b9002e74119e08989e2b3c1d7342fb14.ppt
- Количество слайдов: 40
 Spasticity (and dystonia) from Neurology perspective Dr Ram Kumar Consultant Paediatric Neurologist Alder Hey June 2010
Spasticity (and dystonia) from Neurology perspective Dr Ram Kumar Consultant Paediatric Neurologist Alder Hey June 2010
 Summary Spasticity (and dystonia) – what is it? Overview of treatment strategy Medications Botulinum toxin
Summary Spasticity (and dystonia) – what is it? Overview of treatment strategy Medications Botulinum toxin
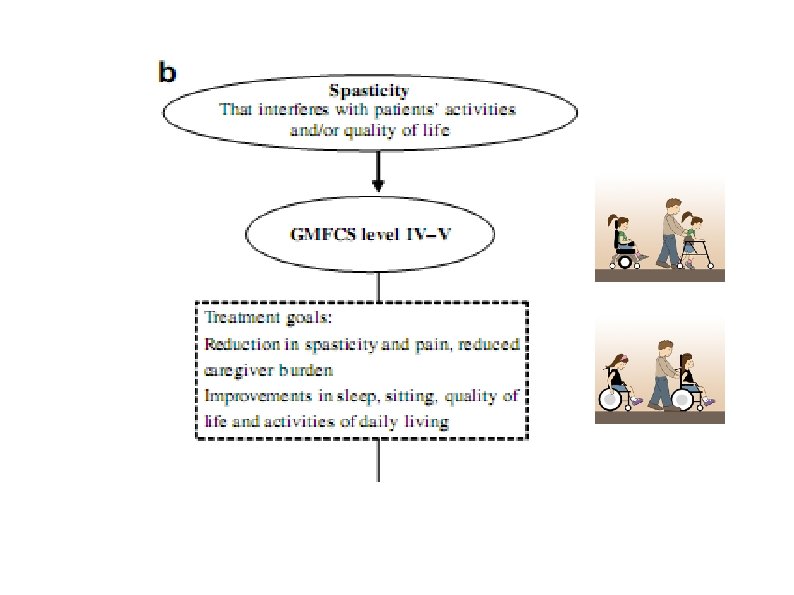
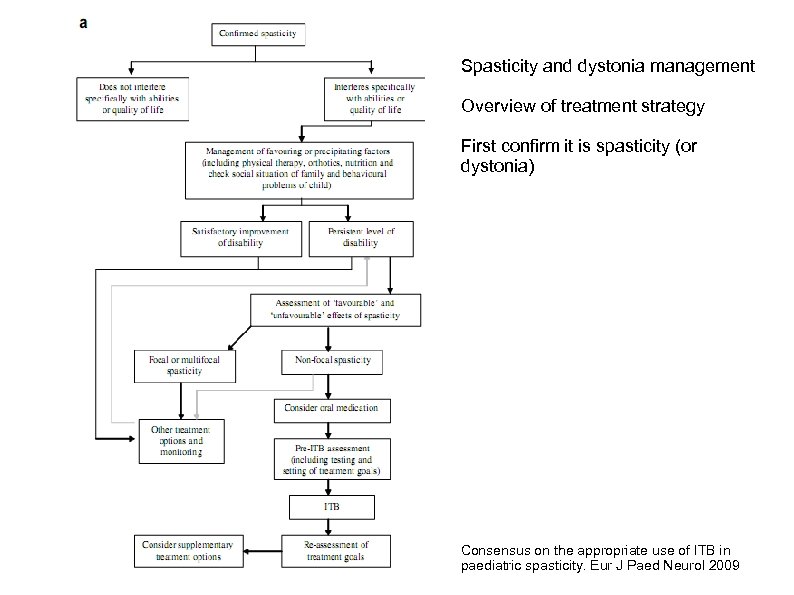 Spasticity and dystonia management Overview of treatment strategy First confirm it is spasticity (or dystonia) Consensus on the appropriate use of ITB in paediatric spasticity. Eur J Paed Neurol 2009
Spasticity and dystonia management Overview of treatment strategy First confirm it is spasticity (or dystonia) Consensus on the appropriate use of ITB in paediatric spasticity. Eur J Paed Neurol 2009
 “Legs feel stiff” - causes Is it a muscle or joint problem? Is it mainly a muscle pain/fatigue problem? Spasticity or dystonia = hypertonia aka increased muscle tone Neuromuscular conditions with increased tone e. g. myotonia Inflammatory conditions of joints + skin > muscles e. g. rheumatoid arthritis, scleroderma Joint and muscle contractures (due to any of the above, disuse)
“Legs feel stiff” - causes Is it a muscle or joint problem? Is it mainly a muscle pain/fatigue problem? Spasticity or dystonia = hypertonia aka increased muscle tone Neuromuscular conditions with increased tone e. g. myotonia Inflammatory conditions of joints + skin > muscles e. g. rheumatoid arthritis, scleroderma Joint and muscle contractures (due to any of the above, disuse)
 What is spasticity? One cause of increased muscle tone Resistance to passive muscle stretch at a joint Velocity and joint-angle dependent Has to be palpated – ie you need to lay on hands Other features: clonus, increased reflexes, upgoing plantars
What is spasticity? One cause of increased muscle tone Resistance to passive muscle stretch at a joint Velocity and joint-angle dependent Has to be palpated – ie you need to lay on hands Other features: clonus, increased reflexes, upgoing plantars
 Spasticity – classic muscles Classic lower limb muscle groups affected - the pyramidal pattern Ankle plantarflexors and invertors Knee extensors Hamstrings Hip flexors and adductors
Spasticity – classic muscles Classic lower limb muscle groups affected - the pyramidal pattern Ankle plantarflexors and invertors Knee extensors Hamstrings Hip flexors and adductors
 Spasticity – classic muscles Classic upper limb muscle groups affected: Elbow flexors – biceps, brachialis, brachioradialis Forearm pronators – pronator teres Wrist flexors – Flexor carpi radialis, ulnaris Finger flexors (long) – Flexor Digitorum Superficialis and Profundus Thumb adductors – thenar group and adductor pollicis
Spasticity – classic muscles Classic upper limb muscle groups affected: Elbow flexors – biceps, brachialis, brachioradialis Forearm pronators – pronator teres Wrist flexors – Flexor carpi radialis, ulnaris Finger flexors (long) – Flexor Digitorum Superficialis and Profundus Thumb adductors – thenar group and adductor pollicis
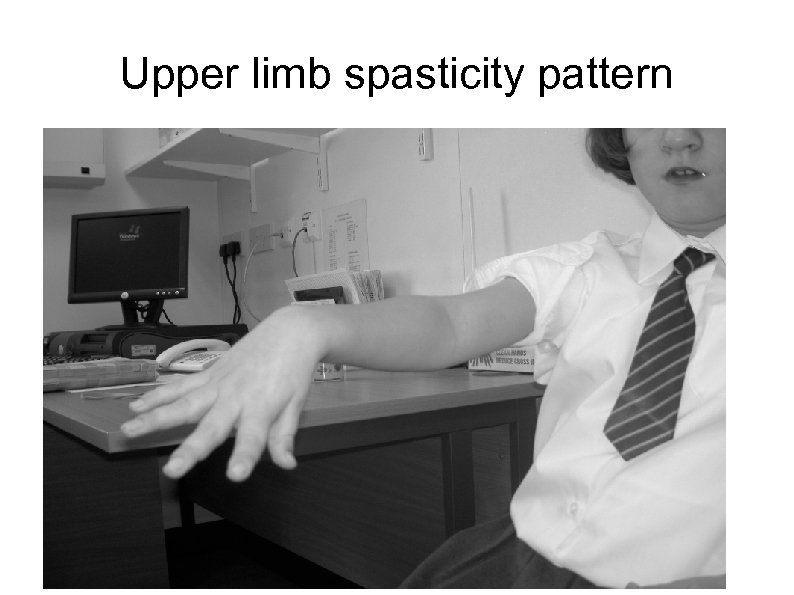 Upper limb spasticity pattern
Upper limb spasticity pattern
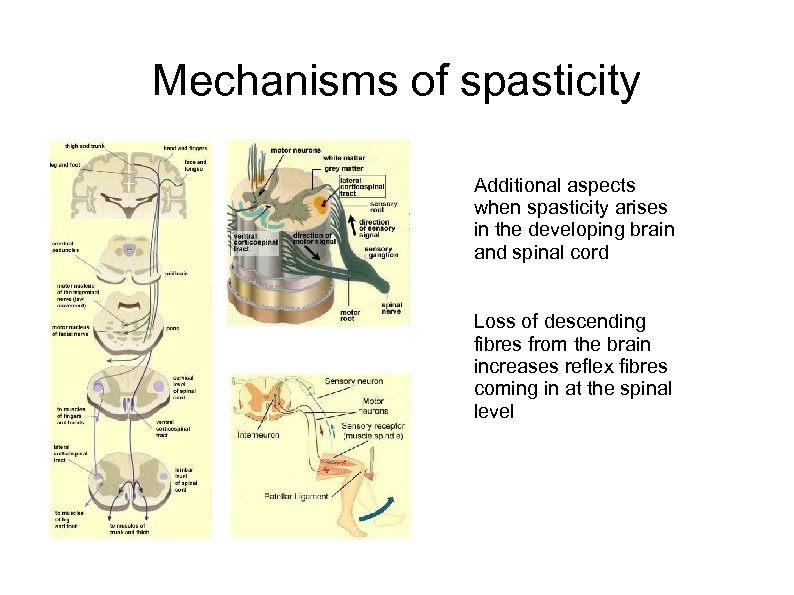 Mechanisms of spasticity Additional aspects when spasticity arises in the developing brain and spinal cord Loss of descending fibres from the brain increases reflex fibres coming in at the spinal level
Mechanisms of spasticity Additional aspects when spasticity arises in the developing brain and spinal cord Loss of descending fibres from the brain increases reflex fibres coming in at the spinal level
 Co-existent muscle, tendon, joint, skin issues Muscle weakness i. e. “-paresis” and “-plegia” Lack of selective motor control Dystonia – sustained postures, active movements Fixed contractures Bone and joint deformities Skin problems – abrasions, Raynaud's Treating spasticity can improve, worsen or not change the above. And vice versa.
Co-existent muscle, tendon, joint, skin issues Muscle weakness i. e. “-paresis” and “-plegia” Lack of selective motor control Dystonia – sustained postures, active movements Fixed contractures Bone and joint deformities Skin problems – abrasions, Raynaud's Treating spasticity can improve, worsen or not change the above. And vice versa.
 What is dystonia? Sustained postures Involuntary movements Incorrect timing of muscle activations Suggests active rather than passive movements Not usually velocity-dependent Very dependent on mental state: alertness, emotion
What is dystonia? Sustained postures Involuntary movements Incorrect timing of muscle activations Suggests active rather than passive movements Not usually velocity-dependent Very dependent on mental state: alertness, emotion
 Types of dystonia Excessive movements: chorea, athetosis, dystonic tremor, myoclonus, “spasms” Decreased movements: extrapyramidal rigidity, hypokinesia
Types of dystonia Excessive movements: chorea, athetosis, dystonic tremor, myoclonus, “spasms” Decreased movements: extrapyramidal rigidity, hypokinesia
 Muscle groups affected Oropharyngeal: mouth, tongue, pharynx, larynx Axial muscles: cervical, erector spinae (opisthotonus) Upper Limbs: Elbow extensor rigidity, fisting Lower limbs: Ankle evertors as well as invertors
Muscle groups affected Oropharyngeal: mouth, tongue, pharynx, larynx Axial muscles: cervical, erector spinae (opisthotonus) Upper Limbs: Elbow extensor rigidity, fisting Lower limbs: Ankle evertors as well as invertors
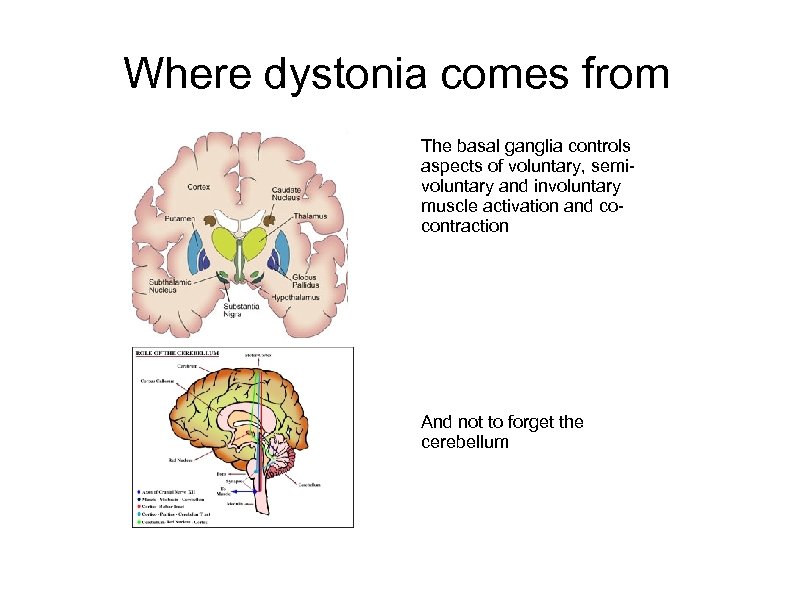 Where dystonia comes from The basal ganglia controls aspects of voluntary, semivoluntary and involuntary muscle activation and cocontraction And not to forget the cerebellum
Where dystonia comes from The basal ganglia controls aspects of voluntary, semivoluntary and involuntary muscle activation and cocontraction And not to forget the cerebellum
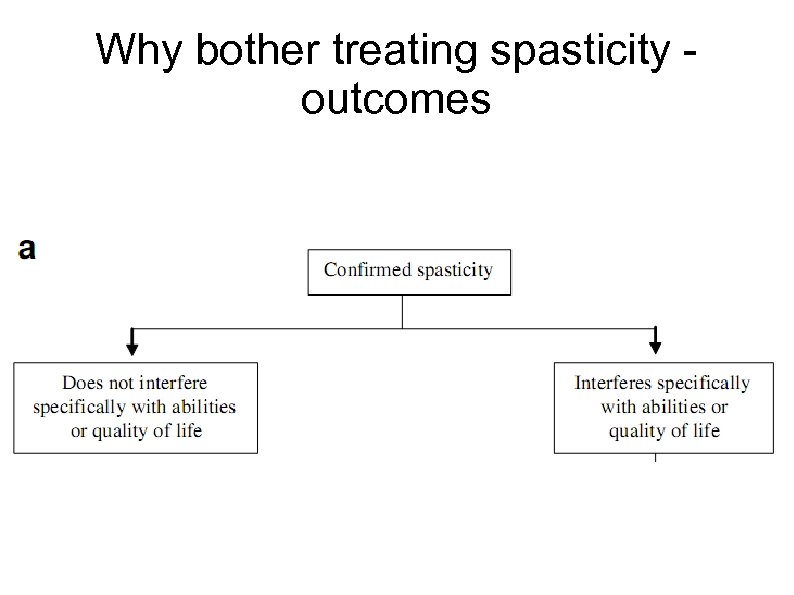 Why bother treating spasticity outcomes
Why bother treating spasticity outcomes
 Assessing impact of spasticity Sitting Walking, Splints - tolerability Posture control equipment - tolerability Other orthopaedic interventions Upper limb ADL Ease of cares Pain e. g. cramps, or agitation Sleep e. g. nocturnal cramps, need for repositioning Long term consequences - controversial
Assessing impact of spasticity Sitting Walking, Splints - tolerability Posture control equipment - tolerability Other orthopaedic interventions Upper limb ADL Ease of cares Pain e. g. cramps, or agitation Sleep e. g. nocturnal cramps, need for repositioning Long term consequences - controversial
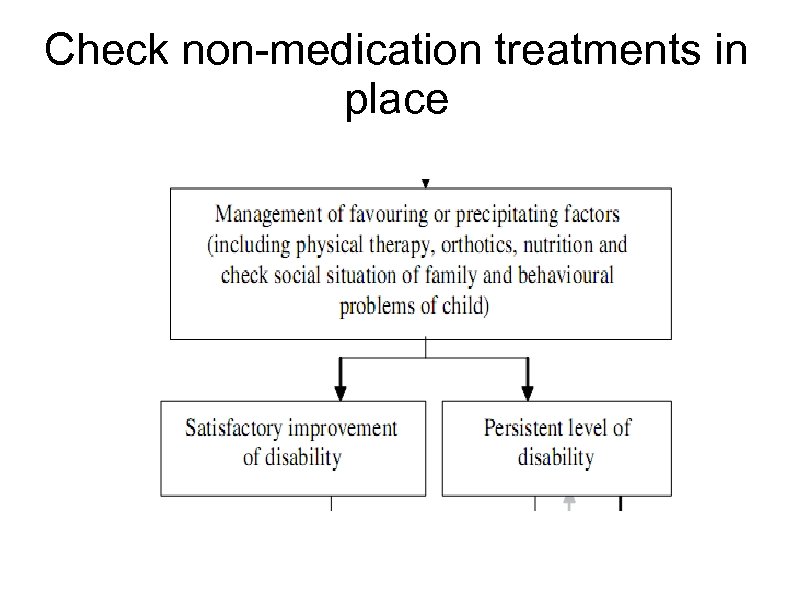 Check non-medication treatments in place
Check non-medication treatments in place
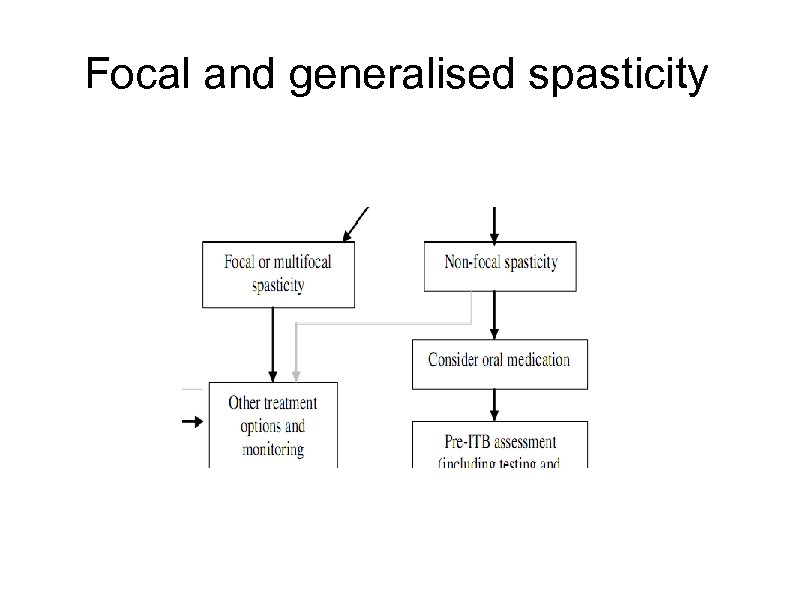 Focal and generalised spasticity
Focal and generalised spasticity
 Intramuscular Botulinum toxin injection Treatment for focal and multi-focal hypertonia Reduces neuromuscular junction transmission Need to identify which muscles to inject and why Transient effect – good and bad features Good for localised therapy Relatively safe Different formulations and doses
Intramuscular Botulinum toxin injection Treatment for focal and multi-focal hypertonia Reduces neuromuscular junction transmission Need to identify which muscles to inject and why Transient effect – good and bad features Good for localised therapy Relatively safe Different formulations and doses
 Botulinum toxin – upper limb Goals of treatment – cares, function, splint tolerance, cosmetic Adjunctive therapies – splint, casting, OT, physio Assessment tools – AHA (bimanual), Melbourne Upper limb (unilateral), COPM, VAS with patient/parent defined goals (simpler) Good evidence of benefit with repeated injections May only need to repeat at 9 months or >1 year
Botulinum toxin – upper limb Goals of treatment – cares, function, splint tolerance, cosmetic Adjunctive therapies – splint, casting, OT, physio Assessment tools – AHA (bimanual), Melbourne Upper limb (unilateral), COPM, VAS with patient/parent defined goals (simpler) Good evidence of benefit with repeated injections May only need to repeat at 9 months or >1 year
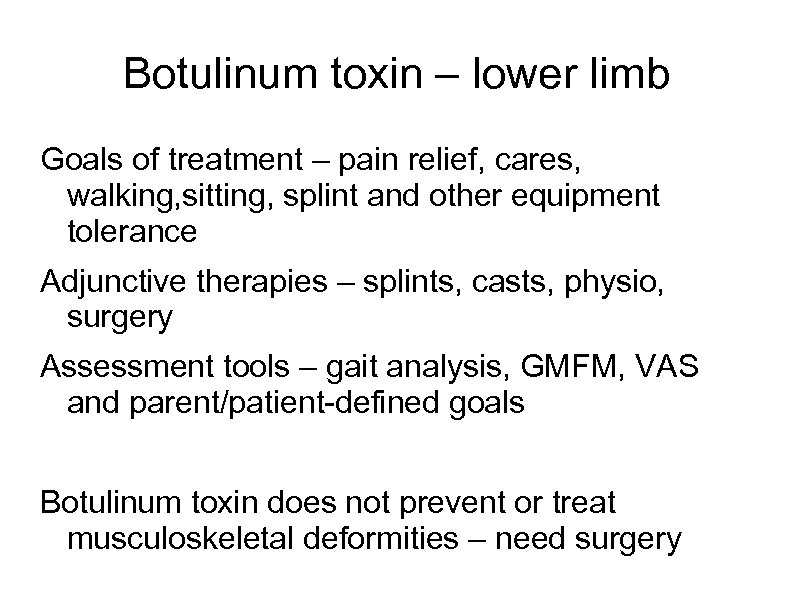 Botulinum toxin – lower limb Goals of treatment – pain relief, cares, walking, sitting, splint and other equipment tolerance Adjunctive therapies – splints, casts, physio, surgery Assessment tools – gait analysis, GMFM, VAS and parent/patient-defined goals Botulinum toxin does not prevent or treat musculoskeletal deformities – need surgery
Botulinum toxin – lower limb Goals of treatment – pain relief, cares, walking, sitting, splint and other equipment tolerance Adjunctive therapies – splints, casts, physio, surgery Assessment tools – gait analysis, GMFM, VAS and parent/patient-defined goals Botulinum toxin does not prevent or treat musculoskeletal deformities – need surgery
 Other focal and multi-focal therapy • Intramuscular phenol injections • Selective peripheral neurotomy • Selective dorsal rhizotomy (more for generalised lower limb )
Other focal and multi-focal therapy • Intramuscular phenol injections • Selective peripheral neurotomy • Selective dorsal rhizotomy (more for generalised lower limb )
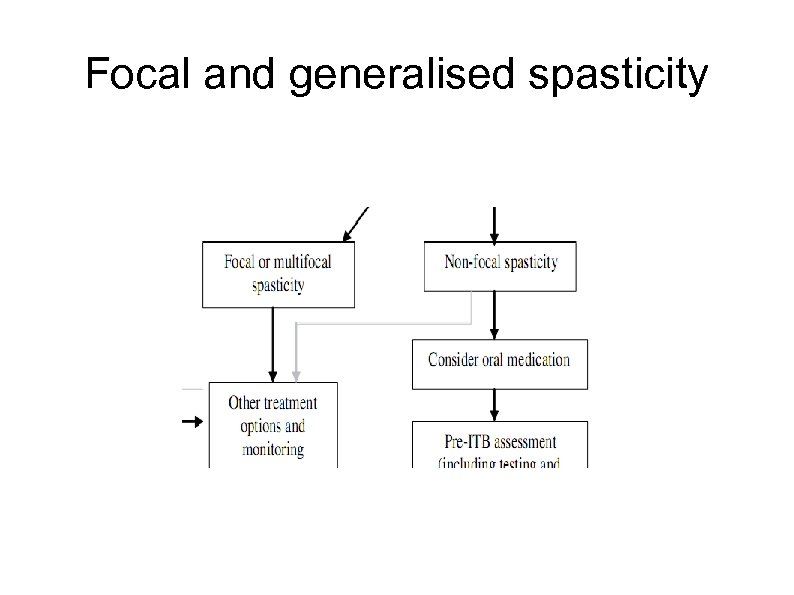 Focal and generalised spasticity
Focal and generalised spasticity
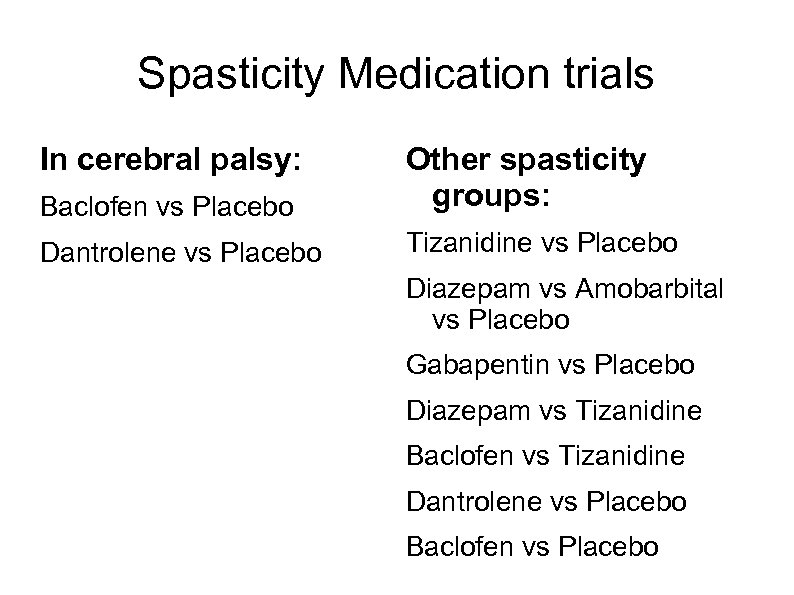 Spasticity Medication trials In cerebral palsy: Baclofen vs Placebo Other spasticity groups: Dantrolene vs Placebo Tizanidine vs Placebo Diazepam vs Amobarbital vs Placebo Gabapentin vs Placebo Diazepam vs Tizanidine Baclofen vs Tizanidine Dantrolene vs Placebo Baclofen vs Placebo
Spasticity Medication trials In cerebral palsy: Baclofen vs Placebo Other spasticity groups: Dantrolene vs Placebo Tizanidine vs Placebo Diazepam vs Amobarbital vs Placebo Gabapentin vs Placebo Diazepam vs Tizanidine Baclofen vs Tizanidine Dantrolene vs Placebo Baclofen vs Placebo
 Baclofen Typical first-line medication GABA-B agonist Needs at lleast three times a day dose Use up to 2. 5 mg/kg/day Additional sleep inducing effects Main adverse effects: sleepiness, decreased trunk tone, ? seizures increased
Baclofen Typical first-line medication GABA-B agonist Needs at lleast three times a day dose Use up to 2. 5 mg/kg/day Additional sleep inducing effects Main adverse effects: sleepiness, decreased trunk tone, ? seizures increased
 Diazepam and similar Used to be first-line before baclofen GABA-A agonist Multiple effects e. g. anxiolytic, anticonvulsant Significant adverse effects e. g. respiratory depression Tolerance Start at low doses e. g. 0. 1 mg/kg/day
Diazepam and similar Used to be first-line before baclofen GABA-A agonist Multiple effects e. g. anxiolytic, anticonvulsant Significant adverse effects e. g. respiratory depression Tolerance Start at low doses e. g. 0. 1 mg/kg/day
 Dantrolene Works on muscle calcium-contraction coupling Not sedative effect of baclofen and diazepam Main adverse effect: liver failure or asymptomatic hepatic enzyme rises Problems not reported at 12 mg/kg/day
Dantrolene Works on muscle calcium-contraction coupling Not sedative effect of baclofen and diazepam Main adverse effect: liver failure or asymptomatic hepatic enzyme rises Problems not reported at 12 mg/kg/day
 Trihexyphenidyl • Treatment for dystonic posturing (hypokinetic) • Possibly for excessive movements as well • Anticholinergic (muscarinic) • Side effects of most anticholinergics: dry mouth (can be useful); behaviour change • Start at 1 mg bd; increase weekly by 0. 1 mg/kg/day to 1 mg/kg/day as tds
Trihexyphenidyl • Treatment for dystonic posturing (hypokinetic) • Possibly for excessive movements as well • Anticholinergic (muscarinic) • Side effects of most anticholinergics: dry mouth (can be useful); behaviour change • Start at 1 mg bd; increase weekly by 0. 1 mg/kg/day to 1 mg/kg/day as tds
 Others L-DOPA preparations e. g. Sinemet Tetrabenazine Tizanidine Gabapentin Pregabalin Azumolene Clonidine Fampridine-SR
Others L-DOPA preparations e. g. Sinemet Tetrabenazine Tizanidine Gabapentin Pregabalin Azumolene Clonidine Fampridine-SR
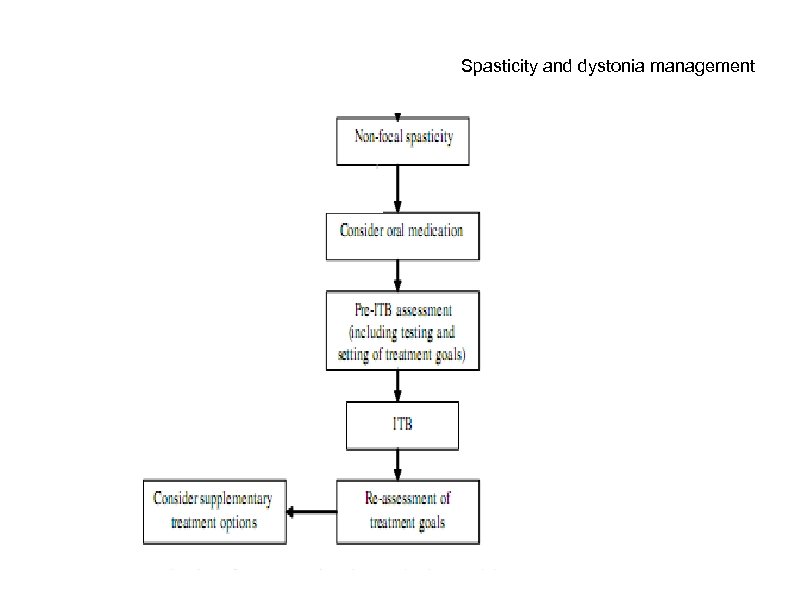 Spasticity and dystonia management
Spasticity and dystonia management
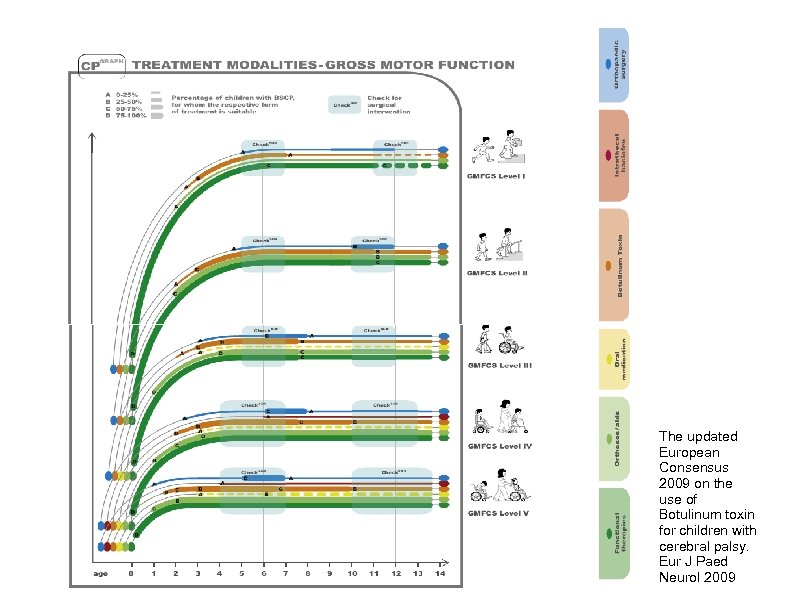 The updated European Consensus 2009 on the use of Botulinum toxin for children with cerebral palsy. Eur J Paed Neurol 2009
The updated European Consensus 2009 on the use of Botulinum toxin for children with cerebral palsy. Eur J Paed Neurol 2009
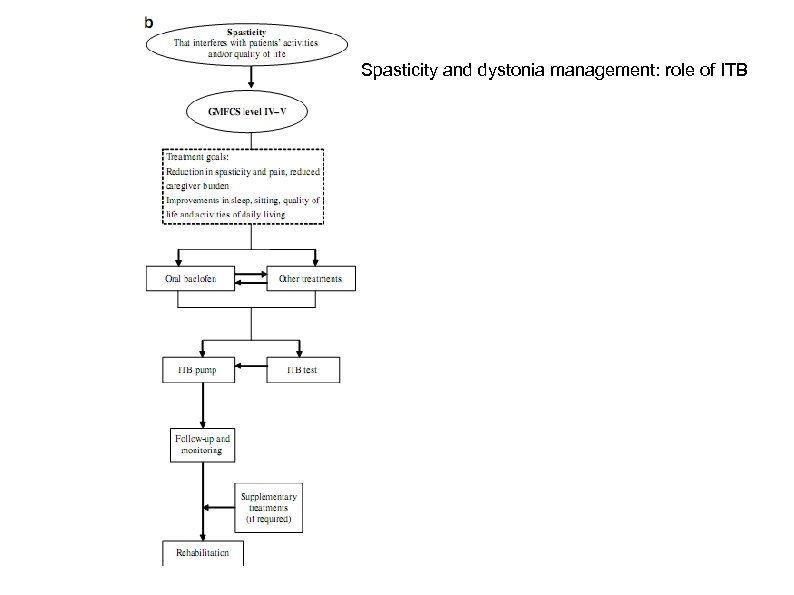 Spasticity and dystonia management: role of ITB
Spasticity and dystonia management: role of ITB

 Goals of treatment • • Reduce spasticity-related pain Improve sleep Aid posture management Reduce carer requirements Improve function eg upper limb Relief from adverse effects of oral medication Possibly improve age-dependent changes : contractures, joint deformities, respiratory problems
Goals of treatment • • Reduce spasticity-related pain Improve sleep Aid posture management Reduce carer requirements Improve function eg upper limb Relief from adverse effects of oral medication Possibly improve age-dependent changes : contractures, joint deformities, respiratory problems
 Evaluation • Multidisciplinary including orthopaedic, physio, neurology, neurosurgery • Co-morbidities • Social factors • Local factors (geography, adaptations) • Physical impairment measures • Care and comfort hypertonicity questionnaire (CCHQ) • Paediatric Pain Profile (PPP)
Evaluation • Multidisciplinary including orthopaedic, physio, neurology, neurosurgery • Co-morbidities • Social factors • Local factors (geography, adaptations) • Physical impairment measures • Care and comfort hypertonicity questionnaire (CCHQ) • Paediatric Pain Profile (PPP)
 Case Study: SK 14 year old boy CP due to neonatal meningitis Asymmetric 4 limb spasticity, left worse Severe intellectual disability, blind Previous bilateral hip surgery ’ 03 Increasing pain 2 years – focal and general
Case Study: SK 14 year old boy CP due to neonatal meningitis Asymmetric 4 limb spasticity, left worse Severe intellectual disability, blind Previous bilateral hip surgery ’ 03 Increasing pain 2 years – focal and general
 Case Study: SK Baseline Paediatric Pain Profile scores (pre-ITB): Good day = 14 Hip pain = 50 Back pain = 26
Case Study: SK Baseline Paediatric Pain Profile scores (pre-ITB): Good day = 14 Hip pain = 50 Back pain = 26
 Care and comfort questions
Care and comfort questions
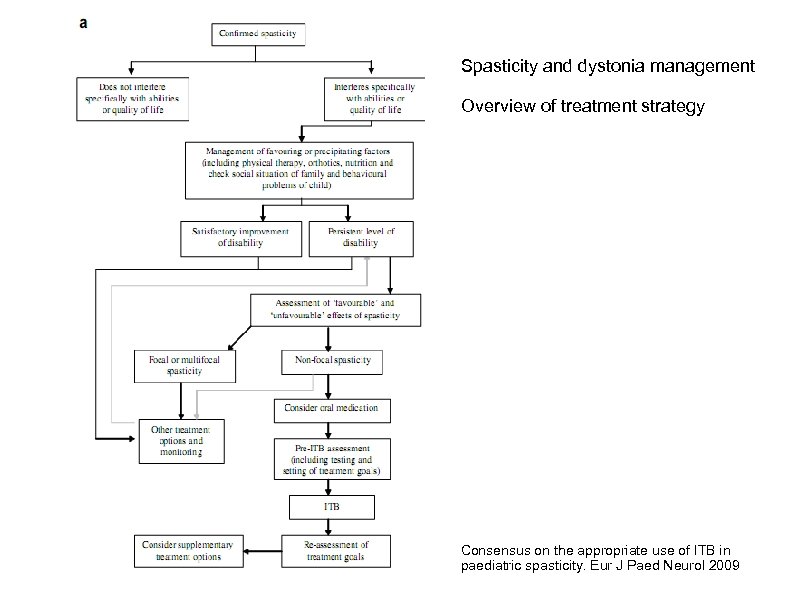 Spasticity and dystonia management Overview of treatment strategy Consensus on the appropriate use of ITB in paediatric spasticity. Eur J Paed Neurol 2009
Spasticity and dystonia management Overview of treatment strategy Consensus on the appropriate use of ITB in paediatric spasticity. Eur J Paed Neurol 2009


