8154df2e343c4a91c7baaedc89ebe5f5.ppt
- Количество слайдов: 135
 SPECIAL NEEDS
SPECIAL NEEDS
 • Life expectancy in 1921 for the average female was 60 years old and in 1996 life expectancy was 81 years old • • Seniors are grouped into 3 categories: Young old, 55 Middle Old: 75 Oldest Old: 85 and older
• Life expectancy in 1921 for the average female was 60 years old and in 1996 life expectancy was 81 years old • • Seniors are grouped into 3 categories: Young old, 55 Middle Old: 75 Oldest Old: 85 and older
 GERONTOLOGY • Comes from the Greek words “geron” (old man), and “logos” (reason or discourse) • Writings about aging can be found in the scriptures, works by the Greek philosophers and medical writings of the middle ages. • In Canada the study of aging grew slowly from the 1950”s to the 1980’s. • Gerontology has 2 goals: (a) to increase our knowledge about old age and (b) to improve the quality of life in old age.
GERONTOLOGY • Comes from the Greek words “geron” (old man), and “logos” (reason or discourse) • Writings about aging can be found in the scriptures, works by the Greek philosophers and medical writings of the middle ages. • In Canada the study of aging grew slowly from the 1950”s to the 1980’s. • Gerontology has 2 goals: (a) to increase our knowledge about old age and (b) to improve the quality of life in old age.
 MYTHS OF AGING • People tend to hold stereotypes about old age. Some are positive and some are negative. • Some stereotypes result in ageism (prejudice against older people) • This occurs because many people know so little about aging. • How does the media contribute to our opinions?
MYTHS OF AGING • People tend to hold stereotypes about old age. Some are positive and some are negative. • Some stereotypes result in ageism (prejudice against older people) • This occurs because many people know so little about aging. • How does the media contribute to our opinions?
 LONG TERM CARE ACT • One of the acts found in the Standards of Practice. • As a Dental Hygienist in the Province of Ontario we need to be aware of its contents. • Recently amendments were made to the act but the CDHO was not happy since it did not include reference to oral care. • We would like to see the bill amended to include reference to oral assessments and treatments in the Resident’s bill of rights, the Plan of Care and residents assessments
LONG TERM CARE ACT • One of the acts found in the Standards of Practice. • As a Dental Hygienist in the Province of Ontario we need to be aware of its contents. • Recently amendments were made to the act but the CDHO was not happy since it did not include reference to oral care. • We would like to see the bill amended to include reference to oral assessments and treatments in the Resident’s bill of rights, the Plan of Care and residents assessments
 THE STUDY OF GERONTOLOGY Course of study involving three large areas; 1. Biomedicine: this area examines the biochemical causes of aging, studies of reaction time and stress, and studies of dementia. 2. Psychosocial studies; examines the changes that take place within individuals and between studies of memory, learning, and personality as well as studies of friendship and recreation. •
THE STUDY OF GERONTOLOGY Course of study involving three large areas; 1. Biomedicine: this area examines the biochemical causes of aging, studies of reaction time and stress, and studies of dementia. 2. Psychosocial studies; examines the changes that take place within individuals and between studies of memory, learning, and personality as well as studies of friendship and recreation. •
 3. Socioeconomic environmental studies, concentrate on the effects of aging on social structures such as health care and education. It also examines policies, health care systems and formal social supports. Theories of aging: Micro level: focus on individuals and their interactions and are used to explain phenomena like the relationship between adult children and their parents.
3. Socioeconomic environmental studies, concentrate on the effects of aging on social structures such as health care and education. It also examines policies, health care systems and formal social supports. Theories of aging: Micro level: focus on individuals and their interactions and are used to explain phenomena like the relationship between adult children and their parents.
 1. 2. 3. Macro-level theories: examines social structures or structural elements. For example: the impact of public pensions and how gender and income may affect older peoples well being. Both micro and macro theories can take one of three perspectives. The interpretive perspective. The functionalist perspective. The conflict perspective.
1. 2. 3. Macro-level theories: examines social structures or structural elements. For example: the impact of public pensions and how gender and income may affect older peoples well being. Both micro and macro theories can take one of three perspectives. The interpretive perspective. The functionalist perspective. The conflict perspective.
 INTERPRETIVE THEORY • Focuses on micro level of social life. • Examines how people define situations, how they create social order and how they relate to one another in daily life. • Gerontologists have used this perspective to study the quality of life for nursing home residents, the social world of nursing home workers and stress in care giving relationships.
INTERPRETIVE THEORY • Focuses on micro level of social life. • Examines how people define situations, how they create social order and how they relate to one another in daily life. • Gerontologists have used this perspective to study the quality of life for nursing home residents, the social world of nursing home workers and stress in care giving relationships.
 FUNCTIONALIST PERSPECTIVE • This perspective holds that “social order is based on cooperation, interdependence and shared values, adjustment by the individual to society and societal equilibrium. • These theories treat society as a system that consist of social institutions like the family, the military and educational institutions. These systems keep society in balance.
FUNCTIONALIST PERSPECTIVE • This perspective holds that “social order is based on cooperation, interdependence and shared values, adjustment by the individual to society and societal equilibrium. • These theories treat society as a system that consist of social institutions like the family, the military and educational institutions. These systems keep society in balance.
 CONFLICT PERSPECTIVE • This perspective hold that society consists of conflicts between dominant and subordinate social groups. • Focuses on conflict and change in social life. • It traces this conflict to the struggle between the social classes and to the resulting dominance of some groups and the subordination of others in society.
CONFLICT PERSPECTIVE • This perspective hold that society consists of conflicts between dominant and subordinate social groups. • Focuses on conflict and change in social life. • It traces this conflict to the struggle between the social classes and to the resulting dominance of some groups and the subordination of others in society.
 METHODOLOGIES • Quantitative: dominant approach in much of the gerontological research. • Emphasizes relationships between and among factors through numerical measures. • Data is accumulated through surveys and questionnaires. • Researchers summarize responses into numerical values (I. e. Stats Canada)
METHODOLOGIES • Quantitative: dominant approach in much of the gerontological research. • Emphasizes relationships between and among factors through numerical measures. • Data is accumulated through surveys and questionnaires. • Researchers summarize responses into numerical values (I. e. Stats Canada)
 • Qualitative: • Uses a multitude of methods including interviews, field observations and life histories, • Does not use stats or quantification of data to observe findings. • Based on observation of human experience. • More in depth, a “personal look” into human experience.
• Qualitative: • Uses a multitude of methods including interviews, field observations and life histories, • Does not use stats or quantification of data to observe findings. • Based on observation of human experience. • More in depth, a “personal look” into human experience.
 PHYSIOLOGY OF AGING • Maximum life span; the number of years a member of a species can live. • Life expectancy; the number of years at birth an average member of society can expect to live. • Scientists believe the maximum life span is between 110 and 125 years. • Average life expectancy is 70 years.
PHYSIOLOGY OF AGING • Maximum life span; the number of years a member of a species can live. • Life expectancy; the number of years at birth an average member of society can expect to live. • Scientists believe the maximum life span is between 110 and 125 years. • Average life expectancy is 70 years.
 THE PHYSIOLOGY OF AGING • Biologic age is not synonymous with chronologic age and therefore signs of aging appear different chronologic ages in different individuals. • Senescence is the term that describes the normal physiologic process of growing old. • Physical changes take place at various rates and depend on accompanying circumstances (environmental, psychosocial and biologic factors)
THE PHYSIOLOGY OF AGING • Biologic age is not synonymous with chronologic age and therefore signs of aging appear different chronologic ages in different individuals. • Senescence is the term that describes the normal physiologic process of growing old. • Physical changes take place at various rates and depend on accompanying circumstances (environmental, psychosocial and biologic factors)
 BIOLOGICAL THEORIES OF AGING • Theories are either cellular or non cellular • Cellular: genetic theory, based on the genetic makeup of the cell suggests that a cell contains “aging” genes that specify the exact number of times the cell can duplicate itself. The limiting number varies from species to species. • Free radical theory (cellular), body generates free radicals which undermine the integrity of cell membranes, damage DNA and inactivate many enzymes and proteins required for normal functioning of cells. Environmental pollution also promotes free radicals.
BIOLOGICAL THEORIES OF AGING • Theories are either cellular or non cellular • Cellular: genetic theory, based on the genetic makeup of the cell suggests that a cell contains “aging” genes that specify the exact number of times the cell can duplicate itself. The limiting number varies from species to species. • Free radical theory (cellular), body generates free radicals which undermine the integrity of cell membranes, damage DNA and inactivate many enzymes and proteins required for normal functioning of cells. Environmental pollution also promotes free radicals.
 NON CELLULAR THEORIES • Immune system: body begins to make errors in protein synthesis producing proteins that the immune system cannot recognize. The immune system then attacks them as it would any foreign substance, destroying cells and impairing body functions. • Metabolism: Connective tissue all over the body is given structural support by fibers of a class of protein called collagen. Collagen becomes stiffer with age and chemically immobilized.
NON CELLULAR THEORIES • Immune system: body begins to make errors in protein synthesis producing proteins that the immune system cannot recognize. The immune system then attacks them as it would any foreign substance, destroying cells and impairing body functions. • Metabolism: Connective tissue all over the body is given structural support by fibers of a class of protein called collagen. Collagen becomes stiffer with age and chemically immobilized.
 AGING
AGING
 THEORIES • Three social-psychological theories of aging: (most common) • 1. Disengagement theory • 2. Activity Theory • 3. Continuity Theory • Some have validity but some encourage stereotypes
THEORIES • Three social-psychological theories of aging: (most common) • 1. Disengagement theory • 2. Activity Theory • 3. Continuity Theory • Some have validity but some encourage stereotypes
 DISENGAGEMENT THEORY • People naturally disengage from activity as they age. • Describe disengagement as inevitable, universal and satisfying to both the person and society. • Serves an important psychological function: it allows older people to reduce their activity naturally as their strength declines. • Serves a useful social function: it allows older people to leave social roles before the final disengagement • However does not address the fact that all seniors are different!
DISENGAGEMENT THEORY • People naturally disengage from activity as they age. • Describe disengagement as inevitable, universal and satisfying to both the person and society. • Serves an important psychological function: it allows older people to reduce their activity naturally as their strength declines. • Serves a useful social function: it allows older people to leave social roles before the final disengagement • However does not address the fact that all seniors are different!
 Activity Theory: Theory states that as people lose social roles in old age, they stay happiest when they continue or replace these roles with new ones. In other words they should be expected to maintain norms of middle age. • Blames society for disengagement, modern society pushes the aged out of social roles. Unfortunately there are barriers to adults doing this. Finances, physical or mental ability.
Activity Theory: Theory states that as people lose social roles in old age, they stay happiest when they continue or replace these roles with new ones. In other words they should be expected to maintain norms of middle age. • Blames society for disengagement, modern society pushes the aged out of social roles. Unfortunately there are barriers to adults doing this. Finances, physical or mental ability.
 CONTINUING THEORY • Psychological theory (state of mind), how people cope with aging, their outlook • People feel satisfied if they continue the roles and activities of their middle years. • Old age is a continuation of a person’s past and that people will choose the lifestyle in old age that is most like the pattern of life they lived in middle age. • Aging depends on the seniors ability to cope and their psychological make up.
CONTINUING THEORY • Psychological theory (state of mind), how people cope with aging, their outlook • People feel satisfied if they continue the roles and activities of their middle years. • Old age is a continuation of a person’s past and that people will choose the lifestyle in old age that is most like the pattern of life they lived in middle age. • Aging depends on the seniors ability to cope and their psychological make up.
 DENTAL HYGIENE CONSIDERATIONS • For all three theories we need to reinforce responsibility for oral health. • For seniors wishing to remain active we may provide information on programs available to them. • Need to provide a stress free environment that promotes open dialogue.
DENTAL HYGIENE CONSIDERATIONS • For all three theories we need to reinforce responsibility for oral health. • For seniors wishing to remain active we may provide information on programs available to them. • Need to provide a stress free environment that promotes open dialogue.
 SELF DEVELOPMENT IN LATER LIFE • Aging poses a number of challenges to the self. • These come from three sources: (1)social attitudes toward the older people, • (2)physical decline and the (3) loss of social roles. • All of the above challenge the older adults sense of self.
SELF DEVELOPMENT IN LATER LIFE • Aging poses a number of challenges to the self. • These come from three sources: (1)social attitudes toward the older people, • (2)physical decline and the (3) loss of social roles. • All of the above challenge the older adults sense of self.
 PERSONALITY AND SOCIAL CONTEXT • • Three types of environmental effects: 1. Non normative events. 2. Normative events history graded events. 3. Normative age graded events.
PERSONALITY AND SOCIAL CONTEXT • • Three types of environmental effects: 1. Non normative events. 2. Normative events history graded events. 3. Normative age graded events.
 NON-NORMATIVE EVENTS • Norms are shared rules and guidelines. • Non normative events include: accidents, sudden changes in health, or the death of a child, layoffs. • These events may lead to shock and fear. • In 1985 Novak studied response to life events in a sample of 25 healthy, middle-class adults. • Common pattern arose: first; a “challenge” or moment of crisis; second. ; they accepted the challenge and interpreted it as a demand for some response. Third; they responded to or affirmed their lives in spite of the challenge.
NON-NORMATIVE EVENTS • Norms are shared rules and guidelines. • Non normative events include: accidents, sudden changes in health, or the death of a child, layoffs. • These events may lead to shock and fear. • In 1985 Novak studied response to life events in a sample of 25 healthy, middle-class adults. • Common pattern arose: first; a “challenge” or moment of crisis; second. ; they accepted the challenge and interpreted it as a demand for some response. Third; they responded to or affirmed their lives in spite of the challenge.
 HISTORY GRADED EVENTS Changes the lives of many cohorts. • For example people born between 1900 and 1910. They lived through the depression and the two world wars. • Tindale did a study of poor old men in a large Canadian city. Their expectations were not high. • The next cohort group born between 1945 and 1955 expected different things from life.
HISTORY GRADED EVENTS Changes the lives of many cohorts. • For example people born between 1900 and 1910. They lived through the depression and the two world wars. • Tindale did a study of poor old men in a large Canadian city. Their expectations were not high. • The next cohort group born between 1945 and 1955 expected different things from life.
 NORMATIVE AGE GRADED EVENTS • Anthropologists report that all societies move people through a series of age grades. • Age grades define certain rights and responsibilities for their members. • Stages in industrialized society includes: infancy, childhood, adolescence, young adulthood, middle age and old age. • People tend to internalize the age system and know the roper time for a life event to occur. • Life events may be termed age-status synchronization.
NORMATIVE AGE GRADED EVENTS • Anthropologists report that all societies move people through a series of age grades. • Age grades define certain rights and responsibilities for their members. • Stages in industrialized society includes: infancy, childhood, adolescence, young adulthood, middle age and old age. • People tend to internalize the age system and know the roper time for a life event to occur. • Life events may be termed age-status synchronization.
 SOCIAL BREAKDOWN SYNDROME 1. Role loss, lack of norms to guide behaviour and the loss of friends as reference groups. 2. The person begins to depend on external labels for a sense of self. 3. Society may view the aged as incompetent. 4. The older person may assume a dependant role. 5. Older person develops skills that fit the dependant role. 6. The person loses previous skills. 7. People label themselves as sick and inadequate.
SOCIAL BREAKDOWN SYNDROME 1. Role loss, lack of norms to guide behaviour and the loss of friends as reference groups. 2. The person begins to depend on external labels for a sense of self. 3. Society may view the aged as incompetent. 4. The older person may assume a dependant role. 5. Older person develops skills that fit the dependant role. 6. The person loses previous skills. 7. People label themselves as sick and inadequate.
 MODELS OF HEALTHCARE • Medical Model: focuses on treatment of disease and injury. Treatment takes place in doctors office or hospital. Favors surgery, drugs. Taught in med school. • Social Model: involves personal and family counseling, adult day care and home care as part of the health care system. Care takes place in the community, and the MD works with the team. Long term care facilities, meals on wheels, homemakers etc.
MODELS OF HEALTHCARE • Medical Model: focuses on treatment of disease and injury. Treatment takes place in doctors office or hospital. Favors surgery, drugs. Taught in med school. • Social Model: involves personal and family counseling, adult day care and home care as part of the health care system. Care takes place in the community, and the MD works with the team. Long term care facilities, meals on wheels, homemakers etc.
 • Health Promotion Model: focus on prevention and self care. Aims to prevent disease through lifestyle change, increased knowledge about healthy behavior and environmental improvement. • Ie: promoting fitness, dangers of smoking, workplace safety, seatbelt legislation and pollution control for factories.
• Health Promotion Model: focus on prevention and self care. Aims to prevent disease through lifestyle change, increased knowledge about healthy behavior and environmental improvement. • Ie: promoting fitness, dangers of smoking, workplace safety, seatbelt legislation and pollution control for factories.
 CANADA PENSION PLAN • Pays a maximum of approx. $850 per month dependant on your contributions. • You pay into this plan all your life. • Plan starts at age 65, but you may take a reduced pension at age 60 if you wish. Or you may wish to start at age 70.
CANADA PENSION PLAN • Pays a maximum of approx. $850 per month dependant on your contributions. • You pay into this plan all your life. • Plan starts at age 65, but you may take a reduced pension at age 60 if you wish. Or you may wish to start at age 70.
 FINANCES • OAS GIS and SA • OAS (approx. $420 per month for all Canadians despite income) • GIS is for people with no income other than the OAS. (approx. $500 single and $819. Per couple). • SA for spouses between 60 and 64 who are married to a GIS pensioner and to widows or widowers of GIS pensioners. • People do not contribute to these payments.
FINANCES • OAS GIS and SA • OAS (approx. $420 per month for all Canadians despite income) • GIS is for people with no income other than the OAS. (approx. $500 single and $819. Per couple). • SA for spouses between 60 and 64 who are married to a GIS pensioner and to widows or widowers of GIS pensioners. • People do not contribute to these payments.
 SPECIAL NEEDS THE AGING CONTINUES
SPECIAL NEEDS THE AGING CONTINUES
 MANAGING THE AGING CLIENT Aging Process: • Has no exact starting time. • Aging is the continuation of maturation which leads to the deterioration and eventual loss of function of an organ. • Number of cells and their ability to proliferate decreases causing; tissue dehydration, atrophy, fibrosis, diminished elasticity, poor repair and death.
MANAGING THE AGING CLIENT Aging Process: • Has no exact starting time. • Aging is the continuation of maturation which leads to the deterioration and eventual loss of function of an organ. • Number of cells and their ability to proliferate decreases causing; tissue dehydration, atrophy, fibrosis, diminished elasticity, poor repair and death.
 HEALTH STATUS AND ASSESSMENT • Includes a functional appraisal as well as a medical history. ADL: activities of daily living such as; bathing dressing, toileting, transferring from a bed or chair, feeding and continence. IADL: instrumental activities of daily living; such as money management, preparing meals, using the phone
HEALTH STATUS AND ASSESSMENT • Includes a functional appraisal as well as a medical history. ADL: activities of daily living such as; bathing dressing, toileting, transferring from a bed or chair, feeding and continence. IADL: instrumental activities of daily living; such as money management, preparing meals, using the phone
 DH ROLE IN HEALTH PROMOTION • Can provide appropriate wellness information and reinforce positive lifestyle habits of older clients, thus facilitating the human need for self-determination and wholesome body image.
DH ROLE IN HEALTH PROMOTION • Can provide appropriate wellness information and reinforce positive lifestyle habits of older clients, thus facilitating the human need for self-determination and wholesome body image.
 TRADITIONAL AND HEALTH Traditional Programs • Focus on a specific disease or problem (caries or perio). • Teaches clients the causes, progression, treatment and prevention Health Promotion • Does not focus solely on disease identification and eradication but includes a broader conception of activities designed to raise an individuals level of functioning
TRADITIONAL AND HEALTH Traditional Programs • Focus on a specific disease or problem (caries or perio). • Teaches clients the causes, progression, treatment and prevention Health Promotion • Does not focus solely on disease identification and eradication but includes a broader conception of activities designed to raise an individuals level of functioning
 FIVE DIMENSIONS OF WELLNESS • • • Self responsibility Nutritional awareness Physical fitness Stress management Environmental sensitivity
FIVE DIMENSIONS OF WELLNESS • • • Self responsibility Nutritional awareness Physical fitness Stress management Environmental sensitivity
 AGE RELATED Cardio Vascular: (Age Related) Most common change is within the myocardium. Muscle fibers decrease and some are replaced by fibrous tissue, therefore oxygen is used less efficiently. With age the heart valves stiffen and become thicker as the collagen degenerates and fatty deposits accumulate Decreased elasticity of arteries is responsible for decreased blood flow to the kidneys, liver and heart.
AGE RELATED Cardio Vascular: (Age Related) Most common change is within the myocardium. Muscle fibers decrease and some are replaced by fibrous tissue, therefore oxygen is used less efficiently. With age the heart valves stiffen and become thicker as the collagen degenerates and fatty deposits accumulate Decreased elasticity of arteries is responsible for decreased blood flow to the kidneys, liver and heart.
 Pathology Induced: Cardiovascular disease accounts for more than 50% of all deaths among the aged. Most adults over 65 have cv disease most commonly in the form of coronary heart disease or hypertension. It is estimated that only 49% take all prescribed medications Dental Office: monitor vital signs; stress and anxiety may trigger an attack. Unmet human needs to be addressed; protection from health risks and freedom from anxiety and stress.
Pathology Induced: Cardiovascular disease accounts for more than 50% of all deaths among the aged. Most adults over 65 have cv disease most commonly in the form of coronary heart disease or hypertension. It is estimated that only 49% take all prescribed medications Dental Office: monitor vital signs; stress and anxiety may trigger an attack. Unmet human needs to be addressed; protection from health risks and freedom from anxiety and stress.
 RESPIRATORY CHANGES Age related: occur gradually, however the efficiency of the system declines with age. This is due to the decreased elasticity of the muscles of the chest and increased rigidity of internal lung structures. Coupled with cellular decline older adults are more susceptible to respiratory infections.
RESPIRATORY CHANGES Age related: occur gradually, however the efficiency of the system declines with age. This is due to the decreased elasticity of the muscles of the chest and increased rigidity of internal lung structures. Coupled with cellular decline older adults are more susceptible to respiratory infections.
 Pathology Induced: Many respiratory disease are linked to lifestyle. Older adults are more susceptible to bronchitis and pneumonia, asthma and flu. More likely to have inactive tuberculosis than any other group. Dental Hygiene Modifications: positioning, low stress environment, asthma meds on hand, and immaculate infection control.
Pathology Induced: Many respiratory disease are linked to lifestyle. Older adults are more susceptible to bronchitis and pneumonia, asthma and flu. More likely to have inactive tuberculosis than any other group. Dental Hygiene Modifications: positioning, low stress environment, asthma meds on hand, and immaculate infection control.
 MUSCULOSKELETAL CHANGES • Affects the posture, function and gait. • Back becomes humped, the hips, wrist and knees are slightly flexed, the muscles of the arms and legs become flabby and weak, overall height is reduced. • Skeletal system loses mass. Disk become thin, causing a shortening of the torso. Posture changes occur primarily because of calcium loss from bone and as a result of atrophy of cartilage and muscle. • Loss of muscle mass due to a decrease in size and number of muscle fibers.
MUSCULOSKELETAL CHANGES • Affects the posture, function and gait. • Back becomes humped, the hips, wrist and knees are slightly flexed, the muscles of the arms and legs become flabby and weak, overall height is reduced. • Skeletal system loses mass. Disk become thin, causing a shortening of the torso. Posture changes occur primarily because of calcium loss from bone and as a result of atrophy of cartilage and muscle. • Loss of muscle mass due to a decrease in size and number of muscle fibers.
 • Fibrous tissues replaces muscle tissue when muscle tissue no longer regenerates resulting in a decrease in the power of the muscle. • Loss of bone mass coupled with changes in muscle fibers affects bone strength, placing the senior at risk for fractures. • Fractures: - decreased mobilization further bone mass loss. • Ligaments, tendons and joints become hardened, more rigid and less flexible.
• Fibrous tissues replaces muscle tissue when muscle tissue no longer regenerates resulting in a decrease in the power of the muscle. • Loss of bone mass coupled with changes in muscle fibers affects bone strength, placing the senior at risk for fractures. • Fractures: - decreased mobilization further bone mass loss. • Ligaments, tendons and joints become hardened, more rigid and less flexible.
 Pathology Induced: Arthritis: the most chronic disability in older adults. Osteoarthritis is a defect of the articular cartilage (causing the gradual loss of cushioning). As exposure continues, inflammation sets in. Rheumatoid arthritis affects connective tissues throughout the body. (hands and feet most common). Osteoporosis: demineralization of the bone and a decrease in bone mass. Four times more prevalent in women.
Pathology Induced: Arthritis: the most chronic disability in older adults. Osteoarthritis is a defect of the articular cartilage (causing the gradual loss of cushioning). As exposure continues, inflammation sets in. Rheumatoid arthritis affects connective tissues throughout the body. (hands and feet most common). Osteoporosis: demineralization of the bone and a decrease in bone mass. Four times more prevalent in women.
 DENTAL HYGIENE CONSIDERATIONS Unmet Human Needs; 1. Freedom from pain 2. Body image. 3. Protection from health risks. 4. Biologically sound dentition. 5. Mucous membrane integrity. 6. Responsibility for oral health.
DENTAL HYGIENE CONSIDERATIONS Unmet Human Needs; 1. Freedom from pain 2. Body image. 3. Protection from health risks. 4. Biologically sound dentition. 5. Mucous membrane integrity. 6. Responsibility for oral health.
 VISION • Visual acuity—fuzzy lens becomes more rigid. • May cause dizziness • Get to their level • Pupil size decrease with age—need more light. • Perception changes • Takes longer to focus • Colours can be difficult to disseminate. Lens becomes more opaque and yellows with age.
VISION • Visual acuity—fuzzy lens becomes more rigid. • May cause dizziness • Get to their level • Pupil size decrease with age—need more light. • Perception changes • Takes longer to focus • Colours can be difficult to disseminate. Lens becomes more opaque and yellows with age.
 Pathology Induced: Cataracts: most common disability of the aging eye. The lens is becoming more opaque. When it interferes with the performance of activities it is removed. Glaucoma: increased pressure in the eye caused by fluid. If left—blindness. Client may report “halos” around light, blurred vision, headaches and tired eyes. Macular degeneration: deterioration in the membrane between the retina and underlying blood vessels.
Pathology Induced: Cataracts: most common disability of the aging eye. The lens is becoming more opaque. When it interferes with the performance of activities it is removed. Glaucoma: increased pressure in the eye caused by fluid. If left—blindness. Client may report “halos” around light, blurred vision, headaches and tired eyes. Macular degeneration: deterioration in the membrane between the retina and underlying blood vessels.
 Dental Office Considerations; Listen to your clients…do they have symptoms? Refer them if they do. Clear a pathway for them Directions and educational materials should be in large print.
Dental Office Considerations; Listen to your clients…do they have symptoms? Refer them if they do. Clear a pathway for them Directions and educational materials should be in large print.
 HEARING LOSS Gradual Affects social interaction Presbycusis—hearing loss associated with aging. General loss of volume. Take mask off, face the client Do not speak from the other room Speak clearly in normal fashion Do not over exaggerate. Ask if message was understood. Have client turn off hearing aids when using ultrasonic or highspeed.
HEARING LOSS Gradual Affects social interaction Presbycusis—hearing loss associated with aging. General loss of volume. Take mask off, face the client Do not speak from the other room Speak clearly in normal fashion Do not over exaggerate. Ask if message was understood. Have client turn off hearing aids when using ultrasonic or highspeed.
 CHANGES IN TASTE AND SMELL • Decreased taste and smell especially denture wearers. • Eat less • Don’t eat the proper food (which may affect their cognitive and social abilities) • May experience dysgeusia (altered taste) • Loss of smell is not clearly understood, but it also affects taste diminished appetite
CHANGES IN TASTE AND SMELL • Decreased taste and smell especially denture wearers. • Eat less • Don’t eat the proper food (which may affect their cognitive and social abilities) • May experience dysgeusia (altered taste) • Loss of smell is not clearly understood, but it also affects taste diminished appetite
 LOSS OF KINESTHETIC ABILITY • Refers to touch, the ability to discriminate temperatures, perceive spatial relationships, and discern pain. • Vulnerable to accidental falls. • Be sure to secure loose rugs and watch the placement of furniture and equipment. • May affect fine motor skills.
LOSS OF KINESTHETIC ABILITY • Refers to touch, the ability to discriminate temperatures, perceive spatial relationships, and discern pain. • Vulnerable to accidental falls. • Be sure to secure loose rugs and watch the placement of furniture and equipment. • May affect fine motor skills.
 DENTAL HYGIENE CARE Office or clinical facilities : Eliminate physical barriers • Hazards are to be removed (equipment/rugs) Assessment: • Patient History: detailed medical and dental history takes on particular significance. • Suggestions for good communication: • Eliminate distractions • Sit facing the patient because hearing may be a problem. • Speak slowly and clearly. • Be courteous and respectful…do not call them by their first name unless granted permission to do so.
DENTAL HYGIENE CARE Office or clinical facilities : Eliminate physical barriers • Hazards are to be removed (equipment/rugs) Assessment: • Patient History: detailed medical and dental history takes on particular significance. • Suggestions for good communication: • Eliminate distractions • Sit facing the patient because hearing may be a problem. • Speak slowly and clearly. • Be courteous and respectful…do not call them by their first name unless granted permission to do so.
 MEDICATIONS Older clients take more medications. 1. Obtain the correct list. Ask the client to bring in the bottles, or a written copy of the labels (you may have to speak to the MD. 2. Have a reference handy for checking meds. 3. Review all meds to determine: side effects, possible drug interactions with any drugs you may recommend, and finally, a clear understanding of the clients state of health to assure the clinician that the treatment is the best
MEDICATIONS Older clients take more medications. 1. Obtain the correct list. Ask the client to bring in the bottles, or a written copy of the labels (you may have to speak to the MD. 2. Have a reference handy for checking meds. 3. Review all meds to determine: side effects, possible drug interactions with any drugs you may recommend, and finally, a clear understanding of the clients state of health to assure the clinician that the treatment is the best
 NEED FOR ANTIBIOTICS • More seniors have conditions that may require premed. • Heart problems. • Joint replacement. • Uncontrolled diabetes. • Chemotherapy • Steroid treatments Vital Signs: should be taken at each and every appointment for our senior clients.
NEED FOR ANTIBIOTICS • More seniors have conditions that may require premed. • Heart problems. • Joint replacement. • Uncontrolled diabetes. • Chemotherapy • Steroid treatments Vital Signs: should be taken at each and every appointment for our senior clients.
 IO AND EO More susceptible to oral cancer in the later years. A thorough exam is recommended at each and every recall appointment. Periodontal exam: Incidence of perio disease increases with age. Recession, wide embrasure space allows for a larger surface area for biofilm accumulation. Exposed cementum with areas of abrasion or dental caries can create undercut areas where special adaptation of plaque removal devices is needed. Decreased saliva production, restorations and prosthetics. Lack of dexterity
IO AND EO More susceptible to oral cancer in the later years. A thorough exam is recommended at each and every recall appointment. Periodontal exam: Incidence of perio disease increases with age. Recession, wide embrasure space allows for a larger surface area for biofilm accumulation. Exposed cementum with areas of abrasion or dental caries can create undercut areas where special adaptation of plaque removal devices is needed. Decreased saliva production, restorations and prosthetics. Lack of dexterity
 PREVENTIVE CARE Modify recommendations. Care for removable prosthetics Use of a power toothbrush Use toothpaste with fluoride, and a desensitizing agent if needed. • Xerostomia • Diet and nutritional counseling (they need same nutrients but not in the same quantity • •
PREVENTIVE CARE Modify recommendations. Care for removable prosthetics Use of a power toothbrush Use toothpaste with fluoride, and a desensitizing agent if needed. • Xerostomia • Diet and nutritional counseling (they need same nutrients but not in the same quantity • •
 PREVENTIVE CARE PLAN • Seniors may require more frequent recalls and debridement therapies. Approach to instruction: • Sometimes change occurs gradually—be patient!
PREVENTIVE CARE PLAN • Seniors may require more frequent recalls and debridement therapies. Approach to instruction: • Sometimes change occurs gradually—be patient!
 ORAL CONDITIONS IN THE AGED
ORAL CONDITIONS IN THE AGED
 DENTAL CHANGES • Age related: • Enamel becomes darker and develops surface cracks (acquired lamellae). • Arrested caries appears brownish-black. • Occlusal fissures appear darkly stained. • Avoid vigorous exploration! • Cementum undergoes increased fluoride and magnesium content. Secondary cementum is deposited at the ends of roots and in the furcas
DENTAL CHANGES • Age related: • Enamel becomes darker and develops surface cracks (acquired lamellae). • Arrested caries appears brownish-black. • Occlusal fissures appear darkly stained. • Avoid vigorous exploration! • Cementum undergoes increased fluoride and magnesium content. Secondary cementum is deposited at the ends of roots and in the furcas
 Dentin: secondary dentin is formed and dentin sclerosis occurs, resulting in loss of vitality for the dentin. Pulp: decreased blood supply and the amount of fibers increases. The size of the pulp chamber reduces due to calcifications. Attrition and abrasion also common. Root caries and coronal caries are active Older adults are more likely to develop new coronal and root caries at a greater rate than the adult population.
Dentin: secondary dentin is formed and dentin sclerosis occurs, resulting in loss of vitality for the dentin. Pulp: decreased blood supply and the amount of fibers increases. The size of the pulp chamber reduces due to calcifications. Attrition and abrasion also common. Root caries and coronal caries are active Older adults are more likely to develop new coronal and root caries at a greater rate than the adult population.
 Root caries----are the most prevalent Caries control and prevention must address three factors: 1) biofilm removal 2) diet (reducing refined carbs) and 3) topical fluoride. Periodontal Changes: Age Related: increase in alveolar bone porosity and a decrease in cortical width. Osteoporosis primarily affects decreases in bone mass and increases in porosity. Reduced metabolism and healing can influence the quality of the bone and greatly affect the older adult’s ability to wear prosthetics.
Root caries----are the most prevalent Caries control and prevention must address three factors: 1) biofilm removal 2) diet (reducing refined carbs) and 3) topical fluoride. Periodontal Changes: Age Related: increase in alveolar bone porosity and a decrease in cortical width. Osteoporosis primarily affects decreases in bone mass and increases in porosity. Reduced metabolism and healing can influence the quality of the bone and greatly affect the older adult’s ability to wear prosthetics.
 Gingiva: epithelium shows no significant changes with aging, however there is a thinning of the epithelium. There is an increase in gingival width due to the increase in alveolar bone. Perio ligament: there are many cellular changes occurring however, clinical changes in perio structures alone are therapeutically insignificant. Pathology Induced: if OSC is good then age has no significant effect on perio status.
Gingiva: epithelium shows no significant changes with aging, however there is a thinning of the epithelium. There is an increase in gingival width due to the increase in alveolar bone. Perio ligament: there are many cellular changes occurring however, clinical changes in perio structures alone are therapeutically insignificant. Pathology Induced: if OSC is good then age has no significant effect on perio status.
 However, there are studies confirming an association between increased age and increased recession, loss of attachment, and gingival inflammation. Perio in middle age can be a good predictor of perio in old age. Oral Mucosal Changes: Age related: no significant changes. Pathology: more related to systemic factors ie: xerostomia (dry lips and elasticity reduced(dehydrated). Fungal infections
However, there are studies confirming an association between increased age and increased recession, loss of attachment, and gingival inflammation. Perio in middle age can be a good predictor of perio in old age. Oral Mucosal Changes: Age related: no significant changes. Pathology: more related to systemic factors ie: xerostomia (dry lips and elasticity reduced(dehydrated). Fungal infections
 • Conditions such as Parkinson's may cause cheilitis (constant drooling). • Ill fitting dentures: may result in irritation and infection. Clients who do not remove their dentures are more prone to infection and irritation as well as fungal growth. Tongue Changes: Age Related: decrease in the number and sensitivity of the papillae, more sublingual varicosities.
• Conditions such as Parkinson's may cause cheilitis (constant drooling). • Ill fitting dentures: may result in irritation and infection. Clients who do not remove their dentures are more prone to infection and irritation as well as fungal growth. Tongue Changes: Age Related: decrease in the number and sensitivity of the papillae, more sublingual varicosities.
 • Pathology induced: may be nutritional factors such as low iron (anemia). This result in atrophic glossitis, tongue appears smooth, shiny and denuded. Clients may complain of a burning sensation. • Tongue may increase in size due to missing teeth or pernicious anemia. Salivary Gland Changes: reduction in flow usually attributed to systemic disease, rad therapy, tumors or medications.
• Pathology induced: may be nutritional factors such as low iron (anemia). This result in atrophic glossitis, tongue appears smooth, shiny and denuded. Clients may complain of a burning sensation. • Tongue may increase in size due to missing teeth or pernicious anemia. Salivary Gland Changes: reduction in flow usually attributed to systemic disease, rad therapy, tumors or medications.
 Sjogrens Syndrome (autoimmune, affecting salivary glands-common in post menopausal women) Drug induced oral changes: most adults take more than 3 meds. Chances of interaction is 6% if taking two meds, and increases to 50% if taking 5 and 100% if taking 8 meds!! Xerostomia: management Drug Induced gingival hyperplasia: phenytoin is a very common medication causing hyperplasia. Plaque control may reduce the amount. Nifedipine and cyclosporine may also cause overgrowth.
Sjogrens Syndrome (autoimmune, affecting salivary glands-common in post menopausal women) Drug induced oral changes: most adults take more than 3 meds. Chances of interaction is 6% if taking two meds, and increases to 50% if taking 5 and 100% if taking 8 meds!! Xerostomia: management Drug Induced gingival hyperplasia: phenytoin is a very common medication causing hyperplasia. Plaque control may reduce the amount. Nifedipine and cyclosporine may also cause overgrowth.
 DH PROCESS OF CARE AND THE AGING CLIENT • Assessment and Diagnosis; • Functional and health assessment. Have client provide a list of all meds. Be alert to cognitive and physical impairments. Be alert to internal and external lesions which the client may not see during the IO/EO • Communication skills imperative here! Biopsy suspicious lesions. Take appropriate radiographs. • Short appointments; morning is best and always provide an appointment card with time and date.
DH PROCESS OF CARE AND THE AGING CLIENT • Assessment and Diagnosis; • Functional and health assessment. Have client provide a list of all meds. Be alert to cognitive and physical impairments. Be alert to internal and external lesions which the client may not see during the IO/EO • Communication skills imperative here! Biopsy suspicious lesions. Take appropriate radiographs. • Short appointments; morning is best and always provide an appointment card with time and date.
 PLANNING AND IMPLEMENTATION • Planning is often more complex due to the fact that many may have at least one chronic condition. Oral situation may be compromised. Attitude of client is important and so is that of the DH. • Avoid trauma because there is a reduction in healing capacity. Loss of elasticity of the lips and dry mouth may make retraction more uncomfortable. Incorporate rinses to supplement mechanical biofilm removal. Fluoride: 0. 05% Na. Fl rinse for dry mouth. If unable to rinse; 1. 1% Na. Fl or. 4% stannous gel in a tray can be applied by toothbrush. If they had radiation or if they have severe xerostomia or rampant decay; then use in a tray for 5 minutes.
PLANNING AND IMPLEMENTATION • Planning is often more complex due to the fact that many may have at least one chronic condition. Oral situation may be compromised. Attitude of client is important and so is that of the DH. • Avoid trauma because there is a reduction in healing capacity. Loss of elasticity of the lips and dry mouth may make retraction more uncomfortable. Incorporate rinses to supplement mechanical biofilm removal. Fluoride: 0. 05% Na. Fl rinse for dry mouth. If unable to rinse; 1. 1% Na. Fl or. 4% stannous gel in a tray can be applied by toothbrush. If they had radiation or if they have severe xerostomia or rampant decay; then use in a tray for 5 minutes.
 CONTINUED • Saliva substitutes are recommended. • Exposed root surfaces may require home applied fluoride and an in office desensitization program. • Upon completion of treatment return the chair back slowly!
CONTINUED • Saliva substitutes are recommended. • Exposed root surfaces may require home applied fluoride and an in office desensitization program. • Upon completion of treatment return the chair back slowly!
 EVALUATION • Need to be re evaluated more frequently due to chronic changes. • Allow a longer time to assess the results of NSPT due to decreased healing of tissues. Perform all necessary post care indices. • Re care interval may be less than usual; some seniors cannot clean as effectively.
EVALUATION • Need to be re evaluated more frequently due to chronic changes. • Allow a longer time to assess the results of NSPT due to decreased healing of tissues. Perform all necessary post care indices. • Re care interval may be less than usual; some seniors cannot clean as effectively.
 ON A FINAL NOTE…. • Keep appointment time short. • Ensure that your office is accessible. • Communications; all info should be in writing for the client. • Informed consent; be sure client can provide it. • Multiple health concerns…. consult with MD.
ON A FINAL NOTE…. • Keep appointment time short. • Ensure that your office is accessible. • Communications; all info should be in writing for the client. • Informed consent; be sure client can provide it. • Multiple health concerns…. consult with MD.
 SPECIAL NEEDS DENTURE CARE
SPECIAL NEEDS DENTURE CARE
 FIXED AND REMOVABLE DENTURES • Tooth loss affects: speech, eating, facial expression and appearance. • Edentulous means without teeth (30% of adults 65+, approx 50% of Canadians 65+ are edentulous) • Prosthesis is a fixed or removable appliance that is functionally and cosmetically designed to replace a missing tooth or teeth. • Clients with prosthetics may present with special needs.
FIXED AND REMOVABLE DENTURES • Tooth loss affects: speech, eating, facial expression and appearance. • Edentulous means without teeth (30% of adults 65+, approx 50% of Canadians 65+ are edentulous) • Prosthesis is a fixed or removable appliance that is functionally and cosmetically designed to replace a missing tooth or teeth. • Clients with prosthetics may present with special needs.
 RISK FACTORS FOR TOOTH LOSS • • • Dental caries Periodontal diseases Low socioeconomic status Inadequate access to professional oral care. Low frequency of professional care. Poor daily oral hygiene
RISK FACTORS FOR TOOTH LOSS • • • Dental caries Periodontal diseases Low socioeconomic status Inadequate access to professional oral care. Low frequency of professional care. Poor daily oral hygiene
 OTHER FACTORS ASSOCIATED WITH TOOTH LOSS Psychological Factors: -client attitude and values influence success of care. -wholesome facial image is unmet human need (fear of aging, decreased self esteem, insecurity, fear of rejection, unrealistic expectations for tooth replacement). -human response to tooth loss can go through the stages of bereavement.
OTHER FACTORS ASSOCIATED WITH TOOTH LOSS Psychological Factors: -client attitude and values influence success of care. -wholesome facial image is unmet human need (fear of aging, decreased self esteem, insecurity, fear of rejection, unrealistic expectations for tooth replacement). -human response to tooth loss can go through the stages of bereavement.
 Physiologic factors: although prosthesis can restore many oral functions when a person experiences tooth loss, remodeling of the orofacial tissues is invariably encountered. Placing prosthetics introduces unfamiliar forces that contribute to: (1)residual ridge and alveolar bone resorption. (2)Oral mucous membrane remodeling and (3)loss of orofacial muscle tone. Following tooth extraction major bony changes such as residual alveolar ridge resorption occur within the first year and continue throughout life
Physiologic factors: although prosthesis can restore many oral functions when a person experiences tooth loss, remodeling of the orofacial tissues is invariably encountered. Placing prosthetics introduces unfamiliar forces that contribute to: (1)residual ridge and alveolar bone resorption. (2)Oral mucous membrane remodeling and (3)loss of orofacial muscle tone. Following tooth extraction major bony changes such as residual alveolar ridge resorption occur within the first year and continue throughout life
 Generally, older adults resorb bone at a faster rate because of anatomic, metabolic, functional and prosthetic factors. Ridge resorption: Diminishes stability and retention of the prosthesis. Changes in the mandible differ from the maxilla. (resorption is 4 x greater in mand). Sharp spikes in the bone may cause pain with prosthetics. Exostoses and tori may cause problems.
Generally, older adults resorb bone at a faster rate because of anatomic, metabolic, functional and prosthetic factors. Ridge resorption: Diminishes stability and retention of the prosthesis. Changes in the mandible differ from the maxilla. (resorption is 4 x greater in mand). Sharp spikes in the bone may cause pain with prosthetics. Exostoses and tori may cause problems.
 TYPES OF APPLIANCES Changing from a natural dentition to a prosthetic can be very stressful. Human needs may include; wholesome facial image, freedom from anxiety and stress and a biologically sound dentition. If needs cannot be met success may be hampered. Prosthetics are fixed or removable: Full (complete) or partial.
TYPES OF APPLIANCES Changing from a natural dentition to a prosthetic can be very stressful. Human needs may include; wholesome facial image, freedom from anxiety and stress and a biologically sound dentition. If needs cannot be met success may be hampered. Prosthetics are fixed or removable: Full (complete) or partial.
 REMOVABLE PARTIAL/FULL/IMPLANT DENTURES Can be removed by the client. Partial Dentures may be supported by retainer clasps around the natural teeth or by a combination of natural teeth and oral tissues. Complete or Full dentures replace the entire arch. If a client has undergone surgery (ie to repair a cleft or oral cancer), an obturator is an appliance that closes an opening. Implant dentures are designed to fit over implant fixtures that are inserted partially or entirely into living bone. This provides increased stability for the wearer.
REMOVABLE PARTIAL/FULL/IMPLANT DENTURES Can be removed by the client. Partial Dentures may be supported by retainer clasps around the natural teeth or by a combination of natural teeth and oral tissues. Complete or Full dentures replace the entire arch. If a client has undergone surgery (ie to repair a cleft or oral cancer), an obturator is an appliance that closes an opening. Implant dentures are designed to fit over implant fixtures that are inserted partially or entirely into living bone. This provides increased stability for the wearer.
 MISSING TEETH… • Physical appearance: alveolar bone resorption affects facial image. • Loss of facial height, reduced lip support, sunken maxillary appearance, increased chin prominence. • Decreased stability, unbalanced occlusion, tmj disorders and dissatisfaction with appearance. • Role of the DH is to boost self esteem.
MISSING TEETH… • Physical appearance: alveolar bone resorption affects facial image. • Loss of facial height, reduced lip support, sunken maxillary appearance, increased chin prominence. • Decreased stability, unbalanced occlusion, tmj disorders and dissatisfaction with appearance. • Role of the DH is to boost self esteem.
 Speech disturbances: transient speech difficulties and oral resonance problems are expected but soon disappear. -instruct clients to practice in front of a mirror. -if problem persists return to DDS for evaluation. Masticatory Efficiency: loss of periodontal support and proprioreception. Advise clients to avoid repeated use of anterior teeth for incision, gum chewing and sticky foods. Consume food in smaller pieces, lengthen chewing time and evenly distribute food to both the left and right sides while chewing.
Speech disturbances: transient speech difficulties and oral resonance problems are expected but soon disappear. -instruct clients to practice in front of a mirror. -if problem persists return to DDS for evaluation. Masticatory Efficiency: loss of periodontal support and proprioreception. Advise clients to avoid repeated use of anterior teeth for incision, gum chewing and sticky foods. Consume food in smaller pieces, lengthen chewing time and evenly distribute food to both the left and right sides while chewing.
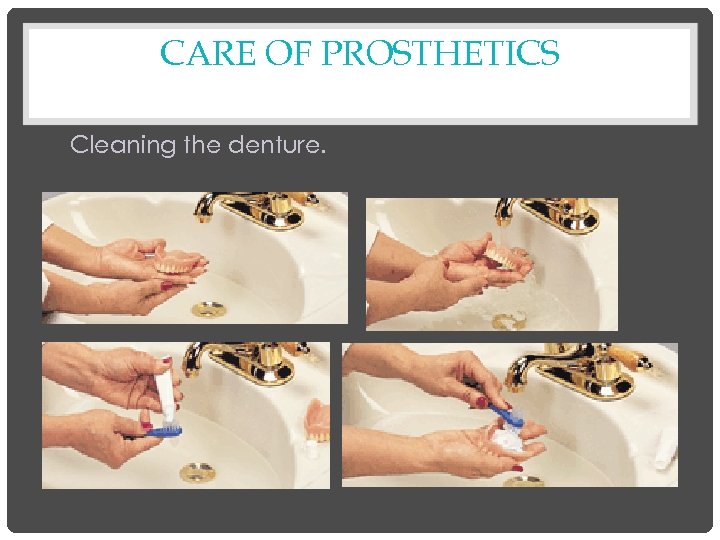 CARE OF PROSTHETICS Cleaning the denture.
CARE OF PROSTHETICS Cleaning the denture.
 Care Continued:
Care Continued:
 DENTURE CLEANING Products: Alkaline Hypochlorite: bactericidal. Fungicidal, bleaches stain and may inhibit calculus. Cannot use on metal!! Alkaline Peroxide: some antibacterial effect, removes stain. Safe for metals. Ultrasonics: do they really help? Antimicrobials: antimicrobial action by chemical agent.
DENTURE CLEANING Products: Alkaline Hypochlorite: bactericidal. Fungicidal, bleaches stain and may inhibit calculus. Cannot use on metal!! Alkaline Peroxide: some antibacterial effect, removes stain. Safe for metals. Ultrasonics: do they really help? Antimicrobials: antimicrobial action by chemical agent.
 SAFE EFFECTIVE SOLUTION (NO METAL) • • • 1 tablespoon of sodium hypochlorite 1 teaspoon of calgon (or other mild detergent) 4 ounces of water Rinse thoroughly before putting back into the mouth. **IMPORTANT SLIDE – QUESTION WAS ON THE LAST BOARD EXAM
SAFE EFFECTIVE SOLUTION (NO METAL) • • • 1 tablespoon of sodium hypochlorite 1 teaspoon of calgon (or other mild detergent) 4 ounces of water Rinse thoroughly before putting back into the mouth. **IMPORTANT SLIDE – QUESTION WAS ON THE LAST BOARD EXAM
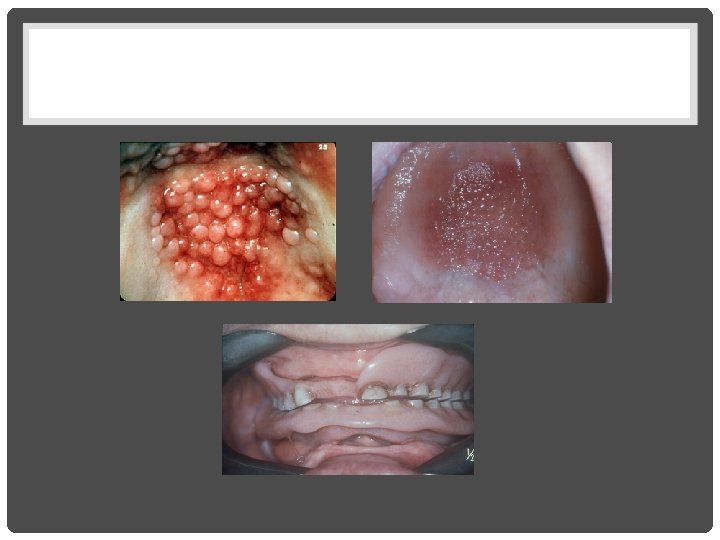
 ORAL HYGIENE Accumulation of plaque, stain, and calculus on the denture and oral mucosa leads to offensive odor and mucosal irritations. Denture stomatitis: inflammation of the oral mucosa underlying the denture, characterized by redness, pain and swelling. Denture sore mouth. Papillary Hyperplasia: abnormal increase in the volume of tissue as a result of irritation. Chronic Candidiasis: long term thrush infection.
ORAL HYGIENE Accumulation of plaque, stain, and calculus on the denture and oral mucosa leads to offensive odor and mucosal irritations. Denture stomatitis: inflammation of the oral mucosa underlying the denture, characterized by redness, pain and swelling. Denture sore mouth. Papillary Hyperplasia: abnormal increase in the volume of tissue as a result of irritation. Chronic Candidiasis: long term thrush infection.
 DENTURE INDUCED LESIONS Tissues react differently between individuals. Response to continuous wear, poor oral hygiene or reaction to poor fit of the denture. Lesions are divided into three categories; 1. Reactive/traumatic 2. Infections 3. Mixed reactive and infectious. • •
DENTURE INDUCED LESIONS Tissues react differently between individuals. Response to continuous wear, poor oral hygiene or reaction to poor fit of the denture. Lesions are divided into three categories; 1. Reactive/traumatic 2. Infections 3. Mixed reactive and infectious. • •
 REACTIVE/TRAUMATIC LESIONS • Commonly secondary to acute or chronic injury. • Lesions include: ulcers, hyperkeratosis, and denture induced hyperplasia (freely moving tissue over the ridges) Infectious Lesions: Denture stomatitis: most common inflammation. (up to 65%) Angular cheilitis: mixed bacterial and fungal infection. Small amounts of saliva accumulate at the commissural angles which promotes the colonization of yeast. Tissues are cracked/eroded and can be painful. Chronic Candidiasis: primarily responsible for denture stomatitis. Appears on the palatal mucosa rather than on the mandible.
REACTIVE/TRAUMATIC LESIONS • Commonly secondary to acute or chronic injury. • Lesions include: ulcers, hyperkeratosis, and denture induced hyperplasia (freely moving tissue over the ridges) Infectious Lesions: Denture stomatitis: most common inflammation. (up to 65%) Angular cheilitis: mixed bacterial and fungal infection. Small amounts of saliva accumulate at the commissural angles which promotes the colonization of yeast. Tissues are cracked/eroded and can be painful. Chronic Candidiasis: primarily responsible for denture stomatitis. Appears on the palatal mucosa rather than on the mandible.
 • Mixed Reactive and Infectious Lesions: -both trauma and infection are causative factors in these types of lesions. -papillary hyperplasia is an example. -presents with a cobblestone type of appearance. -may predispose the client to Candida Albicans
• Mixed Reactive and Infectious Lesions: -both trauma and infection are causative factors in these types of lesions. -papillary hyperplasia is an example. -presents with a cobblestone type of appearance. -may predispose the client to Candida Albicans
 HELPFUL TIPS FOR YOU. • Remember! Removal of a denture for you to assess the tissues may be traumatic for the client. Please be empathetic. • Let the client remove their dentures; if unable to do so; provide assistance. • Explain the importance of proper maintenance visits and home care. • Educate your client on the various products such as denture adhesives or strips. • Educate your clients on how to examine their tissues and their dentures.
HELPFUL TIPS FOR YOU. • Remember! Removal of a denture for you to assess the tissues may be traumatic for the client. Please be empathetic. • Let the client remove their dentures; if unable to do so; provide assistance. • Explain the importance of proper maintenance visits and home care. • Educate your client on the various products such as denture adhesives or strips. • Educate your clients on how to examine their tissues and their dentures.
 ADVICE FOR THE CLIENT Explain the importance of replacing missing teeth Remove dentures every night. Massage tissues with thumb and index finger. Clean tissues with a very soft brush. Check tissues for any sore spots or white areas. Regular checkups to ensure fit and check tissues. Explain the possible harmful effects of improper care. • Recommend techniques and products. • •
ADVICE FOR THE CLIENT Explain the importance of replacing missing teeth Remove dentures every night. Massage tissues with thumb and index finger. Clean tissues with a very soft brush. Check tissues for any sore spots or white areas. Regular checkups to ensure fit and check tissues. Explain the possible harmful effects of improper care. • Recommend techniques and products. • •
 SPECIAL NEEDS
SPECIAL NEEDS
 GENERAL DESCRIPTIONS OF DENTAL HYGIENE CARE • Although each neurologic deficit has its own specific cause and pathology, the clinical manifestations may be similar. • In these situations the oral clinical findings and special considerations may be similar and we will describe them in general terms first.
GENERAL DESCRIPTIONS OF DENTAL HYGIENE CARE • Although each neurologic deficit has its own specific cause and pathology, the clinical manifestations may be similar. • In these situations the oral clinical findings and special considerations may be similar and we will describe them in general terms first.
 ORAL CLINICAL FINDINGS • Many clients with neurologic deficits exhibit extensive plaque biofilm accumulations, food debris, supra and sub gingival calculus, dental caries, and gingival inflammation. • The major factor is the client’s inability to perform adequate self care because of impaired motor coordination.
ORAL CLINICAL FINDINGS • Many clients with neurologic deficits exhibit extensive plaque biofilm accumulations, food debris, supra and sub gingival calculus, dental caries, and gingival inflammation. • The major factor is the client’s inability to perform adequate self care because of impaired motor coordination.
 • There may be inadequate sensation or generalized muscle weakness and fatigue. • Severe debilitation may result in dependence on a caregiver who are at times overwhelmed with the responsibility.
• There may be inadequate sensation or generalized muscle weakness and fatigue. • Severe debilitation may result in dependence on a caregiver who are at times overwhelmed with the responsibility.
 • Oral musculature disturbances observed in many of these clients interfere with the self cleansing mechanism of the tongue, cheek and lip, therefore food and debris is not cleared effectively. • Biofilm and food debris retention is accentuated by the consumption of a soft carbohydrate rich diet, which the client chooses due to problems with mastication and swallowing.
• Oral musculature disturbances observed in many of these clients interfere with the self cleansing mechanism of the tongue, cheek and lip, therefore food and debris is not cleared effectively. • Biofilm and food debris retention is accentuated by the consumption of a soft carbohydrate rich diet, which the client chooses due to problems with mastication and swallowing.
 DENTAL HYGIENE CARE SPECIAL CONSIDERATIONS • Frequent dental hygiene appointments are required to achieve and maintain optimal oral health. • Appointments are best scheduled early in the morning due to weakness and fatigue of the client. • Allow additional appointment time so that the client does not feel rushed in terms of communication and physical movements.
DENTAL HYGIENE CARE SPECIAL CONSIDERATIONS • Frequent dental hygiene appointments are required to achieve and maintain optimal oral health. • Appointments are best scheduled early in the morning due to weakness and fatigue of the client. • Allow additional appointment time so that the client does not feel rushed in terms of communication and physical movements.
 • Clients may be ambulatory but using assistive walking devices or may be confined to a wheelchair. Their needs for assistance will vary. • Some will need assistance others have developed their own coping mechanisms. • Clients with swallowing difficulty and a diminished gag reflex may need to be seated in a more upright position.
• Clients may be ambulatory but using assistive walking devices or may be confined to a wheelchair. Their needs for assistance will vary. • Some will need assistance others have developed their own coping mechanisms. • Clients with swallowing difficulty and a diminished gag reflex may need to be seated in a more upright position.
 • Optimal suctioning and limiting the amount of water may also help to prevent airway obstruction. • Mouth props and bite blocks are helpful but can only be used sparingly. • Instrument fulcrums may need additional stabilization. • Client may need to be restrained or secured with soft belts, pillows. • Use of the client caregiver is often the best support for the client.
• Optimal suctioning and limiting the amount of water may also help to prevent airway obstruction. • Mouth props and bite blocks are helpful but can only be used sparingly. • Instrument fulcrums may need additional stabilization. • Client may need to be restrained or secured with soft belts, pillows. • Use of the client caregiver is often the best support for the client.
 ORAL SELF CARE INSTRUCTIONS • Depends on the client’s level of energy and motor coordination. • Client’s capabilities need to be assessed so that devices may be recommended or created to compensate for physical limitations. • Client may need to prop up their elbows to minimize fatigue.
ORAL SELF CARE INSTRUCTIONS • Depends on the client’s level of energy and motor coordination. • Client’s capabilities need to be assessed so that devices may be recommended or created to compensate for physical limitations. • Client may need to prop up their elbows to minimize fatigue.
 OTHER ADAPTIVE AIDS…. . • Pump dispensers for toothpaste, toothpaste tubes with flip top lids, and floss holders. • Respiratory problems may contraindicate a foamy toothpaste so a brand without the detergent sodium lauryl sulfate might be recommended. • Only clients who are able to control swallowing and gagging should use mouthrinses
OTHER ADAPTIVE AIDS…. . • Pump dispensers for toothpaste, toothpaste tubes with flip top lids, and floss holders. • Respiratory problems may contraindicate a foamy toothpaste so a brand without the detergent sodium lauryl sulfate might be recommended. • Only clients who are able to control swallowing and gagging should use mouthrinses
 MORE INFORMATION FOR YOU! • Recommend nutritious foods. Clients with xerostomia would benefit from fluoride rinses and brush on gels. Do not use alcohol based rinses of course. • Saliva substitutes, sugar free mints. • Clients requiring assistance…provide instructions to the caregiver…written is often the best.
MORE INFORMATION FOR YOU! • Recommend nutritious foods. Clients with xerostomia would benefit from fluoride rinses and brush on gels. Do not use alcohol based rinses of course. • Saliva substitutes, sugar free mints. • Clients requiring assistance…provide instructions to the caregiver…written is often the best.
 DYSFUNCTIONS OF THE MOTOR SYSTEM • Motor actions require the integration of the CNS and the PNS. • Disorders affecting the cells of the cerebellum and basil ganglia project to the motor regions of the cerebral cortex. • There is disturbing of the movements which produce abnormalities of muscle tone, abnormal posturing and tremours.
DYSFUNCTIONS OF THE MOTOR SYSTEM • Motor actions require the integration of the CNS and the PNS. • Disorders affecting the cells of the cerebellum and basil ganglia project to the motor regions of the cerebral cortex. • There is disturbing of the movements which produce abnormalities of muscle tone, abnormal posturing and tremours.
 • Hyperkinesis: increased movement • Hypokinesis: lessening of muscle movement. • A decrease in associated movements (ie swinging the arms) or abnormal involuntary movements. • Degenerative, metabolic, or vascular diseases, toxins, infections, trauma or neoplasm's may cause these abnormalities.
• Hyperkinesis: increased movement • Hypokinesis: lessening of muscle movement. • A decrease in associated movements (ie swinging the arms) or abnormal involuntary movements. • Degenerative, metabolic, or vascular diseases, toxins, infections, trauma or neoplasm's may cause these abnormalities.
 CEREBROVASCULAR ACCIDENT (STROKE) Cerebrovascular Accident: CVA or stroke. Usually caused by a thrombus, embolism or a hemorrhage. CVA is the most common neurologic cause of problems related to coordination and mobility. Ischemia leads to necrosis of brain tissue, hemorrhage, causes leakage of blood into the brain tissue exerting pressure on the brain tissue TIA Transient Ischemic Attack persists for less than 24 hours and is followed by complete recovery. Most TIA’s do not last for more 10 -20 minutes. .
CEREBROVASCULAR ACCIDENT (STROKE) Cerebrovascular Accident: CVA or stroke. Usually caused by a thrombus, embolism or a hemorrhage. CVA is the most common neurologic cause of problems related to coordination and mobility. Ischemia leads to necrosis of brain tissue, hemorrhage, causes leakage of blood into the brain tissue exerting pressure on the brain tissue TIA Transient Ischemic Attack persists for less than 24 hours and is followed by complete recovery. Most TIA’s do not last for more 10 -20 minutes. .
 It is the third most common cause of death in the United States (behind heart disease and cancer. The major risk factor is hypertension. • Often experience temporary or permanent paralysis and may require adaptive aids or assistance in performing oral self care.
It is the third most common cause of death in the United States (behind heart disease and cancer. The major risk factor is hypertension. • Often experience temporary or permanent paralysis and may require adaptive aids or assistance in performing oral self care.
 DEMENTIA • Also called organic brain syndrome, dementia is a progressive brain impairment that interferes with normal intellectual functioning. • Symptoms: significant loss of three of the following: cognition, memory, language, recognition, visual and spatial skills and personality
DEMENTIA • Also called organic brain syndrome, dementia is a progressive brain impairment that interferes with normal intellectual functioning. • Symptoms: significant loss of three of the following: cognition, memory, language, recognition, visual and spatial skills and personality
 • Characterized by a progressive intellectual decline that eventually leads to deterioration of occupational, social, and interpersonal functions. • Onset is usually insidious with memory loss attributed to aging: then other areas of cognition are affected: orientation, language, perceptions of ability to learn new skills, judgment.
• Characterized by a progressive intellectual decline that eventually leads to deterioration of occupational, social, and interpersonal functions. • Onset is usually insidious with memory loss attributed to aging: then other areas of cognition are affected: orientation, language, perceptions of ability to learn new skills, judgment.
 • In severe cases the individual loses self care skills and becomes incontinent. • Dementia is classified as either reversible or irreversible. Cause: tumours, fever, trauma, environmental toxins, chronic lung disease, alcoholism, drug abuse and stroke, brain tumour.
• In severe cases the individual loses self care skills and becomes incontinent. • Dementia is classified as either reversible or irreversible. Cause: tumours, fever, trauma, environmental toxins, chronic lung disease, alcoholism, drug abuse and stroke, brain tumour.
 ALZHEIMER'S DISEASE • Most common form of dementia. Characterized by clumping of the neurofibrils. • More prevalent in females (2 -3 x more). • 3 separate stages (see D &W) which can vary from patient to patient and the decline may take up to 15 years. • If you have a parent or a sibling with the disease you are 4 -5 x more likely to develop the disease. (10%-30% have the inherited type).
ALZHEIMER'S DISEASE • Most common form of dementia. Characterized by clumping of the neurofibrils. • More prevalent in females (2 -3 x more). • 3 separate stages (see D &W) which can vary from patient to patient and the decline may take up to 15 years. • If you have a parent or a sibling with the disease you are 4 -5 x more likely to develop the disease. (10%-30% have the inherited type).
 TREATMENT AND PROGNOSIS • There is no cure for AD treatment is aimed at prevention, slowing the progression of the disease and improving quality of life. • On average from onset of symptoms to death is 8 years. Death is usually due to a secondary infection (urinary, or pneumonia)
TREATMENT AND PROGNOSIS • There is no cure for AD treatment is aimed at prevention, slowing the progression of the disease and improving quality of life. • On average from onset of symptoms to death is 8 years. Death is usually due to a secondary infection (urinary, or pneumonia)
 PARKINSON’S DISEASE Chronic progressive disorder caused by pathologic changes in the basal ganglia of the cerebrum resulting in a deficiency of dopamine. Characterized by muscle rigidity, tremors, loss of postural stability and slowness of spontaneous movements. There is no impairment of intellectual function.
PARKINSON’S DISEASE Chronic progressive disorder caused by pathologic changes in the basal ganglia of the cerebrum resulting in a deficiency of dopamine. Characterized by muscle rigidity, tremors, loss of postural stability and slowness of spontaneous movements. There is no impairment of intellectual function.
 • Clients with Parkinson’s may demonstrate excess salivation and drooling. • Facial expression is motionless with diminished eye blinking. • Tremors in lips and tongue are common and clients may have difficulty swallowing
• Clients with Parkinson’s may demonstrate excess salivation and drooling. • Facial expression is motionless with diminished eye blinking. • Tremors in lips and tongue are common and clients may have difficulty swallowing
 • Most common treatment is the medication: Levodopa which is a dopamine replacement therapy. (this med can cause low blood pressure. . be careful with client positioning). • Be cautious with involuntary movement. • Caregiver will eventually have to provide care for the client
• Most common treatment is the medication: Levodopa which is a dopamine replacement therapy. (this med can cause low blood pressure. . be careful with client positioning). • Be cautious with involuntary movement. • Caregiver will eventually have to provide care for the client
 DRUG THERAPY IN THE ELDERLY • As many as 50% of seniors do not take their meds. • They tend to forget to take it, take the wrong dose, take their meds at the wrong time, or forget which pills require food or drink with them to avoid GI distress or prolong the effects of the meds. • As DH’s we must determine the meds they are on and the possible interaction.
DRUG THERAPY IN THE ELDERLY • As many as 50% of seniors do not take their meds. • They tend to forget to take it, take the wrong dose, take their meds at the wrong time, or forget which pills require food or drink with them to avoid GI distress or prolong the effects of the meds. • As DH’s we must determine the meds they are on and the possible interaction.
 • The terms “as needed” may confuse them and as a result the client takes them routinely or not at all. • They tend to misuse the “over the counter” meds. If the client doesn’t “feel” the med is working, they discontinue it’s use. (hypertensive meds)
• The terms “as needed” may confuse them and as a result the client takes them routinely or not at all. • They tend to misuse the “over the counter” meds. If the client doesn’t “feel” the med is working, they discontinue it’s use. (hypertensive meds)
 PEOPLE WITH DISABILITIES
PEOPLE WITH DISABILITIES
 DEFINING DISABILITY • Disability describes a condition that is either permanent or semi permanent and that interferes with an individuals ability to do something independent. A limitation in a major life activity. • Cause could be trauma, birth defects, accidents or disease. • Differences may be physical, mental or psychological.
DEFINING DISABILITY • Disability describes a condition that is either permanent or semi permanent and that interferes with an individuals ability to do something independent. A limitation in a major life activity. • Cause could be trauma, birth defects, accidents or disease. • Differences may be physical, mental or psychological.
 • Impairment: occurs as a result of accident, or disease and includes any loss or abnormality in function which may or may not be permanent. • Activity limitation: is difficulty in executing activities • Participation restriction: is the inability to take part in conventional life situations for reasons that may be beyond the clients control.
• Impairment: occurs as a result of accident, or disease and includes any loss or abnormality in function which may or may not be permanent. • Activity limitation: is difficulty in executing activities • Participation restriction: is the inability to take part in conventional life situations for reasons that may be beyond the clients control.
 CLASSIFICATION OF DISABILITIES Developmental: occurs congenitally or during the developmental period of the child, a period lasting from birth to 22 years. They are generally chronic in nature, continue throughout life and appear as mental, physical, or combined impairments. Acquired: occurs after the age of 22 or is caused by a disease, trauma, or injury to the body.
CLASSIFICATION OF DISABILITIES Developmental: occurs congenitally or during the developmental period of the child, a period lasting from birth to 22 years. They are generally chronic in nature, continue throughout life and appear as mental, physical, or combined impairments. Acquired: occurs after the age of 22 or is caused by a disease, trauma, or injury to the body.
 CLASSIFICATIONS OF DISABILITIES • Developmental (Mental retardation, cerebral palsy, autism, epilepsy) • Sensory (vision and hearing) • Orthopaedic (paralysis, spinal cord injury, missing extremities) • Medical (CV, Arthritis, AIDS, Cancer etc). • Cognitive Impairment (depression, Alzheimer’s, dementia, stroke, anorexia/bulimia) • Degenerative Nervous system: (MS, Parkinson’s, Alzheimer’s) • Communication. (Aphasia, Apraxia)
CLASSIFICATIONS OF DISABILITIES • Developmental (Mental retardation, cerebral palsy, autism, epilepsy) • Sensory (vision and hearing) • Orthopaedic (paralysis, spinal cord injury, missing extremities) • Medical (CV, Arthritis, AIDS, Cancer etc). • Cognitive Impairment (depression, Alzheimer’s, dementia, stroke, anorexia/bulimia) • Degenerative Nervous system: (MS, Parkinson’s, Alzheimer’s) • Communication. (Aphasia, Apraxia)
 EVALUATING FUNCTIONAL STATUS • Each person presents with varying levels of ability. The dental hygienist must evaluate the ADL of the client. • Impairments can affect five aspects of function. Communication, movement, mental ability, medical health and sensory perception. • Many clients present with complex oral care needs associated with their condition or their medications to control the symptoms of their condition. Please see chart on page 770, D and W. It examines 4 levels of impairment and their needs regarding communication, movement and mental ability.
EVALUATING FUNCTIONAL STATUS • Each person presents with varying levels of ability. The dental hygienist must evaluate the ADL of the client. • Impairments can affect five aspects of function. Communication, movement, mental ability, medical health and sensory perception. • Many clients present with complex oral care needs associated with their condition or their medications to control the symptoms of their condition. Please see chart on page 770, D and W. It examines 4 levels of impairment and their needs regarding communication, movement and mental ability.
 LEVELS OF IMPAIRMENT • Level one is near normal function • Level two is simulation of normal function with adaptive equipment, medication or methods • Level three is simulation of normal function with aid of third party. • Level four is simulation of normal function not possible. Each level will look at communication, movement and mental ability.
LEVELS OF IMPAIRMENT • Level one is near normal function • Level two is simulation of normal function with adaptive equipment, medication or methods • Level three is simulation of normal function with aid of third party. • Level four is simulation of normal function not possible. Each level will look at communication, movement and mental ability.
 BARRIERS TO HEALTHCARE • Financial • Architectural (barrier free design) it is the law that buildings and businesses maintain access to the clients with disabilities. • Transportation • Attitudes of healthcare professionals • Attitude of the client.
BARRIERS TO HEALTHCARE • Financial • Architectural (barrier free design) it is the law that buildings and businesses maintain access to the clients with disabilities. • Transportation • Attitudes of healthcare professionals • Attitude of the client.
 ASSISTIVE DEVICES Tools used to achieve independence in daily functions. Walking devices: canes, leg braces, crutches, and walkers all work by bearing the weight of the client while walking. The device should remain close to the client for access when needed. Once seated always place the device where the client can see it or at least tell them where it is. Wheelchairs: clients may be treated in the wheelchair or transferred to the dental chair.
ASSISTIVE DEVICES Tools used to achieve independence in daily functions. Walking devices: canes, leg braces, crutches, and walkers all work by bearing the weight of the client while walking. The device should remain close to the client for access when needed. Once seated always place the device where the client can see it or at least tell them where it is. Wheelchairs: clients may be treated in the wheelchair or transferred to the dental chair.
 INTERACTING WITH CLIENTS • Avoid the term “handicap” • A person is not their disability (ie not my multiple sclerosis client) • An impairment should not override other client characteristics; therefore address the impairment only if relevant or necessary. • Do not overemphasize their successes • Client is not necessarily sick!!
INTERACTING WITH CLIENTS • Avoid the term “handicap” • A person is not their disability (ie not my multiple sclerosis client) • An impairment should not override other client characteristics; therefore address the impairment only if relevant or necessary. • Do not overemphasize their successes • Client is not necessarily sick!!
 PROSTHETIC DEVICES Prosthetic devices enhance client appearance and improve function. (ie arms, legs etc). Other devices may replace structures or organs due to trauma or disease. Privacy is paramount for the client. If required removal must be for as short a time as is possible. Assistive listening devices: Hearing Aids. May be worn directly in the ear or behind the ear. As a DH you must be aware of high pitched noises from the handpiece or ultrasonic's. It is advisable that the clients turn their hearing aids off or down during treatment.
PROSTHETIC DEVICES Prosthetic devices enhance client appearance and improve function. (ie arms, legs etc). Other devices may replace structures or organs due to trauma or disease. Privacy is paramount for the client. If required removal must be for as short a time as is possible. Assistive listening devices: Hearing Aids. May be worn directly in the ear or behind the ear. As a DH you must be aware of high pitched noises from the handpiece or ultrasonic's. It is advisable that the clients turn their hearing aids off or down during treatment.
 • Visually impaired: corrective lenses. DH should provide material with large print with adequate contrast. Blind clients may wear dark glasses to protect the eyes from light sensitivity. Blind clients depend on tactile sensitivity. Greet the client by grasping their hands. Guide them to the operatory by gently placing their nondominant hand gently under your elbow. Always give specific directions. When you arrive in the room, describe it to the client.
• Visually impaired: corrective lenses. DH should provide material with large print with adequate contrast. Blind clients may wear dark glasses to protect the eyes from light sensitivity. Blind clients depend on tactile sensitivity. Greet the client by grasping their hands. Guide them to the operatory by gently placing their nondominant hand gently under your elbow. Always give specific directions. When you arrive in the room, describe it to the client.
 • Assistive speaking devices: recreate sounds that mimic normal speech patterns. Electronic speech devices held against the throat detect vibrations of air passing through the throat as the person mimics normal speech. The device reproduces a noise that sounds like an automated, robot like speech. • Elimination devices: Paralyzed clients may have a catheter for assistance with urination. Clients who have had ileostomies or colostomies will have elimination devices.
• Assistive speaking devices: recreate sounds that mimic normal speech patterns. Electronic speech devices held against the throat detect vibrations of air passing through the throat as the person mimics normal speech. The device reproduces a noise that sounds like an automated, robot like speech. • Elimination devices: Paralyzed clients may have a catheter for assistance with urination. Clients who have had ileostomies or colostomies will have elimination devices.
 • Communication devices; paralyzed clients have a variety of devices to aid in accomplishing the ADL. The most common oral device is the mouth stick. They are used mainly for communication such as typing on a keyboard or pressing the buttons to dial a telephone. They may be used to use and operate appliances. • Oral Considerations; may traumatize the teeth (which in addition to perio may cause tooth loss). Therefore what two human needs could be paramount to these clients?
• Communication devices; paralyzed clients have a variety of devices to aid in accomplishing the ADL. The most common oral device is the mouth stick. They are used mainly for communication such as typing on a keyboard or pressing the buttons to dial a telephone. They may be used to use and operate appliances. • Oral Considerations; may traumatize the teeth (which in addition to perio may cause tooth loss). Therefore what two human needs could be paramount to these clients?
 Mouthsticks may contribute to muscle fatigue, taste, tmj discomfort. We must be careful when constructing a mouthstick. Key Considerations for mouthstick: Should minimize occlusal trauma Should not cause tooth movement Should be inexpensive and easy to clean. Should be designed to hold a variety of implements to meet needs of client. Should be comfortable.
Mouthsticks may contribute to muscle fatigue, taste, tmj discomfort. We must be careful when constructing a mouthstick. Key Considerations for mouthstick: Should minimize occlusal trauma Should not cause tooth movement Should be inexpensive and easy to clean. Should be designed to hold a variety of implements to meet needs of client. Should be comfortable.
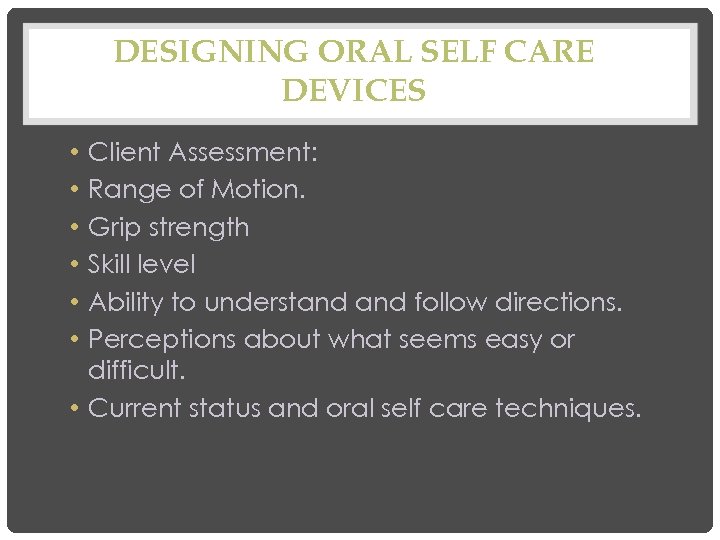 DESIGNING ORAL SELF CARE DEVICES Client Assessment: Range of Motion. Grip strength Skill level Ability to understand follow directions. Perceptions about what seems easy or difficult. • Current status and oral self care techniques. • • •
DESIGNING ORAL SELF CARE DEVICES Client Assessment: Range of Motion. Grip strength Skill level Ability to understand follow directions. Perceptions about what seems easy or difficult. • Current status and oral self care techniques. • • •


