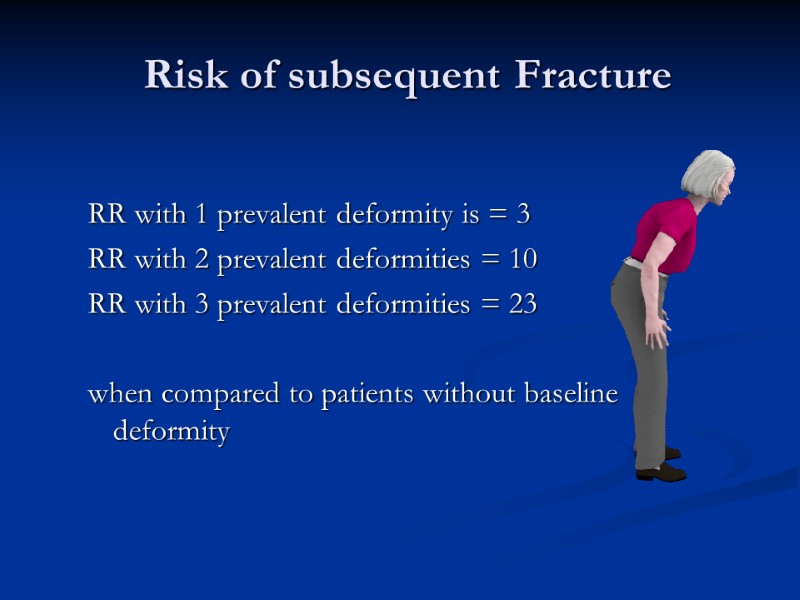
Risk of subsequent Fracture RR with 1 prevalent deformity is = 3 RR with 2 prevalent deformities = 10 RR with 3 prevalent deformities = 23 when compared to patients without baseline deformity
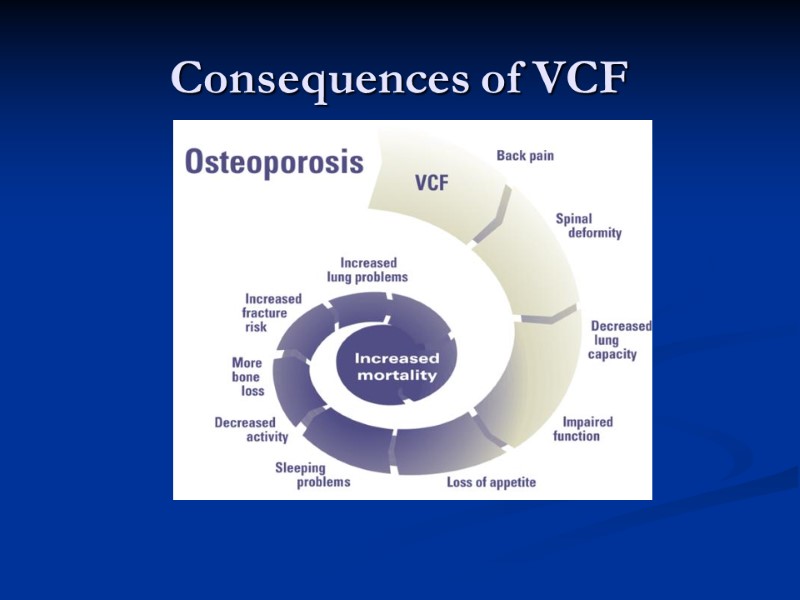
Consequences of VCF
Cost Conservative treatment : Analgesics Bedrest bracing VCF patient :10-20 days in hospital Huge cost for doing nothing! After Balloon Kyphoplasty: Patient will return home after 1 day and needs less analgesics
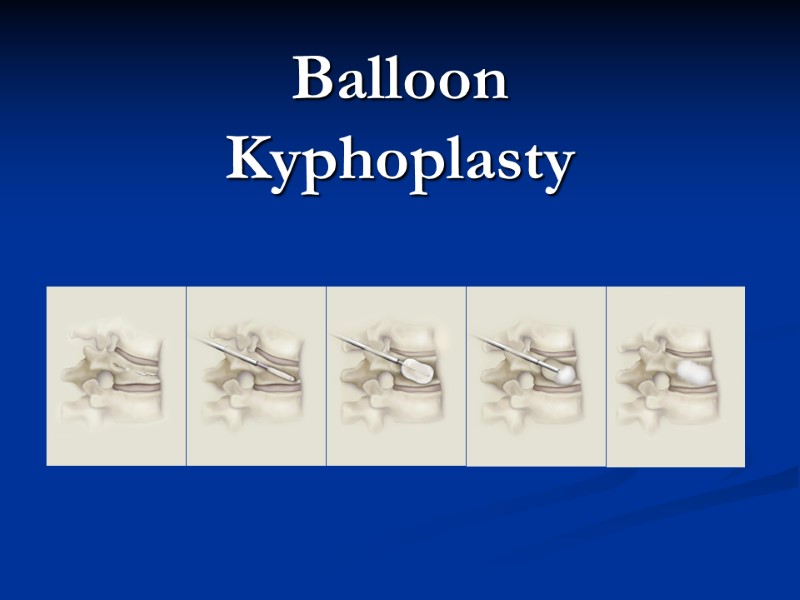
Balloon Kyphoplasty
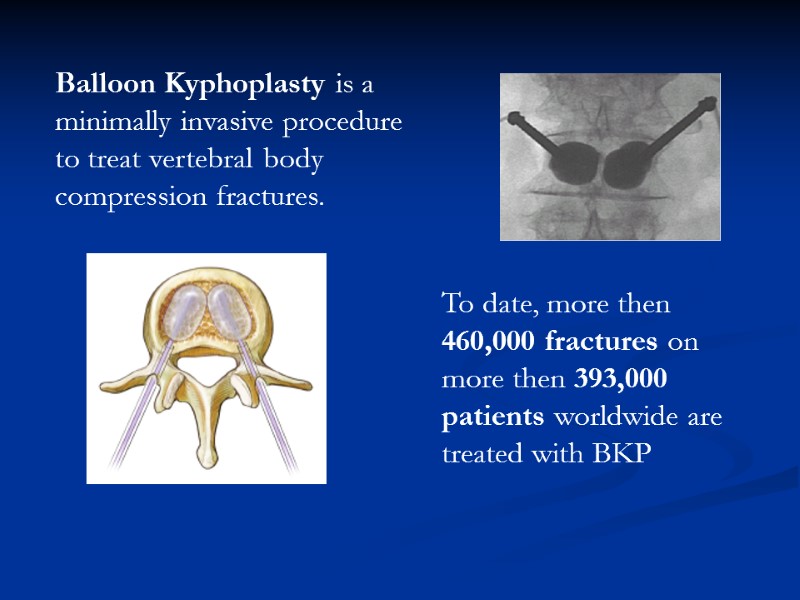
Balloon Kyphoplasty is a minimally invasive procedure to treat vertebral body compression fractures. To date, more then 460,000 fractures on more then 393,000 patients worldwide are treated with BKP
Balloon Kyphoplasty goals The technique is designed to: reduce and stabilise the fracture correct spinal deformity prevent new fractures provide immediate & sustained pain relief and improved quality of life.
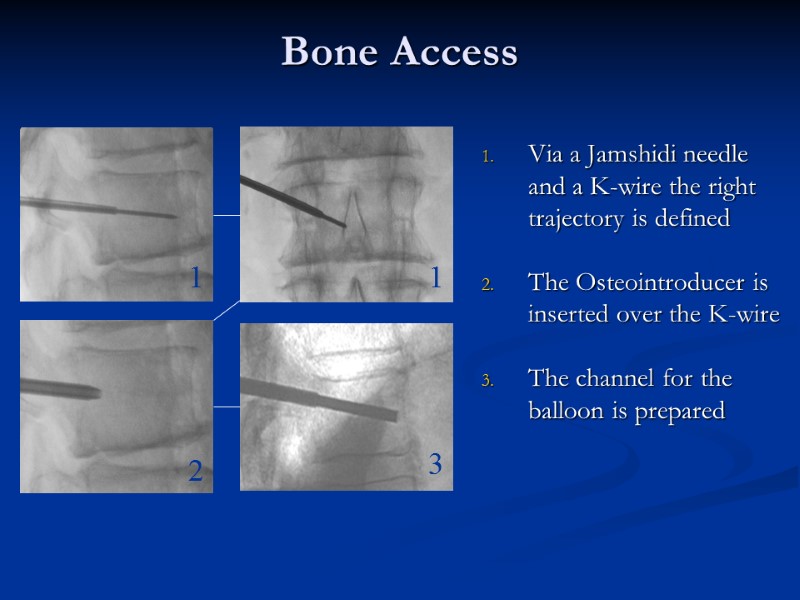
Bone Access Via a Jamshidi needle and a K-wire the right trajectory is defined The Osteointroducer is inserted over the K-wire The channel for the balloon is prepared 1 1 2 3
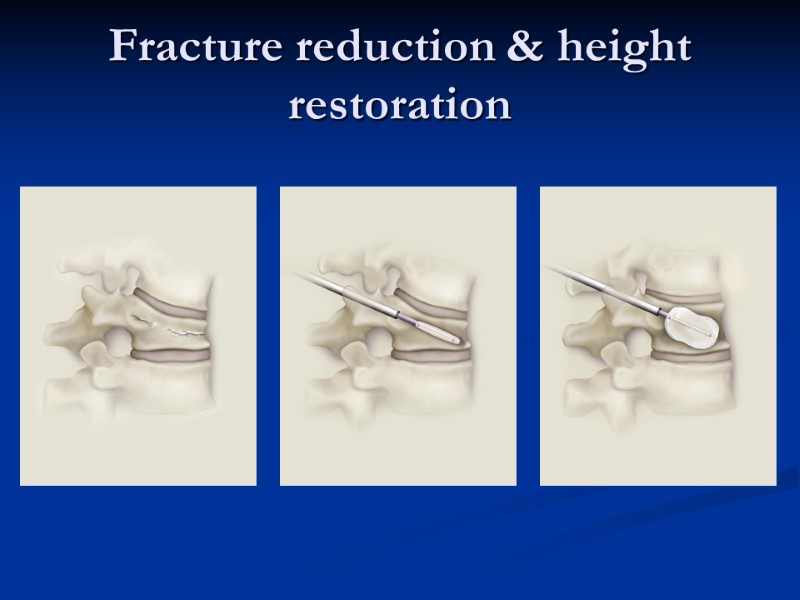
Fracture reduction & height restoration
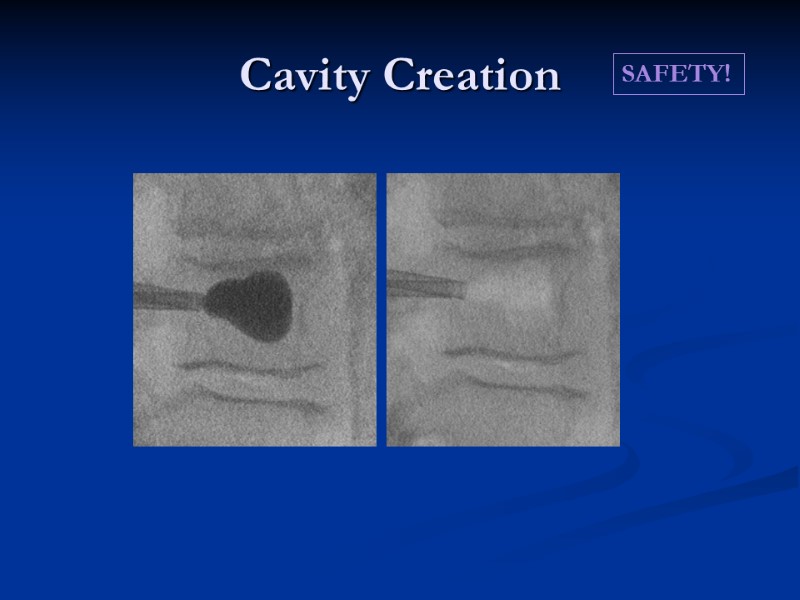
Cavity Creation SAFETY!
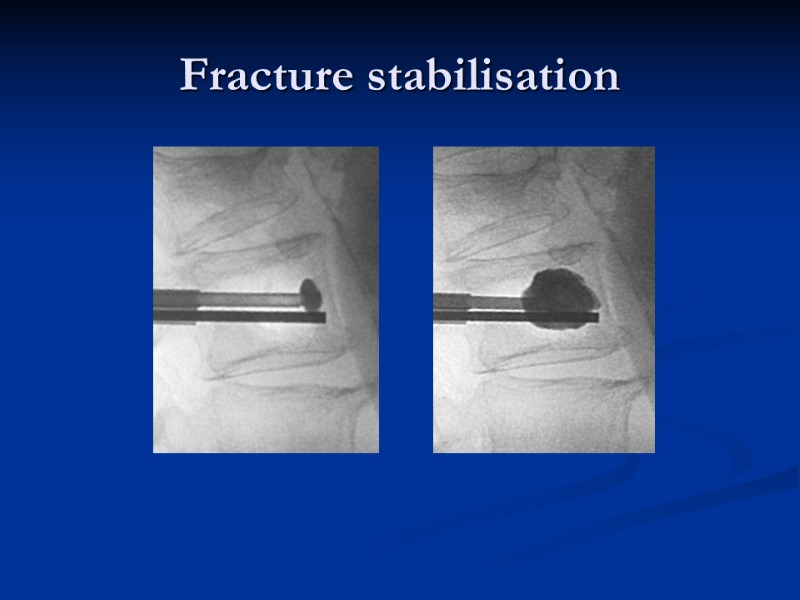
Fracture stabilisation
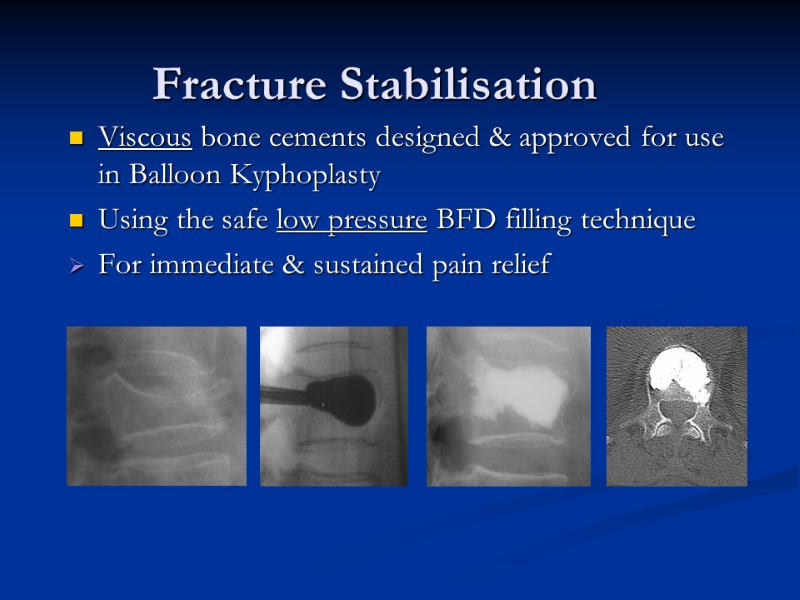
Fracture Stabilisation Viscous bone cements designed & approved for use in Balloon Kyphoplasty Using the safe low pressure BFD filling technique For immediate & sustained pain relief
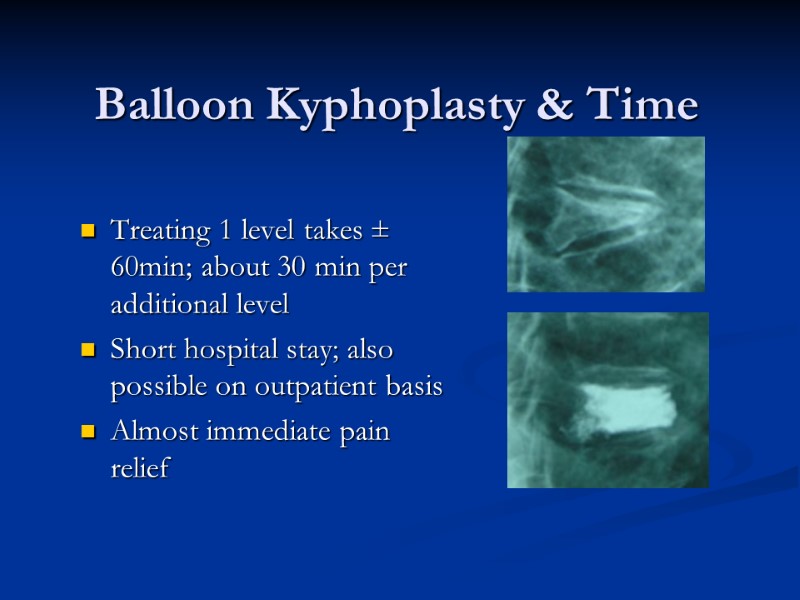
Balloon Kyphoplasty & Time Treating 1 level takes ± 60min; about 30 min per additional level Short hospital stay; also possible on outpatient basis Almost immediate pain relief
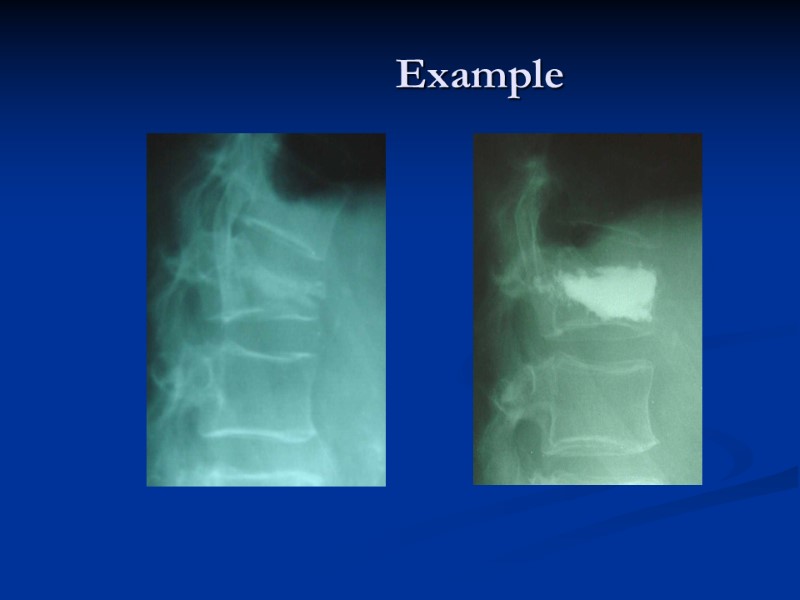
Example
Indications for Balloon Kyphoplasty Painful vertebral compression fractures in the lumbar or thoracic region, due to: Primary osteoporosis Secondary osteoporosis Osteolytic lesions due to multiple myeloma or bone metastasis Trauma
Patient Outcomes Patient Outcomes include: Vertebral body height restoration Angular correction of deformity Significant reduction in pain (95%) Reduced number of days in bed Improved quality of life Improvement in activities of daily living Improvement in mobility High rate of patient satisfaction
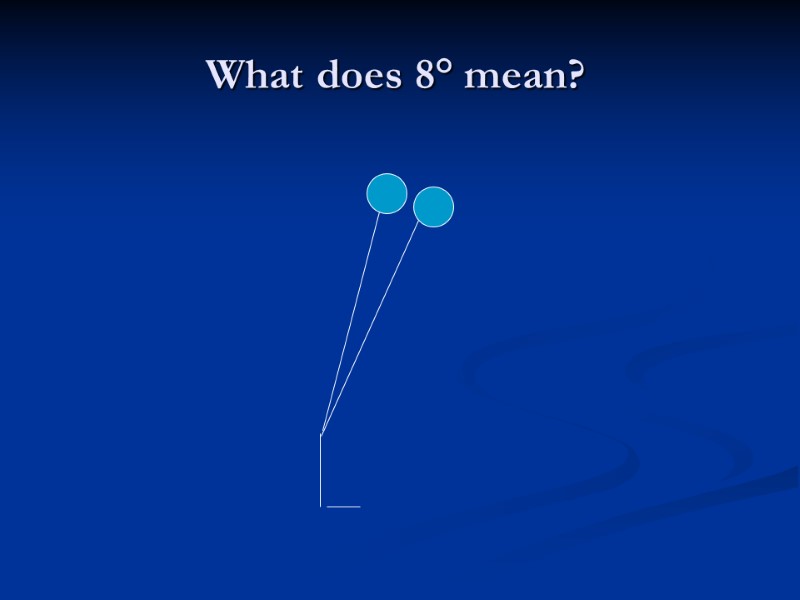
What does 8° mean?
Differences to Vertebroplasty Less safe: Leakage rate complications No height restoration
Focus on Patient Balloon Kyphoplasty offers patients with painful VCF Immediate and sustained pain relief 75% of patients discard narcotic medication Return to a fully active life, functioning without pain Short hospital stay/ day case surgery All these factors will give a significant improvement in Quality Of Life
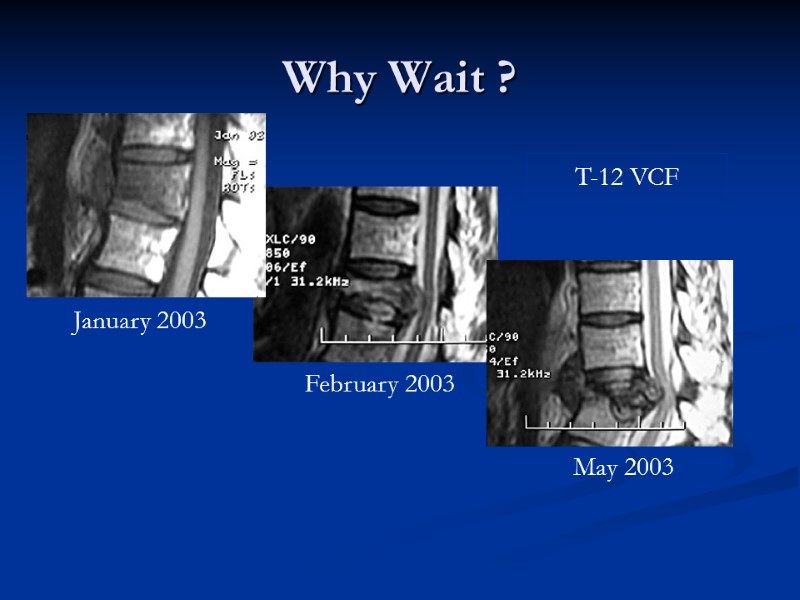
Why Wait ? T-12 VCF January 2003 February 2003 May 2003
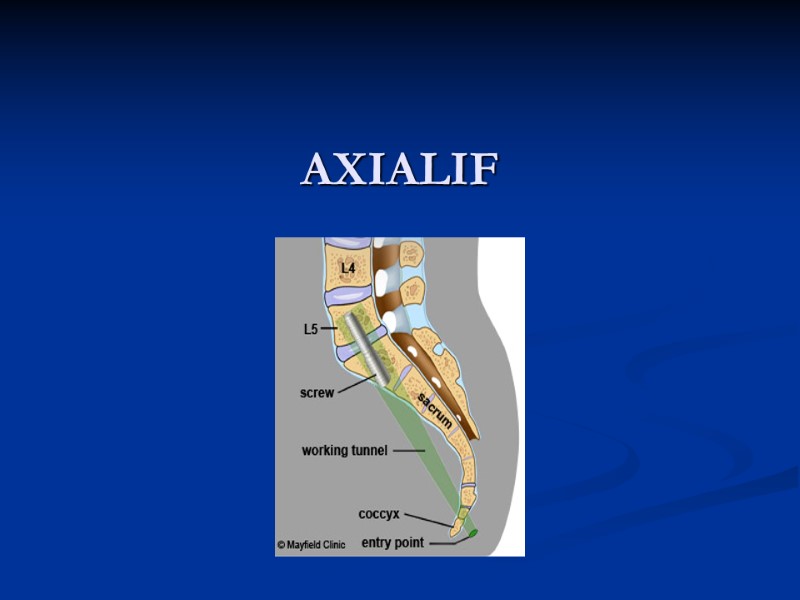
AXIALIF
Axialif Minimally Invasive Anterior Lumbar Interbody Fusion 1cm parasacral incision Working Channel Daycase Surgery
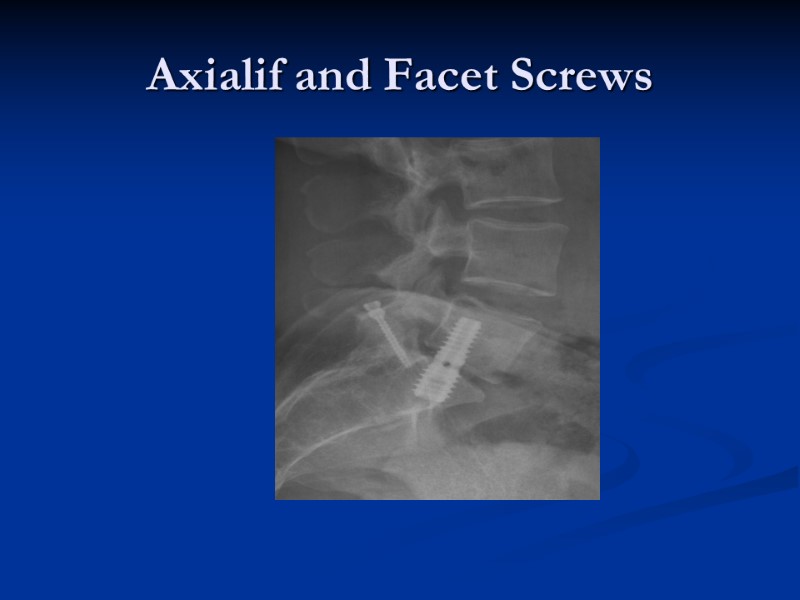
Axialif and Facet Screws
Axialif
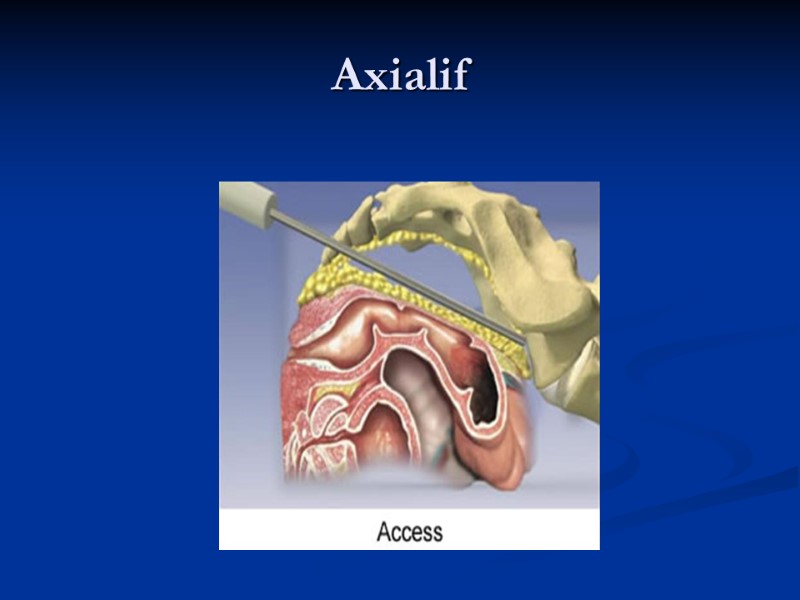
Axialif
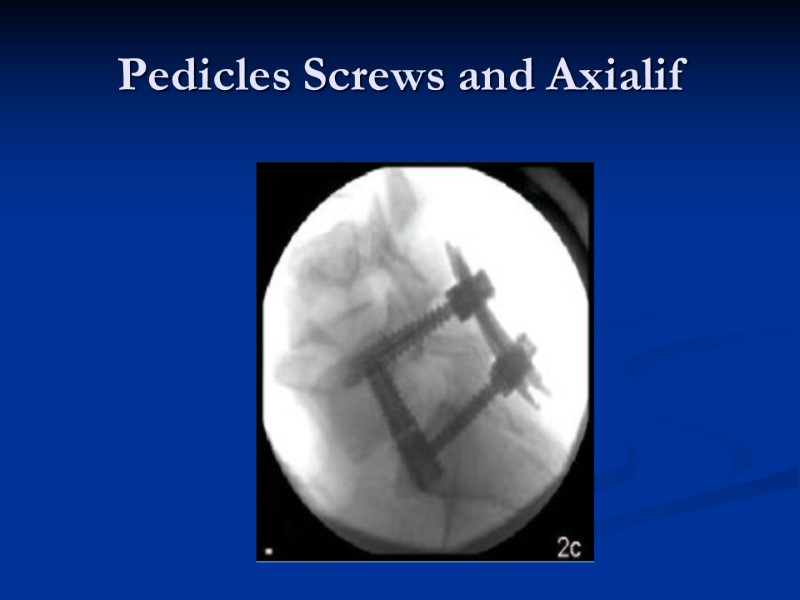
Pedicles Screws and Axialif
Thankyou
6764-spine_and_kyphoplasty_ashtead.ppt
- Количество слайдов: 77

