Spine and kyphoplasty Ashtead.ppt
- Количество слайдов: 77
Spine Anne Mitchener Consultant Neurosurgeon
Back Pain-theory Disc degeneration Micro instability Joint hypertrophy Ligamentous hypertrophy

Back pain-syndromes Disc dehydration Disc prolapse Facet joint pain Canal stenosis Foraminal stenosis Spondylolisthesis Scoliosis
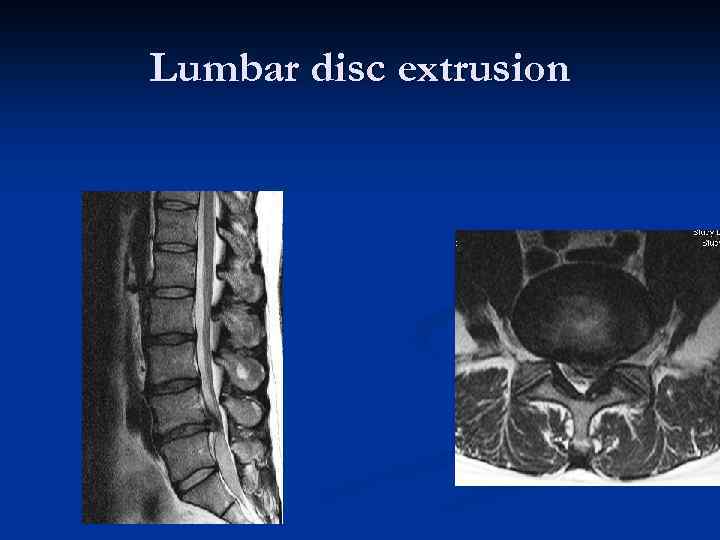
Lumbar disc extrusion
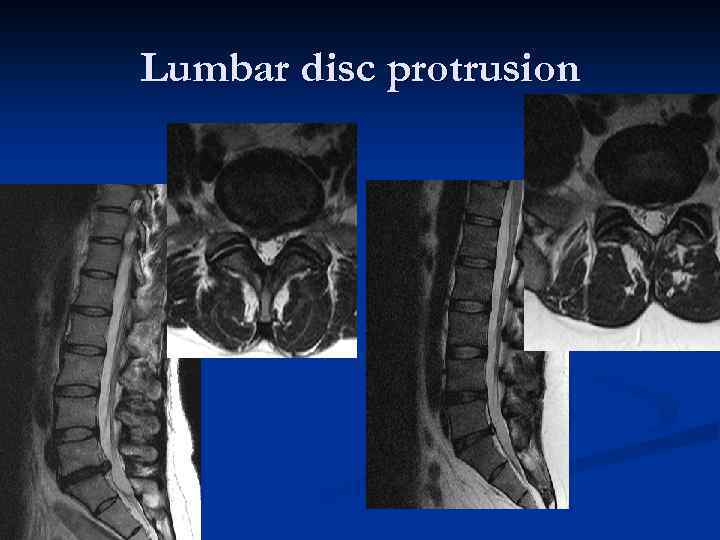
Lumbar disc protrusion
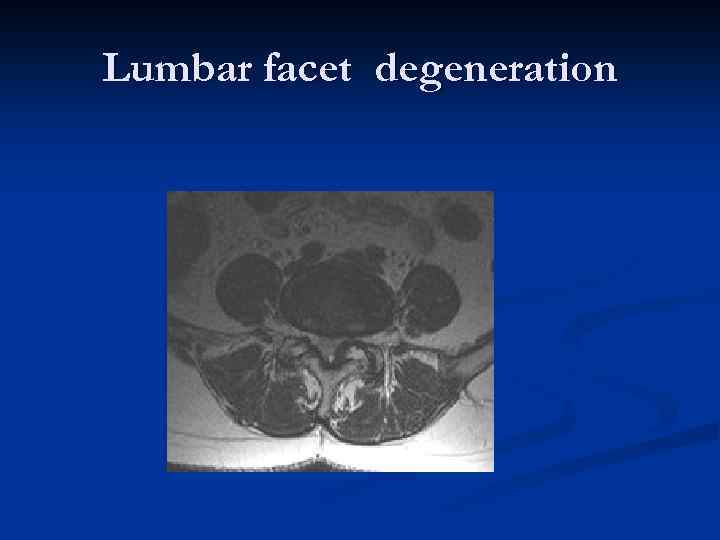
Lumbar facet degeneration
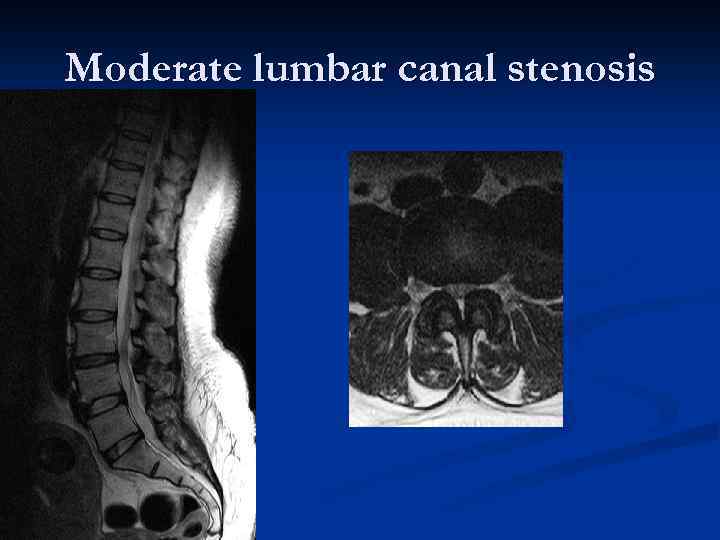
Moderate lumbar canal stenosis

Severe lumbar canal stenosis
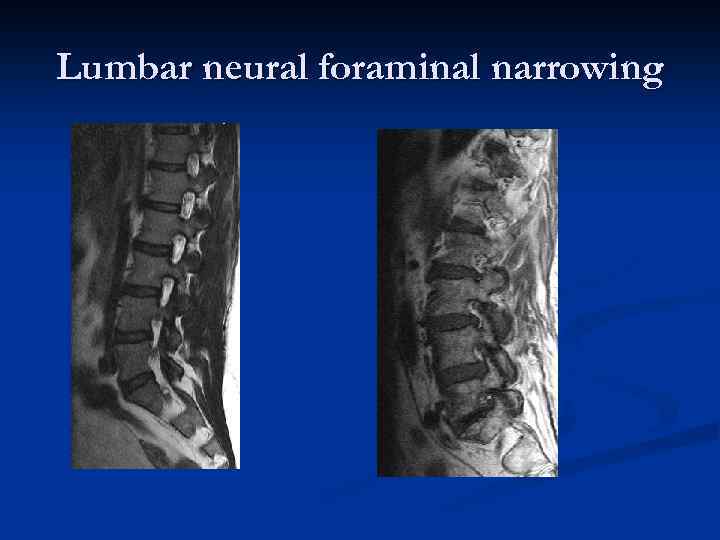
Lumbar neural foraminal narrowing

Degenerative spondylolisthesis
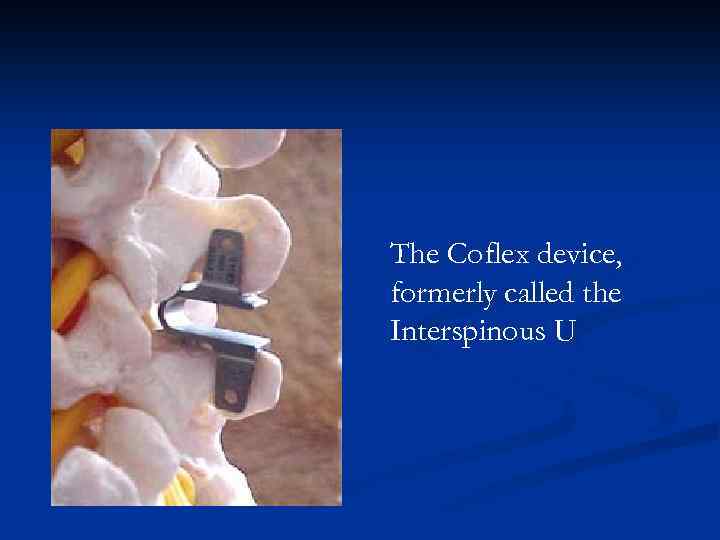
The Coflex device, formerly called the Interspinous U
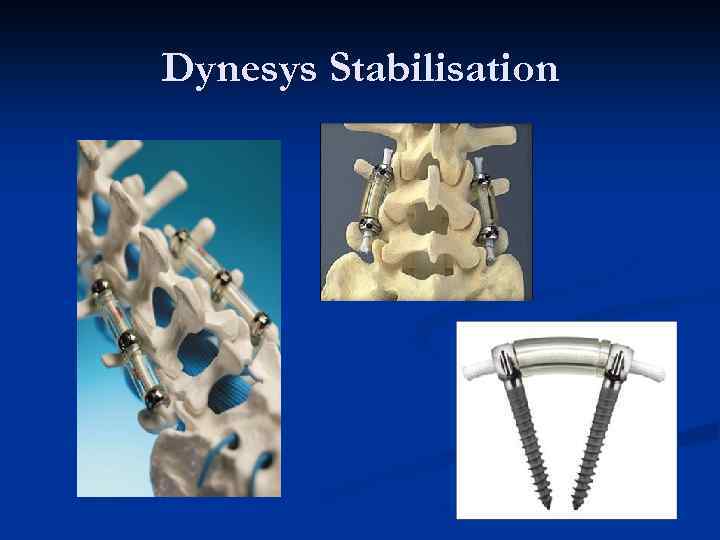
Dynesys Stabilisation

Fusion-titanium vs peek
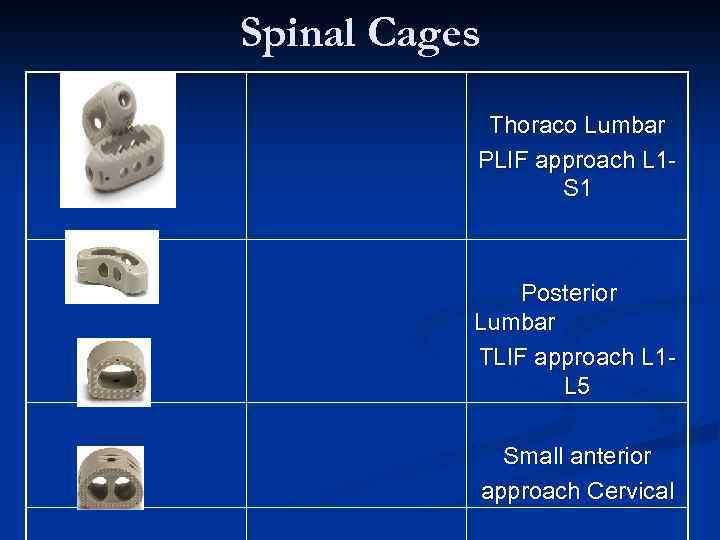
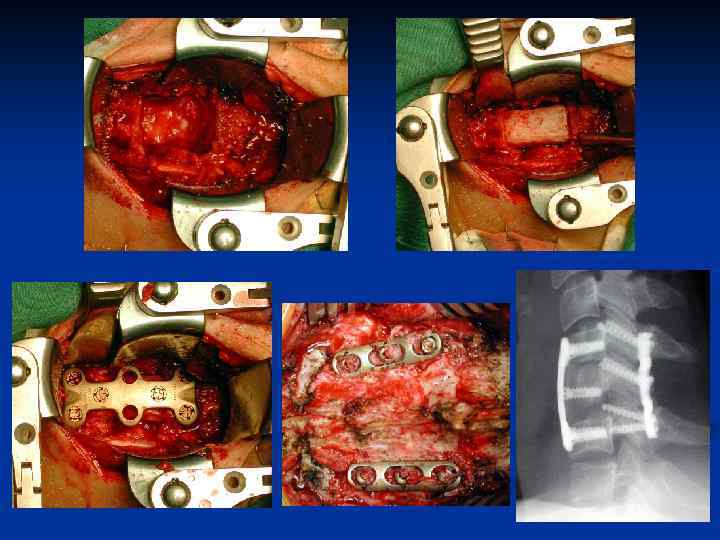
Spinal Cages Thoraco Lumbar PLIF approach L 1 S 1 Posterior Lumbar TLIF approach L 1 L 5 Small anterior approach Cervical
Low Back Pain n Clinical advantages of Spine Arthroplasty: n n n Reduced pain Improved patient recovery times Reduce adjacent segment disease, which occurs in approximately 3050% of today’s rigid fusions Restore and maintain disc height Preserve motion segment Ensure proper facet loading

Disc replacement

Distractible In-situ VBR System
Back pain If the patient appears to be a candidate for intervention consider referral. . . There are many and varied treatment options to be tailored to needs.
Cervical degenerative spine disorders Mrs Anne Mitchener Consultant Neurosurgeon
Cervical Degenerative Disease n Cervical Disc Herniation-protrusion/extrusion of nucleus pulposus-”acute” n Cervical Spondylosis-involves osteophyte formation-”chronic”
Cervical Degenerative Disease Occurs when flexion, extension , rotation or lateral flexion exceeds the strength of the disc annulus and anterior and posterior ligaments n Posterior ligament weak laterally herniations and radiculopathy more common than myelopathy. n Pain, motor, sensory and reflex deficits occur. n Commonest levels C 5/6 and C 6/7 n
Cervical degenerative Disease Myelopathy results from central cervical disc herniation n Complete or commonly incomplete clinically n Segmental damage at the cord level and long tract signs below. n
Cervical Spondylosis Age related progressive changes on imaging n 50% over 50 years and 75% over 65 years show spondylosis n Few develop functional neurological deficits of radiculopathy/myelopathy n
Myelopathic Symptoms Impaired coordination of hands n Gait abnormality-weakness/ataxia n Cervicobrachalgia n Spasticity, para/tetraparesis n Autonomic disturbance such as micturition n L’Hermittes Sign n
Cervical Spondylosis Discs degenerate, loss of water and disc height n Micro movement postulated n Clear instability rarely demonstrated n Facet joints and ligaments hypertrophy bone grows over herniated disc-osteophyte n Canal/foramen narrowsmyelopathy/radiculopathy can result n
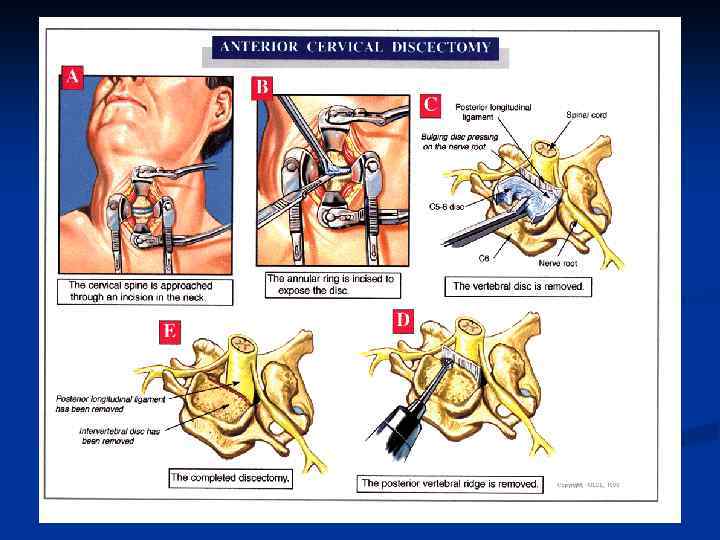
Surgical approaches Posterior surgical approach began with Sir victor Horsley in 1895 -laminectomy /foraminotomy n Anterior approach began in 1958 was developed by Cloward-discectomy and fusion n
Results Posterior Approach Laminectomy can lead to instability and incomplete decompression-less reliable n Foraminotomy can have excellent results for radiculopathy n
Results Anterior Approaches Radiculopathy 75 -90% excellent recovery n Myelopathy 85% marked improvement-depends on severity, performed to prevent deterioration n

Cervical spine sagittal midline MR images
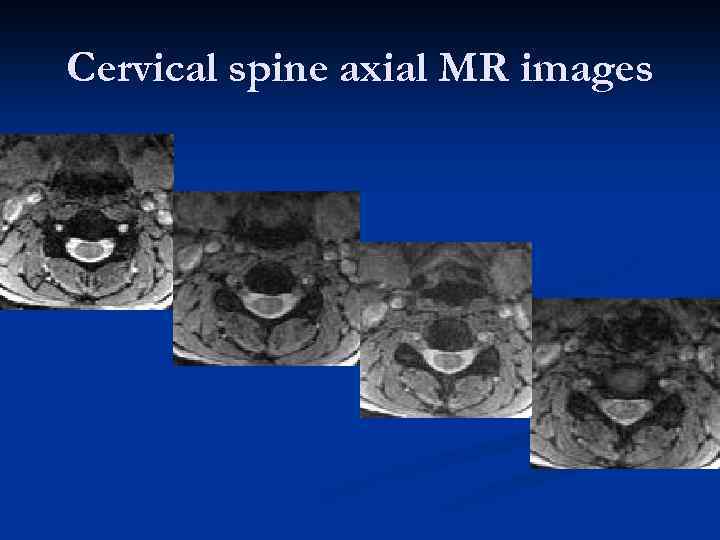
Cervical spine axial MR images
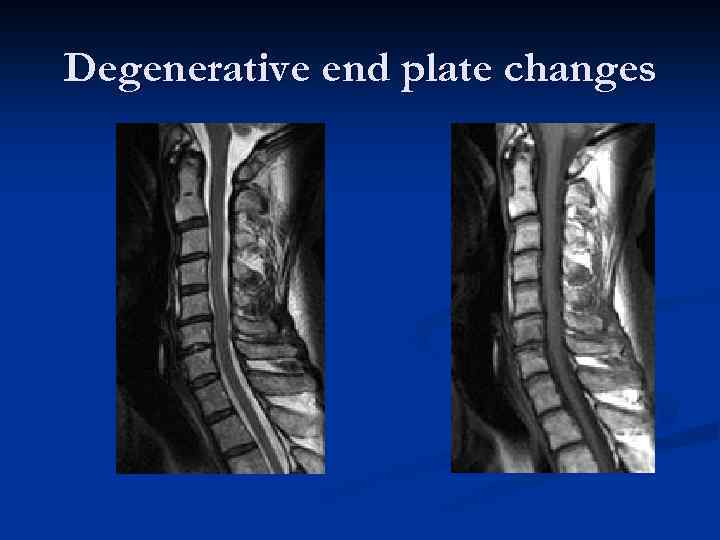
Degenerative end plate changes
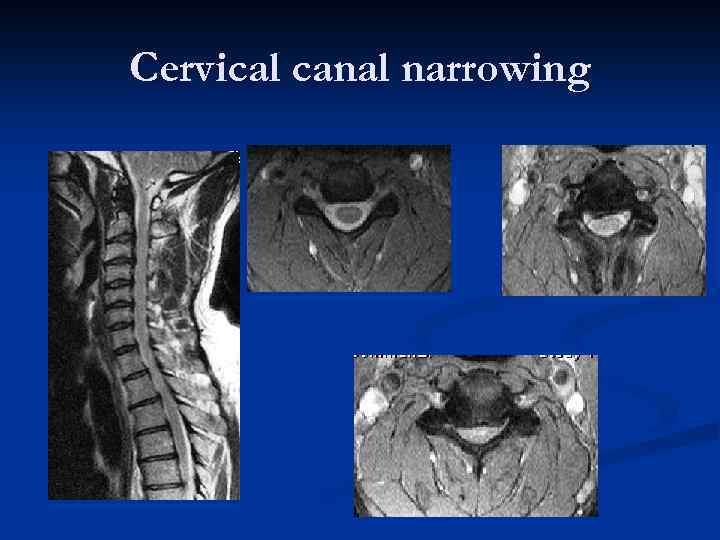
Cervical canal narrowing
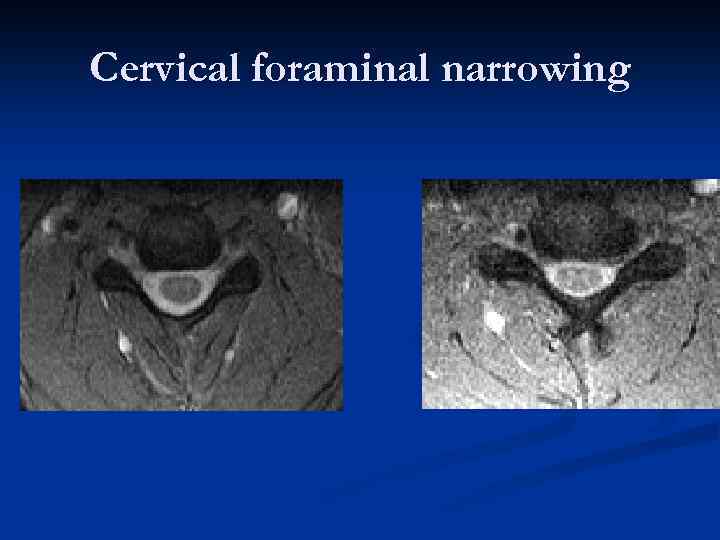
Cervical foraminal narrowing
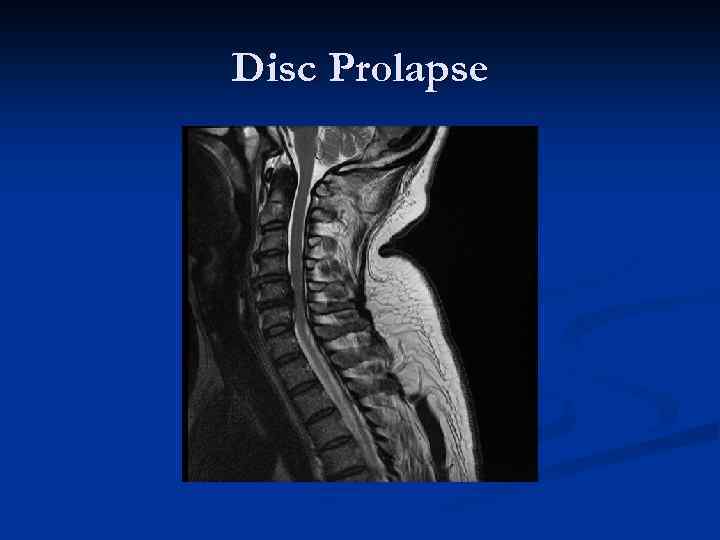
Disc Prolapse
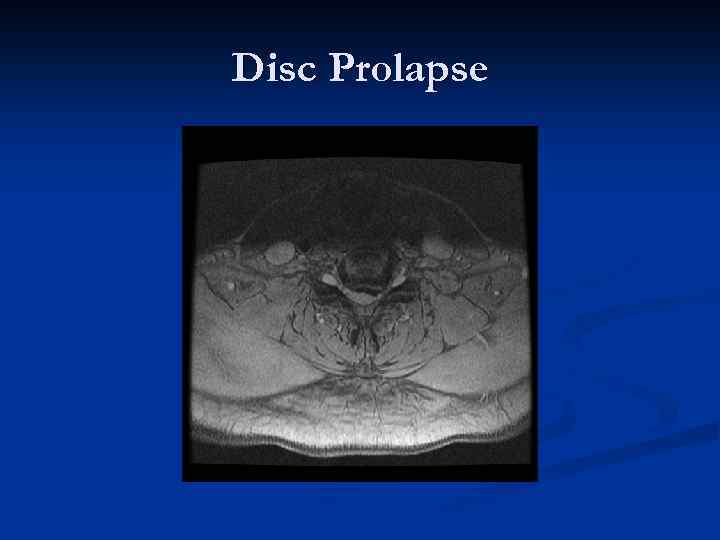
Disc Prolapse
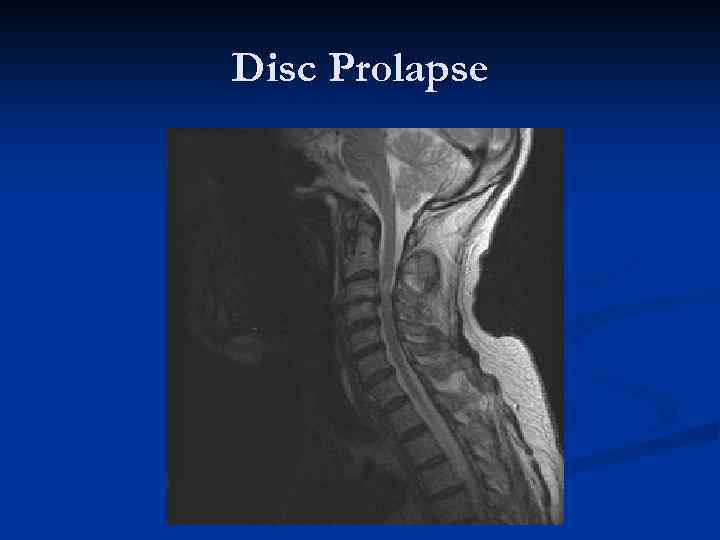
Disc Prolapse
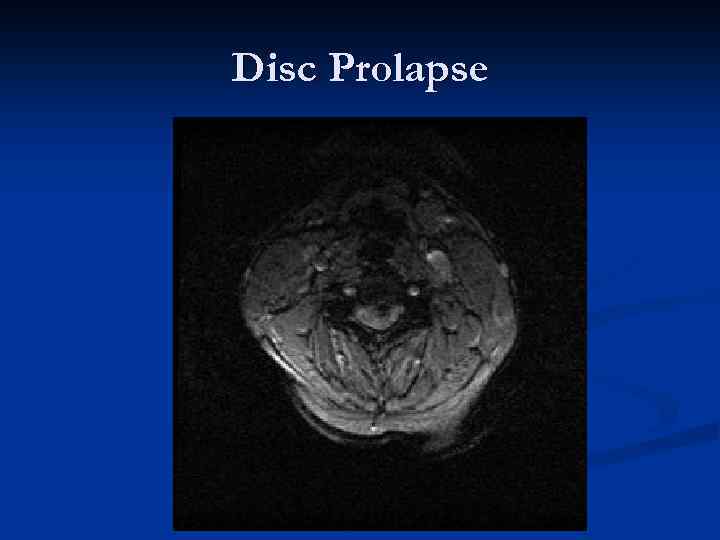
Disc Prolapse
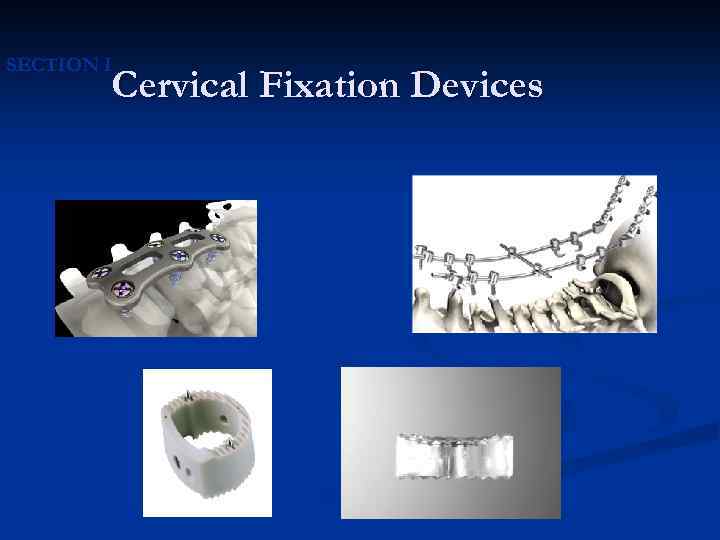
SECTION I Cervical Fixation Devices
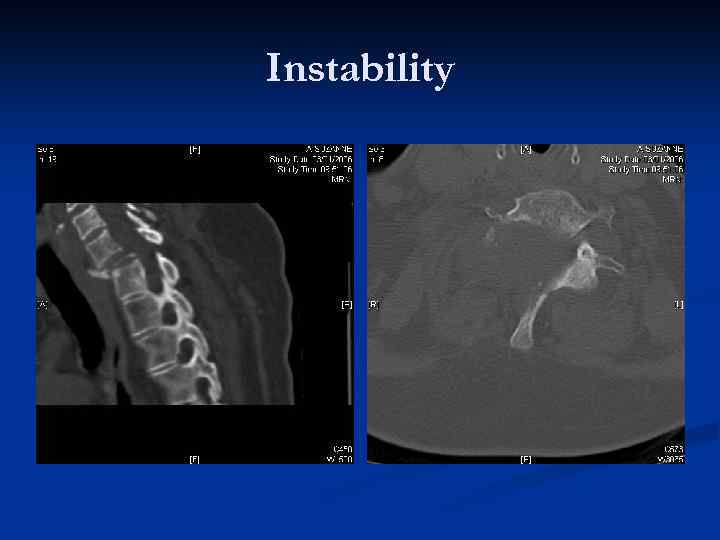
Instability

Cervical disc replacement Flexi. Core®
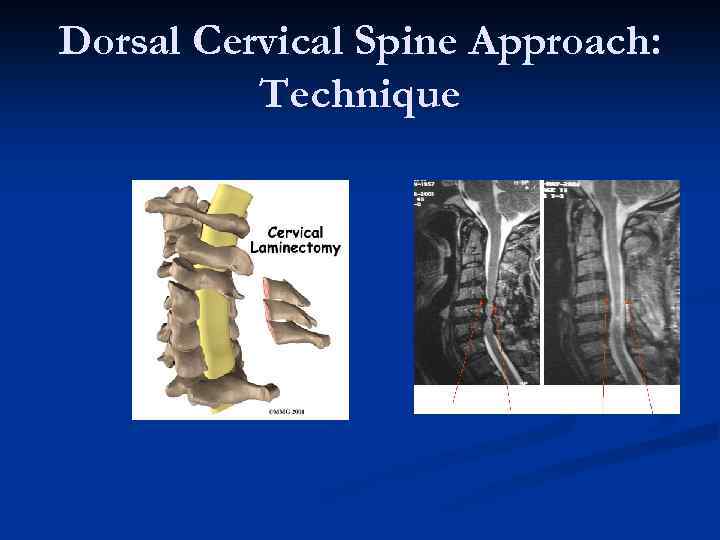
Dorsal Cervical Spine Approach: Technique
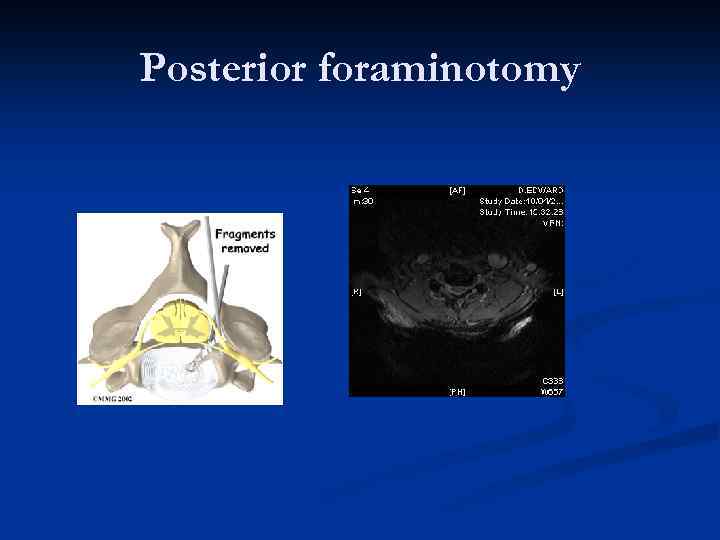
Posterior foraminotomy
KYPHOPLASTY
Minimally Invasive
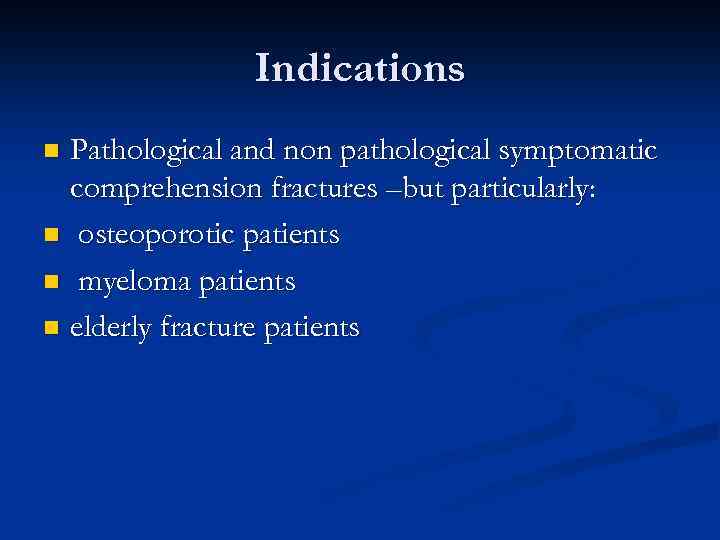
Indications Pathological and non pathological symptomatic comprehension fractures –but particularly: n osteoporotic patients n myeloma patients n elderly fracture patients n
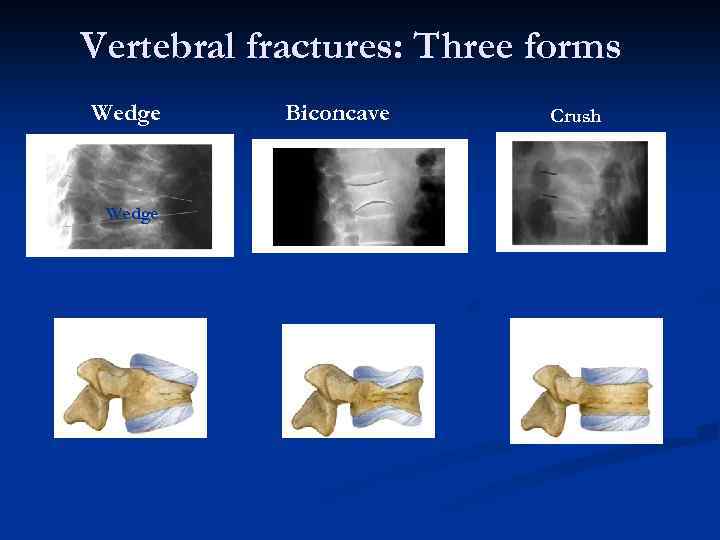
Vertebral fractures: Three forms Wedge Biconcave Crush
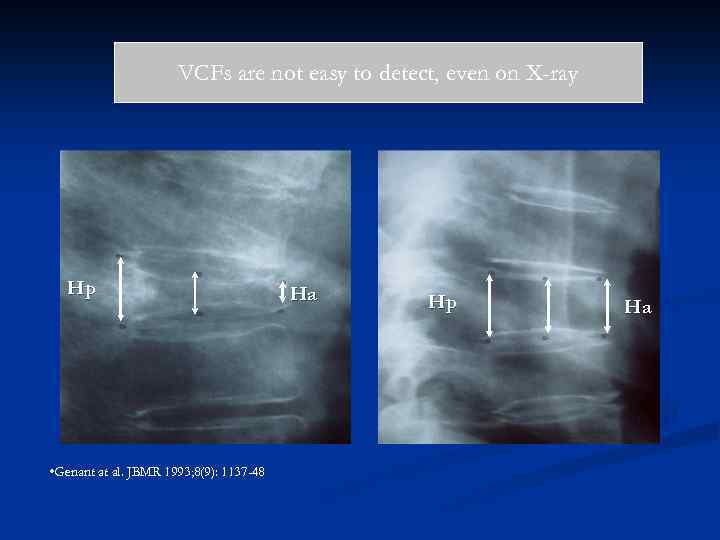
VCFs are not easy to detect, even on X-ray Hp • Genant at al. JBMR 1993; 8(9): 1137 -48 Ha Hp Ha
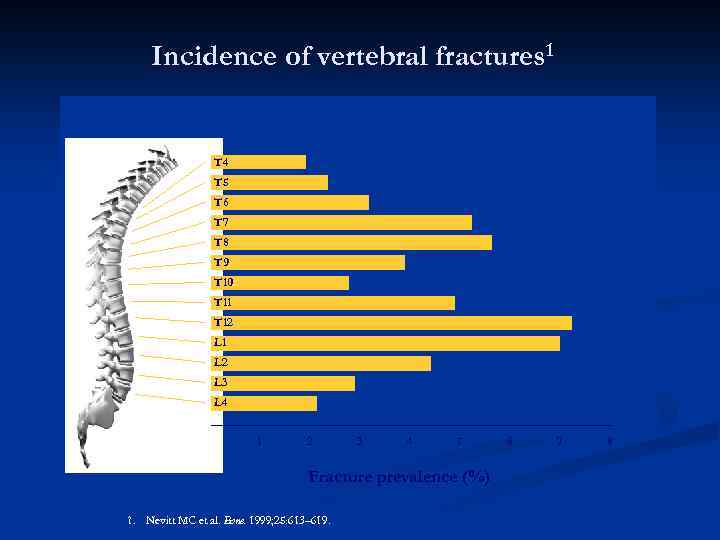
Incidence of vertebral fractures 1 T 4 T 5 T 6 T 7 T 8 T 9 T 10 T 11 T 12 L 1 L 2 L 3 L 4 1 2 3 4 5 Fracture prevalence (%) 1. Nevitt MC et al. Bone. 1999; 25: 613– 619. 6 7 8
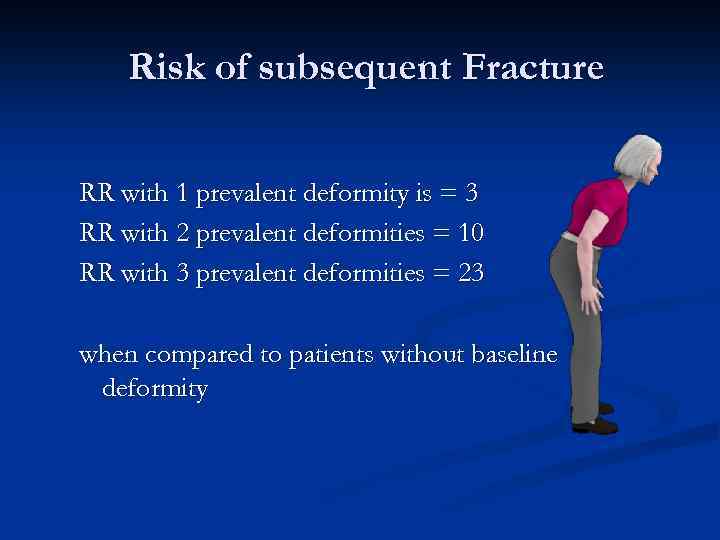
Risk of subsequent Fracture RR with 1 prevalent deformity is = 3 RR with 2 prevalent deformities = 10 RR with 3 prevalent deformities = 23 when compared to patients without baseline deformity
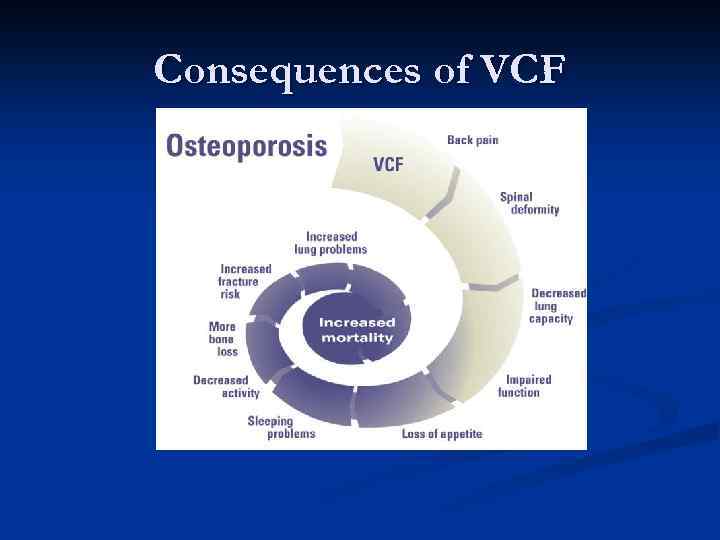
Consequences of VCF
Cost n Conservative treatment : n n n Analgesics Bedrest bracing VCF patient : 10 -20 days in hospital Huge cost for doing nothing! After Balloon Kyphoplasty: Patient will return home after 1 day and needs less analgesics
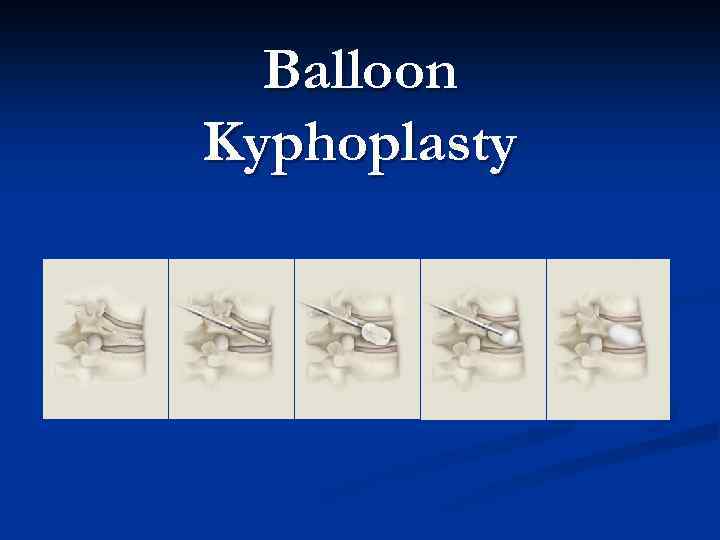
Balloon Kyphoplasty
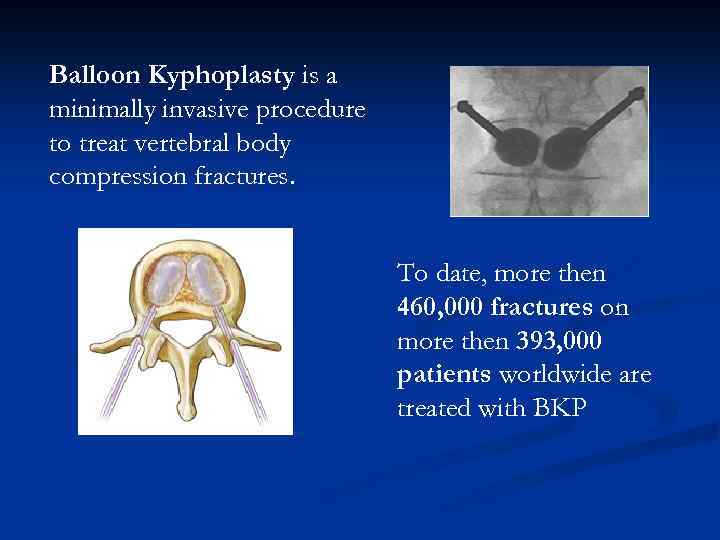
Balloon Kyphoplasty is a minimally invasive procedure to treat vertebral body compression fractures. To date, more then 460, 000 fractures on more then 393, 000 patients worldwide are treated with BKP
Balloon Kyphoplasty goals The technique is designed to: n n reduce and stabilise the fracture correct spinal deformity prevent new fractures provide immediate & sustained pain relief and improved quality of life.
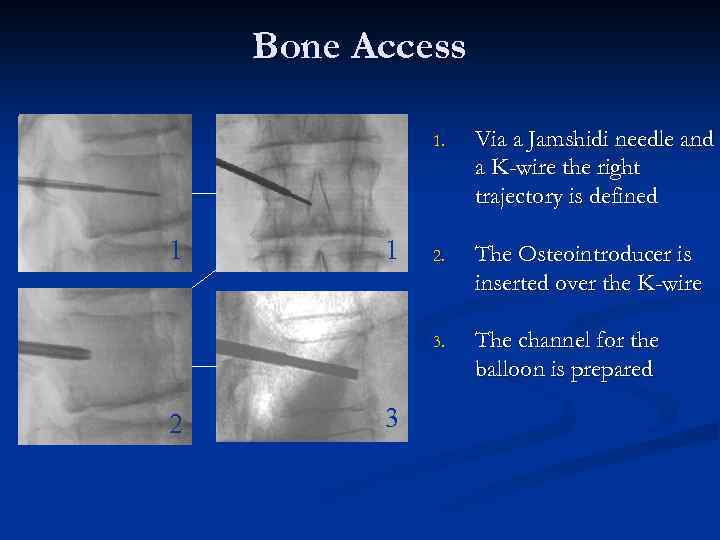
Bone Access 1. 2 1 3 2. The Osteointroducer is inserted over the K-wire 3. 1 Via a Jamshidi needle and a K-wire the right trajectory is defined The channel for the balloon is prepared
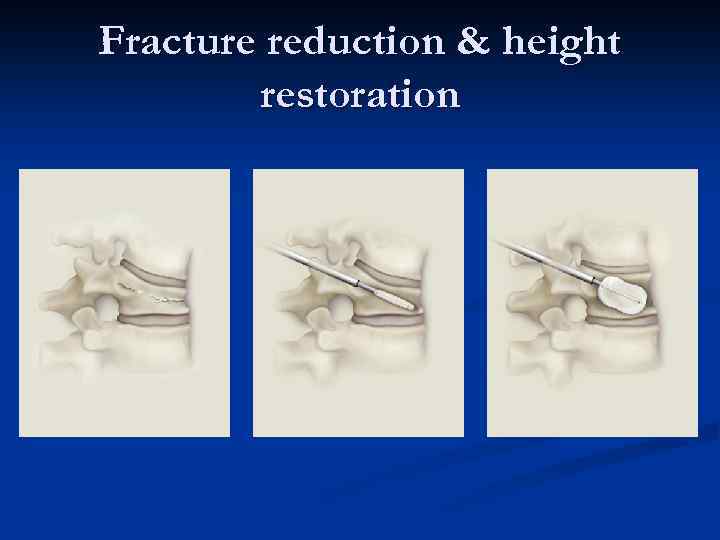
Fracture reduction & height restoration
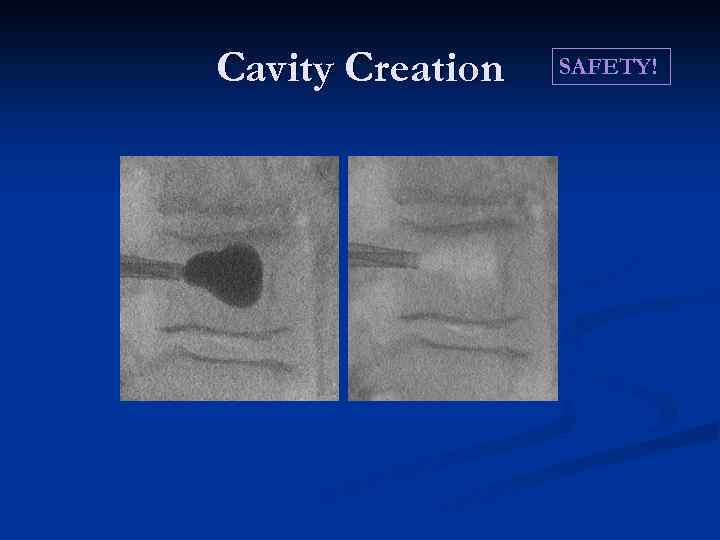
Cavity Creation SAFETY!
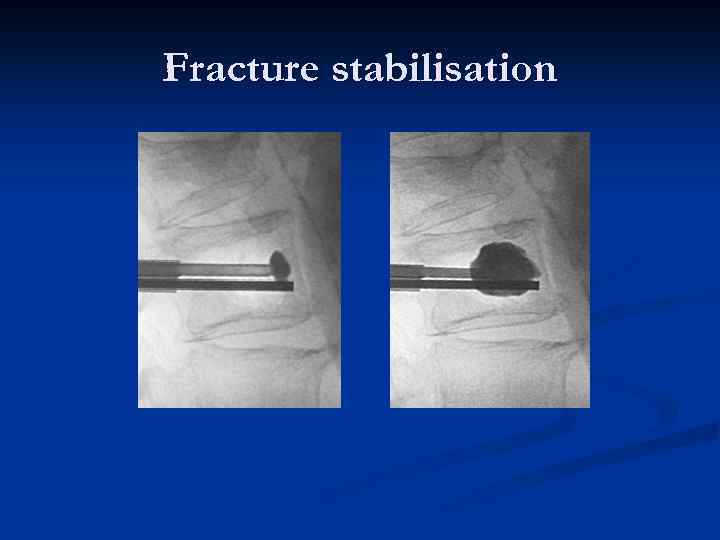
Fracture stabilisation
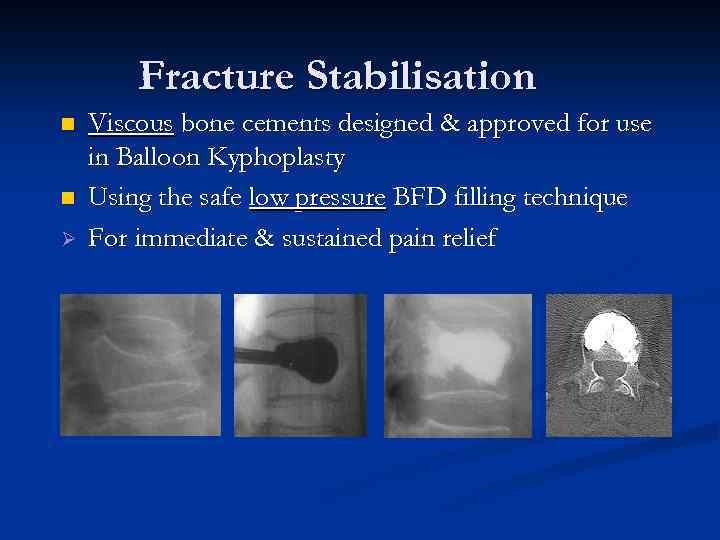
Fracture Stabilisation n n Ø Viscous bone cements designed & approved for use in Balloon Kyphoplasty Using the safe low pressure BFD filling technique For immediate & sustained pain relief
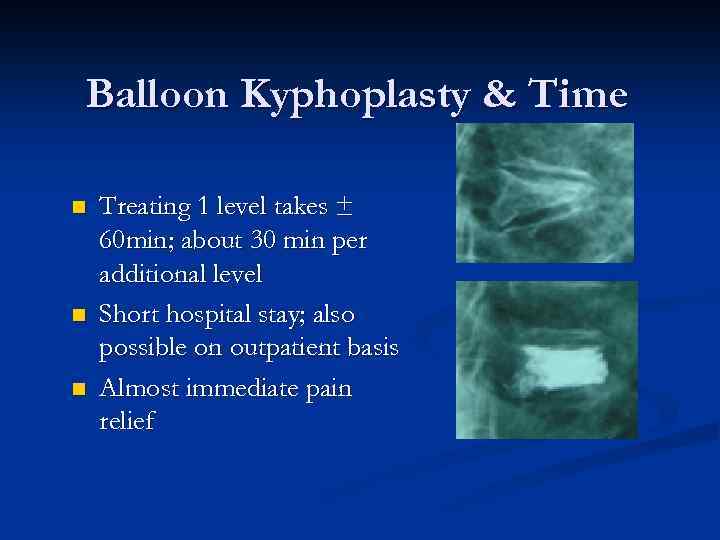
Balloon Kyphoplasty & Time n n n Treating 1 level takes ± 60 min; about 30 min per additional level Short hospital stay; also possible on outpatient basis Almost immediate pain relief
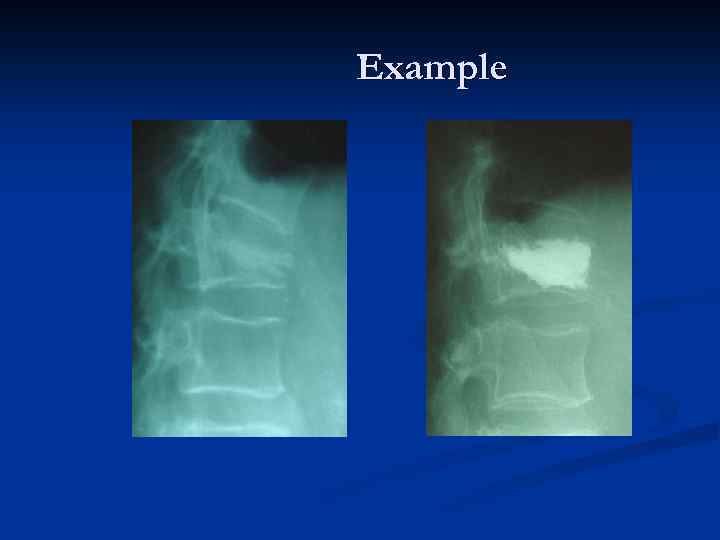
Example
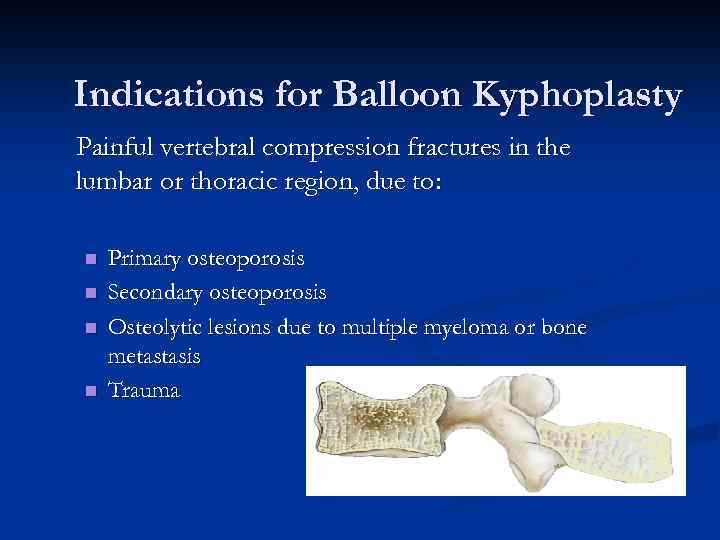
Indications for Balloon Kyphoplasty Painful vertebral compression fractures in the lumbar or thoracic region, due to: n n Primary osteoporosis Secondary osteoporosis Osteolytic lesions due to multiple myeloma or bone metastasis Trauma
Patient Outcomes include: þ þ þ þ Vertebral body height restoration Angular correction of deformity Significant reduction in pain (95%) Reduced number of days in bed Improved quality of life Improvement in activities of daily living Improvement in mobility High rate of patient satisfaction
What does 8° mean?
Differences to Vertebroplasty n Less safe: Leakage rate n complications n n No height restoration
Focus on Patient n Balloon Kyphoplasty offers patients with painful VCF Ø Immediate and sustained pain relief Ø 75% of patients discard narcotic medication Ø Return to a fully active life, functioning without pain Ø Short hospital stay/ day case surgery Ø All these factors will give a significant improvement in Quality Of Life
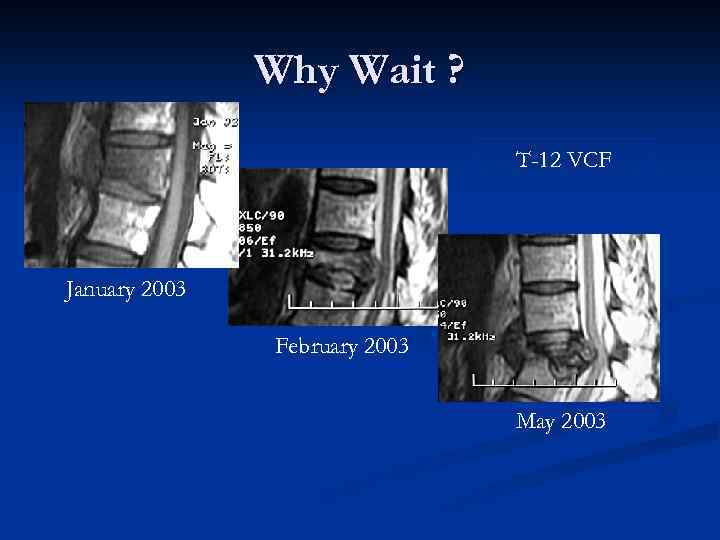
Why Wait ? T-12 VCF January 2003 February 2003 May 2003

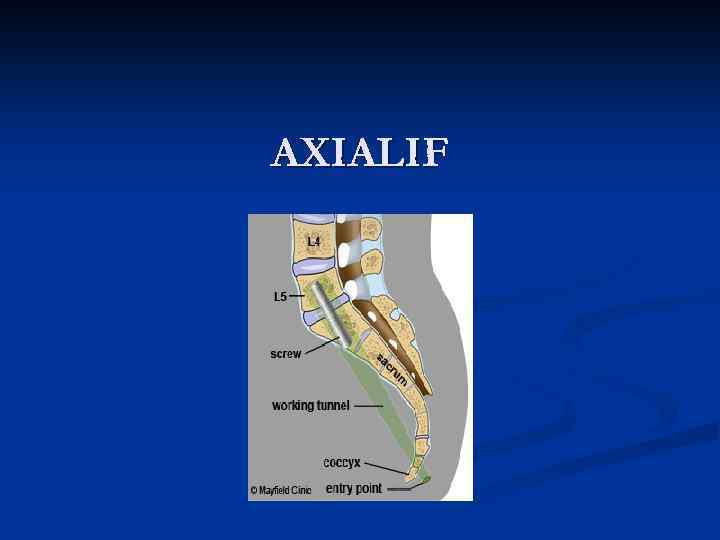
AXIALIF
Axialif Minimally Invasive Anterior Lumbar Interbody Fusion 1 cm parasacral incision Working Channel Daycase Surgery
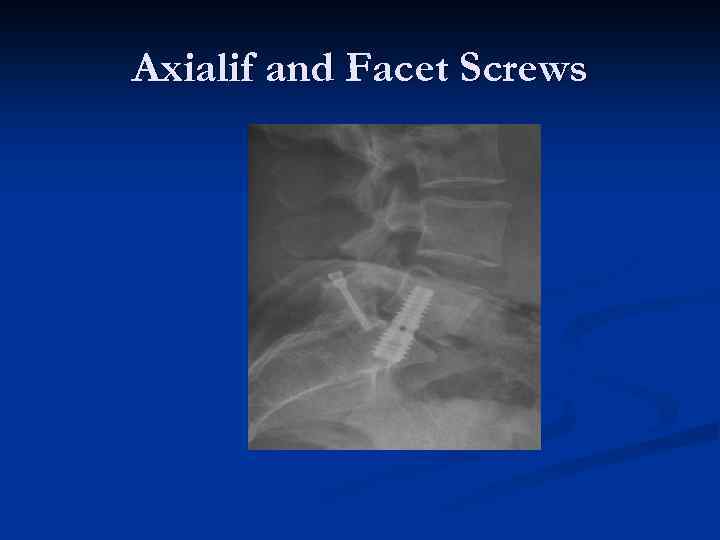
Axialif and Facet Screws
Axialif
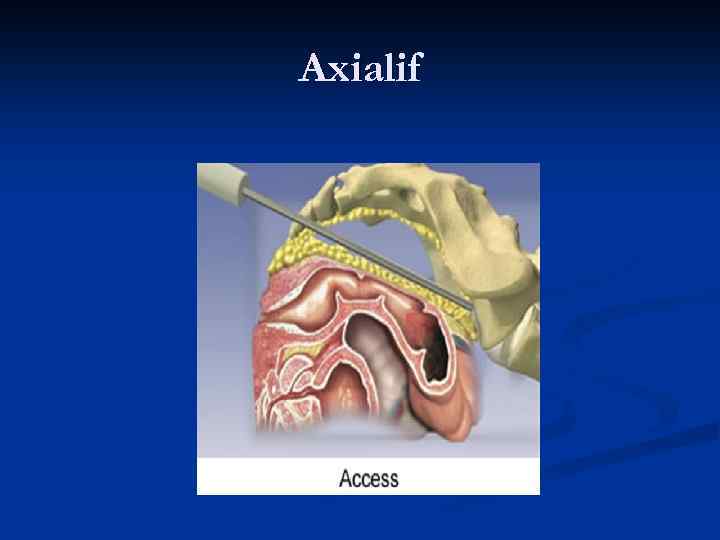
Axialif
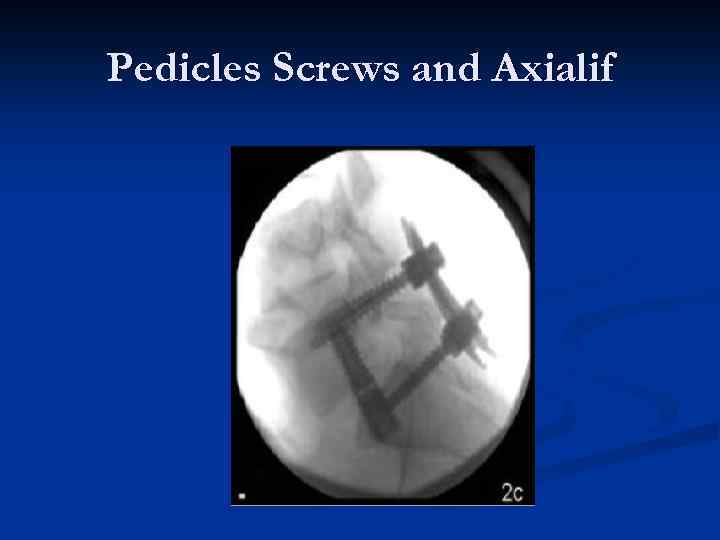
Pedicles Screws and Axialif
Thankyou
Spine and kyphoplasty Ashtead.ppt