229ed45ddefa8996494243fb8fa0c06d.ppt
- Количество слайдов: 36
Spasticity What Causes it and Can it be Inhibited? Kevin Nhan Kyleigh Short Justin De. Long Eric Atristain Paul Broyer PT 224 March 24, 2010
Learning Objectives At the completion of this presentation, the learner will be able to: n Define spasticity n Describe the neurophysiology of spasticity n An accepted and validated technique for measuring spasticity n Can spasticity be inhibited? n The effectiveness of treatments to reduce spasticity
What is Spasticity? “Spasticity is a motor disorder characterized by a velocity-dependant increase in tonic stretch reflexes with exaggerated tendon jerk, resulting from hyperexcitability of the stretch reflex” - James Lance (1980)
What is Spasticity? n Some of the difficulty for clinicians to understand the pathophysiology of spasticity is due to the definition of spasticity. n There is much criticism in definitions. n Definition offered by Lance is generally the most accepted by physiologist. [Barnes and Johnson]
Who else defined spasticity? n n n n The following individuals also contributed to the definition and research of spasticity Bobath and Bobath (1950) Levine et al (1954) Wyke (1976) Lance (1980) Lance (1990) Gottlieb and Myklebust (1993) Morris (2000) [Ibuki and Bernhardt (2007)]
Mechanism of Spasticity n So what causes a muscle to become spastic? • The absence of an upper motor neuron’s inhibitory control on the spinal reflex. Hyperactive stretch reflexes that are mediated by muscle spindle stretch receptors Decreased threshold of the alpha lower motor neurons • •
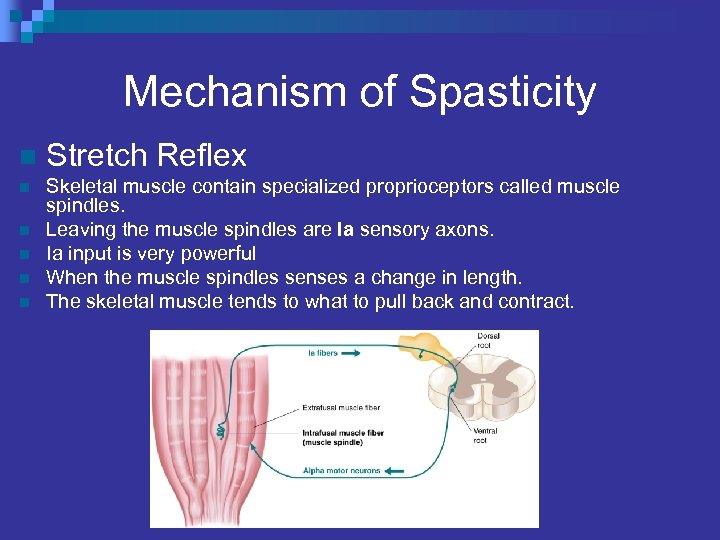
Mechanism of Spasticity n Stretch Reflex n Skeletal muscle contain specialized proprioceptors called muscle spindles. Leaving the muscle spindles are Ia sensory axons. Ia input is very powerful When the muscle spindles senses a change in length. The skeletal muscle tends to what to pull back and contract. n n
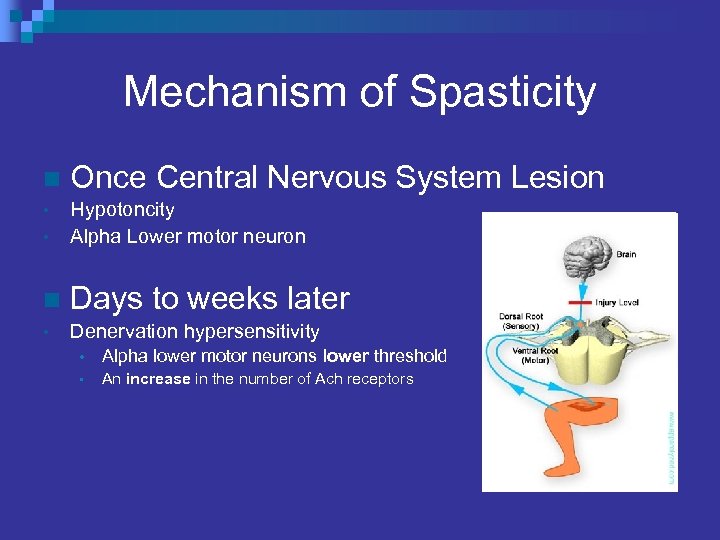
Mechanism of Spasticity n Once Central Nervous System Lesion • • Hypotoncity Alpha Lower motor neuron n Days to weeks later • Denervation hypersensitivity • Alpha lower motor neurons lower threshold • An increase in the number of Ach receptors
Characteristics of Spasticity Rather then being a specific symptom. • • Hyperactive stretch reflex Increased resistance to passive movement Posturing of extremities Stereotypical movement synergies
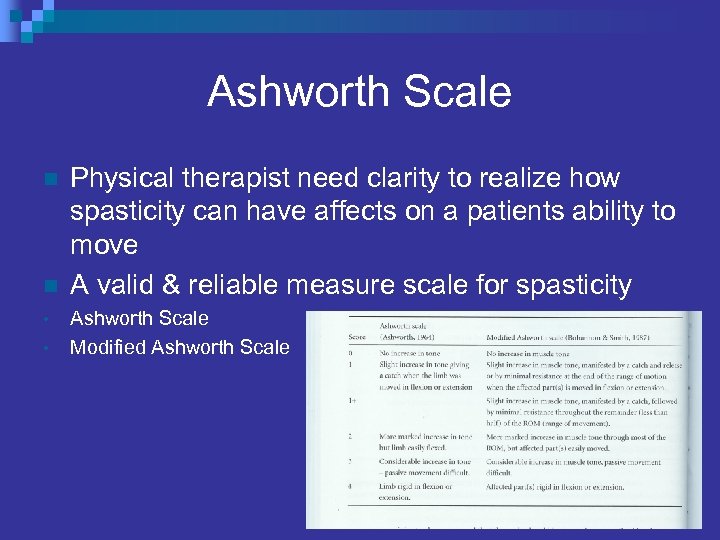
Ashworth Scale n n • • Physical therapist need clarity to realize how spasticity can have affects on a patients ability to move A valid & reliable measure scale for spasticity Ashworth Scale Modified Ashworth Scale
Mock Clinic n Manual Muscle Testing to be valid/invalid • Since we can now measure voluntary contractions “Patients with spasticity have been shown to spend 3 times longer in rehabilitation units than stroke patients without spasticity” [Gilen and Burkhardt]
Physical Therapy Intervention n Can Physical Therapy fix spasticity? • n No! But they can help with function. Disorder of upper motor neuron pathways include: • • • Stroke Traumatic brain injury Multiple sclerosis Spinal cord injury Cerebral palsy
Interventions ¨ Effective Treatments for reducing Spasticity n n n PT Intervention Electrical and Functional Electrical Stimulation Casting Mental Imagery Pharmacological Interventions Surgery
![Physiotherapy Intervention [Richardson (2002)] n Components of PT ¨ n Assess, ID goals, measuring Physiotherapy Intervention [Richardson (2002)] n Components of PT ¨ n Assess, ID goals, measuring](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-14.jpg)
Physiotherapy Intervention [Richardson (2002)] n Components of PT ¨ n Assess, ID goals, measuring problem, implementation of intervention, reassessment. 3 Broad Approaches Biomechanical - (Car & Shepherd) - improve strength, task practice ¨ Neurophysiological (Bobath) - motor hierarchy, not as good as above. ¨ Cognitive - (Fetters) - dynamic systems approach, motivation. ¨ n Modalities Electrical Stimulation & Functional ES ¨ Ice (30 minutes to reduce for 1 -1. 5 hrs), light touch/brushing. ¨
![Physiotherapy Intervention [Richardson (2002)] n Interventions Stretching (6 hr), splinting, casting. ¨ Strength training Physiotherapy Intervention [Richardson (2002)] n Interventions Stretching (6 hr), splinting, casting. ¨ Strength training](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-15.jpg)
Physiotherapy Intervention [Richardson (2002)] n Interventions Stretching (6 hr), splinting, casting. ¨ Strength training (Shean), a stronger muscle will need less force. ¨ n Motor Learning Cortex remapping. ¨ Constraint induced therapy. ¨ n Patient Educators Explanations help Pts understand, enables them to help themselves. ¨ Help with compliance with an agreed upon program. ¨
![Electrical Stimulation n [Chen et al. (2005)] ¨ Looked at treating Achilles Tendon with Electrical Stimulation n [Chen et al. (2005)] ¨ Looked at treating Achilles Tendon with](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-16.jpg)
Electrical Stimulation n [Chen et al. (2005)] ¨ Looked at treating Achilles Tendon with 20 min of E-Stim. n n ¨ Golgi Tendon Organ Ib neuron diminished after stroke. n ¨ ES applied to the muscle tendon junction. Trying to reestablish 1 B inhibitory neuron from GTO. Possible mechanism contributing to spasticity. Decreased MAS score and improved 10 m walking time, after 1 month of treatment. n How its administered important, lasting effects are unknown.
![Electrical Stimulation n [Mesci, N. et al. (2009)] q Treatment group received NMES treatment Electrical Stimulation n [Mesci, N. et al. (2009)] q Treatment group received NMES treatment](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-17.jpg)
Electrical Stimulation n [Mesci, N. et al. (2009)] q Treatment group received NMES treatment for hemiplegic foot dorsiflexor muscles for 4 weeks, 5 days a week. q Showed a significant increase in ankle dorsiflexion and a significant decrease in the level of spasticity.
![Electrical Stimulation n [Chung, B. , et al. (2009)] q Statistical differences of reduction Electrical Stimulation n [Chung, B. , et al. (2009)] q Statistical differences of reduction](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-18.jpg)
Electrical Stimulation n [Chung, B. , et al. (2009)] q Statistical differences of reduction of Composite Spasticity Score, Achilles tendon jerks, resistance to full-range passive ankle dorsiflexion and ankle clonus were calculated. q This study showed that a single session of TENS could immediately reduce spasticity. q -No long term effects
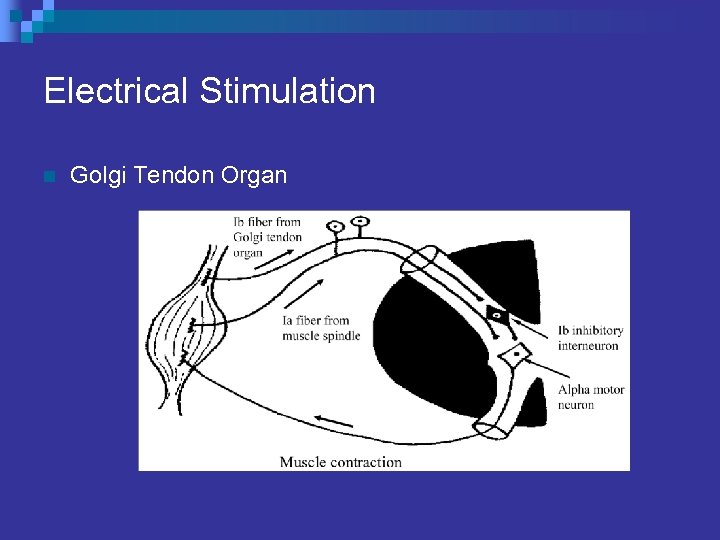
Electrical Stimulation n Golgi Tendon Organ
![Functional Electrical Stimulation n [Krause et al. (2007)] ¨ Used to facilitate movement. n Functional Electrical Stimulation n [Krause et al. (2007)] ¨ Used to facilitate movement. n](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-20.jpg)
Functional Electrical Stimulation n [Krause et al. (2007)] ¨ Used to facilitate movement. n ¨ Looked at the difference between active FES movement and passive movement Greater decrease in spasticity immediately after FES TX, lasting 30 minutes to 1 day. No change a week later. n Benefit of increasing muscle strength for possible long term effects.
![Casting n [Preissner (2001)] ¨ Serial casting is a noninvasive procedure that helps Casting n [Preissner (2001)] ¨ Serial casting is a noninvasive procedure that helps](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-21.jpg)
Casting n [Preissner (2001)] ¨ Serial casting is a noninvasive procedure that helps children and adults improve their range of motion so they can perform daily activities with less difficulty. ¨ Serial casting may be indicated when an individual presents with range of motion limitations due to contracture, or the potential of developing contracture as a result of spasticity. ¨ Serial casting has also been used in cases of heterotopic ossification, fractures, and ligament injuries, but may not be as effective for these conditions.
![Casting n [Singer et al. (2004)] ¨ Looked at serial casting in reducing spasticity Casting n [Singer et al. (2004)] ¨ Looked at serial casting in reducing spasticity](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-22.jpg)
Casting n [Singer et al. (2004)] ¨ Looked at serial casting in reducing spasticity related ankle contractures. ¨ Must be able to differentiate from dystonia. ¨ Serial casting more effective along with botulinum and physiotherapy.
![Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ The participants were asked to imagine Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ The participants were asked to imagine](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-23.jpg)
Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ The participants were asked to imagine on the visual and kinesthetic domain about the task being performed. ¨ Motor imagery appears to be a feasible technique for use during stretching exercises in individuals with spasticity.
![Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ Is therapeutic stretching with motor imagery Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ Is therapeutic stretching with motor imagery](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-24.jpg)
Mental Imagery n [Bovend’Eerdt et al. (2008)] ¨ Is therapeutic stretching with motor imagery more effective than stretch alone? ¨ Does it work? Not statistically. n The variability in the population and the small sample size could be factors affecting the results of the study.
![Pharmacological Intervention n [Ward (2002)] ¨ Generalized spasticity n ¨ Regional spasticity n ¨ Pharmacological Intervention n [Ward (2002)] ¨ Generalized spasticity n ¨ Regional spasticity n ¨](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-25.jpg)
Pharmacological Intervention n [Ward (2002)] ¨ Generalized spasticity n ¨ Regional spasticity n ¨ Oral agents Intrathecal baclofen phenol nerve block Focal Spasticity n Botulinum toxin phenol block

Pharmacological Intervention: Generalized Spasticity n Oral Agents - also administered enterally. ¨ Diazepam n ¨ Dantrolne Sodium n n ¨ Peripherally acting muscle relaxant. Shown to increase ADL, transfers, hygiene, no LT effects. Tizanide Hydrocholride n n ¨ Brainstem reticular formation and spinal polysnaptic pathways. GABA receptor inhibitor. Inhibits both pre and post synapses. Fewer side effects than diazepam. Also functional improvements, ambulation distance on flat ground. General Side Effects n Fatigue, drowsiness, alcohol-like sedation, reduced motor coordination, impaired intellect, attention, addiction, weakness.
Pharmacological Intervention: Regional Spasticity n Intrathecal Drug Therapy - administered directly into subarachnoid space of CNS with a programmable pump. ¨ Intrathecal Baclofen, Morphine Sulphate (Infumorph), Fentanyl. n n n Improvement in walking speed, functional mobility without impairing uninvolved extremity. Fewer systemic side effects because not circulating in blood stream. Infection, impaired wound healing, pump malfunction, and catheter dislocation in 20 -25% of cases.
Pharmacological Intervention: Focal Spasticity n Chemical Neurolytics - destruction of a portion of the nerve. ¨ Phenol Injections - causes chemical (Wallerian) denervation. n n n ¨ Dose dependent, hit proximal muscles first. Works at alpha motorneurons directly. Pain at administered site, causalgia w/ sensory nerve injury. Botulinum Toxin - binds to presynaptic cell and prevents NT release. n n Begins 3 -7 days and last 2 -6 months, specific muscles. May have diminishing returns (A &B), small muscles. .
![Pharmacological Intervention • [Gallichio, (2004)] Drug Site of Action Adverse Effects Oral Drugs Diazepam Pharmacological Intervention • [Gallichio, (2004)] Drug Site of Action Adverse Effects Oral Drugs Diazepam](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-29.jpg)
Pharmacological Intervention • [Gallichio, (2004)] Drug Site of Action Adverse Effects Oral Drugs Diazepam Brainstem reticular formation and spinal polysynaptic pathways Fatigue; reduced motor coordination, intellect, attention, memory Dantrolene Sodium Skeletal muscle calcium stores Hepatotoxicity, generalized muscle weakness Oral Baclofen GABA-b receptors Drowsiness, confusion, headache, lethargy Tizanidine Hydrochloride a 2 -adrenergic receptors Dizziness, sedation, dry mouth Gaba-b receptors Pump malfunction/ dislocation Phenol Injection Neuromuscular junction Causalgia with sensory nerve injury, pain at injection site, hematoma Botulinum Toxin Nerve Injection site pain, muscle weakness in injected muscle, hematoma, muscle necrosis, phlebitis Intrathecal Drugs Intrathecal Baclofen Focal Drugs
![Surgical Intervention n [Woo (2001)] ¨ Tendon Lengthening - preferred method n n ¨ Surgical Intervention n [Woo (2001)] ¨ Tendon Lengthening - preferred method n n ¨](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-30.jpg)
Surgical Intervention n [Woo (2001)] ¨ Tendon Lengthening - preferred method n n ¨ Tendon Transfer - used on children (Shriner’s) n ¨ Gait analysis with dynamic electromyographic monitory helps reduce common errors associated with this procedure. Osteotomy - for skeletal deformity n n ¨ Allow full passive range with some residual muscle tension. Muscle must be immobilized under tension. Restore boney architecture, muscle-length can be improved. Used along with tendon lengthening. Artrhodesis - joint fusion n n When the above are prohibited. Stabilize unstabel joints (subtalar, thumb, wrist).
![Surgical Intervention [Lazorthes et al. (2002)] n Neurosurgery - severe and painful spasticity, irreversible. Surgical Intervention [Lazorthes et al. (2002)] n Neurosurgery - severe and painful spasticity, irreversible.](https://present5.com/presentation/229ed45ddefa8996494243fb8fa0c06d/image-31.jpg)
Surgical Intervention [Lazorthes et al. (2002)] n Neurosurgery - severe and painful spasticity, irreversible. ¨ Dorsal rhizotomies - Regional spasticity. n Cut dorsal cords and grey mater (gelatinosa area). n Can cause decrease in voluntary mobility, sepsis, decreased lemniscal sensitivity, and death. ¨ Peripheral neurotomies - Focal spasticity. n Used if botulinum toxin failed. n Done distally only reducing the myotatic reflex. ¨ Cervical Spinal Cord Stimulation - reversible. n E Stim administered directly to spinal area. n Intrathecal Baclofen is more commonly used.
Learning Objectives n Turn to the person beside you and review these learning objectives: ¨ ¨ ¨ Define spasticity Describe the neurophysiology of spasticity An accepted and validated technique for measuring spasticity The effectiveness of treatments to reduce spasticity Can spasticity be inhibited?
The End
References n n n Barnes, M. Management of Spasticity. Age and Ageing. 1998; 27: 239 -245 Bohvend’Eerdt, T. JH. , Dawes, H. , Sackley, C. , Izadi, H. , and Wade, D. T. Mental Techniques During Manual Stretching in Spasticity - a pilot randomized controlled trial. Clinical Rehabilitation. 2006; 23: 137 -145 Chen S-C, Chen Y-L, Chen C-J, Lai C-H, Chiang W-H, and Chen W-L. Effects of surface electrical stimulation on the muscle-tendon junction of spastic gastrocnemius in stroke patients. Disability & Rehabilitation. 2005; 27(3): 105 -110. Chung, B. , & Cheng, B. (2010). Immediate effect of transcutaneous electrical nerve stimulation on spasticity in patients with spinal cord injury. Clinical Rehabilitation, 24(3), 202 -210. Gallichio, Joann E. Pharmacologic Management of Spasticity Following Stroke. Physical Therapy Journal. 2004; 84: 973 -981
References n n n Ibuki A, Bernhardt J. What is spasticity? The discussion continues. International Journal of Therapy and Rehabilitation. 2007; 14: 391 -395 Krause, P. , Szecsi, J. , and Straube, A. Changes in Spastic Muscle Tone Increase in Patients with Spinal Cord Injury Using Functional Electical Stimulation and Passive Leg Movements. Clinical Rehabilitation. 2008; 22: 627 -634 Lazorthes, Y. , Sol, J-C. , Verdie, S. , & J-C. The Surgical Management of Spasticity. European Journal of Neurology. 2002; 9(1): 35 -41 Preissner, K. (2001). The effects of serial casting on spasticity: a literature review. Occupational Therapy in Health Care, 14(2), 99 -106. Retrieved from CINAHL Plus with Full Text database. Mesci, N. , Ozdemir, F. , Demirbag Kabayel, D. , & Tokuc, B. (2009). The effects of neuromuscular electrical stimulation on clinical improvement in hemiplegic lower extremity rehabilitation in chronic stroke: A single-blind, randomised, controlled trial. Disability & Rehabilitation, 31(24), 2047 -2054.
References n n n Richardson, D. Physical Therapy in Spasticity. European Journal of Neurology. 2002; 9(1): 17 -22 Singer, B. J. , Dunne, J. W. , Singer, K. P. , Jegasothy, G. M. , and Allison, G. T. Non-surgical Management of Ankle Contracture Following Acquired Brain Injury. Disability and Rehabilitation. 2004; 26(6): 335 -345 Verplancke, D. , Snape, S. , Salisbury, C. , Jones, P. , & Ward, A. (2005). A randomized controlled trial of botulinum toxin on lower limb spasticity following acute acquired severe brain injury. Clinical Rehabilitation, 19(2), 117 -125. Retrieved from CINAHL Plus with Full Text database. Ward A. B. A Summary of Spasticity Management - a Treatment Algorithm. European Journal of Neurology. 2002; 9: 48 -52 Woo, R. Spasticity: Orthopedic Perspective. Journal of Child Neurology. 2001; 16(1): 47 -53
229ed45ddefa8996494243fb8fa0c06d.ppt