cddb719ddcd83e8b97347c889f3ba660.ppt
- Количество слайдов: 37
 Sodium Disorders: Hyponatremia William Harper, MD, FRCPC Endocrinology & Metabolism Assistant Professor of Medicine Mc. Master University
Sodium Disorders: Hyponatremia William Harper, MD, FRCPC Endocrinology & Metabolism Assistant Professor of Medicine Mc. Master University
![Normal Serum [Na] (135 -145 m. Eq/L) Closely Guarded ADH (p. M) ↓ ECFv Normal Serum [Na] (135 -145 m. Eq/L) Closely Guarded ADH (p. M) ↓ ECFv](https://present5.com/presentation/cddb719ddcd83e8b97347c889f3ba660/image-3.jpg) Normal Serum [Na] (135 -145 m. Eq/L) Closely Guarded ADH (p. M) ↓ ECFv Thirst 5 0 135 140 145 PNa (m. Eq/L)
Normal Serum [Na] (135 -145 m. Eq/L) Closely Guarded ADH (p. M) ↓ ECFv Thirst 5 0 135 140 145 PNa (m. Eq/L)
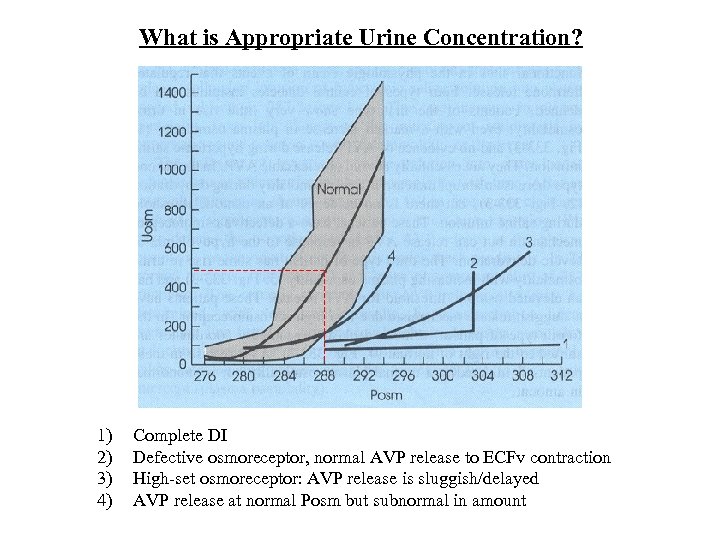 What is Appropriate Urine Concentration? 1) 2) 3) 4) Complete DI Defective osmoreceptor, normal AVP release to ECFv contraction High-set osmoreceptor: AVP release is sluggish/delayed AVP release at normal Posm but subnormal in amount
What is Appropriate Urine Concentration? 1) 2) 3) 4) Complete DI Defective osmoreceptor, normal AVP release to ECFv contraction High-set osmoreceptor: AVP release is sluggish/delayed AVP release at normal Posm but subnormal in amount
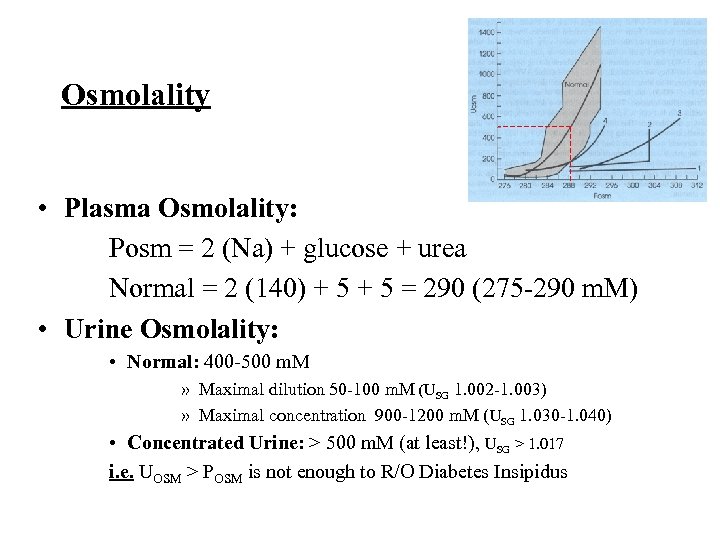 Osmolality • Plasma Osmolality: Posm = 2 (Na) + glucose + urea Normal = 2 (140) + 5 = 290 (275 -290 m. M) • Urine Osmolality: • Normal: 400 -500 m. M » Maximal dilution 50 -100 m. M (USG 1. 002 -1. 003) » Maximal concentration 900 -1200 m. M (USG 1. 030 -1. 040) • Concentrated Urine: > 500 m. M (at least!), USG > 1. 017 i. e. UOSM > POSM is not enough to R/O Diabetes Insipidus
Osmolality • Plasma Osmolality: Posm = 2 (Na) + glucose + urea Normal = 2 (140) + 5 = 290 (275 -290 m. M) • Urine Osmolality: • Normal: 400 -500 m. M » Maximal dilution 50 -100 m. M (USG 1. 002 -1. 003) » Maximal concentration 900 -1200 m. M (USG 1. 030 -1. 040) • Concentrated Urine: > 500 m. M (at least!), USG > 1. 017 i. e. UOSM > POSM is not enough to R/O Diabetes Insipidus
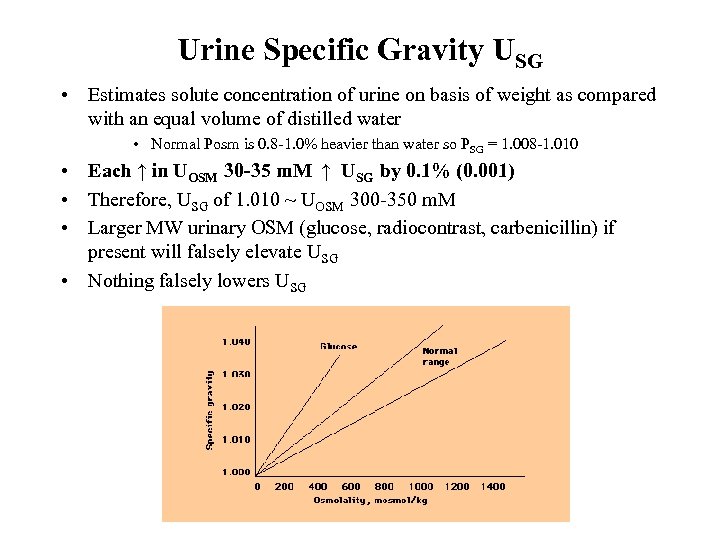 Urine Specific Gravity USG • Estimates solute concentration of urine on basis of weight as compared with an equal volume of distilled water • Normal Posm is 0. 8 -1. 0% heavier than water so PSG = 1. 008 -1. 010 • Each ↑ in UOSM 30 -35 m. M ↑ USG by 0. 1% (0. 001) • Therefore, USG of 1. 010 ~ UOSM 300 -350 m. M • Larger MW urinary OSM (glucose, radiocontrast, carbenicillin) if present will falsely elevate USG • Nothing falsely lowers USG
Urine Specific Gravity USG • Estimates solute concentration of urine on basis of weight as compared with an equal volume of distilled water • Normal Posm is 0. 8 -1. 0% heavier than water so PSG = 1. 008 -1. 010 • Each ↑ in UOSM 30 -35 m. M ↑ USG by 0. 1% (0. 001) • Therefore, USG of 1. 010 ~ UOSM 300 -350 m. M • Larger MW urinary OSM (glucose, radiocontrast, carbenicillin) if present will falsely elevate USG • Nothing falsely lowers USG
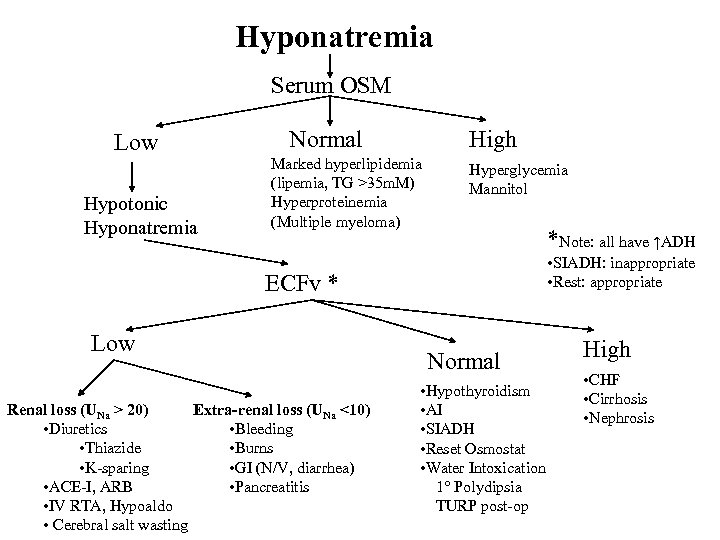 Hyponatremia Serum OSM Low Hypotonic Hyponatremia Normal High Marked hyperlipidemia (lipemia, TG >35 m. M) Hyperproteinemia (Multiple myeloma) Hyperglycemia Mannitol *Note: all have ↑ADH • SIADH: inappropriate • Rest: appropriate ECFv * Low Renal loss (UNa > 20) Extra-renal loss (UNa <10) • Diuretics • Bleeding • Thiazide • Burns • K-sparing • GI (N/V, diarrhea) • ACE-I, ARB • Pancreatitis • IV RTA, Hypoaldo • Cerebral salt wasting Normal • Hypothyroidism • AI • SIADH • Reset Osmostat • Water Intoxication 1° Polydipsia TURP post-op High • CHF • Cirrhosis • Nephrosis
Hyponatremia Serum OSM Low Hypotonic Hyponatremia Normal High Marked hyperlipidemia (lipemia, TG >35 m. M) Hyperproteinemia (Multiple myeloma) Hyperglycemia Mannitol *Note: all have ↑ADH • SIADH: inappropriate • Rest: appropriate ECFv * Low Renal loss (UNa > 20) Extra-renal loss (UNa <10) • Diuretics • Bleeding • Thiazide • Burns • K-sparing • GI (N/V, diarrhea) • ACE-I, ARB • Pancreatitis • IV RTA, Hypoaldo • Cerebral salt wasting Normal • Hypothyroidism • AI • SIADH • Reset Osmostat • Water Intoxication 1° Polydipsia TURP post-op High • CHF • Cirrhosis • Nephrosis
![Rx Hyponatremia • Na deficit = 0. 6 x wt(kg) x (desired [Na] - Rx Hyponatremia • Na deficit = 0. 6 x wt(kg) x (desired [Na] -](https://present5.com/presentation/cddb719ddcd83e8b97347c889f3ba660/image-8.jpg) Rx Hyponatremia • Na deficit = 0. 6 x wt(kg) x (desired [Na] - actual [Na]) (mmol) • When do you need to Rx quickly? – Acute (<24 h) severe (< 120 m. Eq/L) Hyponatremia • Prevent brain swelling or Rx brain swelling – Symptomatic Hyponatremia (Seizures, coma, etc. ) • Alleviate symptoms • “Quickly”: 3% NS, 1 -2 m. Eq/L/h until: • Symptoms stop • 3 -4 h elapsed and/or Serum Na has reached 120 m. Eq/L • Then SLOW down correction to 0. 5 m. Eq/L/h with 0. 9% NS or simply fluid restriction. Aim for overall 24 h correction to be < 10 -12 m. Eq/L/d to prevent myelinolysis
Rx Hyponatremia • Na deficit = 0. 6 x wt(kg) x (desired [Na] - actual [Na]) (mmol) • When do you need to Rx quickly? – Acute (<24 h) severe (< 120 m. Eq/L) Hyponatremia • Prevent brain swelling or Rx brain swelling – Symptomatic Hyponatremia (Seizures, coma, etc. ) • Alleviate symptoms • “Quickly”: 3% NS, 1 -2 m. Eq/L/h until: • Symptoms stop • 3 -4 h elapsed and/or Serum Na has reached 120 m. Eq/L • Then SLOW down correction to 0. 5 m. Eq/L/h with 0. 9% NS or simply fluid restriction. Aim for overall 24 h correction to be < 10 -12 m. Eq/L/d to prevent myelinolysis
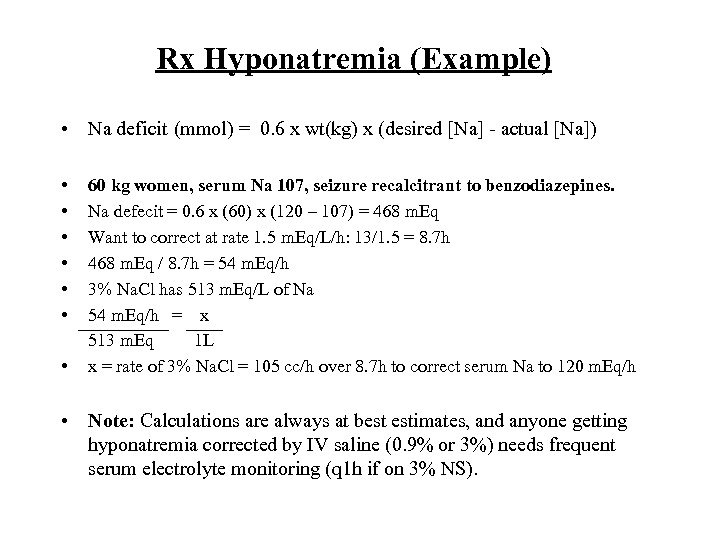 Rx Hyponatremia (Example) • Na deficit (mmol) = 0. 6 x wt(kg) x (desired [Na] - actual [Na]) • • 60 kg women, serum Na 107, seizure recalcitrant to benzodiazepines. Na defecit = 0. 6 x (60) x (120 – 107) = 468 m. Eq Want to correct at rate 1. 5 m. Eq/L/h: 13/1. 5 = 8. 7 h 468 m. Eq / 8. 7 h = 54 m. Eq/h 3% Na. Cl has 513 m. Eq/L of Na 54 m. Eq/h = x 513 m. Eq 1 L x = rate of 3% Na. Cl = 105 cc/h over 8. 7 h to correct serum Na to 120 m. Eq/h • Note: Calculations are always at best estimates, and anyone getting hyponatremia corrected by IV saline (0. 9% or 3%) needs frequent serum electrolyte monitoring (q 1 h if on 3% NS).
Rx Hyponatremia (Example) • Na deficit (mmol) = 0. 6 x wt(kg) x (desired [Na] - actual [Na]) • • 60 kg women, serum Na 107, seizure recalcitrant to benzodiazepines. Na defecit = 0. 6 x (60) x (120 – 107) = 468 m. Eq Want to correct at rate 1. 5 m. Eq/L/h: 13/1. 5 = 8. 7 h 468 m. Eq / 8. 7 h = 54 m. Eq/h 3% Na. Cl has 513 m. Eq/L of Na 54 m. Eq/h = x 513 m. Eq 1 L x = rate of 3% Na. Cl = 105 cc/h over 8. 7 h to correct serum Na to 120 m. Eq/h • Note: Calculations are always at best estimates, and anyone getting hyponatremia corrected by IV saline (0. 9% or 3%) needs frequent serum electrolyte monitoring (q 1 h if on 3% NS).
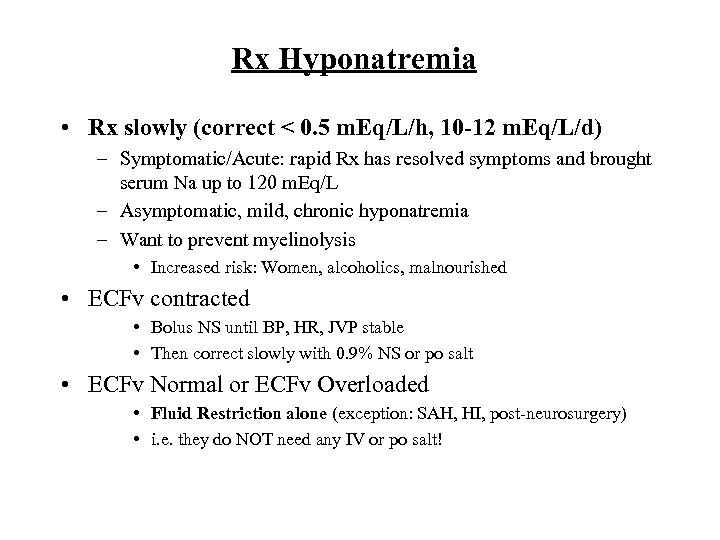 Rx Hyponatremia • Rx slowly (correct < 0. 5 m. Eq/L/h, 10 -12 m. Eq/L/d) – Symptomatic/Acute: rapid Rx has resolved symptoms and brought serum Na up to 120 m. Eq/L – Asymptomatic, mild, chronic hyponatremia – Want to prevent myelinolysis • Increased risk: Women, alcoholics, malnourished • ECFv contracted • Bolus NS until BP, HR, JVP stable • Then correct slowly with 0. 9% NS or po salt • ECFv Normal or ECFv Overloaded • Fluid Restriction alone (exception: SAH, HI, post-neurosurgery) • i. e. they do NOT need any IV or po salt!
Rx Hyponatremia • Rx slowly (correct < 0. 5 m. Eq/L/h, 10 -12 m. Eq/L/d) – Symptomatic/Acute: rapid Rx has resolved symptoms and brought serum Na up to 120 m. Eq/L – Asymptomatic, mild, chronic hyponatremia – Want to prevent myelinolysis • Increased risk: Women, alcoholics, malnourished • ECFv contracted • Bolus NS until BP, HR, JVP stable • Then correct slowly with 0. 9% NS or po salt • ECFv Normal or ECFv Overloaded • Fluid Restriction alone (exception: SAH, HI, post-neurosurgery) • i. e. they do NOT need any IV or po salt!
 SIADH Ddx • • Intracranial disease Pulmonary disease Chest wall disorder (surgery, VZV) Severe pain or emotional distress Severe N/V Ectopic ADH: Small cell lung cancer Drugs: opiods, carbamazepine, chlorpropamide, cyclophosphamide, cisplatin, vincristine, vinblastine, amitriptylline, SSRI, neuroleptics, bromocriptine, ecstasy (MDMA)
SIADH Ddx • • Intracranial disease Pulmonary disease Chest wall disorder (surgery, VZV) Severe pain or emotional distress Severe N/V Ectopic ADH: Small cell lung cancer Drugs: opiods, carbamazepine, chlorpropamide, cyclophosphamide, cisplatin, vincristine, vinblastine, amitriptylline, SSRI, neuroleptics, bromocriptine, ecstasy (MDMA)
 SIADH Diagnosis • • • Normal ECFv (or slightly increased) Hypothyroidism & AI ruled out ↓ serum Na/OSM UOSM > 100 m. M, UNa > 40 m. Eq/L Low plasma uric acid (< 238 umol/L) Treatment • • • Fluid Restriction Oral Salt, Hi-protein diet or Urea(30 g/d): promote solute diuresis Lasix 20 mg po od-bid: Loop direct diminishes medullary gradient Demeclocycline 300 -600 mg bid (can be nephrotoxic) Lithium (induces NDI) IV salt solution: • Rarely if ever needed (i. e. only if symptomatic with SZ/coma) • Solution given must be of greater OSM than UOSM or in long run will just make hyponatremia worse (often IV NS not sufficient)
SIADH Diagnosis • • • Normal ECFv (or slightly increased) Hypothyroidism & AI ruled out ↓ serum Na/OSM UOSM > 100 m. M, UNa > 40 m. Eq/L Low plasma uric acid (< 238 umol/L) Treatment • • • Fluid Restriction Oral Salt, Hi-protein diet or Urea(30 g/d): promote solute diuresis Lasix 20 mg po od-bid: Loop direct diminishes medullary gradient Demeclocycline 300 -600 mg bid (can be nephrotoxic) Lithium (induces NDI) IV salt solution: • Rarely if ever needed (i. e. only if symptomatic with SZ/coma) • Solution given must be of greater OSM than UOSM or in long run will just make hyponatremia worse (often IV NS not sufficient)
 SIADH: Example • UOSM fixed 600 m. M due to ADH action • 1 L NS given: 300 m. M (154 m. M each of Na and Cl) • All sodium will be excreted as renal sodium handling is intact in SIADH. • 300 mmoles of osmols given excreted in 500 cc urine (300 mmoles/500 m. L = 600 m. M) • Therefore net gain of 500 cc free water! • 1 L 3% saline given: 1026 mmoles • Excreted in 1. 7 L to keep UOSM 600 m. M • Therefore net loss of 700 cc free water! • NOT advocating use of any IV NS (0. 9% or 3%) in SIADH unless absolutely neccesary (i. e. SZ, coma). Most SIADH hyponatremia is chronic and should be corrected slowly with fluid restriction ONLY.
SIADH: Example • UOSM fixed 600 m. M due to ADH action • 1 L NS given: 300 m. M (154 m. M each of Na and Cl) • All sodium will be excreted as renal sodium handling is intact in SIADH. • 300 mmoles of osmols given excreted in 500 cc urine (300 mmoles/500 m. L = 600 m. M) • Therefore net gain of 500 cc free water! • 1 L 3% saline given: 1026 mmoles • Excreted in 1. 7 L to keep UOSM 600 m. M • Therefore net loss of 700 cc free water! • NOT advocating use of any IV NS (0. 9% or 3%) in SIADH unless absolutely neccesary (i. e. SZ, coma). Most SIADH hyponatremia is chronic and should be corrected slowly with fluid restriction ONLY.
 Reset Osmostat • 25 -30% of circumstances which cause SIADH • Downward resetting of the threshold for both ADH release and thirst. • Mild asymptomatic hyponatremia (Na 125 -135 m. Eq/L) • Distinguish from SIADH by observing response to water load (10 -15 m. L/kg po or IV) • Normal subjects and those with reset osmostat will secrete the entire water load over 4 h without any worsening of the hyponatremia • Attempts to correct hyponatremia in reset osmostat are not needed and will cause severe thirst
Reset Osmostat • 25 -30% of circumstances which cause SIADH • Downward resetting of the threshold for both ADH release and thirst. • Mild asymptomatic hyponatremia (Na 125 -135 m. Eq/L) • Distinguish from SIADH by observing response to water load (10 -15 m. L/kg po or IV) • Normal subjects and those with reset osmostat will secrete the entire water load over 4 h without any worsening of the hyponatremia • Attempts to correct hyponatremia in reset osmostat are not needed and will cause severe thirst
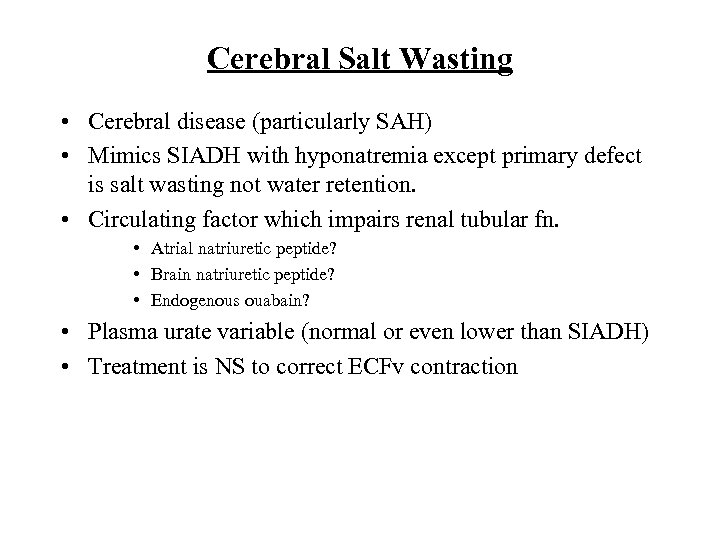 Cerebral Salt Wasting • Cerebral disease (particularly SAH) • Mimics SIADH with hyponatremia except primary defect is salt wasting not water retention. • Circulating factor which impairs renal tubular fn. • Atrial natriuretic peptide? • Brain natriuretic peptide? • Endogenous ouabain? • Plasma urate variable (normal or even lower than SIADH) • Treatment is NS to correct ECFv contraction
Cerebral Salt Wasting • Cerebral disease (particularly SAH) • Mimics SIADH with hyponatremia except primary defect is salt wasting not water retention. • Circulating factor which impairs renal tubular fn. • Atrial natriuretic peptide? • Brain natriuretic peptide? • Endogenous ouabain? • Plasma urate variable (normal or even lower than SIADH) • Treatment is NS to correct ECFv contraction
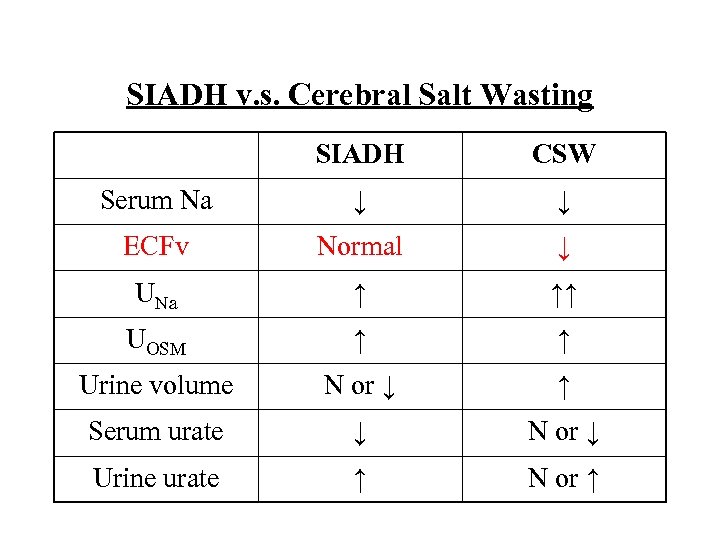 SIADH v. s. Cerebral Salt Wasting SIADH CSW Serum Na ↓ ↓ ECFv Normal ↓ UNa ↑ ↑↑ UOSM ↑ ↑ Urine volume N or ↓ ↑ Serum urate ↓ N or ↓ Urine urate ↑ N or ↑
SIADH v. s. Cerebral Salt Wasting SIADH CSW Serum Na ↓ ↓ ECFv Normal ↓ UNa ↑ ↑↑ UOSM ↑ ↑ Urine volume N or ↓ ↑ Serum urate ↓ N or ↓ Urine urate ↑ N or ↑
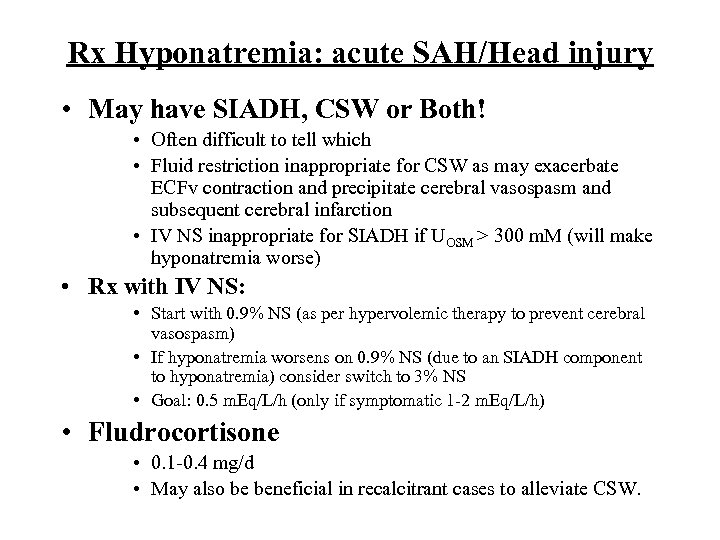 Rx Hyponatremia: acute SAH/Head injury • May have SIADH, CSW or Both! • Often difficult to tell which • Fluid restriction inappropriate for CSW as may exacerbate ECFv contraction and precipitate cerebral vasospasm and subsequent cerebral infarction • IV NS inappropriate for SIADH if UOSM > 300 m. M (will make hyponatremia worse) • Rx with IV NS: • Start with 0. 9% NS (as per hypervolemic therapy to prevent cerebral vasospasm) • If hyponatremia worsens on 0. 9% NS (due to an SIADH component to hyponatremia) consider switch to 3% NS • Goal: 0. 5 m. Eq/L/h (only if symptomatic 1 -2 m. Eq/L/h) • Fludrocortisone • 0. 1 -0. 4 mg/d • May also be beneficial in recalcitrant cases to alleviate CSW.
Rx Hyponatremia: acute SAH/Head injury • May have SIADH, CSW or Both! • Often difficult to tell which • Fluid restriction inappropriate for CSW as may exacerbate ECFv contraction and precipitate cerebral vasospasm and subsequent cerebral infarction • IV NS inappropriate for SIADH if UOSM > 300 m. M (will make hyponatremia worse) • Rx with IV NS: • Start with 0. 9% NS (as per hypervolemic therapy to prevent cerebral vasospasm) • If hyponatremia worsens on 0. 9% NS (due to an SIADH component to hyponatremia) consider switch to 3% NS • Goal: 0. 5 m. Eq/L/h (only if symptomatic 1 -2 m. Eq/L/h) • Fludrocortisone • 0. 1 -0. 4 mg/d • May also be beneficial in recalcitrant cases to alleviate CSW.
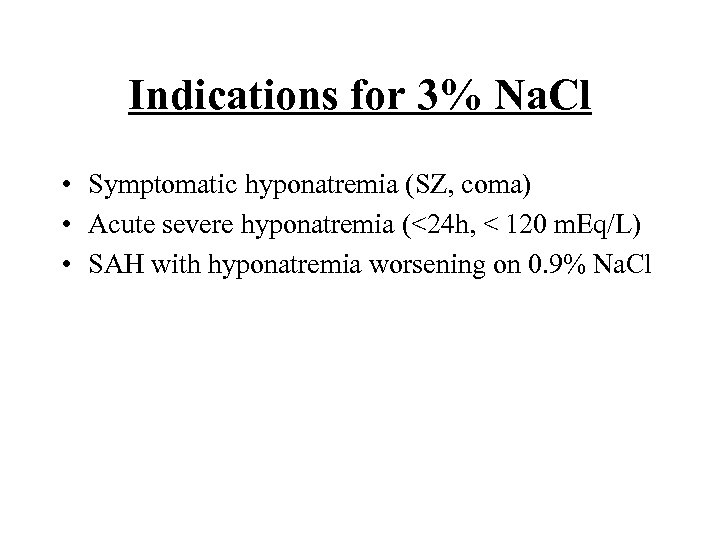 Indications for 3% Na. Cl • Symptomatic hyponatremia (SZ, coma) • Acute severe hyponatremia (<24 h, < 120 m. Eq/L) • SAH with hyponatremia worsening on 0. 9% Na. Cl
Indications for 3% Na. Cl • Symptomatic hyponatremia (SZ, coma) • Acute severe hyponatremia (<24 h, < 120 m. Eq/L) • SAH with hyponatremia worsening on 0. 9% Na. Cl
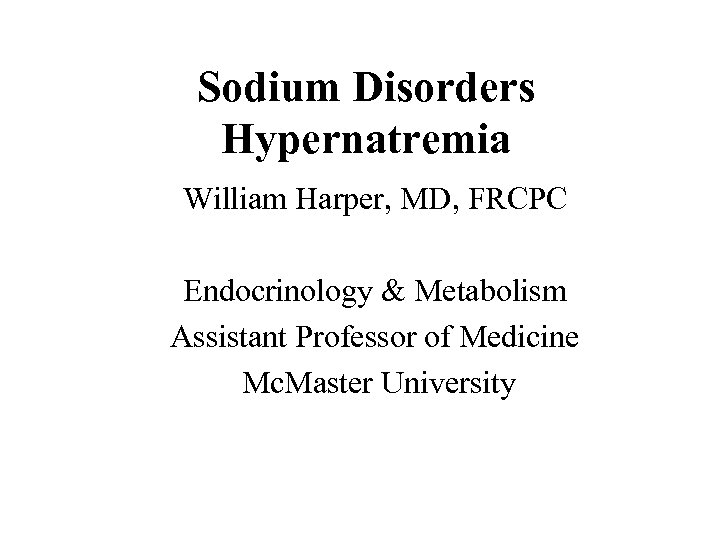 Sodium Disorders Hypernatremia William Harper, MD, FRCPC Endocrinology & Metabolism Assistant Professor of Medicine Mc. Master University
Sodium Disorders Hypernatremia William Harper, MD, FRCPC Endocrinology & Metabolism Assistant Professor of Medicine Mc. Master University
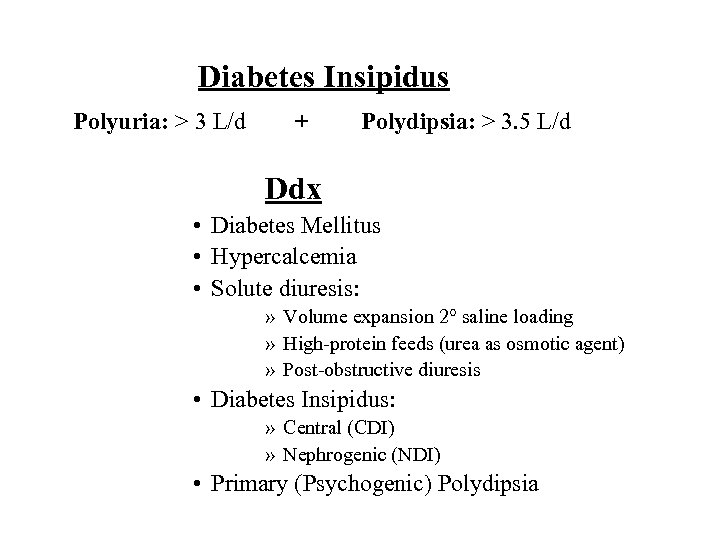 Diabetes Insipidus Polyuria: > 3 L/d + Polydipsia: > 3. 5 L/d Ddx • Diabetes Mellitus • Hypercalcemia • Solute diuresis: » Volume expansion 2° saline loading » High-protein feeds (urea as osmotic agent) » Post-obstructive diuresis • Diabetes Insipidus: » Central (CDI) » Nephrogenic (NDI) • Primary (Psychogenic) Polydipsia
Diabetes Insipidus Polyuria: > 3 L/d + Polydipsia: > 3. 5 L/d Ddx • Diabetes Mellitus • Hypercalcemia • Solute diuresis: » Volume expansion 2° saline loading » High-protein feeds (urea as osmotic agent) » Post-obstructive diuresis • Diabetes Insipidus: » Central (CDI) » Nephrogenic (NDI) • Primary (Psychogenic) Polydipsia
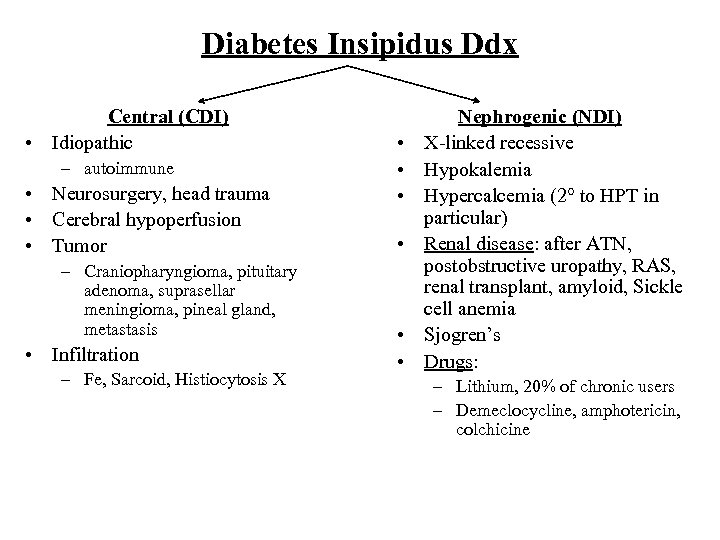 Diabetes Insipidus Ddx Central (CDI) • Idiopathic – autoimmune • Neurosurgery, head trauma • Cerebral hypoperfusion • Tumor – Craniopharyngioma, pituitary adenoma, suprasellar meningioma, pineal gland, metastasis • Infiltration – Fe, Sarcoid, Histiocytosis X • • • Nephrogenic (NDI) X-linked recessive Hypokalemia Hypercalcemia (2° to HPT in particular) Renal disease: after ATN, postobstructive uropathy, RAS, renal transplant, amyloid, Sickle cell anemia Sjogren’s Drugs: – Lithium, 20% of chronic users – Demeclocycline, amphotericin, colchicine
Diabetes Insipidus Ddx Central (CDI) • Idiopathic – autoimmune • Neurosurgery, head trauma • Cerebral hypoperfusion • Tumor – Craniopharyngioma, pituitary adenoma, suprasellar meningioma, pineal gland, metastasis • Infiltration – Fe, Sarcoid, Histiocytosis X • • • Nephrogenic (NDI) X-linked recessive Hypokalemia Hypercalcemia (2° to HPT in particular) Renal disease: after ATN, postobstructive uropathy, RAS, renal transplant, amyloid, Sickle cell anemia Sjogren’s Drugs: – Lithium, 20% of chronic users – Demeclocycline, amphotericin, colchicine
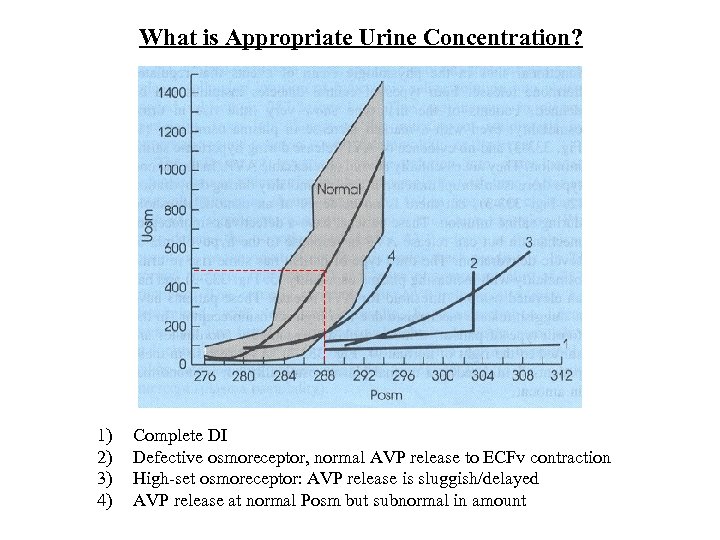 What is Appropriate Urine Concentration? 1) 2) 3) 4) Complete DI Defective osmoreceptor, normal AVP release to ECFv contraction High-set osmoreceptor: AVP release is sluggish/delayed AVP release at normal Posm but subnormal in amount
What is Appropriate Urine Concentration? 1) 2) 3) 4) Complete DI Defective osmoreceptor, normal AVP release to ECFv contraction High-set osmoreceptor: AVP release is sluggish/delayed AVP release at normal Posm but subnormal in amount
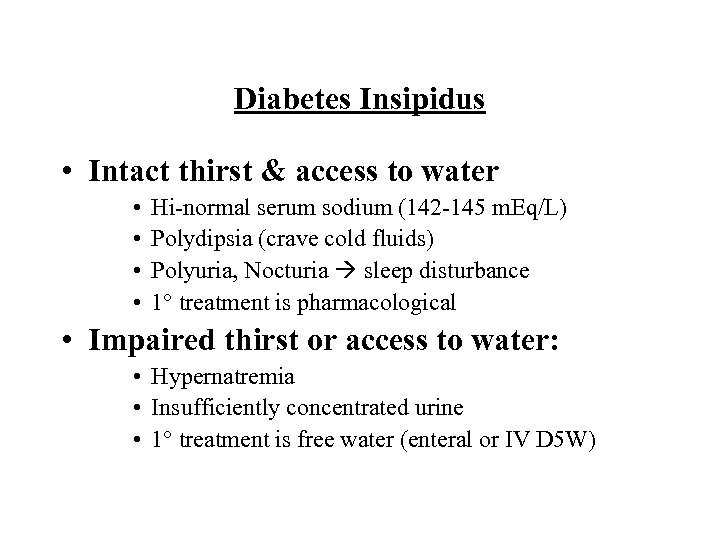 Diabetes Insipidus • Intact thirst & access to water • • Hi-normal serum sodium (142 -145 m. Eq/L) Polydipsia (crave cold fluids) Polyuria, Nocturia sleep disturbance 1° treatment is pharmacological • Impaired thirst or access to water: • Hypernatremia • Insufficiently concentrated urine • 1° treatment is free water (enteral or IV D 5 W)
Diabetes Insipidus • Intact thirst & access to water • • Hi-normal serum sodium (142 -145 m. Eq/L) Polydipsia (crave cold fluids) Polyuria, Nocturia sleep disturbance 1° treatment is pharmacological • Impaired thirst or access to water: • Hypernatremia • Insufficiently concentrated urine • 1° treatment is free water (enteral or IV D 5 W)
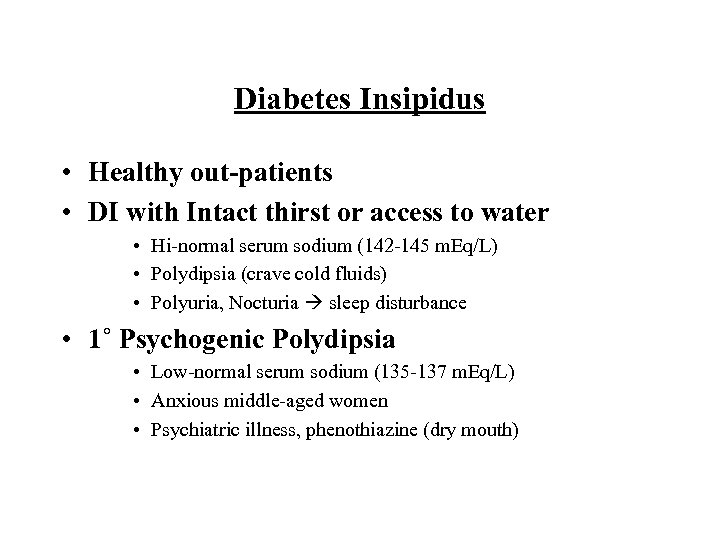 Diabetes Insipidus • Healthy out-patients • DI with Intact thirst or access to water • Hi-normal serum sodium (142 -145 m. Eq/L) • Polydipsia (crave cold fluids) • Polyuria, Nocturia sleep disturbance • 1˚ Psychogenic Polydipsia • Low-normal serum sodium (135 -137 m. Eq/L) • Anxious middle-aged women • Psychiatric illness, phenothiazine (dry mouth)
Diabetes Insipidus • Healthy out-patients • DI with Intact thirst or access to water • Hi-normal serum sodium (142 -145 m. Eq/L) • Polydipsia (crave cold fluids) • Polyuria, Nocturia sleep disturbance • 1˚ Psychogenic Polydipsia • Low-normal serum sodium (135 -137 m. Eq/L) • Anxious middle-aged women • Psychiatric illness, phenothiazine (dry mouth)
 1˚ Polydipsia
1˚ Polydipsia
 1˚ Polydipsia: “What came first? ” The Polyuria or the Polydipsia? The Chicken or the Egg? (Egg)
1˚ Polydipsia: “What came first? ” The Polyuria or the Polydipsia? The Chicken or the Egg? (Egg)
 Water Deprivation Test • Hold water intake for 2 -3 h prior to coming in. • Continue to hold water & Monitor: • Urine volume, UOSM q 1 h • Serum Na, OSM q 2 h • If serum OSM/sodium do not rise above normal ranges & UOSM reaches 600 1˚ Polydipsia • If serum OSM reaches 295 -300 m. M & UOSM doesn’t ↑ • Diabetes Insipidus established • Endogenous ADH should be maximal, check serum ADH – 2 green rubber stopper tubes, pre-chilled, on ice, need biochemist • Give DDAVP 10 ug IN – CDI: UOSM ↑ by 100 -800% (complete CDI), ↑ by 15 -50% (partial CDI) with absolute UOSM > 345 m. M – NDI: UOSM ↑ by up to < 9%, sometimes ↑ as high as 45% but absolute UOSM always < isotonic (290 m. M)
Water Deprivation Test • Hold water intake for 2 -3 h prior to coming in. • Continue to hold water & Monitor: • Urine volume, UOSM q 1 h • Serum Na, OSM q 2 h • If serum OSM/sodium do not rise above normal ranges & UOSM reaches 600 1˚ Polydipsia • If serum OSM reaches 295 -300 m. M & UOSM doesn’t ↑ • Diabetes Insipidus established • Endogenous ADH should be maximal, check serum ADH – 2 green rubber stopper tubes, pre-chilled, on ice, need biochemist • Give DDAVP 10 ug IN – CDI: UOSM ↑ by 100 -800% (complete CDI), ↑ by 15 -50% (partial CDI) with absolute UOSM > 345 m. M – NDI: UOSM ↑ by up to < 9%, sometimes ↑ as high as 45% but absolute UOSM always < isotonic (290 m. M)
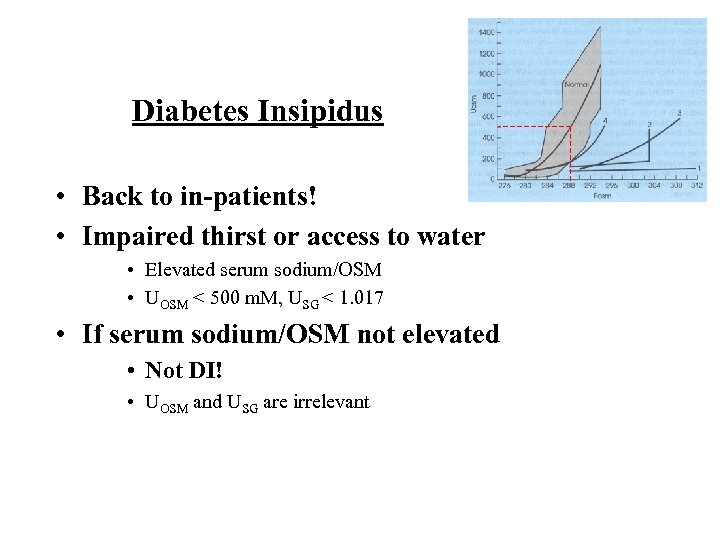 Diabetes Insipidus • Back to in-patients! • Impaired thirst or access to water • Elevated serum sodium/OSM • UOSM < 500 m. M, USG < 1. 017 • If serum sodium/OSM not elevated • Not DI! • UOSM and USG are irrelevant
Diabetes Insipidus • Back to in-patients! • Impaired thirst or access to water • Elevated serum sodium/OSM • UOSM < 500 m. M, USG < 1. 017 • If serum sodium/OSM not elevated • Not DI! • UOSM and USG are irrelevant
 Pituitary Surgery • Triphasic response to surgery • Phase 1: DI • Axonal injury 2° surgery/swelling • Begins after POD #1 (pre-existing DI can occur earlier) • Lasts 1 -5 d • Phase 2: SIADH • Axonal necrosis of AVP secreting neurons with uncontrolled AVP release • Lasts 1 -5 days • Phase 3: DI • Axonal death with cessation of AVP production • Usually permanent
Pituitary Surgery • Triphasic response to surgery • Phase 1: DI • Axonal injury 2° surgery/swelling • Begins after POD #1 (pre-existing DI can occur earlier) • Lasts 1 -5 d • Phase 2: SIADH • Axonal necrosis of AVP secreting neurons with uncontrolled AVP release • Lasts 1 -5 days • Phase 3: DI • Axonal death with cessation of AVP production • Usually permanent
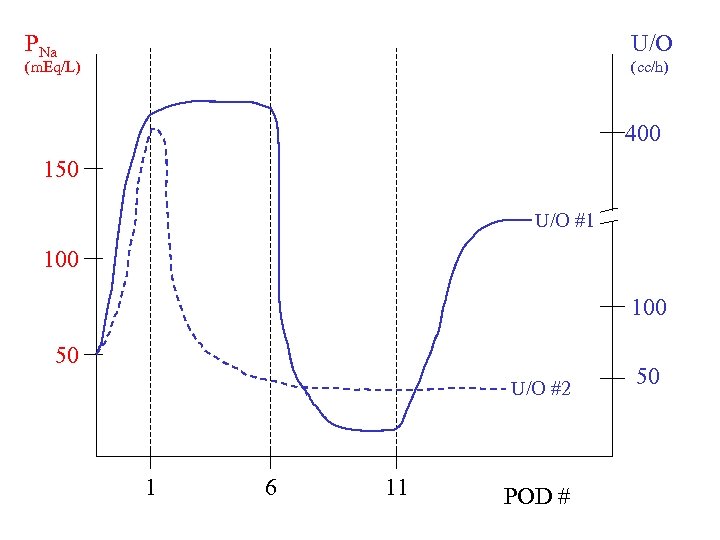 PNa U/O (m. Eq/L) (cc/h) 400 150 U/O #1 100 50 U/O #2 1 6 11 POD # 50
PNa U/O (m. Eq/L) (cc/h) 400 150 U/O #1 100 50 U/O #2 1 6 11 POD # 50
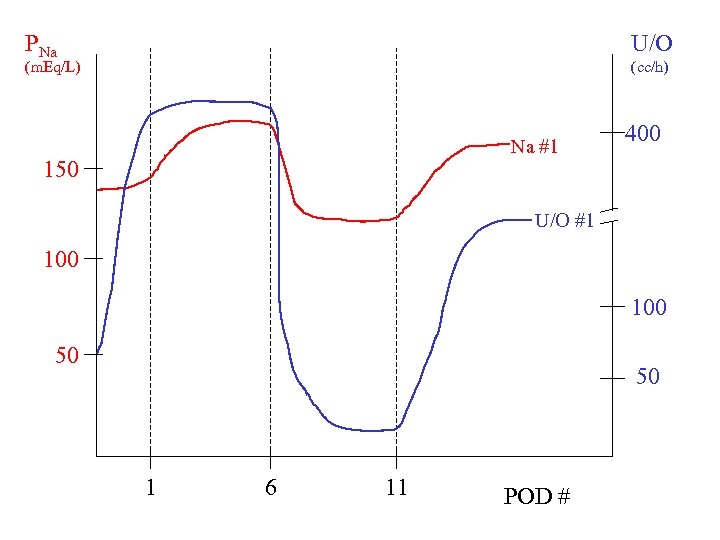 PNa U/O (m. Eq/L) (cc/h) Na #1 150 400 U/O #1 100 50 50 1 6 11 POD #
PNa U/O (m. Eq/L) (cc/h) Na #1 150 400 U/O #1 100 50 50 1 6 11 POD #
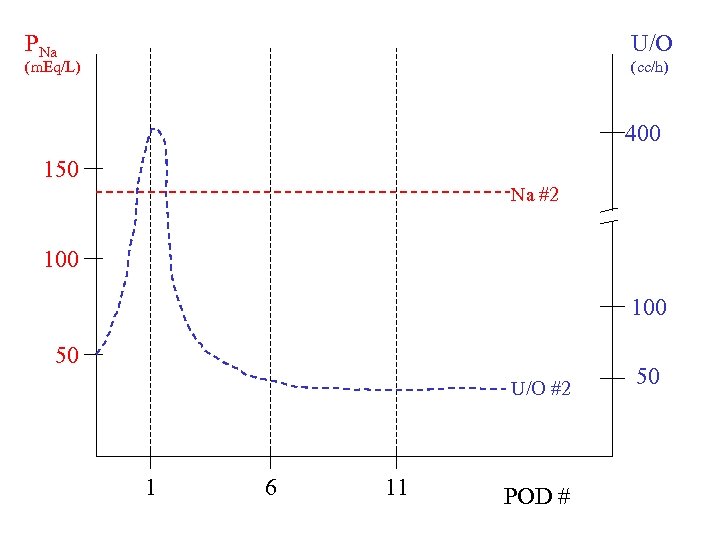 PNa U/O (m. Eq/L) (cc/h) 400 150 Na #2 100 50 U/O #2 1 6 11 POD # 50
PNa U/O (m. Eq/L) (cc/h) 400 150 Na #2 100 50 U/O #2 1 6 11 POD # 50
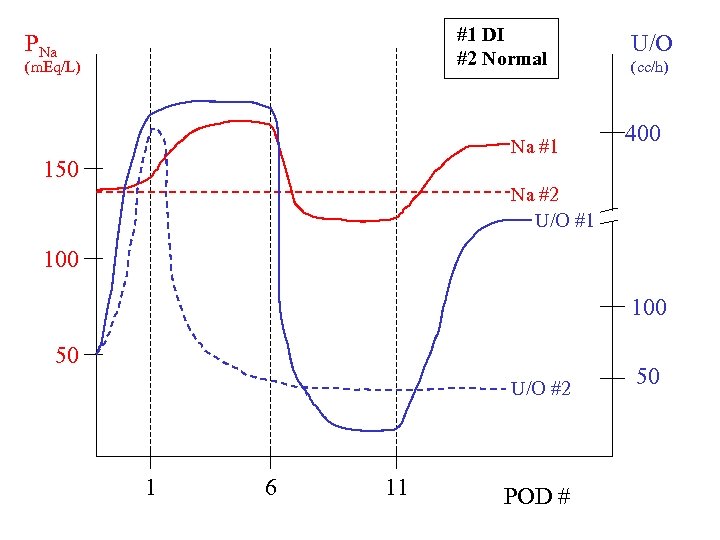 #1 DI #2 Normal PNa (m. Eq/L) Na #1 150 U/O (cc/h) 400 Na #2 U/O #1 100 50 U/O #2 1 6 11 POD # 50
#1 DI #2 Normal PNa (m. Eq/L) Na #1 150 U/O (cc/h) 400 Na #2 U/O #1 100 50 U/O #2 1 6 11 POD # 50
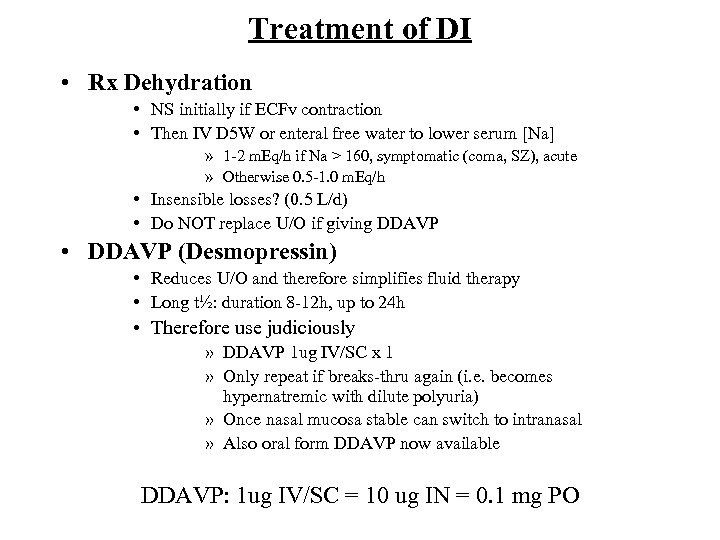 Treatment of DI • Rx Dehydration • NS initially if ECFv contraction • Then IV D 5 W or enteral free water to lower serum [Na] » 1 -2 m. Eq/h if Na > 160, symptomatic (coma, SZ), acute » Otherwise 0. 5 -1. 0 m. Eq/h • Insensible losses? (0. 5 L/d) • Do NOT replace U/O if giving DDAVP • DDAVP (Desmopressin) • Reduces U/O and therefore simplifies fluid therapy • Long t½: duration 8 -12 h, up to 24 h • Therefore use judiciously » DDAVP 1 ug IV/SC x 1 » Only repeat if breaks-thru again (i. e. becomes hypernatremic with dilute polyuria) » Once nasal mucosa stable can switch to intranasal » Also oral form DDAVP now available DDAVP: 1 ug IV/SC = 10 ug IN = 0. 1 mg PO
Treatment of DI • Rx Dehydration • NS initially if ECFv contraction • Then IV D 5 W or enteral free water to lower serum [Na] » 1 -2 m. Eq/h if Na > 160, symptomatic (coma, SZ), acute » Otherwise 0. 5 -1. 0 m. Eq/h • Insensible losses? (0. 5 L/d) • Do NOT replace U/O if giving DDAVP • DDAVP (Desmopressin) • Reduces U/O and therefore simplifies fluid therapy • Long t½: duration 8 -12 h, up to 24 h • Therefore use judiciously » DDAVP 1 ug IV/SC x 1 » Only repeat if breaks-thru again (i. e. becomes hypernatremic with dilute polyuria) » Once nasal mucosa stable can switch to intranasal » Also oral form DDAVP now available DDAVP: 1 ug IV/SC = 10 ug IN = 0. 1 mg PO
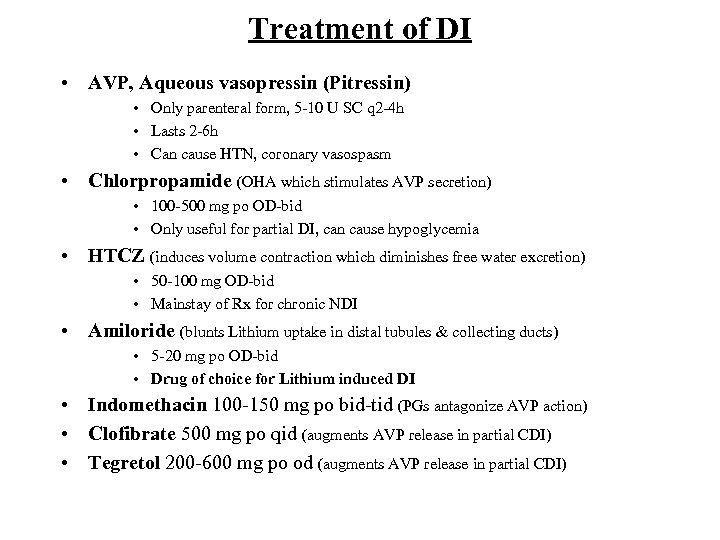 Treatment of DI • AVP, Aqueous vasopressin (Pitressin) • Only parenteral form, 5 -10 U SC q 2 -4 h • Lasts 2 -6 h • Can cause HTN, coronary vasospasm • Chlorpropamide (OHA which stimulates AVP secretion) • 100 -500 mg po OD-bid • Only useful for partial DI, can cause hypoglycemia • HTCZ (induces volume contraction which diminishes free water excretion) • 50 -100 mg OD-bid • Mainstay of Rx for chronic NDI • Amiloride (blunts Lithium uptake in distal tubules & collecting ducts) • 5 -20 mg po OD-bid • Drug of choice for Lithium induced DI • Indomethacin 100 -150 mg po bid-tid (PGs antagonize AVP action) • Clofibrate 500 mg po qid (augments AVP release in partial CDI) • Tegretol 200 -600 mg po od (augments AVP release in partial CDI)
Treatment of DI • AVP, Aqueous vasopressin (Pitressin) • Only parenteral form, 5 -10 U SC q 2 -4 h • Lasts 2 -6 h • Can cause HTN, coronary vasospasm • Chlorpropamide (OHA which stimulates AVP secretion) • 100 -500 mg po OD-bid • Only useful for partial DI, can cause hypoglycemia • HTCZ (induces volume contraction which diminishes free water excretion) • 50 -100 mg OD-bid • Mainstay of Rx for chronic NDI • Amiloride (blunts Lithium uptake in distal tubules & collecting ducts) • 5 -20 mg po OD-bid • Drug of choice for Lithium induced DI • Indomethacin 100 -150 mg po bid-tid (PGs antagonize AVP action) • Clofibrate 500 mg po qid (augments AVP release in partial CDI) • Tegretol 200 -600 mg po od (augments AVP release in partial CDI)


