21c20aee8ac725d5bc93ab0c85b68334.ppt
- Количество слайдов: 71
Spina Bifida David Cancel MD, JD Montefiore/Albert Einstein Medical Center
Goals of the Spina Bifida Module • • Pathogenesis Risk Factors Types Clinical Signs and Course Associated Malformations Orthopedic Complications Rehabilitation Medical Complications
Spina Bifida • Definition: Any birth defect involving incomplete closure of the spine (Source: PM&R Knowledge Now) • U. S. prevalence is 2: 10, 000 live births • Considered the second most common disability in children • Most cases occur without any known cause • Some can have multiple factors as a cause
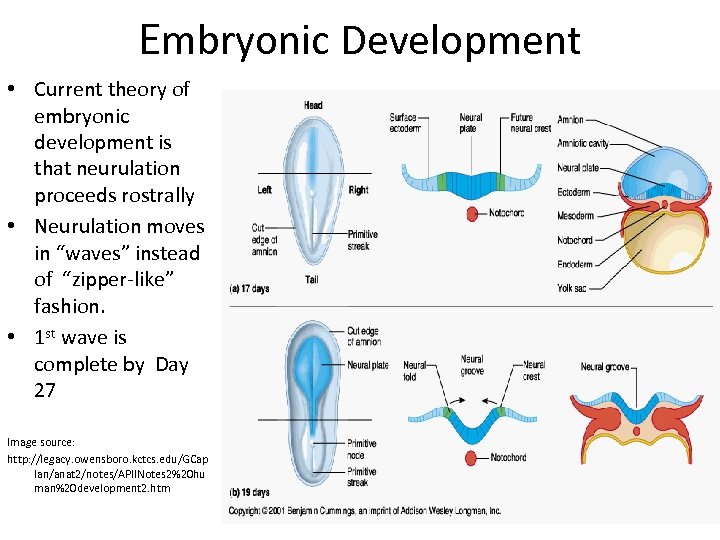
Embryonic Development • Current theory of embryonic development is that neurulation proceeds rostrally • Neurulation moves in “waves” instead of “zipper-like” fashion. • 1 st wave is complete by Day 27 Image source: http: //legacy. owensboro. kctcs. edu/GCap lan/anat 2/notes/APIINotes 2%20 hu man%20 development 2. htm
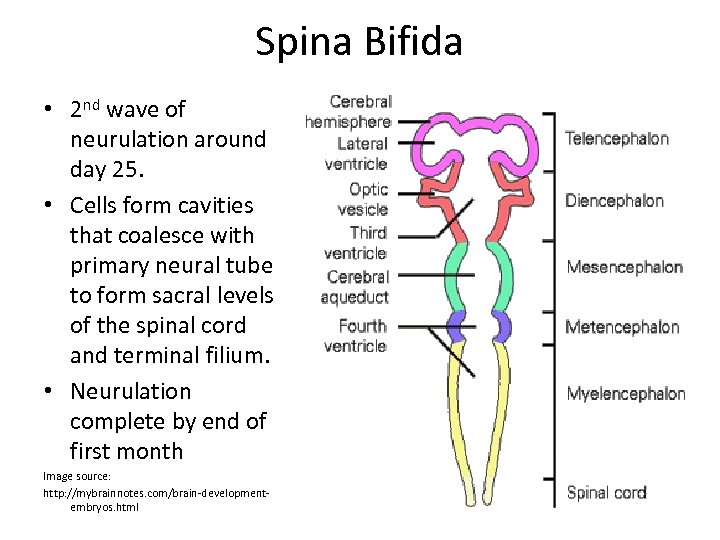
Spina Bifida • 2 nd wave of neurulation around day 25. • Cells form cavities that coalesce with primary neural tube to form sacral levels of the spinal cord and terminal filium. • Neurulation complete by end of first month Image source: http: //mybrainnotes. com/brain-developmentembryos. html
Neurulation Video source: http: //www. lsic. ucla. edu/classes/lifesci/central/ps 107/lectures/em-slide_19. html
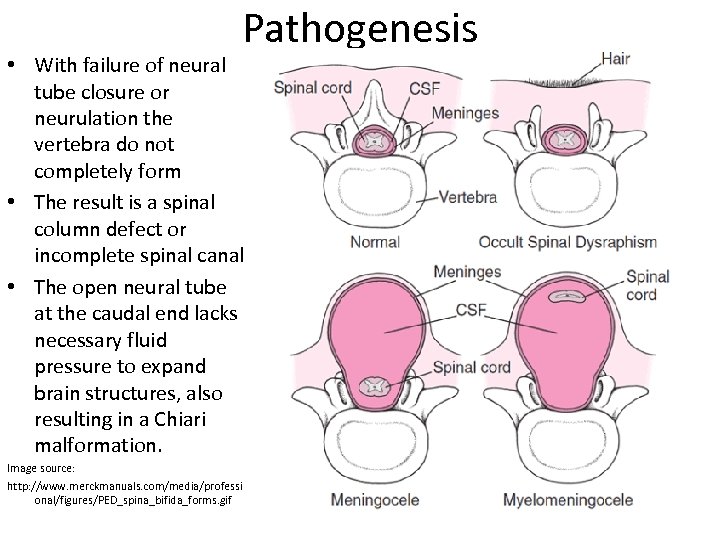
Pathogenesis • With failure of neural tube closure or neurulation the vertebra do not completely form • The result is a spinal column defect or incomplete spinal canal • The open neural tube at the caudal end lacks necessary fluid pressure to expand brain structures, also resulting in a Chiari malformation. Image source: http: //www. merckmanuals. com/media/professi onal/figures/PED_spina_bifida_forms. gif
Risk Factors in Spina Bifida • Possible viral etiology – there are sources that note a higher rate of Spina Bifida in children born during the early winter months (Pubmed) • Possible environmental - radiation (Pubmed). • Risk for recurrence is 2%-5% after first child; 10 -15% if 2 siblings affected • Parent with Spina Bifida – 4% risk (Alexander)
Spina Bifida • • • Genetic influences Sonic hedgehog (SHH) gene – a vertebrate gene expressed by notochord cells. Provides signal sequencing for cell differentiation Patched gene (PTC) – provides negative feedback to SHH Mutations in the 5, 10 Methylenetetrahydrofolate reductase (MTHFR) gene are implicated in decreased plasma folate levels Homozygosity for the C 677 T gene has been found in Hispanics Possible polymorphism exists in the Irish Also seen in chromosomal disorders such as Trisomies 13 and 21
Risk Factors Folic acid deficiency • Major risk factor • Supplements reduce risk 50 -70% • Current AAP guidelines for Folic Acid supplementation: – All women of childbearing age - 0. 4 mg dadily – Women with previous neural tube defect – 4 mg daily at least one month prior to conception and in the 1 st trimester – Women with high risk (valproic acid, maternal diabetes) – 4 mg daily
Risk Factors • Maternal risk factors – Obesity – Diabetes – Hyperthermia (hot tubs) – Elevated homocysteine levels – Medications - Valproic acid, Carbamazepine, HIV retroviral medications (HAART) – Exposure to solvents – Ethnicity. Highest rates among Hispanics (due to genetic risks), lowest among Asian and African. Americans
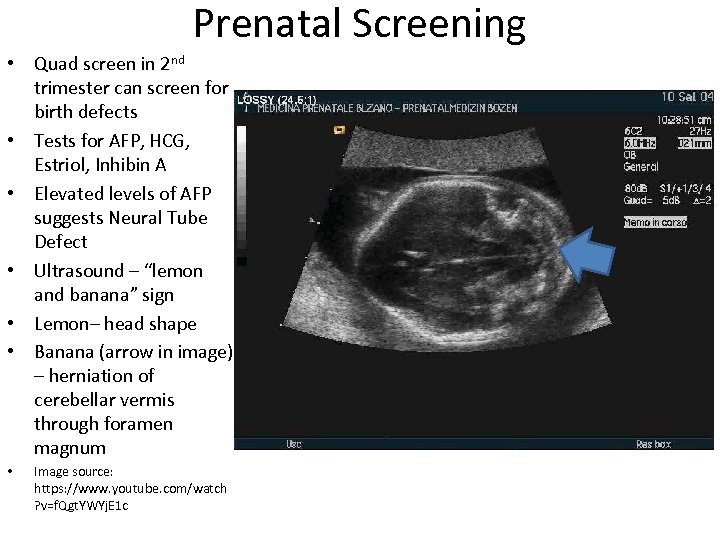
Prenatal Screening • Quad screen in 2 nd trimester can screen for birth defects • Tests for AFP, HCG, Estriol, Inhibin A • Elevated levels of AFP suggests Neural Tube Defect • Ultrasound – “lemon and banana” sign • Lemon– head shape • Banana (arrow in image) – herniation of cerebellar vermis through foramen magnum • Image source: https: //www. youtube. com/watch ? v=f. Qgt. YWYj. E 1 c

Ultrasound of Fetal Spine – Coronal View Normal (left) vs. Spina Bifida (right) Source: http: //sonoworld. com/fetus/page. aspx? id=135
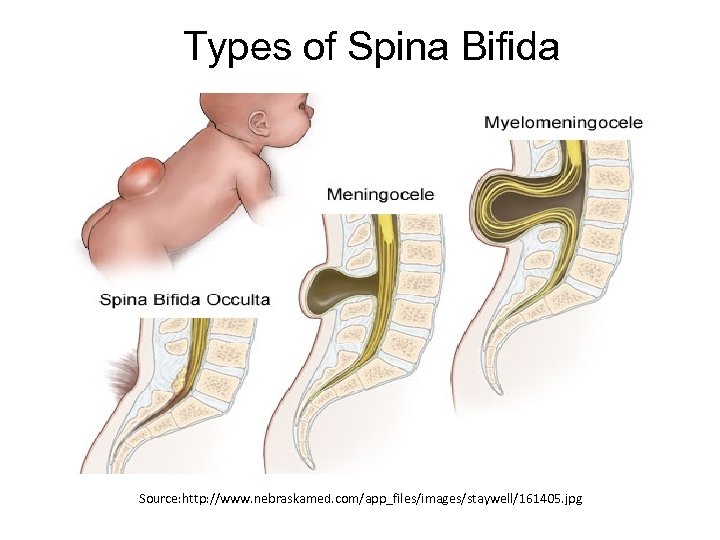
Types of Spina Bifida Source: http: //www. nebraskamed. com/app_files/images/staywell/161405. jpg
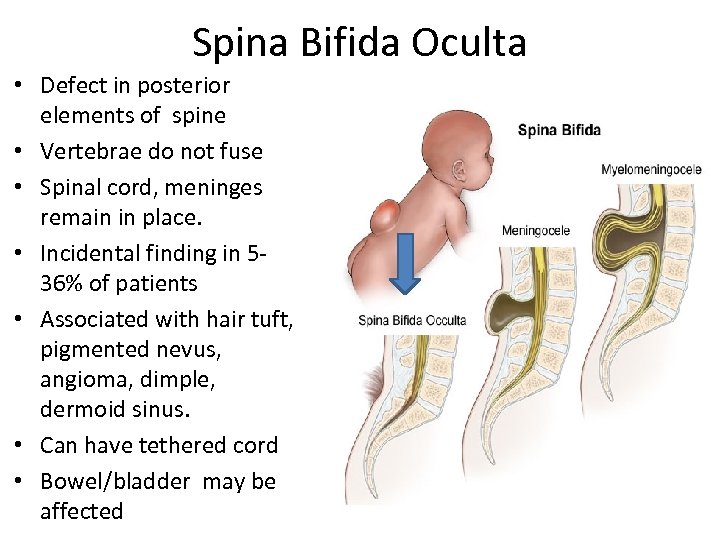
Spina Bifida Oculta • Defect in posterior elements of spine • Vertebrae do not fuse • Spinal cord, meninges remain in place. • Incidental finding in 536% of patients • Associated with hair tuft, pigmented nevus, angioma, dimple, dermoid sinus. • Can have tethered cord • Bowel/bladder may be affected
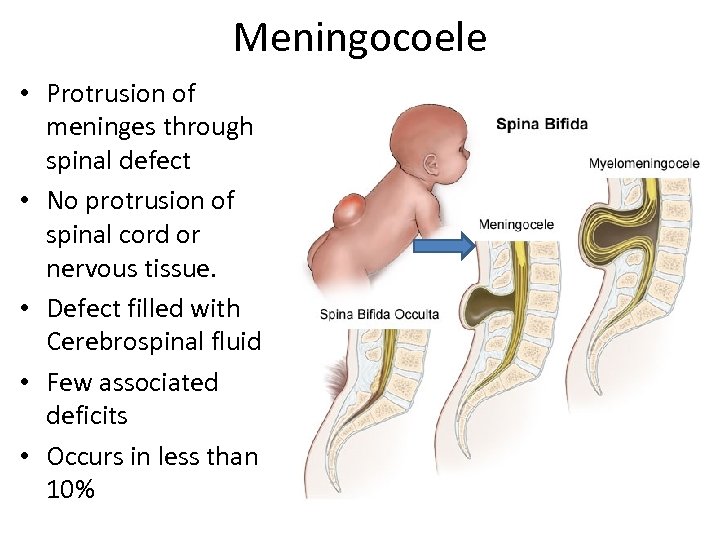
Meningocoele • Protrusion of meninges through spinal defect • No protrusion of spinal cord or nervous tissue. • Defect filled with Cerebrospinal fluid • Few associated deficits • Occurs in less than 10%
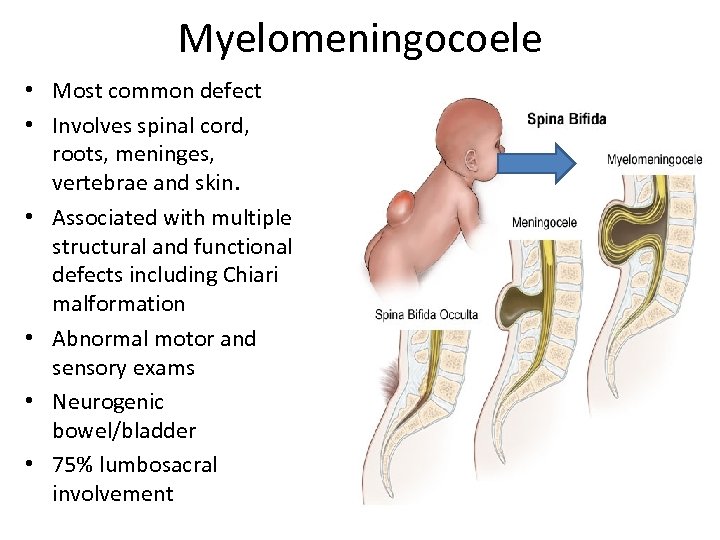
Myelomeningocoele • Most common defect • Involves spinal cord, roots, meninges, vertebrae and skin. • Associated with multiple structural and functional defects including Chiari malformation • Abnormal motor and sensory exams • Neurogenic bowel/bladder • 75% lumbosacral involvement
Caudal regression • Type of Spinal Dysraphism • Absence of sacrum and portions of Lumbar spine • Failure in 2 nd wave of neurulation • Associated with maternal diabetes • Findings include syringomyelia, anorectal stenosis, renal, genital and cardiac abnormalities Image Source: http: //www. healthinset. com/caudal-regressionsyndrome. html
Clinical Signs and Course • There are 2 levels to consider in evaluating patients – anatomic and functional (Alexander) • Findings can show asymmetric motor and sensory deficits • Thoracic level lesions Respiratory dysfunction Kyphosis, Kyphoscoliosis LE deformities – hip ext rotation, abduction, ankle PF Deformities can result from sitting • L 1 – L 3 level lesions Contractures and hip dislocation Pelvic obliquity enhances scoliosis Ambulation dependent on level of knee extension
Clinical Signs and Course • L 4 -L 5 segmental lesions Acetabular dysplasia, coxa valga If L 4 level spared – hip flexion, adduction and knee extension If L 5 level spared – calcaneovarus foot deformity • Sacral segmental lesions Cavus foot, toe clawing • Sensory deficits Increased risk of pressure ulcers and complications Vasomotor instability Charcot joints Osteoporosis • Spina Bifida is usually lower motor neuron process If there is spasticity above the level of lesion – must rule out brain, spinal cord involvement
• • • Pauly M, Cremer R “Levels of mobility in children and adolescents with spina bifidaclinical parameters predicting mobility and maintenance of these skills” Eur J Pediatr Surg. 2013 Apr; 23(2): 110 -4 Retrospective study applying "Hoffer criteria" (community walker, household walker, exercise walker, nonwalker) as classification of mobility in spina bifida patients. Assessed clinical parameters and factors to predict future mobility and development. Data on 90 patients using a questionnaire, medical records. Patients grouped by walking distances according to Hoffer s criteria. The development of the mobility skills over the years was documented. 42% of the patients were community walkers, 16% household, 16% exercise walkers, and 27% wheelchair dependent. Significant correlations between the Hoffer criteria, the level of lesion the walking distance and the ability to stand upright. Also significant relation between the Hoffer criteria and the frequency of fractures and the age of the patients. Fractures directly related to the level of lesion and to the level of mobility. 39% had improved mobility, 37% retained their achieved state, and 24% worsened. Improvement only appeared to occur up to Lumbar level lesions. Others may require surgical intervention. Predictive factors not only dependent on the level of lesion but also rely on aftercare. Data can be used for counseling of parents and patients.
Services for Spina Bifida Requires a comprehensive approach to care: • Neurosurgery • Urology • Gastroenterology • Orthopedics • Rehabilitation • Pediatrics (General/Genetics/Developmental/Behavioral) • Nursing • Therapy (includes Vocational and Orthotics) • Transition to Adult Care
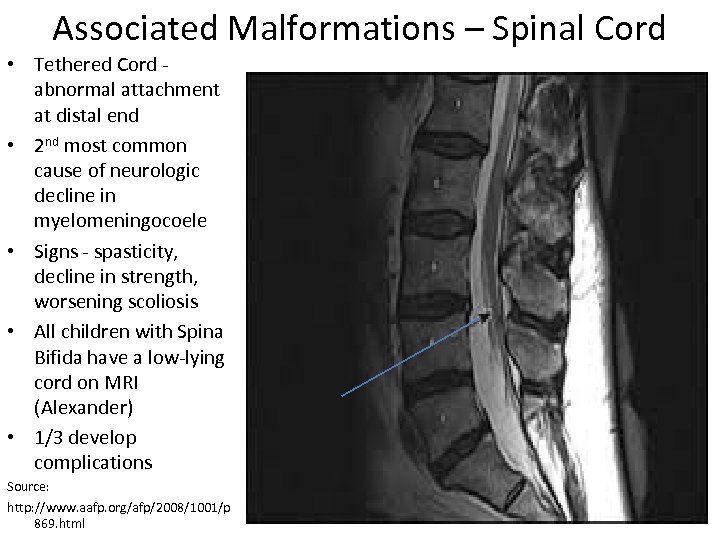
Associated Malformations – Spinal Cord • Tethered Cord - abnormal attachment at distal end • 2 nd most common cause of neurologic decline in myelomeningocoele • Signs - spasticity, decline in strength, worsening scoliosis • All children with Spina Bifida have a low-lying cord on MRI (Alexander) • 1/3 develop complications Source: http: //www. aafp. org/afp/2008/1001/p 869. html
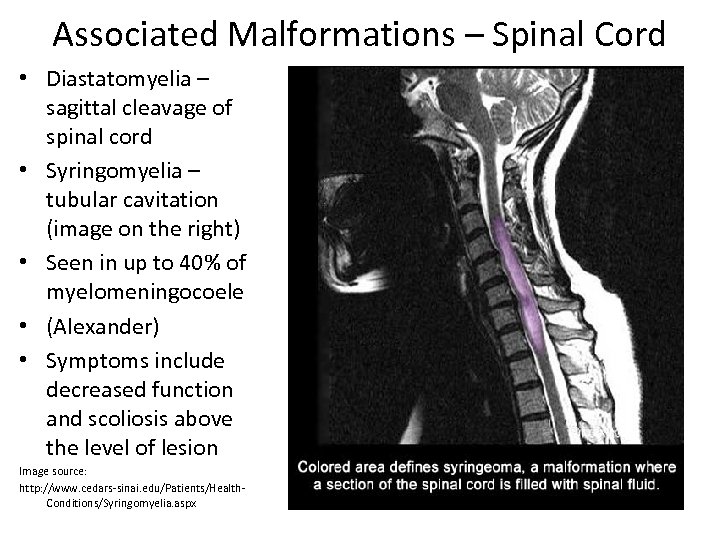
Associated Malformations – Spinal Cord • Diastatomyelia – sagittal cleavage of spinal cord • Syringomyelia – tubular cavitation (image on the right) • Seen in up to 40% of myelomeningocoele • (Alexander) • Symptoms include decreased function and scoliosis above the level of lesion Image source: http: //www. cedars-sinai. edu/Patients/Health. Conditions/Syringomyelia. aspx
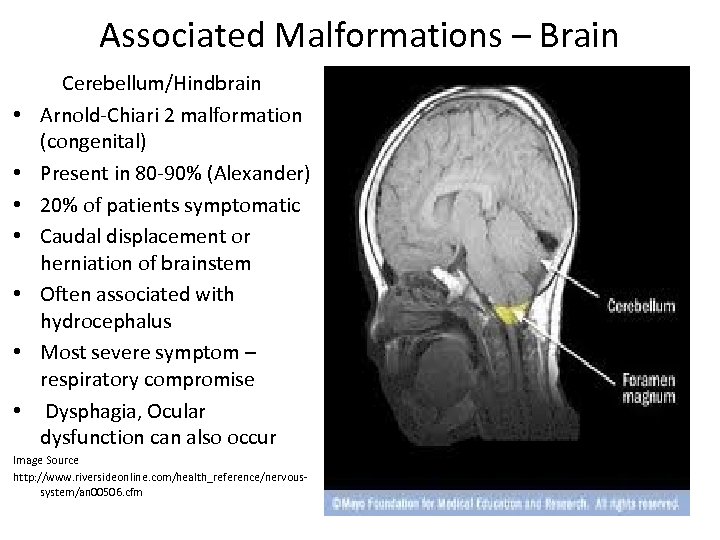
Associated Malformations – Brain • • Cerebellum/Hindbrain Arnold-Chiari 2 malformation (congenital) Present in 80 -90% (Alexander) 20% of patients symptomatic Caudal displacement or herniation of brainstem Often associated with hydrocephalus Most severe symptom – respiratory compromise Dysphagia, Ocular dysfunction can also occur Image Source http: //www. riversideonline. com/health_reference/nervoussystem/an 00506. cfm
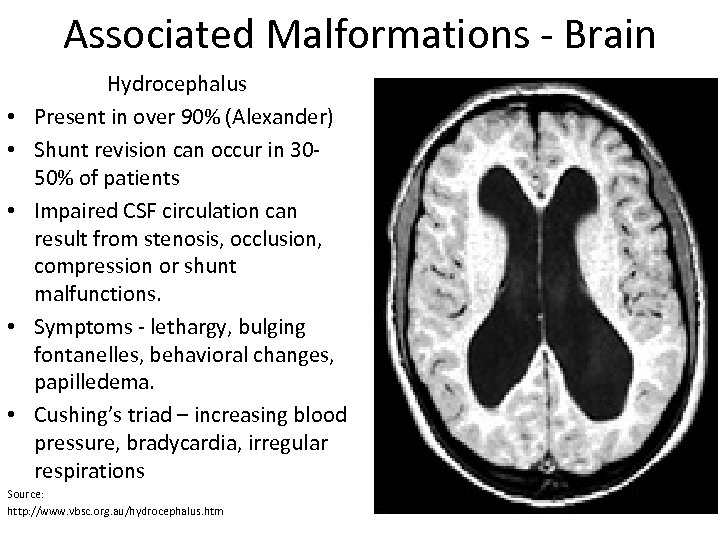
Associated Malformations - Brain • • • Hydrocephalus Present in over 90% (Alexander) Shunt revision can occur in 3050% of patients Impaired CSF circulation can result from stenosis, occlusion, compression or shunt malfunctions. Symptoms - lethargy, bulging fontanelles, behavioral changes, papilledema. Cushing’s triad – increasing blood pressure, bradycardia, irregular respirations Source: http: //www. vbsc. org. au/hydrocephalus. htm
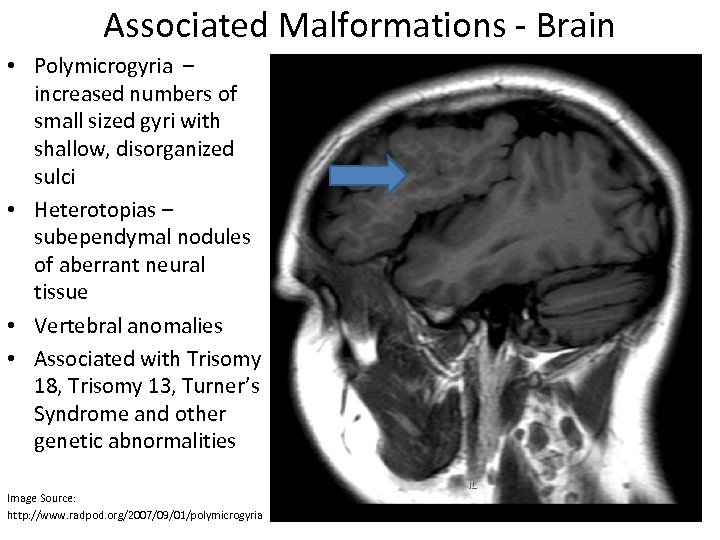
Associated Malformations - Brain • Polymicrogyria – increased numbers of small sized gyri with shallow, disorganized sulci • Heterotopias – subependymal nodules of aberrant neural tissue • Vertebral anomalies • Associated with Trisomy 18, Trisomy 13, Turner’s Syndrome and other genetic abnormalities Image Source: http: //www. radpod. org/2007/09/01/polymicrogyria
• • Saadai P, Farmer DL “Fetal surgery for myelomeningocele. ”Clin Perinatol. 2012 Jun; 39(2): 279 -88. Review article on advances in myelomeningocele repair. New advances and shift from open repair have resulted in improvement in hindbrain malformation and need for shunt repair. Human and animal studies noted early function of lower extremities in utero which was then lost. Repair showed improvement or reversal of defects. Results noted that 57% of patients had neurologic dysfunction better than predicted based on their level of defect. No improvement in urologic function. The recently completed Management of Myelomeningocoele Study (MOMS) by CHOP, UCSF, Vanderbilt. randomized controlled trial of 183 patients has shown that fetal repair can improve hydrocephalus and hindbrain herniation, can reduce the need for vetriculoperitoneal shunting, and may improve distal neurologic function in some patients (percentage of children able to independently ambulate at 30 months increased from 21% to 42% after prenatal repair vs. postnatal repair). Prospect for neural stem cells, grafts and robotic-assisted closures.

Orthopedic Complications • Spine – Observational (serial Xrays) – Nonsurgical: bracing (usually for curves over 20 degrees), seating systems (contoured or molded wheelchair backs) , therapy – Surgical (when scoliosis exceeds 45 degrees) • Hips – Severity depends on level of lesion – Unilateral dislocations can cause pelvic obliquity – Surgical vs. Nonsurgical treatment
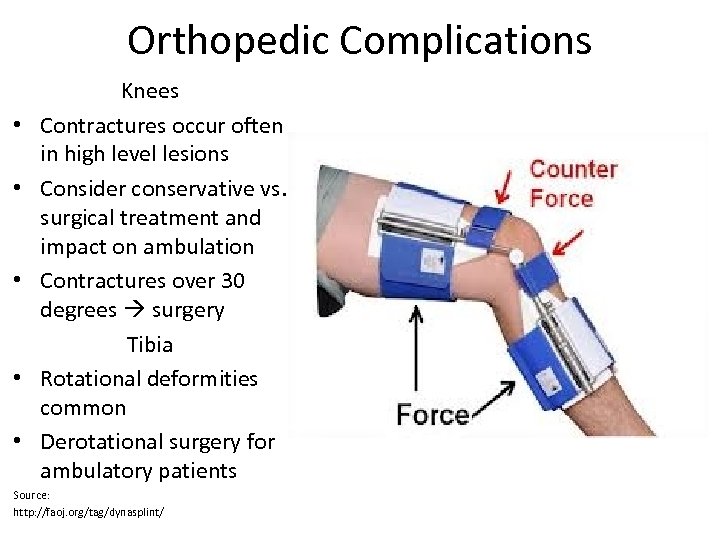
Orthopedic Complications • • • Knees Contractures occur often in high level lesions Consider conservative vs. surgical treatment and impact on ambulation Contractures over 30 degrees surgery Tibia Rotational deformities common Derotational surgery for ambulatory patients Source: http: //faoj. org/tag/dynasplint/
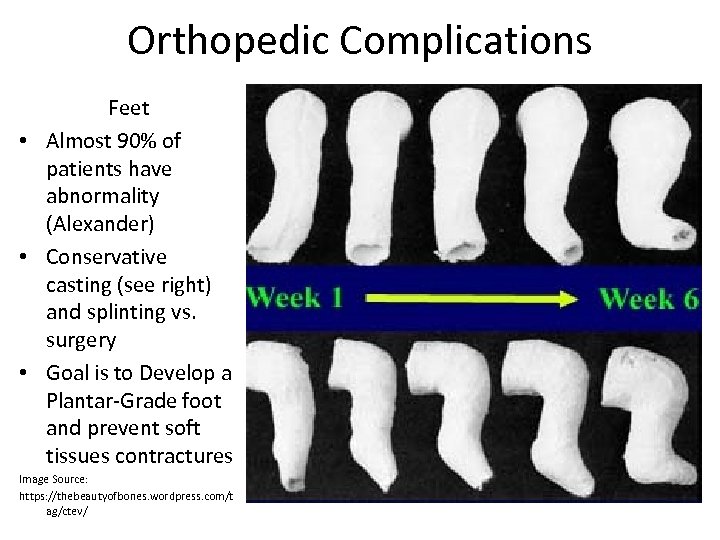
Orthopedic Complications Feet • Almost 90% of patients have abnormality (Alexander) • Conservative casting (see right) and splinting vs. surgery • Goal is to Develop a Plantar-Grade foot and prevent soft tissues contractures Image Source: https: //thebeautyofbones. wordpress. com/t ag/ctev/
Dosa et al. “Incidence, prevalence, and characteristics of fractures in children, adolescents, and adults with spina bifida. ” J Spinal Cord Med. 2007; 30 Suppl 1: S 5 -9. • Determine age-specific incidence, prevalence, and characteristics of fractures • Year-long cross-sectional chart review (annual visits) of 221 patients aged 2 -58 y/o. • Younger age and higher level appeared to be risk factors for fractures: • Twenty percent (n=44) were children age 2 -10 years; 30% (n=68) were adolescents age 11 -18 years; and 50% (n=109) were adults age 19 -58 years. Fifty-five percent (n=121) were female; 64% (n=141) had shunted hydrocephalus. Fifty-eight percent (n=129) were community ambulators. Defect levels included 14% (n=31) thoracic; 37% (n=81) mid-lumbar; 35% (n=79) low-lumbar; and 14% (n = 30) sacral. • Comparisons between adult- and childhood-onset fractures were not significant for difference in sex, BMI, defect level, functional independence, shunted hydrocephalus, epilepsy, or other congenital anomalies. • 1/4 patients with fractures reported multiple fractures. Median age at first fracture was 11 years. Most fractures involved the femur or tibia. • Annual incidence of fractures among children, adolescents, and adults was 23/1000; 29/1000; and 18/1000, respectively. Overall prevalence was 200/1000. • Fractures most common during early adolescence, and environmental modifications may be more effective than pharmacological treatment in reducing the prevalence of fractures. • Note: Predominantly Caucasian (93%) group, multiple confounding comorbidities/syndromes
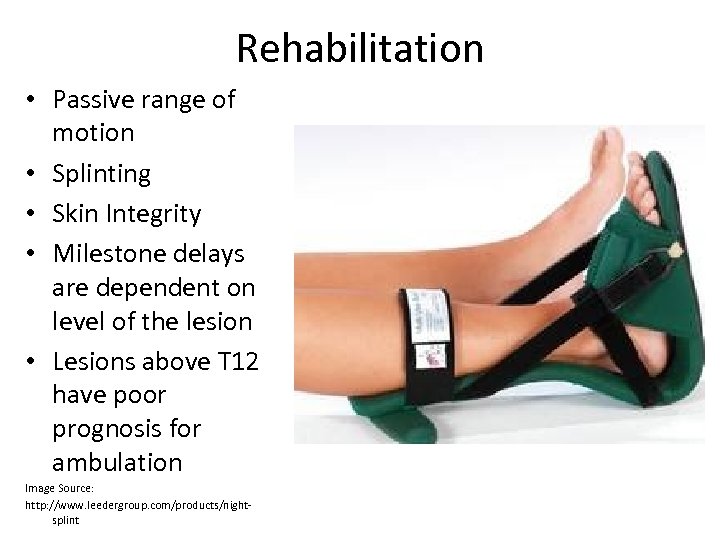
Rehabilitation • Passive range of motion • Splinting • Skin Integrity • Milestone delays are dependent on level of the lesion • Lesions above T 12 have poor prognosis for ambulation Image Source: http: //www. leedergroup. com/products/nightsplint

Rehabilitation Bracing • For Thoracic level lesions • HKAFO • With walker or crutches can allows swing-through gait • Allows trunk, pelvic and hip support • Weight of the HKAFO may make limit use or become more difficult as child grows Video Source: https: //www. youtube. com/watch? v=k Hd 3 FGpv. Lnc
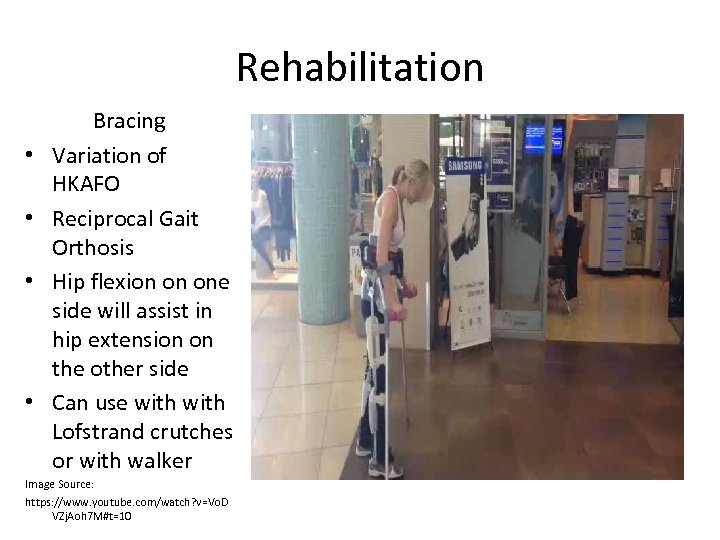
Rehabilitation • • Bracing Variation of HKAFO Reciprocal Gait Orthosis Hip flexion on one side will assist in hip extension on the other side Can use with Lofstrand crutches or with walker Image Source: https: //www. youtube. com/watch? v=Vo. D VZj. Aoh 7 M#t=10
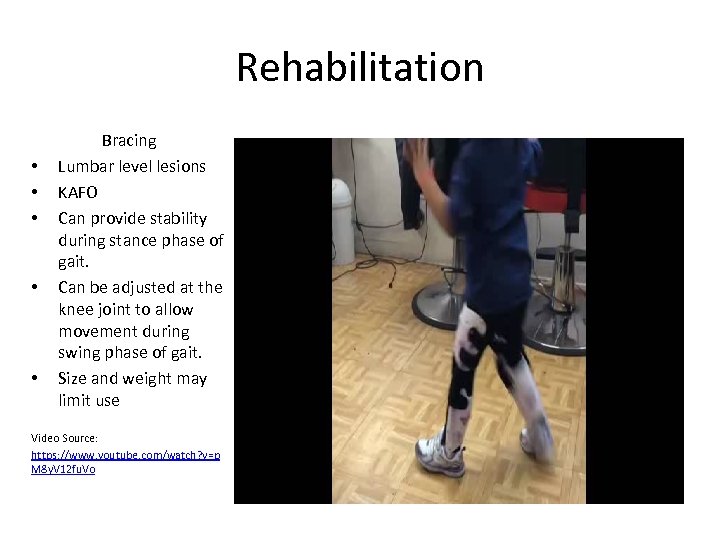
Rehabilitation • • • Bracing Lumbar level lesions KAFO Can provide stability during stance phase of gait. Can be adjusted at the knee joint to allow movement during swing phase of gait. Size and weight may limit use Video Source: https: //www. youtube. com/watch? v=p M 8 y. V 12 fu. Vo
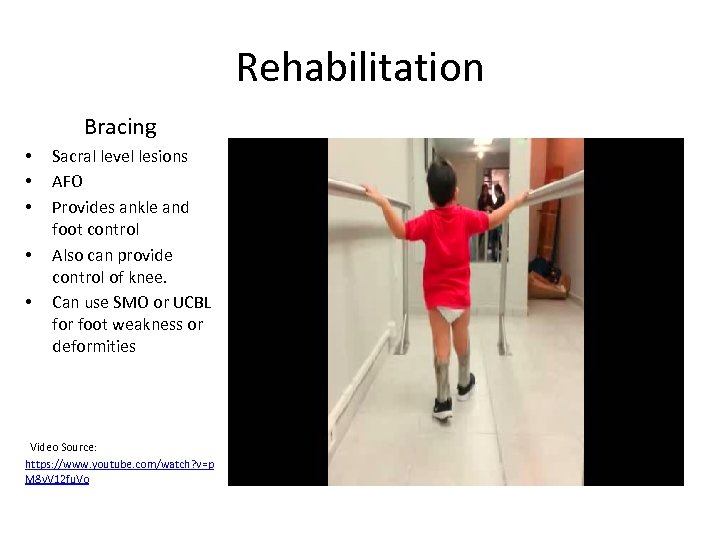
Rehabilitation Bracing • • • Sacral level lesions AFO Provides ankle and foot control Also can provide control of knee. Can use SMO or UCBL for foot weakness or deformities Video Source: https: //www. youtube. com/watch? v=p M 8 y. V 12 fu. Vo
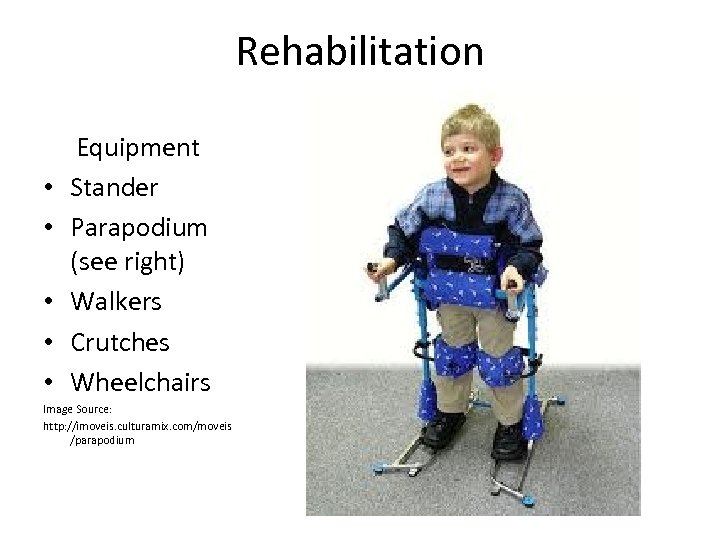
Rehabilitation • • • Equipment Stander Parapodium (see right) Walkers Crutches Wheelchairs Image Source: http: //imoveis. culturamix. com/moveis /parapodium
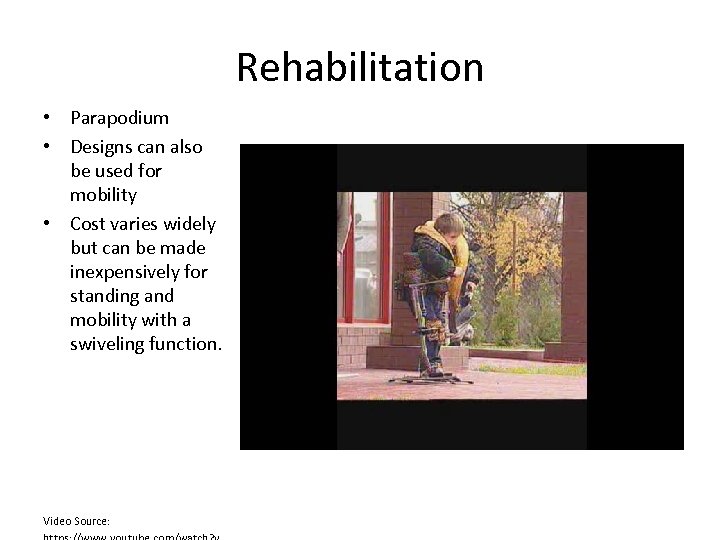
Rehabilitation • Parapodium • Designs can also be used for mobility • Cost varies widely but can be made inexpensively for standing and mobility with a swiveling function. Video Source:
Medical Complications • Latex allergy – Prevalance as high as 72% – Association with latex exposure, neurosurgical procedures – “Latex-Fruit Syndrome” cross reactivity with fruit – Medical Alert Bracelet – Patient/Family Education
• • Cremer R, Mennicken O “Longitudinal study on specific Ig. E against natural rubber latex, banana and kiwi in patients with spina bifida. ”Klin Padiatr. 2011 Nov; 223(6): 352 -5 Retrospective study of sera of 96 patients for specific Ig. E ab against natural rubber latex, banana and kiwi as examples for crossreacting fruit. Tests repeated up to 3 times In the first testing only 2 of 50 latex-Ig. E negative patients (4%) had ab against banana or kiwi. 4 of the 46 latex-Ig. E positive patients (8%) showed ab against banana (2) or kiwi (2), 3 (7%) against both fruit. Symptoms of fruit allergy were presented by 3 patients, all symptomatic patients had high levels of specific fruitab. In the follow-up study 2 patients with low sensitization against NRL lost their NRL ab and their fruit ab, another 2 only the fruit ab, whereas 4 NRL-sensitized patients newly developed ab against banana and 1 against kiwi. Only 2 patients developed ab against fruit without being sensitized against NRL. 7 out of 10 patients with banana and kiwi ab were atopics. Investigators concluded that in most cases the sensitization against fruit follows the natural rubber latex sensitization. There is no need to recommend patients without late sensitization to primarily avoid tropical fruit.
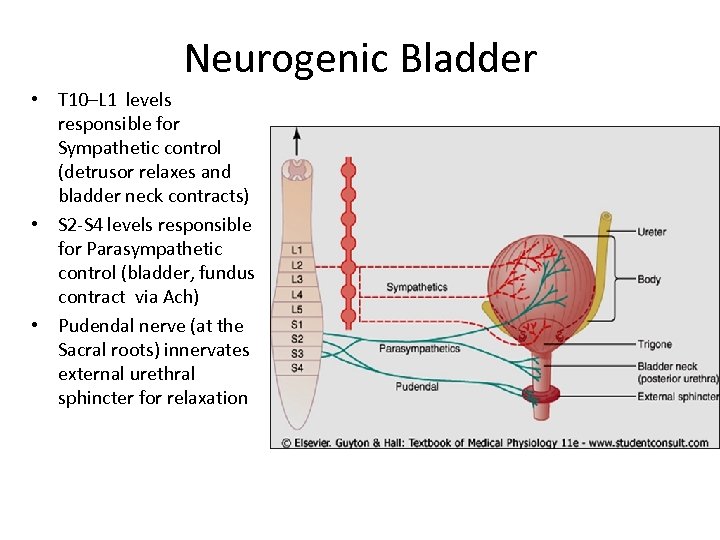
Neurogenic Bladder • T 10–L 1 levels responsible for Sympathetic control (detrusor relaxes and bladder neck contracts) • S 2 -S 4 levels responsible for Parasympathetic control (bladder, fundus contract via Ach) • Pudendal nerve (at the Sacral roots) innervates external urethral sphincter for relaxation
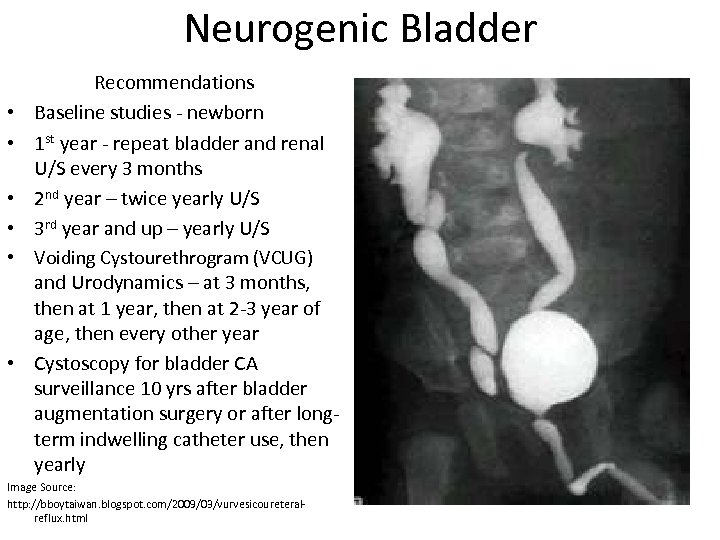
Neurogenic Bladder • • • Recommendations Baseline studies - newborn 1 st year - repeat bladder and renal U/S every 3 months 2 nd year – twice yearly U/S 3 rd year and up – yearly U/S Voiding Cystourethrogram (VCUG) and Urodynamics – at 3 months, then at 1 year, then at 2 -3 year of age, then every other year Cystoscopy for bladder CA surveillance 10 yrs after bladder augmentation surgery or after longterm indwelling catheter use, then yearly Image Source: http: //bboytaiwan. blogspot. com/2009/03/vurvesicoureteralreflux. html
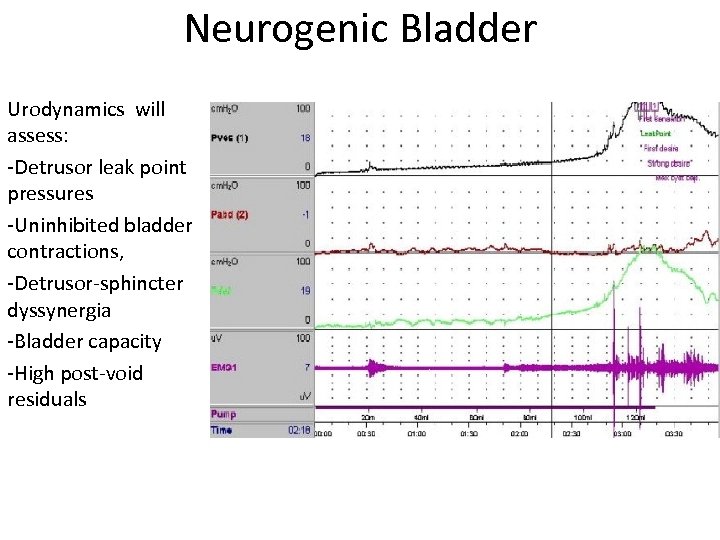
Neurogenic Bladder Urodynamics will assess: -Detrusor leak point pressures -Uninhibited bladder contractions, -Detrusor-sphincter dyssynergia -Bladder capacity -High post-void residuals
Neurogenic Bladder • Treatment goals – preserve renal function and continence, avoid UTI’s, normalize lifestyle • Early treatment even as neonates • Storage dysfunction – anticholinergics • Emptying dysfunction – intermittent catheterization q 4 hrs, avoid Crede’s or Valsalva maneuvers. • Weak detrusor - Bethanecol (Urecholine - muscarinic receptor agonist) rarely used • Hyperactive external urethral sphincter – Baclofen, Neuromuscular re-education, Botox, Surgery (Augmentation) • Mitrofanoff procedure – appendix used to create a catheterizable conduit between bladder and umbilicus • Only treat clinical UTI’s unless there is VUR
Neurogenic Bowel • Most children with SB have poor sphincter tone, absent cutaneous reflex response, and perianal sensory deficit. • Lesion is usually at S 2 -S 4 • Lesions above L 2 have an intact reflex arc to maintain sphincter tone • Bowel Program – Gastrocolic reflex, Polyethylene glycol, high-fiber diet, glycerin suppository, digital stimulation. • Consider enemas after ruling out obstruction via X-ray. • Timed Transanal Irrigation can be used as part of a bowel regimen • Anorectal manometry (measures balloon pressure) and biofeedback with intact or partial sensation has been used to improve symptoms
Medical Complications Osteoporosis • Treatment: Vit D supplementation 400 IU daily • Bisphonate use unclear at this time (most studies on patients with Cerebral Palsy) • Weight bearing exercises not well studied in SB population
Marreiros et al. “Osteoporosis in paediatric patients with spina bifida. ”J Spinal Cord Med. 2012 Jan; 35(1): 9 -21. • Review article concerning fracture risks and low bone density, describing state-ofthe-art treatments and for prevention of secondary osteoporosis. • The main outcome measures were incidence of fractures and risk factors for fracture, an association between BMD and occurrence of fracture, risk factors of low BMD, and effects of pharmacological and non-pharmacological treatments on the incidence of fractures. • A secondary outcome was the occurrence of fractures in relation to the mechanism of injury. • Patients are at increased risk for fractures and low BMD. Risk factors include higher levels of neurological involvement, non-ambulatory status, physical inactivity, hypercalciuria, higher body fat levels, contractures, and a previous spontaneous fracture. • Limitations in the number and quality of studies concerning osteoporosis prevention and treatment in pediatric patients. The safety and efficiency of drugs to treat osteoporosis in adults have not been evaluated satisfactorily in children. • Additionally, true incidence likely higher due to fractures from minor stress or occuring spontaneously that are unrecognized • Distal lateral femoral scan most important area in SB to scan as it is the most common fracture site.

Medical Complications • Obesity – Secondary to immobility – Increased risk of pressure ulcers – Education at earlier age – Preventative anticipatory guidance
Simşek et al“Examination of the relationship between body mass index (BMI) and functional independence level in children with spina bifida. ”Dev Neurorehabil. 2013 Jul 19. • Study examining BMI and functional independence level in children with spina bifida. Patients were 116 children between 5 and 18 years from special education and rehabilitation institution. • Subjects' socio-demographic characteristics, BMI values and functional independence levels recorded using a Wee. FIM (18 items on a 7 point scale). • 55 Female, 51 male patients. 2. 1% Thoracic, 26. 7% Thoracolumbar, 50. 2%Lumbar, 17. 4%Lumbosacral, 3. 5% Sacral • Results showed a negative correlation between BMI and communication and social cognition in girls, no correlation between BMI and Wee. FIM in boys. • Results indicated that body weight in children with spina bifida affected functional independency and that precautions to control weight was important in these children.
Medical Complications • Precocious Puberty – Defined as Tanner Stage II before eight years of age – Associated with accelerated growth and early epiphyseal plate fusion – Central Puberty is a Hypothalamic – Pituitary axis dysfunction. Chiari malformations and Hydrocephalus may be causes of inappropriate secretion of Gn. RH – Labs: Luteinizing hormone, estradiol or testosterone levels – Imaging: Xrays for Bone Age
Associated Medical Issues Learning Disability • Hydrocephalus is a major risk factor • Level of lesion may be a factor • Poor executive functioning noted • Poor nonverbal skills • Superficial level of verbal skill leads to overestimation of verbal abilities – the so called “Cocktail party chatter” effect (Alexander)
Bellin et al. “Family satisfaction, pain, and quality-of-life in emerging adults with spina bifida: a longitudinal analysis” Am J Phys Med Rehabil. 2013 Aug; 92(8): 641 -55. • Use of a Life Course Model to advance knowledge of factors associated with change in quality-of-life (QOL) among emerging adults with Spina Bifida • 48 participants completing questionnaires at two time points, 15 mos apart. Use of 4 quality of life domains (physical health, psychological, social relationships, and environment) measured using the World Health Organization QOL-BREF version. • RESULTS: No significant group-level differences in the QOL domains were found between time 1 and time 2, but there was substantial individual variation in QOL over time. Severity was related to a decline only in psychological QOL. Increased pain was associated with reduced physical health and psychological QOL at time 2, whereas greater family satisfaction was related to improved QOL in several domains. • CONCLUSIONS: Clinicians should be aware of the negative impact of pain and the protective influence of family satisfaction on QOL in emerging adults with SB.
Associated Medical Issues • • • Aging with a Disability Shoulder Impingement Carpal Tunnel Chronic hip, knee pain Chronic pressure ulcers Sexuality Pregnancy
Klingbeil et al. “Aging with a disability. ”Arch Phys Med Rehabil 2004 Jul; 85(7 Suppl 3): S 68 -73 • Focused review highlighting important issues in the care of persons aging with a disability. • Focus on significant medical and rehabilitation issues pertinent to persons with cerebral palsy, spina bifida, postpoliomyelitis syndrome, and selected other neurologic and neuromuscular diseases. • In Spina Bifida, notable issues included overuse syndromes, carpal tunnel, rotator cuff syndrome. • In males, 72% report a capacity for erection, with 80% of patients with dysfunction improved on Viagra. 14% able to father children (related to level of lesion). • In females, 88% have adequate vaginal secretions, and appear to conceive children with low complication rates.
Conclusion • Spina Bifida is a condition that requires initial involvement of multiple specialties • Red flags include changes in neurologic status and physical examination • Identify risk factors for complications (fractures, obesity) • Continuing care evolves throughout lifespan of the patient
References • Alexander, Michael. Pediatric Rehabilitation: Principles and Practice, 4 th ed. New York: Demos Publishing, 2010: 199 -230 • Bellin et al. “Family satisfaction, pain, and quality-of-life in emerging adults with spina bifida: a longitudinal analysis” Am J Phys Med Rehabil. 2013 Aug; 92(8): 641 -55. • Braddom RL. Physical Medicine and Rehabilitation, 4 th ed. Philadelphia : Elsevier Saunders, 2011: 1275 -1292 • Cremer R, Mennicken O. “Longitudinal study on specific Ig. E against natural rubber latex, banana and kiwi in patients with spina bifida. ” Klin Padiatr. 2011 Nov; 223(6): 352 -5. • Dosa et al. “Incidence, prevalence, and characteristics of fractures in children, adolescents, and adults with spina bifida. ” J Spinal Cord Med. 2007; 30 Suppl 1: S 5 -9. • Kaplowitz, Paul B. “Precocious Puberty. ” Medscape. http: //emedicine. medscape. com/article/924002 -overview. Last updated October 14, 2014. Accessed January 30, 2014.
References • Klingbeil et al. “Aging with a disability. ”Arch Phys Med Rehabil 2004 Jul; 85(7 Suppl 3): S 68 -73 • Lee, Kimberly G (Editor). “Myelomeningocoele”. Pubmed. http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0002525/. Last Reviewed October 23, 2013. Accessed Jan 30, 2015 • Marreiros et al. “Osteoporosis in paediatric patients with spina bifida. ”J Spinal Cord Med. 2012 Jan; 35(1): 9 -21. • Mc. Mahon, Mary. Melomeningocele (Spina Bifida) PM&R Knowledge Now. http: //now. aapmr. org/cns/sci-disorders/Pages/Myelomeningocele-(Spina. Bifida). aspx. October 29, 2013. Accessed Jan 30, 2015. • Pauly M, Cremer R “Levels of mobility in children and adolescents with spina bifida-clinical parameters predicting mobility and maintenance of these skills” Eur J Pediatr Surg. 2013 Apr; 23(2): 110 -4
References • Phleps, Patricia E. “Neurulation” Online video clip. UCLA Dept. of Integrative Biology and Physiology. https: //www. ibp. ucla. edu/research/phelps/neuru. php. 2006. Accessed Jan 31 st, 2015. • Rackley, Raymond, Gill Bradley C. “Urodynamic Studies for Urinary Incontinence. ” Medscape. http: //emedicine. medscape. com/article/1988665 -overview#aw 2 aab 6 b 4. Updated Nov. 25, 2013. Accessed Jan 30, 2015. • Saadai P, Farmer DL “Fetal surgery for myelomeningocele. ”Clin Perinatol. 2012 Jun; 39(2): 279 -88. • Simşek et al“Examination of the relationship between body mass index (BMI) and functional independence level in children with spina bifida. ”Dev Neurorehabil. 2013 Jul 19. [Epub ahead of print] • Tulay et al. “Examination of the relationship between body mass index (BMI) and functional independence level in children with spina bifida. ” Developmental Neurorehabilitation (2013) : Web. 18 July 2013
Questions You are asked to see a 12 year old girl with L 4 level Spina Bifida who is noted to have increased difficulty walking for the 2 weeks, with changes in sensation and bowel/bladder incontinence. On examination she exhibits new findings of spasticity and 3+ reflexes at the lower extremities. What is the most likely reason for the change in physical examination? A. hydrocephalus B. tethered cord C. increased spasticity secondary to growth D. Arnold Chiari malformation
Questions You are asked to see a 12 year old girl with L 4 level Spina Bifida who is noted to have increased difficulty walking for the 2 weeks, with changes in sensation and bowel/bladder incontinence. On examination she exhibits new findings of spasticity and 3+ reflexes at the lower extremities. What is the most likely reason for the change in physical examination? A. hydrocephalus B. tethered cord C. increased spasticity secondary to growth D. Arnold Chiari malformation Tethered cord is the 2 nd most common cause of neurologic decline in myelomeningocoele. During periods of growth, tethered cords may become problematic. Findings include increased weakness, scoliosis, spasticity, reflexes. Changes may occur in bowel/bladder continence and sensation.
Questions 7 year old boy with T 12 level Spina bifida presents with several weeks of increased lethargy, weakness and has been doing worse in class participation. He had a VP shunt revised 4 years ago and a low lying cord on MRI that is being followed by Neurosurgery. What is the most likely cause of his symptoms? A) new onset seizures B) hydrocephalus C) syringomyelia D) change in medication
Questions 7 year old boy with T 12 level Spina bifida presents with several weeks of increased lethargy, weakness and has been doing worse in class participation. He had a VP shunt revised 4 years ago and a low lying cord on MRI that is being followed by Neurosurgery. What is the most likely cause of his symptoms? A) new onset seizures B) hydrocephalus C) syringomyelia D) change in medication Hydrocephalus is present in over 90% of patients, with shunt revision in 30 -50% of cases. Lethargy, weakness and behavioral changes can occur. Physical signs in infants can include bulging fontanelles and papilledema. More dangerous signs can include Cushing’s Triad of increasing blood pressure, bradycardia and irregular respirations.
Questions A pediatric patient with spina bifida begins to develop new onset symptoms of aphonia, difficulty swallowing and oculomotor abnormalities. What is your diagnostic impression? A) Hydrocephalus B) Arnold-Chiari malformation C) Tethered cord D) Shunt failure
Questions A pediatric patient with spina bifida begins to develop new onset symptoms of aphonia, difficulty swallowing and oculomotor abnormalities. What is your diagnostic impression? A) Hydrocephalus B) Arnold-Chiari malformation C) Tethered cord D) Shunt failure Arnold-Chiari malformation can be present in 80 -90% of patients. It is often associated with hydrocephalus, with caudal displacement or herniation of the brainstem. Dysphagia and ocular dysfunction can occur. The most severe symptom is respiratory compromise.
Questions A key component in the development of cognitive impairment in Spina bifida is A) Hydrocephalus B) Arnold Chiari malformation C) Agenesis of the corpus callosum D) Tethered cord
Questions A key component in the development of cognitive impairment in Spina bifida is A) Hydrocephalus B) Arnold Chiari malformation C) Agenesis of the corpus callosum D) Tethered cord Learning disability can often go unrecognized in some patients with spina bifida. Some patients appear to have a high verbal ability, as many patients present with “cocktail party chatter”. This can often hide a lower level of cognitive and verbal ability.
Questions After baseline studies in Spina Bifida, bladder and renal ultrasounds are repeated: A) Every 3 months the first year, twice in the second, then yearly afterwards B) Every 6 months the first year, once in the second, then every 2 years C) Every 6 months the first 2 years, twice in the third, then yearly afterwards D) Every 3 months the first year, twice in the second and 3 rd , then yearly
Questions After baseline studies in Spina Bifida, bladder and renal ultrasounds are repeated: A) Every 3 months the first year, twice in the second, then yearly afterwards B) Every 6 months the first year, once in the second, then every 2 years C) Every 6 months the first 2 years, twice in the third, then yearly afterwards D) Every 3 months the first year, twice in the second and 3 rd , then yearly Neurogenic bladder can occur in patients with lesions from T 10 down to the sacral roots. T 10 -L 1 roots are responsible for sympathetic control (detrusor relaxation and bladder neck contraction), the S 2 -S 4 levels control parasympathetic activity (bladder and fundus contraction). The pudendal nerve at the sacral roots innervate the external urethral sphincter for relaxation. Additionally, central nervous system control at the voiding pathway through the pons is also disrupted.
Questions What is the most likely brace for a child with a thoracic level lesion in Spina Bifida? A) HKAFO B) RGO C) KAFO D) AFO E) A and B are acceptable choices
Questions What is the most likely brace for a child with a thoracic level lesion in Spina Bifida? A) HKAFO B) RGO C) KAFO D) AFO E) A and B are acceptable choices Spina Bifida is not a static, symmetric lesion of the spinal cord. The spinal lesions can vary along different levels and from left to right sides of the spinal cord. Patients with thoracic level lesions may have varying levels of strength. HKAFO braces can help support weakened trunk, pelvic an hip muscles. An RGO can help support the trunk and use hip flexor movement to assist in contralateral hip extension during ambulation. Both can be assisted with Lofstrand crutches to use a swing-through gait.
21c20aee8ac725d5bc93ab0c85b68334.ppt