acutediarrhea-131209014829-phpapp02.pptx
- Количество слайдов: 28
 SOEPEL Session 3 Internal Medicine Clinical Rotation (Hepato-gastroenterology) 1
SOEPEL Session 3 Internal Medicine Clinical Rotation (Hepato-gastroenterology) 1
 S § Subjective: § Patient: A 77 year-old male presented to the Emergency Department with complaints of two days of copious watery diarrhea. He denied abdominal pain or cramping, nausea, fever, and blood or mucus in the stool. The patient had a recent travel history including one week of boating in the Chesapeake Bay During the boat trip the patient and other travelers consumed raw oysters. Approximately 24 hours after returning from the trip, the patient developed symptoms. 2
S § Subjective: § Patient: A 77 year-old male presented to the Emergency Department with complaints of two days of copious watery diarrhea. He denied abdominal pain or cramping, nausea, fever, and blood or mucus in the stool. The patient had a recent travel history including one week of boating in the Chesapeake Bay During the boat trip the patient and other travelers consumed raw oysters. Approximately 24 hours after returning from the trip, the patient developed symptoms. 2
 OEP § Objective: § § § Temp: 36. 7. Pulse: 112 b/min RR: 16 /minute. BP: 132/80 mm. Hg. Mucous membranes were tacky. His abdomen was soft and non- tender, and without rebound, guarding, or flank pain § Evaluation: § DDx: traveler diarrhea, food poisoning, infectious diarrhea (bacterial). § Plan: § CBC: § WBC: 9. 1 x 10^9 / L with a slight left shift of 83% neutrophils. § Stool analysis: § +ive for occult blood § - ive for Clostridium difficile toxin and ova and parasites § Moderate white blood cells were present 3
OEP § Objective: § § § Temp: 36. 7. Pulse: 112 b/min RR: 16 /minute. BP: 132/80 mm. Hg. Mucous membranes were tacky. His abdomen was soft and non- tender, and without rebound, guarding, or flank pain § Evaluation: § DDx: traveler diarrhea, food poisoning, infectious diarrhea (bacterial). § Plan: § CBC: § WBC: 9. 1 x 10^9 / L with a slight left shift of 83% neutrophils. § Stool analysis: § +ive for occult blood § - ive for Clostridium difficile toxin and ova and parasites § Moderate white blood cells were present 3
 EL § Elaboration: § Relieve the symptoms. § Causes of this presentation. § Proper treatment strategy for this situation. § Learning Goals: §Acute diarrhea. 4
EL § Elaboration: § Relieve the symptoms. § Causes of this presentation. § Proper treatment strategy for this situation. § Learning Goals: §Acute diarrhea. 4
 § Increase in the stool weight to >250 g/d, accompanied by increase frequency and liquidity of stool. 1. Sudden onset of frequency with cramp pains, and a fever = infective cause. 2. bowel frequency with loose blood-stained stools = inflammatory basis. 3. passage of pale offensive stools that float, often accompanied by loss of appetite and weight loss, to steatorrhoea. Nocturnal bowel frequency and urgency usually = organic cause. 4. Passage of frequent small-volume stools (often formed) = functional cause. 5
§ Increase in the stool weight to >250 g/d, accompanied by increase frequency and liquidity of stool. 1. Sudden onset of frequency with cramp pains, and a fever = infective cause. 2. bowel frequency with loose blood-stained stools = inflammatory basis. 3. passage of pale offensive stools that float, often accompanied by loss of appetite and weight loss, to steatorrhoea. Nocturnal bowel frequency and urgency usually = organic cause. 4. Passage of frequent small-volume stools (often formed) = functional cause. 5
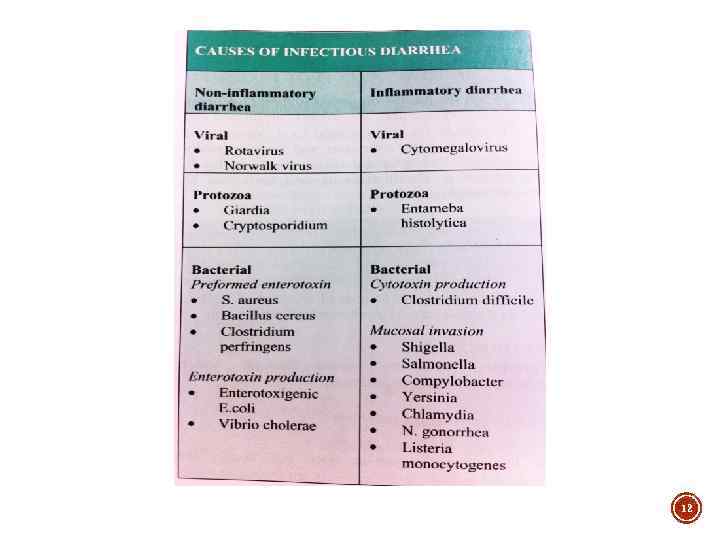
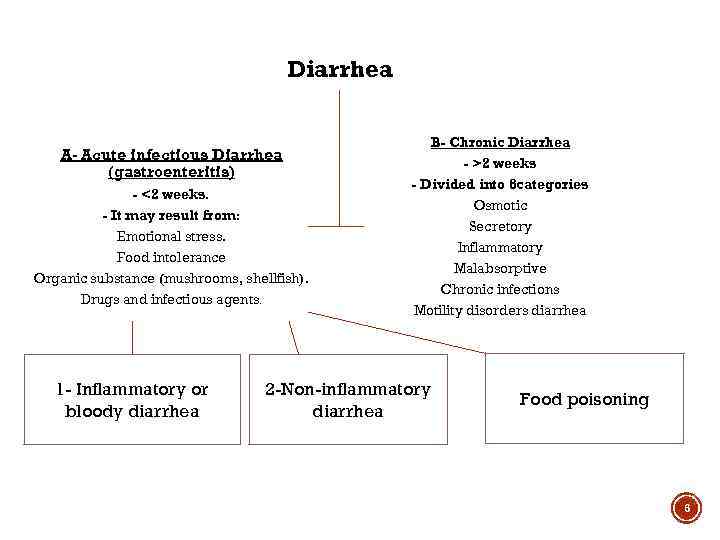 Diarrhea A- Acute infectious Diarrhea (gastroenteritis) - <2 weeks. - It may result from: Emotional stress. Food intolerance Organic substance (mushrooms, shellfish). Drugs and infectious agents. 1 - Inflammatory or bloody diarrhea B- Chronic Diarrhea - >2 weeks - Divided into 6 categories Osmotic Secretory Inflammatory Malabsorptive Chronic infections Motility disorders diarrhea 2 -Non-inflammatory diarrhea Food poisoning 6
Diarrhea A- Acute infectious Diarrhea (gastroenteritis) - <2 weeks. - It may result from: Emotional stress. Food intolerance Organic substance (mushrooms, shellfish). Drugs and infectious agents. 1 - Inflammatory or bloody diarrhea B- Chronic Diarrhea - >2 weeks - Divided into 6 categories Osmotic Secretory Inflammatory Malabsorptive Chronic infections Motility disorders diarrhea 2 -Non-inflammatory diarrhea Food poisoning 6
 § Suggest involvement of large intestine by invasive: o Bacteria. o Parasites. o Toxins. § Clinical pt. presentation: o Frequent bloody, small volume stools. o often +fever, +abdominal cramps, + tenesmus and fecal urgency. 7
§ Suggest involvement of large intestine by invasive: o Bacteria. o Parasites. o Toxins. § Clinical pt. presentation: o Frequent bloody, small volume stools. o often +fever, +abdominal cramps, + tenesmus and fecal urgency. 7
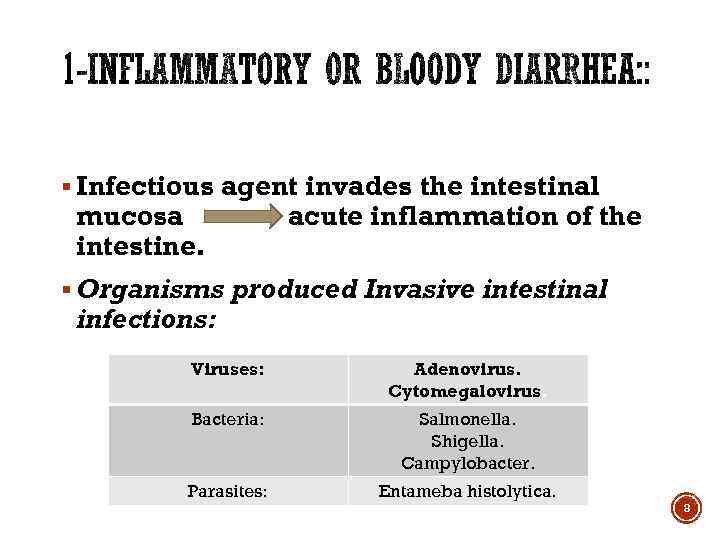 § Infectious agent invades the intestinal mucosa intestine. acute inflammation of the § Organisms produced Invasive intestinal infections: Viruses: Adenovirus. Cytomegalovirus. Bacteria: Salmonella. Shigella. Campylobacter. Parasites: Entameba histolytica. 8
§ Infectious agent invades the intestinal mucosa intestine. acute inflammation of the § Organisms produced Invasive intestinal infections: Viruses: Adenovirus. Cytomegalovirus. Bacteria: Salmonella. Shigella. Campylobacter. Parasites: Entameba histolytica. 8
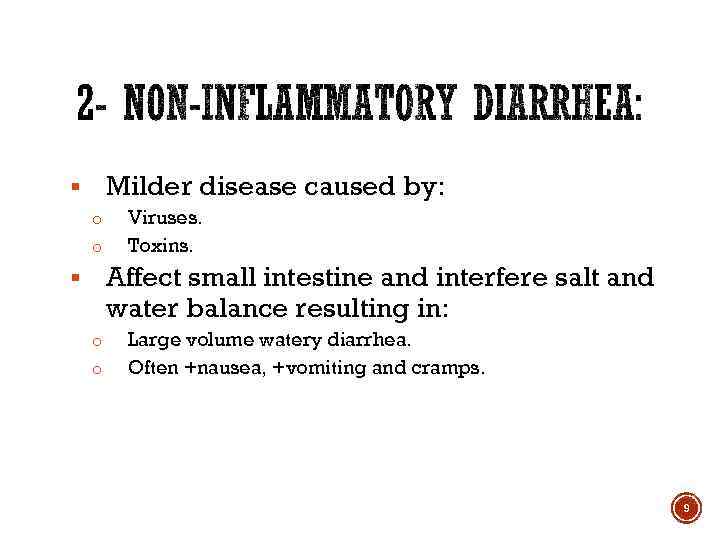 Milder disease caused by: § o o Viruses. Toxins. Affect small intestine and interfere salt and water balance resulting in: § o o Large volume watery diarrhea. Often +nausea, +vomiting and cramps. 9
Milder disease caused by: § o o Viruses. Toxins. Affect small intestine and interfere salt and water balance resulting in: § o o Large volume watery diarrhea. Often +nausea, +vomiting and cramps. 9
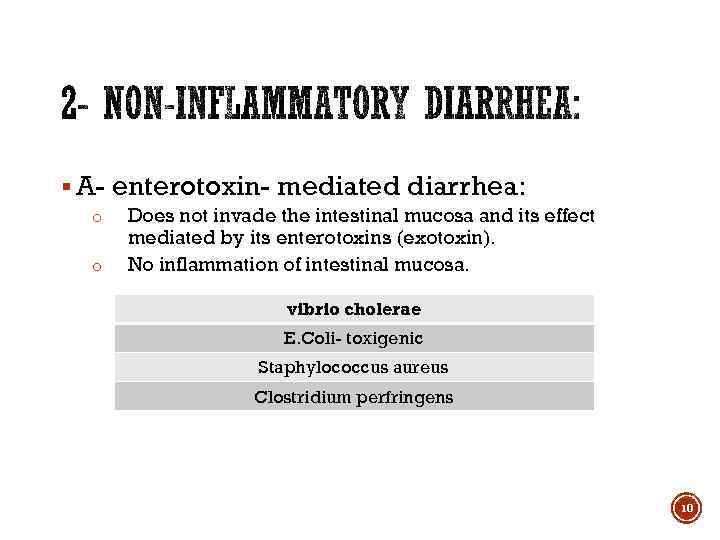 § A- enterotoxin- mediated diarrhea: o o Does not invade the intestinal mucosa and its effect mediated by its enterotoxins (exotoxin). No inflammation of intestinal mucosa. vibrio cholerae E. Coli- toxigenic Staphylococcus aureus Clostridium perfringens 10
§ A- enterotoxin- mediated diarrhea: o o Does not invade the intestinal mucosa and its effect mediated by its enterotoxins (exotoxin). No inflammation of intestinal mucosa. vibrio cholerae E. Coli- toxigenic Staphylococcus aureus Clostridium perfringens 10
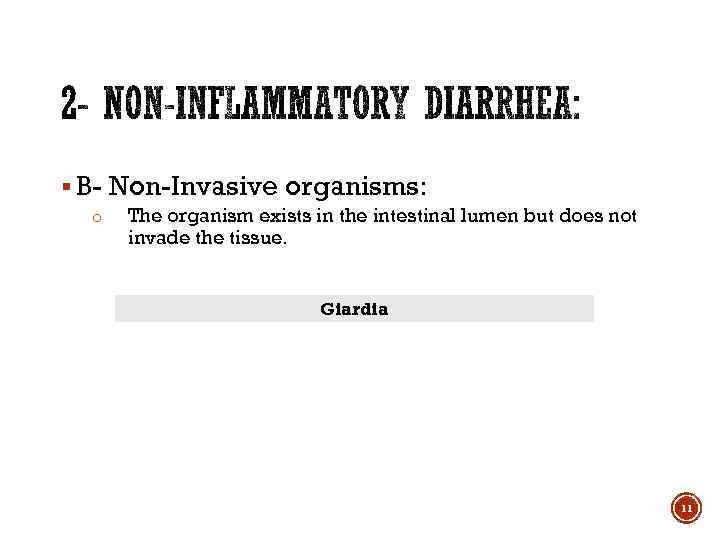 § B- Non-Invasive organisms: o The organism exists in the intestinal lumen but does not invade the tissue. Giardia 11
§ B- Non-Invasive organisms: o The organism exists in the intestinal lumen but does not invade the tissue. Giardia 11
 12
12
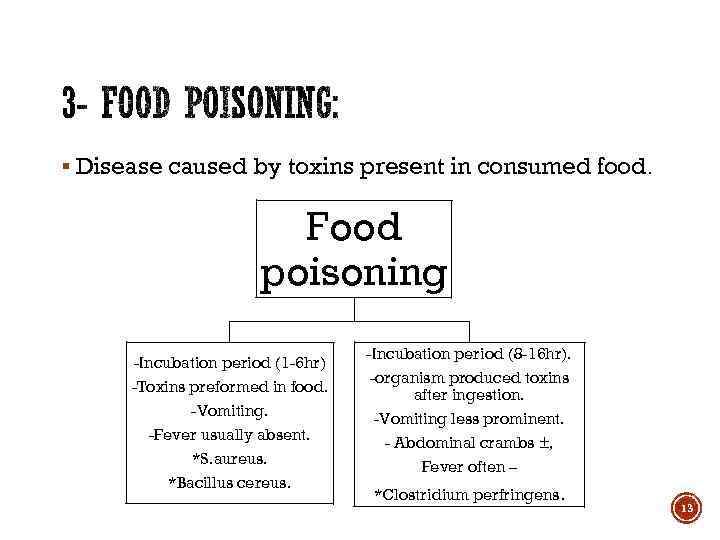 § Disease caused by toxins present in consumed food. Food poisoning -Incubation period (1 -6 hr) -Toxins preformed in food. -Vomiting. -Fever usually absent. *S. aureus. *Bacillus cereus. -Incubation period (8 -16 hr). -organism produced toxins after ingestion. -Vomiting less prominent. - Abdominal crambs ±, Fever often – *Clostridium perfringens. 13
§ Disease caused by toxins present in consumed food. Food poisoning -Incubation period (1 -6 hr) -Toxins preformed in food. -Vomiting. -Fever usually absent. *S. aureus. *Bacillus cereus. -Incubation period (8 -16 hr). -organism produced toxins after ingestion. -Vomiting less prominent. - Abdominal crambs ±, Fever often – *Clostridium perfringens. 13
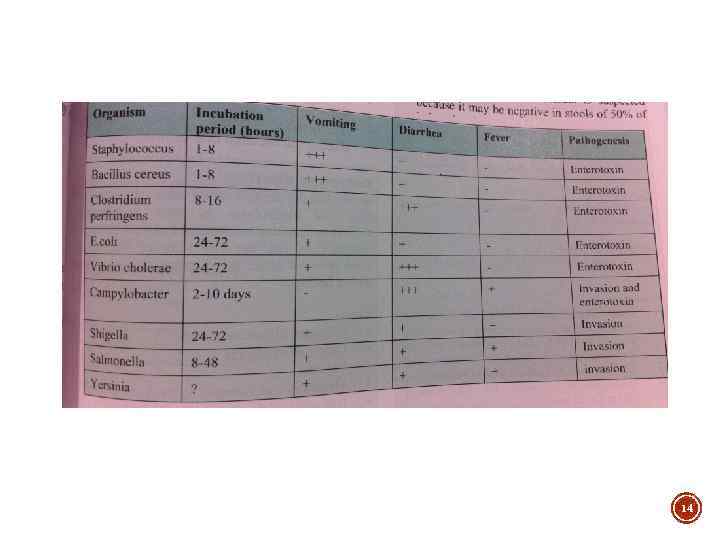 14
14
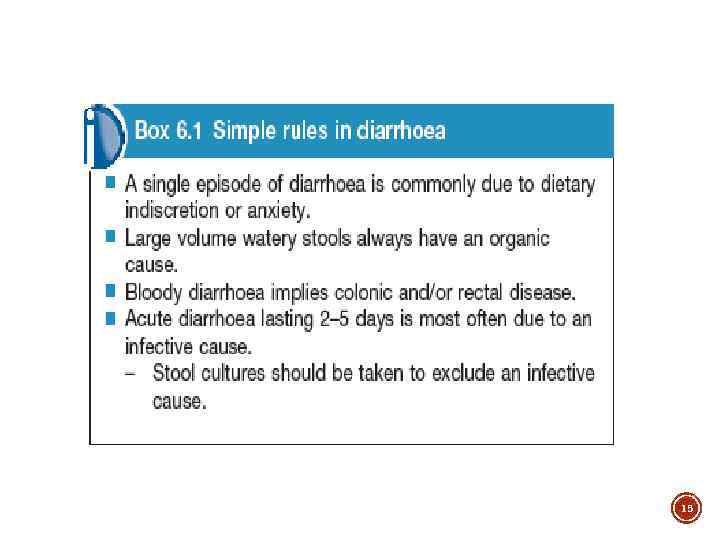 15
15
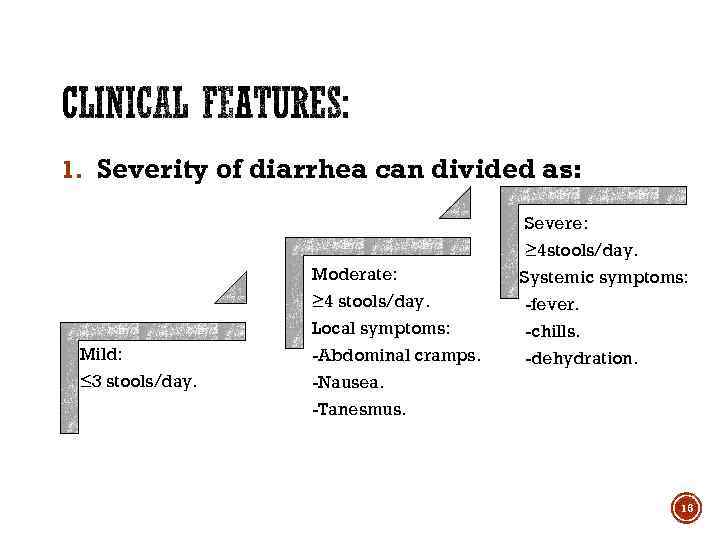 1. Severity of diarrhea can divided as: Severe: Moderate: Mild: ≤ 3 stools/day. ≥ 4 stools/day. Local symptoms: -Abdominal cramps. -Nausea. -Tanesmus. ≥ 4 stools/day. Systemic symptoms: -fever. -chills. -dehydration. 16
1. Severity of diarrhea can divided as: Severe: Moderate: Mild: ≤ 3 stools/day. ≥ 4 stools/day. Local symptoms: -Abdominal cramps. -Nausea. -Tanesmus. ≥ 4 stools/day. Systemic symptoms: -fever. -chills. -dehydration. 16
 2. Features suggest infectious diarrhea: § Similar recent illness in family members. § Recent ingestion of improperly stored or prepared food. § Exposure to unpurified water in camping. § Recent travel aboard causing( traveler diarrhea). § Antibiotics adm. Within the preceding several weeks increase likelihood of clostridium difficile colitis. 17
2. Features suggest infectious diarrhea: § Similar recent illness in family members. § Recent ingestion of improperly stored or prepared food. § Exposure to unpurified water in camping. § Recent travel aboard causing( traveler diarrhea). § Antibiotics adm. Within the preceding several weeks increase likelihood of clostridium difficile colitis. 17
 3. symptoms: § Nausea. § Vomiting. § Abd. Pain. § Fever. § Diarrhea: § Watery. § Bloody. 18
3. symptoms: § Nausea. § Vomiting. § Abd. Pain. § Fever. § Diarrhea: § Watery. § Bloody. 18
 4. Signs: § General appearance. § Mental status. § Dehydration manifestation: § Dry mouth. § Inelastic skin. § Oliguria. § Weakness. § Lethargy. § Sunken eyes. v. Depend of the degree of dehydration. § Abdominal examination: § Tenderness. § Peritonitis. § Features of metabolic acidosis. 19
4. Signs: § General appearance. § Mental status. § Dehydration manifestation: § Dry mouth. § Inelastic skin. § Oliguria. § Weakness. § Lethargy. § Sunken eyes. v. Depend of the degree of dehydration. § Abdominal examination: § Tenderness. § Peritonitis. § Features of metabolic acidosis. 19
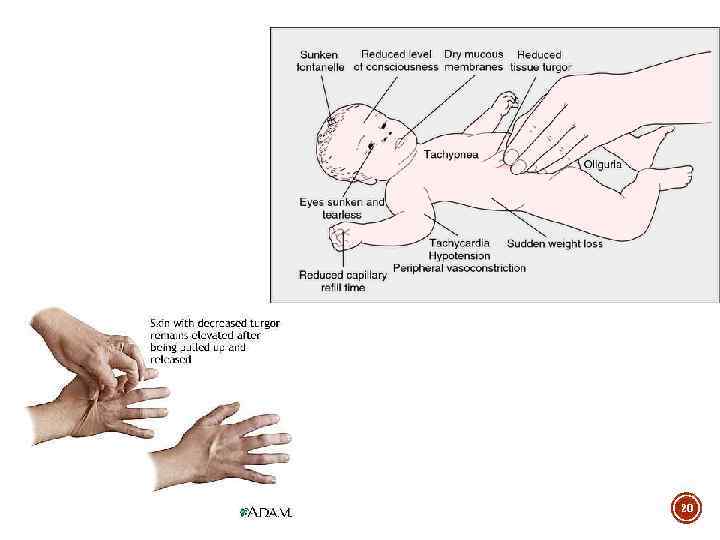 20
20
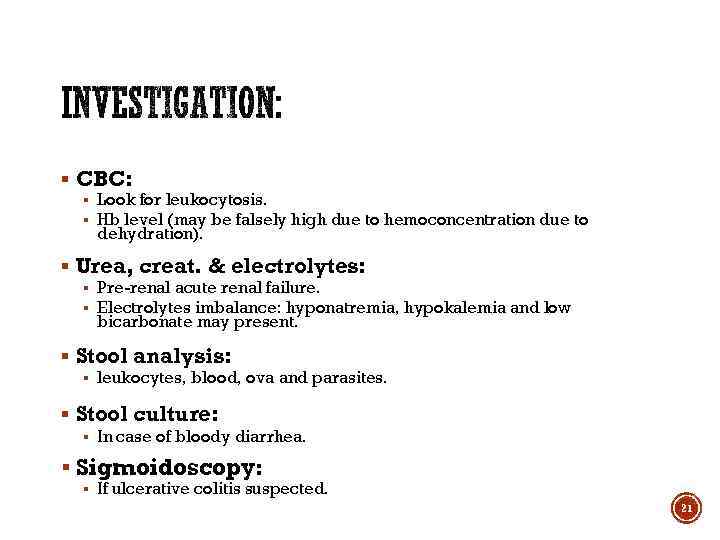 § CBC: § Look for leukocytosis. § Hb level (may be falsely high due to hemoconcentration due to dehydration). § Urea, creat. & electrolytes: § Pre-renal acute renal failure. § Electrolytes imbalance: hyponatremia, hypokalemia and low bicarbonate may present. § Stool analysis: § leukocytes, blood, ova and parasites. § Stool culture: § In case of bloody diarrhea. § Sigmoidoscopy: § If ulcerative colitis suspected. 21
§ CBC: § Look for leukocytosis. § Hb level (may be falsely high due to hemoconcentration due to dehydration). § Urea, creat. & electrolytes: § Pre-renal acute renal failure. § Electrolytes imbalance: hyponatremia, hypokalemia and low bicarbonate may present. § Stool analysis: § leukocytes, blood, ova and parasites. § Stool culture: § In case of bloody diarrhea. § Sigmoidoscopy: § If ulcerative colitis suspected. 21
 ØCirculatory shock. ØAcute renal failure. ØElectrolytes depletion leading to lethargy and paralytic ileus. ØMetabolic acidosis. 22
ØCirculatory shock. ØAcute renal failure. ØElectrolytes depletion leading to lethargy and paralytic ileus. ØMetabolic acidosis. 22
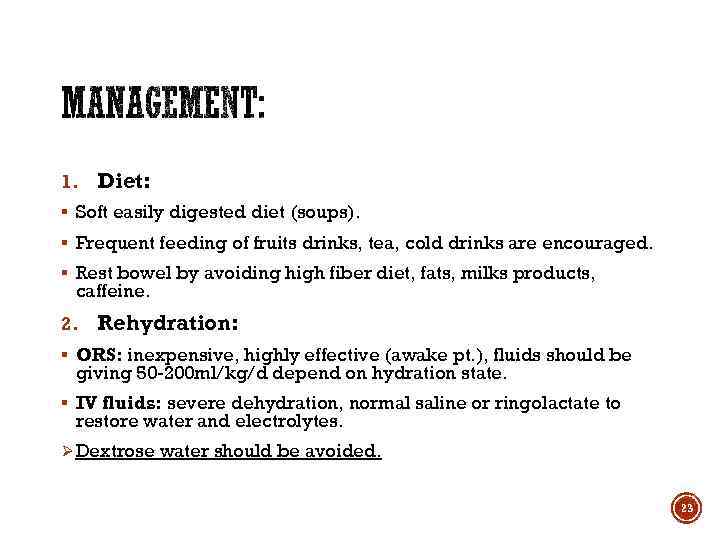 1. Diet: § Soft easily digested diet (soups). § Frequent feeding of fruits drinks, tea, cold drinks are encouraged. § Rest bowel by avoiding high fiber diet, fats, milks products, caffeine. 2. Rehydration: § ORS: inexpensive, highly effective (awake pt. ), fluids should be giving 50 -200 ml/kg/d depend on hydration state. § IV fluids: severe dehydration, normal saline or ringolactate to restore water and electrolytes. Ø Dextrose water should be avoided. 23
1. Diet: § Soft easily digested diet (soups). § Frequent feeding of fruits drinks, tea, cold drinks are encouraged. § Rest bowel by avoiding high fiber diet, fats, milks products, caffeine. 2. Rehydration: § ORS: inexpensive, highly effective (awake pt. ), fluids should be giving 50 -200 ml/kg/d depend on hydration state. § IV fluids: severe dehydration, normal saline or ringolactate to restore water and electrolytes. Ø Dextrose water should be avoided. 23
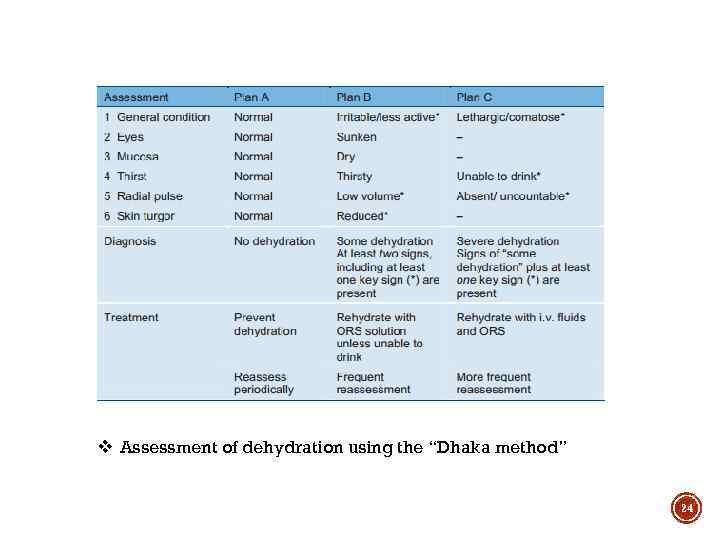 v Assessment of dehydration using the “Dhaka method” 24
v Assessment of dehydration using the “Dhaka method” 24
 3. Antidiarrheal agents: § Mild to moderate diarrhea (improve pt. comfort). § Contraindicated in : § Bloody diarrhea. § High fever. § Systemic toxicity. ØLoperamide (cap. Imodium 2 mg) : initially 4 mg followed by 2 mg after each loose stool. (max. 16 mg/24 hr) 25
3. Antidiarrheal agents: § Mild to moderate diarrhea (improve pt. comfort). § Contraindicated in : § Bloody diarrhea. § High fever. § Systemic toxicity. ØLoperamide (cap. Imodium 2 mg) : initially 4 mg followed by 2 mg after each loose stool. (max. 16 mg/24 hr) 25
 3. Antibiotic therapy (empirical treatment): § Not recommended for all pts. With acute diarrhea. § Only Invasive bacterial infection suggested by clinical manifestation: § § Moderate- sever fever. Tanesmus. Bloody stool. Present of fecal leukocytes while stool culture in process. ØDrug of choice is quinolone such as: Ø Ciprofloxacin (ciproxin)500 mg TPD/5 -7 days. Ø If suspect Giardia give metronidazole (flagyl) 250 -500 mg four times /day. (Giardia appear –ive in 50% of pts. 26
3. Antibiotic therapy (empirical treatment): § Not recommended for all pts. With acute diarrhea. § Only Invasive bacterial infection suggested by clinical manifestation: § § Moderate- sever fever. Tanesmus. Bloody stool. Present of fecal leukocytes while stool culture in process. ØDrug of choice is quinolone such as: Ø Ciprofloxacin (ciproxin)500 mg TPD/5 -7 days. Ø If suspect Giardia give metronidazole (flagyl) 250 -500 mg four times /day. (Giardia appear –ive in 50% of pts. 26
 § (World Gastroenterology Organization Global Guidelines 2012) § http: //www. worldgastroenterology. org/assets/export/userfiles/Ac ute%20 Diarrhea_long_FINAL_120604. pdf § Medical diagnosis and management (INAM DANISH). 27
§ (World Gastroenterology Organization Global Guidelines 2012) § http: //www. worldgastroenterology. org/assets/export/userfiles/Ac ute%20 Diarrhea_long_FINAL_120604. pdf § Medical diagnosis and management (INAM DANISH). 27
 28
28


