f7e9097a7caa2e7989f0e0f1897a6a8f.ppt
- Количество слайдов: 54
 Spinal Cord Syndromes Resident Rounds April 12, 2007 Juliette Sacks
Spinal Cord Syndromes Resident Rounds April 12, 2007 Juliette Sacks
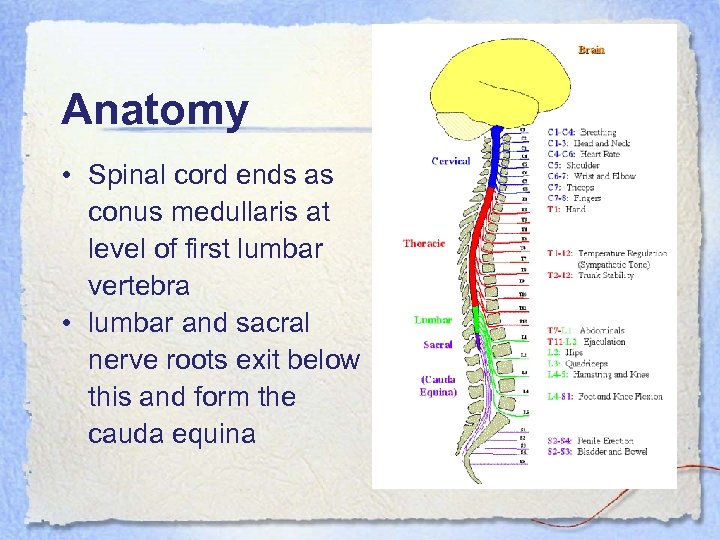 Anatomy • Spinal cord ends as conus medullaris at level of first lumbar vertebra • lumbar and sacral nerve roots exit below this and form the cauda equina
Anatomy • Spinal cord ends as conus medullaris at level of first lumbar vertebra • lumbar and sacral nerve roots exit below this and form the cauda equina
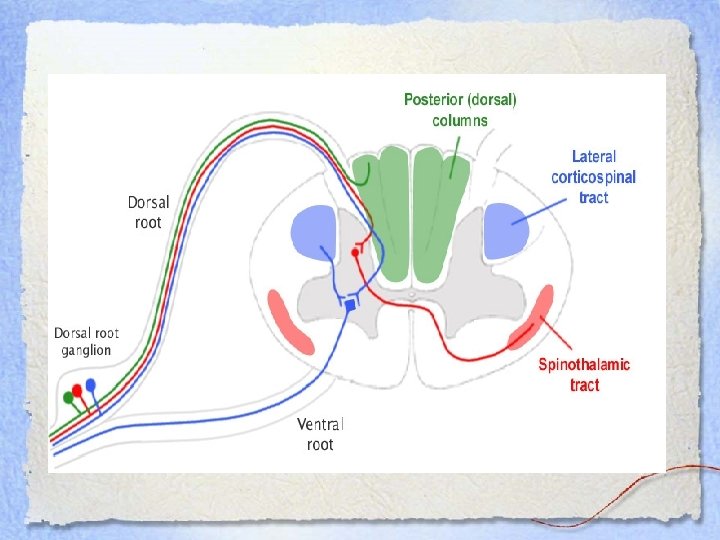
 Neuroanatomy • Corticospinal tracts • Spinothalamic tracts • Dorsal (posterior) columns
Neuroanatomy • Corticospinal tracts • Spinothalamic tracts • Dorsal (posterior) columns
 Corticospinal Tract • Descending motor pathway • Forms the pyramid of the medulla • In the lower medulla, 90% of fibers decussate and descend as the lateral corticospinal tract • Synapse on LMN in the spinal cord • 10% that do not cross descend as the ventral corticospinal tract • Damage to this part cause ipsilateral UMN findings
Corticospinal Tract • Descending motor pathway • Forms the pyramid of the medulla • In the lower medulla, 90% of fibers decussate and descend as the lateral corticospinal tract • Synapse on LMN in the spinal cord • 10% that do not cross descend as the ventral corticospinal tract • Damage to this part cause ipsilateral UMN findings
 Spinothalmic Tract • Ascending sensory tract from skin and muscle via dorsal root ganglia to cerebral cortex • Temperature and pain sensation • Damage to this part of the spinal cord causes: – Loss of pain and temperature sensation in the contralateral side – Loss begins 1 -2 segments below the level of the lesion
Spinothalmic Tract • Ascending sensory tract from skin and muscle via dorsal root ganglia to cerebral cortex • Temperature and pain sensation • Damage to this part of the spinal cord causes: – Loss of pain and temperature sensation in the contralateral side – Loss begins 1 -2 segments below the level of the lesion
 Dorsal (Posterior) Columns • Ascending neurons that do not synapse until they reach the medulla at which point they cross the midline to the thalamus • Transmits vibration and proprioceptive information • Damage will cause ipsilateral loss of vibration and position sense at the level of the lesion
Dorsal (Posterior) Columns • Ascending neurons that do not synapse until they reach the medulla at which point they cross the midline to the thalamus • Transmits vibration and proprioceptive information • Damage will cause ipsilateral loss of vibration and position sense at the level of the lesion
 Complete vs Incomplete • Incomplete: – Sensory, motor or both functions are partially present below the neurologic level of injury – Some degree of recovery • Complete: – Absence of sensory and motor function below the level of injury – Loss of function to lowest sacral segment – Minimal chance of functional motor recovery
Complete vs Incomplete • Incomplete: – Sensory, motor or both functions are partially present below the neurologic level of injury – Some degree of recovery • Complete: – Absence of sensory and motor function below the level of injury – Loss of function to lowest sacral segment – Minimal chance of functional motor recovery

 Light touch… • Transmitted through both the dorsal columns and the spinothalamic tracts • Lost entirely ONLY if both tracts are damaged
Light touch… • Transmitted through both the dorsal columns and the spinothalamic tracts • Lost entirely ONLY if both tracts are damaged
 Case #1 • • 33 yo F fell off a 20’ cliff snowboarding C/o inability to move both legs GCS 15 BP 130/68 HR 89 regular Normal UE exam No power in LE Vibration and position sense normal in LE Sensation normal in LE No rectal tone or perianal sensation
Case #1 • • 33 yo F fell off a 20’ cliff snowboarding C/o inability to move both legs GCS 15 BP 130/68 HR 89 regular Normal UE exam No power in LE Vibration and position sense normal in LE Sensation normal in LE No rectal tone or perianal sensation
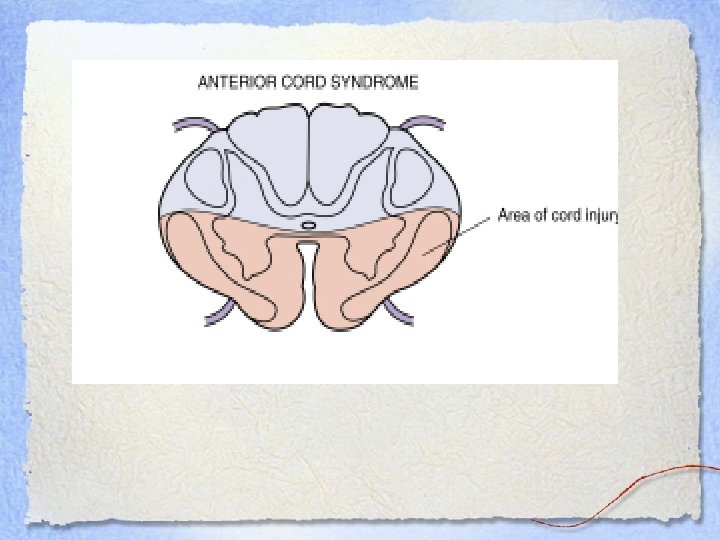
 Anterior Cord Syndrome • Damage to the corticospinal and spinothalamic tracts • Dorsal column function is intact • Loss of: – Motor function – Pain and temperature sensation • Vibration, position and crude touch are maintained
Anterior Cord Syndrome • Damage to the corticospinal and spinothalamic tracts • Dorsal column function is intact • Loss of: – Motor function – Pain and temperature sensation • Vibration, position and crude touch are maintained
 ACS cont’d • Causes: – Direct injury to anterior spinal cord – Flexion injury of cervical spine causing a cord contusion – Bony injury causing secondary cord injury – Thrombosis of anterior spinal artery
ACS cont’d • Causes: – Direct injury to anterior spinal cord – Flexion injury of cervical spine causing a cord contusion – Bony injury causing secondary cord injury – Thrombosis of anterior spinal artery
 Symptoms • Complete paralysis below the level of the lesion with loss of pain and temperature sensation • Preservation of proprioception and vibration sense
Symptoms • Complete paralysis below the level of the lesion with loss of pain and temperature sensation • Preservation of proprioception and vibration sense
 What to do? • Urgent CT/MRI • Surgical decompression may be an option • Prognosis: POOR
What to do? • Urgent CT/MRI • Surgical decompression may be an option • Prognosis: POOR
 Case #2 • 24 y. o. M came off motorcycle at high speed • Wore no helmet and sustained severe head injury • C-spine films were unremarkable apart from a narrow spinal canal • Once conscious, he was quadriparetic with 2/5 power in most muscle groups • No other neurological findings
Case #2 • 24 y. o. M came off motorcycle at high speed • Wore no helmet and sustained severe head injury • C-spine films were unremarkable apart from a narrow spinal canal • Once conscious, he was quadriparetic with 2/5 power in most muscle groups • No other neurological findings
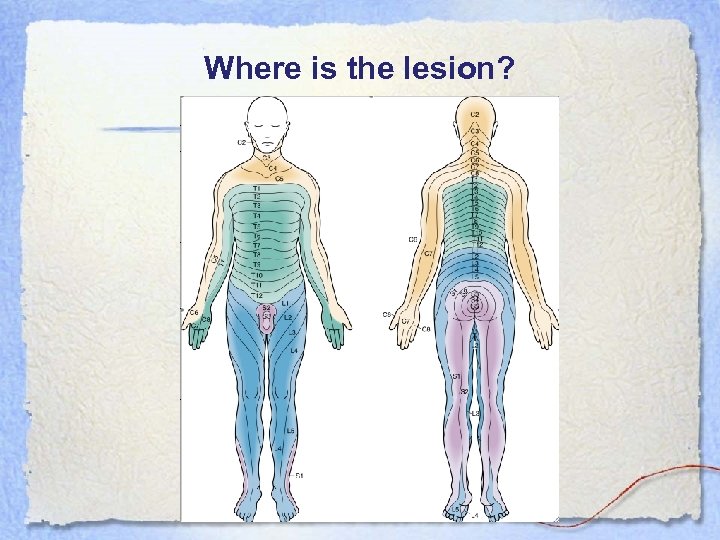 Where is the lesion?
Where is the lesion?

 What’s the deal? • MRI: – Mild swelling of the cord at C 3/4 – Prevertebral soft tissue swelling and disruption of anterior longitudinal ligament • Prognosis: – Within 48 h, power in UE 3/5 and LE 4/5 – At 2/12, further but not full recovery
What’s the deal? • MRI: – Mild swelling of the cord at C 3/4 – Prevertebral soft tissue swelling and disruption of anterior longitudinal ligament • Prognosis: – Within 48 h, power in UE 3/5 and LE 4/5 – At 2/12, further but not full recovery
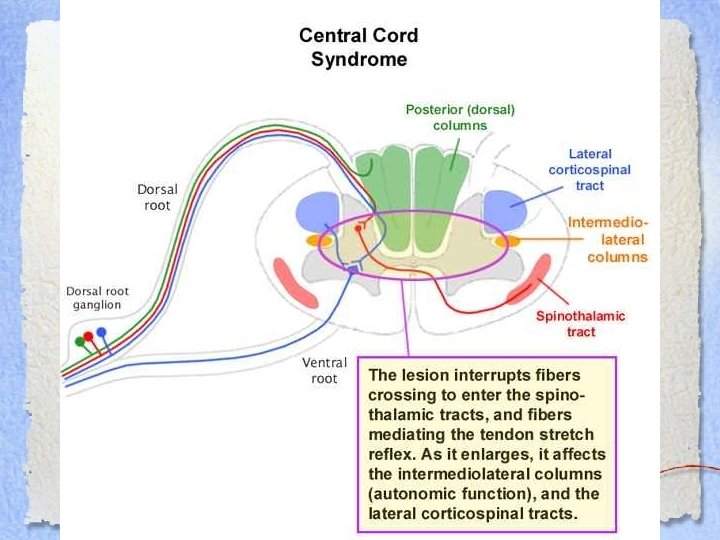
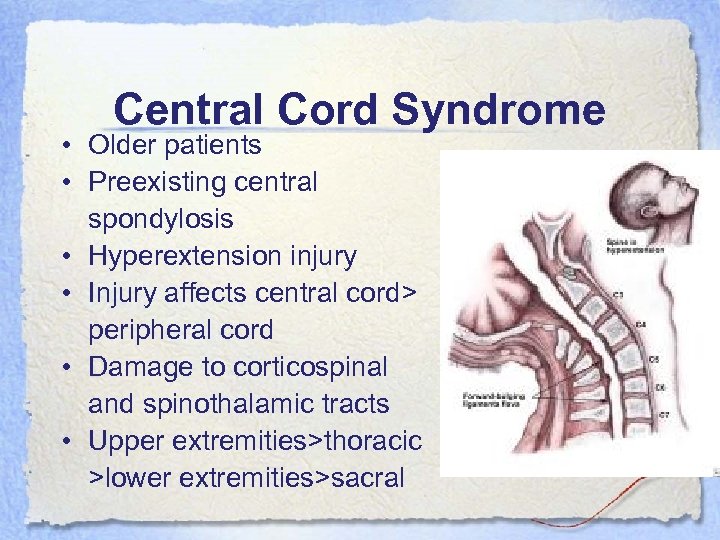 Central Cord Syndrome • Older patients • Preexisting central spondylosis • Hyperextension injury • Injury affects central cord> peripheral cord • Damage to corticospinal and spinothalamic tracts • Upper extremities>thoracic >lower extremities>sacral
Central Cord Syndrome • Older patients • Preexisting central spondylosis • Hyperextension injury • Injury affects central cord> peripheral cord • Damage to corticospinal and spinothalamic tracts • Upper extremities>thoracic >lower extremities>sacral
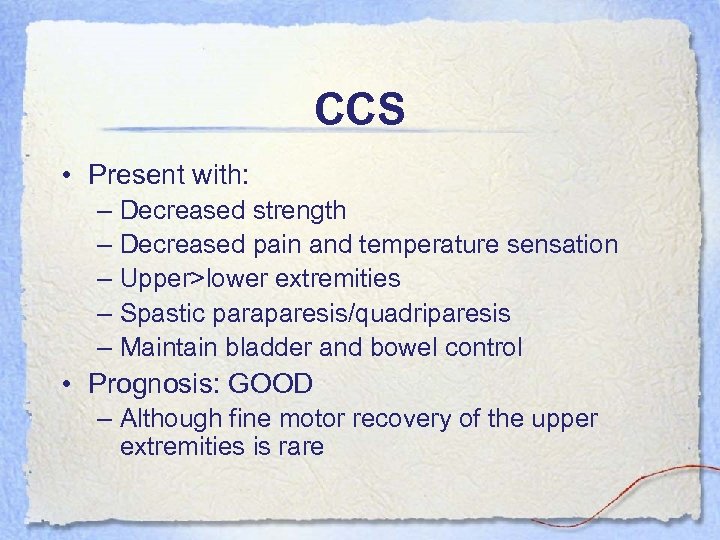 CCS • Present with: – Decreased strength – Decreased pain and temperature sensation – Upper>lower extremities – Spastic paraparesis/quadriparesis – Maintain bladder and bowel control • Prognosis: GOOD – Although fine motor recovery of the upper extremities is rare
CCS • Present with: – Decreased strength – Decreased pain and temperature sensation – Upper>lower extremities – Spastic paraparesis/quadriparesis – Maintain bladder and bowel control • Prognosis: GOOD – Although fine motor recovery of the upper extremities is rare
 Case #3 • 24 y. o. M stabbed in the neck during stampede argument over whose doolie tires were bigger • No LOC • C/o inability to pick up his hat with his left hand • Unaware of his girl holding his right arm
Case #3 • 24 y. o. M stabbed in the neck during stampede argument over whose doolie tires were bigger • No LOC • C/o inability to pick up his hat with his left hand • Unaware of his girl holding his right arm
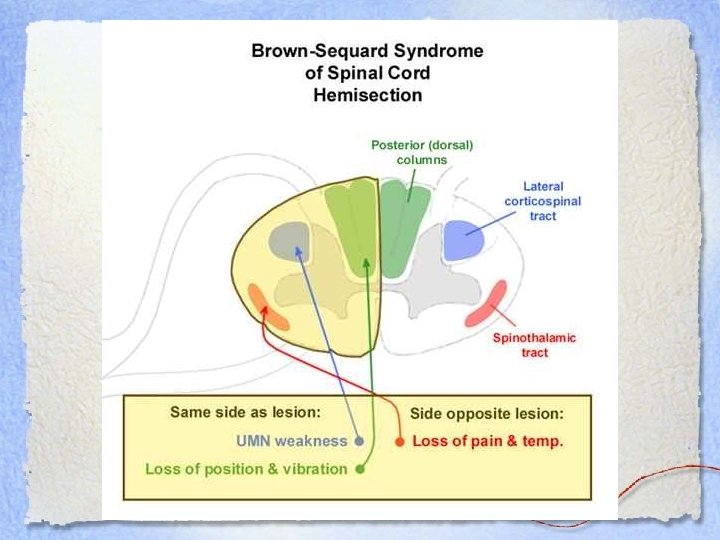
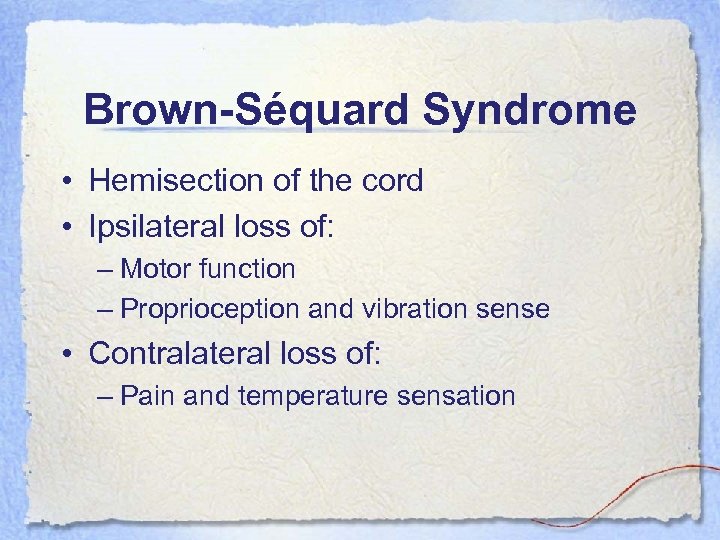 Brown-Séquard Syndrome • Hemisection of the cord • Ipsilateral loss of: – Motor function – Proprioception and vibration sense • Contralateral loss of: – Pain and temperature sensation
Brown-Séquard Syndrome • Hemisection of the cord • Ipsilateral loss of: – Motor function – Proprioception and vibration sense • Contralateral loss of: – Pain and temperature sensation
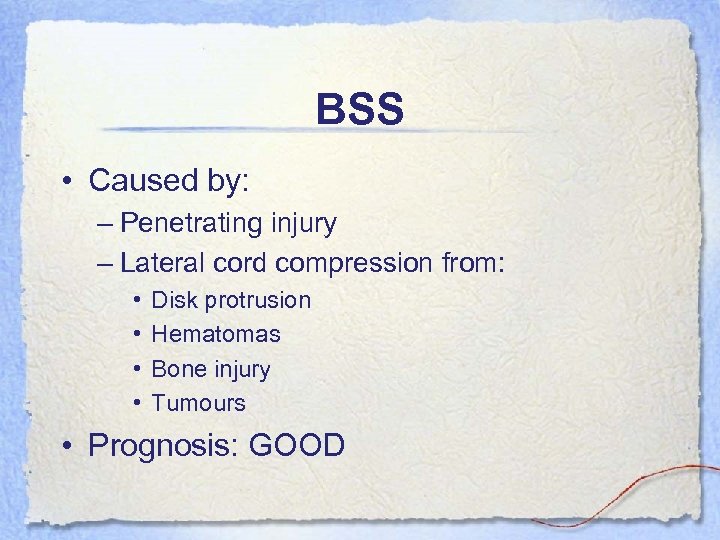 BSS • Caused by: – Penetrating injury – Lateral cord compression from: • • Disk protrusion Hematomas Bone injury Tumours • Prognosis: GOOD
BSS • Caused by: – Penetrating injury – Lateral cord compression from: • • Disk protrusion Hematomas Bone injury Tumours • Prognosis: GOOD
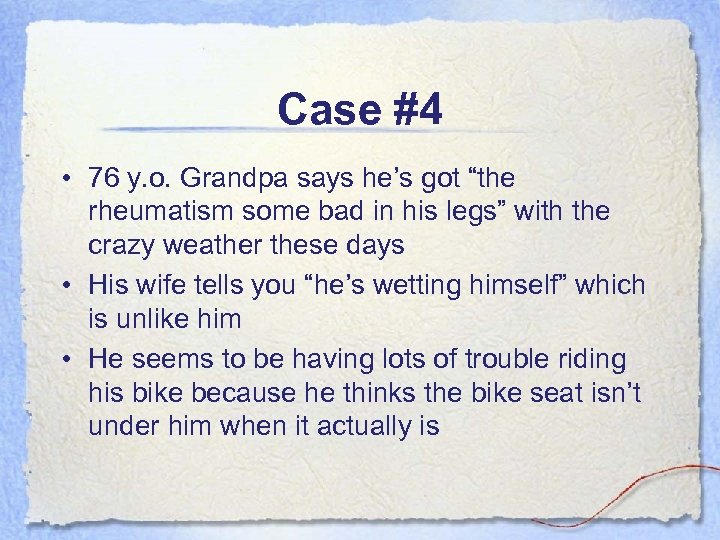 Case #4 • 76 y. o. Grandpa says he’s got “the rheumatism some bad in his legs” with the crazy weather these days • His wife tells you “he’s wetting himself” which is unlike him • He seems to be having lots of trouble riding his bike because he thinks the bike seat isn’t under him when it actually is
Case #4 • 76 y. o. Grandpa says he’s got “the rheumatism some bad in his legs” with the crazy weather these days • His wife tells you “he’s wetting himself” which is unlike him • He seems to be having lots of trouble riding his bike because he thinks the bike seat isn’t under him when it actually is
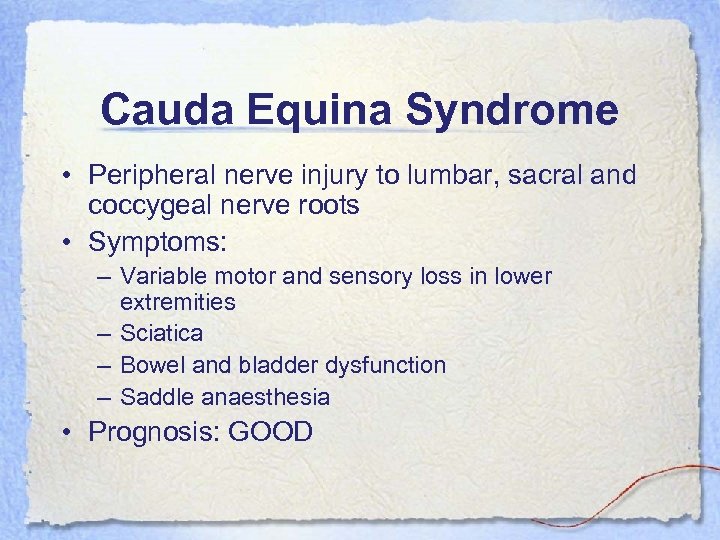 Cauda Equina Syndrome • Peripheral nerve injury to lumbar, sacral and coccygeal nerve roots • Symptoms: – Variable motor and sensory loss in lower extremities – Sciatica – Bowel and bladder dysfunction – Saddle anaesthesia • Prognosis: GOOD
Cauda Equina Syndrome • Peripheral nerve injury to lumbar, sacral and coccygeal nerve roots • Symptoms: – Variable motor and sensory loss in lower extremities – Sciatica – Bowel and bladder dysfunction – Saddle anaesthesia • Prognosis: GOOD
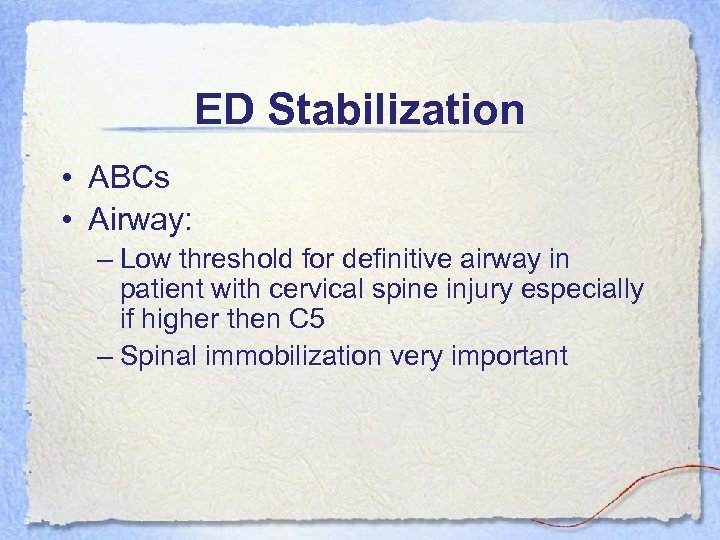 ED Stabilization • ABCs • Airway: – Low threshold for definitive airway in patient with cervical spine injury especially if higher then C 5 – Spinal immobilization very important
ED Stabilization • ABCs • Airway: – Low threshold for definitive airway in patient with cervical spine injury especially if higher then C 5 – Spinal immobilization very important
 Spinal Shock • Loss of neurological function and autonomic tone below level of lesion • Loss of all reflexes • Resolves over 24 -48 h but may last for days • Bulbocavernosus reflex returns first
Spinal Shock • Loss of neurological function and autonomic tone below level of lesion • Loss of all reflexes • Resolves over 24 -48 h but may last for days • Bulbocavernosus reflex returns first
 Spinal Shock • Symptoms: – – – – Flaccid paralysis Loss of sensation Loss of DTRs Bladder incontinence Bradycardia Hypotension Hypothermia Intestinal ileus
Spinal Shock • Symptoms: – – – – Flaccid paralysis Loss of sensation Loss of DTRs Bladder incontinence Bradycardia Hypotension Hypothermia Intestinal ileus
 Hypotension • Must determine cause: – – Spinal cord injury Blood loss Cardiac injury Combination of above • Blood loss is the cause of hypotension until proven otherwise! • Vitals are often non specific • R/O other causes with: CXR, FAST, CT
Hypotension • Must determine cause: – – Spinal cord injury Blood loss Cardiac injury Combination of above • Blood loss is the cause of hypotension until proven otherwise! • Vitals are often non specific • R/O other causes with: CXR, FAST, CT
 Neurogenic Shock • Neurogenic Shock: – Warm – Peripherally vasodilated – Bradycardic • Bradycardia may be caused by something other than neurogenic shock • Cervical spine injury may cause sympathetic denervation • Resuscitate with fluids +/- vasopressors
Neurogenic Shock • Neurogenic Shock: – Warm – Peripherally vasodilated – Bradycardic • Bradycardia may be caused by something other than neurogenic shock • Cervical spine injury may cause sympathetic denervation • Resuscitate with fluids +/- vasopressors
 Corticosteroids • Controversial • Based on NASCIS trials • Methylprednisolone improved both motor and sensory functional outcomes in complete and incomplete injuries • Benefit dependent on dose and timing of dose
Corticosteroids • Controversial • Based on NASCIS trials • Methylprednisolone improved both motor and sensory functional outcomes in complete and incomplete injuries • Benefit dependent on dose and timing of dose
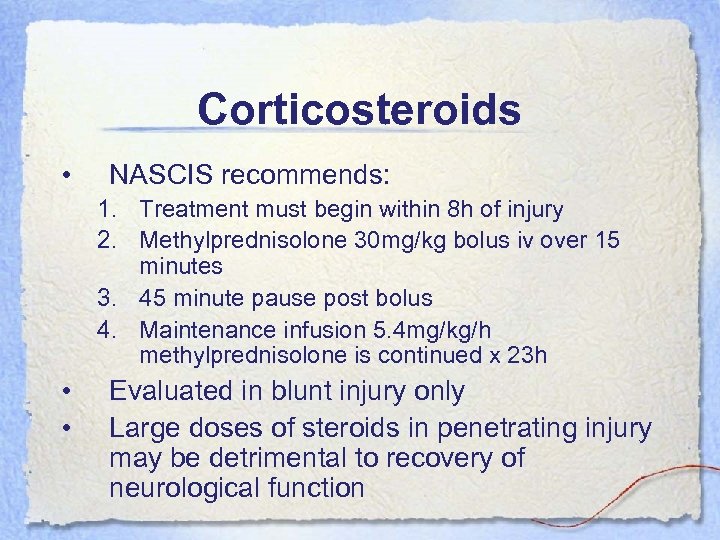 Corticosteroids • NASCIS recommends: 1. Treatment must begin within 8 h of injury 2. Methylprednisolone 30 mg/kg bolus iv over 15 minutes 3. 45 minute pause post bolus 4. Maintenance infusion 5. 4 mg/kg/h methylprednisolone is continued x 23 h • • Evaluated in blunt injury only Large doses of steroids in penetrating injury may be detrimental to recovery of neurological function
Corticosteroids • NASCIS recommends: 1. Treatment must begin within 8 h of injury 2. Methylprednisolone 30 mg/kg bolus iv over 15 minutes 3. 45 minute pause post bolus 4. Maintenance infusion 5. 4 mg/kg/h methylprednisolone is continued x 23 h • • Evaluated in blunt injury only Large doses of steroids in penetrating injury may be detrimental to recovery of neurological function
 Steroid Therapy as per NACSIS • Attributed to antioxidant effects • Treat for 24 h in patients treated within 3 h of injury • Treat for 48 h in patients treated within 3 -8 h of injury • Worse outcome if started 8 h post injury • Conflicting evidence re benefit therefore more trials required
Steroid Therapy as per NACSIS • Attributed to antioxidant effects • Treat for 24 h in patients treated within 3 h of injury • Treat for 48 h in patients treated within 3 -8 h of injury • Worse outcome if started 8 h post injury • Conflicting evidence re benefit therefore more trials required
 Pros • Believed to inhibit formation of free radicalinduced peroxidation • May increase spinal cord blood flow • Increase extracellular calcium • Prevent potassium loss from cord Cons • • • Pneumonia Sepsis Wound infection GIB Delayed healing
Pros • Believed to inhibit formation of free radicalinduced peroxidation • May increase spinal cord blood flow • Increase extracellular calcium • Prevent potassium loss from cord Cons • • • Pneumonia Sepsis Wound infection GIB Delayed healing
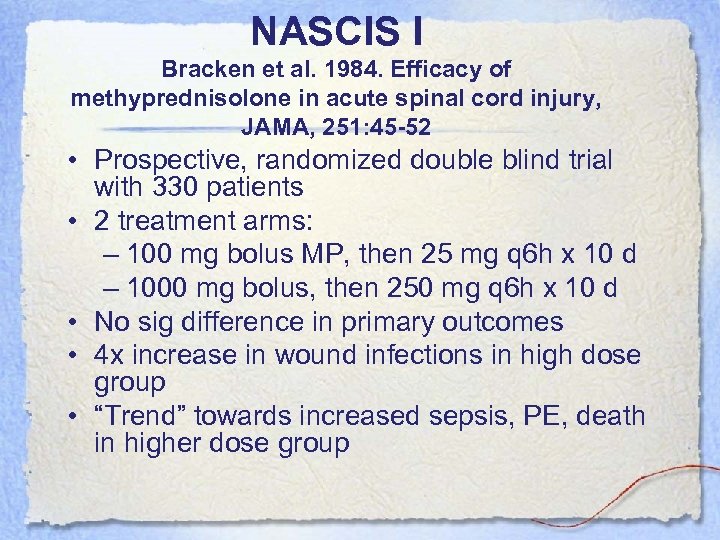 NASCIS I Bracken et al. 1984. Efficacy of methyprednisolone in acute spinal cord injury, JAMA, 251: 45 -52 • Prospective, randomized double blind trial with 330 patients • 2 treatment arms: – 100 mg bolus MP, then 25 mg q 6 h x 10 d – 1000 mg bolus, then 250 mg q 6 h x 10 d • No sig difference in primary outcomes • 4 x increase in wound infections in high dose group • “Trend” towards increased sepsis, PE, death in higher dose group
NASCIS I Bracken et al. 1984. Efficacy of methyprednisolone in acute spinal cord injury, JAMA, 251: 45 -52 • Prospective, randomized double blind trial with 330 patients • 2 treatment arms: – 100 mg bolus MP, then 25 mg q 6 h x 10 d – 1000 mg bolus, then 250 mg q 6 h x 10 d • No sig difference in primary outcomes • 4 x increase in wound infections in high dose group • “Trend” towards increased sepsis, PE, death in higher dose group
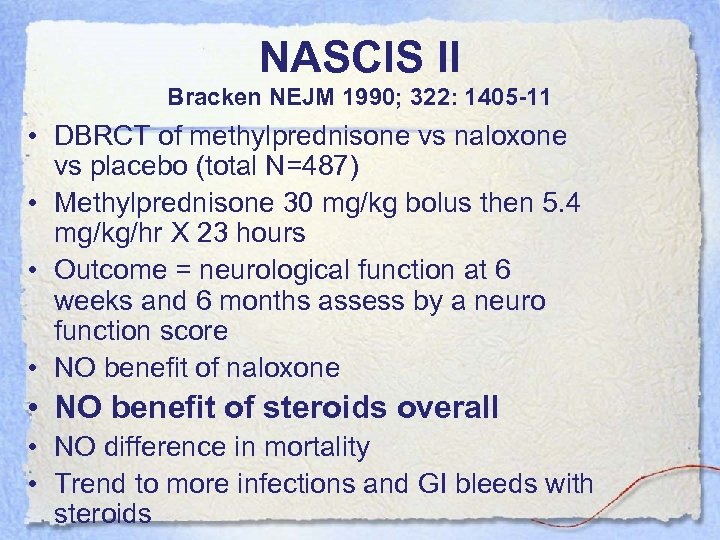 NASCIS II Bracken NEJM 1990; 322: 1405 -11 • DBRCT of methylprednisone vs naloxone vs placebo (total N=487) • Methylprednisone 30 mg/kg bolus then 5. 4 mg/kg/hr X 23 hours • Outcome = neurological function at 6 weeks and 6 months assess by a neuro function score • NO benefit of naloxone • NO benefit of steroids overall • NO difference in mortality • Trend to more infections and GI bleeds with steroids
NASCIS II Bracken NEJM 1990; 322: 1405 -11 • DBRCT of methylprednisone vs naloxone vs placebo (total N=487) • Methylprednisone 30 mg/kg bolus then 5. 4 mg/kg/hr X 23 hours • Outcome = neurological function at 6 weeks and 6 months assess by a neuro function score • NO benefit of naloxone • NO benefit of steroids overall • NO difference in mortality • Trend to more infections and GI bleeds with steroids
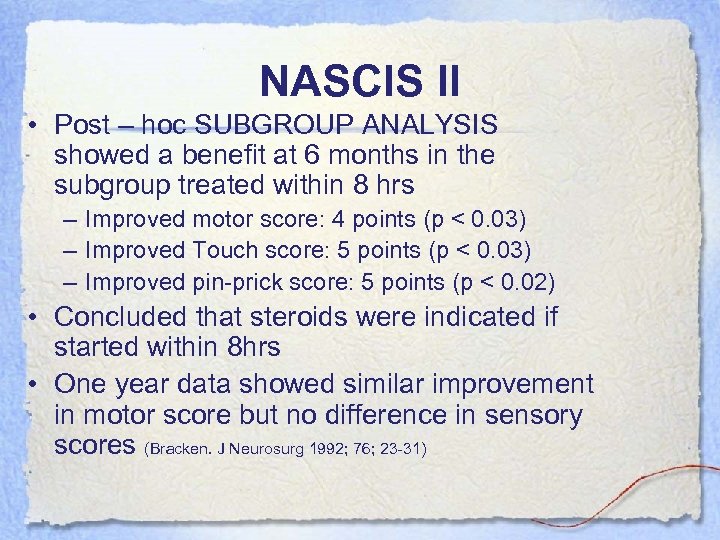 NASCIS II • Post – hoc SUBGROUP ANALYSIS showed a benefit at 6 months in the subgroup treated within 8 hrs – Improved motor score: 4 points (p < 0. 03) – Improved Touch score: 5 points (p < 0. 03) – Improved pin-prick score: 5 points (p < 0. 02) • Concluded that steroids were indicated if started within 8 hrs • One year data showed similar improvement in motor score but no difference in sensory scores (Bracken. J Neurosurg 1992; 76; 23 -31)
NASCIS II • Post – hoc SUBGROUP ANALYSIS showed a benefit at 6 months in the subgroup treated within 8 hrs – Improved motor score: 4 points (p < 0. 03) – Improved Touch score: 5 points (p < 0. 03) – Improved pin-prick score: 5 points (p < 0. 02) • Concluded that steroids were indicated if started within 8 hrs • One year data showed similar improvement in motor score but no difference in sensory scores (Bracken. J Neurosurg 1992; 76; 23 -31)
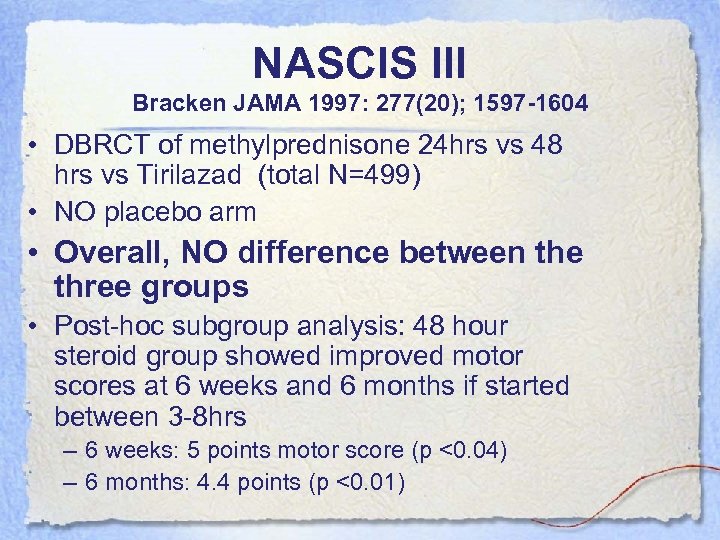 NASCIS III Bracken JAMA 1997: 277(20); 1597 -1604 • DBRCT of methylprednisone 24 hrs vs 48 hrs vs Tirilazad (total N=499) • NO placebo arm • Overall, NO difference between the three groups • Post-hoc subgroup analysis: 48 hour steroid group showed improved motor scores at 6 weeks and 6 months if started between 3 -8 hrs – 6 weeks: 5 points motor score (p <0. 04) – 6 months: 4. 4 points (p <0. 01)
NASCIS III Bracken JAMA 1997: 277(20); 1597 -1604 • DBRCT of methylprednisone 24 hrs vs 48 hrs vs Tirilazad (total N=499) • NO placebo arm • Overall, NO difference between the three groups • Post-hoc subgroup analysis: 48 hour steroid group showed improved motor scores at 6 weeks and 6 months if started between 3 -8 hrs – 6 weeks: 5 points motor score (p <0. 04) – 6 months: 4. 4 points (p <0. 01)
 NASCIS III • Adverse outcomes – Severe pneumonia higher in 48 hr group • 2. 6% vs 5. 8% (p<0. 02) – Severe sepsis higher in 48 hr group • 0. 6% vs 2. 6% (p< 0. 07) • They concluded – Steroids indicated for SCI – If started within 3 hrs, treat for 24 hrs – If started within 3 -8 hrs, treat for 48 hrs
NASCIS III • Adverse outcomes – Severe pneumonia higher in 48 hr group • 2. 6% vs 5. 8% (p<0. 02) – Severe sepsis higher in 48 hr group • 0. 6% vs 2. 6% (p< 0. 07) • They concluded – Steroids indicated for SCI – If started within 3 hrs, treat for 24 hrs – If started within 3 -8 hrs, treat for 48 hrs
 Cochrane Review • “the randomized trials of MPSS in the treatment of acute SCI provide evidence for a significant improvement in motor function recovery after treatment with the high dose regimen within 8 hours of injury” • Bracken November 2000 • Update in Spine 2001 by Bracken • 4 trials and 797 patients randomized to get high dose methylpred vs placebo for 24 hours
Cochrane Review • “the randomized trials of MPSS in the treatment of acute SCI provide evidence for a significant improvement in motor function recovery after treatment with the high dose regimen within 8 hours of injury” • Bracken November 2000 • Update in Spine 2001 by Bracken • 4 trials and 797 patients randomized to get high dose methylpred vs placebo for 24 hours
 Cochrane Review Results • Primary outcome = neurological improvement at 6 weeks, 6 months, 1 year • Complicated motor and sensory exam • High dose methylpred associated with 4/70 point increase in motor function at 6 weeks, 6 months but not one year
Cochrane Review Results • Primary outcome = neurological improvement at 6 weeks, 6 months, 1 year • Complicated motor and sensory exam • High dose methylpred associated with 4/70 point increase in motor function at 6 weeks, 6 months but not one year
 SCI and Steroids • Clinical relevance? – 4 points spread over 14 muscle segments unilaterally – Not validated score – No inter-rater reliability • Conclusions based on post-hoc analysis of small subgroup from 1 trial – 65 patients per arm – Data drudging – High risk of alpha error • Serious complications (not statistically significant) – GI bleed and wound infection (RR 4. 00, 95% CI 0. 4535. 58) – Severe pneumonia (RR 2. 25, 95% CI 0. 71 -7. 15) – Range of values in CI huge do the risks outweigh the benefits? ?
SCI and Steroids • Clinical relevance? – 4 points spread over 14 muscle segments unilaterally – Not validated score – No inter-rater reliability • Conclusions based on post-hoc analysis of small subgroup from 1 trial – 65 patients per arm – Data drudging – High risk of alpha error • Serious complications (not statistically significant) – GI bleed and wound infection (RR 4. 00, 95% CI 0. 4535. 58) – Severe pneumonia (RR 2. 25, 95% CI 0. 71 -7. 15) – Range of values in CI huge do the risks outweigh the benefits? ?
 SCI and Steroids • Author consultant for Pharmacia (they make methylprednisolone) • Weak support for use of high dose methylpred in acute SCI + may be increased risk of severe adverse outcomes.
SCI and Steroids • Author consultant for Pharmacia (they make methylprednisolone) • Weak support for use of high dose methylpred in acute SCI + may be increased risk of severe adverse outcomes.
 Bottom Line • CAEP position statement : steroids are NOT STANDARD OF CARE • There is insufficient evidence to support the use of high dose methyprednisolone within 8 h of acute SCI • Significant harm to using steroids • NASCIS subgroup data needs to be validated in prospective, randomized, blinded trials • No new literature to argue for or against this
Bottom Line • CAEP position statement : steroids are NOT STANDARD OF CARE • There is insufficient evidence to support the use of high dose methyprednisolone within 8 h of acute SCI • Significant harm to using steroids • NASCIS subgroup data needs to be validated in prospective, randomized, blinded trials • No new literature to argue for or against this
 Neurological Examination • LOC • Deteriorating course • Neck, back pain and/or bladder, bowel incontinence should increase suspicion of sc injury • Define level of lesion • Motor function • Sensory level • Proprioception testing • DTRs • Anogenital reflexes
Neurological Examination • LOC • Deteriorating course • Neck, back pain and/or bladder, bowel incontinence should increase suspicion of sc injury • Define level of lesion • Motor function • Sensory level • Proprioception testing • DTRs • Anogenital reflexes
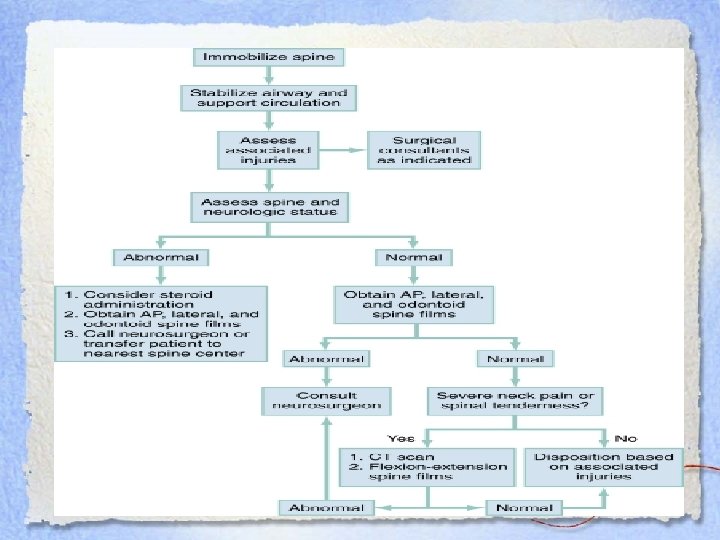
 DI • C-spine films as per c-spine rules/nexus • CT • MRI: better for visualizing neurological, muscular and soft tissue – If CT negative and patient has positive neurological findings, this is next step – Important to image entire spine as 10% have 2 nd injury
DI • C-spine films as per c-spine rules/nexus • CT • MRI: better for visualizing neurological, muscular and soft tissue – If CT negative and patient has positive neurological findings, this is next step – Important to image entire spine as 10% have 2 nd injury
 Treatment • • Prevent secondary injury Alleviate cord compression Establish spinal stability Assess the neurological deficit and spinal stability • Imaging • Consult spine/neurosurgery
Treatment • • Prevent secondary injury Alleviate cord compression Establish spinal stability Assess the neurological deficit and spinal stability • Imaging • Consult spine/neurosurgery
 Other cord lesions… • Malignancy • Epidural hematoma • Abscesses
Other cord lesions… • Malignancy • Epidural hematoma • Abscesses
 At the end of my rope… • Urgent care necessary • MRI is better than CT for imaging spinal cord • Comprehensive serial neurological exams important re management options • Steroids are not the standard of care in Canada • Consider spinal shock, neurogenic shock and other causes of shock in someone with a spinal cord injury
At the end of my rope… • Urgent care necessary • MRI is better than CT for imaging spinal cord • Comprehensive serial neurological exams important re management options • Steroids are not the standard of care in Canada • Consider spinal shock, neurogenic shock and other causes of shock in someone with a spinal cord injury


