3ff904c44471b2db7943a3945d11c07c.ppt
- Количество слайдов: 35

Spend-down HP Provider Relations October 2010
Agenda – Objectives – Spend-down Rule – Spend-down Eligibility – Eligibility Verification System – Enhanced Spend-down Information – Billing a Member – Claims Processing – Examples of Application of Spend -down – Quiz – Helpful Tools – Questions & Answers 2 Spend-down October 2010
Objectives – To provide a thorough explanation of spend-down rules and eligibility – To explain when it is appropriate to bill Medicaid members for spend-down – To outline claims processing procedures related to spend-down – To provide illustrative examples of how spend-down calculations are made 3 Spend-down October 2010
Spend-down Rule 405 IAC 1 -1 -3. 1 – Providing services to members enrolled under the Medicaid spend-down provision – Subsection (d) states: • • 4 A provider may not refuse service to a Medicaid member pending verification that the monthly spend-down obligation has been satisfied A provider may not refuse service to a Medicaid member solely on the basis of the member’s spend-down status Spend-down October 2010

Define Spend-down eligibility
Spend-down Eligibility – 405 IAC 2 -3 -10 – Spend-down eligibility • Certain types of income are counted in determining Medicaid eligibility • Income greater than a certain threshold is considered "excess income” and is referred to as "spend-down obligation" – Spend-down, therefore, is very similar to a "deductible" • The Medicaid member is liable for their initial Medicaid expenses each month, up to their spenddown amount • Spend-down amounts are deducted from the first claim(s) processed each month Ø Pharmacy providers that bill claims on a point of sale (POS) system receive immediate claim adjudication and may collect the amount of spend-down credit at the time of service 6 Spend-down October 2010
Spend-down Eligibility – Spend-down members are in the Traditional Medicaid, fee-for service program – Spend-down members should not be in Care Select or the risk-based managed care (RBMC) program 7 Spend-down October 2010
Error Codes 0387 and 0388 – Providers may have encountered claim denials due to explanation of benefit (EOB) codes 0387 or 0388 – This service is not payable. The recipient has not satisfied spend-down for the month. – Providers should notify their field consultant when claims deny for these error codes. Note: Claims adjudicate to a paid status when spend-down is credited on a claim. Spend-down-related claims should not adjudicate to a denied status. 8 Spend-down October 2010
Eligibility Verification System Enhanced spend-down information – Enhanced spend-down information became available on the Eligibility Verification System (EVS) beginning January 1, 2010 – Enhanced spend-down information is available on the following EVS tools: • Web inter. Change • Omni • Automated Voice Response (AVR) • Health Insurance Portability and Accountability Act (HIPAA) 270/271 electronic transactions – Review Bulletin BT 200950 for detailed information 9 Spend-down October 2010
Eligibility Verification System Enhanced spend-down information – Spend-Down – Yes – Remaining Obligation For This Month – $241. 00 – This amount is based on claims processed at the time of this eligibility verification • • 10 It is subject to change at any time following this eligibility verification as claims continue to process in the system A provider may bill a member for the spend-down amount deducted from the adjudicated claim; however, with the exception of point of sale (POS) pharmacy claims, the member is not required to pay the provider until the member receives the monthly Medicaid Spend-down Summary Notice listing the amount applied to spend-down Spend-down October 2010
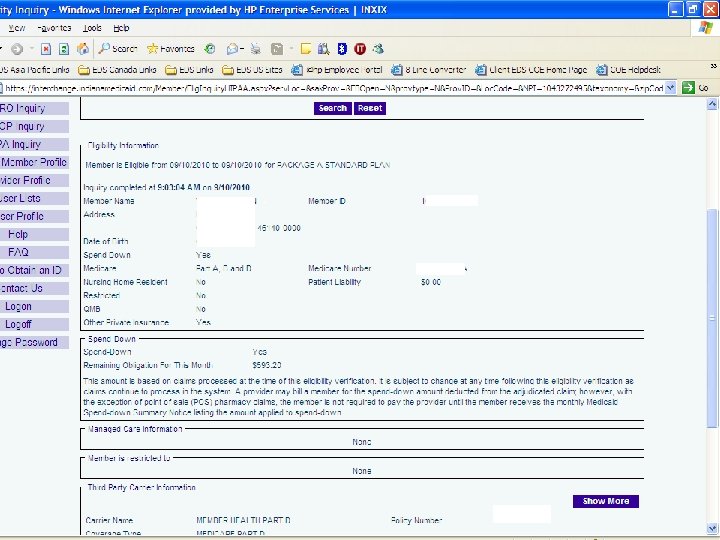
Eligibility Verification System Enhanced spend-down information 11 Spend-down October 2010

Learn Billing a member
Billing a Member – A provider may bill a member for the dollar amount identified beside Adjustment Reason Code (ARC) 178 on the Remittance Advice (RA) statement – This amount will also show up in the "Patient Responsibility" column 13 Spend-down October 2010

Billing a Member – The member is not obligated to pay the provider until the member receives the Medicaid Spend-down Summary Notice listing the amount applied to spend-down • Notices are sent on the second business day following the end of the month • The notices give a detailed itemization of how the spend-down was applied for that month, including provider name, amounts, and dates of service 14 Spend-down October 2010
Billing a Member – Providers should always review the second-to-last page of the Remittance Advice to see if ARC 178 applies to any claims on the RA • This page lists all adjustment reason codes present on the RA – ARC 178 indicates there is a spend-down amount billable to at least one member on that week's RA – Examples: • 132 PREARRANGED DEMONSTRATION PROJECT ADJUSTMENT • 178 PATIENT HAS NOT MET THE REQUIRED SPEND-DOWN REQUIREMENTS • 18 • 24 CHARGES ARE COVERED UNDER A MANAGED CARE PLAN • 94 PROCESSED IN EXCESS OF CHARGES • B 5 15 DUPLICATE CLAIM/SERVICE COVERAGE/PROGRAM GUIDELINES WERE NOT MET OR WERE EXCEEDED Spend-down October 2010
Billing a Member – Providers must bill their usual and customary charge to the Indiana Health Coverage Programs (IHCP) – Members cannot be billed for more than their spend-down amount 16 Spend-down October 2010
Billing a Member – Providers may discharge a member from their care if a member does not adhere to established payment arrangements of outstanding copayments or spend-down – Providers cannot be more restrictive with spend-down members than with other patients 17 Spend-down October 2010

Explain Claims processing
Claims Processing – The first claim processed by the IHCP applies to spend-down, regardless of the date of service within the month – The system uses the billed amount to credit spend-down – Third Party Liability (TPL) amounts are deducted from billed amount prior to crediting spend-down – State-mandated copayments for pharmacy and transportation claims credit spend-down first 19 Spend-down October 2010
Claims Processing The Division of Family Resources may credit spend-down for the following: – Medical expenses incurred by a recipient’s spouse or other person whose income is considered in determining eligibility – Medical services provided by non. Medicaid providers – Services rendered prior to eligibility 20 Spend-down October 2010
Claims Processing Hierarchy of spend-down credits: – Non-claim items entered by the caseworker • Including spousal medical expenses and expenses for children under age 18 – State-mandated transportation and pharmacy copayments – Denied details, when permitted – Paid details 21 Spend-down October 2010
Claims Processing Denied services – Services that are not covered by the Medicaid program do not credit spend-down – Exceptions: • A service that is denied because the member exceeds a benefit limitation, which cannot be overridden with prior authorization (PA), may credit spend-down • Denied services may be split between spend -down months 22 Spend-down October 2010
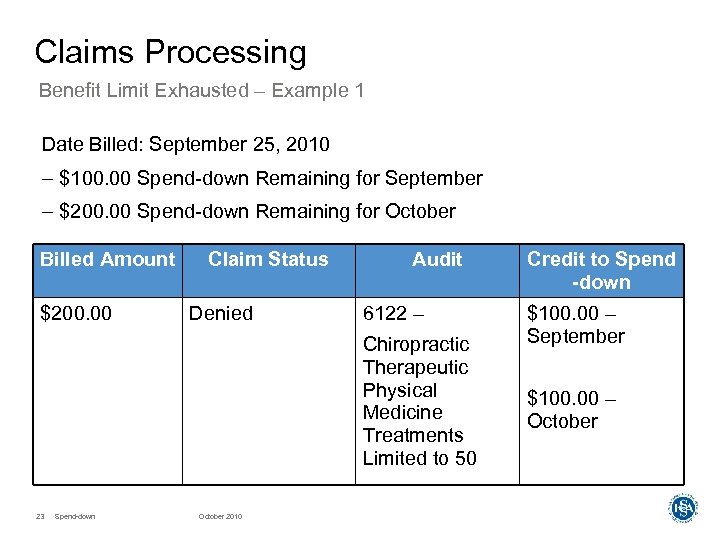
Claims Processing Benefit Limit Exhausted – Example 1 Date Billed: September 25, 2010 – $100. 00 Spend-down Remaining for September – $200. 00 Spend-down Remaining for October Billed Amount $200. 00 Claim Status Denied Audit 6122 – Chiropractic Therapeutic Physical Medicine Treatments Limited to 50 23 Spend-down October 2010 Credit to Spend -down $100. 00 – September $100. 00 – October
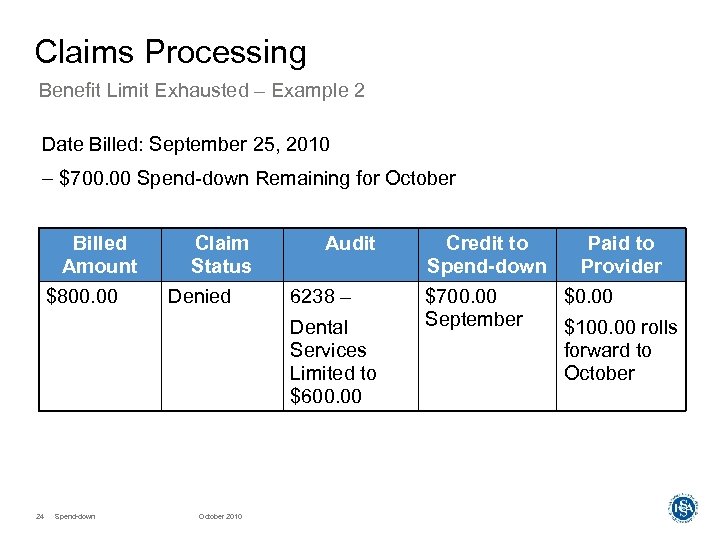
Claims Processing Benefit Limit Exhausted – Example 2 Date Billed: September 25, 2010 – $700. 00 Spend-down Remaining for October Billed Amount $800. 00 Claim Status Denied Audit 6238 – Dental Services Limited to $600. 00 24 Spend-down October 2010 Credit to Spend-down $700. 00 September Paid to Provider $0. 00 $100. 00 rolls forward to October
Claims Processing Voids and replacements – When a claim is paid and credits the member’s spend-down, a provider-initiated void or replacement can cause an increase or decrease in spend-down amount owed to a provider for the claim – In the event a refund is due to the member as a result of a voided claim, the member is notified in the Medicaid Spend-down Summary Notice • The member must have paid the provider to be eligible for a refund – Voids and replacements adjust the spend-down credit immediately 25 Spend-down October 2010
Claims Processing Month-end balancing – If the caseworker makes changes to the spend-down amount during the current month or previous month, the total spend-down amount only decreases, never increases – Each month, HP performs a monthend balancing process that ensures all credits applied by the county are used first 26 Spend-down October 2010
Claims Processing Month-end balancing – This process ensures that any Indiana Client Eligibility System (ICES) nonclaim and claim items and Statemandated copayments are applied correctly – Claims affected by the month-end balancing have an internal control number (ICN) with region code 64 – The amount used to credit spenddown on a claim only decreases by this process 27 Spend-down October 2010
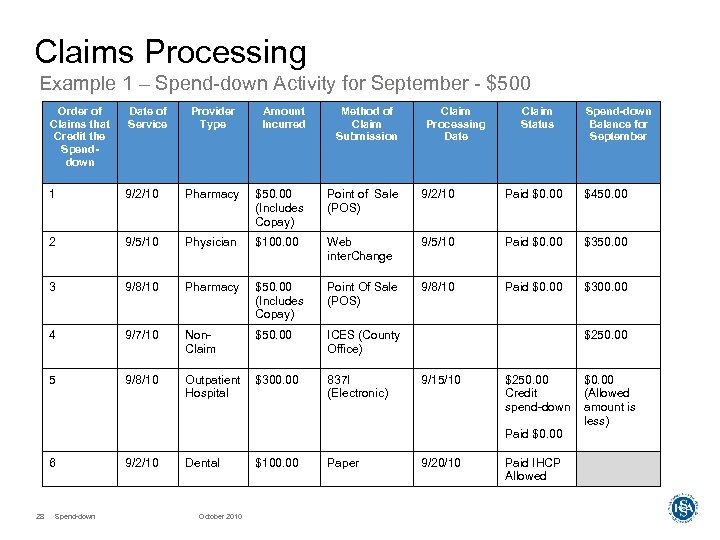
Claims Processing Example 1 – Spend-down Activity for September - $500 Order of Claims that Credit the Spenddown Date of Service Provider Type Amount Incurred Method of Claim Submission Claim Processing Date Claim Status Spend-down Balance for September 1 9/2/10 Pharmacy $50. 00 (Includes Copay) Point of Sale (POS) 9/2/10 Paid $0. 00 $450. 00 2 9/5/10 Physician $100. 00 Web inter. Change 9/5/10 Paid $0. 00 $350. 00 3 9/8/10 Pharmacy $50. 00 (Includes Copay) Point Of Sale (POS) 9/8/10 Paid $0. 00 $300. 00 4 9/7/10 Non. Claim $50. 00 ICES (County Office) 5 9/8/10 Outpatient Hospital $300. 00 837 I (Electronic) $250. 00 9/15/10 $250. 00 Credit spend-down Paid $0. 00 6 28 Spend-down 9/2/10 Dental October 2010 $100. 00 Paper 9/20/10 Paid IHCP Allowed $0. 00 (Allowed amount is less)
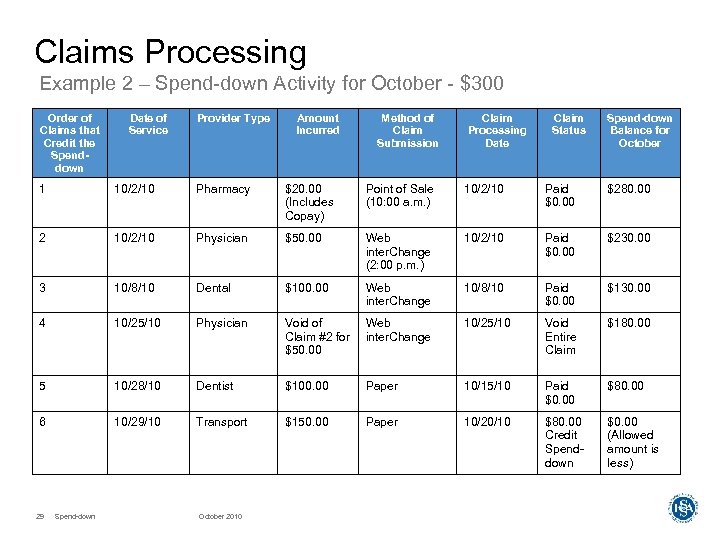
Claims Processing Example 2 – Spend-down Activity for October - $300 Order of Claims that Credit the Spenddown Date of Service Provider Type Amount Incurred Method of Claim Submission Claim Processing Date Claim Status Spend-down Balance for October 1 10/2/10 Pharmacy $20. 00 (Includes Copay) Point of Sale (10: 00 a. m. ) 10/2/10 Paid $0. 00 $280. 00 2 10/2/10 Physician $50. 00 Web inter. Change (2: 00 p. m. ) 10/2/10 Paid $0. 00 $230. 00 3 10/8/10 Dental $100. 00 Web inter. Change 10/8/10 Paid $0. 00 $130. 00 4 10/25/10 Physician Void of Claim #2 for $50. 00 Web inter. Change 10/25/10 Void Entire Claim $180. 00 5 10/28/10 Dentist $100. 00 Paper 10/15/10 Paid $0. 00 $80. 00 6 10/29/10 Transport $150. 00 Paper 10/20/10 $80. 00 Credit Spenddown $0. 00 (Allowed amount is less) 29 Spend-down October 2010
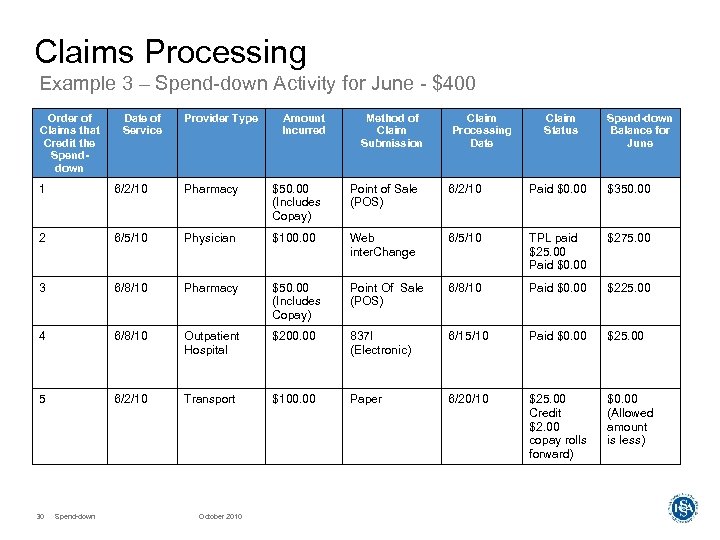
Claims Processing Example 3 – Spend-down Activity for June - $400 Order of Claims that Credit the Spenddown Date of Service Provider Type Amount Incurred Method of Claim Submission Claim Processing Date Claim Status Spend-down Balance for June 1 6/2/10 Pharmacy $50. 00 (Includes Copay) Point of Sale (POS) 6/2/10 Paid $0. 00 $350. 00 2 6/5/10 Physician $100. 00 Web inter. Change 6/5/10 TPL paid $25. 00 Paid $0. 00 $275. 00 3 6/8/10 Pharmacy $50. 00 (Includes Copay) Point Of Sale (POS) 6/8/10 Paid $0. 00 $225. 00 4 6/8/10 Outpatient Hospital $200. 00 837 I (Electronic) 6/15/10 Paid $0. 00 $25. 00 5 6/2/10 Transport $100. 00 Paper 6/20/10 $25. 00 Credit $2. 00 copay rolls forward) $0. 00 (Allowed amount is less) 30 Spend-down October 2010
Spend-down Quiz (True or False) – A provider may refuse to provide service to a member if they verify eligibility and determine the member has a spend-down? – A provider may refuse to provide service to a member who has not yet met his or her spend-down obligation for the month? – A provider may refuse to provide a service to a member who has a legitimate past-due balance for a spend-down, but refuses to pay it? – A provider may bill the member for spend-down as soon as they receive a Remittance Advice that includes ARC 178? – A member must pay his or her spend-down obligation at time of service? – Care Select members may have a spend-down? – Spend-down is credited based on the provider’s usual and customary charge? – Members have no way of knowing how their spend-down was applied each month, unless they keep track of it on their own? 31 Spend-down October 2010
Spend-down Quiz (True or False) – A provider may refuse to provide service to a member if they verify eligibility and determine the member has a spend-down? FALSE – A provider may refuse to provide service to a member who has not yet met his or her spend-down obligation for the month? FALSE – A provider may refuse to provide a service to a member who has a legitimate past-due balance for a spend-down, but refuses to pay it? TRUE – A provider may bill the member for spend-down as soon as they receive a Remittance Advice that includes ARC 178? TRUE – A member must pay his or her spend-down obligation at time of service? FALSE – Care Select members may have a spend-down? FALSE – Spend-down is credited based on the provider’s usual and customary charge? TRUE – Members have no way of knowing how their spend-down was applied each month, unless they keep track of it on their own? FALSE 32 Spend-down October 2010

Find Help Resources Available

Helpful Tools Avenues of resolution – IHCP Web site at www. indianamedicaid. com – IHCP Provider Manual (Web, CD-ROM, or paper) – Customer Assistance • Local • All (317) 655 -3240 others 1 -800 -577 -1278 – Written Correspondence • HP Provider Written Correspondence P. O. Box 7263 Indianapolis, IN 46207 -7263 – Provider field consultant 34 Spend-down October 2010
Q&A
3ff904c44471b2db7943a3945d11c07c.ppt