2ef2b02260ccd8ec8e65f2589d2127b7.ppt
- Количество слайдов: 63
Sound Test Audio for this webinar will be broadcast through your computer’s speakers or headphones. We are currently testing microphones. If you do not hear anything, check your audio connections and volume levels on your computer. If problems continue, technical support is available by clicking the “Help” button in the upper-left corner of the screen or by visiting http: //www. cilt. und. edu/tech_support. html

Welcome Patricia Moulton, Ph. D. Principal Investigator, Rural Health Research Gateway www. ruralhealthresearch. org
Feature Presentation Mark Doescher, MD, MSPH Director, WWAMI Rural Health Research and UW Center for Health Workforce Studies University of Washington School of Medicine
Informing Rural Primary Care Workforce Policy: What Does the Evidence Tell Us? Mark Doescher, MD, MSPH Director, WWAMI Rural Health Research and UW Center for Health Workforce Studies University of Washington School of Medicine Rural Health Research Gateway Webinar September 23, 2010 6
Goals and Objectives 1. 2. Review the rural primary care supply literature Discuss policies aimed at improving rural primary care supply 7
Primary Care is Beneficial GAO report Feb 2008: “Ample research concludes that the nation’s over reliance on specialty care services at the expense of primary care leads to a health system that is less efficient. ” “Research shows that preventive care, care coordination for the chronically ill, and continuity of care—all hallmarks of primary care medicine— can achieve better health outcomes and cost savings. ” 8
The Crumbling Primary Care Infrastructure 9
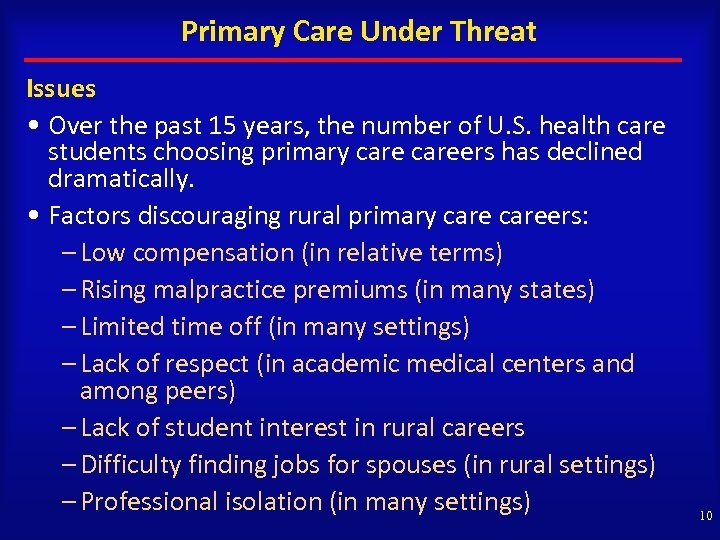
Primary Care Under Threat Issues • Over the past 15 years, the number of U. S. health care students choosing primary careers has declined dramatically. • Factors discouraging rural primary careers: – Low compensation (in relative terms) – Rising malpractice premiums (in many states) – Limited time off (in many settings) – Lack of respect (in academic medical centers and among peers) – Lack of student interest in rural careers – Difficulty finding jobs for spouses (in rural settings) – Professional isolation (in many settings) 10
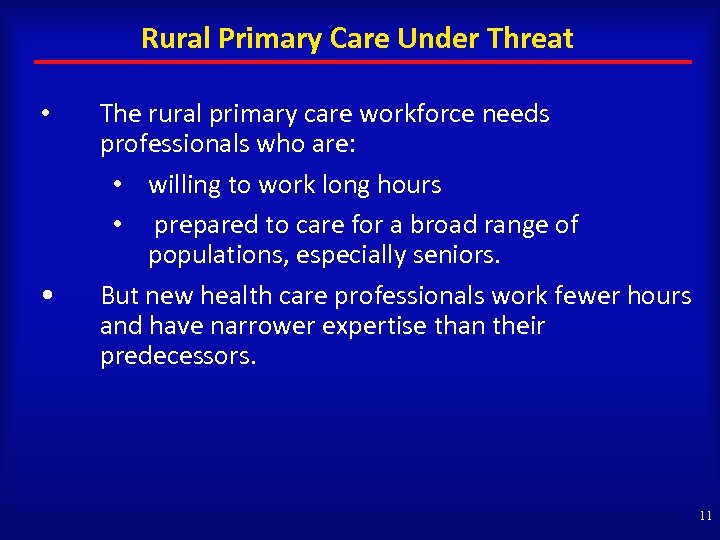
Rural Primary Care Under Threat • • The rural primary care workforce needs professionals who are: • willing to work long hours • prepared to care for a broad range of populations, especially seniors. But new health care professionals work fewer hours and have narrower expertise than their predecessors. 11
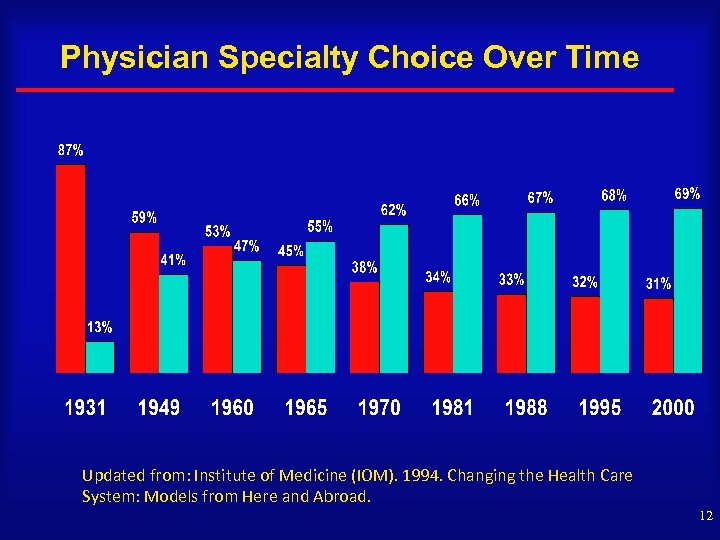
Physician Specialty Choice Over Time Updated from: Institute of Medicine (IOM). 1994. Changing the Health Care System: Models from Here and Abroad. 12
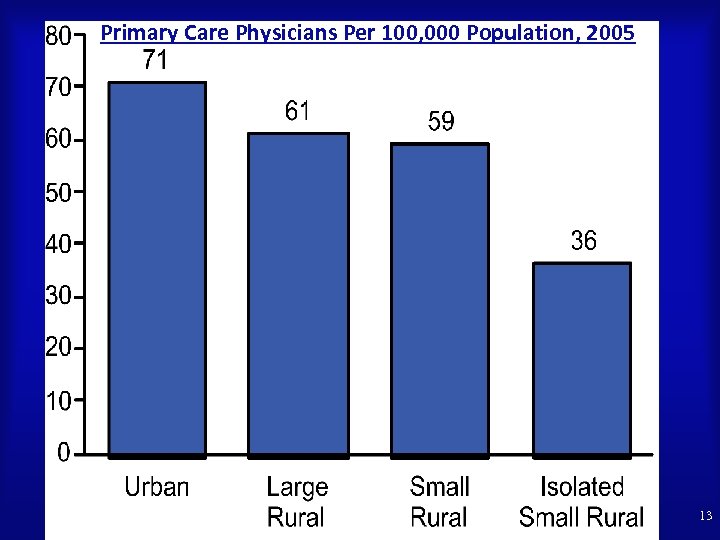
Primary Care Physicians Per 100, 000 Population, 2005 13
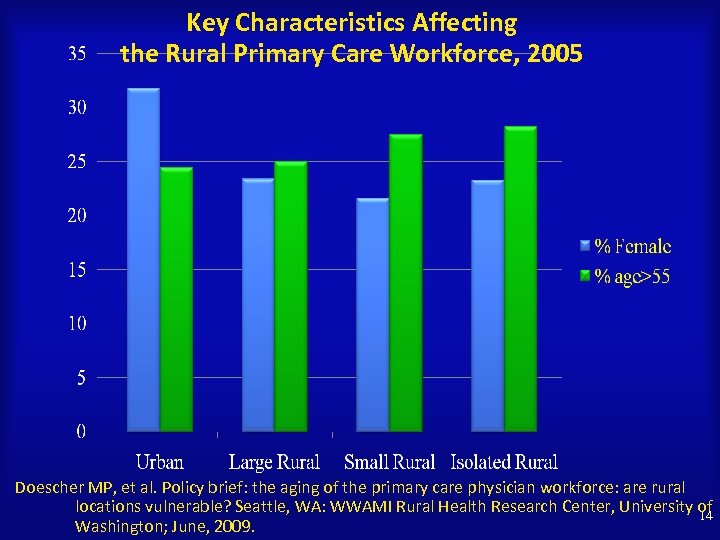
Key Characteristics Affecting the Rural Primary Care Workforce, 2005 Doescher MP, et al. Policy brief: the aging of the primary care physician workforce: are rural locations vulnerable? Seattle, WA: WWAMI Rural Health Research Center, University of 14 Washington; June, 2009.
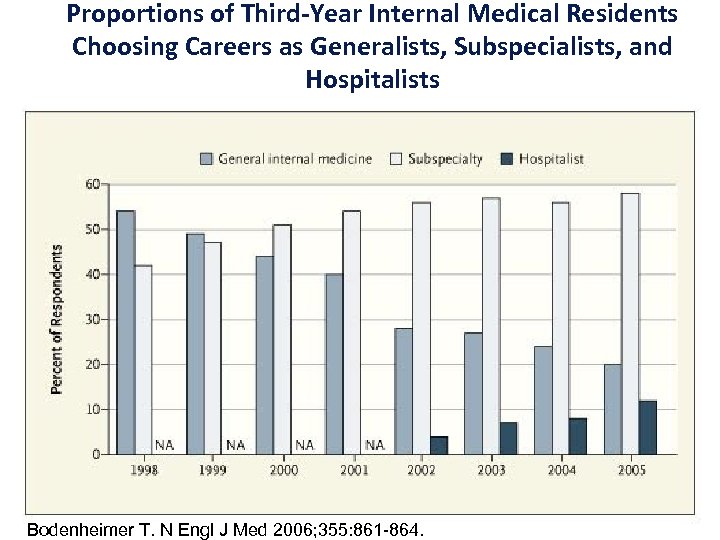
Proportions of Third-Year Internal Medical Residents Choosing Careers as Generalists, Subspecialists, and Hospitalists Bodenheimer T. N Engl J Med 2006; 355: 861 -864. 15
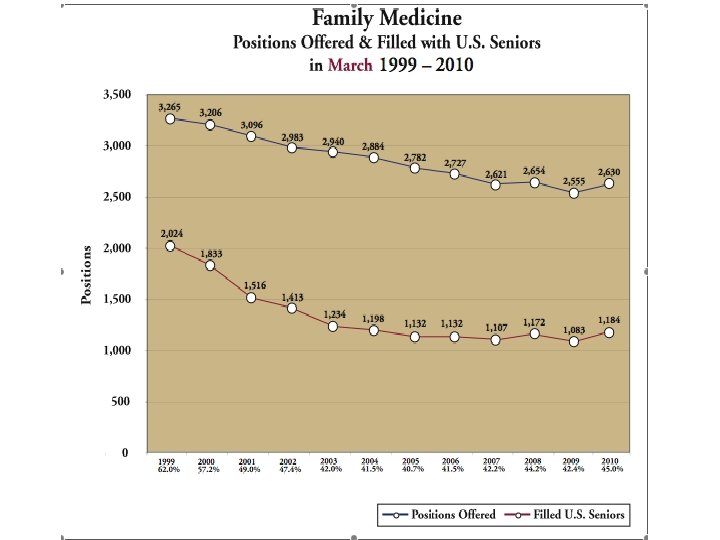
16
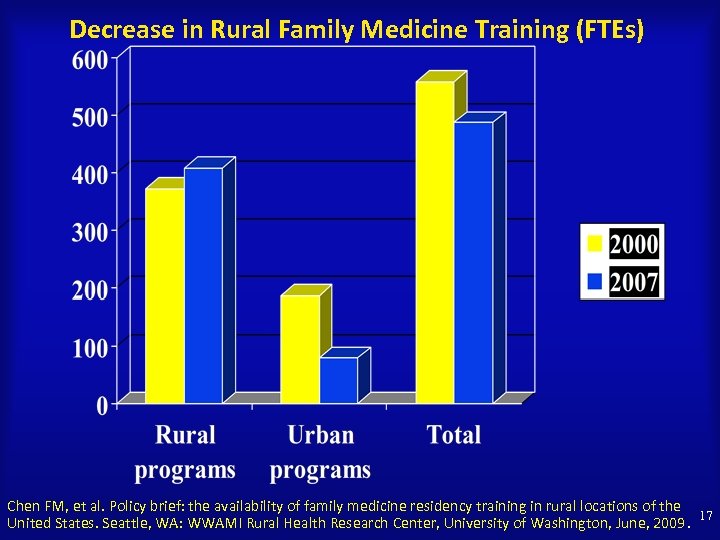
Decrease in Rural Family Medicine Training (FTEs) Chen FM, et al. Policy brief: the availability of family medicine residency training in rural locations of the 17 United States. Seattle, WA: WWAMI Rural Health Research Center, University of Washington, June, 2009.
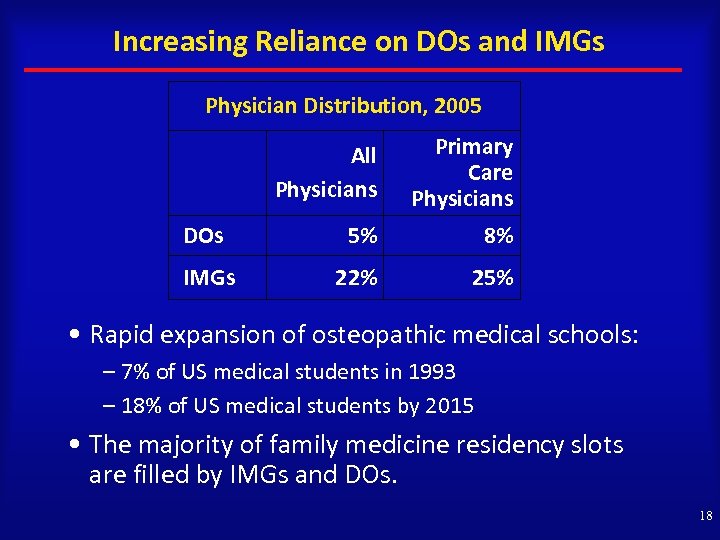
Increasing Reliance on DOs and IMGs Physician Distribution, 2005 All Physicians Primary Care Physicians DOs 5% 8% IMGs 22% 25% • Rapid expansion of osteopathic medical schools: – 7% of US medical students in 1993 – 18% of US medical students by 2015 • The majority of family medicine residency slots are filled by IMGs and DOs. 18
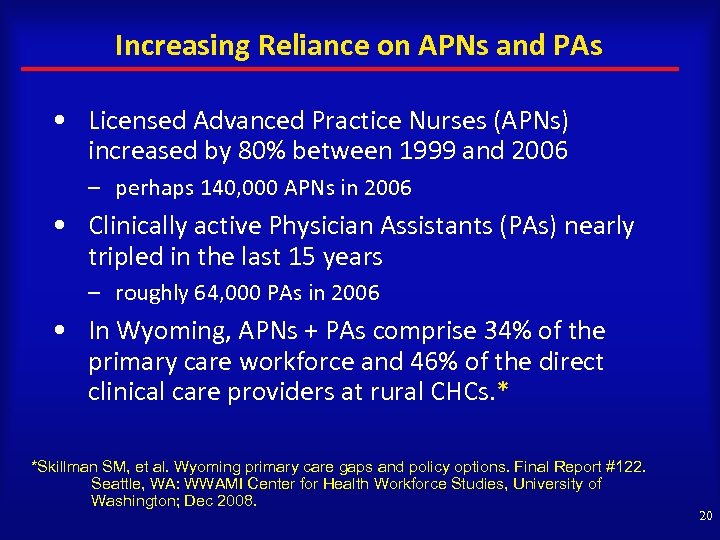
Increasing Reliance on APNs and PAs • Licensed Advanced Practice Nurses (APNs) increased by 80% between 1999 and 2006 – perhaps 140, 000 APNs in 2006 • Clinically active Physician Assistants (PAs) nearly tripled in the last 15 years – roughly 64, 000 PAs in 2006 • In Wyoming, APNs + PAs comprise 34% of the primary care workforce and 46% of the direct clinical care providers at rural CHCs. * *Skillman SM, et al. Wyoming primary care gaps and policy options. Final Report #122. Seattle, WA: WWAMI Center for Health Workforce Studies, University of Washington; Dec 2008. 20
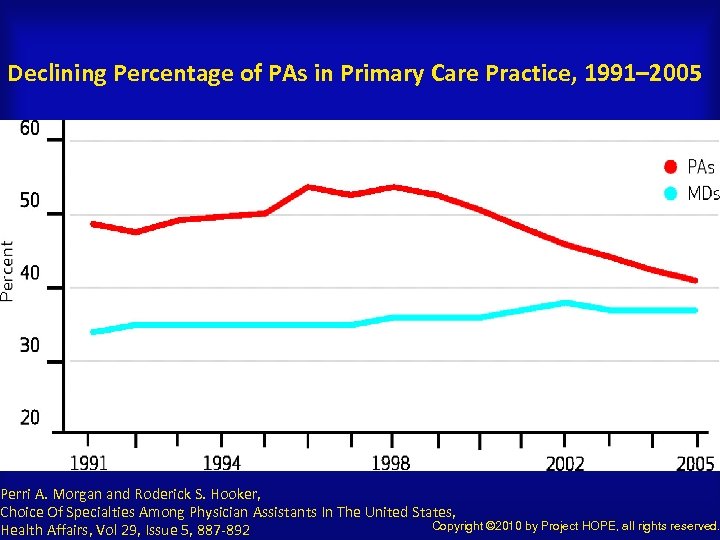
Declining Percentage of PAs in Primary Care Practice, 1991– 2005 Perri A. Morgan and Roderick S. Hooker, Choice Of Specialties Among Physician Assistants In The United States, Copyright © 2010 by Project HOPE, all rights reserved. Health Affairs, Vol 29, Issue 5, 887 -892
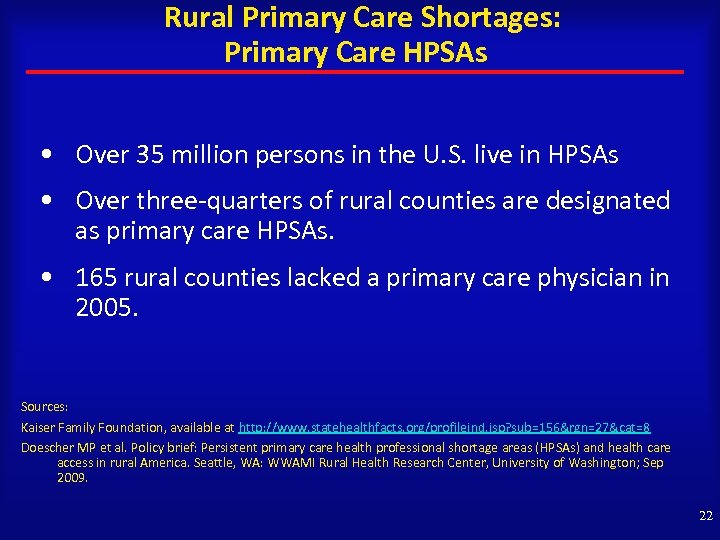
Rural Primary Care Shortages: Primary Care HPSAs • Over 35 million persons in the U. S. live in HPSAs • Over three-quarters of rural counties are designated as primary care HPSAs. • 165 rural counties lacked a primary care physician in 2005. Sources: Kaiser Family Foundation, available at http: //www. statehealthfacts. org/profileind. jsp? sub=156&rgn=27&cat=8 Doescher MP et al. Policy brief: Persistent primary care health professional shortage areas (HPSAs) and health care access in rural America. Seattle, WA: WWAMI Rural Health Research Center, University of Washington; Sep 2009. 22
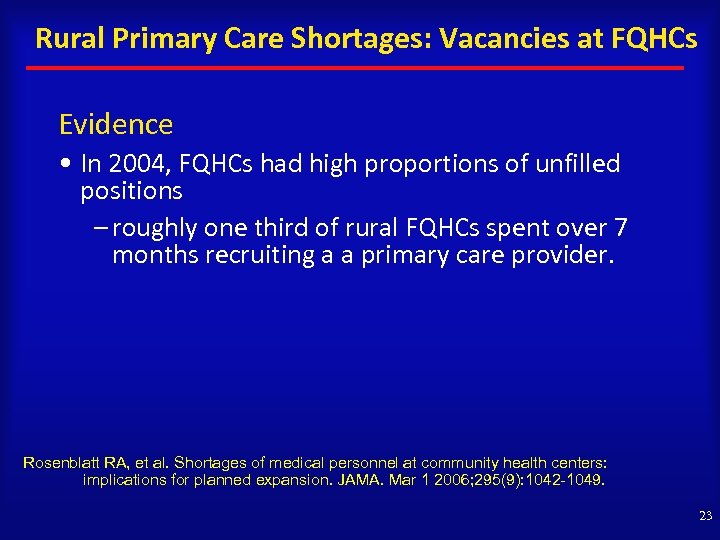
Rural Primary Care Shortages: Vacancies at FQHCs Evidence • In 2004, FQHCs had high proportions of unfilled positions – roughly one third of rural FQHCs spent over 7 months recruiting a a primary care provider. Rosenblatt RA, et al. Shortages of medical personnel at community health centers: implications for planned expansion. JAMA. Mar 1 2006; 295(9): 1042 -1049. 23
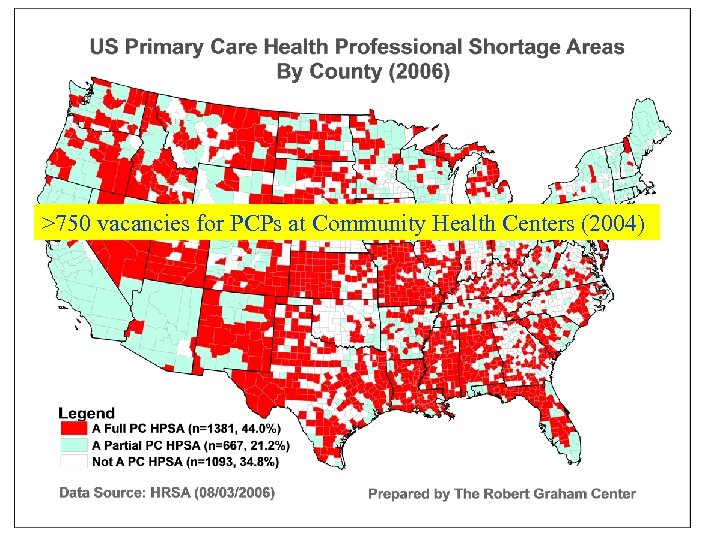
>750 vacancies for PCPs at Community Health Centers (2004) 24
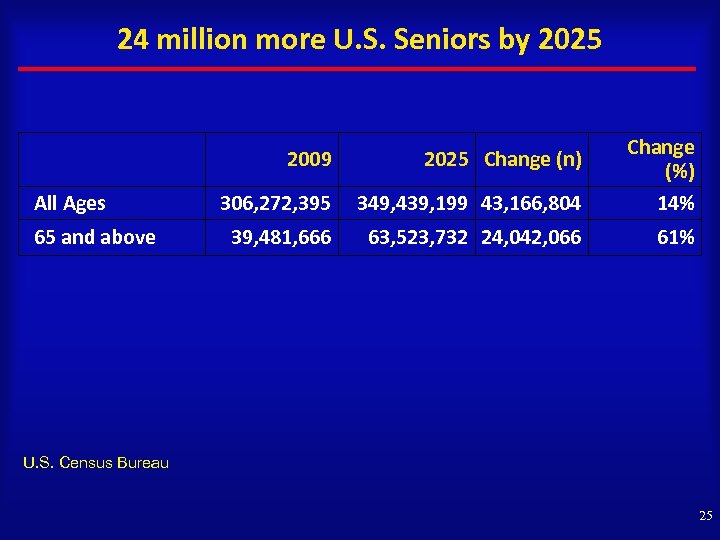
24 million more U. S. Seniors by 2025 2009 All Ages 65 and above 2025 Change (n) 306, 272, 395 349, 439, 199 43, 166, 804 Change (%) 14% 39, 481, 666 63, 523, 732 24, 042, 066 61% U. S. Census Bureau 25
Population Trends + Health Care Reform = Worsening Rural Shortages • 30% or greater increase in primary care workload by 2025. • 7% increase in primary care supply, at best. • Translates to a shortfall of 35, 000 to 44, 000 primary care providers nationally who treat adults (if the “business as usual” approach to primary care continues). Based on: Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Health Aff (Millwood). 2008 May-Jun; 27(3): w 232 -41. 26
Policies Needed to Reinvigorate Primary Care To be effective, policies must address: – Training pipeline – Lifestyle – Compensation 27
Policies Needed to Reinvigorate Rural Primary Care Training pipeline 28
The Rural Primary Care Challenge: Most training is in the city… 29

…but we need folks who choose to work here. 30
The Applicant Pool Need to increase the number of rural students who apply to health professions schools. Need to improve K-12 education, especially in science and math. Need to support post-baccalaureate programs to help disadvantaged students succeed in health professions schools. 31
The Admissions Process States have an obligation to meet the health care needs of their populations. Selective admissions processes can be used to meet those needs: Location of upbringing Plan to become primary care provider (earlier the better) Size and type of undergraduate college Objective, unbiased admissions process, including unbiased interviews 32
The Educational Experience Curricula • Intensive long-term relevant integrated clinical curriculum • Multiple primary care courses and rotations • For physicians, residency programs that reinforce primary care values and teach relevant skills for rural settings • Other Factors • Manageable student debt (<$150, 000 for physicians) • Strong psychosocial support for students • Institutional values and commitment 33
Policies to Expand Rural Medical Education • The “Affordable Care Act” (ACA) creates a special grant program for medical schools to “establish, improve, or expand rural focused education and training”, including: – helping recruit students most likely to practice in underserved rural communities – providing rural training experiences – increasing the number of graduates who ultimately practice in rural communities 34
Policy to Expand Rural Residency Training • The ACA redistributes unused physician residency training slots to other institutions; priority given to primary care and general surgery, states with the lowest resident-to-population ratios, and rural areas (effective 2011). • The ACA counts resident training time in all training sites as long as the hospital pays the resident stipends and benefits (effective 2010). • Bottom line: helps ensure availability of residency programs in rural and underserved areas. 35
Creation of an Advanced Practice Nurse Training Program • A Medicare demonstration project will pay hospitals to cover costs of training APNs – an approach that builds on Medicare GME for physicians. • However, it is limited to five hospitals across the nation. • Half of the training must occur in community-based settings. 36
The Advent of Teaching Health Centers • The ACA creates “Teaching Health Centers” under Title VII to train primary care medical and dental residents in FQHCs and a few other settings. 37
Policies Needed to Reinvigorate Rural Primary Care Lifestyle 38
Lifestyle A primary care physician with a panel of 2500 average patients would spend: 7. 4 hours per day to deliver all recommended preventive care. 10. 6 hours per day to deliver all recommended chronic care services. Yarnall et al. Am J Public Health 2003; 93: 635. Ostbye et al. Annals of Fam Med 2005; 3: 209. 39
Practice Support Needed Networks/Care Coordination • Clinic support: e. g. , team care to deal with preventive care, chronic illness care, etc. • After hours support: e. g. , after hours call coverage, shared practice arrangements, etc. • Adequate urgent care/emergency care support • Adequate specialist support 40
Expansion in Title VII Funding Aimed at Improving Practice Support • ACA expands Title VII to include demonstration projects providing training to physicians and PAs focusing on new models of care, such as – medical homes – team management of chronic disease – integration of physical and mental health services (effective 2010 -2014). 41
Major Health Center Investment May Increase Practice Support • Opportunities for community-based, team-oriented primary care practice in more than 8, 000 sites across the nation will be created. – The ACA increases funding for federally-qualified health centers (FQHCs) by $11 billion over 5 years with a goal of serving 20 million more patients – Establishes new programs to support school-based health centers (effective fiscal year 2010) – Establishes new nurse-managed health clinics (effective fiscal year 2010) 42

Policies Needed to Reinvigorate Rural Primary Care $ $ Compensation $ $ $ $ $ 43
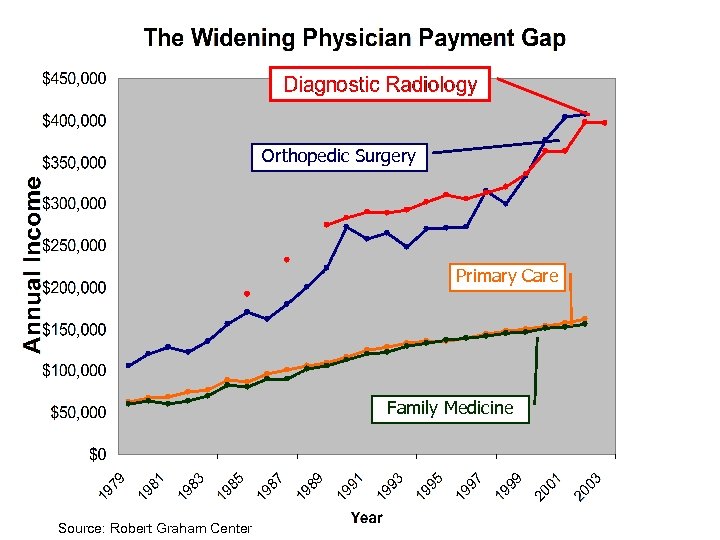
Orthopedic Surgery Primary Care Family Medicine Source: Robert Graham Center 44
Major Boost in Loan Repayment • ACA provides for a doubling of the National Health Service Corps field strength – $1. 5 billion over five years, which will place an estimated 15, 000 primary care providers in provider shortage communities. – Allow for part-time service and teaching to count for obligated clinical service. • Bottom Line: This expansion will benefit state recruitment programs that seek to bring primary care providers into rural communities. 45
Modest Increase in Fee for Service Payment for Primary Care Services – The ACA provides for a 10% Medicare bonus payment to primary care physicians practicing in HPSAs. (Effective for five years beginning January 1, 2011). – Increases Medicaid payments to 100% of the Medicare rates for primary care services provided by primary care doctors. (Effective 2013 and 2014. ) 46
Pilots of Prospective Payment for Primary Care Services • The ACA establishes the Community-based Collaborative Care Network Program to support consortiums to coordinate and integrate health care services, for low-income uninsured and underinsured populations. • Allows insurance exchanges to include qualified primary care medical homes. • Pilots: bundled payments and Accountable Care Organizations. 47
Questions? Mark Doescher mdoesche@u. washington. edu 206 -616 -9207 University of Washington WWAMI Rural Health Research Center http: //depts. washington. edu/uwrhrc/index. php Center for Health Workforce Studies http: //depts. washington. edu/uwchws/ 48
Respondent Laura Tobler Health Program National Conference of State Legislatures
State Fiscal Situation Laura Tobler Health Program NCSL Laura. tobler@ncsl. org
Overview § Although state revenue challenges continue, the steep drop appears to be subsiding. § Many states continue to face sizeable budget gaps. § To date, states have reported a total estimated budget gap of US$537. 2 billion (FY 2008 through FY 2013).
It's not over … Mike Keefe, The Denver Post, August 20, 2009 52
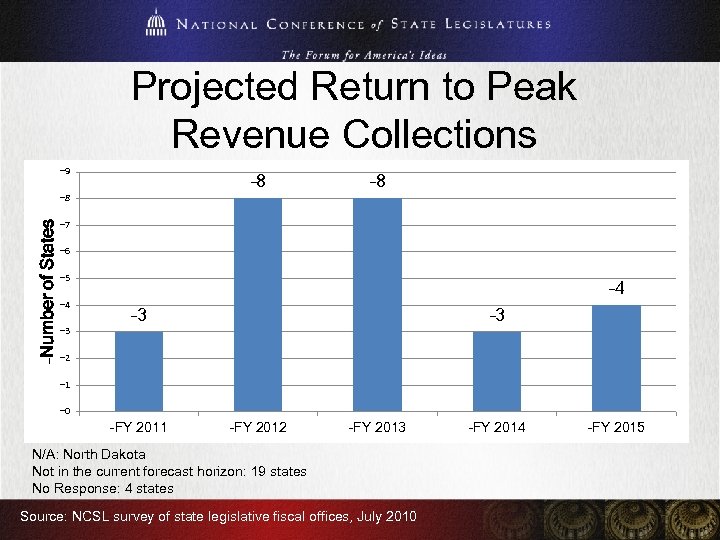
Projected Return to Peak Revenue Collections – 9 – 8 –Number of States – 8 – 7 – 6 – 5 – 4 – 3 – 3 – 2 – 1 – 0 –FY 2011 –FY 2012 –FY 2013 N/A: North Dakota Not in the current forecast horizon: 19 states No Response: 4 states Source: NCSL survey of state legislative fiscal offices, July 2010 –FY 2014 –FY 2015
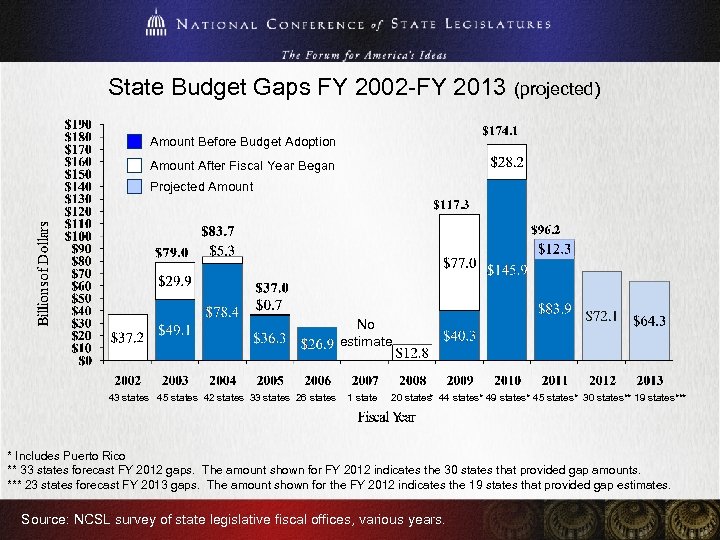
State Budget Gaps FY 2002 -FY 2013 (projected) Amount Before Budget Adoption Amount After Fiscal Year Began Projected Amount No estimate 43 states 45 states 42 states 33 states 26 states 1 state 20 states 44 states* 49 states* 45 states* 30 states** 19 states*** * * Includes Puerto Rico ** 33 states forecast FY 2012 gaps. The amount shown for FY 2012 indicates the 30 states that provided gap amounts. *** 23 states forecast FY 2013 gaps. The amount shown for the FY 2012 indicates the 19 states that provided gap estimates. Source: NCSL survey of state legislative fiscal offices, various years.
55
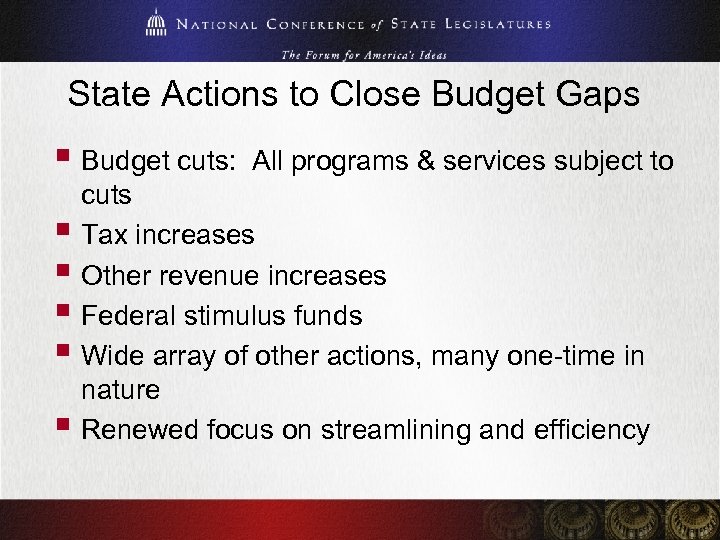
State Actions to Close Budget Gaps § Budget cuts: All programs & services subject to cuts § Tax increases § Other revenue increases § Federal stimulus funds § Wide array of other actions, many one-time in nature § Renewed focus on streamlining and efficiency
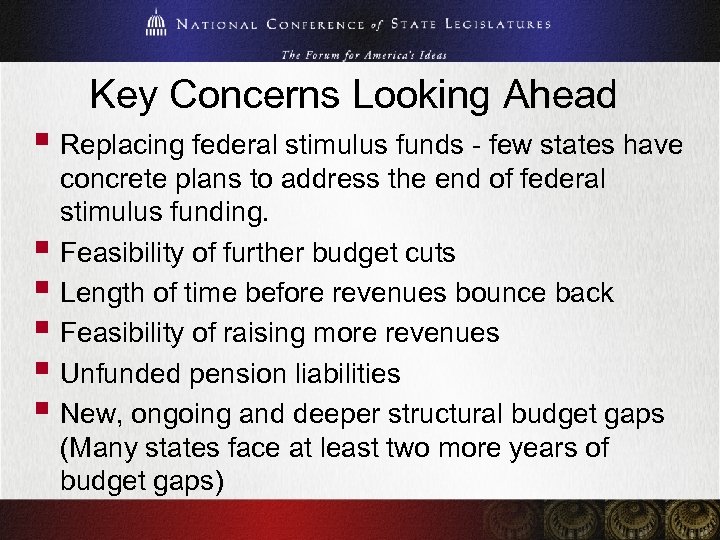
Key Concerns Looking Ahead § Replacing federal stimulus funds - few states have concrete plans to address the end of federal stimulus funding. § Feasibility of further budget cuts § Length of time before revenues bounce back § Feasibility of raising more revenues § Unfunded pension liabilities § New, ongoing and deeper structural budget gaps (Many states face at least two more years of budget gaps)
Mike Keefe, The Denver Post, Oct. 30, 2009
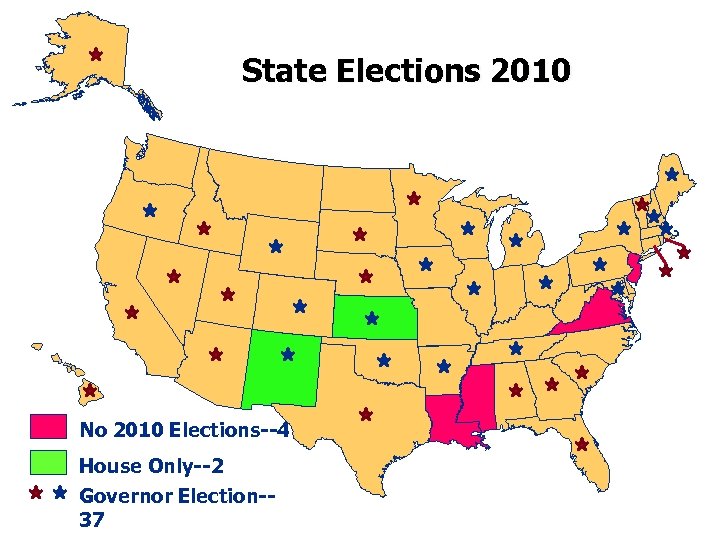
State Elections 2010 No 2010 Elections--4 House Only--2 Governor Election-37

www. ncsl. org For more information
Respondent Tom Ricketts, Ph. D, MPH Deputy Director, Policy Analysis Cecil G. Sheps Center for Health Services Research University of North Carolina
Discussion If you have a question for the speakers, please enter it in the chat window to your left. Time permitting, Gateway staff will raise them. If there is not sufficient time, Gateway staff will contact the presenters on your behalf and get back to you.
Thank You! We thank you for your interest and support. All Rural Health Research Center products can be accessed for free via the Rural Health Research Gateway at www. ruralhealthresearch. org. For more information related to health workforce, visit the Health Workforce Information Center at www. hwic. org. WWAMI: http: //depts. washington. edu/uwrhrc/ NCSL: http: //www. ncsl. org Sheps Center: http: //www. shepscenter. unc. edu
2ef2b02260ccd8ec8e65f2589d2127b7.ppt